Introduction
Ultrasonography (US) of the thyroid is a
well-established method for evaluating thyroid nodules. However,
occasionally, non-thyroidal lesions such as diverticula may be
confused with thyroid nodules on physical examination or imaging
studies (1–3).
Pharyngoesophageal diverticula, including
Killian-Jamieson diverticulum (KJD) and Zenker's diverticulum (ZD),
are rare hypopharyngeal diverticula that could easily be
misdiagnosed as thyroid nodules (2,4,5). ZD was reported to be the most common
diverticula of the esophagus, but the rate of KJD was only about a
forth of that of ZD (6,7). In a small number of patients, KJD and ZD
can coexist (8). The two types of
diverticula protrude through a muscular gap of anatomical weakness
in the cervical esophagus near the cricopharyngeus muscle. KJD
originates in the anterolateral wall just inferior to the
cricopharyngeus muscle and superolateral to the longitudinal muscle
of the esophagus (9), whereas ZD
originates in the posterior wall above the cricopharyngeus, which
protrudes posteriorly, and usually projects to the left (10). Few clinicians or sonographers are
aware of the possibility of diverticula mimicking thyroid
nodules.
The current study presents a case of an asymptomatic
unilateral KJD that mimicked a calcified thyroid nodule, and
reviews the literature of this uncommon presentation. This will
enable clinicians to view another source of information on the
subject and means that unnecessary invasive procedures such as
surgery can be avoided.
Case report
A 40-year-old man presented with a suspected thyroid
nodule that was identified incidentally on a routine checkup in a
local hospital on November 10, 2014. Thyroid US demonstrated a
hypoechoic nodule in the left thyroid lobe. The patient presented
with no dysphagia, hoarseness, regurgitation, odynophagia,
halitosis, chronic coughing, neck discomfort, gastroesophageal
reflux symptoms or fever, and the medical and surgical histories
were unremarkable. The patient was subsequently referred to Nanfang
Hospital (Guangzhou, Guangdong, China) for further evaluation on
December 14, 2014. The physical examination of the head and neck
was unremarkable. In addition, laboratory data revealed no
abnormalities. Serum triiodothyronine, thyroxine and
thyroid-stimulating hormone concentrations were 0.88 ng/mL (normal
range, 0.60–1.81 ng/ml), 7.3 µg/dl (normal range, 4.5–10.9 µg/dl)
and 2.22 mIU/l (normal range, 0.55–4.78 mIU/l), respectively, and
no thyroid autoantibodies were detected. A further US examination
was performed following admission, which showed a 1.3×1.0-cm
hypoechoic lesion containing internal-hyperechoic foci and a
hypoechoic rim in the upper portion of the left thyroid gland,
suggesting papillary carcinoma with punctate calcifications
(Fig. 1). On power Doppler imaging,
the lesion also showed internal vascularity. The rest of the
thyroid gland was normal. No pathological lymphadenopathy was noted
at the time. The patient reported a history of hypertension for 2
years that was not treated by medication, with the highest blood
pressure reaching 140/90 mmHg (normal values, <120/80 mmHg).
In order to remove the suspected malignant thyroid
nodule, the patient underwent a left thyroid lobectomy and a neck
exploration under general anesthesia on December 19, 2014, taking
care not to injure the recurrent laryngeal nerve, which runs in the
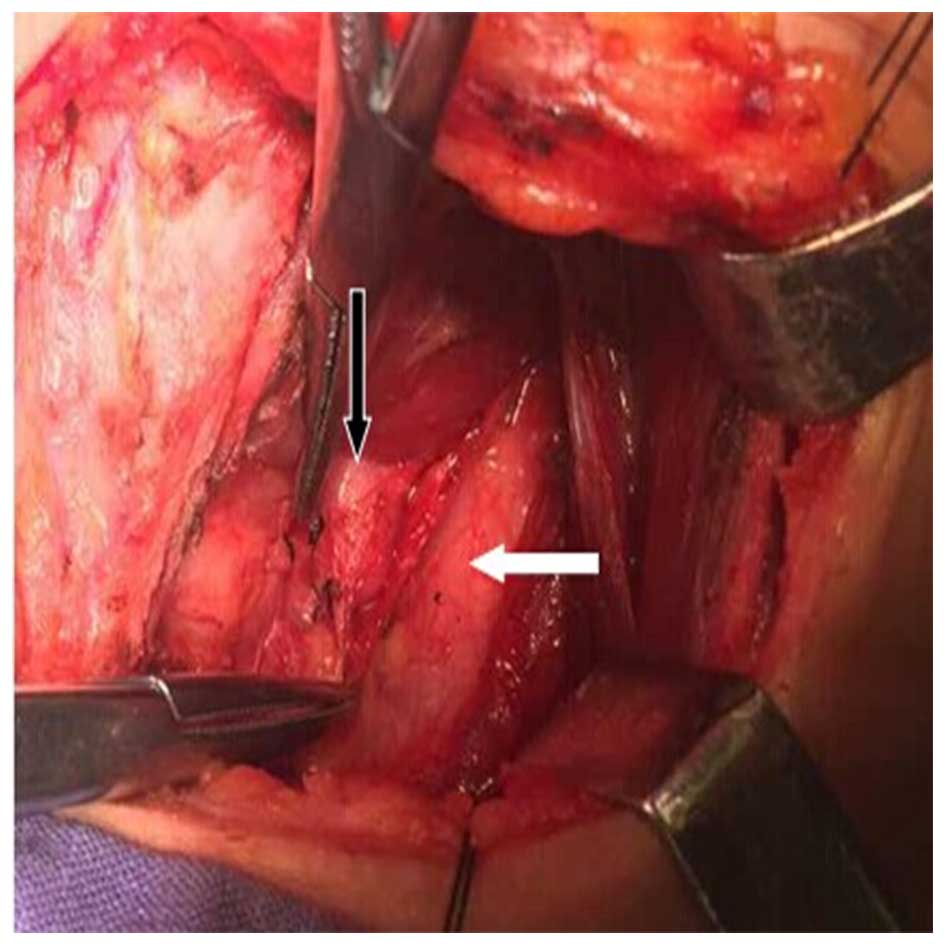
tracheoesophageal groove. However, when surgical cutdowns were
performed for the removed left thyroid gland tissue, no visible
suspected tumor was observed, only calcification. Histopathological
examination revealed a (left thyroid) nodular goiter with focal
calcifications. During the further exploration, a sac was found
protruding from the left anterolateral wall of the cervical
esophagus, which is visible under the cricopharyngeus muscle
(Fig. 2). The sac was located ~5 mm
lateral to the point where the recurrent laryngeal nerve enters the
pharynx. Considering the diverticulum was asymptomatic and small,
further surgery was not performed. The wound was closed in layers
with placement of a closed suction drain. The drain was removed on
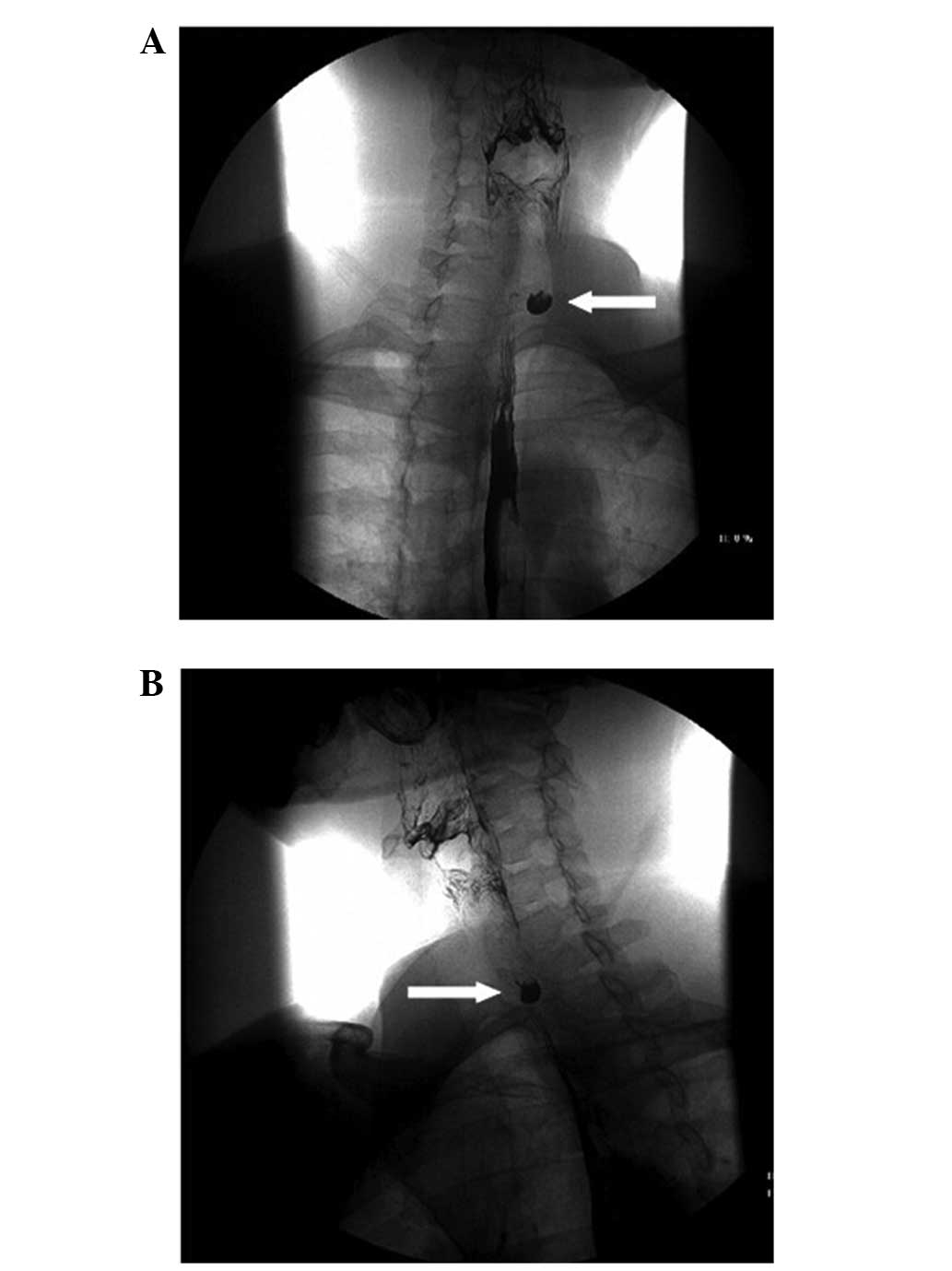
post-operative day 2. On post-operative day 3, subsequent upper
gastrointestinal radiography on the anteroposterior (Fig. 3A) and lateral (Fig. 3B) projections demonstrated a
1.3×1.0-cm KJD originating from the left wall of the esophagus
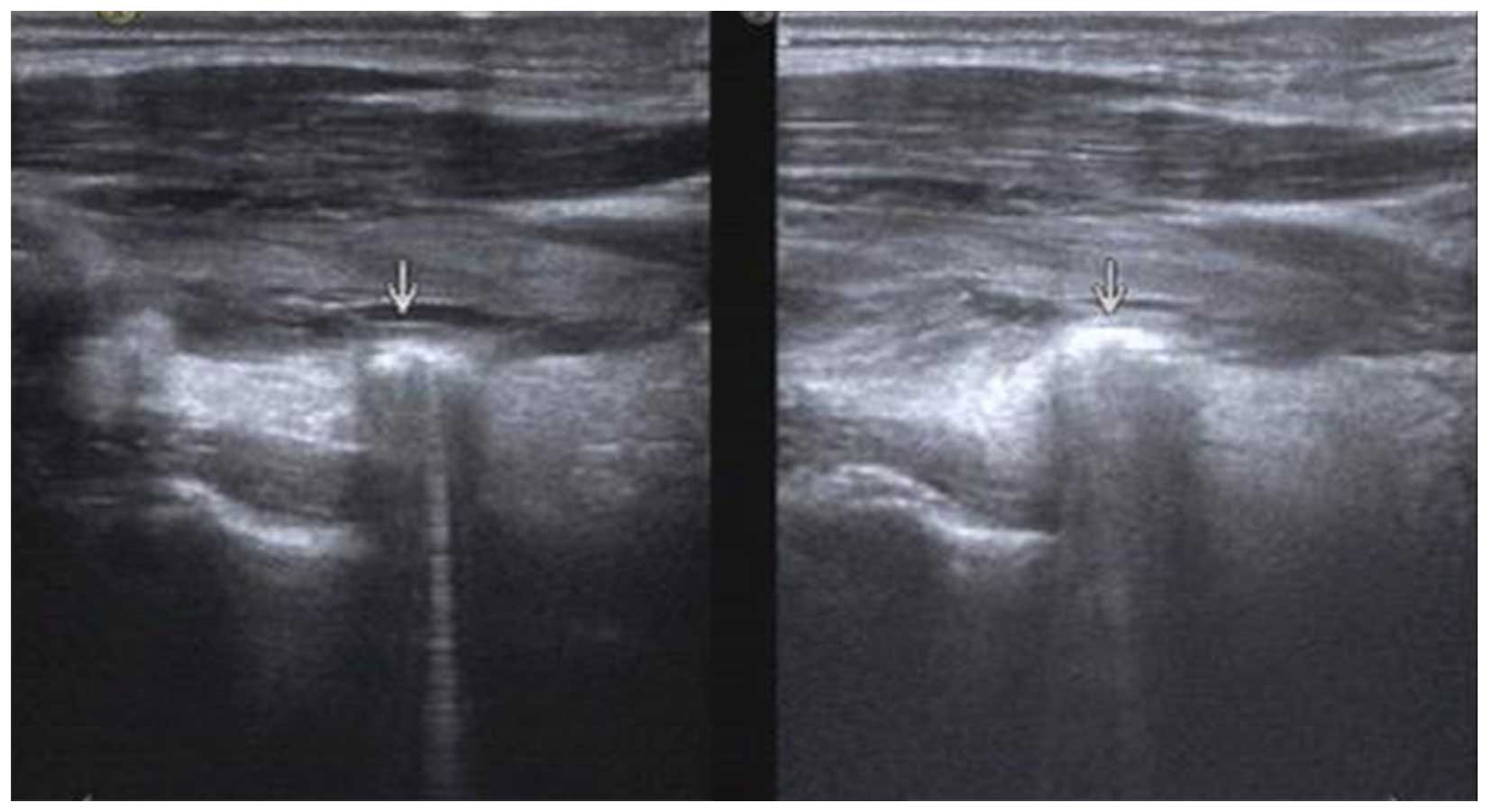
(C6-C7 level). To confirm the diagnosis of an esophageal
diverticulum, the patient was administered a swallow test during US
on post-operative day 4. When the patient swallowed, multiple
hyperechoic spots were observed (Fig.
4). Real-time US was performed showing that the movements of
the hyperechoic spots were consistent with air and water moving
into the esophagus. Transient changes were also demonstrated,
including an increase in the size of the lesion, a reduction in the
definition of the margins and heterogeneous echogenicity of the
contents of the lesion. The patient recovered without complications
such as nerve damage or hemorrhage, and was then discharged from
hospital. During the 3-month follow-up observations, the patient
did not show any abnormalities, such as diverticular relapse,
dysphagia or stenosis.
Discussion
KJD is an outpouching from the lateral wall of the
proximal cervical esophagus. KJD protrudes through a muscular gap
called the KJ triangle, which was first described by Killian and
then confirmed by Jamieson (11,12). The
muscular gap is in the anterolateral wall of the proximal
esophagus, inferior to the cricopharyngeus muscle and superolateral
to the longitudinal muscle of the esophagus (11–13).
The pathogenesis of KJD is unclear. It is
hypothesized that the KJD is the result of a functional outflow
obstruction in the esophagus, the anatomical muscle weakness of the
KJ space, high intraluminal pressure building against a weakness in
the gastrointestinal tract wall or food residue accumulation within
the diverticulum, with possible non-specific chronic inflammation
within and around the diverticulum resulting in esophageal
dysmotility (10,14).
Previously reported cases of KJD mimicking thyroid
nodules were reviewed in the present study to determine the
clinical and US characteristics of KJD (9,10,14–17). The
following terms were searched in the title and/or abstract of
articles published in the PubMed database on December 26, 2014:
‘Killian-Jamieson diverticula’, ‘Killian-Jamieson diverticulum’ or
‘KJD’. Ultimately, 10 cases of KJD, including the present case,
were analyzed (Table I). Of the 10
patients reviewed, 6 patients were men and 4 were women. The mean
age of all 10 patients was 57.8 years, with a range of 40–77 years.
In total, 12 KJD were detected on pharyngoesophagograms in 10
patients, including 7 (70%) with unilateral left-sided diverticula,
1 (10%) with right-sided diverticula and 2 (20%) with bilateral
diverticula. Additionally, 6 out of the 10 patients exhibited no
symptoms, with the exception of 1 patient, who exhibited a neck
mass. The remaining 4 patients exhibited symptoms such as
dysphagia, coughing, hoarseness, gastroesophageal reflux and a
globus sensation. The mean maximal dimension of the diverticula was
2.95 cm, ranging from 1.1–10 cm. A total of 7 patients were treated
with surgical intervention, including fine-needle aspiration (FNA),
open surgical excision of the diverticulum or endoscopic
diverticulotomy.
 | Table I.Clinical and ultrasonographic findings
of Killian-Jamieson diverticulum presenting as a thyroid nodule
reported in the literature. |
Table I.
Clinical and ultrasonographic findings
of Killian-Jamieson diverticulum presenting as a thyroid nodule
reported in the literature.
| First author,
year | Age/gender | Chief complaint | Size, cm | Side | Surgical
intervention | (Ref.) |
|---|
| Boisvert et
al, 2010 | 69/M | Progressive
dysphagia, nighttime coughing, hoarseness and gastroesophageal
reflux | Left: 3.5 Right:
4.4 | Bilaterally | Yes | (9) |
| Kim et al,
2012 | 55/F | Increased size of
known thyroid nodule | 4.0 | Left | Yes | (10) |
|
| 50/M | Incidentally
detected | 1.2 | Left | Yes |
|
|
| 55/M | Incidentally
detected | 1.2 | Left | No |
|
|
| 59/F | Incidentally
detected | 1.7 | Left | No |
|
| Tang et al,
2008 | 51/F | Dysphagia, a globus
sensation posterior to the sternum | 1.5 | Left | Yes | (14) |
| Kim et al,
2012 | 68/M | Epigastric pain | 10.0 | Right | Yes | (15) |
| Mimatsu et al,
2013 | 77/F | Mild dysphagia | Left: 4.0 Right:
1.5 | Bilaterally | Yes | (16) |
| Pang et al,
2009 | 54/M | Incidentally
detected | 1.1 | Left | Yes | (17) |
| Present study | 40/M | Incidentally
detected | 1.3 | Left | No |
|
Unlike the other pharyngoesophageal diverticulum,
ZD, which is more common and symptomatic, KJD is smaller and more
likely to be asymptomatic, resulting in its increased chance to be
misdiagnosed as a thyroid nodule (5).
As in the present study, the study by Rubesin and Levine (8) found KJD to be asymptomatic in the
majority of patients (89%). Dysphagia, coughing and epigastric pain
are the most common symptoms experienced by patients with KJD
(1). Retention of food material in
the diverticulum may lead to regurgitation after meals and chronic
coughing, and even to aspiration pneumonia, particularly in large
diverticula (8).
Esophageal diverticula are usually detected
incidentally by an esophagography. On occasion, diverticula can be
found by thyroid US when they mimic thyroid nodules (10). The diagnostic rate is closely
associated with the doctor's working attitude and practical skill.
Due to the existence of air bubbles and food material, diverticula
can be imaged as heterogeneous internal echoes with strong
echogenic foci, which strongly suggest microcalcifications of
papillary thyroid cancer (4,18). Thus, in order to avoid unnecessary
treatment resulting from a misdiagnosis, principles to distinguish
between esophageal diverticula and thyroid nodules should be noted
clearly. Kim et al summarized the US characteristics of
esophageal diverticula (10). The
real-time US used in a swallow test may be of great assistance.
When the patient was swallowing, the hyperechoic lesions and
internal echogenic foci may change to be consistent with air and
water moving into the esophagus, as in the present case (19). However, it should be mentioned that
these changes and even the connection with the esophageal wall
cannot be observed in all cases, suggesting a further barium
swallow pharyngoesophagography is necessary when a diverticulum is
considered (20,21).
When a diverticulum masquerades as a thyroid nodule,
FNA may be performed to obtain a pathological diagnosis (3). However, complications have not been
recorded or reported in such cases. To the best of our knowledge,
as the KJ triangle is directly adjacent to the entry point of the
recurrent laryngeal nerve into the larynx, FNA or endoscopic
treatment is quite dangerous (6). If
patients have large diverticula or are symptomatic, they should be
treated with surgical intervention. Therefore, it is important to
note that careful dissection in this area is necessary to avoid
nerve injury. We recommend that FNA or endoscopic treatment should
be chosen cautiously. However, the traditional open surgical
approach is currently being challenged by the use of endoscopic
diverticulotomy (22). One of the
potential explanations for this may be its advantage of
intracavitary drainage over open surgical treatment. Time is
required to prove which one technique is more efficient.
In conclusion, the present study reported the case
of a man who presented with a ‘suspected malignant thyroid nodule’
in the left thyroid gland, and subsequently underwent left thyroid
lobectomy and a neck exploration. During the surgery, the nodule
was identified as a KJD. The present findings suggest that
real-time US and pharyngoesophagography are important techniques to
distinguish a KJD from a thyroid nodule, so that unnecessary
surgical intervention can be avoided. Open surgical or endoscopic
diverticulotomy is required when patients have large diverticula or
are symptomatic, although the preference for either technique is
controversial. However, considering that the recurrent laryngeal
nerve crosses the KJ space, we suggest that FNA or endoscopic
treatment should be chosen cautiously in order to avoid nerve
injury.
References
|
1
|
DeFriend DE and Dubbins PA: Sonographic
demonstration of a pharyngoesophageal diverticulum. J Clin
Ultrasound. 28:485–487. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hayashi N, Tamaki N, Konishi J, Endo K,
Misaki T, Torizuka K and Mori T: Lateral pharyngoesophageal
diverticulum simulating thyroid adenoma on sonography. J Clin
Ultrasound. 12:592–594. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Seiberling KA, Dutra JC and Gunn J:
Ultrasound-guided fine needle aspiration biopsy of thyroid nodules
performed in the office. Laryngoscope. 118:228–231. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kumar A, Aggarwal S and Pham DH:
Pharyngoesophageal (Zenker's) diverticulum mimicking thyroid nodule
on ultrasonography: Report of two cases. J Ultrasound Med.
13:319–322. 1994.PubMed/NCBI
|
|
5
|
Mercer D, Blachar A, Khafif A, Weiss J and
Kessler A: Real-time sonography of Killian-Jamieson diverticulum
and its differentiation from thyroid nodules. J Ultrasound Med.
24:557–560. 2005.PubMed/NCBI
|
|
6
|
Rekhtman N, Rekhtman K, Sheth S and Ali
SZ: A 62-year-old woman with a suspected thyroid nodule. Arch
Pathol Lab Med. 129:1497–1498. 2005.PubMed/NCBI
|
|
7
|
Puricelli MD and Zitsch RP III: Is it
really a thyroid nodule? Another cause of a lower midline neck
mass. Otolaryngol Head Neck Surg. 147:397–398. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rubesin SE and Levine MS: Killian-Jamieson
diverticula: Radiographic findings in 16 patients. AJR Am J
Roentgenol. 177:85–89. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Boisvert RD, Bethune DC, Acton D and
Klassen DR: Bilateral Killian-Jamieson diverticula: A case report
and literature review. Can J Gastroenterol. 24:173–174. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kim HK, Lee JI, Jang HW, Bae SY, Lee JH,
Kim YS, Shin JH, Kim SW and Chung JH: Characteristics of
Killian-Jamieson diverticula mimicking a thyroid nodule. Head Neck.
34:599–603. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jamieson EB: Section II, Head and Neck,
(64 plates), 15s. netIllustrations of Regional Anatomy. 3rd. E.
& S. Livingstone; Edinburgh: pp. p441941
|
|
12
|
Zanwar VG, Gambhirel PA, Choksey AS and
Rathi PM: Killian-Jamieson diverticulum: Cervical oesophageal
diverticulum. Journal of the Association of Physicians of India.
63:65–66. 2015.
|
|
13
|
Zaino C, Jacobson HG, Lepow H and Ozturk
C: The Pharyngo- esophageal Sphincter. Charles C. Thomas,
Publisher, Ltd.; Springfield, IL: pp. 29–144. 1950
|
|
14
|
Tang SJ, Tang L, Chen E and Myers LL:
Flexible endoscopic Killian-Jamieson diverticulotomy and literature
review (with video). Gastrointest Endosc. 68:790–793. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kim DC, Hwang JJ, Lee WS, Lee SA, Kim YH
and Chee HK: Surgical treatment of killian-jamieson diverticulum.
Korean J Thorac Cardiovasc Surg. 45:272–274. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mimatsu K, Oida T, Kano H, Kawasaki A,
Fukino N, Kida K, Kuboi Y and Amano S: Killian-Jamieson diverticula
presenting synchronously with thyroid adenoma. Case Rep
Gastroenterol. 7:188–194. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Pang JC, Chong S, Na HI, Kim YS, Park SJ
and Kwon GY: Killian-Jamieson diverticulum mimicking a suspicious
thyroid nodule: Sonographic diagnosis. J Clin Ultrasound.
37:528–530. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kang HC: A case of Zenker's diverticulum
masquerading as a thyroid nodule. Korean J Med. 67:757–760.
2004.
|
|
19
|
Lixin J, Bing H, Zhigang W and Binghui Z:
Sonographic diagnosis features of Zenker diverticulum. Eur J
Radiol. 80:e13–e19. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huang YC, Chen JW and Chang CH: Is it
really a thyroid nodule? Gastroenterology. 145:726–729. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kim J, Kim YJ, Kim EK and Park CS:
Incidentally found pharyngoesophageal diverticulum on
ultrasonography. Yonsei Med J. 43:271–273. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chea CH, Siow SL, Khor TH and Azim NA Nik:
Killian-jamieson diverticulum: The rarer cervical esophageal
diverticulum. Med J Malaysia. 66:73–74. 2011.PubMed/NCBI
|