Introduction
Multiple primary cancers (MPCs) occur at a rate of
37% in all types of cancer (1). A
patient with cancer is 1.29 times more likely to develop an
additional primary cancer when compared with the risk of cancer in
the general population (1).
Synchronous tumors are defined as primary tumors that are diagnosed
at the same time or within 6 months of each other, while primary
tumors diagnosed 6 months after the initial primary tumor are
defined as secondary or metachronous cancer (2). Secondary primary tumors most commonly
occur in the lungs (27.6%), head and neck (20.3%), and urinary
system (10.4%) (3).
A genetic predisposition, which involves mutations
in genes that have been shown to be recurrently mutated in specific
cancers, has been postulated as a cause for MPC (4,5). Other
possibilities include the accumulation of free radicals, mistakes
in DNA replication, and the reduced function of lipid-laden
macrophages leading to impaired host immune surveillance (4). The increased detection of MPC and
potentially synchronous tumors may be attributed to the increased
use of advanced diagnostic techniques (4,6). At
present, there is no consensus on treatment recommendations for
synchronous tumors. The treatment of synchronous tumors is
dependent on the tumor's histological subtype, location, and stage
(7). The surgical preference is for
resection of both tumors simultaneously, whilst modification of
behavioral risk factors may prevent the occurrence of MPCs
(4).
In the present study, a rare case of synchronous
bladder cancer and squamous cell carcinoma with sarcomatoid
differentiation of the scalp was reported.
Case report
A 76-year-old man was admitted to Sakarya University
Training and Research Hospital (Sakarya, Turkey) in March 2014 with
swelling of the head, which had been apparent for 15 days. The
patient had been diagnosed with papillary urothelial carcinoma at
the Urology Department of Sakarya University Training and Research
Hospital 3 months previously (December 2013). The patient had a
history of smoking. Dermatological examination of the right
temporal and occipital regions identified three erythematous
indurated nodules, which were hard and painful on palpation
(Fig. 1). Laboratory examination
revealed leukocytosis [white blood cell count, 42.6 K/µl (normal
range, 4.6–10.2 K/µl)], anemia [hemoglobin count, 11.8 g/dl (normal
range, 12.2–18.1 g/dl)], neutrophilia [neutrophil count, 36.6 K/µl
(normal range, 2.0–6.9 K/µl)], abnormal renal function [creatine,
2.8 mg/dl (normal range, 0.7–1.2 mg/dl); uric acid, 12.8 mg/dl
(normal range, 3.4–7.0 mg/dl)], and electrolyte imbalances
[K+, 7.5 mmol/l (normal range, 3.5–5.1 mmol/l);
Ca2+, 11.4 mg/dl (normal range, 8.8–10.2 mg/dl)].
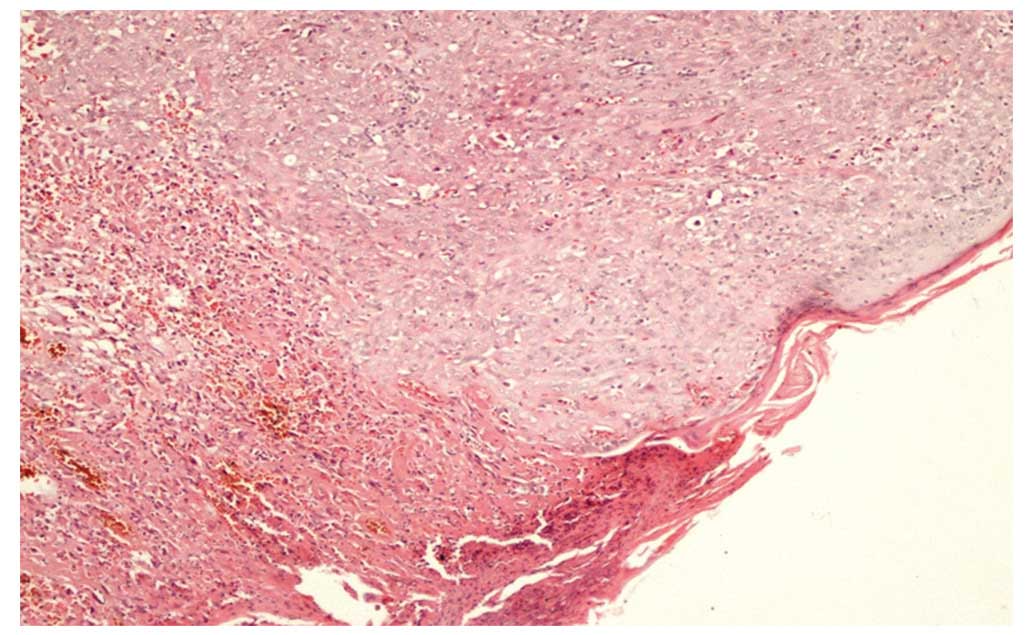
An excisional biopsy of the temporal region was
performed, and the biopsy specimen was fixed in 10% formalin and
embedded in paraffin blocks. The paraffin-embedded specimens were
cut into 5 µm-sections and stained with hematoxylin and eosin for
histological analysis under a light microscope. The histological
analysis revealed pleomorphic mitotic cells with a large pale
nucleus and coarse chromatin, as well as malignant epithelioid
infiltration and the formation of vortex-like structures.
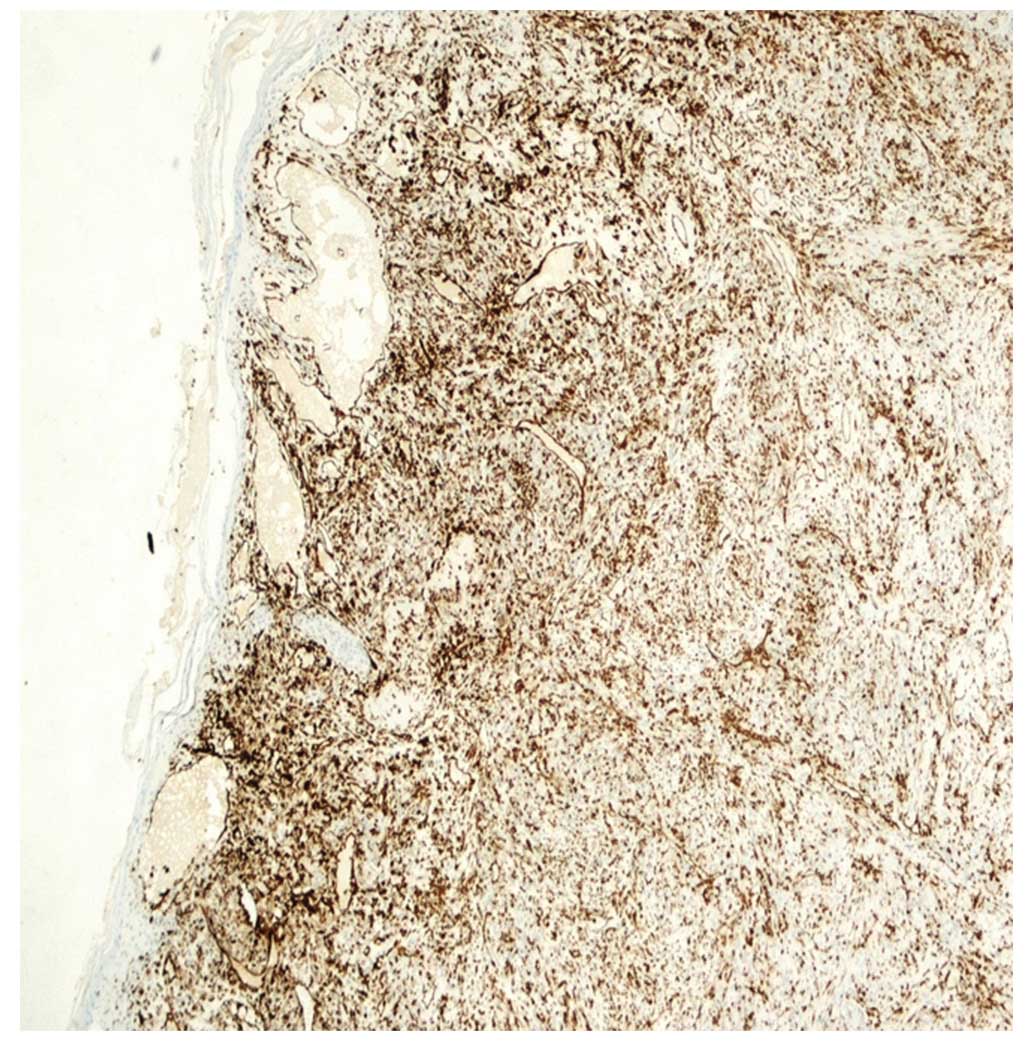
An immunohistochemical analysis involved staining
the biospy sections with the following antibodies: Mouse anti-pan
cytokeratin (CK) monoclonal mixture (1:300; cat. no. 313M-14; Cell
Marque™; Sigma-Aldrich, Rocklin, CA, USA); mouse anti-epithelial
membrane antigen (EMA) monoclonal antibody (1:200; cat. no.
AC13038A,C; Biocare Medical, LLC., Concord, CA, USA); mouse
anti-CK5/6 monoclonal antibody (1:50; cat. no. 356M-14; Cell
Marque™; Sigma-Aldrich); mouse anti-vimentin monoclonal antibody
(1:400; cat. no. NCL-C-VIM572; Thermo Fisher Scientific, Inc.);
rabbit anti-focal p63 monoclonal antibody (1:50; cat. no. BSB5852;
Bio SB, Inc., Goleta, CA, USA); mouse anti-desmin monoclonal
antibody (1:100; cat. no. 61-0077-2; Genemed Biotechnologies, Inc.,
South San Francisco, CA, USA); and mouse anti-cluster of
differentiation 34 (CD34) monoclonal antibody (1:600; cat. no.
MS-363-P0; Thermo Fisher Scientific, Inc., Waltham, MA, USA).
Subsequently, the biopsy sections were incubated with horseradish
peroxidase-conjugated rabbit anti-mouse and polymer anti-rabbit
secondary antibodies (Bond™Polymer Refine Detection; cat. no.
DS9800; Leica Microsystems GmbH, Wetzlar, Germany), followed by
3,3′-diaminobenzidine tetrahydrochloride hydrate. The stained
sections were observed under a light microscope. Staining revealed
positivity for pan CK, EMA, CK5/6, vimentin and focal p63, and
negativity for desmin and CD34. The patient was diagnosed with
synchronous squamous cell carcinoma with sarcomatoid
differentiation of the scalp (Figs.
2–5).
The patient was referred to the Department of
Plastic Surgery (Sakarya University Training and Research Hospital)
for resection; however, he refused treatment and was subsequently
discharged to seek treatment at a different hospital in Ankara,
Turkey. However, after 6 months, we were informed by a relative of
the patient that he had succumbed to respiratory failure. Written
informed consent was obtained from the patient for the publication
of the present study.
Discussion
The prolongation of the human life span, as well as
the continuous development of diagnostic and therapeutic
strategies, have increased the incidence of secondary primary
malignancies (7). According to Warren
and Gate's criteria, synchronous tumors are diagnosed based on
three factors: i) The diagnosis of malignancy for any tumor must be
made conclusively; ii) each must be a different tumor; and iii)
tumors must not result from the metastasis of another tumor
(8). In patients with a malignancy,
the occurrence of secondary malignancies may be coincidental or a
multifactorial process (9). Smoking
is an etiological risk factor for bladder, head, neck, lung and
uterus cancer (9,10). Following the diagnosis of a primary
malignancy, patients who stop smoking significantly prolong the
time it takes for a second primary malignancy to develop (11). Synchronous or metachronous tumors are
rare in the urogenital system and may be associated with genetic
disorders, including von Hippel Lindau disease, tuberous sclerosis
and 3:8 chromosomal translocations (12). Stamey et al (13) reported that, in a previous study,
prostate adenocarcinoma occurred in 40% of patients that underwent
cystoprostatectomy for the treatment of bladder cancer.
Furthermore, Pastore et al (14) reported the synchronous occurrence of
transitional cell carcinoma of the urinary bladder, breast and
primary neoplasms of the skin in one patient. The patient in the
present case developed synchronous squamous cell carcinoma of the
scalp 3 months subsequent to the diagnosis of papillary bladder
cancer.
In conclusion, the present study supported the
hypothesis that, in patients with a primary cancer, the possibility
of a secondary primary malignancy in the same or a different organ
is increased. Furthermore, if a secondary tumor is identified, the
risk of relapse or metastasis must be considered. To the best of
our knowledge, no cases of synchronous skin malignancy and
urothelial carcinoma of the bladder have been reported
previously.
References
|
1
|
Shikhani AH, Matanoski GM, Jones MM,
Kashima HK and Johns ME: Multiple primary malignancies in head and
neck cancer. Arch Otolaryngol Head Neck Surg. 112:1172–1179. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Martini N and Melamed MR: Multiple primary
lung cancers. J Thorac Cardiovasc Surg. 70:606–612. 1975.PubMed/NCBI
|
|
3
|
Duchateau CS and Stokkel MP: Second
primary tumors involving non-small cell lung cancer: Prevalence and
its influence on survival. Chest. 127:1152–1158. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mydlo JH and Gerstein M: Patients with
urologic cancer and other nonurologic malignancies: Analysis of a
sample and review of the literature. Urology. 58:864–869. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
An G, Ng AY, Meka CS, Lou G, Bright SP,
Cazares L, Wright GL Jr and Veltri RW: Cloning and characterization
of UROC28, a novel gene overexpressed in prostate, bladder and
breast cancers. Cancer Res. 60:7014–7020. 2000.PubMed/NCBI
|
|
6
|
López ML, Lana A, Díaz S, Folgueras MV,
Sánchez L, Comendador MA, Belyakova E, Rodríguez JM and Cueto A:
Multiple primary cancer: An increasing health problem. Strategies
for prevention in cancer survivors. Eur J Cancer Care (Engl).
18:598–605. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wallace D, Arul D and Chitale S:
Synchronous tumours of the breast and bladder. J Surg Case Rep.
2014:rju0662014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Warren S and Gates O: Multiple primary
malignant tumors; A survey of the literature and statistical study.
Am J Cancer. 16:1358–1414. 1932.
|
|
9
|
van Bodegom PC, Wagenaar SS, Corrin B,
Baak JP, Berkel J and Vanderschueren RG: Second primary lung
cancer: Importance of long term follow up. Thorax. 44:788–793.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Antal A and Vallent K: Cases of multiple
tumors in our clinic. Orv Hetil (abstract). 138:1507–1510.
1997.
|
|
11
|
Ozseker F, Bilgin S, Baran A, Dilek İ,
Bayram U and Akkaya E: Second Primary Lung Cancers. Solunum
Hastalıkları. 14:239–244. 2003.(In Turkish).
|
|
12
|
Conquy S, Steg A and Ferry M: Bilateral
kidney cancer in a patient with Von Hippel-Lindau disease. Ann Urol
(Paris). 21:350–352. 1987.(In French). PubMed/NCBI
|
|
13
|
Stamey TA, Freiha FS, McNeal JE, Redwine
EA, Whittemore AS and Schmid HP: Localized prostate cancer.
Relationship of tumor volume to clinical significance for treatment
of prostate cancer. Cancer. 71(Suppl 3): S933–S938. 1993.
|
|
14
|
Pastore AL, Palleschi G, Autieri D, Leto
A, Ripoli A, Maggioni C, Moschese D, Al Salhi Y, Porta N, Di
Cristofano C, et al: Sapienza University of Rome, Faculty of
Pharmacy and Medicine: Synchronous primary neoplasms of the
bladder, skin and breast in a male patient: A case report. World J
Surg Oncol. 11:2822013. View Article : Google Scholar : PubMed/NCBI
|