Introduction
Myxoinflammatory fibroblastic sarcoma is a rare
neoplasm, accounting for 1% of all adult malignancies (1). The tumor most commonly occurs in the
distal extremities and usually affects males and females equally in
the fourth and fifth decades of life. Myxoinflammatory fibroblastic
sarcomas usually present as a slow-growing painless mass that can
mimic infection, ganglion or benign tumors. Accurate diagnosis is
based on the postoperative pathological result. Wide local excision
is the first choice of treatment. For acral tumors with multiple
recurrences, amputation may be considered. The efficacy of
chemotherapy and radiotherapy remains unclear. Myxoinflammatory
fibroblastic sarcoma is a low-grade sarcoma with a low rate of
mortality and metastasis, demonstrating a long-term clinical
course. However, the local recurrence rate is extremely high
(2).
Tumors that invade the brachial plexus present a
significant challenge as surgical procedures may lead to sensory
disturbance and dyskinesia (2).
In this study, the rare case of large
myxoinflammatory fibroblastic sarcoma with invasion of the brachial
plexus, which that was successfully managed with surgery, is
presented.
Case report
A 54-year-old man, who had suffered from a right
cervicothoracic mass for nearly 16 years and did not obtain any
medical treatment, was referred to the Department of Hand Surgery
(Huashan Hospital, Fudan University, Shanghai, China) in January
2013. The patient presented with a huge mass with no pain and no
sensory or motor dysfunction. The patient previously presented to
Shanghai Changhai Hospital (Shanghai, China) in November 2012.
Magnetic resonance imaging (MRI) and fine-needle aspiration was
performed. Subsequently, the patient was referred from Shanghai
Changhai Hospital to Huashan Hospital.
Physical examination revealed a right
cervicothoracic mass that was palpable from the supraclavicular
fossa to the infraclavicular region. The supraclavicular and
infraclavicular portions of the mass were ~10×5×3 cm and 25×18×8 cm
in size, respectively. On palpation the mass was hard with no
tenderness, clear boundaries and negativity for Tinel's sign. The
active and passive activity of the right upper limb was normal and
no abnormal sensation in the affected limb was reported.
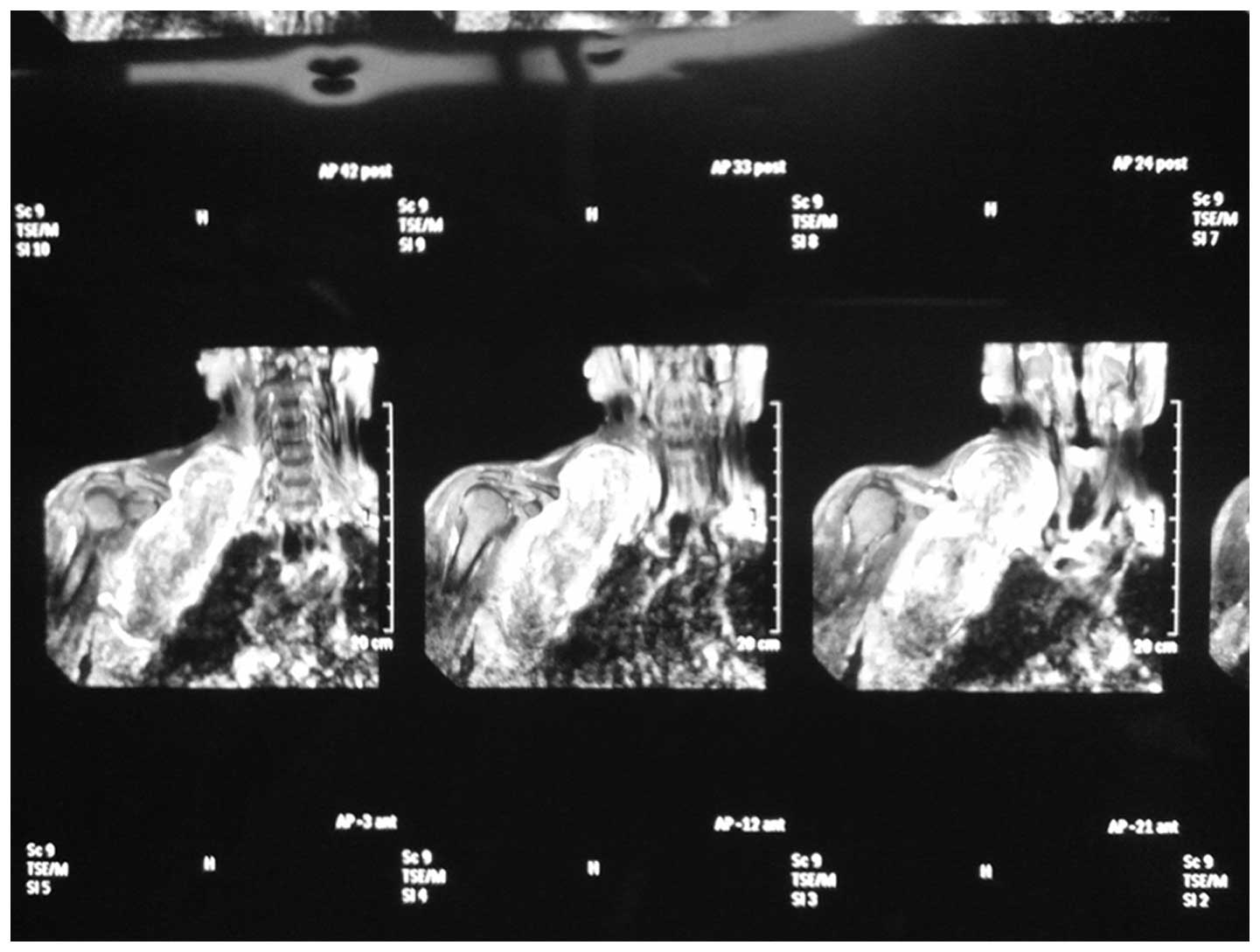
B-ultrasound examination revealed a low echo-level
mass located between the right neck and shoulder, extending from
the right anterior chest wall to the right anterior axillary
region. A chest radiograph identified a dense shadow at the right
clavicular region. MRI revealed a large occupying lesion at the
supraclavicular and infraclavicular region (Fig. 1). A pre-operative pathological
examination performed at Shanghai Changhai Hospital in November
2012 indicated the diagnosis of a benign mesenchymal tumor.
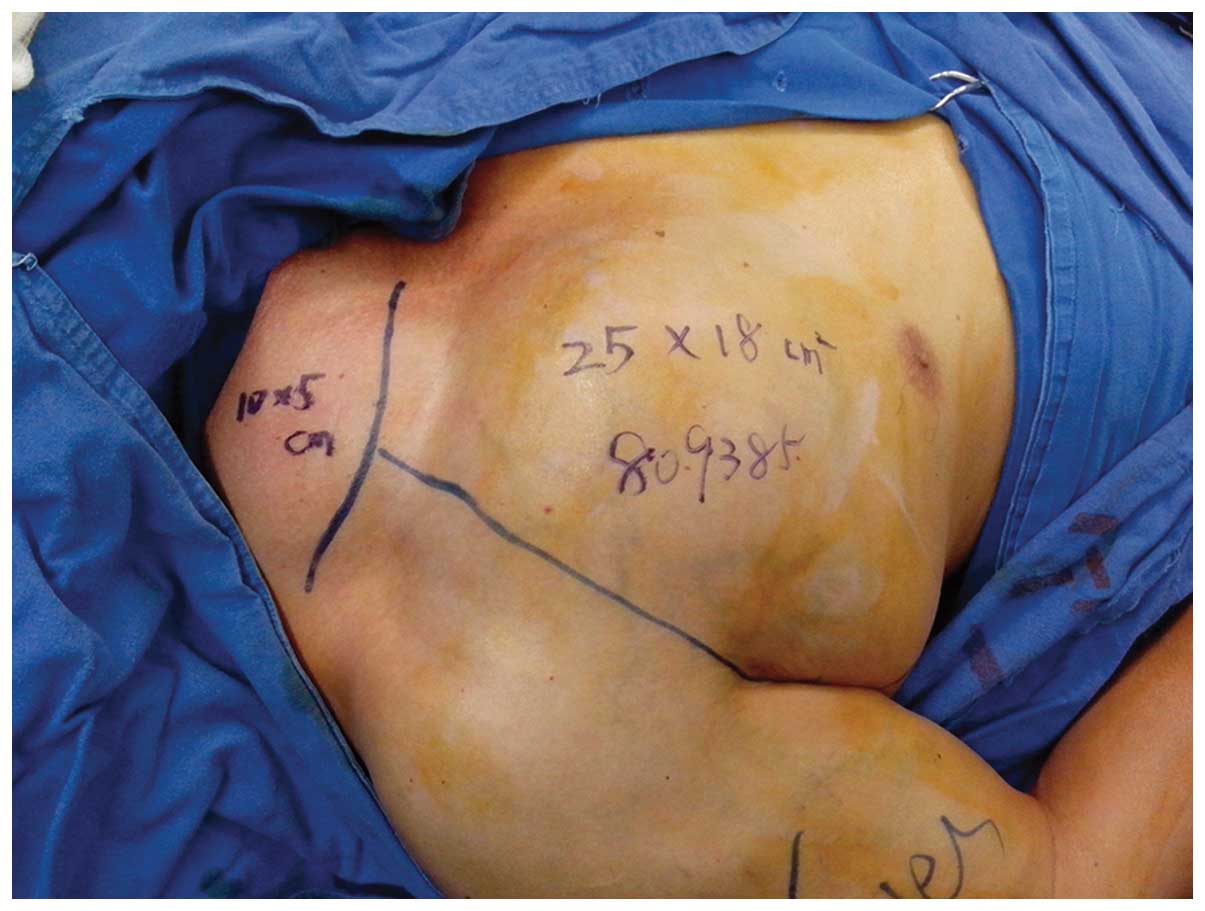
The mass was extremely large, with a supraclavicular
portion measuring 10×5×3 cm and an infraclavicular portion
measuring 25×18×8 cm (Fig. 2). The
mass was exposed via supraclavicular incision and the
supraclavicular portion of the hard mass, measuring 10×5×3 cm, with
clear boundaries and an abundant blood supply, was identified. The
tumor oppressed the brachial plexus and vessels, and could not be
separated by only supraclavicular incision. The mass extended from
the supraclavicle to the infraclavicle and could not be completely
exposed by only supraclavicular incision. An additional incision
from the infraclavicle region to the deltopectoral interval and
midaxillary line was made, and the infraclavicular portion of the
hard mass, sized 25×18×8 cm, with clear boundaries and an abundant
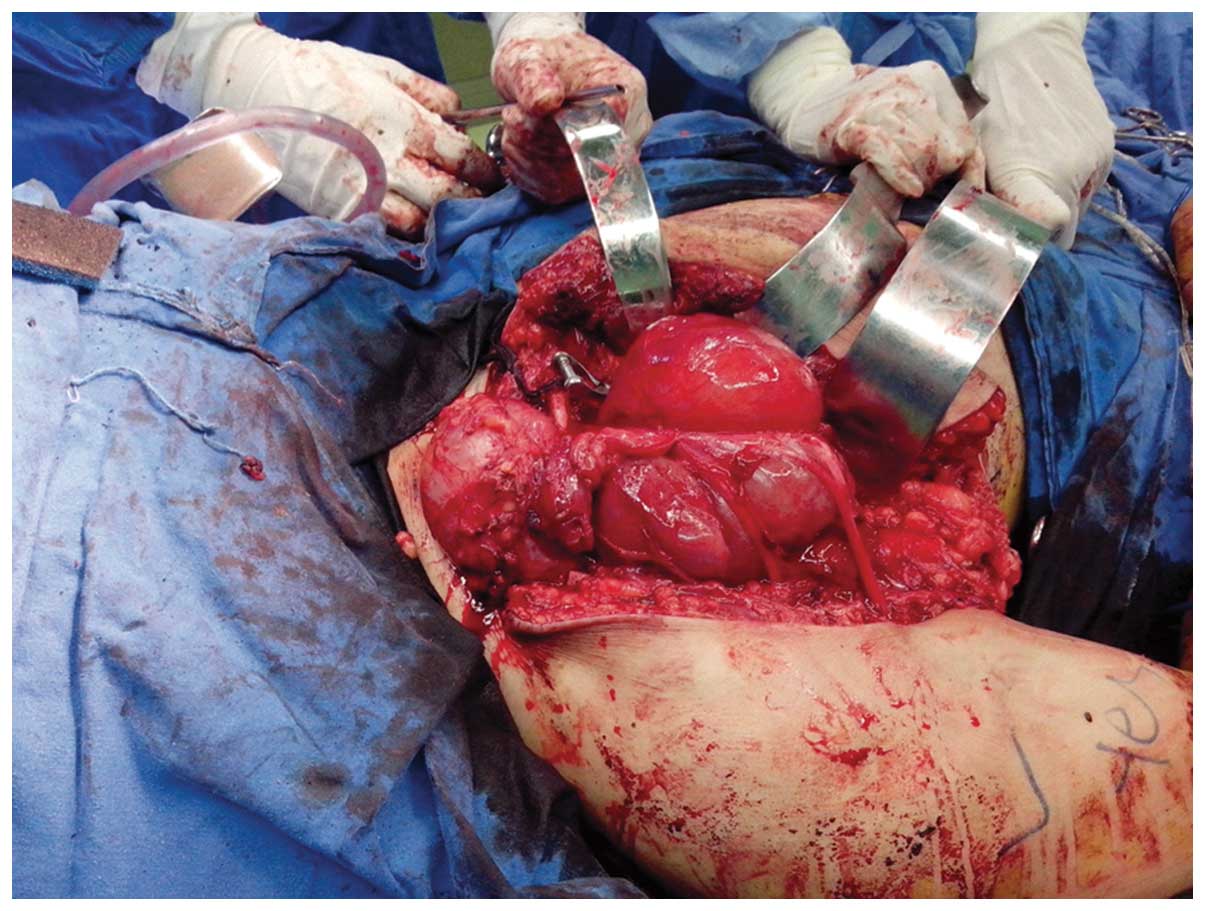
blood supply, was identified. The tumor was lobulated. The mass was
enwrapped and separated by the medial, lateral and posterior cords
and the axillary, musculocutaneus, median and ulnar nerves
(Fig. 3). The mass was evidently
adhered to the aforementioned nerves and could not be easily
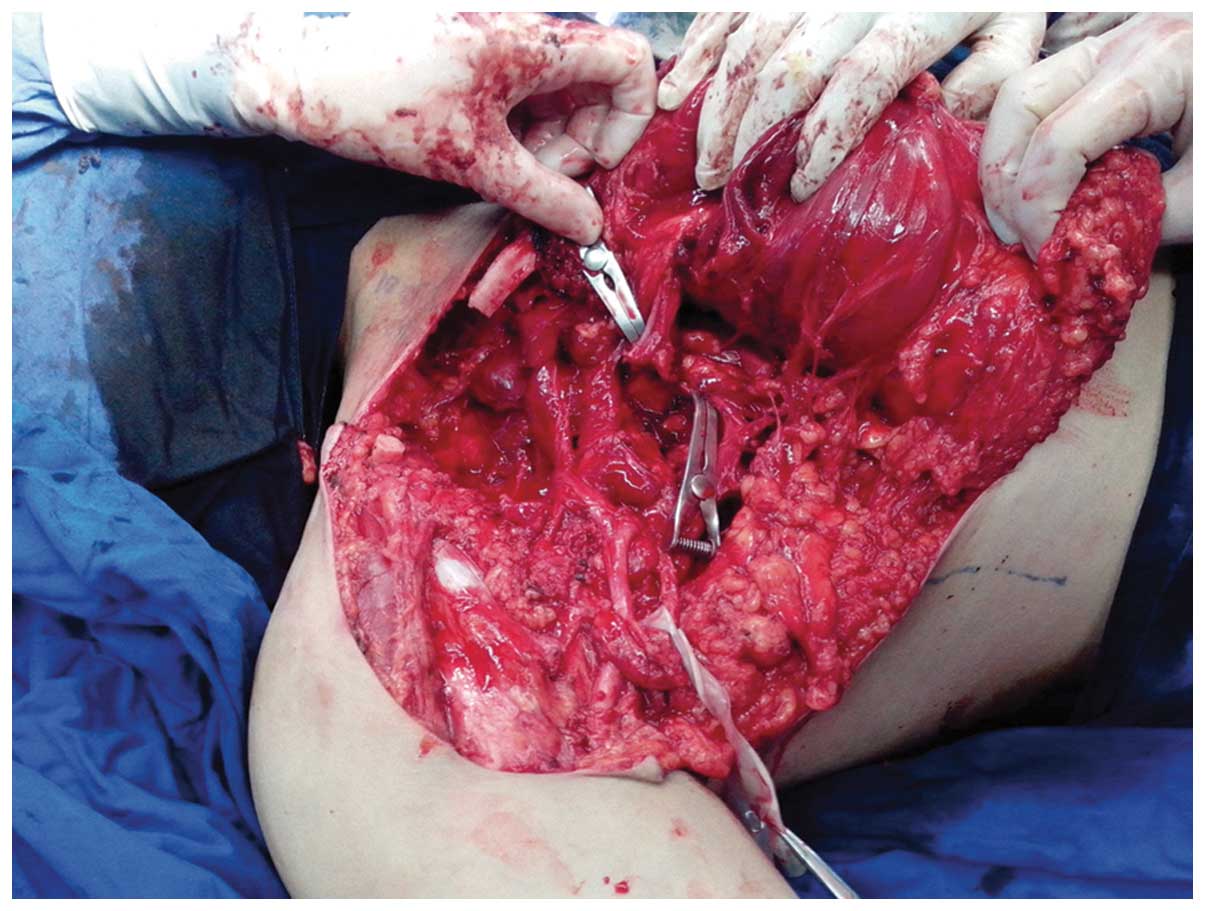
separated. The mass was gradually resected carefully to maintain
the integrity of the nerves (Fig. 4).
Clavicotomy was performed prior to separation of the nerves and
vessels surrounding the mass. Finally, the mass was completely
resected (Fig. 5). Tumor invasion of
the clavicle without bone destruction was observed. Intraoperative
electromyography recorded the somatosensory evoked potential by
stimulating the axillary, musculocutaneus, median, radial and ulnar
nerves. Following surgery, the activity and sensation of the right
upper limb were normal.
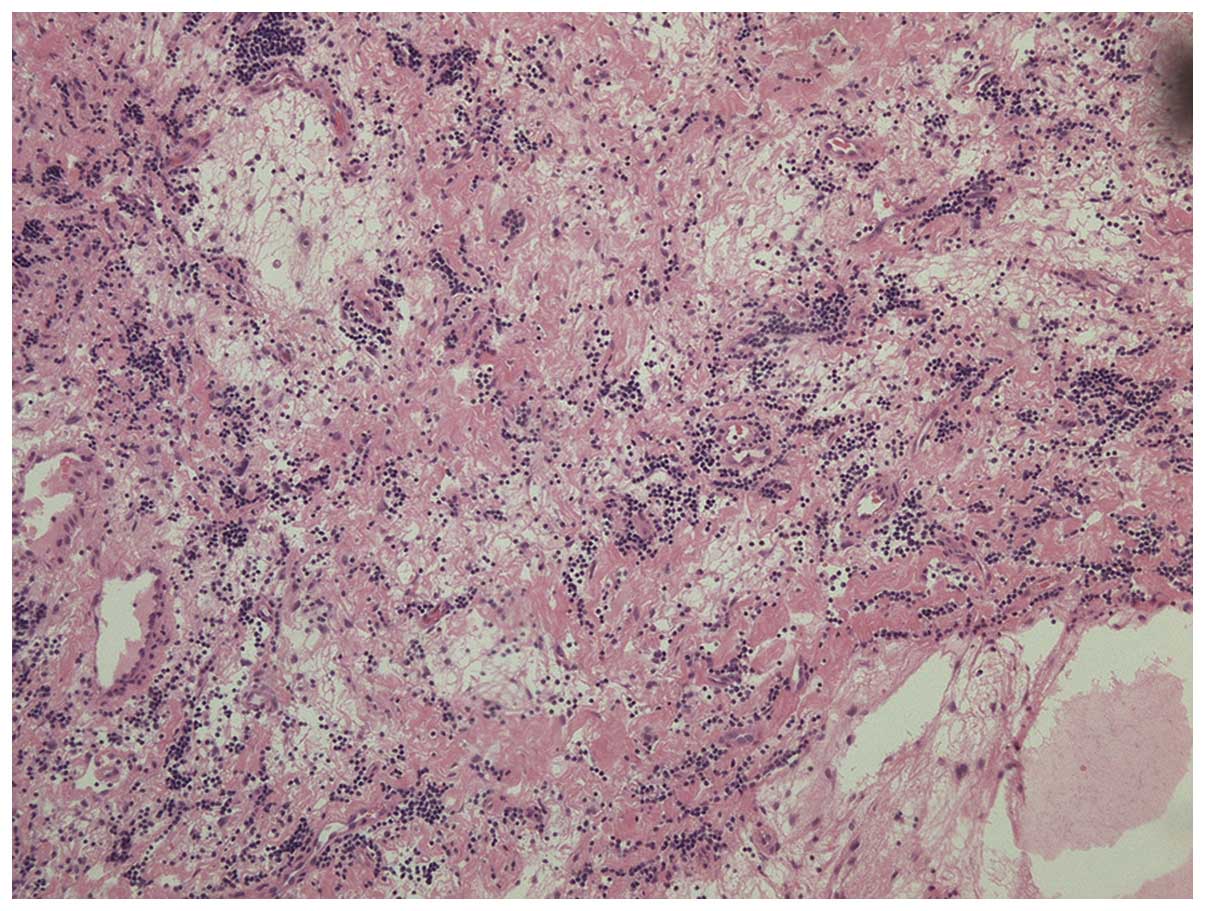
The tissue used for histological analysis was
embedded in paraffin and sectioned. The histological results showed
a prominent mixed inflammatory infiltrate, macrophages, Touton-type
giant cells and myxoid matrix, which confirmed the pathological
diagnosis of myxoinflammatory fibroblastic sarcoma (Fig. 6) (3).
Histopathologically, the lesion demonstrated numerous
poly-morphonuclear leukocytes, each with a large vesicular nucleus.
The tumor tissue was composed of atypical cells with boundaries
that could not be clearly defined.
Immunostaining was performed by two certified
pathologists in the present department who were blinded to the
clinical characteristics of the patient. Micrometer-thick tissue
sections were autoclaved in buffer, and incubated with antibodies.
Immunostaining was performed using the biotin-free horseradish
peroxidase enzyme-labeled polymer of the Envision Plus detection
system. The antibodies used were as follows: anti-vimentin antibody
(clone, EPR3776; catalog no., ab92547; dilution, 1:200; 60 min at
room temperature; Abcam, Cambridge, UK); anti-CD68 antibody (clone,
KP1; catalog no., ab955; dilution, 1:200; 60 min at room
temperature; Abcam); anti-CD34 antibody (clone, EP373Y; catalog
no., ab81289; dilution, 1:250; 60 min at room temperature; Abcam);
anti-S100 β antibody (clone, EP1576Y; catalog no., ab52642;
dilution, 1:500; 60 min at room temperature; Abcam);
anti-cytokeratin antibody (clone, AE1/AE3; catalog no., M351501;
dilution, 1:200; 60 min at room temperature; Dako, Glostrup,
Denmark); anti-EMA antibody (clone, 2F6; catalog no., ab156947;
dilution, 1:150; 60 min at room temperature; Abcam); and
anti-Desmin antibody (clone, D33; catalog no., ab8470; dilution,
1:200; 60 min at room temperature; Abcam). The Periodic Acid Schiff
(PAS) Stain kit (Baso, Zhuhai, China) was also used.
Immunohistochemical staining revealed positivity for vimentin,
periodic acid-Schiff, cluster of differentiation (CD)68, CD34, S100
and negativity for cytokeratin, epithelial membrane antigen and
desmin.
Follow-up MRI examination 24-months after surgery
revealed no evidence of tumor recurrence and no sensory disturbance
or dyskinesia.
The patient was followed up every month in the first
3 months. Subsequently, the patient was followed up every 3 months
until April 2016. Subsequently, the patient will be followed-up
every 6 months.
Discussion
Myxoinflammatory fibroblastic sarcoma, originally
termed ‘acral myxoinflammatory fibroblastic sarcoma’ was first
identified by Meis-Kindblom and Kindblom (4) in 1998. In the same year, Montgomery
et al (5) reported an
inflammatory myxohyaline tumor of the distal extremities with
virocyte or Reed-Sternberg-like cells, while Michal (6) reported inflammatory myxoid tumor of the
soft parts with bizarre giant cells. In addition, Jurcić et
al (7) demonstrated that
occurrence of such tumors in the proximal regions of the limbs and
thus the term ‘myxoinflammatory fibroblastic sarcoma’ was coined.
Myxoinflammatory fibroblastic sarcoma develops in patients of all
ages with no clear gender predilection.
Laskin et al (2) analyzed 104 myxoinflammatory fibroblastic
sarcoma patients, which revealed that in 61% of cases, the tumor
occurred in the fingers, hands and feet and in 73% of cases the
tumor occurred in the dorsal soft tissue involving distal acral
sites. Other affected regions included the knees and lower leg,
elbow and forearm, ankle, upper leg, upper arm, shoulder and the
inguinal region (2). To the best of
our knowledge, the present case of a cervicothoracic
myxoinflammatory fibroblastic sarcoma with brachial plexus invasion
is the first to be reported in the literature. The largest
myxoinflammatory fibroblastic sarcoma reported previously was 16 cm
in size (8), while the
supraclavicular and infraclavicular masses identified in this case
were 10×5×3 cm and 25×18×8 cm, respectively.
A painless slow-growing mass or swelling is the most
common initial complaint in patients with myxoinflammatory
fibroblastic sarcoma. A number of individuals also present with
pain, tenderness or dysfunction of the affected area (8). The symptoms observed in the patient in
the present case are consistent with those reported in the
literature (2).
Preoperative auxiliary examinations indicated a
benign tumor in the present study; however, postoperative
histological analysis diagnosed low-grade malignant
myxoinflammatory fibroblastic sarcoma. We hypothesize that in the
context of diagnosis and treatment of large tumors, which are
commonly benign, malignancy must always be suspected and therefore
the use of pre-operative biopsy may improve diagnosis and
treatment.
In the present case, the tumor was carefully
resected to protect the medial, lateral and posterior cords, as
well as the median, axillary and musculocutaneous nerves, which
surrounded the tumor. The postoperative activity and sensation of
the limb was normal. Surgery was difficult due to the large tumor
size and invasion of the brachial plexus. Therefore, the tumor was
separated carefully as injury of the brachial plexus may lead to
dysfunction of the upper limb.
The histological differential diagnosis of
myxoinflammatory fibroblastic sarcoma may be associated with the
myxoid, inflammatory and atypical features. Differential diagnosis
includes tenosynovitis, giant cell tumor of the tendon sheath,
inflammatory myofibroblastic tumor, liposarcoma, epithelioid
sarcoma and myxoid malignant fibrous histiocytoma (9).
Lombardi et al (10) performed immunohistochemical analysis
in 138 myxoinflammatory fibroblastic sarcoma patients, which
revealed that vimentin was strongly positive in all lesions. A
total of 84 and 57% of tumors exhibited focal positivity for CD68
and CD34, respectively. Focal positivity for smooth muscle actin,
S-100 protein, activin receptor-like kinase 1 and keratin was also
observed in 6–16% of patients (10).
These results were consistent with the immunohistochemical staining
results observed in the patient of the present case: Vimentin(+),
CD68(+), CD34(+) and S100(+).
Wide resection is generally accepted as the first
choice of treatment for myxoinflammatory fibroblastic sarcoma. At
present, the efficacy of chemotherapy and radiotherapy remains
unclear and the rate of local recurrence is high (11,12). In
the present case, MRI performed during follow-up 24 months after
surgery revealed no tumor recurrence. This case reported the
successful surgical management of a huge myxoinflammatory
fibroblastic sarcoma, which invaded the brachial plexus.
For such a large tumor with invasion of the brachial
plexus, the neurological function of the brachial plexus may be
preserved through a precise surgical procedure. The association
between adjuvant therapy and the prognosis require observation in
additional cases.
References
|
1
|
Silver AG, Baynosa RC, Mahabir RC, Wang
WZ, Zamboni WA and Khiabani KT: Acral myxoinflammatory fibroblastic
sarcoma: A case report and literature review. Can J Plast Surg.
21:92–94. 2013.PubMed/NCBI
|
|
2
|
Laskin WB, Fetsch JF and Miettinen M:
Myxoinflammatory fibroblastic sarcoma: A clinicopathologic analysis
of 104 cases, with emphasis on predictors of outcome. Am J Surg
Pathol. 38:1–12. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nishio J: Updates on the cytogenetics and
molecular cytogenetics of benign and intermediate soft tissue
tumors. Oncol Lett. 5:12–18. 2013.PubMed/NCBI
|
|
4
|
Meis-Kindblom JM and Kindblom LG: Acral
myxoinflammatory fibroblastic sarcoma: A low-grade tumor of the
hands and feet. Am J Surg Pathol. 22:911–924. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Montgomery EA, Devaney KO, Giordano TJ and
Weiss SW: Inflammatory myxohyaline tumor of distal extremities with
virocyte or Reed-Sternberg-like cells: A distinctive lesion with
features simulating inflammatory conditions, Hodgkin's disease and
various sarcomas. Mod Pathol. 11:384–391. 1998.PubMed/NCBI
|
|
6
|
Michal M: Inflammatory myxoid tumor of the
soft parts with bizarre giant cells. Pathol Res Pract. 194:529–533.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jurcić V, Zidar A, Montiel MD,
Frković-Grazio S, Nayler SJ, Cooper K, Suster S and Lamovec J:
Myxoinflammatory fibroblastic sarcoma: A tumor not restricted to
acral sites. Ann Diagn Pathol. 6:272–280. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Togral G, Arikan M, Aktas E and Gungor S:
Giant myxoinflammatory fibroblastic sarcoma with bone invasion: A
very rare clinical entity and literature review. Chin J Cancer.
33:406–410. 2014.PubMed/NCBI
|
|
9
|
Lang JE, Dodd L, Martinez S and Brigman
BE: Case reports: Acral myxoinflammatory fibroblastic sarcoma: A
report of five cases and literature review. Clin Orthop Relat Res.
445:254–260. 2006.PubMed/NCBI
|
|
10
|
Lombardi R, Jovine E, Zanini N, Salone MC,
Gambarotti M, Righi A, Balladelli A, Colangeli M and Rocca M: A
case of lung metastasis in myxoinflammatory fibroblastic sarcoma:
Analytical review of one hundred and thirty eight cases. Int
Orthop. 37:2429–2436. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kovarik CL, Barrett T, Auerbach A and
Cassarino DS: Acral myxoinflammatory fibroblastic sarcoma: Case
series and immunohistochemical analysis. J Cutan Pathol.
35:192–196. 2008.PubMed/NCBI
|
|
12
|
Tejwani A, Kobayashi W, Chen YL, Rosenberg
AE, Yoon S, Raskin KA, Rosenthal DI, Nielsen GP, Hornicek FJ and
Delaney TF: Management of acral myxoinflammatory fibroblastic
sarcoma. Cancer. 116:5733–5739. 2010. View Article : Google Scholar : PubMed/NCBI
|