Introduction
Squamous cell carcinoma (SCC), derived from
epidermal keratinocytes of the skin, is one of the most common and
malignant skin cancers (1),
accounting for 20% of all skin cancers. The disease usually
originates from certain types of skin or precancerous lesions.
Currently, there are ~1,000,000 new cases every year, and the
number of mortalities from this disease is gradually increasing
(2,3).
Human DNA-binding protein A (dbpA) is a
multifunctional protein containing a cold shock domain, and it
participates in gene transcription and translation by directly or
indirectly binding the target gene sequence (4,5). DbpA is
primarily expressed in the nucleus and the cytoplasm, and it acts
on the transcription, shear action and translation processes of
target genes (6,7). Previous studies have shown that dbpA is
upregulated in numerous tumour cells, and that this upregulation is
associated with the growth of the tumour cells and their resistance
to chemotherapy. Therefore, dbpA is considered a cancer prognosis
marker. The overexpression of dbpA in tumours usually indicates
that the proliferation and invasion of tumour cells is increasing
(8–10). Additionally, previous studies have
found that by regulating the expression of cyclin D1 and
upregulating the cell nuclear antigen, dbpA promotes tumour cell
proliferation, and that the increase in dbpA is closely associated
with the increase in the transcription factor, E2F transcription
factor 1 (E2F1) (10,11). These results demonstrated that dbpA
expression is closely associated with tumour development and
progression.
The effect of human anti-microbial protein 18
(hCAP-18) on tumour progression has drawn much attention (12). LL-37 is a cationic peptide composed of
37-amino acid residues in the hCAP-18 C-terminal, and it is the
only cathelin family member in the human body. LL-37 is also an
important component of the innate immune system, which is mediated
by neutrophils (12–14). In addition to its role against
bacterial infection, LL-37 also regulates immune activity,
angiogenesis and cell proliferation (13,15).
Studies have shown that LL-37 is not only upregulated in a variety
of solid tumours, but that it is also involved in the progression
mechanisms of a variety of tumours by promoting the proliferation,
migration and invasion of lung cancer, ovarian cancer, breast
cancer, prostate cancer and melanoma tumour cells (16–21).
Additionally, several studies have reported that these features may
be associated with formyl peptide receptor-like 1 (FPRL1),
epidermal growth factor receptor (EGFR) and insulin-like growth
factor 1 receptor (14,22–24). It is
unclear how LL-37 affects the proliferation and invasion of skin
squamous cells. DbpA is associated with tumour proliferation and
invasion. However, LL-37 stimulates dbpA expression in skin
squamous cells, and its effect on tumour cells is a focus of
interest.
In the present study, the effects of LL-37 on dbpA
expression and the changes in the dbpA concentration during the
proliferation and invasion of skin squamous cells were
investigated. The results showed that LL-37 may promote the
occurrence and development of skin squamous cells by upregulating
dbpA expression and that this process is mediated by the nuclear
factor-κB (NF-κB) signalling pathway.
Materials and methods
Tissue collection
Fresh skin SCC and adjacent normal tissues were
obtained from 18 patients who underwent surgery at the Department
of Dermatological Surgery, Second Affiliated Hospital of Xi'an
Jiaotong University (Xi'an, Shaanxi, China). A total of 18 samples
of normal tissues and 18 samples of SCC were obtained during
surgery. All tissues were embedded in liquid paraffin to form
tissue blocks. All skin SCC cases were clinically and
pathologically verified. Standard protocols established by the
Hospital's Protection of Human Subjects Committee were followed in
this study. Written informed consent was obtained from all patients
for publication of this study and the study was approved by the
Ethics Committee of the Second Affiliated Hospital of Xi'an
Jiaotong University.
Immunohistochemistry
The normal skin tissues, the uninvolved tissue of
the SCC and the lesions of the SCC were analysed via
immunohistochemistry. First, the paraffin-embedded blocks were
sliced into 4-µm sections and dewaxed in xylene, followed by
re-hydration in an alcohol gradient. Next, the tissues were
incubated on slides with rabbit anti-human dbpA polyclonal antibody
(catalog no. ab48952; Abcam, Cambridge, UK) at a 1:50 dilution. The
slides were placed in a humid environment at 4°C overnight, washed
twice with phosphate-buffered saline (PBS) and incubated in goat
anti-rabbit antibody (Abcam) at 37°C for 1 h. The slides were then
washed twice with PBS, stained with 3,3′-diaminobenzidine
(Sigma-Aldrich, Munich, Germany) and observed using a microscope.
Next, the slides were rinsed with PBS and re-stained with
haematoxylin for ~2 min. After mounting, the results were observed
using light microscopy. Normal skin tissue samples were used as the
negative controls.
Cell culture
A human SCC cell line (A431) was cultured in F12
medium (Gibco, Karlsruhe, Germany) containing 10% foetal bovine
serum (FBS; Gibco), 100 U/ml penicillin and 100 µg/ml streptomycin
(Sigma-Aldrich). The cells were cultured in a 37°C environment
containing 5% CO2.
Inhibiting the dbpA expression using
small interfering (si)RNA
The siRNA oligonucleotide sequence was synthesized
by Shanghai GenePharma (Shanghai, China) as follows: DbpA siRNA 1,
5′-GUCCUUGGCACUGUCAAAUTT-3′ (sense) and 5′-AUUUGACAGUGCCAAGGACTT-3′
(antisense); dbpA siRNA 2, 5′-GAGAGGCUGAAGAUAAAGATT-3′ (sense) and
5′-UCUUUAUCUUCAGCCUCUCTT-3′ (antisense); and dbpA siRNA 3,
5′-CUGCCAUCAAGAAGAAUAATT-3′ (sense) and 5′-UUAUUCUUCUUGAUGGCAGTT-3′
(antisense). The negative control duplexes of siRNA (siRNA-NC) were
random sequences and did not target any known mammalian gene
according to Genbank searches. The cells had a density of
1×105 cells/well and were seeded in 6-well plates. When
the fusion reached 70–80% ~24 h later, the cells were treated with
serum-free medium according to the manufacturer's instructions
(Lipofectamine 2000; Invitrogen; Thermo Fisher Scientific Inc.,
Waltham, MA, USA). Next, the cells were cultured for 48 h, and the
dbpA inhibition rate was analysed using western blotting.
Proliferation and invasion assay of
the transfected cells
The transfected cells were seeded at a density of
3×103 cells/well in 96-well plates. After 12 h, the
medium was replaced with serum-free medium and the cells were
cultured for another 24 h. Subsequently, 10 µl
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT;
5 mg/ml; Sigma-Aldrich) was added to each well and incubated for an
additional 4 h. The supernatant was discarded and 150 µl dimethyl
sulphoxide (Sigma-Aldrich) was added. The absorbance of each well
was measured at 490 nm using a microplate reader (Bio-Rad
Laboratories Inc., Hercules, CA, USA). The invasion assay was
performed using Transwell chambers (Costar; Corning Inc., Corning,
NY, USA) pre-coated with Matrigel (BD Biosciences, Heidelberg,
Germany). The transfected cells were cultured without serum for 12
h and then resuspended in serum-free medium, with the density
adjusted to 2.5×105 cells/ml. Next, 200 µl of cell
suspension was added to each Transwell chamber, and 500 µl of
culture medium with 10% FBS was added to the lower chamber. After
culturing for 24 h, the residual cells on the surface were gently
wiped away using a cotton swab. The cells that invaded the lower
chamber were stained with a staining solution (0.1% crystal violet
ethanol). Under a microscope (×200 magnification), three
representative fields were randomly selected and the average number
of invaded cells was calculated.
Cell proliferation assay
The cells were seeded at a density of
3×103 cells/well in 96-well plates. After 12 h, the
medium was replaced with serum-free medium and the cells were
cultured for an additional 24 h. The LL-37 (Sigma-Aldrich, Munich,
Germany) was used to stimulate the cells at 10 mg/ml for 24, 48 and
72 h. Next, the aforementioned MTT assay was used to evaluate the
degree of cell proliferation.
Migration and invasion assay after
LL-37 stimulation
The aforementioned Transwell assays were used to
test cell migration and invasion abilities after LL-37 stimulation.
In the upper chamber, a specific concentration (0.05, 0.5 or 5
µg/ml) of LL-37 was added. The chambers with pre-coated Matrigel
were used for invasion assays or without Matrigel for migration
assays.
Total RNA extraction and quantitative
polymerase chain reaction (qPCR)
TRIzol reagent (Sigma-Aldrich) was used to extract
total RNA from the A431 cells after stimulation by LL-37. The total
RNA (3 µg) was reverse transcribed to cDNA in a total volume of 20
µl using a reverse transcription reaction kit (Promega Corporation,
Madison, WI, USA). qPCR was performed using an Mx 3000P Real-Time
PCR system (Applied Biosystems; Thermo Fisher Scientific Inc.)
according to the manufacturer's instructions. SYBR Premix Ex Taq II
(Takara Biotechnologies Co., Ltd., Dalian, China) was used as a
DNA-specific fluorescent dye. PCR was performed for 50 cycles of
95°C for 10 sec and 60°C for 30 sec. Primer sequences for the
detection of mRNA expression were synthesized as follows: DbpA
specific primers, 5-CTCTACAGTTTCTCCATCTCCTAC-3 (forward) and
5-TTCTCGCCACCAAAGTCCT-3 (reverse); and human β-actin primers,
5-TTCCATATCGTCCCAGTTGGT-3 (forward) and 5-CCAGGGCGTTATGGTAGGCA-3
(reverse). The dbpA transcriptional level was corrected based on
the corresponding level of β-actin transcription. All the values
are from the results of at least three independent experiments.
Immunofluorescence staining
Once a monolayer of cells had been placed on the
climbing film, LL-37 of the appropriate concentration (0.05, 0.5 or
5 µg/ml) was added for 48 h. The cells were then fixed with 4%
paraformaldehyde at room temperature for 10 min, followed by
permeabilisation with 5% Triton X100 (Sigma-Aldrich) for 15 min.
The cells were then blocked with 2% goat serum for 30 min. The
cells were incubated with a rabbit anti-human dbpA polyclonal
antibody diluted at 1:50 (Abcam) overnight at 4°C, and washed 3
times with PBS. The cells were incubated with fluorescein
isothiocyanate-labelled goat anti-rabbit antibody (Abcam) at 37°C
for 1 h, washed with PBS 3 times and finally stained with DAPI
(Sigma, Munich, Germany) for 1 min. The cells were rinsed with PBS
and the staining intensity was observed using an inverted
fluorescence microscope (LSM 700; Zeiss GmbH, Jena, Germany).
Protein extraction and western blot
analysis
Total protein was extracted following LL-37
stimulation. Protein isolates (~10 µg) from each sample were
separated with 10% sodium dodecyl sulfate-polyacrylamide gel
electrophoresis and transferred to a polyvinylidene difluoride
membrane. The membrane was blocked with 5% skimmed milk and a 0.1%
Tween-20 phosphate-buffered solution at room temperature for 2 h,
and then treated with rabbit polyclonal anti-human dbpA antibody
diluted at 1:500 (Abcam) at 4°C overnight. Next, it was hybridized
with secondary antibody (1:5,000, Abcam) for 1 h. The results were
detected by exposing the film to enhanced chemiluminescence colour
detection solutions (EMD Millipore, Billerica, MA, USA).
Analysis of the signal transduction
pathways of the dbpA induction by LL-37
The SCC cells were seeded at 1×105
cells/well in 6-well plates. First, the cells were treated with the
mitogen-activated protein kinase (MAPK) kinase (MEK) inhibitor,
PD98059 (10 µM; Abcam), the p38/MAPK inhibitor, SB203580 (10 µM;
Abcam) and the NF-κB inhibitor, PDTC (1 µM; Abcam), for 30 min.
Next, LL-37 (0.5 µM) was added for 24 h. The protein was then
extracted for western blot analysis.
Statistical analysis
All data are presented as the mean ± standard
deviation. Pearson's χ2 test was used for the
immunohistochemical analysis. Student's t-test was used for
comparisons between groups and an analysis of variance was used for
three or more groups. All analyses were performed using SPSS 13.0
(SPSS Inc, Chicago, IL, USA). Results were considered statistically
significant at P<0.05.
Results
DbpA is upregulated in SCC
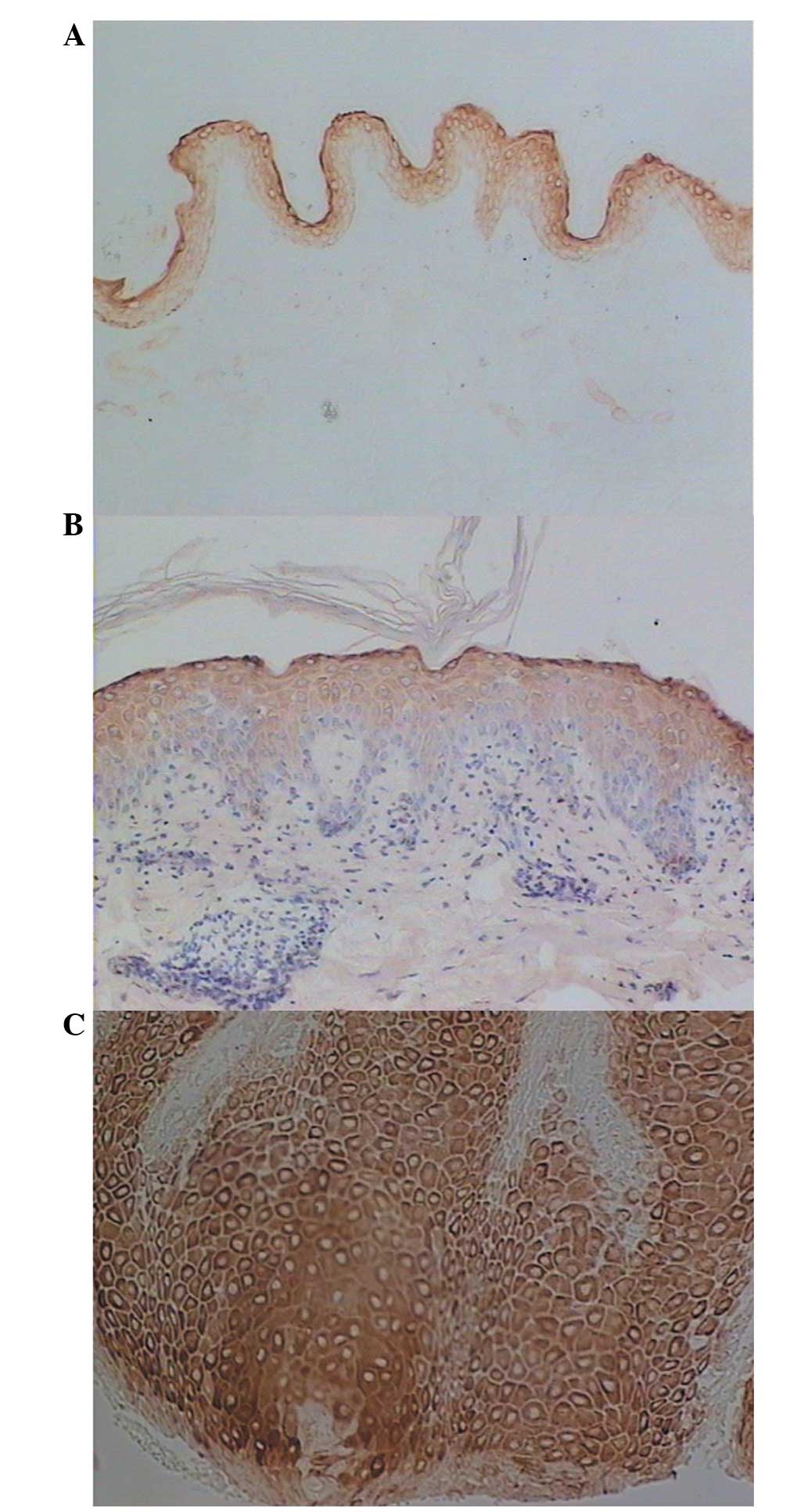
In the normal skin tissues, the dbpA protein was
strongly expressed in the granular layers and weakly expressed in
the upper layers of the stratum spinosum (Fig. 1A), and the positive rate in the
stratum spinosum was 20.0% (4/20). In the uninvolved epidermis of
SCC, dbpA was strongly expressed in the granular layers and in the
upper layers of the stratum spinosum (Fig. 1B), and the positive rate in the
stratum spinosum was 27.8% (5/18). However, in SCC, dbpA was
detected in significant quantities in nearly all of the tumour
cells (Fig. 1C), and the positive
rate was 83.3% (15/18). The dbpA expression in SCC was stronger
than that in the normal skin tissues (χ2=15.5;
P<0.01) or the uninvolved epidermis (χ2=10.7;
P<0.01).
dbpA siRNA decreases the protein
levels of dbpA, and reduces the proliferation and invasion of the
SCC cells
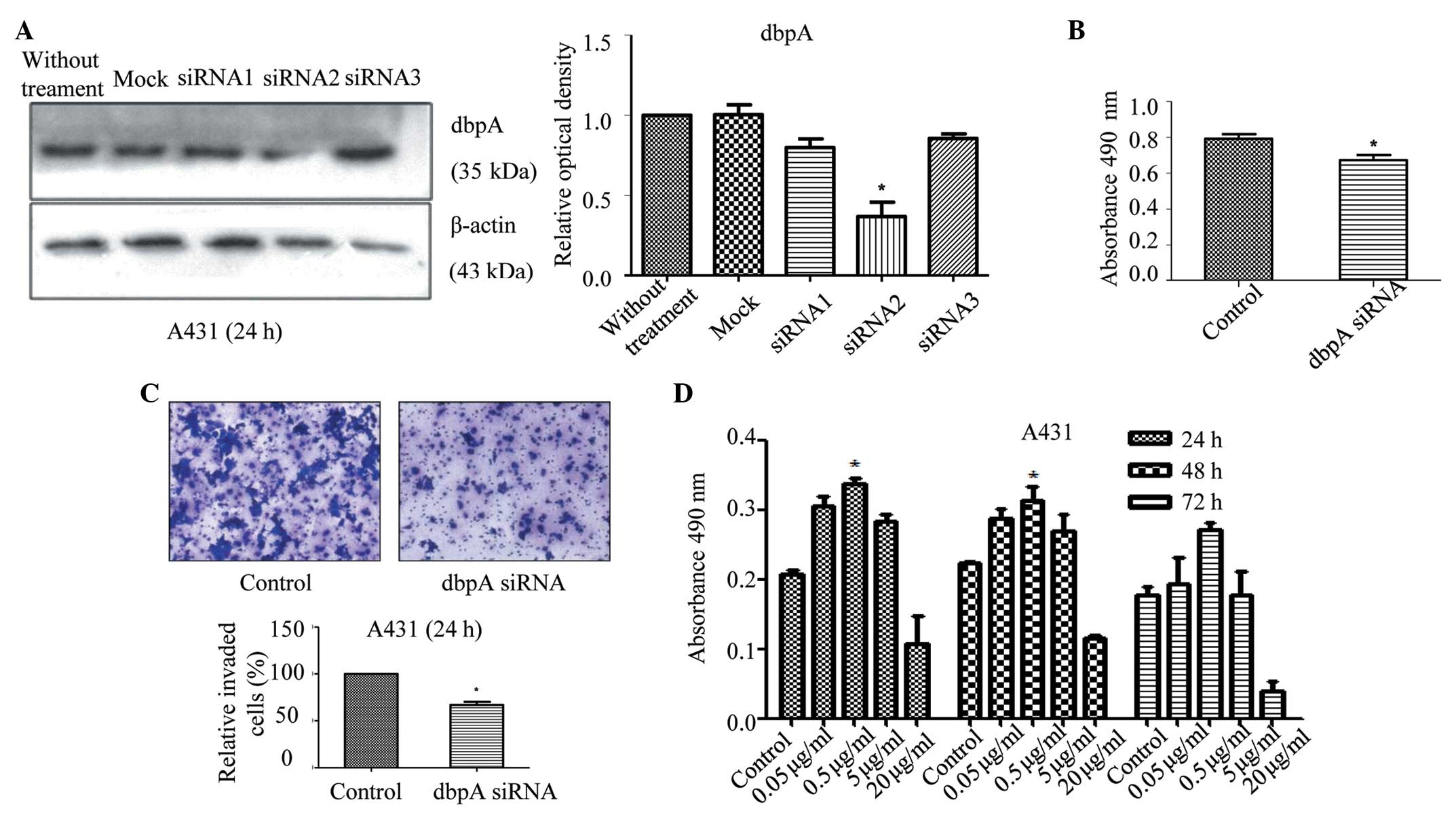
After 48 h of culture, total protein was extracted
from the transfected cells and analysed using western blotting.
Compared with the control group, the protein expression of dbpA in
the dbpA siRNA 2 group was significantly reduced (P=0.008; Fig. 2A); thus, dbpA siRNA 2 was chosen for
the subsequent experiments. Compared with the control group, cell
proliferation in the presence of the siRNA decreased after 24 h,
indicating that the dbpA expression was correlated with the
proliferation of the tumour cells (P=0.028; Fig. 2B). Transwell chambers coated with
Matrigel were used to study the invasion ability of the A431 cells
after inhibiting the dbpA expression. Compared with the control
group, the number of invading cells that crossed the membranes
diminished after 24 h, indicating that dbpA was correlated with the
invasiveness of the tumour cells (P<0.034; Fig. 2C). Thus, the inhibition of dbpA may
reduce the proliferation and invasiveness of A431 cells.
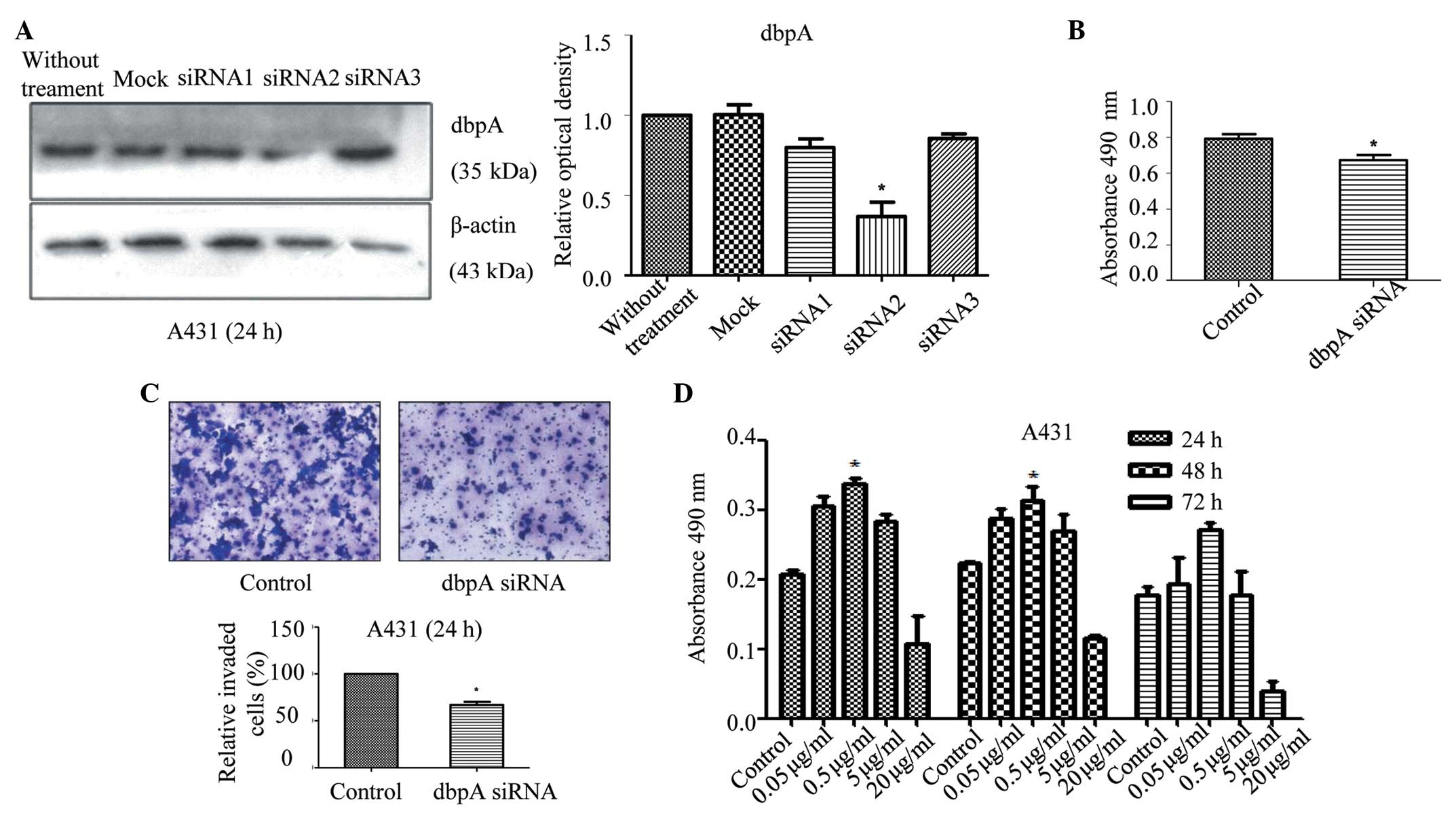 | Figure 2.(A) Expression of dbpA in A431 cells
after treatment with dbpA siRNA. Western blot analysis of dbpA and
β-actin expression in the dbpA siRNA(1–3) and
control siRNA groups. (B) DbpA siRNA reduced the proliferation
ability in the A431 cells. After treatment with dbpA siRNA for 24
h, an MTT assay was performed to analyse cell proliferation by
reading absorbance at 490 nm in each well using an automatic
microplate reader and (C) the invasion ability of the cells was
also assessed (magnification, ×200). (D) The proliferation of the
A431 cells was promoted by culturing with 0.05, 0.5, 5 or 20 µg/ml
LL-37 for 24, 48 or 72 h. Cell proliferation levels were also
analysed by MTT assay. The results from three independent
experiments are shown as the mean ± standard deviation. n=5 samples
in each group. *P<0.05 vs. control. siRNA, small interfering
RNA; dbpA, DNA-binding protein A; MTT,
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide. |
LL-37 promotes the proliferation of
SCC cells
The A431 cells were stimulated using different
concentrations of LL-37 and its effect on the cell proliferation
was observed at various time intervals. Compared with the control
group, stimulation with LL-37 at different times and concentrations
increased the proliferation of the A431 cells (Fig. 2D), and these increases were
significant for 24 or 48 h of culture with 0.5 µg/ml of LL-37
(P=0.028).
LL-37 promotes the migration and
invasion of SCC cells
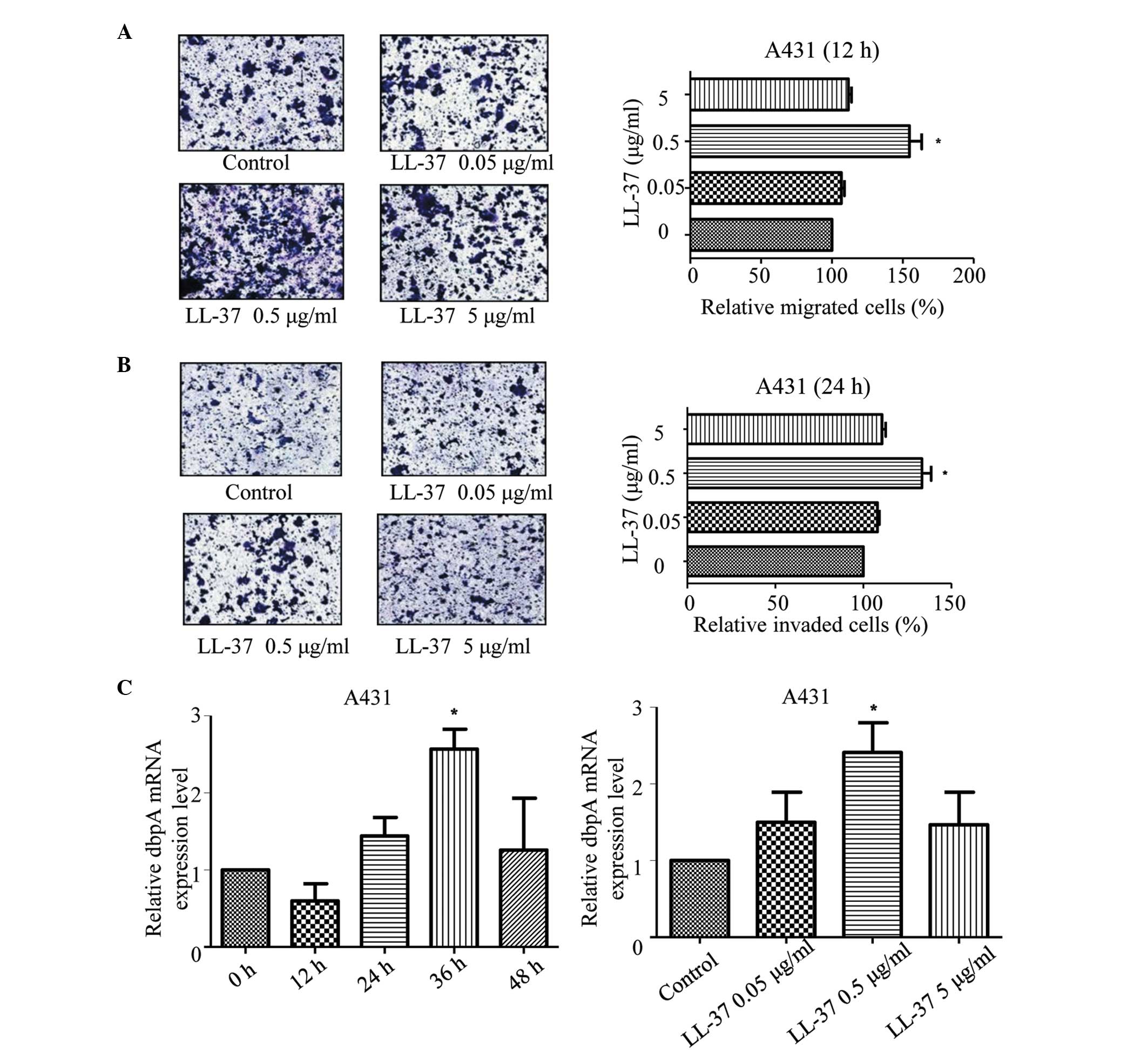
Compared with the control group, different
concentrations of LL-37 enhanced the migration of the A431 cells
after 12 h of culture (P=0.001; Fig.
3A) and the invasiveness of the A431 cells after 24 h of
culture (Fig. 3B). The most effective
concentration was 0.5 µg/ml (P=0.002).
LL-37 promotes the mRNA and protein
expression of dbpA in SCC cells
Compared with the control group, stimulation of the
A431 cells with LL-37 for 36 h increased the mRNA expression of
dbpA (P=0.004), with the most significant increase observed for 0.5
µg/ml LL-37 (P=0.003; Fig. 3C).
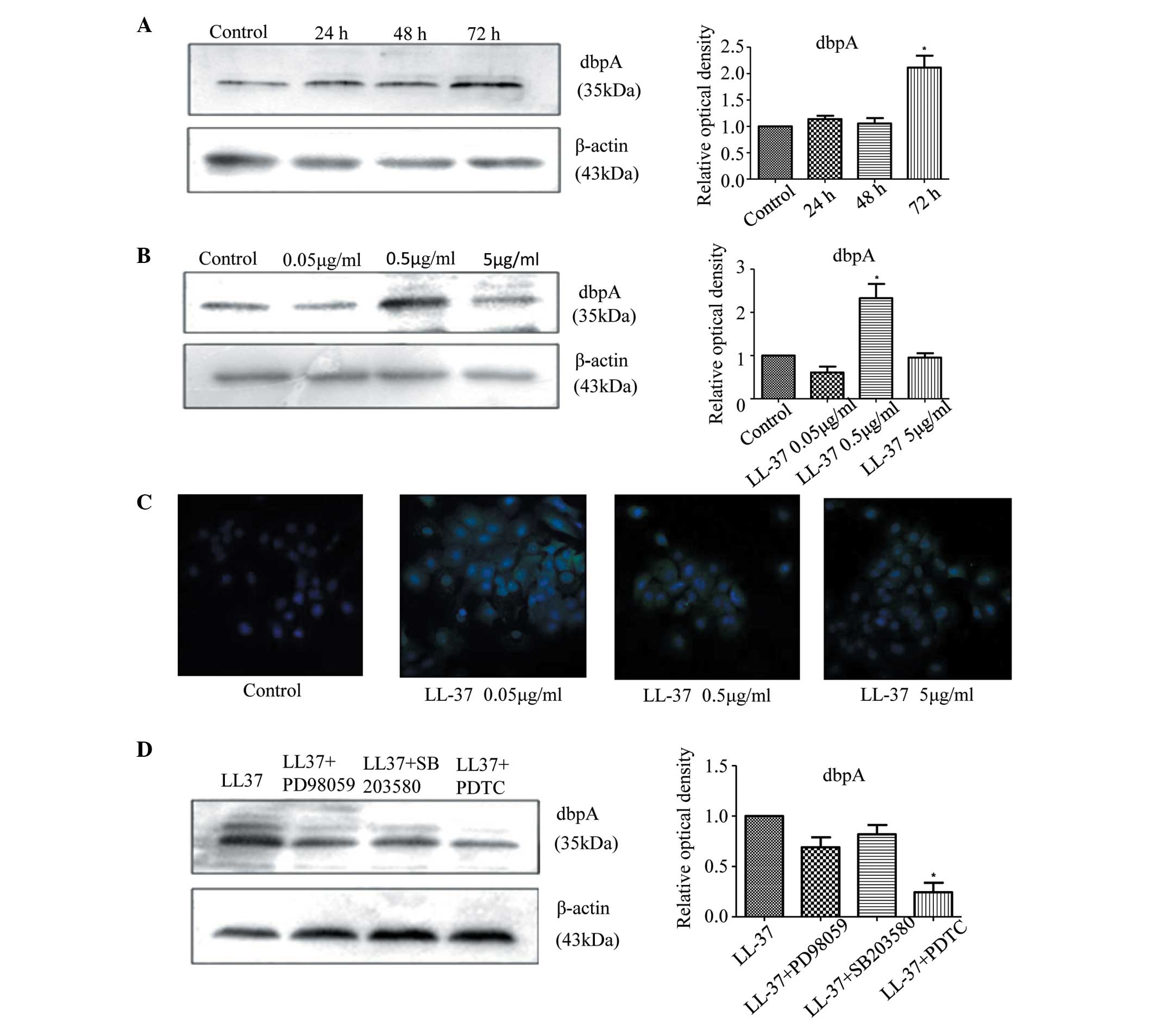
Western blot showed that after stimulating the A431 cells with
LL-37 for 72 h, the protein expression of dbpA increased (P=0.041;
Fig. 4A) and again, the most
significant increase was observed for 0.5 µg/ml LL-37 (P=0.029;
Fig. 4B). Moreover, stimulating the
A431 cells with various concentrations of LL-37 increased the
fluorescence intensity of dbpA immunostaining, and 0.5 µg/ml was
the most effective concentration (Fig.
4C). Thus, LL-37 promoted the expression of dbpA in the A431
cells.
An NF-κB inhibitor inhibits dbpA
expression induced by LL-37 in SCC cells
To study the signalling pathway downstream of LL-37
that induced the expression of dbpA, inhibition experiments were
performed. The A431 cells were pretreated with the MEK inhibitor,
PD98059, the p38/MAPK inhibitor, SB203580, and the NF-κB inhibitor,
PDTC, to inhibit the effect of LL-37 on the induction of dbpA
expression. PDTC significantly inhibited the LL-37-induced
expression of dbpA in the A431 cells (P=0.011; Fig. 4D), indicating that the increased dbpA
expression that was stimulated by LL-37 may occur via an NF-κB
signalling pathway.
Discussion
The present results indicated that dbpA was not
expressed in the basal layer in normal skin tissue, but its
expression increased in SCC as it was expressed in almost all of
the tumour cells. When stimulated by LL-37, the protein level of
dbpA increased in the cutaneous SCC cells in a time- and
concentration-dependent manner. The inhibition of the NF-κB
signalling pathway led to a lower amount of LL-37-induced dbpA
protein expression in the A431 cells. This indicated that LL-37
could regulate the expression of dbpA in the A431 cells and that
this process may occur via the activation of the NF-κB signalling
pathway.
LL-37 is a member of the antibacterial peptide
family and is correlated with the proliferation of epidermal cells
(13,14). Previous studies have shown that LL-37
can promote malignant tumours, including lung cancer, ovarian
cancer, melanoma, prostate cancer and oral SCC, and this process is
primarily associated with the upregulation of EGFR and the receptor
tyrosine kinase ErbB2 (25). Through
the induction of the membrane-associated protein kinase, EGFRs
cleave the matrix metalloproteinase (MMP), and LL-37 activates
EGFR. This process may be dependent on the G protein-coupled
receptors (GPCRs) present in different cell types (14,22–24). In
lung SCC, LL-37 stimulates the proliferation and invasion of tumour
cells, accompanied by its mitogenic effect of EGFR phosphorylation
and the subsequent activation of the Ras/MAPK cascade. EGFR
signalling in lung cancer cells plays a direct role in
proliferation, anti-apoptosis, angiogenesis generation, invasion
and metastasis (14,21). The majority of the EGFR ligands, such
as transforming growth factor and heparin-binding epidermal growth
factor, are expressed as soluble transmembrane precursors that are
released after cleavage by a protease. These precursors can diffuse
freely and bind and activate EGFR. Thus, the oncogenic effect of
LL-37 in certain tissues occurs via the activation of the
EGFR-mediated transcriptional mechanism (23,26,27). In
breast cancer, LL-37 promotes tumour progression via the
ErbB-mediated pathway, upregulating the expression of ErbB2 or EGFR
to enhance ErbB signalling, thereby promoting growth and metastasis
(19). Additionally, formyl peptide
receptor 2 (FPR2) may be involved in this process. LL-37 stimulates
the activation of MAPK and Janus kinase/signal transducer and
activator of transcription and undergoes a biochemical cascade with
transcription factor signalling, thereby leading to significant
activation of several transcription factors. This process may be
dependent on FPR2 or may be independent of it (22,24,28). In
ovarian cancer, the fact that LL-37 may stimulate cell
proliferation has been considered not dependent of the GPCR.
However, LL-37 enhances the invasiveness of ovarian cancer cells
via the upregulation of tissue remodelling enzymes, such as MMP-2,
and this enhancement is GPCR-mediated. FPR2 in ovarian cancer cells
can increase the expression of MMP-2, thus inhibiting or blocking
the invasive ability of the receptors of LL-37 and thereby
promoting the invasiveness of tumour cells (20,23,26,27).
Previous studies have shown that the Y box binding protein (Y-BOX)
family member of dbpA could regulate the proliferation of
epithelial cells and is abnormally expressed in liver cancer,
stomach cancer and other tumours (29–32). In
transgenic mice, the increase in FPR2 can promote the expression of
dbpA mRNA (11,33). Studies have also suggested that
proteins of the Y-BOX family regulate the expression of EGFR and
ErbB2. By binding to the EGFR receptor, Y-BOX proteins regulate the
transcription of these receptors by binding to the enhancer region
of the EGFR gene and to the promoter region of the ErbB2
(HER-2/neu) gene. EGFR and ErbB2 are considered to be associated
with the proliferation and invasion of epidermal tumours to
increase the degree of malignancy (6,8). A
previous study showed that the upregulation of dbpA during cell
proliferation is due to the upregulation of E2F1 activity. The E2F1
activity in cell proliferation and apoptosis is extremely
important. Therefore, dbpA is a downstream target of E2F1 that
promotes cell proliferation and transformation (10,34).
The results of the present study showed that the
expression of dbpA is increased in SCC. siRNA was used to inhibit
the expression of dbpA in A431 cells, and in vitro MTT and
Transwell invasion assays confirmed that the reduced expression of
dbpA inhibits the proliferation and invasion of A431 cells. The
A431 cells were stimulated with LL-37, and it was found that dbpA
mRNA expression increased as a function of time and concentration.
Immunofluorescence and western-blot analyses were used to detect
the dbpA cell protein expression changes in the A431 cells and dbpA
protein expression was also found to increase as a function of time
and concentration. These results suggested that LL-37 can
upregulate dbpA expression in A431 cells. A previous study
(35) reported that LL-37 increases
the degree of malignancy of tumour cells, and that this is
associated with the Ras/MAPK signalling cascade and the NF-κB
pathway. Therefore, inhibitors of the extracellular
signal-regulated kinase, MAPK and NF-κB signalling pathways were
tested and it was found that the increase in dbpA protein
expression that was induced by LL-37 could be blocked by the NF-κB
inhibitor. This result indicated that LL-37 upregulates dbpA
expression via the NF-κB signalling pathway. Through the induction
of EGFR to cleave MMP-2, LL-37 activates EGFR and ErbB2,
accompanied by the phosphorylation of EGFR and the activation of
the downstream Ras/MAPK cascade. This enhances the ErbB signal and
promotes the expression of MMP-2 via FPR2. Thus, EGFR, ErbB2 and
FPR2 are involved in the regulation of dbpA expression, and the
overexpression of these factors may increase the proliferation and
invasion of tumour cells, indicating that that LL-37 promotes the
proliferation and invasion of A431 cells by upregulating dbpA
expression. NF-κB is a transcription factor that is known to
regulate the expression of multiple genes and is involved in a wide
range of cellular responses. When found in tumour cells, LL-37 can
increase the levels of NF-κB p65, which can regulate the expression
of genes, such cyclin D1, to promote cell growth. The activation of
NF-κB has a significant role in promoting metastasis, and
inhibiting NF-κB can prevent the apoptotic process in tumour cells
(36). The present study showed that
the inhibition of the NF-κB signalling pathway suppressed the
upregulation of dbpA that was induced by the LL-37 in A431 cells,
indicating that this process is associated with the NF-κB
signalling pathway.
In conclusion, the present study confirms that the
expression of dbpA is increased in SCC, and that it can be a marker
for the degree of malignancy. The antimicrobial peptide LL-37
upregulates dbpA expression and promotes proliferation and invasion
in A431 cells. This process may be regulated by the activation of
the NF-κB signalling pathway. This study introduces a novel
perspective on the association between LL-37 and dbpA in SCC, and
provides a possible strategy for clinical drug development.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (grant nos. 81071299, 81371732 and
81573055) and was partially supported by the Fundamental Research
Funds for the Central Universities and for Changjiang Scholars and
Innovative Research Team in University (grant no. PCSIRT:1171).
References
|
1
|
Knackstedt TJ, Brennick JB, Perry AE, Li
Z, Quatrano NA and Samie FH: Frequency of squamous cell carcinoma
(SCC) invasion in transected SCC in situ referred for Mohs surgery:
The Dartmouth-Hitchcock experience. Int J Dermatol. 54:830–833.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rogers HW, Weinstock MA, Feldman SR and
Coldiron BM: Incidence estimate of nonmelanoma skin cancer
(keratinocyte carcinomas) in the US population, 2012. JAMA
Dermatol. 151:1081–1086. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sapijaszko M, Zloty D, Bourcier M, Poulin
Y, Janiszewski P and Ashkenas J: Canadian Non-melanoma Skin Cancer
Guidelines Committee: Non-melanoma skin cancer in Canada chapter 5:
Management of squamous cell carcinoma. J Cutan Med Surg.
19:249–259. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sakura H, Maekawa T, Imamoto F, Yasuda K
and Ishii S: Two human genes isolated by a novel method encode
DNA-binding proteins containing a common region of homology. Gene.
73:499–507. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kudo S, Mattei MG and Fukuda M:
Characterization of the gene for dbpA, a family member of the
nucleic-acid-binding proteins containing a cold-shock domain. Eur J
Biochem. 231:72–82. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Balda MS and Matter K: The tight junction
protein ZO-1 and an interacting transcription factor regulate
ErbB-2 expression. EMBO J. 19:2024–2033. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wolffe AP: Structural and functional
properties of the evolutionarily ancient Y-box family of nucleic
acid binding proteins. Bioessays. 16:245–251. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kohno K, Izumi H, Uchiumi T, Ashizuka M
and Kuwano M: The pleiotropic functions of the Y-box-binding
protein, YB-1. Bioessays. 25:691–698. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Uramoto H, Izumi H, Ise T, Tada M, Uchiumi
T, Kuwano M, Yasumoto K, Funa K and Kohno K: p73 Interacts with
c-Myc to regulate Y-box-binding protein-1 expression. J Biol Chem.
277:31694–31702. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sourisseau T, Georgiadis A, Tsapara A, Ali
RR, Pestell R, Matter K and Balda MS: Regulation of PCNA and cyclin
D1 expression and epithelial morphogenesis by the ZO-1-regulated
transcription factor ZONAB/DbpA. Mol Cell Biol. 26:2387–2398. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tobita H, Kajino K, Inami K, Kano S, Yasen
M, Imamura O, Kinoshita Y and Hino O: Gene expression profile of
DNA binding protein A transgenic mice. Int J Oncol. 29:673–679.
2006.PubMed/NCBI
|
|
12
|
Dürr UH, Sudheendra US and Ramamoorthy A:
LL-37, the only human member of the cathelicidin family of
antimicrobial peptides. Biochim Biophys Acta. 1758:1408–1425. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bucki R, Leszczynska K, Namiot A and
Sokolowski W: Cathelicidin LL-37: A multitask antimicrobial
peptide. Arch Immunol Ther Exp (Warsz). 58:15–25. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wu WK, Wang G, Coffelt SB, Betancourt AM,
Lee CW, Fan D, Wu K, Yu J, Sung JJ and Cho CH: Emerging roles of
the host defense peptide LL-37 in human cancer and its potential
therapeutic applications. Int J Cancer. 127:1741–1747. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Coffelt SB and Scandurro AB: Tumors sound
the alarmin(s). Cancer Res. 68:6482–6485. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hensel JA, Chanda D, Kumar S, Sawant A,
Grizzle WE, Siegal GP and Ponnazhagan S: LL-37 as a therapeutic
target for late stage prostate cancer. Prostate. 71:659–670. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gill K, Mohanti BK, Singh AK, Mishra B and
Dey S: The over expression of cathelicidin peptide LL37 in head and
neck squamous cell carcinoma: The peptide marker for the prognosis
of cancer. Cancer Biomark. 10:125–134. 2011.2012. PubMed/NCBI
|
|
18
|
Kim JE, Kim HJ, Choi JM, Lee KH, Kim TY,
Cho BK, Jung JY, Chung KY, Cho D and Park HJ: The antimicrobial
peptide human cationic antimicrobial protein-18/cathelicidin LL-37
as a putative growth factor for malignant melanoma. Br J Dermatol.
163:959–967. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Heilborn JD, Nilsson MF, Jimenez CI,
Sandstedt B, Borregaard N, Tham E, Sørensen OE, Weber G and Ståhle
M: Antimicrobial protein hCAP18/LL-37 is highly expressed in breast
cancer and is a putative growth factor for epithelial cells. Int J
Cancer. 114:713–719. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Coffelt SB, Waterman RS, Florez L, Höner
zu Bentrup K, Zwezdaryk KJ, Tomchuck SL, LaMarca HL, Danka ES,
Morris CA and Scandurro AB: Ovarian cancers overexpress the
antimicrobial protein hCAP-18 and its derivative LL-37 increases
ovarian cancer cell proliferation and invasion. Int J Cancer.
122:1030–1039. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
von Haussen J, Koczulla R, Shaykhiev R,
Herr C, Pinkenburg O, Reimer D, Wiewrodt R, Biesterfeld S, Aigner
A, Czubayko F, et al: The host defence peptide LL-37/hCAP-18 is a
growth factor for lung cancer cells. Lung Cancer. 59:12–23. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Coffelt SB, Tomchuck SL, Zwezdaryk KJ,
Danka ES and Scandurro AB: Leucine leucine-37 uses formyl peptide
receptor-like 1 to activate signal transduction pathways, stimulate
oncogenic gene expression, and enhance the invasiveness of ovarian
cancer cells. Mol Cancer Res. 7:907–915. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Coffelt SB, Marini FC, Watson K, Zwezdaryk
KJ, Dembinski JL, LaMarca HL, Tomchuck SL, Honer zu Bentrup K,
Danka ES, Henkle SL and Scandurro AB: The pro-inflammatory peptide
LL-37 promotes ovarian tumor progression through recruitment of
multipotent mesenchymal stromal cells. Proc Natl Acad Sci USA.
106:3806–3811. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Girnita A, Zheng H, Grönberg A, Girnita L
and Ståhle M: Identification of the cathelicidin peptide LL-37 as
agonist for the type I insulin-like growth factor receptor.
Oncogene. 31:352–365. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Choi KY, Napper S and Mookherjee N: Human
cathelicidin LL-37 and its derivative IG-19 regulate
interleukin-32-induced inflammation. Immunology. 143:68–80. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chuang CM, Monie A, Wu A, Mao CP and Hung
CF: Treatment with LL-37 peptide enhances antitumor effects induced
by CpG oligodeoxynucleotides against ovarian cancer. Hum Gene Ther.
20:303–313. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Li D, Wang X, Wu JL, Quan WQ, Ma L, Yang
F, Wu KY and Wan HY: Tumor-produced versican V1 enhances
hCAP18/LL-37 expression in macrophages through activation of TLR2
and vitamin D3 signaling to promote ovarian cancer progression in
vitro. PLoS One. 8:e566162013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kittaka M, Shiba H, Kajiya M, Ouhara K,
Takeda K, Kanbara K, Fujita T, Kawaguchi H, Komatsuzawa H and
Kurihara H: Antimicrobial peptide LL37 promotes vascular
endothelial growth factor-A expression in human periodontal
ligament cells. J Periodontal Res. 48:228–234. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Yasen M, Kajino K, Kano S, Tobita H,
Yamamoto J, Uchiumi T, Kon S, Maeda M, Obulhasim G, Arii S and Hino
O: The up-regulation of Y-box binding proteins (DNA binding protein
A and Y-box binding protein-1) as prognostic markers of
hepatocellular carcinoma. Clin Cancer Res. 11:7354–7361. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zhang LL, He DL, Li X, Li L, Zhu GD, Zhang
D and Wang XY: Overexpression of coxsackie and adenovirus receptor
inhibit growth of human bladder cancer cell in vitro and in vivo.
Acta Pharmacol Sin. 28:895–900. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Guay D, Garand C, Reddy S, Schmutte C and
Lebel M: The human endonuclease III enzyme is a relevant target to
potentiate cisplatin cytotoxicity in Y-box-binding protein-1
overexpressing tumor cells. Cancer Sci. 99:762–769. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wang GR, Zheng Y, Che XM, Wang XY, Zhao
JH, Wu KJ, Zeng J, Pan CE and He DL: Upregulation of human DNA
binding protein A (dbpA) in gastric cancer cells. Acta Pharmacol
Sin. 30:1436–1442. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Koike K, Uchiumi T, Ohga T, Toh S, Wada M,
Kohno K and Kuwano M: Nuclear translocation of the Y-box binding
protein by ultraviolet irradiation. FEBS Lett. 417:390–394. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Arakawa Y, Kajino K, Kano S, Tobita H,
Hayashi J, Yasen M, Moriyama M, Arakawa Y and Hino O: Transcription
of dbpA, a Y box binding protein, is positively regulated by E2F1:
Implications in hepatocarcinogenesis. Biochem Biophys Res Commun.
322:297–302. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Bandurska K, Berdowska A,
Barczyńska-Felusiak R and Krupa P: Unique features of human
cathelicidin LL-37. Biofactors. 41:289–300. 2015.PubMed/NCBI
|
|
36
|
Liu J and Du L: PERK pathway is involved
in oxygen-glucose-serum deprivation-induced NF-κB activation via
ROS generation in spinal cord astrocytes. Biochem Biophys Res
Commun. 467:197–203. 2015. View Article : Google Scholar : PubMed/NCBI
|