Introduction
Hepatocellular carcinoma (HCC) is the third highest
cause of cancer-associated mortality worldwide following stomach
and lung cancer (1). Liver cancer is
the sixth most common cancer worldwide, accounting for 5.7% of all
novel cancer cases. A total of ~82% of liver cancer cases occur in
developing countries, with 55% occurring in China alone. There is a
high incidence rate of HCC in Asia, and particularly so in China
due to endemic hepatitis B and C (2,3). However,
only <10% of patients in Asia and ~30% of patients in the West
are eligible at diagnosis for potentially curative treatments,
including resection or liver transplantation (4,5) and
radiofrequency ablation (6,7).
Despite regular medical examinations, certain
patients that are diagnosed with HCC also present with extensive
tumor thrombi, typically extending into the inferior vena cava
(IVC) and right atrium (RA) through the hepatic vein (8,9); this
condition is considered as terminal-stage HCC. Intracardiac tumor
thrombus and liver resection treatment have been reported in the
current literature, alongside alternative therapeutic approaches
(i.e., radiotherapy), but long-term results from such treatments
remain unsatisfactory (10–15). Transcatheter arterial
chemoembolization (TACE) has since been recommended for the
treatment of these patients (16).
The present study describes the case of a patient
with HCC and metastatic tumor thrombi of the right branch of the
portal vein, inferior hepatic vein, IVC and RA, with pulmonary
metastases. Following two effective TACE treatments, the patient
remains alive at 40 months follow-up, without any signs of
recurrence.
Case report
A 29-year-old woman with hepatitis B was referred to
the First Affiliated Hospital of Guangxi Traditional Chinese
Medical University (Nanning, China) on September 5, 2011,
presenting with a 1-month history of right upper quadrant abdominal
pain and abnormal shadows in the liver on an abdominal computed
tomography (CT) scan (performed using a BrightSpeed Elite 16 slice
CT scanner; GE Healthcare Life Sciences, Chalfont, UK) that had
been performed prior to referral. Physical examination identified
mild abdominal tenderness in the upper right quadrant, with no
rebound tenderness. Cardiovascular, respiratory and neurological
examinations were normal. The family history of the patient was
non-contributory. Laboratory analysis provided the following
results: Platelets, 201×109/l (normal range,
100–300×109/l); serum aspartate aminotransferase, 107
U/l (normal range, <40 U/l); alanine aminotransferase, 94 U/l
(normal range, <40 U/l); total bilirubin, 9.1 µmol/l (normal
range, <20 µmol/l); albumin, 31.7 g/l (normal range, 34–54 g/l);
and prothrombin time, 14.5 sec (normal range, 12–14 sec). Screening
for hepatitis B was positive for all antigens and negative for
antibodies. The serum level of α-fetoprotein (AFP) was >1,000
ng/ml (normal range, <20 ng/ml). No abnormalities were observed
on the electrocardiogram.
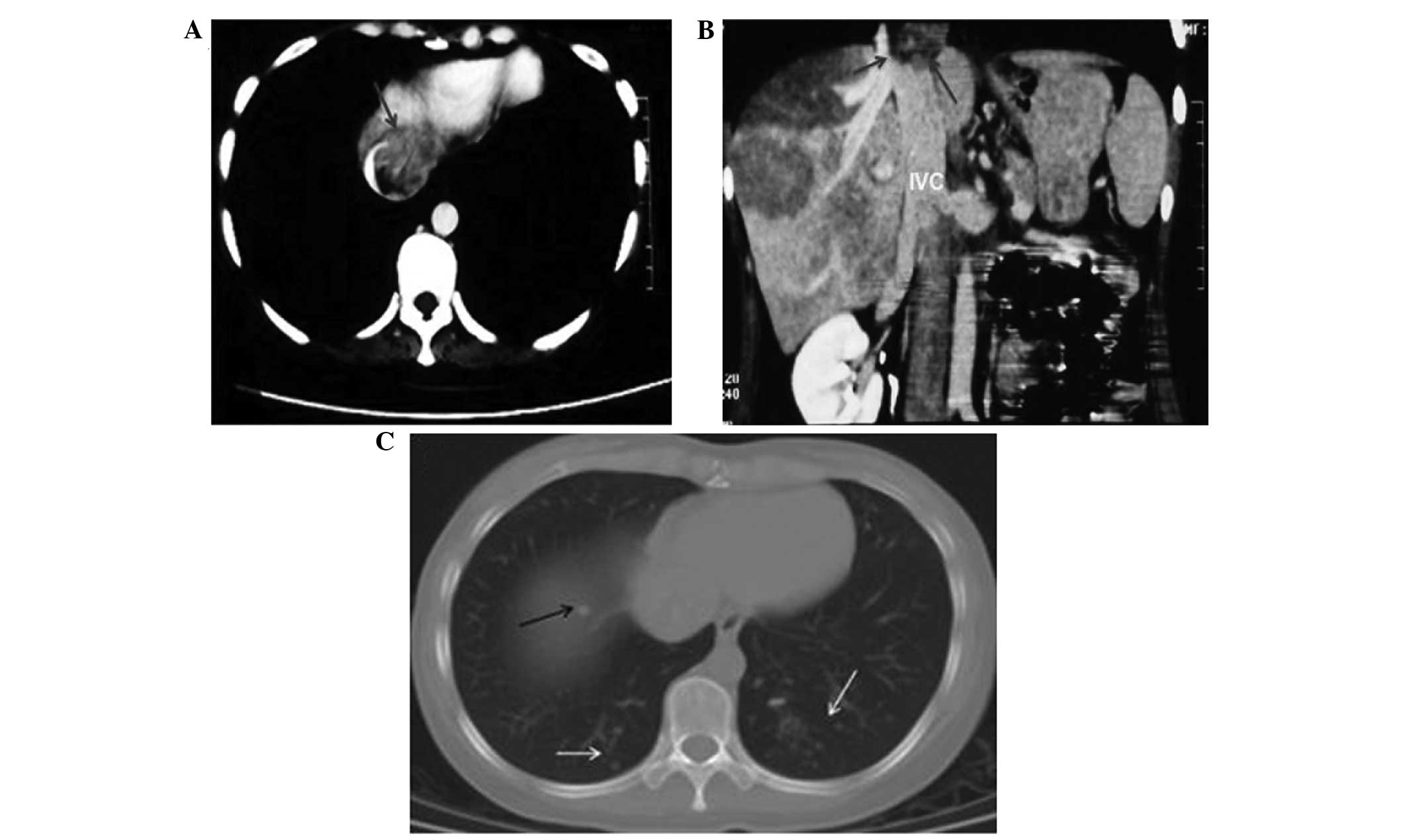
An abdominal enhanced CT scan was performed at the
Guangxi Tumor Hospital (Nanning, China) hospital 4 days prior to
admission, and revealed multifocal liver lesions of various sizes,
ranging from 2.0–8.5 cm in diameter in segments 4, 5, 7 and 8, and
a right portal vein tumor thrombus extending through the middle
hepatic vein and IVC into the RA (Fig. 1A
and B). A CT scan of the chest identified several solitary
nodules in the bilateral lower lobes of the lungs, all of which
were <0.5 cm in diameter (Fig.
1C). Echocardiography was not performed at that time, as the
tumor thrombus could not be clearly observed on the CT scan.
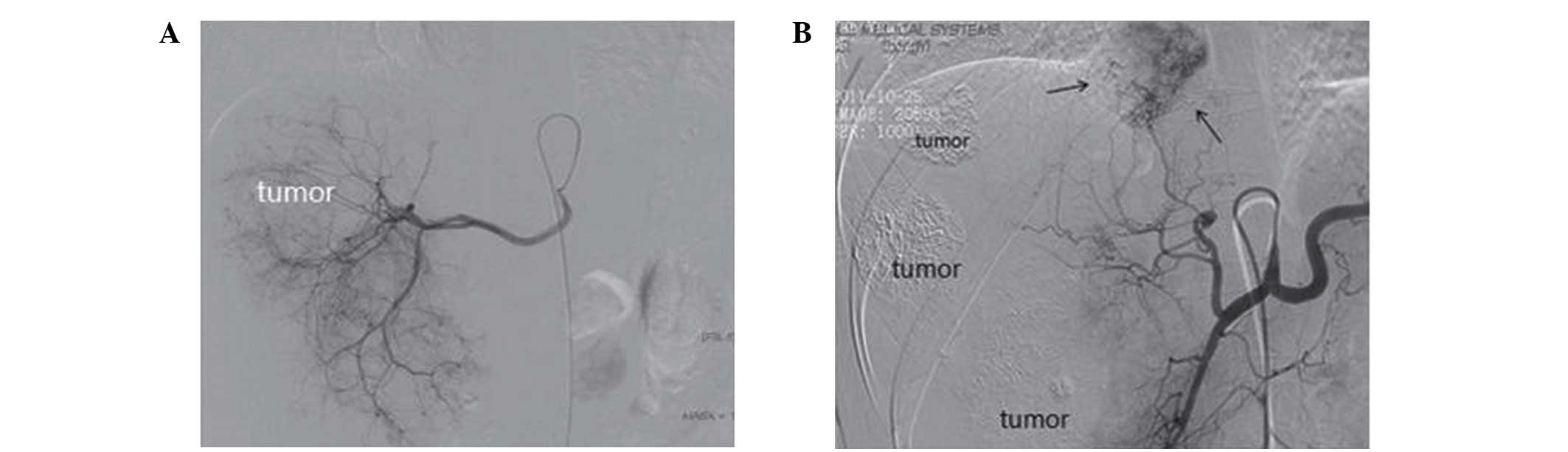
A selective hepatic angiogram was performed during
the first TACE treatment and revealed three large hypervascular
areas in the right lobe of the liver supplied by the right hepatic
artery (Fig. 2). These hypervascular
areas were typical of HCC, and extended into the IVC and RA through
the middle hepatic vein. The feeding arteries of the tumor thrombus
and the tumor itself originated from the left and right hepatic
arteries. Therefore, following imaging analysis, the patient was
diagnosed with HCC complicated by portal vein, middle hepatic vein
and metastatic right atrial tumor thrombi, with pulmonary
metastases (no biopsy was performed to confirm the exact nature of
these masses).
In September 2011, the patient underwent the first
6-week cycle of TACE treatment with fluorouracil (5-FU; 500 mg),
pirarubicin (20 mg), mitomycin C (10 mg), super-liquid iodized oil
(Lipiodol®; 9.5 ml; Guerbet, Aulnay-sous-Bois, France)
and sodium alginate microball (KMG; 1.0 g; Beijing Shengyiyao
Science & Technology Development Co., Ltd., Beijing, China). At
1 month after the initial TACE treatment, serum AFP levels remained
at >1,000 ng/ml. No complications of TACE were observed, and the
symptoms were partially relieved. CT revealed necrosis of a few of
the tumor masses, but a number of active lesions remained.
Therefore, in October 2011, the patient underwent a second 6-week
cycle of TACE treatment with 5-FU (500 mg), pirarubicin (10 mg),
mitomycin C (10 mg), super-liquid iodized oil (2 ml) and KMG (0.3
g).
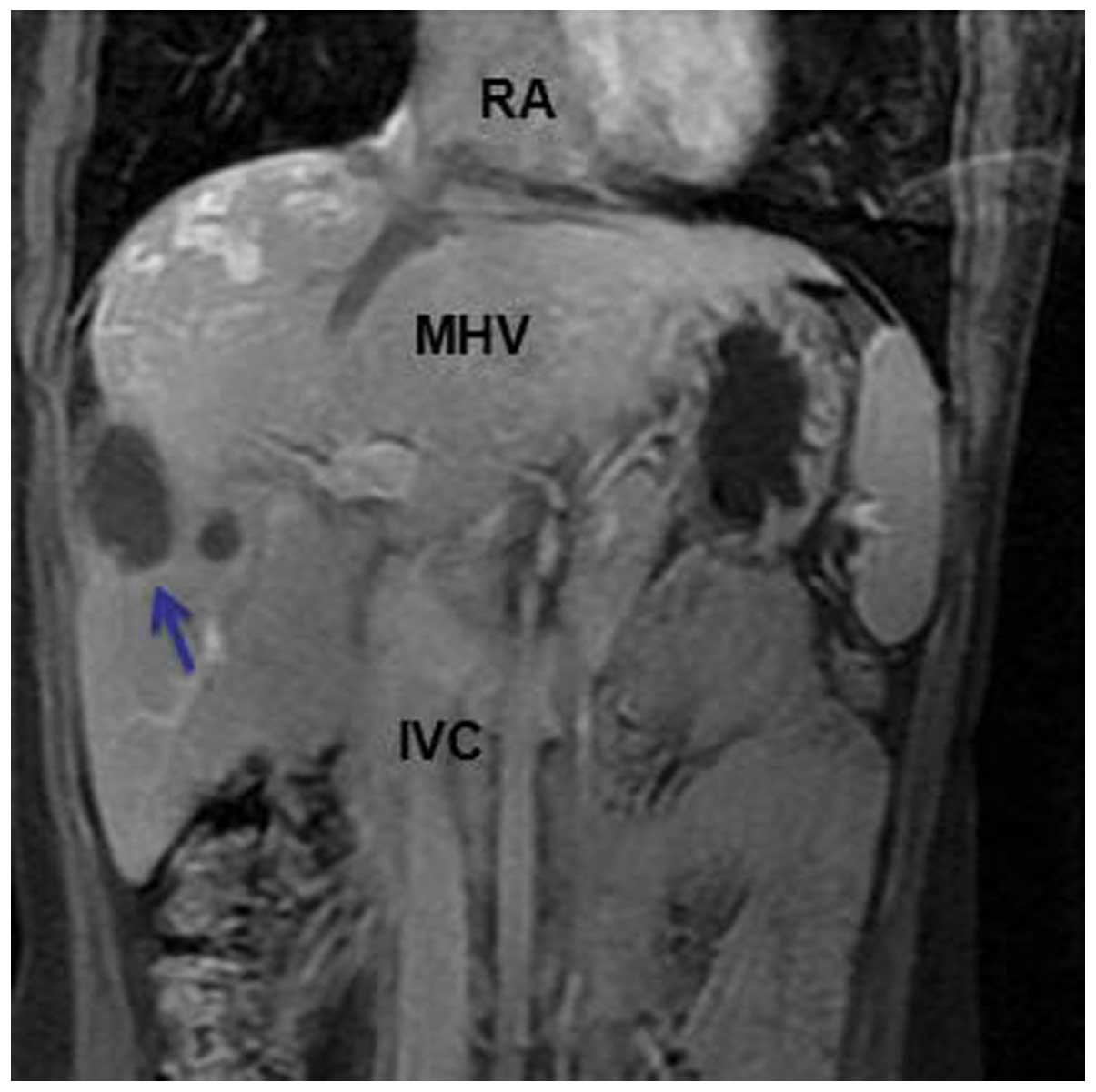
At 1 month after the second TACE treatment, the
right upper quadrant abdominal pain had disappeared. The serum AFP
levels gradually decreased and fell within the normal range (<20
ng/ml). At a total of 4 months after the second TACE treatment, CT
revealed that the lung metastases had disappeared. A magnetic
resonance imaging (MRI) scan was performed (using a Signa HDxt 1.5T
MRI scanner; GE Healthcare Life Sciences) 14 months after the
second TACE treatment in order to detect any lesions that had been
missed on the CT scan. MRI indicated that there was no active
lesion, that the tumor thrombus in the right branch of the portal
vein and RA had disappeared, and that the liver tumors and the
tumor thrombus in the IVC and middle hepatic vein had markedly
decreased in size (Fig. 3).
Subsequent to therapy, the patient was not administered any further
drug treatments, as the liver function remained normal. The patient
has been regularly followed up, and at 40 months post-treatment is
currently alive and well, exhibiting no signs of tumor progression
and with excellent quality of life. The present study was approved
by the Ethics Committee of the First Affiliated Hospital of Guangxi
Traditional Chinese Medical University. Full informed consent was
obtained from the patient.
Discussion
HCC is particularly prevalent in East Asia due to
the high incidence of hepatitis B and C infection (2,3,17). Liver transplantation or hepatic
resection is limited to a small number of HCC patients (18). Advanced HCC presenting with extensive
intravascular tumor thrombi is a rare condition and is considered
as a terminal stage of HCC (19–21). The
majority of patients with terminal-stage HCC receive no anticancer
treatment and typically succumb to the disease within a few months
of diagnosis, with a median survival time of 2.0–3.5 months
(11,22). The most appropriate treatment for
patients with HCC metastases to the RA remains controversial
(8–10,12,13,15,16,19,23).
As the majority of patients are already in the advanced stage of
the disease at diagnosis, aggressive treatment is not recommended.
It was previously reported that the survival time following
surgical removal of intra-atrial HCC ranged from 18 days to 56
months (median, 11 months), depending on the characteristics of
each individual patient (23).
However, regarding patients with HCC and tumor thrombi of the
hepatic vein, portal vein and RA, plus pulmonary metastases, no
effective therapy has yet been reported, with surgical resection
being unsuitable for such patients. Alternative non-surgical
therapies, including percutaneous ethanol injection, microwave
coagulation therapy and irradiation, have also produced
unsatisfactory results in patients with advanced HCC (5,11,21,24,25).
Therefore, no standard regimens have yet been approved.
TACE has become the most successful treatment for
advanced HCC, providing a survival benefit for selected patients
(26). The treatment is extensively
used in patients with HCC invading the portal vein, and also in
those who are not suitable for surgery (27). Hepatic artery infusion chemotherapy is
particularly effective in treating the disease and may offer
survival benefits, even when the patient presents with extrahepatic
metastases (28).
In the present study, TACE with 5-FU, pirarubicin,
mitomycin C, Lipiodol and KMG achieved a marked anticancer effect,
not only on the primary tumor, but also on the tumor thrombi in the
portal and hepatic veins and the RA, and on the pulmonary
metastases. The patient is currently alive at 40 months
post-treatment, which is far longer than the 2.0 to 3.5-month
survival time typically observed in patients with this disease;
however, it should be noted that the survival time of the patient
is within the 18-day to 56-month range reported with the use of
other treatment strategies. Emulsions of Lipiodol and chemotherapy
have been reported to remain in the hepatic tissues for a long
period of time after infusion through the portal vein and hepatic
artery (29). The use of KMG induces
permanent hepatic artery embolization and leads to long-term
anticancer drug retention in the tumor.
A previous systematic review indicated that TACE
improves the survival time of patients with unresectable HCC, and
that it should be considered as a standard treatment (4). Another previous study in patients with
HCC and thrombi of the IVC and RA treated with TACE reported that
the median survival time in responders was 13.5 months (range,
1.5–79.7 months) compared with 3.3 months (range, 2.1–24.3 months)
in non-responders (16). However, the
tumor burden in these patients was less than that observed in the
present case. Further trials should be conducted to assess the
efficacy of TACE in such patients, however, the rarity of the
disease would be a limiting factor on the number of trials that may
be undertaken. Nevertheless, the few reported cases, including the
present case, suggest that TACE may be an appropriate and
successful approach to treat HCC patients presenting with multiple
venous thrombi and distant metastases.
In conclusion, the current case may suggest that
TACE, using 5-FU, pirarubicin, mitomycin C, Lipiodol and KMG, may
serve as an effective treatment in patients presenting with
unresectable advanced HCC with pulmonary metastases, and with
extensive tumor thrombi in the IVC, the RA and one branch of the
portal vein.
References
|
1
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Llovet JM, Fuster J and Bruix J: Prognosis
of hepatocellular carcinoma. Hepatogastroenterology. 49:7–11.
2002.PubMed/NCBI
|
|
3
|
Tan CK, Law NM, Ng HS and Machin D: Simple
clinical prognostic model for hepatocellular carcinoma in
developing countries and its validation. J Clin Oncol.
21:2294–2298. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Llovet JM and Bruix J: Systematic review
of randomized trials for unresectable hepatocellular carcinoma:
Chemoembolization improves survival. Hepatology. 37:429–442. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lencioni R, Chen XP, Dagher L and Venook
AP: Treatment of intermediate/advanced hepatocellular carcinoma in
the clinic: How can outcomes be improved? Oncologist. 15(Suppl 4):
42–52. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kawano Y, Sasaki A, Kai S, Endo Y, Iwaki
K, Uchida H, Shibata K, Ohta M and Kitano S: Short- and long-term
outcomes after hepatic resection for hepatocellular carcinoma with
concomitant esophageal varices in patients with cirrhosis. Ann Surg
Oncol. 15:1670–1676. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Saab S, Yeganeh M, Nguyen K, Durazo F, Han
S, Yersiz H, Farmer DG, Goldstein LI, Tong MJ and Busuttil RW:
Recurrence of hepatocellular carcinoma and hepatitis B reinfection
in hepatitis B surface antigen-positive patients after liver
transplantation. Liver Transpl. 15:1525–1534. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kato Y, Tanaka N, Kobayashi K, Ikeda T,
Hattori N and Nonomura A: Growth of hepatocellular carcinoma into
the right atrium. Report of five cases. Ann Intern Med. 99:472–474.
1983. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kojiro M, Nakahara H, Sugihara S, Murakami
T, Nakashima T and Kawasaki H: Hepatocellular carcinoma with
intra-atrial tumor growth. A clinicopathologic study of 18 autopsy
cases. Arch Pathol Lab Med. 108:989–992. 1984.PubMed/NCBI
|
|
10
|
Fujisaki M, Kurihara E, Kikuchi K,
Nishikawa K and Uematsu Y: Hepatocellular carcinoma with tumor
thrombus extending into the right atrium: Report of a successful
resection with the use of cardiopulmonary bypass. Surgery.
109:214–219. 1991.PubMed/NCBI
|
|
11
|
Zeng ZC, Fan J, Tang ZY, Zhou J, Qin LX,
Wang JH, Sun HC, Wang BL, Zhang JY, Jiang GL and Wang YQ: A
comparison of treatment combinations with and without radiotherapy
for hepatocellular carcinoma with portal vein and/or inferior vena
cava tumor thrombus. Int J Radiat Oncol Biol Phys. 61:432–443.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ohwada S, Tanahashi Y, Kawashima Y, Satoh
Y, Nakamura S, Kobayashi I, Ohya T, Ishikawa S, Ohtaki A, Iino Y,
et al: Surgery for tumor thrombi in the right atrium and inferior
vena cava of patients with recurrent hepatocellular carcinoma.
Hepatogastroenterology. 41:154–157. 1994.PubMed/NCBI
|
|
13
|
Kanematsu M, Imaeda T, Minowa H, Yamawaki
Y, Mochizuki R, Goto H, Seki M, Doi H and Okumura S: Hepatocellular
carcinoma with tumor thrombus in the inferior vena cava and right
atrium. Abdom Imaging. 19:313–316. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Le Treut YP, Hardwigsen J, Ananian P,
Saïsse J, Grégoire E, Richa H and Campan P: Resection of
hepatocellular carcinoma with tumor thrombus in the major
vasculature. A European case-control series. J Gastrointest Surg.
10:855–862. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang Y, Yuan L, Ge RL, Sun Y and Wei G:
Survival benefit of surgical treatment for hepatocellular carcinoma
with inferior vena cava/right atrium tumor thrombus: Results of a
retrospective cohort study. Ann Surg Oncol. 20:914–922. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chern MC, Chuang VP, Cheng T, Lin ZH and
Lin YM: Transcatheter arterial chemoembolization for advanced
hepatocellular carcinoma with inferior vena cava and right atrial
tumors. Cardiovasc Intervent Radiol. 31:735–744. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Taura N, Hamasaki K, Nakao K, Ichikawa T,
Nishimura D, Goto T, Fukuta M, Kawashimo H, Miyaaki H, Fujimoto M,
et al: Aging of patients with hepatitis C virus-associated
hepatocellular carcinoma: Long-term trends in Japan. Oncol Rep.
16:837–843. 2006.PubMed/NCBI
|
|
18
|
Fan HL, Chen TW, Hsieh CB, Jan HC, His SC,
De-Chuan C, Chu CH and Yu JC: Liver transplantation is an
alternative treatment of hepatocellular carcinoma beyond the Milan
criteria. Am J Surg. 200:252–257. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nam SW, Baek JT, Kang SB, Lee DS, Kim JI,
Cho SH, Park SH, Han JY, Ahn BM, Kim JK and Chung KW: A case of the
hepatocellular carcinoma during the pregnancy and metastasis to the
left atrium. Korean J Hepatol. 11:381–385. 2005.PubMed/NCBI
|
|
20
|
Chong VH, Jamaludin AZ, Lim KS, Abdullah
HM and Nair RT: Hepatocellular carcinoma with intravascular and
right atrial extension. Indian J Gastroenterol.
27:2552008.PubMed/NCBI
|
|
21
|
Tanaka A, Morimoto T, Ozaki N, Ikai I,
Yamamoto Y, Tsunekawa S, Kitai T and Yamaoka Y: Extension of
surgical indication for advanced hepatocellular carcinoma: Is it
possible to prolong life span or improve quality of life?
Hepatogastroenterology. 43:1172–1181. 1996.PubMed/NCBI
|
|
22
|
Cheng HY, Wang XY, Zhao GL and Chen D:
Imaging findings and transcatheter arterial chemoembolization of
hepatic malignancy with right atrial embolus in 46 patients. World
J Gastroenterol. 14:3563–3568. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Inoue Y, Hayashi M, Katsumata T, Shibayama
Y and Tanigawa N: Hepatocellular carcinoma with right atrial tumor
thrombus: Report of a case. Surg Today. 41:1122–1129. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lin SM, Lin CJ, Lin CC, Hsu CW and Chen
YC: Randomised controlled trial comparing percutaneous
radiofrequency thermal ablation, percutaneous ethanol injection,
and percutaneous acetic acid injection to treat hepatocellular
carcinoma of 3 cm or less. Gut. 54:1151–1156. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Itoh S, Ikeda Y, Kawanaka H, Okuyama T,
Kawasaki K, Eguchi D, Korenaga D and Takenaka K: Efficacy of
surgical microwave therapy in patients with unresectable
hepatocellular carcinoma. Ann Surg Oncol. 18:3650–3656. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Takayasu K, Arii S, Ikai I, et al:
Prospective cohort study of transarterial chemoembolization for
unresectable hepatocellular carcinoma in 8510 patients.
Gastroenterology. 131:461–469. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Xue TC, Xie XY, Zhang L, Yin X, Zhang BH
and Ren ZG: Transarterial chemoembolization for hepatocellular
carcinoma with portal vein tumor thrombus: A meta-analysis. BMC
Gastroenterol. 13:602013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Nishikawa H, Osaki Y, Kita R and Kimura T:
Hepatic arterial infusion chemotherapy for advanced hepatocellular
carcinoma in Japan. Cancers (Basel). 4:165–183. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Miyazaki M, Suzuki H, Itoh H, et al:
Portal vein infusion of cancer chemotherapeutic agent emulsified
with Lipiodol in regenerating liver after partial hepatectomy in
rats. Res Exp Med (Berl). 193:231–240. 1993. View Article : Google Scholar : PubMed/NCBI
|