Introduction
Breast disease seriously affects the physical and
mental health of women. In recent years, the incidence rates of
benign breast tumors (BBTs) and malignant tumors have been rising.
BBTs are much more common than malignant breast cancer, accounting
for >90% of referrals to secondary care (1,2). BBTs
include fibroadenoma, intraductal papilloma and lipomyoma, among
others (3). There is a possibility
for malignant transformation in BBTs. Surgical resection is the
main method for the treatment of the tumors (4).
The traditional method of BBT resection used at our
hospital is a radial or arc incision along the dermatoglyph on the
skin above the pathological changes of the breast, in order to
minimize damage to the mammary ducts. However, obvious
post-operative scarring seriously affects the appearance of the
breast. If there are multiple lesions, there will be more scars
left after removal of the tumors and the bilateral breasts will be
asymmetrical. This can cause the patient much psychological
pressure and affect their quality of life.
With the continuous development of the social
economy and the gradual improvement of living standards, demands
for breast appearance are higher. Surgery should not only cure the
breast disease, but it should also avoid damage to the functions
and appearance of the breasts. Therefore the choice of method for
BBT resection should aim to minimize obvious scarring and maintain
the overall appearance of the breasts.
In our experience at Qilu Hospital, Shandong
University (Jinan, China), the periareolar incision should be
considered the first choice for BBT. This allows good treatment of
the BBT and minimal local periareolar scarring. When minimal
external scarring and changes to the overall appearance of the
breast are requested by the patients, a periareolar incision is a
good solution. The present study reports the results of the use of
this technique by a single institution in a retrospective analysis
of 153 BBT patients.
Materials and methods
Patients
A total of 153 patients (182 breasts) operated upon
using a periareolar incision between January 2010 and December 2012
were enrolled in this retrospective study. Patient information and
written consent forms were obtained from the Pathology Tissue Bank
of Qilu Hospital. The present study was approved by Medical Ethics
Committee of of Qilu Hospital. Patient ages ranged between 14 and
62 years old. The clinical characteristics of the patients are
listed in Table I. Of all the
patients with breast masses, 92 had a single mass and 70 had
multiple masses. The remaining breasts were operated on due to
nipple discharge. The masses of 40 breasts were located under or
around the areola, while other masses located in each quadrant of
the breast. The longest distance from the mass to the edge of the
areola was 7.5 cm. The largest mass was 5×3 cm and the smallest was
0.5×0.5 cm. Pre-operative examination (ultrasonography or
mammography) was performed to exclude the malignant tumors.
Table II shows the association
between the surgical method and the type of BBT.
 | Table I.Clinical characteristics of the
patients. |
Table I.
Clinical characteristics of the
patients.
| Clinical data | Value |
|---|
| Total patients,
n | 153 |
| Mean age ± standard
deviation, years | 38.0±9.4 |
| Marital and fertility
status, n (%) |
|
| Single
and nulliparous | 15 (9.8) |
| Married
and nulliparous | 13 (8.5) |
| Married
with children | 125 (81.7) |
| Affected breasts, n
(%) |
|
|
Unilateral | 124 (81.0) |
|
Bilateral | 29
(19.0) |
| Reason for treatment,
n (%) |
|
| Breast
mass | 119 (77.8) |
| Nipple
discharge | 26
(17.0) |
| Breast
mass and nipple discharge | 4
(2.6) |
|
Other | 4
(2.6) |
| Previous breast
history, n (%) |
|
| Benign
breast tumor | 16
(10.5) |
|
Contralateral breast
cancer | 2
(1.3) |
 | Table II.Association between surgical method
and type of benign breast tumor. |
Table II.
Association between surgical method
and type of benign breast tumor.
| Surgical method | Fibroadenoma | Intraductal
papilloma | Mastoplasia | Other |
|---|
| Tumor resection,
n | 87 | 1 | 3 | 3 |
| Gland lobectomy,
segment or quadrant resection, n | 24 | 18 | 0 | 3 |
| Subcutaneous
mastectomy, n | 9 | 25 | 8 | 1 |
The follow-up time ranged between 1 month and 3
years, and the results were evaluated by the person who had
performed the surgery.
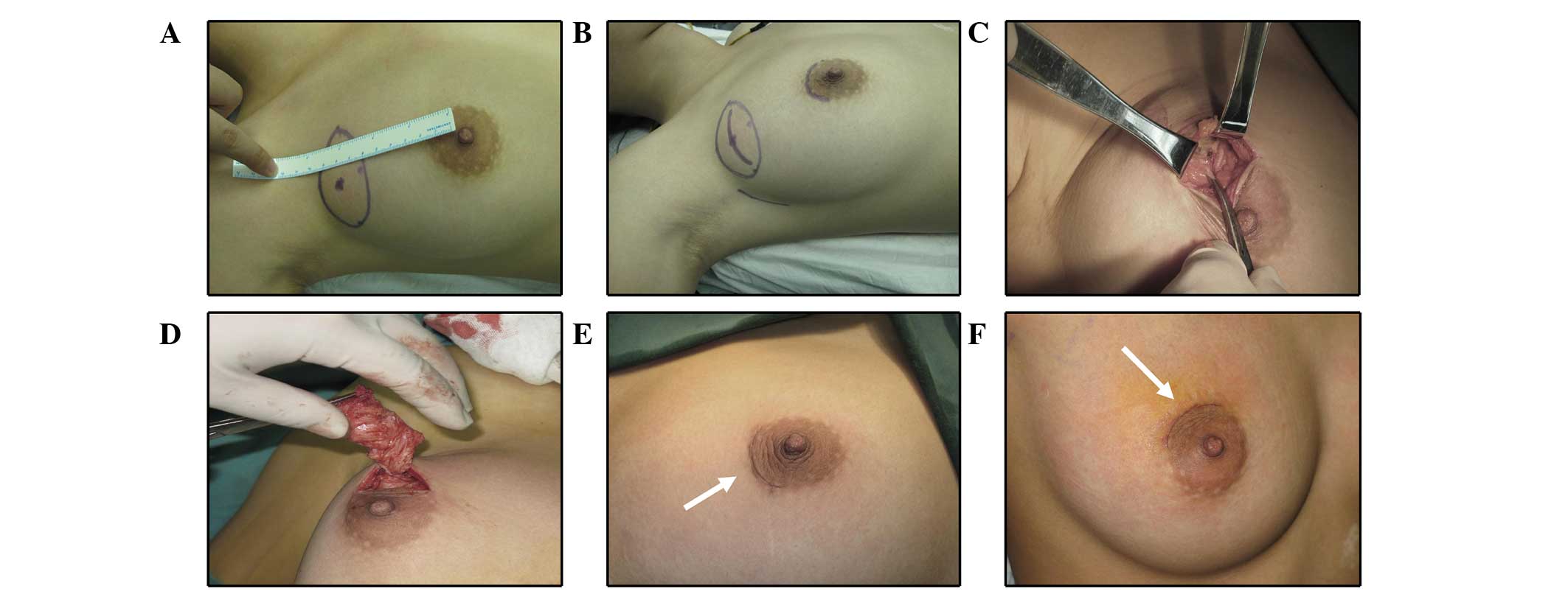
Surgical technique
The procedure was performed under general anesthesia
and the patient was placed in a supine position. The surface
projection of the mass was marked on the skin and the distance from
the mass to the areola was measured. The nearest periareolar
incision area to the mass was chosen. If there were multiple
masses, the incision was chosen by taking into account the location
of the majority of the masses or the incision on the upper outer
edge of the areola was chosen to ensure the normal sensation of the
nipple and areola. The length of the incision was determined based
on the size of the tumor and the distance from the tumor to areola,
and was no more than half of the length of the perimeter of
areola.
The skin, subcutaneous tissue and superficial fascia
were incised in turn until the gland surface. The incision was
opened and the tissues between the subcutaneous adipose and mammary
gland capsule were sharply separated until reaching the surface of
the mass. If the mass was far from the areola, it was pushed or
pulled with forceps towards the incision. The gland layer was
radially incised and the mass, together with part of its
surrounding normal glands and adipose tissue, were completely
removed. Electrocoagulation was used to stop any bleeding. The
surgical residual cavity was not sutured and a drainage tube was
not placed. The subcutaneous adipose layer was sutured with 5-0
absorbable interrupted sutures, followed by intradermal sutures.
The incision was covered using medical biological glue. After the
surgery, the resection site was compressed using bandages. The
aforementioned procedures involved in the mammary tumor resection
are shown in Fig. 1.
For patients with multiple and relatively
concentrated masses, mammary gland lobectomy, segment and quadrant
resection could be performed. During the procedure, the gland layer
was radially incised along the direction of the mammary ducts until
the retromammary cellular space. The surgeon explored the gland
layer completely using their fingers. The glands, including all the
masses, were pulled below the incision. Multiple masses, together
with part of the surrounding normal mammary glands, were removed
completely.
For the patients who received a subcutaneous
mastectomy, part of the normal mammary glands was maintained under
the nipple and areola to ensure the blood supply of the
nipple-areolar complex. The nipple-areola plasty was routinely
performed to avoid post-operative nipple collapse.
After the surgery, the breast collapsed
significantly for patients with a thin subcutaneous fatty layer and
more gland tissues. For these patients, silastic gel breast
prosthesis implantation could be surgically performed based on the
patient's requirements.
Results
All incisions were primary healing. In the early
post-operative days, swelling of the surgical area was commonly
observed. Of the 153 patients 1 (0.7%) developed hematoma and 2
(1.3%) developed slight nipple ischemia. No infections or other
complications were observed.
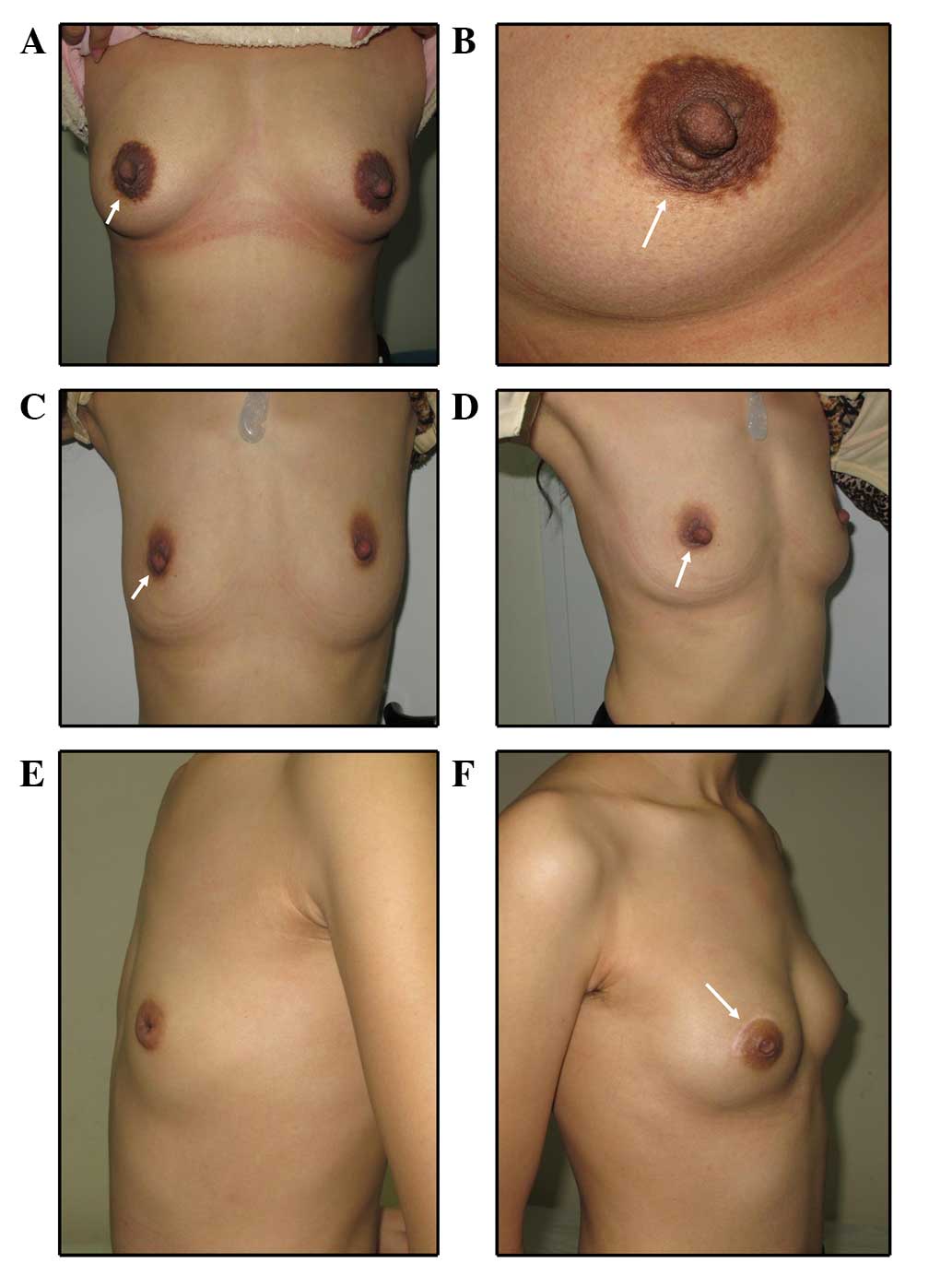
After 1 month to 3 years of follow-up, there was no
obvious scarring, with the exception of 3 patients (2.0) with scar
diathesis. In total, 2 patients underwent silastic gel breast
prosthesis implantation successfully. Fig. 2 showed representative post-surgical
images of 3 patients. A total of 32 breasts (17.6%) developed
areola collapse and 51 breasts (28.0%) developed nipple
paresthesia. Tables III and
IV show the associations between
areola collapse, nipple paresthesia, surgical method and the type
of BBT. Patient satisfaction was 98.0%, with unsatisfactory results
for 3 patients who had undergone subcutaneous mastectomy, but
without silastic gel breast prosthesis implantation.
 | Table III.Association between areola collapse,
nipple paresthesia and surgical method. |
Table III.
Association between areola collapse,
nipple paresthesia and surgical method.
| Side effect | Tumor resection | Gland lobectomy,
segment or quadrant resection | Subcutaneous
mastectomy |
|---|
| Areola collapse, n
(%) |
|
|
|
| Yes | 2 (2.1) | 11 (24.4) | 19 (44.2) |
| No | 92 (97.9) | 34 (75.6) | 24 (55.8) |
| Nipple paresthesia, n
(%) |
|
|
|
| Yes | 11 (11.7) | 13 (28.9) | 27 (62.8) |
| No | 83 (88.3) | 32 (71.1) | 16 (37.2) |
 | Table IV.Association between areola collapse,
nipple paresthesia and type of benign breast tumor. |
Table IV.
Association between areola collapse,
nipple paresthesia and type of benign breast tumor.
| Side effect | Fibroadenoma | Intraductal
papilloma | Mastoplasia | Other |
|---|
| Areola collapse, n
(%) |
|
| Yes | 9
(7.5) | 21 (47.7) | 1 (9.1) | 1 (14.3) |
| No | 111 (92.5) | 23 (52.3) | 10 (90.9) | 6 (85.7) |
| Nipple paresthesia, n
(%) |
|
| Yes | 21
(17.5) | 24 (54.5) | 3
(27.3) | 3 (42.8) |
| No | 99
(82.5) | 20 (45.5) | 8
(72.7) | 4 (57.2) |
During the follow-up, 2 patients who underwent tumor
resection and 2 patients who underwent mammary gland lobectomy
experienced a lactation period after the surgery. All patients
retained the ability to breastfeed.
Discussion
Plump and elastic breasts are important functionally
and esthetically. Generally, conservative treatment cannot cure
BBT, and surgical resection is the most effective and thorough
treatment. Traditional incisions for BBT are radial or arc
incisions along the dermatoglyph on the skin above the pathological
changes of the breast. The surgery is easy to perform, however, its
disadvantage is the obvious scarring which seriously affects the
appearance of the breast, particularly in patients with multiple
lesions. Nowadays, the requirements for a beautiful post-operative
breast appearance are higher.
Mammary glands are located between the superficial
layer and the deep layer of the superficial fascia. The superficial
layer of the superficial fascia is tightly connected with the skin,
and the deep layer of the superficial fascia is connected with the
superficial layer of the pectoralis major fascia by loose
connective tissues. Mammary tissues have good elasticity and
softness (5). These anatomical
structures ensure that the breast has a certain mobility and is
relatively stable. The skin of the areola area is relatively thin,
and has good elasticity and strength, with a wide range of
resection techniques available. In the majority of cases,
post-operative scarring is not obvious and can quickly heal. All
these reasons make a periareolar incision possible, and surgery
through periareolar incisions are gradually being welcomed by
female patients with BBT. For the 153 patients in the present
study, there were no obvious scarring, with the exception of 3
patients with scar diathesis. The patient satisfaction was high at
98%. Due to its cosmetic role, periareolar incision has also been
widely used in the treatment of gynecomastia (6–8).
Certain studies have previously reported that there
are no differences between a periareolar incision and a traditional
incision with regard to the duration of surgery or the amount of
bleeding (9,10). However, other studies have reported
the opposite, stating that a resection through a periareolar
incision requires more time (~2 min) and results in more bleeding
(~10 ml) compared with the traditional surgical method (11). Although this result was supported by
statistics, it has little practical significance in clinical
practice. A periareolar incision causes more damage to the
subcutaneous tunnel and mammary glands, thus it requires more focus
on the surgical techniques, including intraoperative exposure,
intraoperative bleeding and incision closure, otherwise the risk of
surgical complications could increase. Of the 153 patients, only 1
(0.7%) developed hematoma, while 2 (1.3%) developed slight nipple
ischemia. No cases were administered post-operative antibiotics and
no infections occurred. It has previously been reported that a
periareolar incision is not suitable when the diameter of the tumor
is >5 cm or when the distance between the tumor and the areola
is >3–4 cm, since the surgery would cause significant damage to
the lactiferous ducts (12). However,
in the present cases, a periareolar incision was used even when the
distance between the tumor and the areola was 7.5 cm to ensure good
patient outcomes. A periareolar incision was also used in
subcutaneous mastectomy with good surgical effects.
In the body, the residual cavity generally requires
closure by sutures following removal of tissue, and for larger
residual cavities and wound bleeding, a drainage tube should be
placed to avoid complications such as subcutaneous hemorrhage and
infection. However, it has been reported that for patients with
more mammary tissues, the suture of the residual cavity is more
difficult. Thus, if the residual cavity was forced closed by
sutures, it would cause appearance changes of varying degrees
(13). In the 153 patients of the
present study, electrocoagulation was chosen to stop any bleeding
instead of suturing the residual cavity. This method did not cause
appearance changes of the breast, and following the surgery,
discharge could fill the residual cavity and maintain the
appearance of the breast. Within 3 months of the surgery, the
residual cavity narrowed gradually, probably as it was filled by
fiber granulation tissues, and the discharge was absorbed.
Additionally, drainage tubes were not placed in any of the 153
patients. Instead, compression was applied using bandages. This
reduced the exudation of the surgical area and contributed to the
recovery of the breast. Particular attention was paid to avoid
compression of the incision, nipple and areola, so as to prevent
necrosis of the skin edge and incision flap, and ischemic necrosis
of the nipple and areola.
The only drawback of periareolar incision with
regard to appearance is the possibility of flatness or collapse of
the nipple-areola area. Reasons for this include i) the
characteristics of the breast, such as more mammary glands and a
thin fatty layer; ii) surgical factors, such as too much resection
of the subcutaneous mammary tissues, particularly tissues under the
nipple-areola area; and iii) breast mass factors, such as a large
mass occupying the whole breast or a tumor located in the deep
areola. Of the 182 breasts, 32 developed nipple collapse. Of these,
21 (65.6%) initially exhibited intraductal papilloma (IDP). The
treatment of IDP often requires a larger extent of resection and
greater resection of tissues under the areolar area. This may be
the reason why 17.6% (n=32) of breasts developed nipple
collapse.
Additionally, 51 breasts (28.0%) developed nipple
paresthesia. It can be concluded that the majority of patients who
had developed nipple paresthesia initially presented with IDP and
underwent surgery to a greater extent. A previous study reported
that the incidence of nipple paresthesia for periareolar incision
was higher compared with that found for traditional incision
(11). We hypothesize that when the
extent of surgery is larger it is more likely to damage the nerve
endings. The incision could also be overstretched in the surgery
causing nerve injury. A study also reported that the differences in
the times of sensory recovery for different locations and lengths
showed no statistical significances. Therefore, the location and
cut length by periareolar incision in treatment of BBT could be
chosen according to the location and size of the tumor, which did
not affect the time of the sensory recovery of the skin (14). During the follow-up in the present
study, it was found that patients with nipple paresthesia gradually
recovered over time. No irreversible damage occurred.
Subcutaneous mastectomy has good treatment effects
for certain types of BBT. However, it seriously affects the
appearance of the breast and brings a great psychological burden to
patients. Therefore, for patients with higher cosmetic
requirements, silastic gel breast prosthesis implantations can be
performed at the same time as the subcutaneous mastectomy. Of the
153 patients, only 2 underwent silastic gel breast prosthesis
implantation. Subsequent to the surgery, the bilateral breasts were
symmetric with a good appearance, and the patient satisfaction was
high.
In conclusion, a periareolar incision brings hope to
female patients with BBT; it enables the disease to be cured while
maintaining the appearance of the breast. A quick recovery, hidden
incision, small scar and other advantages mean that the periareolar
incision should be used a main surgical technique for BBT. However,
periareolar incision requires higher technical requirements from
the surgeons and may cause areola collapse. From the point of the
appearance of the breast, we advise patients with high cosmetic
requirements to receive silastic gel breast prosthesis
implantations in order to maintain a good breast shape.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (grant nos. 81172529 and 81272903) and
the Shandong Science and Technology Development Plan (grant no.
2013GRC31801).
References
|
1
|
Chen W, Zheng R, Zhang S, Zhao P, Li G, Wu
L and He J: The incidences and mortalities of major cancers in
China, 2009. Chin J Cancer. 32:106–112. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Onstad M and Stuckey A: Benign breast
disorders. Obstet Gynecol Clin North Am. 40:459–473. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Laufer M and Goldstein D: The breast:
Examination and lesionsPediatric and Adolescent Gynecology. 5th.
Sydor A: Lippincott Williams and Wilkins; Philidelphia: pp.
729–759. 2005
|
|
4
|
Dixon JM, Dobie V, Lamb J, Walsh JS and
Chetty U: Assessment of the acceptability of conservative
management of fibroadenoma of the breast. Br J Surg. 83:264–265.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hamdi M, Würinger E, Schlenz I and Kuzbari
R: Anatomy of the breast: A clinical application. Vertical Scar
Mammaplasty. Springer. 1–8. 2005. View Article : Google Scholar
|
|
6
|
Lapid O, Klinkenbijl JH, Oomen MW and van
Wingerden JJ: Gynaecomastia surgery in the Netherlands: What, why,
who, where. J Plast Reconstr Aesthet Surg. 67:702–706. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lee JH, Kim IK, Kim TG and Kim YH:
Surgical correction of gynecomastia with minimal scarring.
Aesthetic Plast Surg. 36:1302–1306. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cannistra C, Piedimonte A and Albonico F:
Surgical treatment of gynecomastia with severe ptosis: Periareolar
incision and dermal double areolar pedicle technique. Aesthetic
Plast Surg. 33:834–837. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chen XY: Clinical observation on surgery
through a minimal incision around areola mammae in treatment of
benign tumor of mammary glands. Hebei Yixue. 20:777–780. 2014.(In
Chinese).
|
|
10
|
Hu N: The clinical effects of different
resection type of breast Fibroids. Zhongguo YIyao Daokan.
15:1135–1137. 2013.(In Chinese).
|
|
11
|
Liu XF, Zhang JX, Zhou Q, Chen F, Shao ZM
and Lu C: A clinical study on the resection of breast fibroadenoma
using two types of incision. Scand J Surg. 100:147–152.
2011.PubMed/NCBI
|
|
12
|
Zhao XY: Application value of areola
incision at the edge of the benign breast tumor resection. Zhongguo
Shiyong Yiyao. 5:57–58. 2010.(In Chinese).
|
|
13
|
Cao MZ: An improvement for dead-space
management in partial mastectomy. Qingdao Daxue Yixueyuan Xuebao.
39:235–236. 2003.(In Chinese).
|
|
14
|
Kong LW, Ma XJ, Liu YH, Wang J and Han JQ:
Influence of the circumareolar incision exsection in treatment of
benign breast tumour on the nipple-areola complex sensibility.
Jiefangjun Yiyao Zazhi. 26:84–86. 2014.(In Chinese).
|