Introduction
Gliomas, as brain intrinsic neoplasms, are the most
common primary brain tumors in adults, and are classified by the
World Health Organization into four malignancy grades (I–IV)
(1,2).
When visualized using computed tomography (CT) or magnetic
resonance image (MRI), glioma may appear as a solid or cystic
lesion with an unclear boundary. The lesions are clearly enhanced
on contrast enhanced CT or MRI scans (3). Glioma coexisting with cerebrovascular
malformation in the brain is rare, with only a few cases reported
in the literature at present (4–7).
Angiographically occult cerebrovascular malformation (AOVM) is a
small vascular malformation that is not visible on digital
subtraction angiography (DSA). It comprises cavernous hemangioma,
arteriovenous malformation (AVM), intravenous vascular malformation
and capillary expansion. There may be no obvious symptoms of AOVM
until hemorrhage occurs. Diagnosis of AOVM is difficult, but MRI
may be considered as the first choice of diagnostic method, as it
is superior to CT or DSA (8–11). This superiority is due to a number of
reasons: MRI is able to show lesions more clearly compared with CT
or DSA; MRI is able to more specifically identify AOVM compared
with CT and DSA; MRI results may allow collection of data that can
contribute to the surgical strategy; MRI allows visualization of
the association between the AOVM and adjacent brain tissues; MRI
allows clearer visualization of the feeding and draining arteries,
compared with CT and DSA; and MRI is able to identify smaller AOVMs
more easily than CT and DSA.
As its incidence is low and diagnosis is
challenging, the diagnosis of glioma coexisting with AOVM is rare
and has been reported in extremely few cases in the literature
(4,5,12–14). Cemil et al (4) reported the case of a 58-year-old man
presenting with sudden development of severe headache and vomiting,
who was subsequently diagnosed with glioblastoma multiforme
combined with arteriovenous malformation following MRI examination.
Misdiagnosis and missed diagnosis are common in cases of glioma
coexisting with AOVM, which can sometimes lead to unfavorable
surgical outcomes. The present study reports a rare case of glioma
coexisting with AOVM, in order to improve the understanding of this
disease and prevent missed diagnosis and misdiagnosis.
Case report
A 30-year-old man presented in November 2014 as
Huishan People's Hospital (Wuxi, China), with a sudden syncope and
aphasia, with the symptoms gradually deteriorating over a 3-h
period. The patient had no medical history of trauma, hypertension
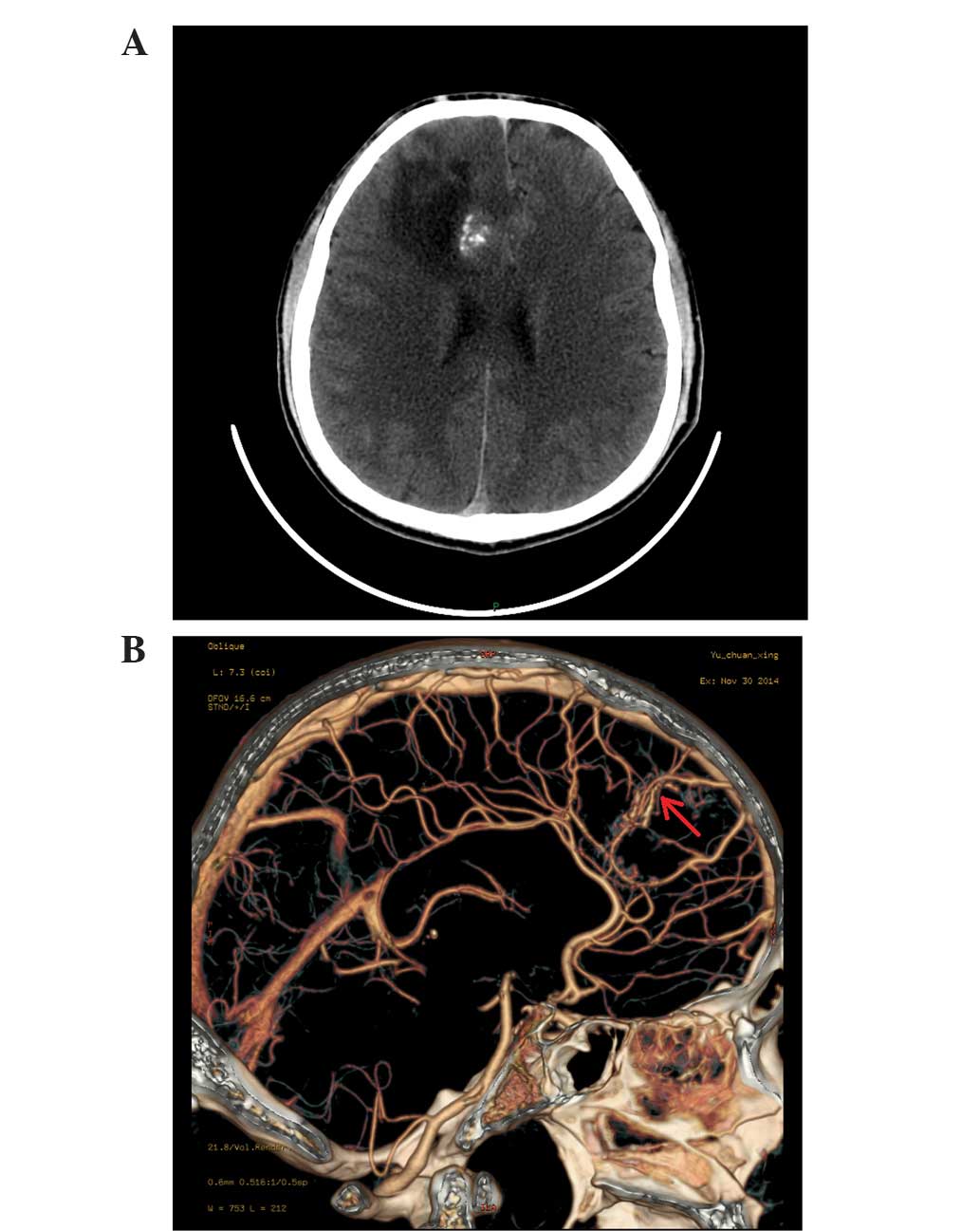
or any other condition. CT scans performed at the local community
hospital (Huishan People's Hospital, Wuxi, China) revealed a
calcified, edematous, minimal subarachnoid hemorrhage in the right
frontal lobe. The patient was then referred to the 101st Hospital
of People's Liberation Army (Wuxi, China) within 3 h of the
original presentation, where physical examination and routine blood
tests were performed, with normal results. CT scans revealed a
large area of edema and calcification in the right frontal lobe;
however, no subarachnoid hemorrhage was observed in that area
(Fig. 1A). Due to the similar
radiologic characteristics on CT angiography (CTA) to
cerebrovascular malformation, a cerebrovascular malformation in the
right frontal lobe was suspected (Fig.
1B). However, abnormal cerebrovascular malformation was not
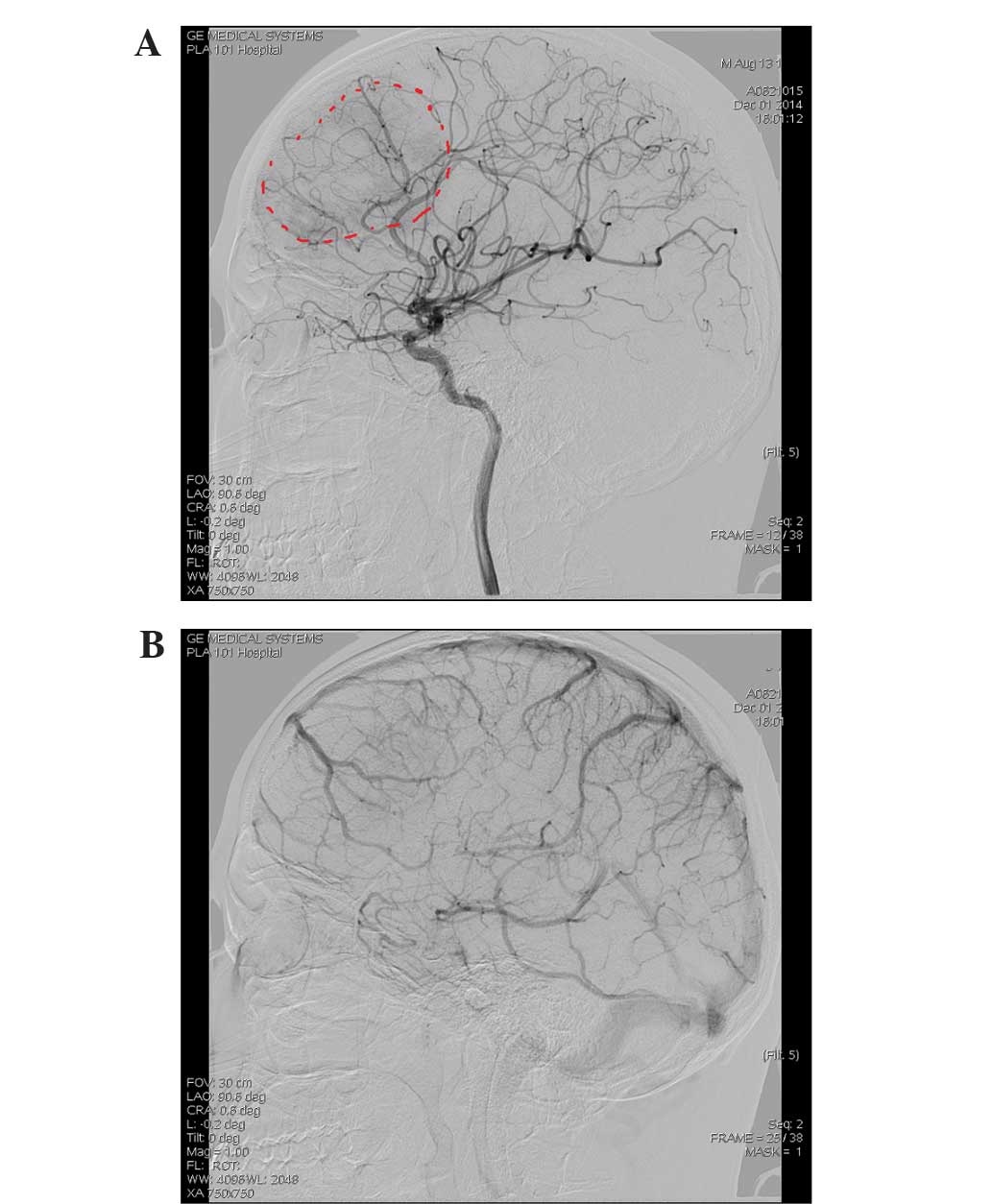
observed at the arterial and venous phases during DSA, but an
abnormally stained area was revealed following injection of
contrast medium (Fig. 2A and B),
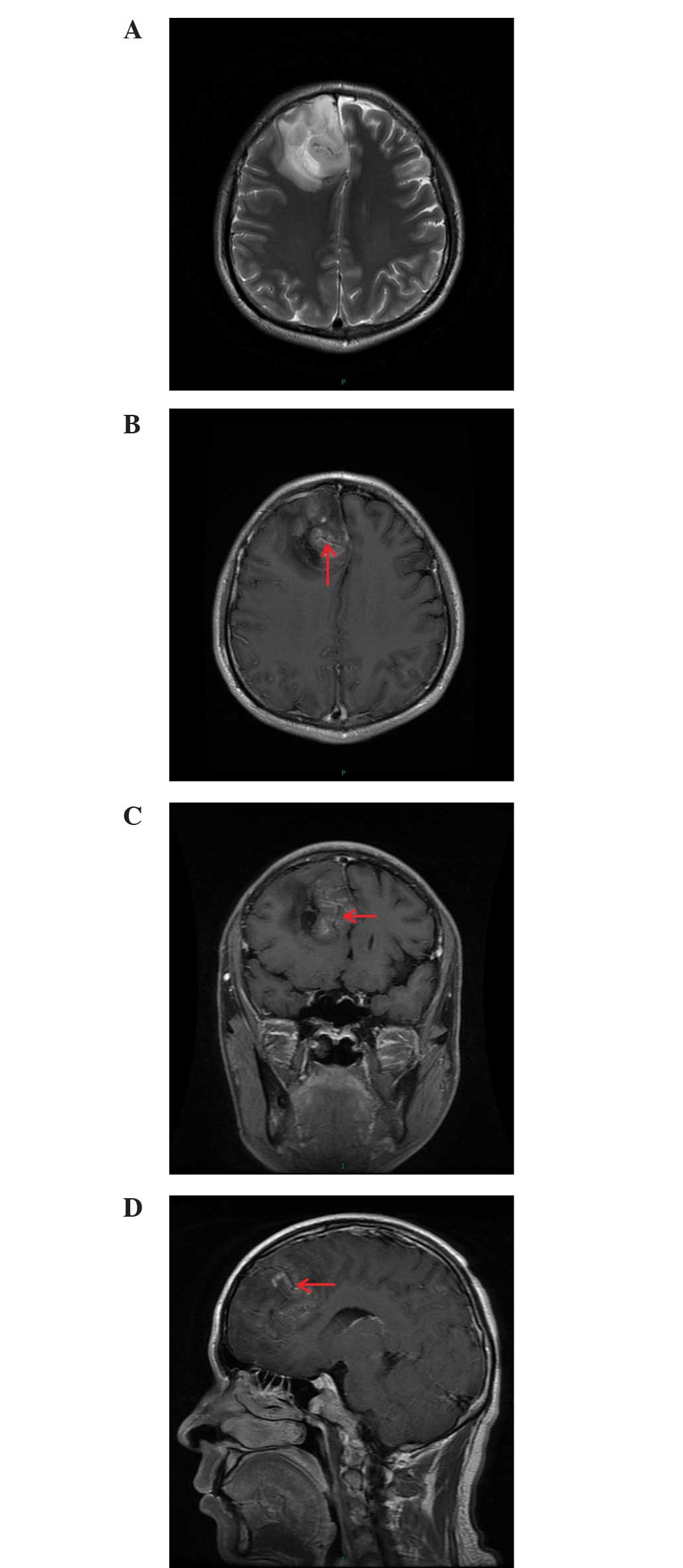
which indicated the presence of abnormal tissue. MRI examination
assessment by T1-weight (T1W), gradient-echo T2 (T2) and dynamic
contrast-enhanced MRI revealed mixed signals with long T1 and long
T2 signals, and a 5.8×5.2×6.0-cm cystic and necrotic lesion with no
clear margin in the right frontal lobe. The lesion also exhibited
dark signals similar to caput medusae on T2W images. In addition,
an edema belt (Fig. 3A-D) around the
lesion was observed. Thus, MRI confirmed the prediction that the
lesion was a glioma with coexistence of a cerebrovascular
malformation.
The negative DSA result led to an initial
misdiagnosis and missed diagnosis. The bleeding, calcification and
brain edema found on CT examination had indicated that an AVM was
most likely, and the CTA appeared to confirm this. However, the
gold-standard DSA examination did not confirm the diagnosis of an
AVM. In order to help explain this inconsistency, MRI was performed
which found an AVM and a brain tumor; this explained the
calcification and brain edema identified by the CT scans. It also
explained the sole finding of an AVM by CTA and the abnormal
staining on the DSA. In combination, these examinations provided
the best interpretation of the results.
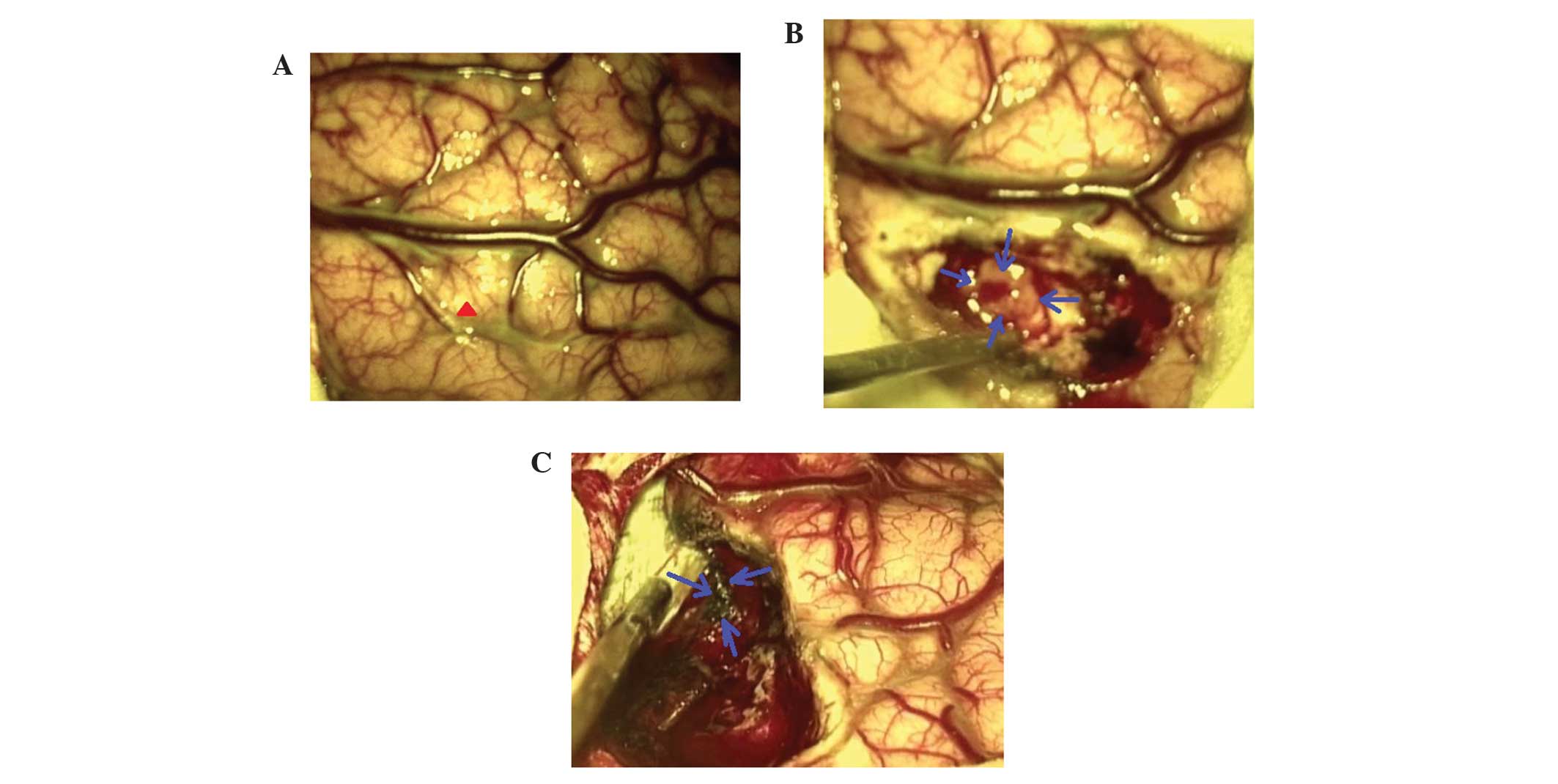
Following adequate imaging examination, as detailed
above, physician-patient communication and academic discussion,
surgery was performed. Following the administration of tracheal
intubation and general anesthesia, the patient underwent right
frontotemporal craniotomy (longitudinal fissure + pterion). The
cerebral cortex was incised between the frontotemporal and middle
frontal veins (Fig. 4A). A diseased
tissue and abnormal honeycomb mass, 5×3×4-cm in size, was removed
piece by piece (Fig. 4B).
Frontotemporal craniotomy was closed after achieving a good
haemostasis. A postoperative CT scan revealed no hemorrhagic
complications and the patient was sent to the neurosurgery
intensive-care unit.
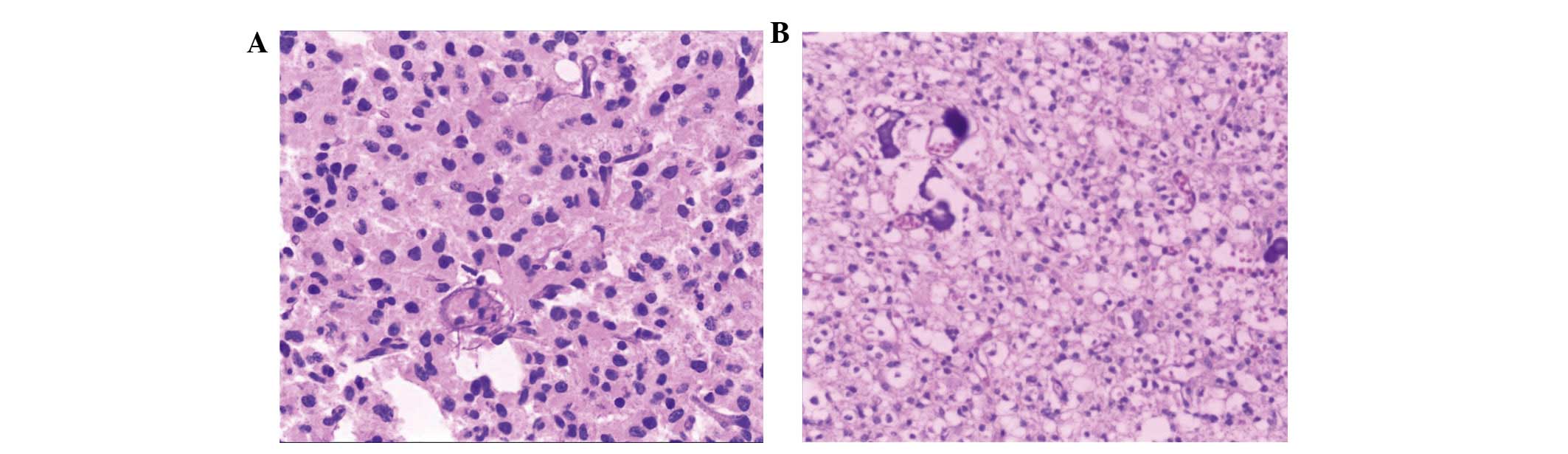
Following removal of the lesion from the patient,
the tumor was immediately fixed in neutral formalin liquid,
followed by embedding in paraffin 24 h later. The tissue was sliced
into 2 mm specimens and stained with hematoxylin and eosin. Stained
tumor samples were observed under a light microscope (Olympus
Corporation, Tokyo, Japan).
The patient received general treatment (0.4 g/day
aminomethylbenzoic acid injection; 60 mg/day lansoprazole
injection; 30 mg/day nimodipine injection; 1200 mg/day sodium
valproate injection; 6 g/day piperacillin-sulbactam; 500 ml/day
glucose injection) for 10 days, and was subsequently discharged 10
days after surgery without complications. MRI scan performed at the
6-month follow-up showed that the diseased lesion had been
completely removed.
Postoperative histopathological examination revealed
that glioma cells and Nidus confirmed an AOVM coexisting with
glioma (Fig. 5).
Discussion
Glioma coexisting with AVM are rare, and as AOVM has
a high rate of missed diagnosis and misdiagnosis, glioma coexisting
with AOVM simultaneously in the same location are extremely rare in
the clinic. Certain studies have suggested that the occurrence of
two lesions within the same tissue may be coicindental (12,13,15). Other
studies have reported that two lesions may be preoperatively
diagnosed as one (4,14). This was the case in the present study,
where the patient was initially diagnosed with AVM by CT and CTA.
Intraoperative and histopathological examination finally confirmed
the additional presence of the glioma, co-occurring with AOVM.
Other studies did not regard the coexistence of the
two lesions as fortuitous, and it was suggested that the lesions
had an effect on one another (4,5,16). Harris et al (16) reported that glioblastoma multiforme
can improve the overexpression of vascular endothelial growth
factor (VEGF); however, the expression of VEGF was high in the
endothelial layer and media of AVM vessels (17). VEGF can promote growth of endothelial
cells of blood vessels and the glioma cells can promote growth,
migration and tubular formation of endothelial cells. VEGF plasma
concentrations were significantly higher in patients with cerebral
AVMs compared to a healthy control group (18). Zuccarello et al (19) observed notable glial cell
proliferation around the AVM and large glial cells gathered among
abnormal blood vessels.
The wide clinical use of CT, MRI and DSA may
markedly improve the accuracy in the diagnosis of intracranial
tumors and cerebrovascular disease. However, the incidence of
missed diagnosis and misdiagnosis in the two diseases coexisting in
the same lesion remains high, particularly in combination with
AOVM. Despite DSA being considered the gold standard for the
diagnosis of AVM, certain AOVMs cannot be found, which may lead to
frequent misdiagnosis. Possible reasons for misdiagnosis include:
i) Compression and destruction of blood vessels by tumor tissue,
hematoma and edema, resulting in a lack of blood flow and vascular
occlusion occurs at early time; ii) cerebral vasospasm or thrombus
after bleeding caused by blood vessels in AVM; and iii) failure of
DSA to detect the afferent arteries of AVM, due to their very fine
nature; iv) small size meaning that the AVM is not identified by CT
or DSA (20,21).
In the present case, CTA revealed a suspicious
cerebrovascular malformation, but DSA examination was negative,
which resulted in preoperative diagnosis being challenging. MRI
confirmed AVM coexisted with GBM preoperatively, which was also
confirmed by postoperative histopathological examination. MRI plays
an important role in the diagnosis of intracranial tumors
coexisting with AOVM, as it not only shows the size, boundary and
blood supply of the tumor clearly, but may also provide an
important diagnostic basis, as its special ‘flow-empty actions’; as
the blood flows very fast, this leads to the MR signal being
produced a distance away from the reception range, meaning that no
MR signal is produced (22). In
addition, it is important that MR angiography (MRA) and MR
venography (MRV) may clearly reveal the feeding arteries and
drainage venous of AVM, which is valuable for surgery. Therefore,
MRI, MRA and MRV should be performed in case of doubt or
inconsistencies in CTA or DSA preoperative results.
Microsurgical treatment is considered the best
treatment for glioma coexisting with AOVM (12,13). Both
lesions should be removed through the same incision, unless they
are in different sites. The more dangerous lesion of the two should
be removed first to avoid intraoperative bleeding. In the present
case, the glioma was concluded to be more dangerous than the AOVM,
and thus was removed first. A definite preoperative diagnosis is
key to the success of the surgery.
In conclusion, the present study reported an
extremely rare case of glioma coexisting with AOVM. The imaging
features of the disease, as detected by CT, CTA, DSA and MRI, that
aided with the challenging diagnosis were described. Based on the
findings of the present study, if CTA suggests cerebrovascular
malformation AOVM should be considered, even if the DSA examination
result is negative. MRI plays an important role in the diagnosis of
combined lesions. When possible, complete microsurgical resection
of those lesions is the best choice. Adequate preoperative imaging
evaluation is key to the success of the surgery.
Acknowledgements
The authors would like to thank Yuan Gao (College of
Life Science, University of Science and Technology of China, Hefei,
China) for technical and language assistance.
References
|
1
|
DeAngelis LM: Brain tumors. N Engl J Med.
344:114–123. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Louis DN, Ohgaki H, Wiestler OD, Cavenee
WK, Burger PC, Jouvet A, Scheithauer BW and Kleihues P: The 2007
WHO classification of tumours of the central nervous system. Acta
Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ricard D, Idbaih A, Ducray F, Lahutte M,
Hoang-Xuan K and Delattre JY: Primary brain tumours in adults.
Lancet. 379:1984–96. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cemil B, Tun K, Polat O, Ozen O and
Kaptanoglu E: Glioblastoma multiforme mimicking arteriovenous
malformation. Turk Neurosurg. 19:433–436. 2009.PubMed/NCBI
|
|
5
|
Aucourt J, Jissendi P, Kerdraon O and
Baroncini M: Neuroimaging features and pathology of mixed
glioblastoma-AVM complex: A case report. J Neuroradiol. 39:258–262.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
McKinney JS, Steineke T, Nochlin D and
Brisman JL: De novo formation of large arteriovenous shunting and a
vascular nidus mimicking an arteriovenous malformation within an
anaplastic oligodendroglioma: Treatment with embolization and
resection. J Neurosurg. 109:1098–1102. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Foy PM, Lozada L and Shaw MD: Vascular
malformation simulating a glioma on computerized tomography: Case
report. J Neurosurg. 54:125–127. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee BC, Vo KD, Kido DK, Mukherjee P,
Reichenbach J, Lin W, Yoon MS and Haacke M: MR high-resolution
blood oxygenation level-dependent venography of occult (low-flow)
vascular lesions. AJNR Am J Neuroradiol. 20:1239–1242.
1999.PubMed/NCBI
|
|
9
|
Russell DS and Rubinstein LJ: Pathology of
tumors of the nervous system (3rd). William & Wilkins.
Baltimore: 931971.
|
|
10
|
Ogilvy CS, Heros RC, Ojemann RG and New
PF: Angiographically occult arteriovenous malformations. J
Neurosurg. 69:350–355. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lobato RD, Perez C, Rivas JJ and Cordobes
F: Clinical, radiological, and pathological spectrum of
angiographically occult intracranial vascular malformations.
Analysis of 21 cases and review of the literature. J Neurosurg.
68:518–531. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lombardi D, Scheithauer BW, Piepgras D,
Meyer FB and Forbes GS: Angioglioma and the arteriovenous
malformation-glioma association. J Neurosurg. 75:589–596. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pallud J, Belaid H, Guillevin R, Vallee JN
and Capelle L: Management of associated glioma and arteriovenous
malformation-the priority is the glioma. Br J Neurosurg.
23:197–198. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ziyal IM, Ece K, Bilginer B, Tezel GG and
Ozcan OE: A glioma with an arteriovenous malformation: An
association or a different entity? Acta Neurochir (Wien).
146:83–86; discussion 86. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Goodkin R, Zaias B and Michelsen WJ:
Arteriovenous malformation and glioma: Coexistent or sequential?
Case report = Neurosurg. 72:798–805. 1990.
|
|
16
|
Harris OA, Chang SD, Harris BT and Adler
JR: Acquired cerebral arteriovenous malformation induced by an
anaplastic astrocytoma: An interesting case. Neurol Res.
22:473–477. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Moftakhar P, Hauptman JS, Malkasian D and
Martin NA: Cerebral arteriovenous malformations Part 1: Cellular
and molecular biology. Neurosurg Focus. 26:E102009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Scandalcioglu IE, Wende D, Eggert A,
Müller D, Roggenbuck U, Gasser T, Wiedemayer H and Stolke D:
Vascular endothelial growth factor plasma levels are significantly
elevated in patients with cerebral arteriovenous malformations.
Cerebrovasc Dis. 21:154–158. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zuccarello M, Giordano R, Scanarini M and
Mingrino S: Malignant astrocytoma associated with arteriovenous
malformation. Case report. Acta Neurochir (Wien). 50:305–309. 1979.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wada M, Takahashi H, Matsubara S and Hirai
S: Occult vascular malformations of the spinal cord: Report of four
cases not detected by angiography. Acta Neurol Scand. 101:140–143.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kim JH, Lee SH, Kim ES and Eoh W:
Angiographically occult vascular malformation of the cauda equina
presenting massive spinal subdural and subarachnoid hematoma. J
Korean Neurosurg Soc. 49:373–376. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Osborn AG: Intracranial vascular
malformation. Diagnostic Neuroradiology (1st). Mosby. (St. Louis,
MO). 284–301. 1994.
|