Introduction
Lung cancer is one of the leading cancer types
worldwide with regard to incidence and mortality rates (1). The two major forms are non-small cell
lung cancer (NSCLC), with 85% of of all newly diagnosed lung
cancers, and small cell lung cancer, with 15% (2). NSCLC is further divided into four
subtypes: Adenocarcinoma, squamous carcinoma, large cell carcinoma
and adenosquamous carcinoma. The majority of patients are diagnosed
at an advanced tumor stage and are therefore not candidates for
curative surgical resection. These patients receive multimodal
chemotherapy, with or without radiation (3). Despite all efforts, the overall 5-year
survival rate of NSCLC patients is only ~15% (1,4,5). Due to the poor prognosis of NSCLC,
current research aims to improve our understanding of the
biological and molecular genetic background of the disease in order
to identify novel biomarkers and therapeutic targets.
Tumor growth is not only determined by the
neoplastic cells themselves, but also, depending on the tumor
entity, more or less by the stroma compartment. In carcinomas, the
desmoplastic stroma reaction is a consistent histological feature;
however, the prognostic role of the stroma in NSCLC is not as clear
as it is in other tumor entities (6).
The tumor stroma consists of non-malignant cells, such as
carcinoma-associated fibroblasts, which are specialized mesenchymal
cell types distinctive to each tissue environment. Furthermore, the
extracellular matrix includes and interacts with structural
proteins (such as collagen or elastin), regulatory proteins (such
as periostin, fibrilin and fibronectin), innate and adaptive immune
cells (7,8), the vasculature (endothelial cells and
pericytes) and proteoglycans (9,10). By
consecutive genetic alterations, normal parenchymal cells switch to
malignant tumor cells, while the change of the stromal host
compartment consequently leads to a supportive or hostile
environment for the cancer cells, depending on the temporal and
spatial sequence, and the tumor type. Mandatory alterations in the
microenvironment contributing to cancer invasion consist of
degradation of the basement membrane, activation of the stroma and
formation of new tumor feeding capillaries (11).
In a previous study, we defined the activated stroma
index as an independent prognostic marker for pancreatic ductal
adenocarcinoma (12). In pancreatic
cancer, typically the vast majority of the tumor volume consists of
non-malignant stroma cells, which in turn produce excessive
extracellular matrix proteins, creating a highly desmoplastic
microenvironment (13). The so-called
activated stroma index is defined as the ratio of stromal activity
measured by α-smooth muscle actin (α-SMA) and collagen deposition;
it indicates paracrine secretion of periostin and other tumor
stimulating factors, which is associated with a worsened prognosis
(12,13). Contrary to pancreatic cancer, where
periostin is exclusively produced by the stroma (14), in NSCLC, tumor cells also produce
periostin (15). Thus, periostin
marks epithelial-mesenchymal transition (EMT), which is a
characteristic of highly tumorigenic cells promoting tumor
progression (15,16). The present study investigated the role
of periostin and the activated stroma index in NSCLC.
Patients and methods
Patient and tissue samples
The collection of material and data was approved by
the Ethics Committees of the Bayerische Ärztekammer (Munich,
Germany), the Ludwigs-Maximilian University (Munich, Germany) and
the Technical University of Munich (Munich, Germany). This study
was conducted on an anonymized data set. Clinical data and the
formalin-fixed, paraffin-embedded tissues of 93 patients was
retrospectively collected for analysis. All available tissue from
patients who underwent surgery for NSCLC with curative intent
between February 2003 and December 2006 at the Klinikum Rechts der
Isar, Technical University of Munich, were identified and analyzed,
without further limitations. Patient characteristics are presented
in Table I.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Characteristic | Value |
|---|
| Median age,
years |
|
|
Males | 69 |
|
Females | 62 |
| Gender, n (%) |
|
| Male | 56 (60.2) |
|
Female | 37 (39.8) |
| Histology, n (%) |
|
|
Adenocarcinoma | 66 (71.0) |
| Squamous
carcinoma | 22 (23.7) |
| Large
cell carcinoma | 3 (3.2) |
|
Adenosquamous carcinoma | 2 (2.2) |
| Tumor status, n
(%) |
|
| T1 | 3 (3.2) |
| T2 | 34 (36.6) |
| T3 | 55 (59.1) |
| Not
specified | 1 (1.1) |
| Nodal status, n
(%) |
|
| N0 | 60 (64.5) |
| N1 | 20 (21.5) |
| N2 | 12 (12.9) |
| N3 | 1 (1.1) |
| Grade, n (%) |
|
| G1 | 3 (3.2) |
| G2 | 34 (36.6) |
| G3 | 55 (59.1) |
| Not specified | 1 (1.1) |
Immunohistochemistry
Immunohistochemical analysis of periostin, α-SMA and
cluster of differentiation 31 (CD31), and collagen-specific aniline
blue assessment was performed in 93 samples according to the
manufacturer's instructions, as described previously (13,17,18).
Briefly, 3-µm sections of formalin-fixed, paraffin-embedded tissue
blocks were stained with polyclonal rabbit periostin (1:4,000
dilution; catalog no. RD181045050; Biovendor GmbH, Kassel,
Germany), monoclonal mouse α-SMA (1:1,500 dilution; catalog no.
M0851; Dako, Glostrup, Denmark) and monoclonal mouse CD31 (1:50
dilution; catalog no. M0823; Dako) antibodies, and with the
collagen-specific aniline blue of the Masson trichrome stain,
without applying hematoxylin or Biebrich scarlet-acid fuchsin as
counterstaining.
Slide evaluation
Slides were scanned with a Nikon coolscan V (Nikon
Corporation, Tokyo, Japan) at 4,000 dots per inch. The digital
images were analyzed for the total surface area vs. stained area
using Adobe Photoshop 7.0 (Adobe Systems Inc., San Jose, CA, USA),
as described previously (12).
Briefly, histograms of gray-scale converted images were used to
quantify the surface area in pixels. The upper and lower input
levels were overlapped to create black or white image areas,
without an intermediate zone. For best sensitivity of detection,
the point of overlap was set to the vertex of the initial
exponential phase of the histogram curve. After identifying the
best adjustments, values were kept throughout all analyses. The
median surface area analyzed was 159 mm2 per section,
which corresponds to >1,000 high-power fields (x×
magnification). The immunohistochemical analysis and quantification
of the activated stroma index were arranged in a manner that was
blinded to the clinical data. Median values were used as the
cut-off to define sections with high and low levels. The activated
stroma index, defined as the ratio of the α-SMA-stained area to the
collagen-stained area, was defined in the same manner (12). For visualization, immunohistochemical
analyses were repeated for periostin, α-SMA and CD31 in
representative blocks.
Statistical analysis
Time-dependent survival probabilities were estimated
with the Kaplan-Meier method; the log-rank test was used to compare
subgroups. Overall survival was defined as the time from the date
of diagnosis until mortality or last follow-up. To investigate the
effect on survival of multivariable associations among covariates,
Cox proportional hazard models were used. Survival times and
estimated hazard ratios (HRs) were calculated, and 95% confidence
intervals (95% CIs) were reported. To avoid over-adjustment in the
multivariable survival analysis due to the limited sample size,
consecutively (one by one) testing of the putative confounders
tumor stage (T), lymph node status (N) and grading (G) was
performed. All tests were two-sided, and P-values of <0.05 were
considered to indicate a statistically significant difference. No
correction of P-values was applied to adjust for multiple test
issues. However, the results of all conducted statistical tests are
thoroughly reported, so that an informal adjustment of P-values can
be performed while reviewing the data (19). Statistical testing was performed using
IBM® SPSS® statics software, version 19 (IBM
SPSS, Armonk, NY, USA).
Results
Study group
The study group consisted of 93 patients with NSCLC.
Of those, 66 patients presented with adenocarcinoma, 22 with
squamous cell carcinoma, 3 with large cell carcinoma and 2 with
adenosquamous cell carcinoma. There were 56 men (60.2%) and 37
women (39.8%). The median age at diagnosis was 69 years in the men
and 62 years in the women. Clinical and histopathological patient
characteristics are shown in Table
I.
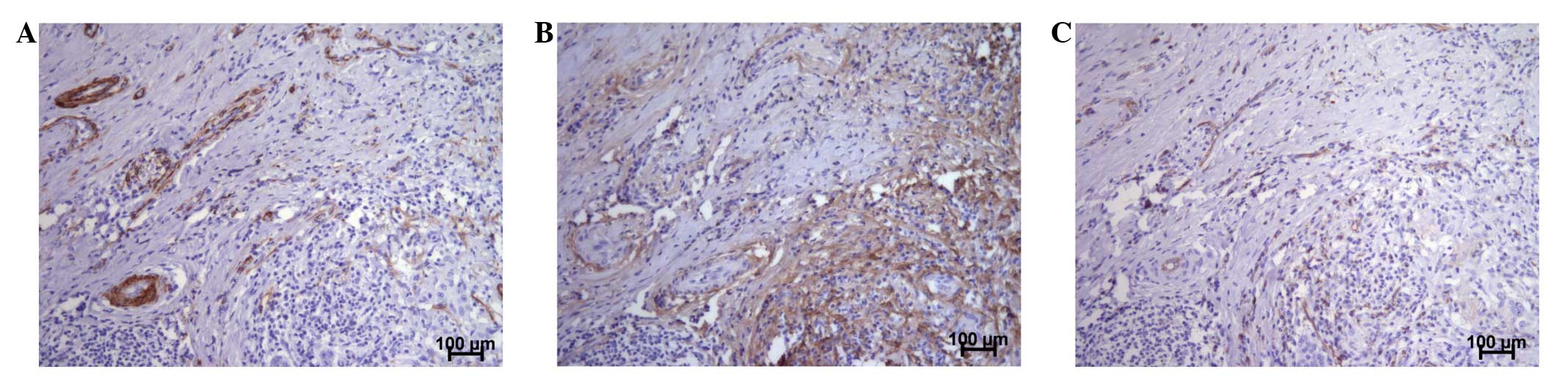
Immunohistochemistry
Sections of NSCLC were stained against periostin as
a matrix protein and against α-SMA to detect myofibroblasts. High
periostin expression was found in areas that co-localized with
myofibroblasts (Fig. 1A and B). These
myofibroblasts were predominantly found around cancer cells. By
contrast, the vessel density analyzed by the endothelial marker
CD31 (Fig. 1C) was evenly distributed
over the whole specimen.
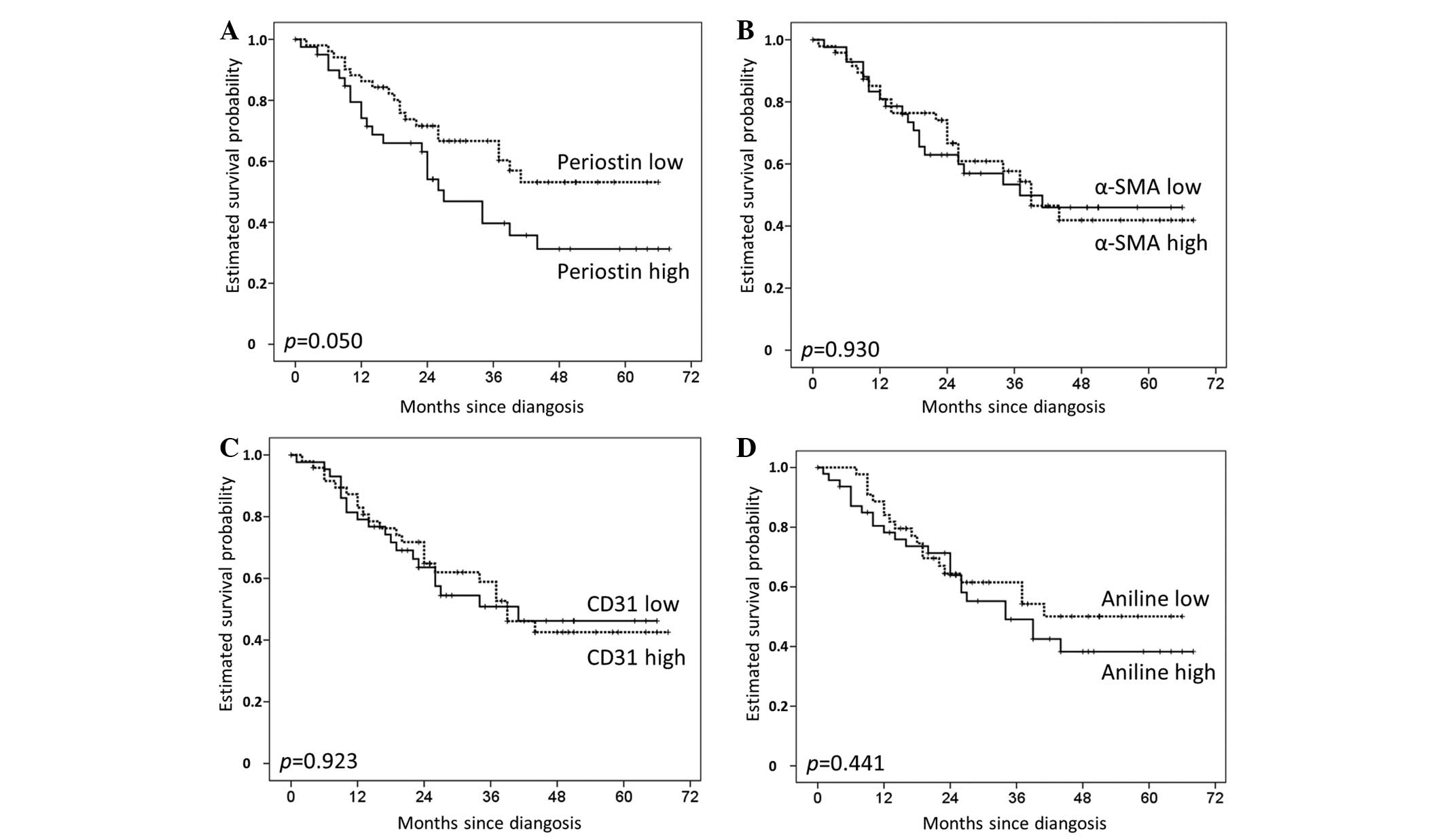
Univariable survival analysis
There was a trend towards reduced overall survival
for patients with high periostin levels, as defined by the median
(HR 1.80; 95% CI, 0.99–3.27; P=0.050). However, this did not reach
statistical significance. The 1− and 2-year survival rates for
patients with high periostin levels were 74 and 63%, respectively,
compared with 85 and 72%, respectively, for those with low
periostin expression (Fig. 2).
Survival differences were even less pronounced for α-SMA (HR, 1.03;
95% CI, 0.56–1.88; P=0.930), CD31 (HR, 1.03; 95% CI, 0.57–1.88;
P=0.923) and aniline (HR, 1.26; 95% CI, 0.69–2.31; P=0.441). No
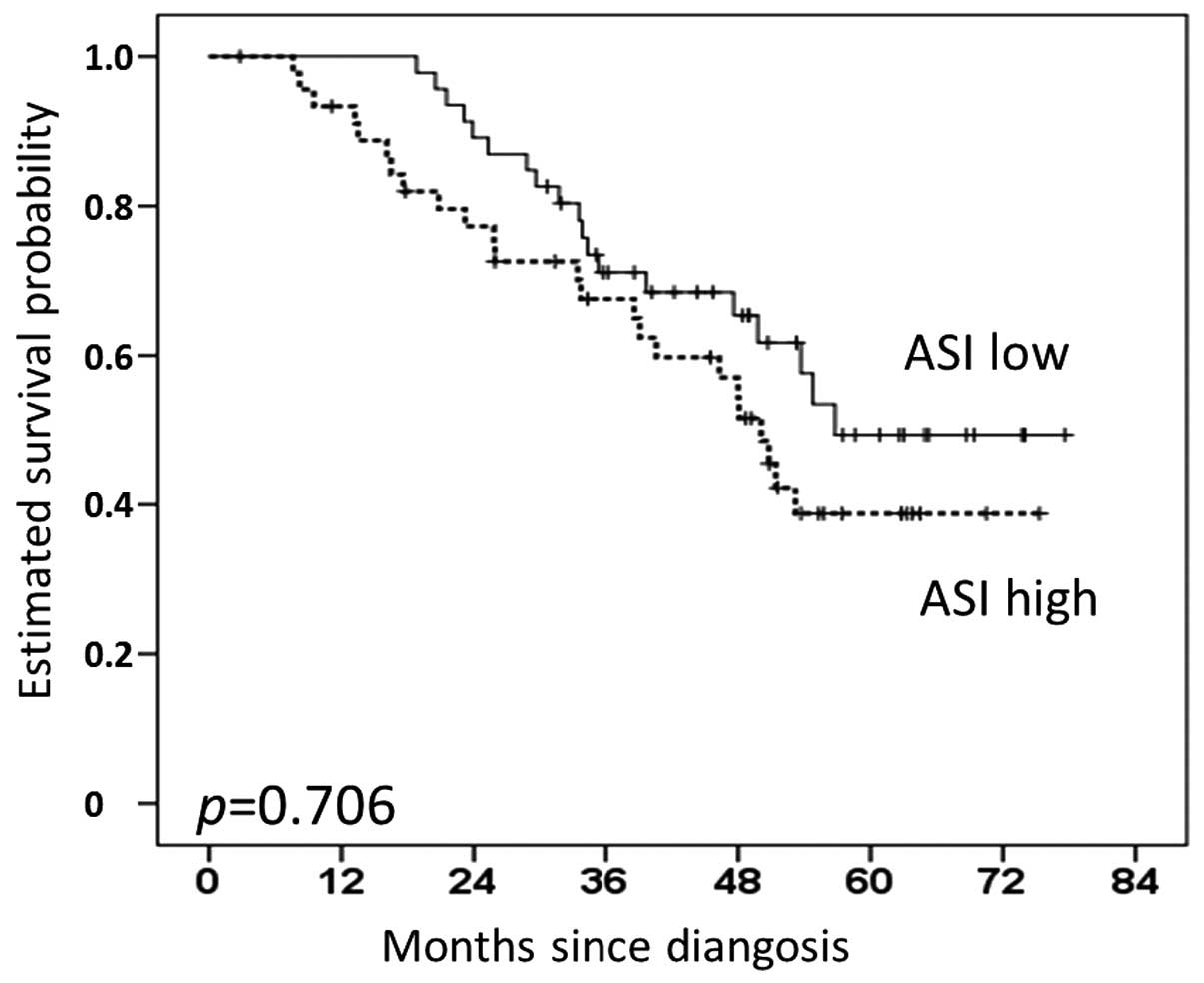
significant survival difference existed for the activated stroma
index, defined as the quotient of the α-SMA- and aniline-stained
areas (HR, 1.12; 95% CI, 0.62–2.04; P=0.706) (Fig. 3). In the univariable survival analysis
of clinical and other histopathological factors, only the resection
status (R0 vs. R1, P=0.030) and nodal tumor involvement were
statistically significant predictors of a poor prognosis. The
hazard ratio was more than doubled for patients with N1 compared
with N0 (P=0.026), and more than four times greater for patients
with N2/3 compared with N0 (P<0.001) (Table II). The histological tumor subtype
(adenocarcinoma, squamous carcinoma, large-cell carcinoma and
adenosquamous carcinoma; P=0.211), T stage (P=0.189), grading
(P=0.507) and gender (P=0.055) exhibited no significant effect on
survival upon univariable analysis [log-rank (Mantel-Cox)].
 | Table II.Univariable cox regression analysis
on overall survival. |
Table II.
Univariable cox regression analysis
on overall survival.
| Parameter | Hazard ratio | 95% confidence
interval | P-value |
|---|
| Periostin
(high) | 1.80 | 0.99–3.27 | 0.050 |
| α-SMA (high) | 1.03 | 0.56–1.88 | 0.930 |
| CD31 (high) | 1.03 | 0.57–1.88 | 0.923 |
| Collagen
(high) | 1.26 | 0.69–2.31 | 0.441 |
| ASI (high) | 1.12 | 0.62–2.04 | 0.706 |
| Nodal status |
|
| 0.001a |
|
N1/N0 | 2.27 | 1.10–4.67 | 0.026 |
|
N2–3/N0 | 4.05 | 1.96–8.37 | <0.001 |
| Grade |
|
| 0.823a |
|
G2/G3 | 0.82 | 0.44–1.54 | 0.533 |
| Tumor status |
|
| 0.222a |
|
T2/T1 | 1.47 | 0.69–3.16 | 0.321 |
|
T3/T1 | 2.06 | 0.73–5.79 | 0.171 |
|
T4/T1 | 3.64 | 0.97–13.6 | 0.055 |
Multivariable survival analysis
A multivariable analysis was performed in order to
investigate the role of periostin as an independent prognostic
factor after adjustment for the clinical and histopathological
parameters: Tumor type, stage (T), lymph node involvement (N),
grading (G), resection status (R) and gender. In concordance with
the univariable analysis, periostin was not identified as an
independent prognostic factor (HR, 0.52; 95% CI, 0.21–1.24;
P=0.137; Table III). Due to the
limited number of patients in the study, not all
immunohistochemical markers (periostin, α-SMA, CD31, aniline, and
the activated stroma index) could be included simultaneously in
order to receive reliable results. Thus, another multivariable
analysis was performed, with consecutive (one by one) adjustment of
the effects of expression profiles for potentially confounding
factors T, N and G. However, none of the immunohistochemical
markers were found to be independent prognostic factors (Table IV).
 | Table III.Multivariable cox regression analysis
on overall survival for periostin, adjusted for clinical and
histopathological factors. |
Table III.
Multivariable cox regression analysis
on overall survival for periostin, adjusted for clinical and
histopathological factors.
|
|
|
| 95% confidence
interval |
|---|
|
|
|
|
|
|---|
| Parameter | P-value | Hazard ratio | Lower | Upper |
|---|
| Periostin low (vs.
high) | 0.137 | 0.52 | 0.21 | 1.24 |
| Adenocarcinoma | 0.047 | 1.00 |
|
|
| vs.
Squamous | 0.036 | 0.08 | 0.01 | 0.85 |
| vs.
Large cell | 0.033 | 0.06 | 0.04 | 0.80 |
| vs.
Adenosquamous | 0.412 | 4.84 | 0.11 | 208.76 |
| T1 | 0.119 | 1.00 |
|
|
| vs.
T2 | 0.058 | 11.75 | 0.92 | 150.64 |
| vs.
T3 | 0.019 | 25.89 | 1.72 | 390.69 |
| vs.
T4 | 0.041 | 10.25 | 1.11 | 95.11 |
| N0 | 0.005 | 1.00 |
|
|
| vs.
N1 | 0.695 | 0.64 | 0.07 | 6.16 |
| vs.
N2 | 0.394 | 2.82 | 0.26 | 30.74 |
| vs.
N3 | 0.124 | 9.66 | 0.54 | 174.09 |
| G1 | 0.773 | 1.00 |
|
|
| vs.
G2 | 0.988 | <0.001 | <0.001 | <0.001 |
| vs.
G3 | 0.473 | 0.70 | 0.26 | 1.87 |
| R0 (vs. R1) | 0.010 | 0.11 | 0.21 | 0.59 |
| Male (vs.
Female) | 0.599 | 1.30 | 0.49 | 3.43 |
 | Table IV.Consecutive (one by one)
multivariable cox regression analysis on overall survival for the
immunohistochemical tested markers, with adjustment for the
putative relevant histopathological confounding factors. |
Table IV.
Consecutive (one by one)
multivariable cox regression analysis on overall survival for the
immunohistochemical tested markers, with adjustment for the
putative relevant histopathological confounding factors.
|
| Periostin (high vs.
low) | α-SMA (high vs.
low) | CD31 (high vs.
low) | Anilin (high vs.
low) | ASI (high vs.
low) |
|---|
|
|
|
|
|
|
|
|---|
| Adjustment variable
(potential confounder) | HR | 95% CI | P-value | HR | 95% CI | P-value | HR | 95% CI | P-value | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Nodal status | 1.52 | 0.83–2.78 | 0.175 | 0.98 | 0.53–1.79 | 0.939 | 0.81 | 0.44–1.49 | 0.492 | 1.08 | 0.58–2.01 | 0.814 | 0.94 | 0.50–1.74 | 0.84 |
| Grade | 1.69 | 0.91–3.13 | 0.097 | 0.93 | 0.50–1.72 | 0.822 | 0.85 | 0.46–1.58 | 0.614 | 1.21 | 0.66–2.23 | 0.544 | 1.09 | 0.60–2.00 | 0.78 |
| Tumor status | 1.69 | 0.91–3.13 | 0.094 | 1.16 | 0.61–2.19 | 0.658 | 1.09 | 0.58–2.05 | 0.795 | 1.46 | 0.76–2.80 | 0.252 | 1.17 | 0.64–2.13 | 0.62 |
Discussion
The invasiveness of cancer cells is facilitated by
EMT, among other things. The basis of EMT involves multiple changes
in expression, distribution and/or function of proteins, such as
periostin, vimentin and integrin (20,21).
Periostin physiologically regulates bone/tooth formation and
maintenance, as well as cardiac development and healing (15). Pathophysiologically, it further plays
an important role in tumor development, with upregulation in a
variety of cancers, including colon, pancreatic, ovarian, breast,
head and neck, thyroid and gastric cancer, and NSCLC (15). Periostin can co-localize with
fibronectin and collagen, thereby promoting an extracellular matrix
organization, which supports invasion and metastasis. This process
is regulated through the binding of periostin on integrin receptors
and the downstream activation of focal adhesion kinase and
Akt/phosphatidylinositol-3-kinase signaling (15). As we have shown previously, a highly
active stroma is characterized by high levels of periostin and
α-SMA, as well as reduced levels of dormant collagen deposits. This
corresponds to a high grade of EMT and is an independent poor
prognostic factor in pancreatic cancer (12). However, a few studies of bladder
cancer and osteosarcoma have described periostin as a
tumor-inhibiting factor in these entities (15,22,23). One
main difference between pancreatic cancer and NSCLC is that in lung
cancer, periostin is not only expressed from activated stellate
cells, likewise, cancer cells are able to produce and secrete this
extracellular matrix molecule (14–16). Morra
and Moch found that upregulation of the extracellular matrix
protein periostin is correlated with a worse prognosis in numerous
tumor entities, and that although dependent on the tumor entity,
periostin can be produced by both the cancer cells and the
peritumoral component of the stroma (15). In the case of NSCLC, detectable
periostin expression was described to be mostly produced by the
tumor cells themselves, rather than by the stroma (15). By contrast, the present study detected
high periostin expression in areas co-localized with
myofibroblasts, which in turn were found around the cancer cells
(Fig. 1B). Thus, the exact mechanism
of periostin production in NSCLC remains unclear and should be a
matter for further investigation.
The activity of myofibroblasts (e.g., stellate cells
in the pancreas) is indicated by α-SMA expression and implicates a
worsened prognosis, as found in the pancreas (12). The present study provides evidence
that patients with elevated α-SMA expression in NSCLC have a
reduced prognosis as well; although these data were not
statistically significant. The activity of myofibroblasts is
associated with collagen deposition. For this, the activated stroma
index, a prognostic factor that is defined as the ratio of
α-SMA-stained regions against collagen-stained areas, was
calculated (12). In pancreatic
cancer with its large collagen deposits, a worse prognosis was
found in patients with high intratumoral stromal activity, defined
by high α-SMA activity together with low collagen deposition
(12). However, NSCLC appears to have
a clearly different stromal composition (6,24), and the
activated stroma index was not confirmed as a significant
prognostic factor in the present study.
Neoangiogenesis plays a crucial role in tumor growth
and metastasis. Several studies have demonstrated that
neoangiogenesis is a significant prognostic factor for overall
survival in lung cancer, and currently there are a number of
inhibitors of angiogenesis in clinical use for the treatment of
cancer (25–28). The intratumoral microvessel density is
a predictor of tumor growth, metastasis and patient survival
(29). However, recent data suggested
no significant differences in the microvessel density of bronchial
normal mucosa, metaplasia, dysplasia and carcinoma in situ
(30). Thus, it is not yet clear in
which step of bronchial carcinogenesis angiogenesis actually plays
the most crucial role (30). Double
immunostaining for CD31 and α-SMA allows the estimation of juvenile
blood vessels in neoplasms (30). In
the present study the impact of microvessel density was analyzed;
however, there was no significant survival difference for patients
with low versus high microvessel density.
The present study described the tumor
microenvironment and EMT in NSCLC. Considering that pancreatic
cancer exhibits mutual activation of tumor cells and the
surrounding stroma (12), these
tumor-stroma interactions were expected for other entities as well.
However, despite the limited sample size and inclusion of different
tumor entities (NSCLC) (16), no such
significant stroma activation was observed in NSCLC. NSCLC has
distinct histopathological characteristics. Tumor-stroma
interactions and the tumor microenvironment play an important role;
however, the most relevant candidate markers and paracrine or
autocrine crosstalk pathways appear to be different from those
known for pancreatic cancer (6,24).
In conclusion, stroma activation was not confirmed
as an independent prognostic factor for patients with NSCLC in this
retrospective study. Together with previous results, this
highlights the heterogeneity of different cancer entities and the
requirement for future highly individualized therapeutic
concepts.
Acknowledgements
This study was supported by a donation from the
Marianne-Lutter Nachlass and by Koc University (Istanbul,
Turkey).
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Herbst RS, Heymach JV and Lippman SM: Lung
cancer. N Engl J Med. 359:1367–1380. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Goldstraw P, Ball D, Jett JR, Le Chevalier
T, Lim E, Nicholson AG and Shepherd FA: Non-small-cell lung cancer.
Lancet. 378:1727–40. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Heukamp LC and Büttner R: Molecular
diagnostics in lung carcinoma for therapy stratification.
Pathologe. 31:22–28. 2010.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ferlay J, Autier P, Boniol M, Heanue M,
Colombet M and Boyle P: Estimates of the cancer incidence and
mortality in Europe in 2006. Ann Oncol. 18:581–592. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
El-Nikhely N, Larzabal L, Seeger W, Calvo
A and Savai R: Tumor-stromal interactions in lung cancer: Novel
candidate targets for therapeutic intervention. Expert Opin
Investig Drugs. 21:1107–1122. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
de Visser KE, Eichten A and Coussens LM:
Paradoxical roles of the immune system during cancer development.
Nat Rev Cancer. 6:24–37. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mantovani A, Allavena P, Sica A and
Balkwill F: Cancer-related inflammation. Nature. 454:436–444. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bremnes RM, Dønnem T, Al-Saad S, Al-Shibli
K, Andersen S, Sirera R, Camps C, Marinez I and Busund LT: The role
of tumor stroma in cancer progression and prognosis: Emphasis on
carcinoma-associated fibroblasts and non-small cell lung cancer. J
Thorac Oncol. 6:209–217. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dunér S, Lindman J Lopatko, Ansari D,
Gundewar C and Andersson R: Pancreatic cancer: The role of
pancreatic stellate cells in tumor progression. Pancreatology.
10:673–681. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kalluri R: Basement membranes: Structure,
assembly and role in tumour angiogenesis. Nat Rev Cancer.
3:422–433. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Erkan M, Michalski CW, Rieder S,
Reiser-Erkan C, Abiatari I, Kolb A, Giese NA, Esposito I, Friess H
and Kleeff J: The activated stroma index is a novel and independent
prognostic marker in pancreatic ductal adenocarcinoma. Clin
Gastroenterol Hepatol. 6:1155–1161. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Erkan M, Kleeff J, Gorbachevski A, Reiser
C, Mitkus T, Esposito I, Giese T, Büchler MW, Giese NA and Friess
H: Periostin creates a tumor-supportive microenvironment in the
pancreas by sustaining fibrogenic stellate cell activity.
Gastroenterology. 132:1447–1464. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kanno A, Satoh K, Masamune A, Hirota M,
Kimura K, Umino J, Hamada S, Satoh A, Egawa S, Motoi F, et al:
Periostin, secreted from stromal cells, has biphasic effect on cell
migration and correlates with the epithelial to mesenchymal
transition of human pancreatic cancer cells. Int J Cancer.
122:2707–2718. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Morra L and Moch H: Periostin expression
and epithelial-mesenchymal transition in cancer: A review and an
update. Virchows Arch. 459:465–475. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hong LZ, Wei XW, Chen JF and Shi Y:
Overexpression of periostin predicts poor prognosis in non-small
cell lung cancer. Oncol Lett. 6:1595–1603. 2013.PubMed/NCBI
|
|
17
|
Erkan M, Kleeff J, Esposito I, Giese T,
Ketterer K, Büchler MW, Giese NA and Friess H: Loss of BNIP3
expression is a late event in pancreatic cancer contributing to
chemoresistance and worsened prognosis. Oncogene. 24:4421–4432.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Michalski CW, Shi X, Reiser C, Fachinger
P, Zimmermann A, Büchler MW, Di Sebastiano P and Friess H:
Neurokinin-2 receptor levels correlate with intensity, frequency,
and duration of pain in chronic pancreatitis. Ann Surg.
246:786–793. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Saville DJ: Multiple comparison
procedures: The practical solution. Am Stat. 44:174–180. 1990.
View Article : Google Scholar
|
|
20
|
Soltermann A, Tischler V, Arbogast S,
Braun J, Probst-Hensch N, Weder W, Moch H and Kristiansen G:
Prognostic significance of epithelial-mesenchymal and
mesenchymal-epithelial transition protein expression in non-small
cell lung cancer. Clin Cancer Res. 14:7430–7437. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yan W and Shao R: Transduction of a
mesenchyme-specific gene periostin into 293T cells induces cell
invasive activity through epithelial-mesenchymal transformation. J
Biol Chem. 281:19700–19708. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kim CJ, Yoshioka N, Tambe Y, Kushima R,
Okada Y and Inoue H: Periostin is down-regulated in high grade
human bladder cancers and suppresses in vitro cell invasiveness and
in vivo metastasis of cancer cells. Int J Cancer. 117:51–58. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yoshioka N, Fuji S, Shimakage M, Kodama K,
Hakura A, Yutsudo M, Inoue H and Nojima H: Suppression of
anchorage-independent growth of human cancer cell lines by the
TRIF52/periostin/OSF-2 gene. Exp Cell Res. 279:91–99. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Choi H, Sheng J, Gao D, Li F, Durrans A,
Ryu S, Lee SB, Narula N, Rafii S, Elemento O, et al: Transcriptome
analysis of individual stromal cell populations identifies
stroma-tumor crosstalk in mouse lung cancer model. Cell Rep.
10:1187–1201. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yano T, Tanikawa S, Fujie T, Masutani M
and Horie T: Vascular endothelial growth factor expression and
neovascularisation in non-small cell lung cancer. Eur J Cancer.
36:601–609. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Giatromanolaki A, Koukourakis MI,
Theodossiou D, Barbatis K, O'Byrne K, Harris AL and Gatter KC:
Comparative evaluation of angiogenesis assessment with
anti-factor-VIII and anti-CD31 immunostaining in non-small cell
lung cancer. Clin Cancer Res. 3:2485–2492. 1997.PubMed/NCBI
|
|
27
|
Han H, Silverman JF, Santucci TS, Macherey
RS, d'Amato TA, Tung MY, Weyant RJ and Landreneau RJ: Vascular
endothelial growth factor expression in stage I non-small cell lung
cancer correlates with neoangiogenesis and a poor prognosis. Ann
Surg Oncol. 8:72–79. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Koukourakis MI, Giatromanolaki A, O'Byrne
KJ, Whitehouse RM, Talbot DC, Gatter KC and Harris AL: Potential
role of bcl-2 as a suppressor of tumour angiogenesis in
non-small-cell lung cancer. Int J Cancer. 74:565–570. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sharma S, Sharma MC and Sarkar C:
Morphology of angiogenesis in human cancer: A conceptual overview,
histoprognostic perspective and significance of neoangiogenesis.
Histopathology. 46:481–489. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Raica M, Cimpean AM and Ribatti D:
Angiogenesis in pre-malignant conditions. Eur J Cancer.
45:1924–1934. 2009. View Article : Google Scholar : PubMed/NCBI
|