Introduction
In the clinical setting, metastatic tumors that
translocate from the primary tumor site to the central nervous
system are the most frequently occurring intracranial tumors
(1). Three methods, including
stereotactic radiosurgery, general surgery and whole-brain
radiation therapy (WBRT), are normally clinically used and are
relatively effective for treating brain metastases (1). However, for a long time, none of these
methods was assigned as the standard therapy in clinical practice.
The median survival time of affected patients is 1–3 months without
therapy (1). The median survival time
increases to ~6 months after WBRT (2)
and to 10 months subsequent to using the Gamma Knife radiosurgery
(GKRS) method (3). The survival time
has been recorded as 12 months in patients who underwent surgery
(prior method) and WBRT (4). With
each of the latter methods, the patients only suffered from single
brain metastasis, however, when using the GKRS and WBRT combined
method for multiple brain metastases, a survival time of >1 year
can also be obtained (5). Recently,
the radiosurgery method has become a focal topic in the area of
brain tumor metastases, and more advantages have been demonstrated
when compared to tumor resection. Radiosurgery has been applied in
multiple metastatic lesions and in metastases in deep locations,
with satisfactory outcomes (6).
Radiosurgery can also be used for patients with other major medical
issues considered as contraindications for general anesthesia and
surgery (6). In particular,
radiosurgery and stereotactic surgery can be combined to complete
treatment; as these two treatment methods are based on the same
technology platform, a number of the patients with cystic
metastases can avoid craniotomy.
Due to cystic components, a number of brain
metastases are characterized by a large volume. The clearance of
this cystic component is critical for the surgical removal of the
tumor. However, certain factors could affect the effects of the
surgery, including tumor multiplicity, patient functional status
and lesion location. Due to the large volume of the tumor, the
radiosurgery method is not suitable for cystic metastatic tumors.
In order to treat such lesions using the radiosurgery method, it is
critical to decrease the cystic component volume. Stereotactic cyst
aspiration, a minimally invasive surgical approach can overcome
these shortcomings, and is not affected by the location of the
lesion, the number of lesions or the patient status (6). Following stereotactic aspiration of the
cystic component, the present study evaluated the clinical outcomes
and efficacy of the GKRS method for the treatment of cystic brain
metastases by assessing the tumor volume.
Materials and methods
Patients
A total of 48 patients diagnosed with large cystic
brain metastases between January 2008 and December 2012 were
involved in this study of GKRS. All patients were diagnosed with
single large cystic brain metastases. Furthermore, the primary
malignancy was determined for each patient, and no patient had a
malignancy of unknown primary site. The pathological results are
listed in Table I. Samples were
obtained as previously described (6).
Consequently, the patients also underwent magnetic resonance
imaging (MRI) to diagnose the brain metastases. The present study
was approved by the Ethics Committee of the Southern Medical
University (Guangzhou, China). Informed consent was obtained from
all patients.
 | Table I.Basic data and clinical
characteristics of the 48 study patients. |
Table I.
Basic data and clinical
characteristics of the 48 study patients.
| Characteristics | Patients, n (%) |
|---|
| Age, years |
|
|
<60 | 15 (31.3) |
|
>60 | 33 (68.8) |
| Gender |
|
| Male | 28 (58.3) |
|
Female | 20 (41.7) |
| Initial symptom |
|
| Motor
weakness | 25 (52.1) |
|
Headaches | 14 (29.2) |
| Gait
disturbance | 6
(12.5) |
| Visual
disturbance | 2 (4.2) |
|
Seizure | 1 (2.1) |
| Primary tumor |
|
| Non-small
cell lung cancer | 29 (60.4) |
| Small
cell lung cancer | 6
(12.5) |
| Breast
cancer | 5
(10.4) |
| Colon and
rectal cancer | 4 (8.3) |
|
Esophageal cancer | 2 (4.2) |
| Kidney
cancer | 1 (2.1) |
| Malignant
melanoma | 1 (2.1) |
| Number of
metastases |
|
| 1 | 18 (37.5) |
| 2 | 10 (20.8) |
| 3 | 13 (27.1) |
| 4 | 7
(14.6) |
| KPS score |
|
| 50 | 3 (6.3) |
| 60 | 8
(16.7) |
| 70 | 21 (43.8) |
| 80 | 12 (25.0) |
| 90 | 4 (8.3) |
The 48 patients included 28 males and 20 females,
with a mean age of 61.4 years old (range, 33–78 years). In this
study, the primary tumors consisted of small cell lung cancer (6
patients, 12.5%), non-small cell lung cancer (29 patients, 60.4%),
breast cancer (5 patients, 10.4%), esophageal cancer (2 patients,
4.2%), colon and rectal cancer (4 patients, 8.3%), and kidney
cancer (1 patients, 2.1%). The initial symptoms of brain metastasis
included headaches (25 patients, 52.1%), seizures (1 patient,
2.1%), motor weakness (14 patients, 29.2%), visual disturbance (2
patients, 4.2%) and gait disturbance (6 patients, 12.5%). The
average number of brain metastases was 2.4 (range, 1–7). The mean
Karnofsky performance status (KPS) score was 71.3 (range, 50–90)
(5). The basic data and
characteristics of the patients are listed in Table I.
MRI
After positioning the stereotactic frame (Leksell G
frame; Elekta AB, Stockholm, Sweden), MRI was performed using the
vantage Titan 3T MRI machine (Toshiba, Japan). The MR T1-weighted
images with gadolinium contrast were recorded and analyzed.
Meanwhile, the slices were also reconstructed in the axial plane
every 3 mm. The Leksell SurgiPlan system (Elekta AB) was applied to
regulate the surgical trajectory. The stereotactic aspiration of
the large cystic brain metastases was performed and recorded in the
operating room. The findings showed that the mean tumor volume was
26.8 cc (range, 19.0–75.7 cc) and the aspiration fluid volume was
~80% of the cyst volume. For the prevention of tumor hemorrhages,
18 lesions (37.5%) with a tumor volume >40 ml were treated with
drainage tube insertion for 24 h following the stereotactic
aspiration. It was confirmed that all of the patients presented
with a markedly reduced cyst volume after the stereotactic
drainage.
A second set of MR images was recorded after cystic
drainage. At the same time, the drainage tube was closed until the
end of Gamma Knife treatment. The Leksell GammaPlan system (Elekta
AB) was used to plan the GKRS. For the GKRS method, the mean tumor
volume was decreased from 26.8 cc (range, 19.0–75.7 cc) to 5.4 cc
(range, 1.0–16.0 cc). The average prescribed radiation dose to the
tumor margin was 18 Gy (range, 14–20 Gy). Ten cases with a tumor
volume of <40 cc underwent exposure to 18 Gy for 20 min. The
other 8 patients underwent exposure to 16 Gy for 20 min Prior to
pulling out the drainage tube, the patients were administered
supplement colloidal phosphorus-32 radiation therapy (0.01 mCi/ml).
This method is often used in the treatment of cystic
craniopharyngioma (7). In this study,
the GKRS was also applied to other areas of the brain, in which,
however, no the large cysts were observed.
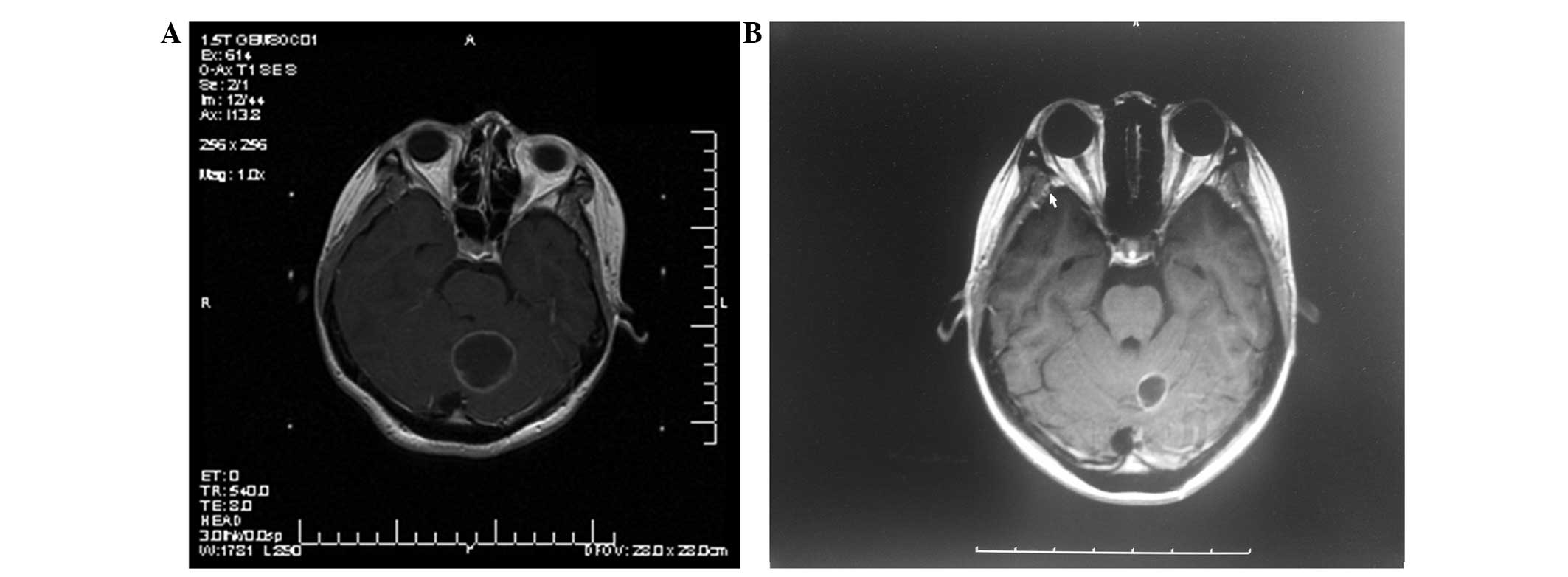
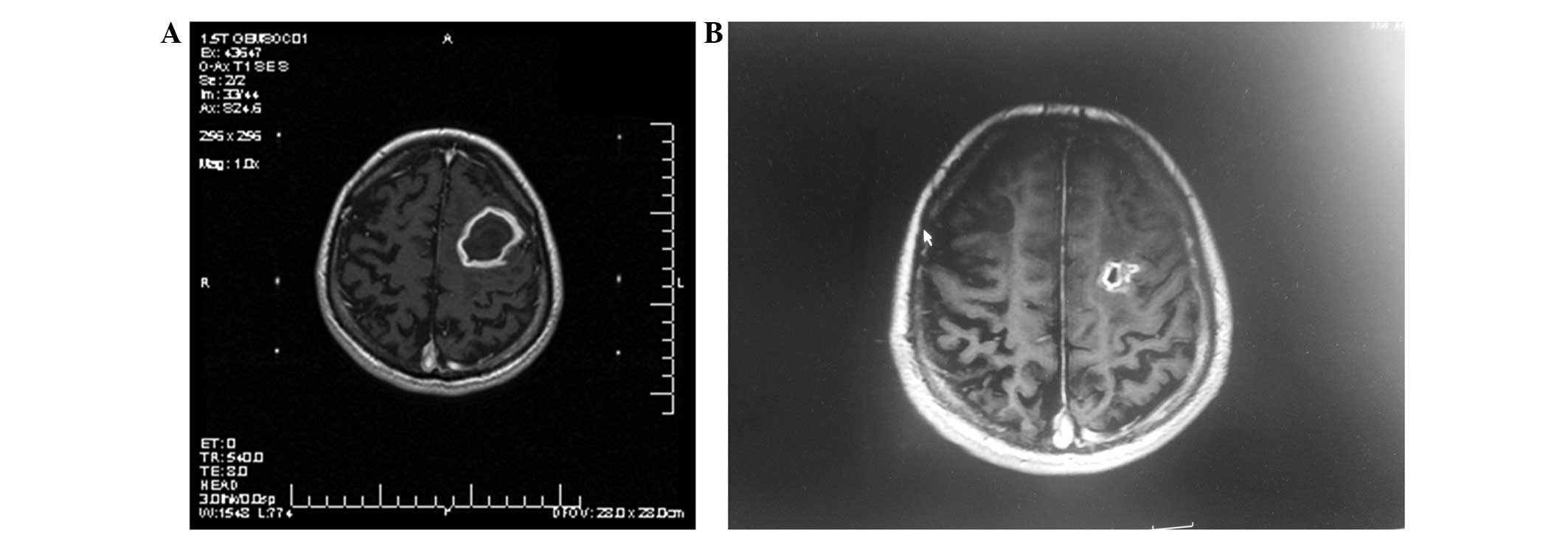
MRI was performed again after an interval of 3
months (Figs. 1 and 2). Tumor control was represented as a
decrease in the tumor size following treatment. Progression of the
local tumor was represented as an increase in size of the
previously treated tumor. Moreover, the progression of the remote
tumor was represented as the appearance of new brain
metastases.
Results
Subsequent to surgery, there was no bleeding,
infection complications or surgical mortality. All the
post-operative clinical symptoms showed improvement at 1 week
post-surgery and the mean KPS score was 90. MRI enhanced scanning
of the head after 3 months showed tumor control, with tumor
shrinkage or disappearance, and significant reduction of the edema
around the tumor in 44 cases (91.7%), while local tumor
progression, with no radioactive brain necrosis, occurred in 4
cases (8.3%). The 10 patients who underwent phosphorus-32
radiotherapy also exhibited no radioactive brain edema. Of the 8
cases (16.7%) that exhibited remote tumor progression, 4 (8.3%)
received WBRT and 3 cases (6.3%) received chemotherapy. The mean
follow-up time of the patients was 36.2 months (range, 24–72
months). A total of 12 cases (25.0%) remained alive and 36 patients
(75.0%) succumbed during the follow-up period. Whereas only 4
patients (8.3%) succumbed to brain metastasis progression, 2
patients (4.2%) succumbed due to unrelated other diseases and 30
patients (62.5%) succumbed due to primary cancer progression. The
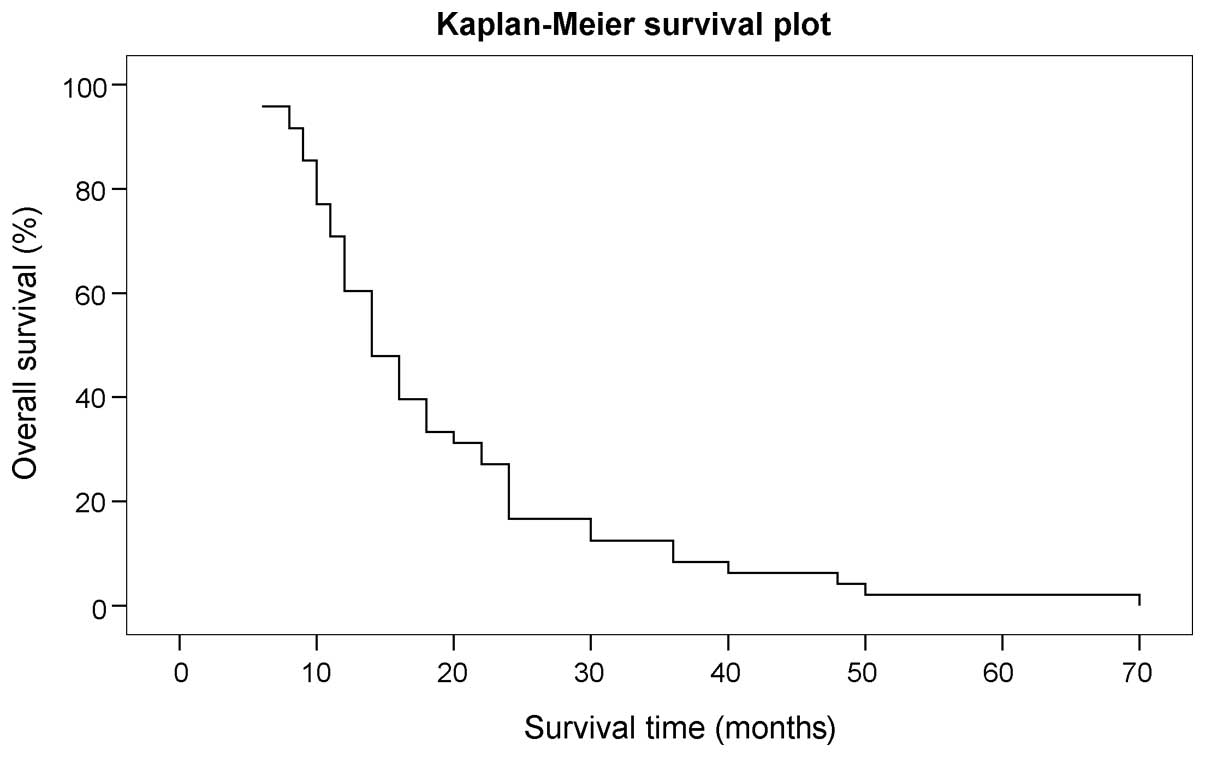
overall median survival time of the patients following the GKRS
treatment was 19.5 months (range, 6–70 months), while the 1-year
survival rate was 70.8% and the 2-year survival rate was 26.2%
(Fig. 3). Furthermore, the mean KPS
score of the patients was 97.7 (range, 80–100).
Discussion
Metastatic brain tumors are normally composed of
cystic components, however, the reasons for the cyst formation have
not been clearly investigated (8).
Stem (9) reported that the brain cyst
fluid protein always presents in the inflammatory exudates. Cumings
(10) also reported that the cyst
fluid formation may be correlated with the tumor degeneration.
Gardner et al (11) found that
fluid accumulating in brain tumors runs in the normal drainage
route, since there are no lymphatic vessels in the tumors.
Conventionally, in the clinic, the presence of a large, single,
cystic brain tumor is considered as an effective indication for
surgery (6). A study by Yoshida and
Morii (12) reported rapid
neurological symptom relief for these large cystic lesions after
surgery. However, surgery cannot treat deep lesions within the
brain, and may cause severe neurologic outcomes. Moreover, surgical
procedures are not safe for patient's with a poor general
condition, as well as being ineffective for those individuals with
multiple lesions. More recently, the stereotactic radiosurgical
procedure and the GKRS procedure have been combined and applied to
cerebral metastatic disease (13).
This method has proved to be valuable due to its minimal
invasiveness, which leads to a decreased hospitalization time and
lower hospital cost. This method could also result in a low
associated tumor morbidity and an excellent local tumor control
rate (14,15). The results for the GKRS method in
tumor patients with multiple or solitary lesions have been reported
to be an improvement on those of other previously reported methods
(16).
Radiosurgery is not always applicable for large
cystic brain metastases. Pan et al (17) reported that GKRS alone could not
control the large cystic components (>10 ml) effectively. When
applied to the solid component of the tumor, the combination of
stereotactic cyst aspiration and GKRS resulted in a good outcome,
with a 1-year survival rate of 60%. A study by Franzin et al
(6) also indicated that ~39.1%
patients did not experience remote or local tumor progression, that
26.3% of patients succumbed from neurological progression and that
the overall median survival was 15 months when stereotactic
drainage and GKRS were applied for the treatment of cystic brain
metastases. In the present study, 91.7% of patients showed marked
tumor inhibition, the overall median survival time was 19.5 months
and only 8.3% patients succumbed from brain metastasis progression
post-treatment. We hypothesize that this result may be associated
with the higher dose exposure to the tumor; phosphorus-32
compensated for the inadequacy of the Gamma Knife exposure dose for
the larger lesions. Following the resection of single brain
metastases, Tendulkar et al (18) reported that the median patient
survival time was 10.6 months. Hong et al (19) found that when surgical resection was
performed in NSCLC patients with multiple brain metastases, the
median survival time was 10.8 months. Faguer et al (20) reported the use of radiosurgery
delivered to the tumor bed for 22 patients with metastases. The
overall median survival time of the patients was 13 months compared
with 11 months for the patients who received WBRT; however, this
difference was not significant.
It is difficult to completely remove tumors if they
are distributed in deep locations or eloquent areas, or if they
have a large cystic volume (5). In
these situations, the GKRS method combined with stereotactic cyst
aspiration could be a better modality compared with surgical
resection, as a number of patients are too weak to undergo general
anesthesia. Such findings further confirm the efficacy of the GKRS
method when combined with stereotactic cyst aspiration for the
treatment of unresectable cystic brain metastases in the
clinic.
There are certain complications associated with
brain tumors, including seizures, neurosurgical deficits,
hemorrhage and infection. However, the mortality rate of patients
in certain large series has been recorded at <1%, and the
complication rates even increase from 0 to 7% following specific
treatments (21). The complications
of stereotactic radiosurgery are always associated with the
proximity of structures and the radiation to the brain (5). There are also a number of associated
early complications, including worsening neurological deficits and
seizures, however, these are rare (6). A few patients also exhibit mild
transitory symptoms, such as nausea, headaches and dizziness.
Complications in the late stage (6 to 9 months after the procedure)
may also be observed, including trigeminal neuropathy, facial palsy
and visual symptoms (5,6). However, Franzin et al (6) found that no acute complications were
observed and that only 7.6% of patients underwent radionecrosis
following treatment with GKRS combined with stereotactic aspiration
for cystic brain metastases. Jung et al (22) reported that stereotactic cyst
aspiration and radiosurgery for cystic brain metastases resulted in
a local control rate of 58.6%; this type of treatment is safe, but
the efficiency is not high. In the present study, 10 cases of
phosphorus-32 radiotherapy patients without radioactive brain
necrosis were also recorded. The main treatment was largely
composed of two stereotactic procedures, consisting of stereotactic
cyst aspiration and GKRS, which is performed by using a single
frame application (23). Therefore,
stereotactic cyst aspiration combined with GKRS could reduce the
hospitalization time and cost, and cause less inconvenience to the
patients.
In conclusion, the cyst aspiration method can
decrease the associated risks of radiation necrosis and
complications, and decrease the tumor volume. The present data
support the application and safety of the combined stereotactic
cyst aspiration and GKRS method, which was effective for patients
with large, single, cystic brain metastases. The method is
particularly useful for patients whose overall condition is poor,
which typically inhibits the use of general anesthesia.
Furthermore, patients with deeply located metastatic lesions or
multiple lesions could also benefit from this treatment.
References
|
1
|
Sun X, Chen Z, Yang W, Yu F, Zhao J, He P
and Wang Z: Rare incidence of a diffuse brain metastatic carcinoma:
A case report. Oncol Lett. 8:1807–1809. 2014.PubMed/NCBI
|
|
2
|
Diener-West M, Dobbins TW, Phillips TL and
Nelson DF: Identification of an optimal subgroup for treatment
evaluation of patients with brain metastases using RTGO study 7916.
Int J Radiat Oncol Bio Phys. 16:669–673. 1989. View Article : Google Scholar
|
|
3
|
Andrews DW, Scott CB, Sperduto PW,
Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J,
Bahary JP, et al: Whole brain radiation therapy with or without
stereotactic radiosurgery boost for patients with one to three
brain metastases: Phase III results of the RTGO 9508 randomized
trial. Lancet. 363:1665–1672. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tsao MN, Lioyd N, Wong R, Chow E,
Rakovitch E and Laperriere N: Whole brain radiotherapy for the
treatment of multiple brain metastases. Cochrane Database Syst Rev.
4:CD0038692012.PubMed/NCBI
|
|
5
|
Aoyama H, Shirato H, Tago M, Nakagawa K,
Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H, et al:
Stereotactic radiosurgery plus whole-brain radiation therapy vs.
stereotactic radiosurgery alone for treatment of brain metastases:
A randomized controlled trial. JAMA. 295:2483–2491. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Franzin A, Vimercati A, Picozzi P, Serra
C, Snider S, Gioia L, da Ferrari Passano C, Bolognesi A and
Giovanelli M: Stereotactic drainage and gamma knife radiosurgery of
cystic brain metastasis. J Neurosurg. 109:259–267. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Barriger RB, Chang A, Lo SS, Timmerman RD,
DesRosiers C, Boaz JC and Fakiris AJ: Phosphorus-32 therapy for
cystic craniopharyngiomas. Radiother Oncol. 98:207–212. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim MS, Lee SL and Sim SH: Brain tumors
with cyst treated with gamma knife radiosurgery: Is microsurgery
indicated? Stereotact Funct Neurosurg. 72(Suppl 1): S38–S44. 1999.
View Article : Google Scholar
|
|
9
|
Stem K: Chemical study of fluids obtained
from cerebral cysts: Report on 56 cases. Brain. 62:881939.
View Article : Google Scholar
|
|
10
|
Cumings JN: The chemistry of cerebral
cysts. Brain. 73:244–250. 1950. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gardner WJ, Collis JS and Lewis LA: Cystic
brain tumors and the blood-brain barrier. Comparison of protein
fractions in cyst fluids and sera. Arch Neurol. 8:291–298. 1963.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yoshida S and Morii K: The role of surgery
in the treatment of brain metastasis: A retrospective review. Acta
Neurochir (Wien). 146:767–770. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Higuchi F, Kawamoto S, Abe Y, Kim P and
Ueki K: Effectiveness of a 1-day aspiration plus gamma knife
surgery procedure for metastatic brain tumor with a cystic
component. J Neurosurg. 117(Suppl): S17–S22. 2012.
|
|
14
|
Uchino M, Nagao T, Seiki Y, Shibata I,
Terao H and Kaneko I: Radiosurgery for cystic metastatic brain
tumor. No Shinkei Geka. 28:417–421. 2000.(In Japanese). PubMed/NCBI
|
|
15
|
Mingione V, Oliveira M, Prasar D, Steiner
M and Steiner L: Gamma surgery for melanoma metastases in the
brain. J Neurosurg. 96:544–551. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Flickiner JC: Radiotherapy and
radiosurgical management of brain metastases. Curr Oncol Rep.
3:484–489. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Pan HC, Sheehan J, Stroila M, Steiner M
and Steiner L: Gamma knife radiosurgery for brain metastases from
lung cancer. J Neurosurg. 102(Suppl): S128–S133. 2005. View Article : Google Scholar
|
|
18
|
Tendulkar RD, Liu SW, Barnett GH,
Vogelbaum MA, Toms SA, Jin T and Suh JH: RPA classification has
prognostic significance for surgically resected single brain
metastasis. Int J Radiat Oncol Biol Phys. 66:810–817. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hong N, Yoo H, Gwak HS, Shin SH and Lee
SH: Outcome of surgical resection of symptomatic cerebral lesions
in non-small cell lung cancer patients with multiple brain
metastases. Brain Tumor Res Treat. 1:64–70. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Faguer R, Boissonneau S, Menei P and
Metellus P: Gamma knife radiosurgery to the tumor bed after
resection of brain metastases. Neurochirurgie. 60:3552014.
View Article : Google Scholar
|
|
21
|
Bernstein M and Parrent A: Complication of
CT-guided stereotactic biopsy of intra-axial brain lesions. J
Neurosurg. 81:165–168. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jung TY, Kim IY, Jung S, Jang WY, Moon KS,
Park SJ and Lim SH: Alternative treatment of stereotactic cyst
aspiration and radiosurgery for cystic brain metastases. Stereotact
Funct Neurosurg. 92:234–241. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shen G, Wang YJ, Shen WJ, Zhou ZS, Wang
JL, Sheng HG, Dong DP, Zhou M, Yang G, Wang QW and Zeng Y:
Stereotactic body radiation therapy for centrally-located lung
tumors. Oncol Lett. 7:1292–1296. 2014.PubMed/NCBI
|