Introduction
A complicated process is involved in wound healing,
including inflammatory, proliferative and remodeling phases
(1). In the initial inflammatory
phase, the most distinguishing features are the infiltration of
neutrophils and macrophages, along with hemostasis. The aim of the
proliferative phase is to increase the density of scaffold for cell
migration subsequent to debridement (2). In the remodeling phase, the process is
induced by various growth factors or signaling molecules, including
epidermal growth factor, transforming growth factor-α,
platelet-derived growth factor, acidic fibroblast growth factor
(FGF), basic FGF, keratinocyte growth factor, interleukin-1 and
insulin-like growth factor, which play critical roles in the
pro-fibrogenic and pro-inflammatory reactions (3). Previous studies have shown that
osteopontin (OPN) participates in several diverse physiological and
pathological processes, including wound healing, bone remodeling,
cancer metastasis and invasiveness, and inhibition of apoptosis
(3–6).
OPN is a secreted phospho-protein that is synthesized by various
immune cells, such as macrophages, dendritic cells and natural
killer cells (7,8). OPN activates cell signaling pathways by
phosphorylation binding to extracellular receptors, including focal
adhesion kinase (FAK), paxillin, tensin and Src (9,10).
Previous studies have demonstrated that OPN is critical during the
migration and proliferation of both human lung fibroblasts and
mouse epithelial cells (11–13). However, whether OPN has an evident
role in improving the ability of cell adhesion and migration in the
deep layers of the wound remains unknown. The mechanism of action
also remains unclear.
In the present study, the effect of knockdown or
overexpression of OPN on human primary renal cortical epithelial
cells is reported. The present study aimed to investigate the role
of OPN in wound healing through its effects on human deep layers of
epithelial cell migration, proliferation and adhesion. It was
hypothesizes that OPN promotes epithelial cell migration,
proliferation by increasing protein expression associated with cell
adhesion.
Materials and methods
Reagents and cell culture
Antibodies against OPN (rabbit polyclonal
anti-human; 1:1,500; ab8448), phosphorylated (p)-Y118-paxillin
(rabbit polyclonal anti-human; 1:1,000; 2541), GAPDH [rabbit
polyclonal anti-human; XP® Rabbit mAb (HRP Conjugate);
1:2,000; 8884), paxillin (rabbit anti-human; 1:1,000; 2542), FAK
(rabbit polyclonal anti-human; 1:1,000; 3285) and pY Tyr576/577-FAK
(rabbit polyclonal anti-human; 1:1,000; 3281) were purchased from
Cell Signaling Technology, Inc. (Danvers, MA, USA). Dulbecco's
modified Eagle's medium (DMEM) was purchased from Gibco (Thermo
Fisher Scientific, Inc., Waltham, MA, USA). Fetal bovine serum
(FBS) was purchased from HyClone (GE Healthcare Life Sciences,
Logan, UT, USA). All other reagents were obtained from
Sigma-Aldrich (Merck Millipore, Darmstadt, Germany) unless
otherwise described. The human primary renal cortical epithelial
cells (Normal; PCS-400-011) were obtained from American Type
Culture Collection (Manassas, VA, USA). The cells were maintained
in DMEM containing 200 U/ml penicillin G (Gibco; Thermo Fisher
Scientific, Inc.), 200 µg/ml streptomycin and 10% FBS (HyClone; GE
Healthcare Life Sciences) at 37°C in a humid atmosphere of 5%
CO2 at 37°C.
Small interfering RNA (siRNA) and
overexpression vector
siRNAs were synthesized by Shanghai GenePharma Co.,
Ltd. (Shanghai, China). The siRNA sequences for mouse OPN siRNA
were as follows: siRNA sense, 5′-GAGGAGCCAUUUAUUGAAACUCG-3′ and
antisense, 5′-CGAGUUUCAAUAAAUGGCUCCUC-3′; and siRNA control (oligos
with no matching GeneBank sequence) sense,
5′-GCGACGAUCUGCCUAAGAU-3′ and antisense, 5′-AUCUUAGGCAGAUCGUCGC-3′.
The pairs of siRNA oligonucleotides were prepared as a 20 µM stock.
The OPN gene was cloned into the pcDNA™3.1 (−) Mammalian Expression
Vector (V79520; Invitrogen; Thermo Fisher Scientific, Inc.) as the
overexpression cassette.
For transient transfection, five groups were
created, consisting of the control, overexpression group
transfected with pcDNA3.1-OPN-GFP (over OPN), empty carrier group
with overexpression of a blank plasmid (over blank), siRNA
interference group (si-OPN) and siRNA blank (si-blank). The primary
renal cortical endothelial cell line was cultured in 6-well plates
to 80% confluence and then transfected using Lipofectamine RNAiMAX
(Invitrogen; Thermo Fisher Scientific, Inc.) according to the
manufacturer's instructions. The cells were collected 24 h
subsequent to transfection for other experiments.
Cell viability assay
Cell viability was determined using the MTT method
(14). The cells were plated into
96-well microtiter plates for 24 h. Subsequently, 10 µl of
MTT-labeling reagent was added to each well and the plates were
incubated at 37°C for 4 h. The cultures were then solubilized and
spectrophotometric absorbance of the samples was detected by a
microtiter plate reader. The wavelength used to measure the
absorbance of the formazan product was 570 nm, with a reference
wavelength of 750 nm. Cell viability was expressed as a percentage
of the positive control.
Wound healing assay
Wound healing experiments were performed for
quantitative investigation of the migration of cells. Cells were
grouped as aforementioned, consisting of the control, over OPN,
over blank, si-OPN and si-blank groups. The initial cell seeding
density was ~1×105 cells/cm2. A square wound
was made using a cell scraper. The cells were washed twice with PBS
and then incubated with fresh DMEM for another 24 h at 37°C. The
cells were then visualized by microscopy (IX71; Olympus,
Corporation, Tokyo, Japan).
Transwell assay
A further cell migration identification was
performed using Transwell assay. The cultured cells were detached
with trypsin subsequent to 8 h, and the treated cells were seeded
into a Millicell (Greiner Bio-One, Frickenhausen, Germany)
containing pores of 8 mm in diameter at an initial seeding density
of 1×105 cells/cm2, suspended in DMEM
containing 1% fetal bovine serum. The Millicell pores were then put
into the wells of a 24-well plate containing 20% fetal bovine serum
in DMEM. The cells on the Millicell pores were transfected with
four types of vectors (over OPN, over blank, si-OPN and si-blank).
Fresh DMEM was added 4 h later, and the cells were kept at 37°C for
another 24 h. The migrated cells were stained with crystal violet
(0.1% wt) and the number of migratory cells was recorded using an
optical microscope at ×100 magnification. The cell number was
randomly counted in 12 different fields of view for each group, and
the data were averaged from three parallel experiments.
RNA extraction and reverse
transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was isolated using TRIzol reagent
(Invitrogen; Thermo Fisher Scientific, Inc.). Subsequent to being
treated with RNase-free DNase I (Roche Applied Science, Penzberg,
Germany), first-strand cDNA was synthesized with Moloney murine
leukemia virus (M-MLV) reverse transcriptase and Oligo-dTs (Takara
Bio, Inc., Otsu, Japan). RT-qPCR was conducted using the ABI Prism
7500 Sequence Detection System, according to the manufacturer's
instructions (Applied Biosystems; Thermo Fisher Scientific, Inc.).
Specific primers used for RT-qPCR were as follows: OPN forward,
5′-GAAGTTTCGCAGACCTGACAT-3′ and reverse,
5′-GTATGCACCATTCAACTCCTCG-3′; FAK forward,
5′-AGTGGACCAGGAAATTGCTTTG-3′ and reverse,
5′-GTGTTTTGGCCTTGACAGAATCPCR-3′; paxillin forward,
CTGCTGGAACTGAACGCTGTA-3′ and reverse, 5′-GGGGCTGTTAGTCTCTGGGA-3′;
GAPDH forward, 5′-ACAACTTTGGTATCGTGGAAGG-3′ and reverse,
5′-GCCATCACGCCACAGTTTC-3′. For the relative comparison of each
gene, we analyzed the Cq value of qPCR data with the
2−ΔΔCq method normalized by the endogenous control GAPDH
(15).
Sample preparation and western
blotting
The procedure for immunoblotting has been previously
described (16). Cells were treated
with cell lysis buffer and then protein samples were collected.
Briefly, 40 µg protein/lane was loaded into the lanes of 12%
denatured polyacrylamide gel. The proteins were separated by
electrophoresis and transferred to nitrocellulose membranes (0.45
µm; Schleicher & Schuell; GE Healthcare Life Sciences). The
membranes were blocked with 3% bovine serum albumin in 0.01 M PBS
(pH 7.4) and 0.05% Tween-20 (PBST) at room temperature for 1 h.
Subsequently, the membrane was incubated with the aforementioned
primary antibodies against the target proteins overnight at 4°C.
Following two quick washes in PBST, the membranes were incubated
with secondary antibodies conjugated with horseradish peroxidase
[Goat Anti-Rabbit IgG H&L (HRP); dilution, 1:4,000 in PBST;
ab97051; Abcam, Cambridge, UK) for 2 h at room temperature.
Following washes as aforementioned, an enhanced chemiluminescence
reagent (Pierce™ DAB Substrate kit; 34002; Thermo Fisher
Scientific, Inc.) was used to produce fluorescence for detection.
The density of immunoblotting was quantified using Quantity One
software (Bio-Rad Laboratories, Inc., Hercules, CA, USA). The
relative expression of the target protein was quantified as a ratio
against GAPDH.
Statistical analysis
Experiments were performed routinely with >4
samples per group, with the values expressed as the mean ± standard
error of the mean. All experiments were replicated at least three
times. Statistical analysis was performed using one-way analysis of
variance and Student's t-test for multiple comparisons. P<0.05
was considered to indicate a statistically significant
difference.
Results
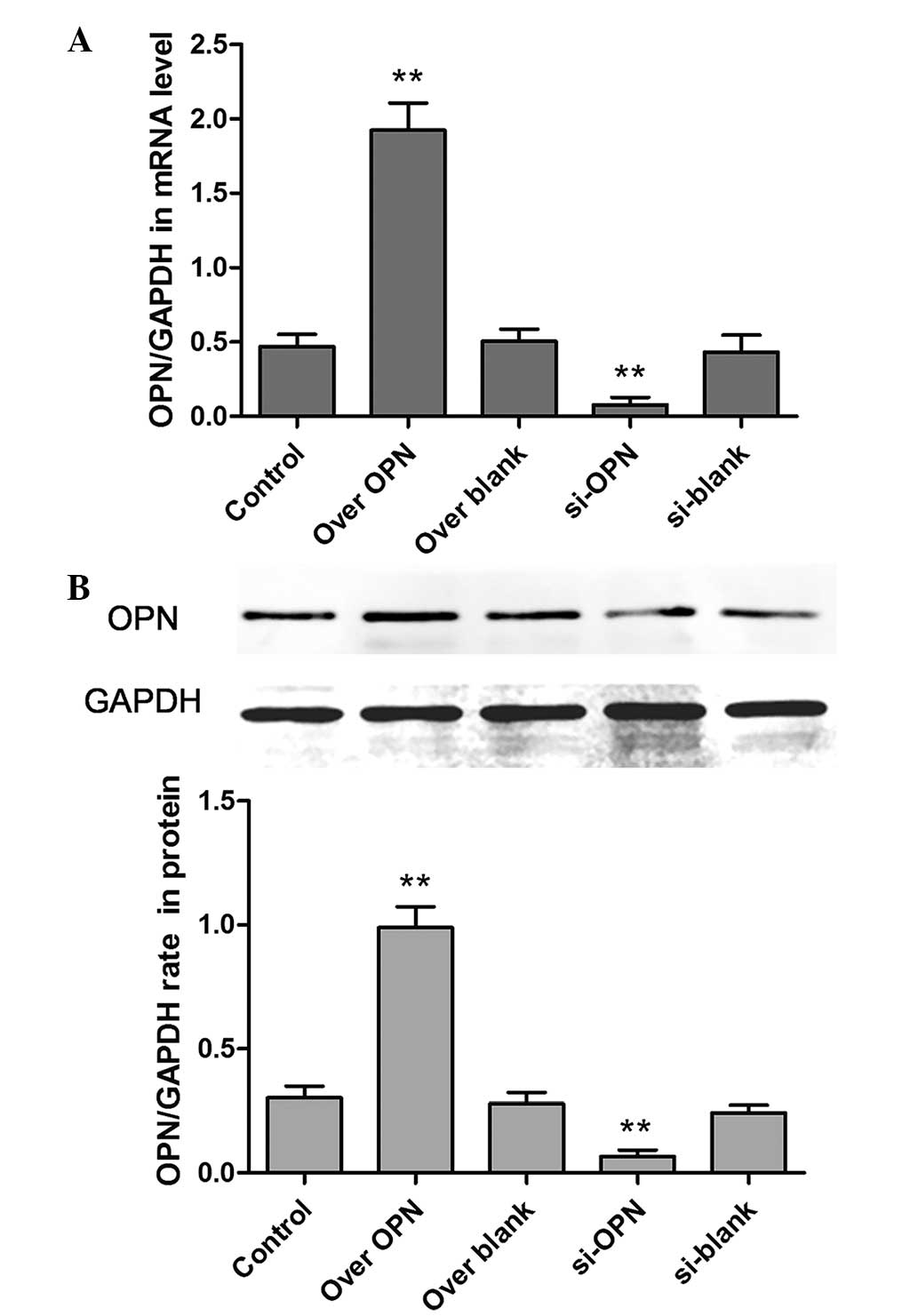
Efficiency of up- or downregulation of
OPN expression
The OPN expression was assessed by analyzing the
protein and mRNA levels. The results showed that the overexpression
vector was evidently effective, while the siRNA, which was selected
from several alternative siRNA sequences, could efficiently disturb
the expression of OPN (Fig. 1). The
expression of the over OPN group was significantly increased
compared with the blank group (P=0.0011). In addition, the
expression of si-OPN group was significantly decreased compared
with the blank (P=0.0021).
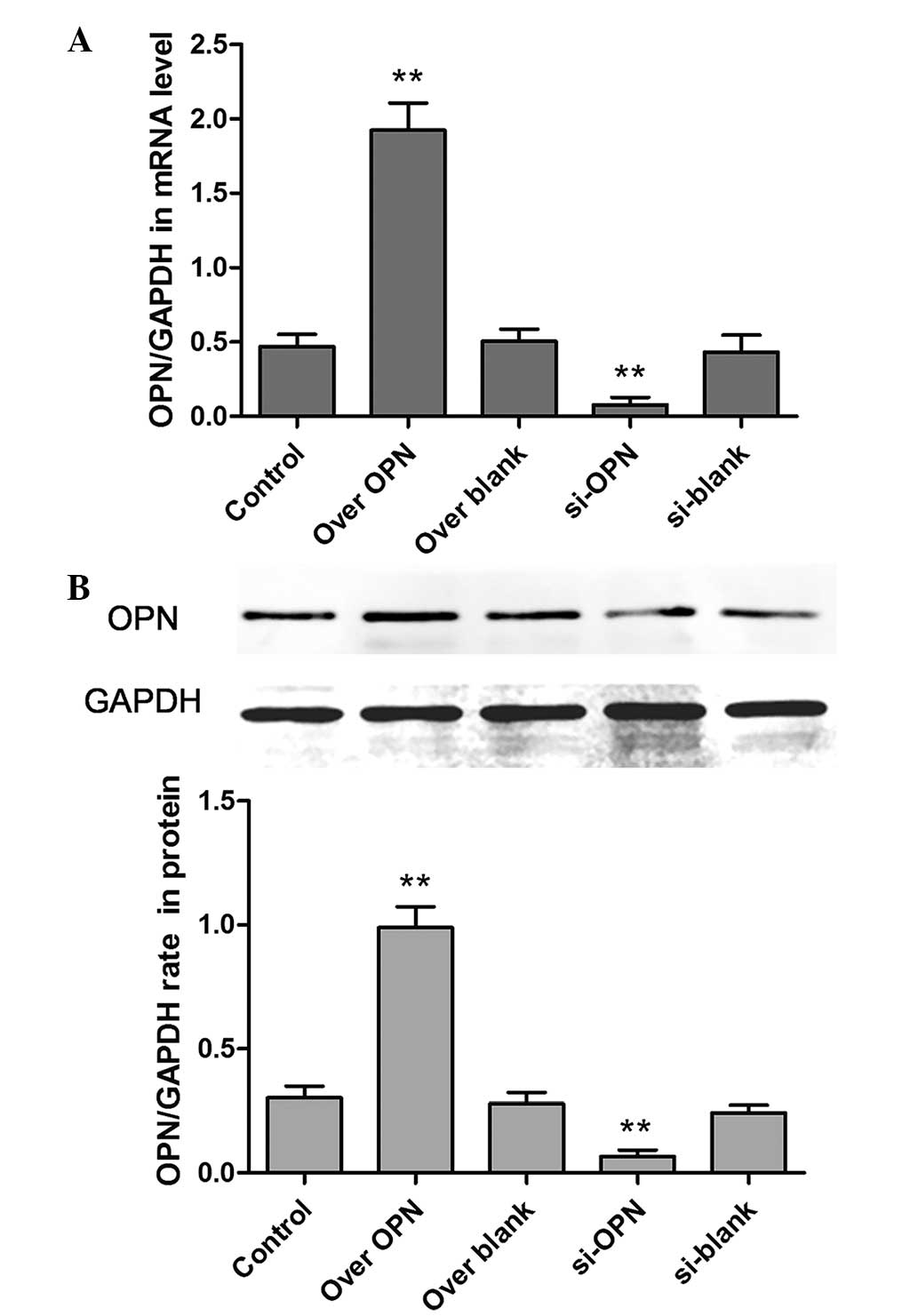 | Figure 1.Efficiency of the up- or
downregulation of OPN. Five groups, consisting of the control, over
OPN, over blank, si-OPN and si-blank groups, were formed based on
the transient transfection of the human primary renal cortical
endothelial cell line. The expression of OPN was detected by (A)
reverse transcription-polymerase chain reaction and (B) western
blot analysis. **P<0.01. OPN, osteopontin; over OPN,
over-expression of pcDNA3.1-OPN-green fluorescent protein; over
blank, empty carrier over-expression; si-OPN, small interfering RNA
interference; si-blank, small interfering RNA. |
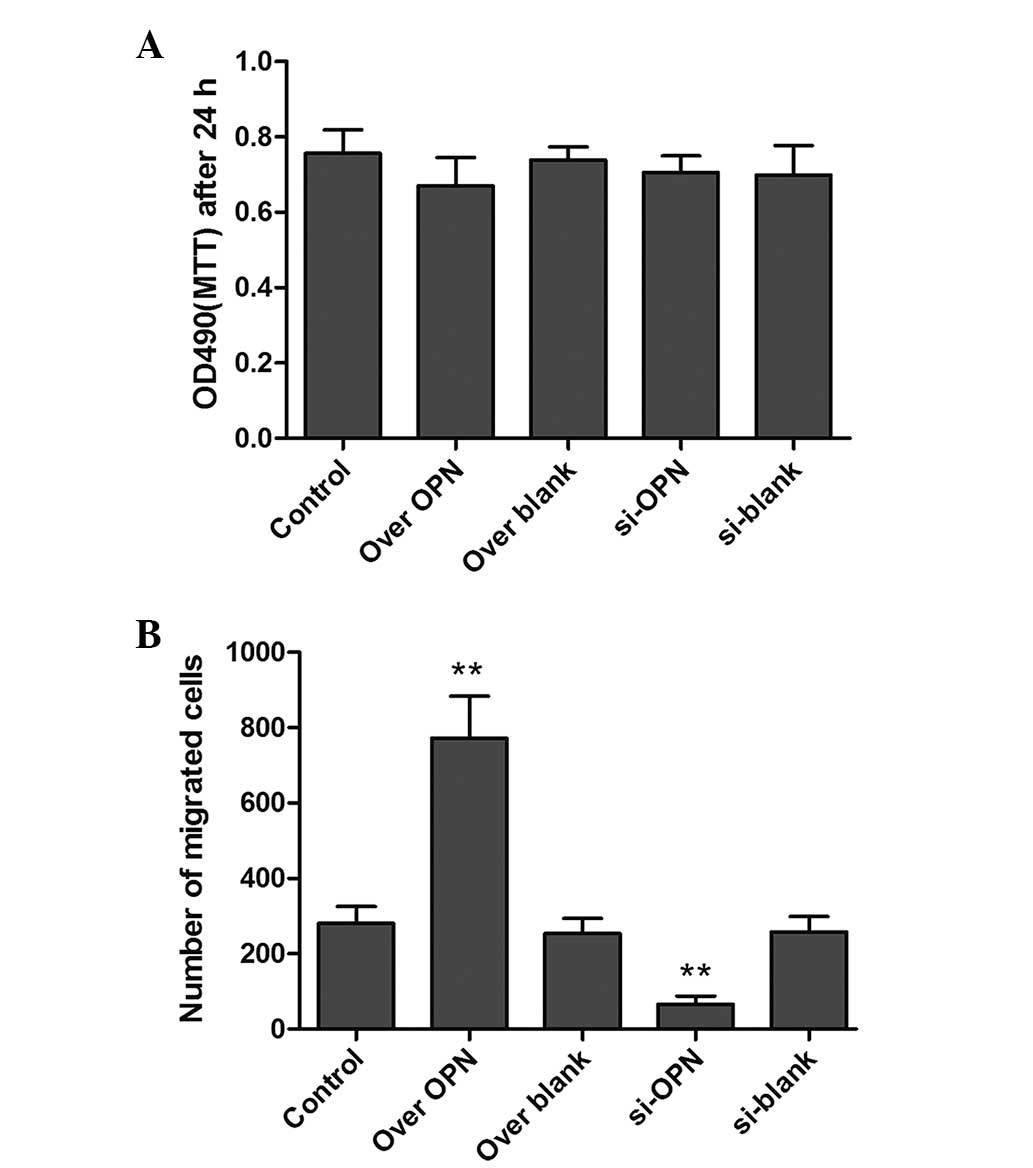
Effects of OPN on cell
proliferation
To investigate the effects of OPN on the
proliferation of human epithelial cells, the MTT assay was used to
examine the cell viability. However, there was no significant
difference between cell viability in the si-OPN group, over OPN
group and the control groups (Fig.
2). The results showed that increasing or decreasing OPN
expression did not significantly affect the cell proliferation.
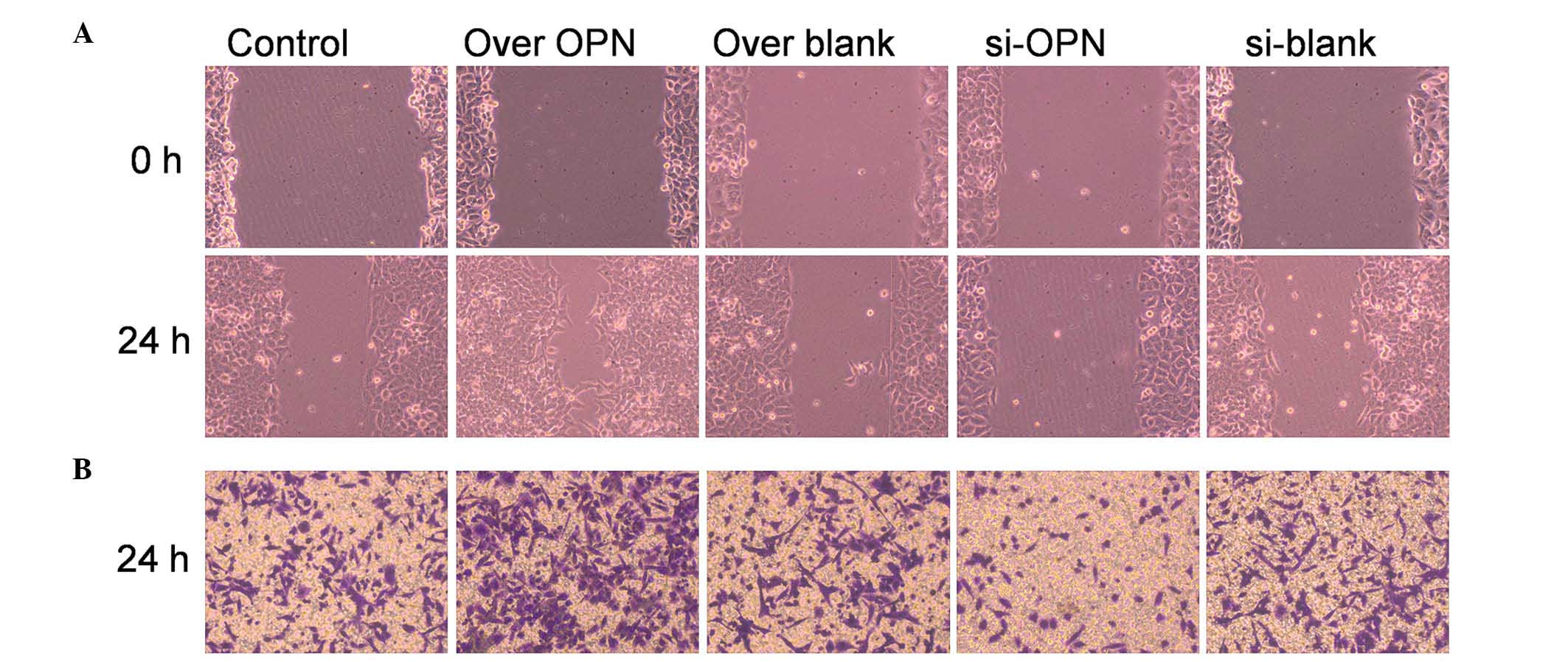
Overexpression of OPN increases human
epithelial cell migration
Macroscopic analyses of time-matched OPN
overexpression vs. control wounds showed that closure was markedly
accelerated (P=0.0372 and P=0.0241, respectively) at early time
points (12 and 18 h). Cells transfected with OPN-overexpressing
vectors exhibited a mean closure of the wound of 56% after 24 h,
while cells transfected with OPN-siRNA vectors achieved a mean
closure of the wound of 12% by 24 h, compared with the 24% average
closure observed in the blank control (Fig. 3A). Since OPN-overexpressing cells are
capable of almost complete and efficient wound closure, OPN may
play a pivotal role in the repair of deep layers of skin.
Transwell assay was also used to detect the
migration of epithelial cells. The number of migrated cells were
counted, and their shape is shown in Fig.
3B. The numbers of migrated cells in the over-OPN and si-OPN
groups were significantly increased (P=0.0223) and decreased
(P=0.0421), respectively, compared with the three blank groups,
indicating that OPN plays a vital role in accelerating cell
migration.
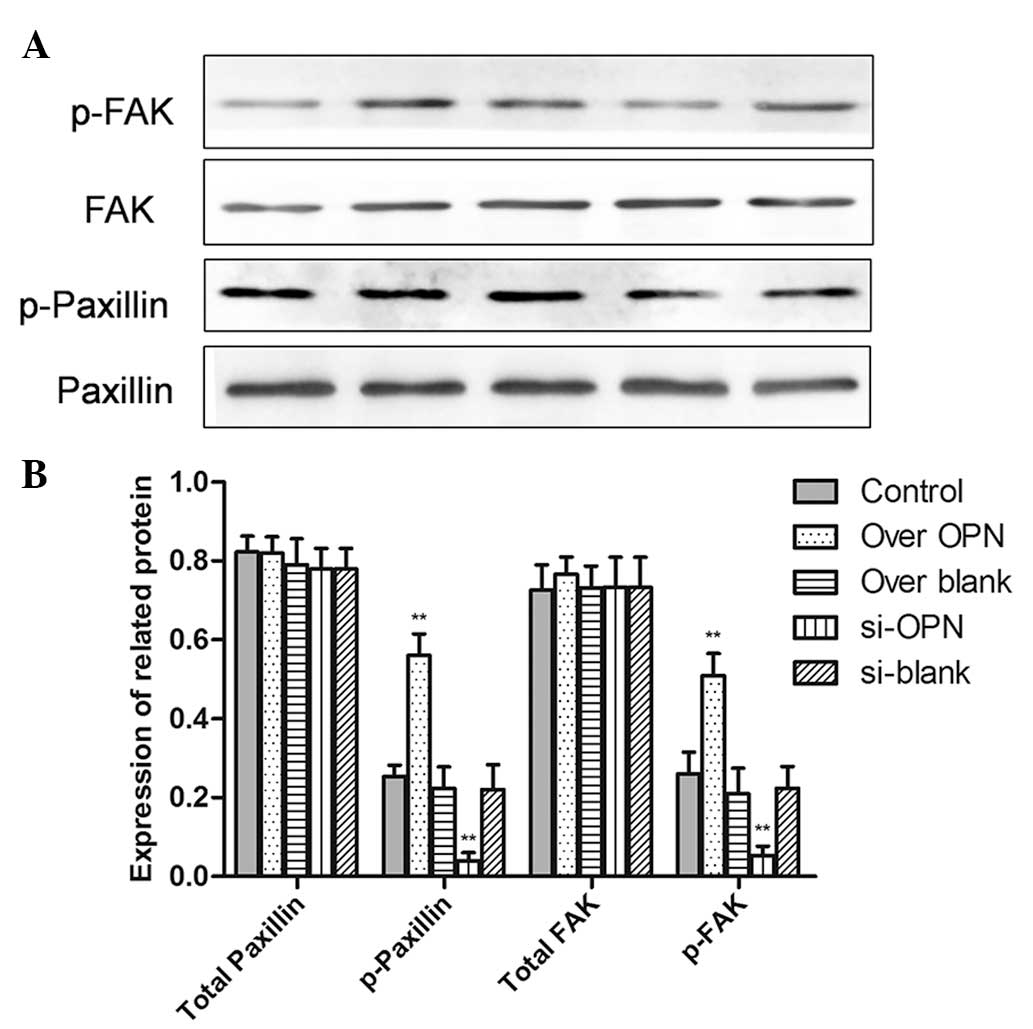
High expression of OPN improves the
adhesion of human epithelial cells
To investigate whether OPN induced stronger cell
attachment to the substrate, the expression of cell adhesion
molecules, including FAK and paxillin were also examined by western
blotting. The overexpression of OPN improved the phosphorylation of
paxillin (P=0.0001) and FAK (P=0.0001). Additionally, protein
expression of pY118-paxillin (P=0.0012) and pY-FAK (P=0.0002) was
inhibited by OPN downregulation. However, there is no difference in
the total FAK or paxillin among the five groups (Fig. 4). This result shows that the ability
of cell adhesion is decreased by OPN, while OPN is involved in
modulating signaling molecules associated with adhesion during
healing of the deep layers of a wound.
Discussion
OPN is an inflammation-dependent gene that is
expressed in wound granulation tissue accompanied by the
inflammatory response (17). OPN is
involved in signal transduction as a secreted chemotactic factor
(18,19), depending on the cellular
microenvironment. In addition, OPN may regulate cell adhesion,
migration, survival and immune reactions, as well as the balance
between osteoblasts and osteoclasts (10). It has been reported that OPN-knockout
mice developed normally, but the healing of skin wounds had a
longer time course compared with wild-type mice. Notably, there was
a large alteration in matrix architecture and collagen fibril
formation in the deep layers of the wound (13). However, the mechanism of this
alteration remains unclear.
OPN combined with cell receptors, particularly
αvβ3-integrin, was considered responsible for cell adhesion,
migration, proliferation and cytoskeletal regulation by
phosphorylation of FAK, paxillin, tensin or Src, which activate
downstream signal pathways in specific cellular responses (20,21).
However, the mechanism of OPN increasing the cell contractility and
adhesion remains unknown, since OPN binding to αvβ3-integrin may
change the cytoskeletal organization by activating FAK (20). In the present study, the expression of
pY118-paxillin and pY-FAK was significantly increased by OPN
overexpression during deep layers of wound healing.
These results provide insight into the role of OPN
in the deep layer of human epithelial cells during wound healing.
Previous studies have demonstrated that OPN plays an important role
in the occurrence and development of hepatic fibrosis by examining
organ fibrosis (12,22,23). Other
studies have also shown that OPN may induce the migration and
proliferation of lung fibroblasts in human idiopathic pulmonary
fibrosis (11). Furthermore, the
function of OPN in certain aspects of wound healing, such as the
effect on human epithelial cells, remains unknown. The present
study contributed to this knowledge by discussing the effects of
OPN on cell adhesion and migration in human epithelial
cells. The current study demonstrated that OPN strongly
advanced the migration and adhesion of epithelial cells with OPN
upregulation, similar effects are evidently inhibited by OPN
downregulation, and the cell viability and proliferation were not
affected by OPN expression.
Therefore, OPN is a key factor for promoting closure
of healing wounds and improving cell adhesion in deep layers of
skin.
Glossary
Abbreviations
Abbreviations:
|
OPN
|
osteopontin
|
|
FAK
|
focal adhesion kinase
|
References
|
1
|
Sen CK: Wound healing essentials: Let
there be oxygen. Wound Repair Regen. 17:1–18. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lee MY and Ehrlich HP: Influence of
vanadate on migrating fibroblast orientation within a fibrin
matrix. J Cell Physiol. 217:72–76. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Miyazaki K, Okada Y, Yamanaka O, Kitano A,
Ikeda K, Kon S, Uede T, Rittling SR, Denhardt DT, Kao WW and Saika
S: Corneal wound healing in an osteopontin-deficient mouse. Invest
Ophthalmol Vis Sci. 49:1367–1375. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hunter C, Bond J, Kuo PC, Selim MA and
Levinson H: The role of osteopontin and osteopontin aptamer
(OPN-R3) in fibroblast activity. J Surg Res. 176:348–358. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
McKee MD, Pedraza CE and Kaartinen MT:
Osteopontin and wound healing in bone. Cells Tissues Organs.
194:313–319. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Miragliotta V, Pirone A, Donadio E, Abramo
F, Ricciardi MP and Theoret CL: Osteopontin expression in healing
wounds of horses and in human keloids. Equine Vet J. 48:72–77.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
O'Regan A and Berman JS: Osteopontin: A
key cytokine in cell-mediated and granulomatous inflammation. Int J
Exp Pathol. 81:373–390. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Buback F, Renkl AC, Schulz G and Weiss JM:
Osteopontin and the skin: Multiple emerging roles in cutaneous
biology and pathology. Exp Dermatol. 18:750–759. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mi Z, Guo H, Russell MB, Liu Y, Sullenger
BA and Kuo PC: RNA aptamer blockade of osteopontin inhibits growth
and metastasis of MDA-MB231 breast cancer cells. Mol Ther.
17:153–161. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Denhardt DT, Noda M, O'Regan AW, Pavlin D
and Berman JS: Osteopontin as a means to cope with environmental
insults: Regulation of inflammation, tissue remodeling, and cell
survival. J Clin Invest. 107:1055–1061. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pardo A, Gibson K, Cisneros J, Richards
TJ, Yang Y, Becerril C, Yousem S, Herrera I, Ruiz V, Selman M and
Kaminski N: Up-regulation and profibrotic role of osteopontin in
human idiopathic pulmonary fibrosis. PLoS Med. 2:e2512005.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Persy VP, Verhulst A, Ysebaert DK, De
Greef KE and De Broe ME: Reduced postischemic macrophage
infiltration and interstitial fibrosis in osteopontin knockout
mice. Kidney Int. 63:543–553. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Liaw L, Birk DE, Ballas CB, Whitsitt JS,
Davidson JM and Hogan BL: Altered wound healing in mice lacking a
functional osteopontin gene (spp1). J Clin Invest. 101:1468–1478.
1998. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen YY, Chen G, Fan Z, Luo J and Ke ZJ:
GSK3beta and endoplasmic reticulum stress mediate rotenone-induced
death of SK-N-MC neuroblastoma cells. Biochem Pharmacol.
76:128–138. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yang G, Meng Y, Li W, Yong Y, Fan Z, Ding
H, Wei Y, Luo J and Ke ZJ: Neuronal MCP-1 mediates microglia
recruitment and neurodegeneration induced by the mild impairment of
oxidative metabolism. Brain Pathol. 21:279–297. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ke ZJ, DeGiorgio LA, Volpe BT and Gibson
GE: Reversal of thiamine deficiency-induced neurodegeneration. J
Neuropathol Exp Neurol. 62:195–207. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Leitner L, Jürets A, Itariu BK, Keck M,
Prager G, Langer F, Grablowitz V, Zeyda M and Stulnig TM:
Osteopontin promotes aromatase expression and estradiol production
in human adipocytes. Breast Cancer Res Treat. 154:63–69. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
El-Tanani MK, Campbell FC, Kurisetty V,
Jin D, McCann M and Rudland PS: The regulation and role of
osteopontin in malignant transformation and cancer. Cytokine Growth
Factor Rev. 17:463–474. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shinohara ML, Lu L, Bu J, Werneck MB,
Kobayashi KS, Glimcher LH and Cantor H: Osteopontin expression is
essential for interferon-alpha production by plasmacytoid dendritic
cells. Nat Immunol. 7:498–506. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sodek J, Ganss B and McKee MD:
Osteopontin. Crit Rev Oral Biol Med. 11:279–303. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Frisch SM, Vuori K, Ruoslahti E and
Chan-Hui PY: Control of adhesion-dependent cell survival by focal
adhesion kinase. J Cell Biol. 134:793–799. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Trueblood NA, Xie Z, Communal C, Sam F,
Ngoy S, Liaw L, Jenkins AW, Wang J, Sawyer DB, Bing OH, et al:
Exaggerated left ventricular dilation and reduced collagen
deposition after myocardial infarction in mice lacking osteopontin.
Circ Res. 88:1080–1087. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Matsui Y, Jia N, Okamoto H, Kon S, Onozuka
H, Akino M, Liu L, Morimoto J, Rittling SR, Denhardt D, et al: Role
of osteopontin in cardiac fibrosis and remodeling in angiotensin
II-induced cardiac hypertrophy. Hypertension. 43:1195–1201. 2004.
View Article : Google Scholar : PubMed/NCBI
|