Introduction
Small cell lung cancer (SCLC) is common in thoracic
neoplasms, which currently accounts for 13.6% of all lung cancers
(1), with a high degree of malignancy
and rapid tumor progression. SCLC is often diagnosed with
widespread metastases at the time of the initial diagnosis. The
tumor is sensitive to chemotherapy and radiotherapy, and in the
majority of patients, can be controlled in the short-term by
chemotherapy. Although many patients are treated with chemotherapy,
either alone or in combination with local therapy such as radiation
therapy. However, in recent decades, there have no substantial
changes in treatment of or improvement in survival from this
disease. The 5-year survival of limited stage SCLC is only 20–25%.
For extensive stage disease, <10% of patients alive at 2 years
(1). However, a small proportion of
patients in the later stage of SCLC are in a poor physical
condition and exhibit disqualifying chemoradiotherapy indications,
which makes them ineligible for chemotherapy treatment.
Unfortunately, no molecularly targeted therapy has demonstrated a
benefit in SCLC. Therefore, treatment options SCLC are limited only
including oral etoposide capsules, pain treatments and other
symptomatic treatment. The present study reports the case of a
patient with SCLC who was admitted to the Department of Chest
Surgery, Sichuan Provincial Cancer Hospital (Chengdu, Sichuan,
China) in January 2014, with an Eastern Cooperative Oncology Group
(ECOG) (2) score of <2. One cycle
of chemotherapy was administered whilst ventilator support was
provided, and the patient's condition improved for a time.
Case report
A 62-year-old female was admitted to the Department
of Chest Surgery, Sichuan Provincial Cancer Hospital on January 15,
2014, due to lumbago and backache that had persisted for >1
month. Upon admittance, the patient experienced unprovoked lumbago,
backache and stomachache, without a cough, sputum, hemoptysis,
melena or any other discomfort. The pain was stopped after taking
ibuprofen and codeine phosphate tablets. Two weeks later, the
patient had to return to hospital since the pain had become
subsequently aggravated and could not be relieved by anodyne
treatment. The patient reported a history of chronic obstructive
pulmonary disease and had been treated with endotracheal intubation
and ventilator support in another hospital due to an acute lung
infection and type II respiratory failure 1 year previously. A
physical examination showed the following: Temperature, 36.3°C;
heart rate, 106 beats/min; respiratory rate, 22 breaths/min; and
blood pressure, 114/75 mmHg. There were no signs of superficial
lymph nodes on the neck, armpit or groin, but an emphysematous
chest, decreased respiratory movement, dullness to percussion at
the lower right chest and reduced breath sounds in each lung
(particularly in the right lower lobe), without any wheezing, rales
or rhonchi, were observed. The patient presented with a normal
border of cardiac dullness, a regular cardiac rhythm and no
pathological murmurs. The abdomen was flat and soft, while pain was
experienced in the mid-upper abdomen under the application of
pressure. A hard tumor mass with a diameter ~4 cm and an irregular
shape could be felt. Furthermore, there were no signs of shifting
dullness in the abdomen or swelling in the lower extremities.
Subsequent to being hospitalized, the patient's
routine blood examination showed the following: Red blood cell
count, 3.63×1012/l; white blood cell count,
8.74×109/l; hemoglobin level, 114 g/l; and platelet
count, 2.13×1014/l. Liver function tests revealed the
following: Aspartate aminotransferase, 6 U/l; alanine
aminotransferase, 13 U/l; serum total bilirubin, 22.5 µmol/l;
conjugated bilirubin, 4.7 µmol/l; and albumin, 37 g/l. Renal
function test results were as follows: Creatinine clearance, 78
ml/min/1.73 m2; creatinine, 47 µmol/l; uric acid, 177
µmol/l; and blood urea nitrogen, 2.0 µmol/l. Other biochemical test
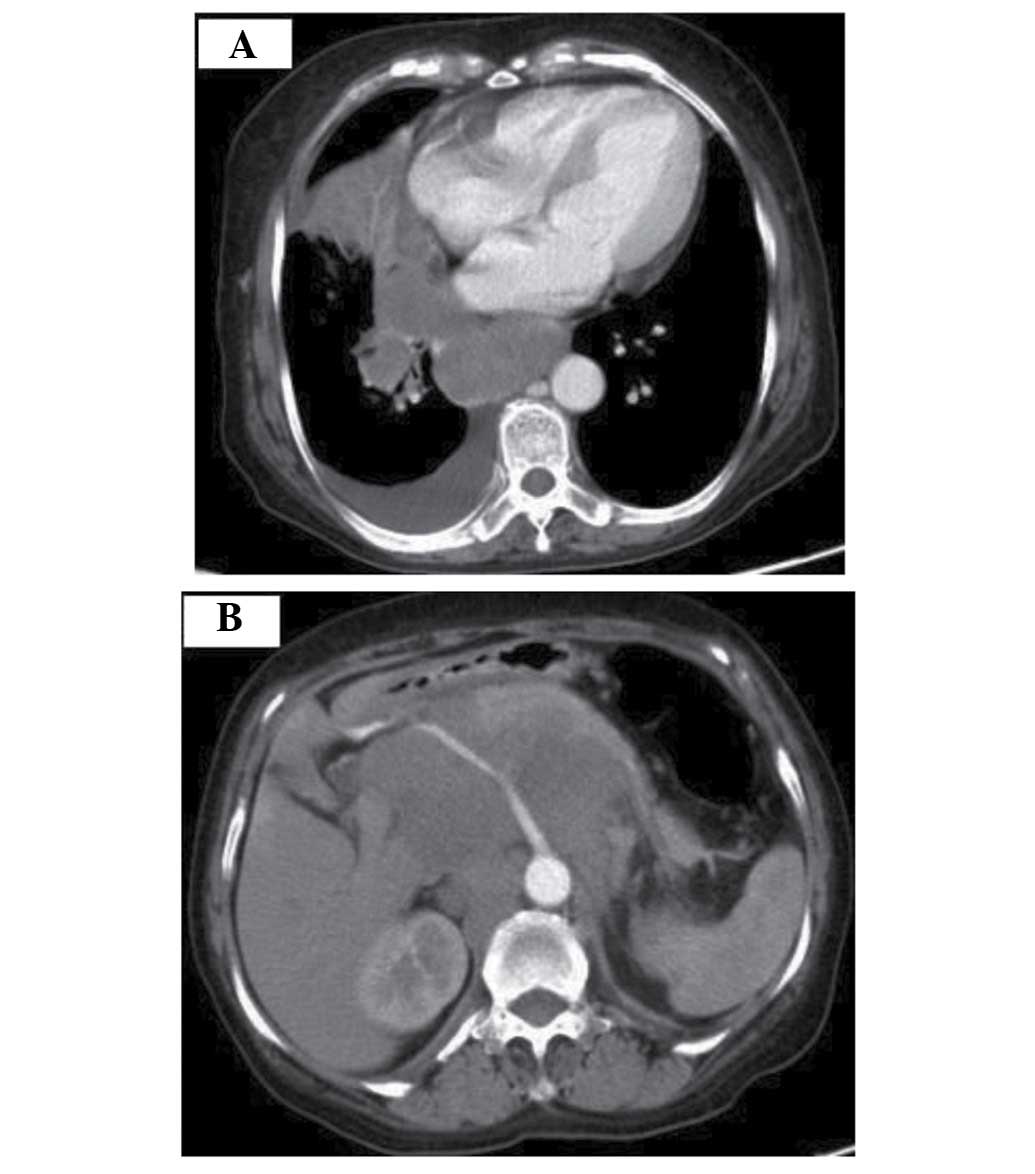
results were normal. Computed tomography (CT) scans performed in
another hospital showed a space-occupying lesion in the hilus of
the right lung, accompanied with pulmonary atelectasis in the lower
lobe, medium pleural effusion in the right chest and a
space-occupying retroperitoneal lesion. The initial diagnosis
considered right-sided lung cancer or lymphoma. A bronchoscopy
showed that there was a neoplasm blocking the lateral branch of the
middle right lung, with a hyperemic surface; the tissue was soft
and bled easily in the process of the biopsy. The biopsy results
showed no signs of cancer, but chronic inflammation of the mucous
membrane of the lateral branch of the middle right lung. Moderate
damage was identified by pulmonary function test. The bones were
not involved according to bone scans. The pre-operative blood gas
analysis results were as follows: pH, 7.49; partial pressure of
carbon dioxide (PCO2), 37.4 mmHg; partial pressure of
oxygen (PO2), 118.1 mmHg; and
HCO3−, 23.9 mmol/l. The enhanced CT scan of
the brain, chest and midsection that was performed in Sichuan
Provincial Cancer Hospital on January 15, 2014, revealed a large
confluent mass of shadows (the largest at ~5.5×4.5 cm) located by
the hilus of the right lung and adjacent organs in the mediastinum
below the aortic knuckle, as well as an arc liquid density shadow
on the dorsal region of the right chest. In addition, multiple
space-occupying lesion shadows (the largest at ~6.0×5.2 cm) were
observed in the retroperitoneal region; some of which were mixed
together as one mass, wrapping around the celiac axis, common
hepatic artery, splenic artery, and left and right renal arteries,
forcing the pancreas to move forward. No craniocerebral
space-occupying focus or other evident abnormalities were
identified (Fig. 1).
In order to determine an exact diagnosis, the
patient underwent a tumor biopsy on the hilus of the right lung via
thoracoscopy under general anesthesia on June 20, 2014.
Intraoperative findings showed consolidation and atelectasis in the
right lobus inferior pulmonis, pale red color and bloody
hydrothorax in the right chest (~500 ml), and a lump of ~6 cm in
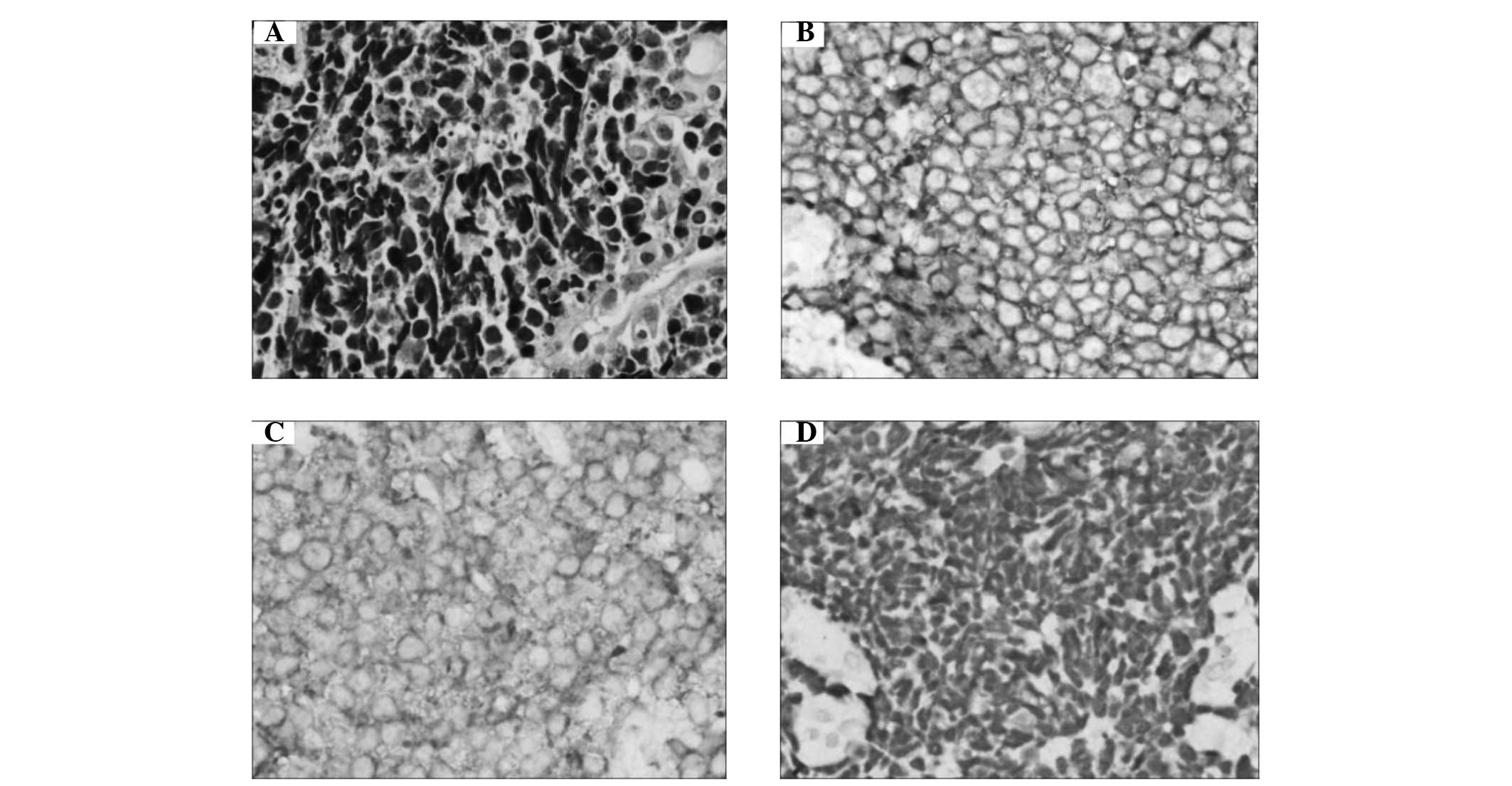
diameter at the hilus of the right lung. The post-operative biopsy
results indicated small cell carcinoma (Fig. 2): Small cells with little cytoplasm,
indistinct cell borders, finely granular nuclear chromatin and
absent or inconspicuous nucleolus, nuclear fission were apparent
(3). Also, based on the positive
tumor immunohistochemical results for cytokeratin, synaptophysin,
cluster of differentiation 56, thyroid transcription factor-1,
paired box protein Pax-5, with a Ki-67 rate of ~80%, small cell
neuroendocrine carcinoma was confirmed.
The post-operative diagnosis showed that the right
pulmonary small cell cancer was in an extensive stage, accompanied
with abdominal lymph node metastasis (www.nccn.org/professionals/physician_gls/f_guidelines.asp).
The patient presented with major discomfort on coughing, sputum
excretion and somnolence on January 27, 2014. Emergency blood gas
analysis indicated respiratory failure and retention of
CO2 (pH, 7.27; PCO2, 116.1 mmHg;
PO2, 104.5 mmHg; and HCO3-, 3.9 mmol/l). The
patient was then transferred to the Intensive Care Unit (ICU) for
respiratory assistance by non-invasive respirator. A blood routine
examination showed a white blood cell count of
18.74×109/l, and sputum culture showed growth of
Acinetobacter baumannii. The symptoms lessened after 2 days
of cefoperazone sodium (3 g, every 8 h) treatment.
However, the somnolence reappeared and the patient
presented with confusion on February 4, 2014. A blood gas analysis
revealed the following: pH, 7.20; PCO2, >130
mmHgPO2, 104 mmHg; and HCO3−, 29.5
mmol/l. The patient was once again transferred to the ICU for a
trachea cannula and respiratory assistance using a respirator.
Retention of CO2 decreased 4 days later, but the patient
experienced shortness of breath when the respirator was stopped.
Use of the respirator long-term would postpone the treatment of the
cancer, and aggravation of the cancer would make extubation even
more difficult. However, since small cell lung cancer is sensitive
to chemotherapy, alveolar recruitment and respiratory function
improvements may be a result of a reduced tumor size following
effective chemotherapy treatment. After communicating with the
patient's family members, chemotherapy was requested. Therefore,
the patient received one cycle of chemotherapy (30 mg cis-platinum
and 100 mg etoposide on days 1–3) while using a ventilator from
February 8–10, 2014. Knowledge of the patient's respiratory failure
and dependence on the ventilator meant that intake and output
volume, and renal function were under strict monitoring and control
during the chemotherapy treatment. In addition, ondansetron (8 mg,
every 12 h) was used in order to prevent gastrointestinal reactions
such as nausea and vomiting. And a gastric tube was used for
gastrointestinal decompression. The patient stopped using the
ventilator 10 days after the chemotherapy with a successful
extubation. Blood gas analysis results were as follows: pH, 7.47;
PCO2, 61.1 mmHg; PO2, 91.4 mmHg; and
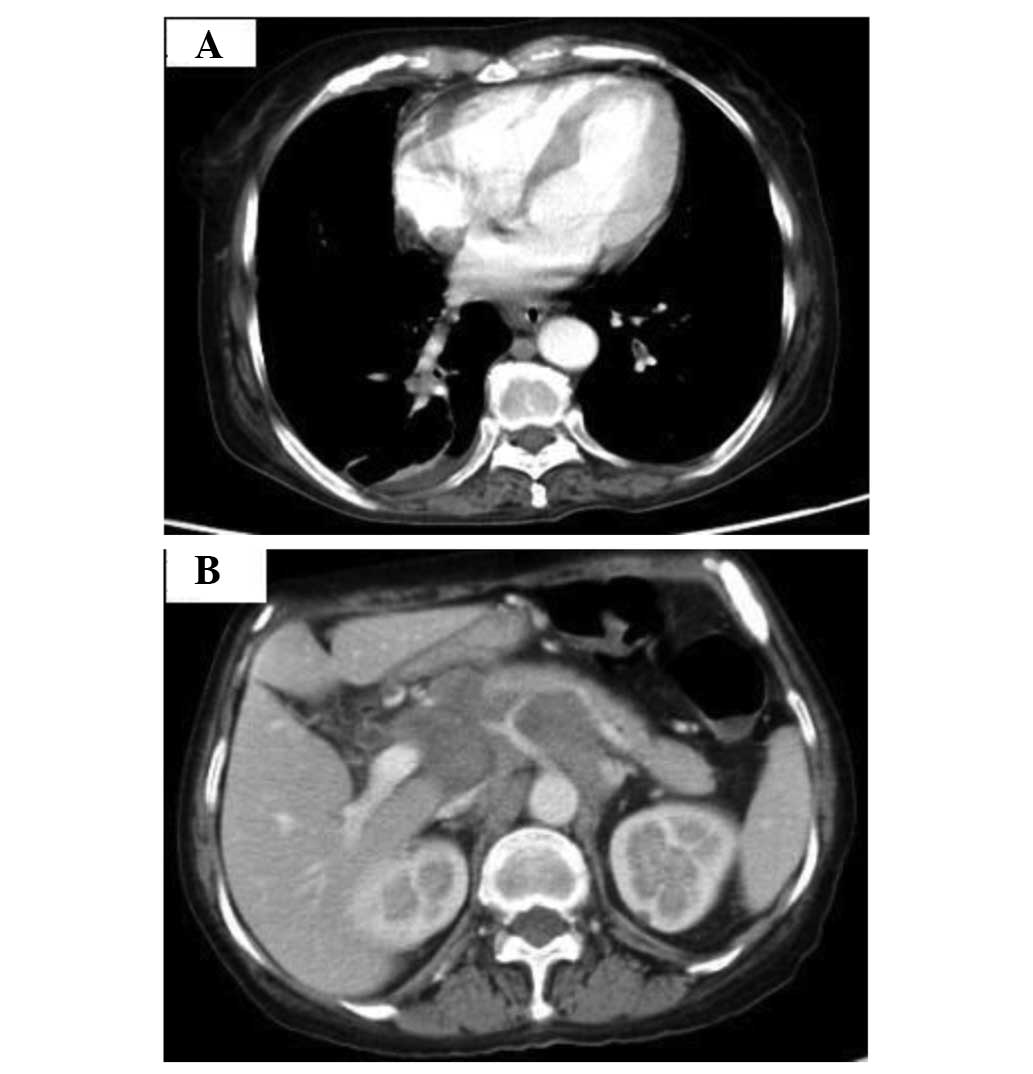
HCO3−, 43.9 mmol/l. CT scans of the chest and
abdominal area on February 24, 2014, showed that the mass located
at the hilus of the right lung was smaller than previously
(~3.9×3.1 cm). The pulmonary atelectasis in the lower lobe of the
right lung was less severe than prior to the treatment. The
multiple, syncretic and swollen lymph nodes of the hilus of the
right lung, abdomen and retroperitoneal area were reduced in number
and size. The lump in the abdomen was ~4.2×3.1 cm in size (Fig. 3). The general condition of the patient
improved and the ECOG score decreased to 1. The intake of oral
etoposide capsules (100 mg per day) beginning at the second cycle
of chemotherapy caused serious myelosuppression, and the patient
rejected oral medication half a month after the start of the
chemotherapy treatment. Follow-up was performed every 3 months by
telephone after the patient was discharged from the hospital. The
patient remained alive with an ECOG score of ~1 until October 2014,
but finally succumbed due to respiratory failure in November
2014.
Discussion
Small cell lung cancer is a type of malignant solid
tumor that is extremely sensitive to chemotherapy and radiotherapy,
with an objective remission rate of 50–70% in recent years
(4). The first-line treatments for
extensive-stage small cell lung cancer are chemotherapy-oriented
therapies for the whole body. For patients with a good physical
condition [Zubrod-ECOG-World Health Organization (ZPS) score
between 0 and 2], strategies such as standard-dose etoposide and
cisplatin (EP) and carboplatin and etoposide (CE) can be selected
(5,6).
For patient with a ZPS score between 3 and 4 points, based on the
best supportive treatment, the treatment details should be decided
with careful evaluations of the advantages and disadvantages
according to the comprehensive tumor score, the patient's
physiological functions, and the decisions of the patient and their
family (7,8).
In the present study, the patient was confirmed with
extensive-stage small cell lung cancer and required ventilator
support due to respiratory insufficiency prior to chemotherapy.
Furthermore, according to the ECOG standard for physical status
(ZPS, 5-points method) (5), the
patient had a dissatisfactory score of 4 points. According to ZPS
staging, the patient was not suitable for chemotherapy. Lastly, no
clinical report on implementing chemotherapy under ventilator
support exists in this field.
However, for this case, if the tumor could not be
controlled, long-term treatment with the ventilator may have
resulted in the patient developing a lung infection and even
succumbing to systemic failure. In the case of emergencies caused
by tumors that are sensitive to chemotherapy, chemotherapy
treatment could relieve symptoms and save the patient's life prior
to further treatments (9,10). The present patient exhibited normal
liver and kidney functions so that chemotherapy could be tolerated
regardless of the respiratory insufficiency. Additionally,
ventilator support was able to improve the respiratory function.
Therefore, it was determined that the patient may tolerate
chemotherapy. Additionally, further treatments may have performed
if the patient's condition improved after the first cycle of
chemotherapy.
The study results showed that the patient responded
to the chemotherapy well, with an improved health status (reduction
in tumor size and partial response), which reached the goal of a
successful treatment. The treatment experiences of this case
suggest that such patients who lose chemotherapy indications
according to traditional standard remain able to receive
chemotherapy and may obtain good results when the tumor is
sensitive to chemotherapy and supportive measures are
effective.
Acknowledgements
The authors greatly appreciate the assistance of the
staff of the Department of Thoracic Surgery, Sichuan Cancer
Hospital, Sichuan University, and thank them for their efforts.
References
|
1
|
Jett JR, Schild SE, Kesler KA and
Kalemkerian GP: Treatment of small cell lung cancer: Diagnosis and
management of lung cancer, 3rd ed: American College of Chest
Physicians evidence-based clinical practice guidelines. Chest.
2013:1432013.
|
|
2
|
Oken MM, Creech RH, Tormey DC, et al:
Toxicity and response criteria of the Eastern Cooperative Oncology
Group. Am J Clin Oncol. 5:649–655. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Meerbeeck JP, Fennell DA and De Ruysscher
DK: Small-cell lung cancer. Lancet. 378:1741–1755. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Von Pawel J, Schiller JH, Shepherd FA,
Fields SZ, Kleisbauer JP, Chrysson NG, Stewart DJ, Clark PI, Palmer
MC, Depierre A, et al: Topotecan versus cyclophosphamide,
doxorubicin, and vincristine for the treatment of recurrent
small-cell lung cancer. J Clin Oncol. 17:658–667. 1999.PubMed/NCBI
|
|
5
|
Buccheri G, Ferrigno D and Tamburini M:
Karnofsky and ECOG performance status scoring in lung cancer: A
prospective, longitudinal study of 536 patients from a single
institution. Eur J Cancer. 32A:1135–1141. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Verger E, Salamero M and Conill C: Can
Karnofsky performance status be transformed to the Eastern
Cooperative Oncology Group scoring scale and vice versa? Eur J
Cancer. 28A:1328–1330. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
DeVita VT Jr, Lawrence TS and Rosenberg
SA: Devita, Hellman & Rosenbergs Cancer: Principles and
Practice of Oncology (8th). Lippincott Williams and Wilkins. New
York: 2008.
|
|
8
|
Rubin P: Clinical Oncology: A
Multi-Disciplinary Approach for Physicians and Students (8th).
Saunders. London: 2001.
|
|
9
|
Hanna L, Crosby T and Macbeth F: Practical
Clinical Oncology. Cambridge University Press. New York: 2008.
View Article : Google Scholar
|
|
10
|
Jim Cassidy, Donald Bissett and Spence
RAJ: Oxford Handbook of Oncology. Oxford University Press. New
York: 2002.
|