Introduction
Prostate cancer (CaP) is a leading cause of cancer
mortality in western countries, and is mainly observed as
adenocarcinoma of epithelial cell-origin (1). Although CaP morbidity in China is low
compared with that in western countries, it is on the rise
(2). Early stage CaP requires
androgens for growth, and thus responds well to androgen
deprivation therapy (3). However,
following the remittent stage (18–24 months in average), androgen
dependent prostate cancer (ADPC) may become androgen-independent
prostate cancer (AIPC). There is currently no curative therapy
available for AIPC.
The mechanism underlying AIPC transformation is of
importance in the CaP field. The primary mechanisms for the
conversion of ADPC into AIPC are variations in gene expression,
signal pathway abnormity, dysregulation of proto-oncogenes, cancer
suppressor genes and growth factors (4,5). Thus far,
a number of relevant genes and signal pathways in CaP have been
described (6). However, due to the
extremely complex biological behavior of CaP, no theory has
clarified the pathogenic mechanism of AIPC (6,7).
Therefore, the identification of genes involved in the transition
from ADPD to AIPC is important to expand the current knowledge of
AIPC (7).
Signal regulatory protein (SIRP)-α is a
transmembrane regulatory protein originally identified in rat cells
through its association with cytoplasmic tyrosine phosphatase Src
homology region 2 domain-containing phosphatase (SHP-2). SHP-2 was
later shown to be highly conserved in other mammals, including
humans, mice, and cattle. The cytoplasmic region of SIRP-α contains
2 immunoreceptor tyrosine-based inhibitory motifs with 4 tyrosine
residues that are phosphorylated in response to a variety of growth
factors and ligand binding. This phosphorylation enables the
recruitment and activation of Src homology region 1
domain-containing phosphatase (SHP-1) and SHP-2, which in turn
dephosphorylate specific protein substrates involved in the
mediation of various physiological effects (8,9).
Previously, decreased SIRP-α expression levels have
been reported in various types of cancer, indicating its important
role in oncology (9,10). The present study identified that
SIRP-α expression tended to be lower in AIPC tissues compared with
paired ADPC tissues. The present study also established the human
prostate cancer LNCaP and LNCaP-A cell model to further explore the
regulatory mechanism of SIRP-α in CaP, and demonstrated that it
modulates CaP cell apoptosis and proliferation through the p38
mitogen activated protein kinase (MAPK)/nuclear factor
(NF)-κB/cyclooxygenase (COX)-2 pathway.
Materials and methods
Cell culture and transfection
LNCaP, PC-3 and C4-2 cells were purchased from
American Type Culture Collection (Manassas, VA, USA) and maintained
in RPMI 1640 medium (Gibco; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA) supplemented with 10% fetal bovine serum (FBS), 2
mM L-glutamine, and 25 mM
4-(2-hydroxylethyl)-1-piperazineethanesulphonic acid. The LNCaP-A
cell line, an androgen independent LNCaP variant, was maintained in
phenol-red free RPMI 1640 (Gibco; Thermo Fisher Scientific, Inc.)
supplemented with 10% charcoal stripped FBS, 300 mg/l L-glutamine,
2,000 mg/l glucose, and 2,000 mg/l NaHCO3. The normal
prostate PWR-1E and RWPE-1 cell lines were cultured in keratinocyte
serum free medium (Gibco; Thermo Fisher Scientific, Inc.).
pcDNA3.1-myc-COX-2 was purchased from Biogot Technology Co., Ltd.,
(Nanjing, China). Vector-based shRNAs containing the target
sequences 5′-AAGTGAAGGTGACTCAGCCTG-3′ and
5′-AATCAGTGTCTGTTGCTGCTG-3′ for SIRP-α were constructed using the
pSUPER-neo vector (OligoEngine, Seattle, WA, USA) according to the
manufacturer's protocol. COX-2 siRNA was obtained from Guangzhou
RiboBio Co., Ltd (Guangzhou, China) and sequence was as follows:
Forward, 5′-GCUGGGAAGCCUUCUCUAA-3′ and reverse,
5′-TCGACCCUUCGGAAGAGAUU-3′. The pcDNA3.1-SIRP-α plasmid was
constructed according to a previous study (11). The plasmid pcDNA3.1 was used as the
control vector. Transfections were performed using
Lipofectamine® 2000 (Invitrogen; Thermo Fisher
Scientific, Inc.).
Clinical samples
CaP tissues included in the present study were from
28 cases with adenocarcinoma of the prostate that were diagnosed by
2 pathologists at The People's Liberation Army 309th Hospital
(Beijing, China). Medical history, transrectal ultrasound, computed
tomography, magnetic resonance imaging and isotope scanning of the
skeleton were combined to determine the clinical staging. A total
of 12 patients who accepted radical prostatectomy did not exhibit
metastasis and maintained very low prostate specific antigen (PSA)
levels (<0.2 ng/ml) with no relapse. They were considered as
androgen dependent prostate cancer (ADPC) patients according to
previous studies (2). AIPC were
defined as following: 1, serum testosterone <50 ng/ml; 2, high
PSA level (as measured 3 times, every 2 weeks); 3, anti-androgen
treatment failure. A total of 16 AIPC patients were used in the
present study. The study was approved by the ethics committee of
The People's Liberation Army 309th Hospital. Written informed
consent was gained prior to the start of the study.
Cell viability assays
The MTT assay was used in the present study to
quantify cell viability. Medium without cells served as a negative
control for this experiment. Cells were incubated in 96-well
culture plates (5×103 cells per well) at 37°C for 72 h.
50 µl MTT solution was added to each well and incubated at 37°C for
a further 4 h. Following incubation, MTT was aspirated and 150 µl
of dimethyl sulfoxide was added to each well to dissolve the
formazan precipitate. Subsequently, an ELISA plate reader was used
to obtain absorbance values at 570 nm.
Cell apoptosis assay
An Annexin V-Fluos staining kit (cat. no.
11988549001; Roche Applied Science, Penzberg, Germany) was used to
assess early apoptosis, as represented by a phosphatidylinositol
flip to the outer membrane. Cells were washed with PBS and stained
with Annexin V and propidium iodide according to the manufacturer's
protocol. Subsequently, slides were mounted with the Permafluor
mounting medium (Immunotech; Beckman Coulter, Inc., Brea, CA, USA)
and viewed under a fluorescence microscope (Axiophot, Olympus
Corporation, Tokyo, Japan).
Cell cycle analysis
CaP cells were synchronized in G0 by serum
starvation for 3 days followed by stimulation in DMEM supplemented
with 10% FBS. Progression through the cell cycle was monitored by
detection of the DNA content as previously described (12).
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was extracted from cells using TRIzol
reagent (Invitrogen; Thermo Fisher Scientific, Inc.) according to
the manufacturer's protocol. Medium without cells served as a
negative control for this experiment. Subsequently, RT-qPCR was
carried out with the PrimeScript RT-PCR kit (Takara, Bio, Inc.,
Shiga, Japan), using β-actin as an internal control, in the
Eppendorf Realplex4 machine (cat. no. X222687G; Hamburg, Germany).
The sequences of primers used for SIRP-α and β-actin were as
previously described (11). Reverse
transcription reactions were performed using the following
parameters: 16°C for 30 min, 42°C for 30 min and 84°C for 5 min.
The 2−∆∆Cq method was used for normalization (13). All experiments were repeated three
times.
Western blotting
SIRP-α (cat. no. 13379) and GAPDH (cat. no. 2118)
antibodies were purchased from Cell Signaling Technology, Inc.
(Danvers, MA, USA). A COX-2 antibody (cat. no. sc-7951) was
purchased from Santa Cruz Biotechnology, Inc. (Dallas, TX, USA);
Bcl-2 (cat no. ab694) and Bcl-2 associated × (Bax; cat. no.
ab32503) antibodies were purchased from Abcam (Cambridge, UK).
Anti-rabbit (cat. no. sc-2054) and anti-mouse (cat. no. sc-358914)
secondary antibodies were purchased from Santa Cruz Biotechnology,
Inc.
Cells were washed with ice-cold PBS and lysed with
protein lysis buffer (Pierce; Thermo Fisher Scientific, Inc.).
Subsequent to centrifugation at 5,000 × g for 15 min at 4°C,
the protein concentration was measured with a bicinchoninic acid
protein assay kit (Pierce; Thermo Fisher Scientific, Inc.). A total
of 50 µg aliquots of lysates were separated by 10% SDS-PAGE and
transferred onto a polyvinylidene difluoride membrane. The
membranes were blocked with 5% dried skimmed milk in Tris-buffered
saline (pH 7.4) containing 0.05% Tween 20, and sequentially
incubated with primary (dilution, 1:200) and horseradish
peroxidase-conjugated secondary (dilution, 1:5,000) antibodies,
according to the manufacturers' protocols. The proteins of interest
were visualized using an enhanced chemiluminescence western
blotting substrate (Pierce; Thermo Fisher Scientific, Inc.) and the
Chemidoc XRS Gel Documentation System (Bio-Rad Laboratories, Inc.,
Hercules, CA, USA).
Cytokine assay
ELISA kits for tumor necrosis factor α (TNFα; cat.
no. MTA00B), interleukin (IL)-6 (cat no. HS600B), nitric oxide
(cat. no. KGE001), CC chemokine ligand (CCL) 2 (cat. no. DCP00),
CCL5 (cat. no. DRN00B) and chemokine (C-X-C motif) ligand 2 (CXCL2;
cat. no. DY995) were purchased from R&D Systems, Inc.
(Minneapolis, MN, USA). Cytokine levels in culture supernatant or
sera were determined using the ELISA kits, according to the
manufacturer's protocols.
Signal inhibitors
NF-κB (BAY-117082; cat. no. EY1330), p38 MAPK
(SB203580; cat. no. EY0411), ERK1/2 (U0126; cat. no. EY1161) and
JNK (SP600125; cat. no. EY0021) inhibitors were purchased from
Amquar Biological Technology Co., Ltd. (Shanghai, China). The LNCaP
cells were incubated in 6-well plates (106 cells/well).
The inhibitors BAY-117082 (20 µM), SB203580 (20 µM), U0126 (10 µM)
and SP600125 (20 µM) were added to the appropriate well and
incubated at 37°C for 45 min. The cells were subsequently incubated
at 37°C for 24 h prior to being harvested.
Statistical analyses
Data are represented as the mean ± standard
deviation from ≥3 separate experiments performed in triplicate. The
differences between groups were determined using two-tailed
Student's t-test with SPSS 16.0 software (SPSS, Inc., Chicago, IL,
USA). The differences of ELISA data between groups were determined
using analysis of variance. P<0.05 was considered to indicate a
statistically significant difference. The χ2 test or
Fisher's exact test was used to analyze the association between
SIRP-α expression and clinicopathological features.
Results
SIRP-α expression is decreased in CaP
tissues
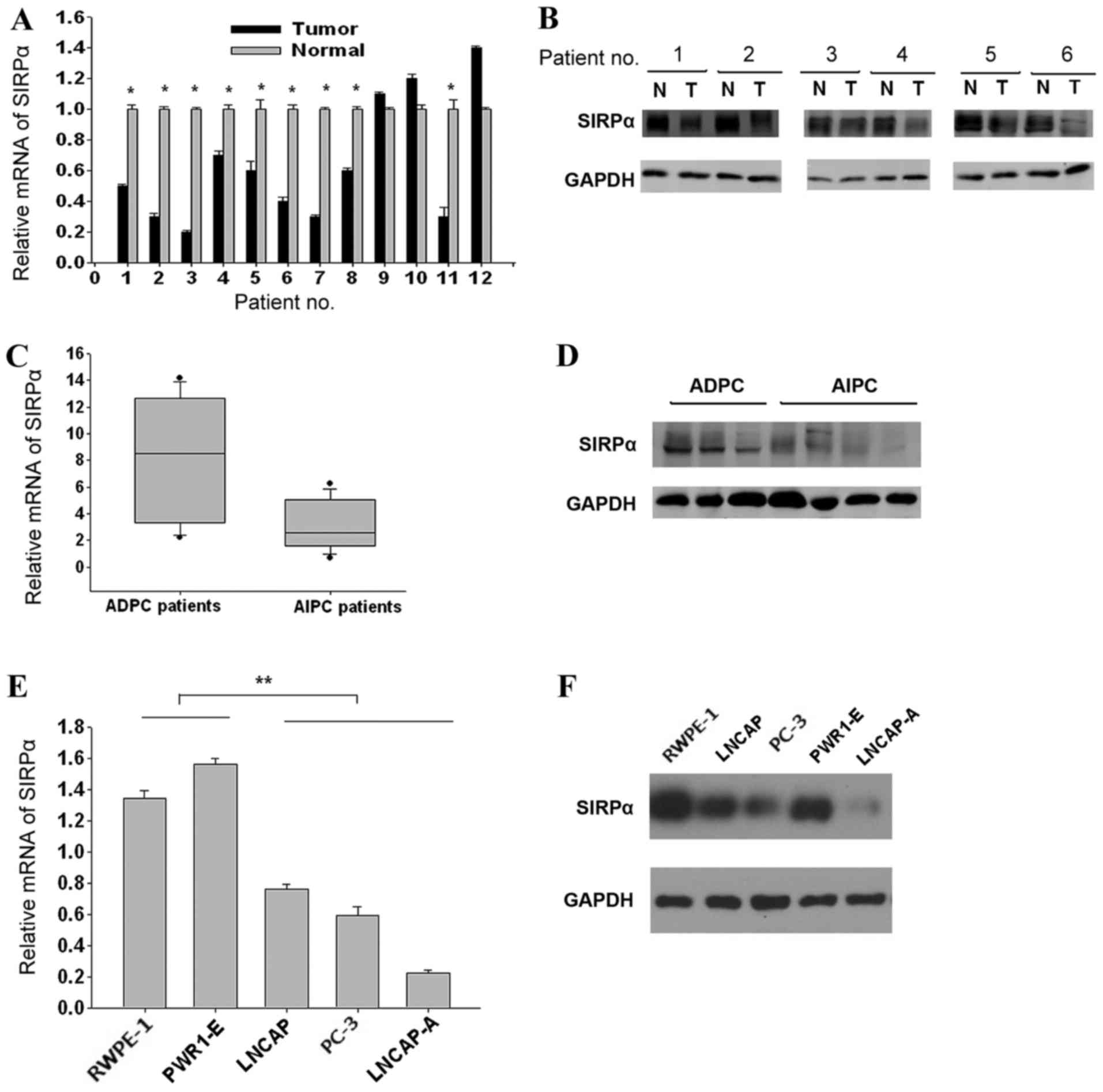
PCR results demonstrated that 9/12 (75%) CaP samples
showed lower SIRP-α levels compared with matched normal tissues
(Fig. 1A; P=0.044). Western blotting
data confirmed this SIRP-α expression trend in the same patient
groups (Fig. 1B, data of 6 patients
are shown; P=0.042). The SIRP-α expression levels between the AIPC
and ADPC groups were compared; it was revealed that they were
significantly lower in AIPC samples compared with the ADPC groups
(RT-qPCR, Fig. 1C, P=0.026; western
blotting, Fig. 1D, P=0.031). To
confirm these findings, SIRP-α expression levels were assessed in 3
prostate cancer LNCaP, LNCaP-A, and PC3 cell lines along with the 2
normal prostate epithelial RWPE-1 and PWR-1E cell lines. The
expression of SIRP-α was lowest in LNCaP-A cells, followed by PC3
and LNCaP, whereas RWPE-1 and PWR-1E showed higher SIRP-α
expression levels (RT-qPCR, Fig. 1E,
P=0.006; western blotting, Fig. 1F,
P=0.008). The data indicated that SIRP-α expression was decreased
in CaP tissues and cell lines, with AIPC showing lower SIRP-α
expression compared with ADPC.
SIRP-α negatively regulates CaP cell
proliferation by enhancing cell apoptosis
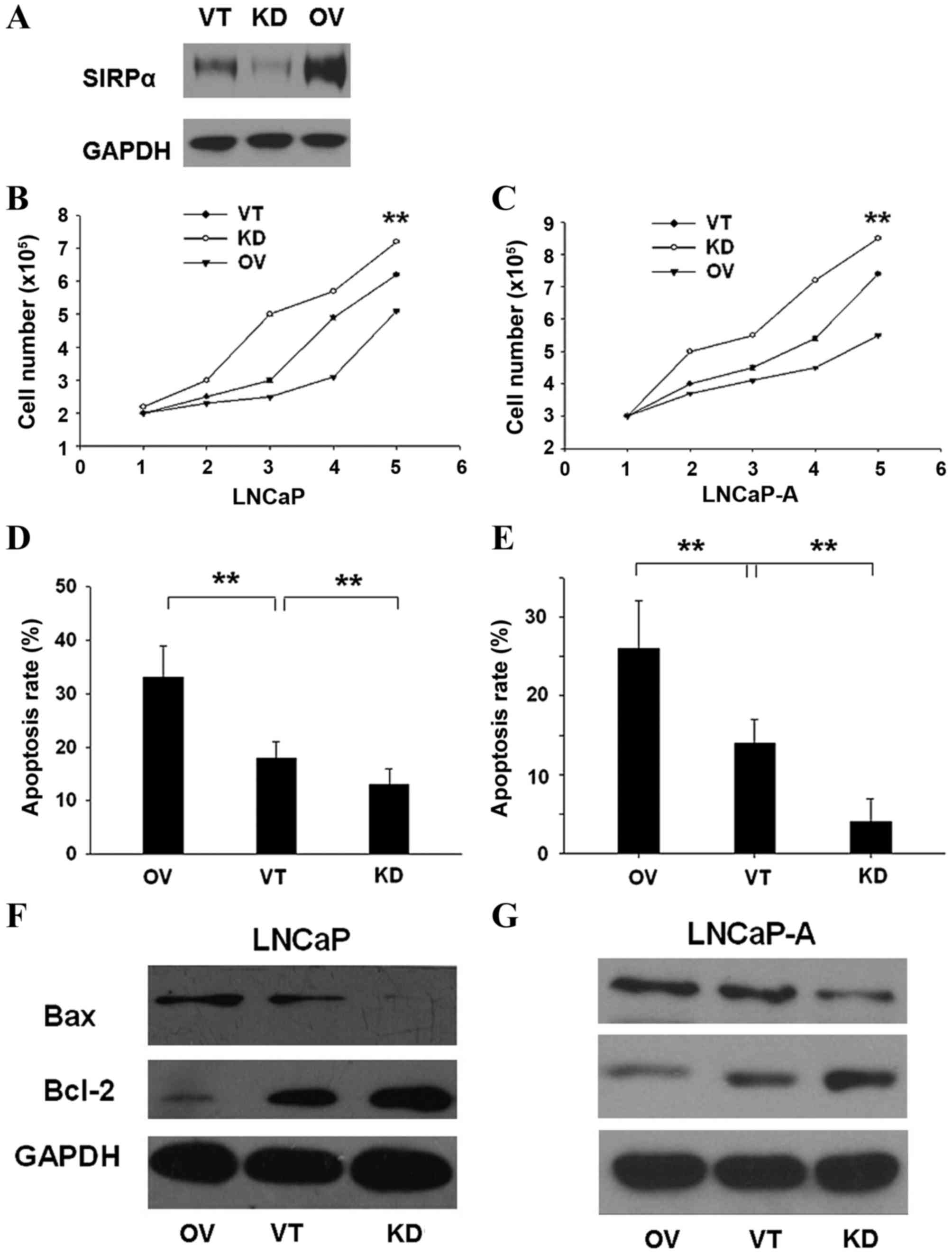
To investigate the biological function of SIRP-α in
CaP cell lines, SIRP-α was overexpressed by transfecting
pcDNA3.1-SIRP-α (OV), and suppressed by shRNA-SIRP-α (KD) in 2 cell
lines: LNCaP and LNCaP-A. Control vector (VT) transfection was also
performed (Fig. 2A). As shown in
Fig. 2B, OV transfection of LNCaP
cells resulted in significantly reduced number of live cells,
whereas KD transfection increased CaP cellular viability (P=0.003).
The same trend was observed in LNCaP-A cells (Fig. 2C; P=0.005). Cell apoptosis rates were
determined using the Annexin V-Fluos staining kit. OV significantly
enhanced the apoptosis rate (Fig. 2D;
P=0.005), whereas KD had the opposite effect (Fig. 2E; P=0.004). Additionally, OV resulted
in overtly higher Bax (pro-apoptotic) and lower Bcl-2
(anti-apoptotic) mRNA and protein expression levels 24 h after
transfection (LNCaP cells, Fig. 2F,
P=0.004; LNCaP-A cells, Fig. 2G,
P=0.006).
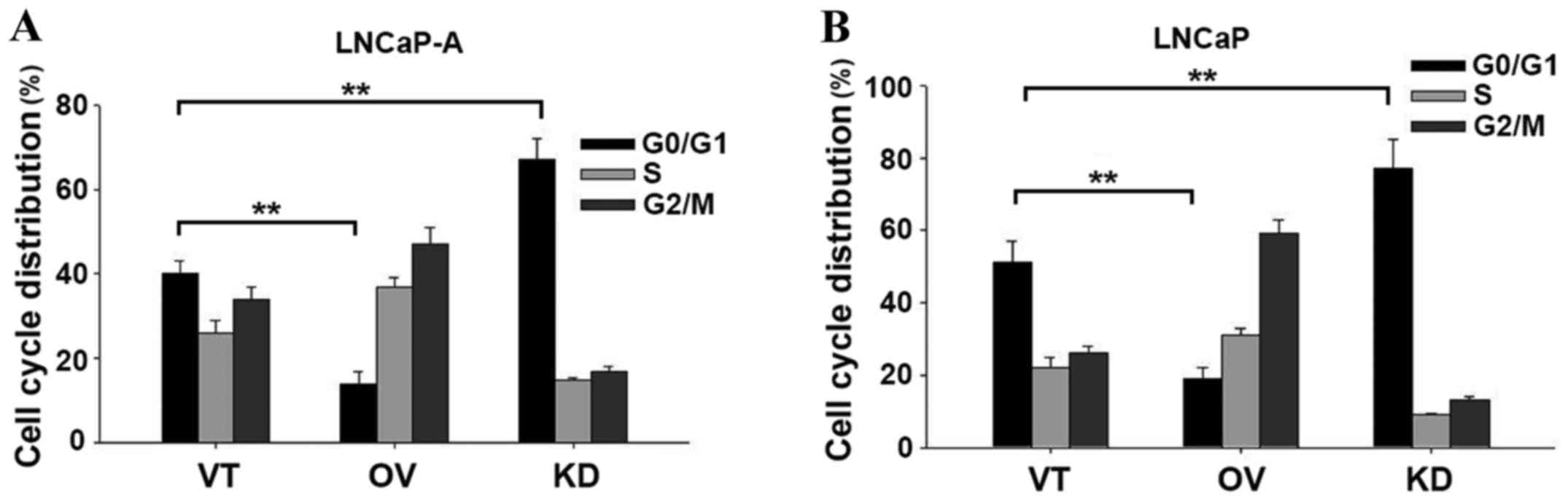
Based on the growth inhibitory effects of SIRP-α in
CaP cells, the present study then examined its effect on cell cycle
progression. As demonstrated in LNCaP-A cells in Fig. 3A (P=0.008) and LNCaP cells in Fig. 3B (P=0.006), downregulation of SIRP-α
increased the number of G0/G1 cell numbers. This data indicated an
important role for SIRP-α in apoptosis.
SIRP-α alters the production pattern
of various cytokines in CaP cells
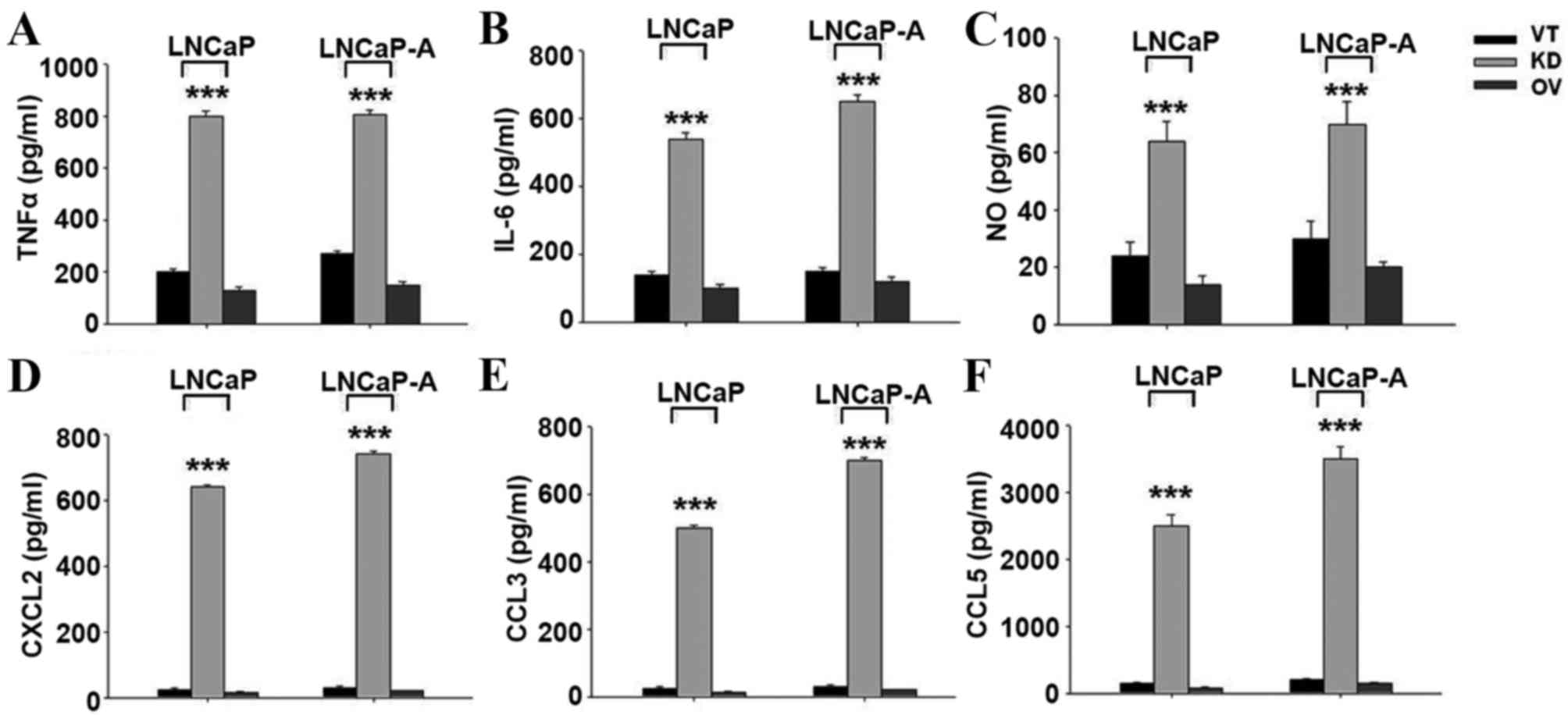
It is known that SIRP-α regulates the production of
various cytokines. In LNCaP and LNCaP-A cells, transfection with KD
produced significantly more TNFα (Fig.
4A), IL-6 (Fig. 4B), and nitric
oxide (Fig. 4C) compared with control
and SIRP-α overexpression groups (P<0.001). The chemoattractants
CXCL2 (Fig. 4D), CCL3 (Fig. 4E) and CCL5 (Fig. 4F) were also upregulated following
SIRP-α knockdown (P<0.001).
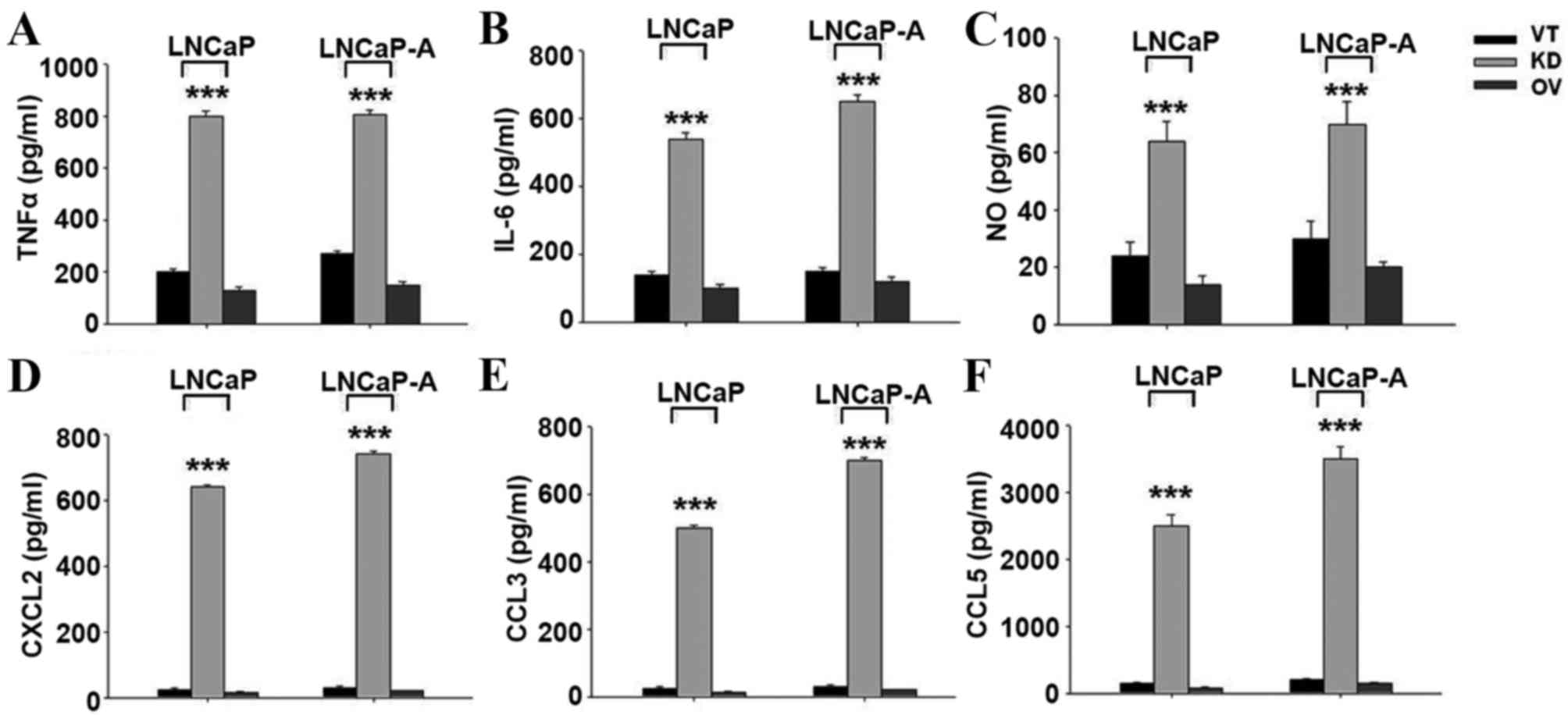 | Figure 4.Increased cytokine production of
SIRP-α knockdown in CaP cells. Cells were transfected with VT, KD
and OV, and cytokine production was determined using ELISA kits.
(A) TNFα, (B) IL-6, (C) NO, (D) CXCL2, (E) CCL3, (F) CCL5. SIRP,
signal regulatory protein; CaP, prostate cancer; VT, control
vector; KD, shRNA for SIRP-α; OV, pcDNA3.1-SIRP-α; TNF, tumor
necrosis factor; IL-6, interleukin-6; NO, nitric oxide; CXCL2,
chemokine (C-X-C motif) ligand 2; CCL, CC chemokine ligand. |
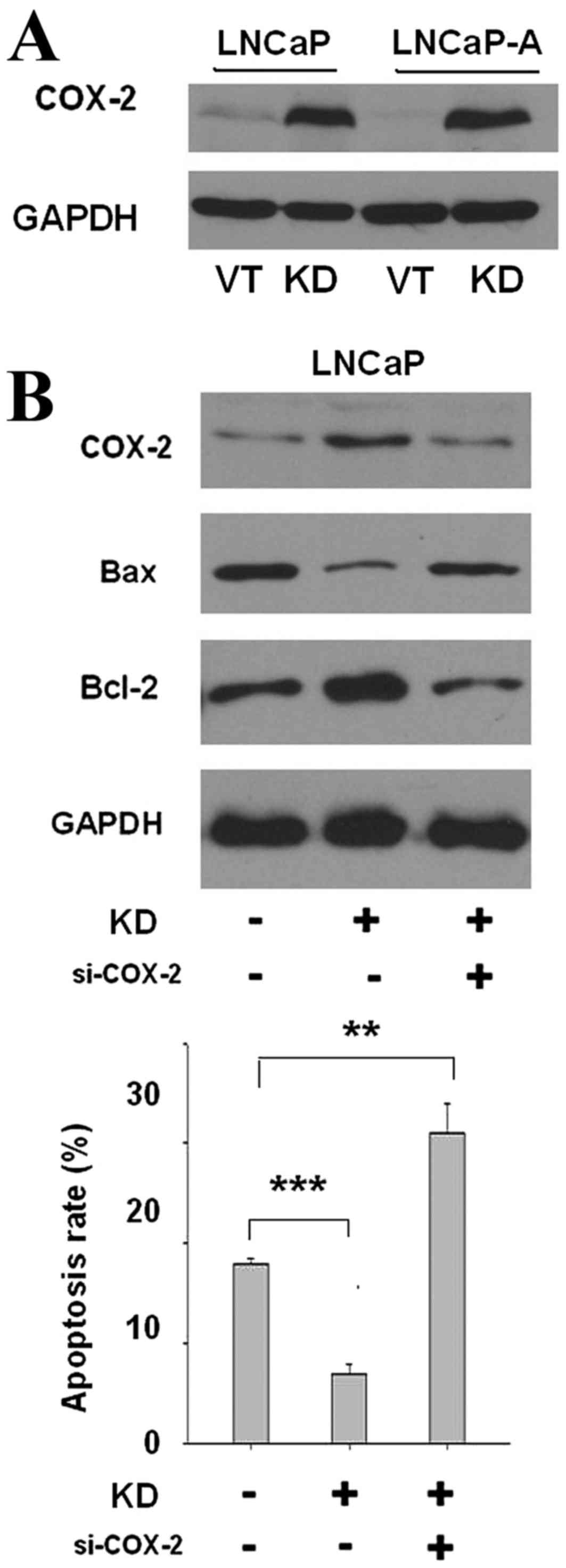
SIRP-α knockdown decreases cell
apoptosis by enhancing COX-2 expression
Using LNCaP and LNCaP-A cells as models, the present
study identified that SIRP-α silencing significantly upregulated
COX-2 expression (Fig. 5A,
P<0.001). Considering that COX-2 is positively associated with
cancer cell apoptosis, it was then explored whether silencing of
SIRP-α could suppress apoptosis by increasing COX-2 expression.
Cells were transiently co-transfected with COX-2 siRNA (si-COX-2)
and si-SIRP-α for 24 h. As shown in Fig.
5B, co-transfection of si-COX-2 blocked COX-2 expression
enhancement (P<0.001). Bax was also upregulated in the si-COX-2
group, and Bcl-2 was downregulated (P<0.001). The apoptosis rate
was sharply reduced in the si-SIRP-α group, and si-COX-2
co-transfection blocked this apoptosis inhibition (P=0.002). The
COX-2 independent inhibitor NS-398 did not downregulate COX-2
expression, but also caused elevated apoptosis rates (data not
shown). Taken together, these findings suggested that SIRP-α
knockdown decreased cell apoptosis by enhancing COX-2
expression.
SIRP-α decreases COX-2 expression and
cytokine production by negatively regulating p38 MAPK and
NF-κB
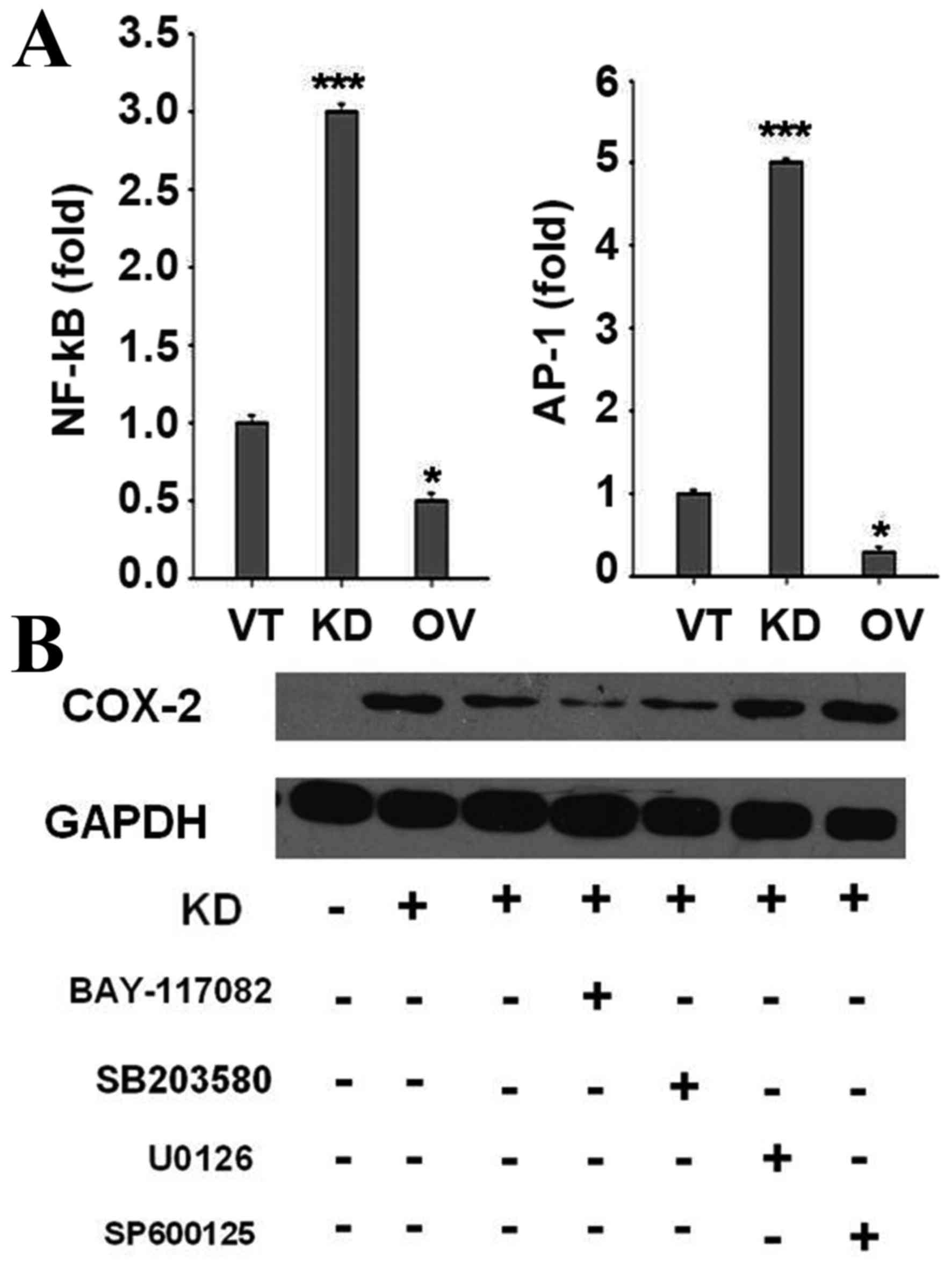
In the present study, NF-κB and AP-1, targets of
TLR-activated MAPKs and inhibitors of κB kinase, were enhanced by
SIRP-α knockdown, as assessed by a luciferase reporter assay
(Fig. 6A). LNCaP cells were
pre-treated with NF-κB, p38 MAPK, ERK1/2 or JNK inhibitors,
followed by SIRP-α knockdown. Notably, NF-κB and p38MAPK inhibitors
could block SIRP-α knockdown induced COX-2 expression (Fig. 6B, P<0.001), indicating that SIRP-α
decreased COX-2 expression by negatively regulating p38 MAPK and
NF-κB.
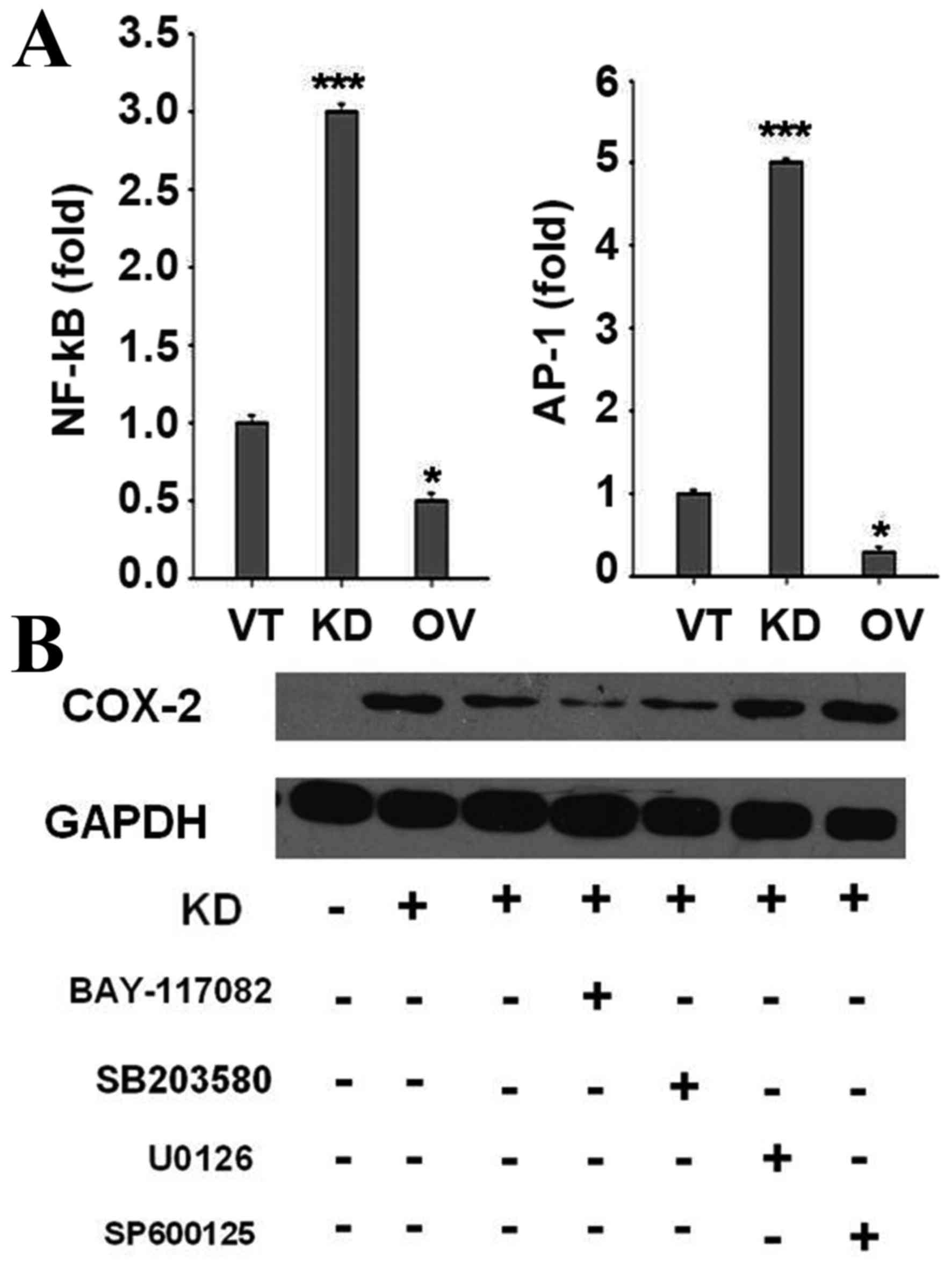 | Figure 6.SIRP-α decreases COX-2 expression and
cytokine production by negatively regulating p38 MAPK and NF-κB.
(A) Cells were transfected with VT, KD and OV, together with the
NF-κB or AP-1 reporter plasmids (0.2 µg), and the control plasmid
pRL-TK (0.02 µg), and then luciferase activities were detected. (B)
Cells were transfected with VT, KD, together with various key
protein inhibitors, and then the expression of COX-2 were
determined. SIRP, signal regulatory protein; COX-2,
cyclooxygenase-2; MAPK, mitogen activated protein kinase; NF,
nuclear factor; VT, control vector; KD, shRNA for SIRP-α; OV,
pcDNA3.1-SIRP-α; AP-, activator protein-; pRL-TK, thymidine kinase
promoter-Renilla luciferase reporter plasmid. |
Discussion
SIRP-α levels were shown to be decreased in human
CaP tissues. Specifically, SIRP-α expression was significantly
lower in the AIPC group compared with ADPC cases. The abnormity of
pro-apoptotic regulatory genes is considered a main factor in the
AIPC transformation mechanism. Previous studies have demonstrated
that polyinosinic-polycytidylic acid [poly (I:C)] induces apoptosis
in the ADPC cell line LNCaP in a TLR3-dependent manner, but not in
AIPC cell lines (14,15). Considering that suppression of SIRP-α
expression by RNA interference results in enhanced apoptosis
following poly (I:C) treatment (14),
it was deduced that SIRP-α may be involved in AIPC transformation
by regulating apoptosis.
SIRP-α has been shown to promote cell apoptosis in
liver cancer (10) and breast
carcinoma (9), but the molecular
mechanism remains unclear. The present study confirmed that SIRP-α
is involved in the regulation of cellular proliferation and
apoptosis in ADPC and AIPC cell lines. Notably, the present study
elucidated the negative regulatory effect of SIRP-α on COX-2 as the
main cause of apoptosis promotion. COX-2 is an oncogenic protein,
which is involved in numerous signaling pathways of apoptosis.
Inhibition of COX-2 leads to reduced proliferation and induction of
apoptosis, in connection with Bcl-2 downregulation and Bax
upregulation (16). It has been
previously demonstrated that COX-2 inhibits apoptosis in cancer
cells by inducing a P53 mutation (17). Other studies indicated that COX-2
weakens the apoptotic signal mediated by the Fas protein (18,19). The
above findings indicate that COX-2 is a negative regulator of
apoptosis. In the present study, apoptosis was sharply reduced in
the si-SIRP-α group, and co-transfection with si-COX-2 could block
this apoptosis reduction, suggesting that SIRP-α regulated cell
apoptosis was dependent on COX-2.
A number of past studies have demonstrated that
chemokines, including CXCL2, CCL2, CCL3, and CCL5, are produced at
the tumor site by CaP cells that also express their receptors, as
well as the supporting tissues. These chemokines are likely to
promote tumor development and angiogenesis (20,21). As
demonstrated in the present study, CXCL2, CCL2 and CCL5 are overtly
upregulated by SIRP-α knockdown. Lu et al (21) showed in 2006 that CCL2 expression
correlates with pathology in human CaP. In addition, Izhak et
al (20) demonstrated that
effective neutralization of CCL2 could slow tumor development.
Therefore, the present results provide another possible pathway for
tumor inhibition by SIRP-α.
Previous studies have shown that all 3 JNK, ERK, and
p38MAPK pathways can regulate COX-2 and cytokine expression. The
present study, identified that JNK and ERK were upregulated along
with p38MAPK and NF-κB, however, only p38MAPK and NF-κB inhibitors
blocked COX-2 and cytokine expression change, indicating that
SIRP-α affects CaP mainly through the p38MAPK/NF-κB pathway.
In conclusion, this is, to the best of our
knowledge, the first study assessing the role of SIRP-α in CaP.
SIRP-α may function as a novel negative regulator to modulate
cellular proliferation, survival and migration in CaP cells. The
heightened sensitivity of cells restoring SIRP-α function could be
exploited in the development of therapeutics that may potentiate
the antineoplastic effects of conventional cytokines or
chemotherapeutic agents.
Acknowledgements
The present study was supported by the China
Postdoctoral Science Foundation (grant no. 2015M572724) and the
People's Liberation Army 309th Foundation (grant no.
2013MS-021).
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2017. CA Cancer J Clin. 67:7–30. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ren SC, Chen R and Sun YH: Prostate cancer
research in China. Asian J Androl. 15:350–353. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sooriakumaran P, Nyberg T, Akre O,
Haendler L, Heus I, Olsson M, Carlsson S, Roobol MJ, Steineck G and
Wiklund P: Comparative effectiveness of radical prostatectomy and
radiotherapy in prostate cancer: Observational study of mortality
outcomes. BMJ. 348:g15022014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kahn B, Collazo J and Kyprianou N:
Androgen receptor as a driver of therapeutic resistance in advanced
prostate cancer. Int J Biol Sci. 10:588–595. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shi X, Gipp J, Dries M and Bushman W:
Prostate progenitor cells proliferate in response to castration.
Stem Cell Res. 13:154–163. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ianni M, Porcellini E, Carbone I,
Potenzoni M, Pieri AM, Pastizzaro CD, Benecchi L and Licastro F:
Genetic factors regulating inflammation and DNA methylation
associated with prostate cancer. Prostate Cancer Prostatic Dis.
16:56–61. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liu JB, Dai CM, Su XY, Cao L, Qin R and
Kong QB: Gene microarray assessment of multiple genes and signal
pathways involved in androgen-dependent prostate cancer becoming
androgen independent. Asian Pac J Cancer Prev. 15:9791–9795. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Barclay AN and Brown MH: The SIRP family
of receptors and immune regulation. Nat Rev Immunol. 6:457–464.
2006. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hara K, Senga T, Biswas MH, Hasegawa H,
Ito S, Hyodo T, Hirooka Y, Niwa Y, Goto H and Hamaguchi M: Recovery
of anoikis in Src-transformed cells and human breast carcinoma
cells by restoration of the SIRP α1/SHP-2 signaling system. Cancer
Res. 71:1229–1234. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yan HX, Wang HY, Zhang R, Chen L, Li BA,
Liu SQ, Cao HF, Qiu XH, Shan YF, Yan ZH, et al: Negative regulation
of hepatocellular carcinoma cell growth by signal regulatory
protein alpha1. Hepatology. 40:618–628. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kong XN, Yan HX, Chen L, Dong LW, Yang W,
Liu Q, Yu LX, Huang DD, Liu SQ, Liu H, et al: LPS-induced
down-regulation of signal regulatory protein {alpha} contributes to
innate immune activation in macrophages. J Exp Med. 204:2719–2731.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hinz M, Krappmann D, Eichten A, Heder A,
Scheidereit C and Strauss M: NF-kappaB function in growth control:
Regulation of cyclin D1 expression and G0/G1-to-S-phase transition.
Mol Cell Biol. 19:2690–2698. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Palchetti S, Starace D, de Cesaris P,
Filippini A, Ziparo E and Riccioli A: Transfected poly((I:C))
activates different dsRNA receptors, leading to apoptosis or
immunoadjuvant response in androgen-independent prostate cancer
cells. J Biol Chem. 290:5470–5483. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Paone A, Starace D, Galli R, Padula F, de
Cesaris P, Filippini A, Ziparo E and Riccioli A: Toll-like receptor
3 triggers apoptosis of human prostate cancer cells through a
PKC-alpha-dependent mechanism. Carcinogenesis. 29:1334–1342. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sun WH, Zhu F, Chen GS, Su H, Luo C, Zhao
QS, Zhang Y, Shao Y, Sun J, Zhou SM, et al: Blockade of
cholecystokinin-2 receptor and cyclooxygenase-2 synergistically
induces cell apoptosis, and inhibits the proliferation of human
gastric cancer cells in vitro. Cancer Lett. 263:302–311. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Han JA, Kim JI, Ongusaha PP, Hwang DH,
Ballou LR, Mahale A, Aaronson SA and Lee SW: P53-mediated induction
of Cox-2 counteracts p53- or genotoxic stress-induced apoptosis.
EMBO J. 21:5635–5644. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Casado M, Mollá B, Roy R,
Fernández-Martinez A, Cucarella C, Mayoral R, Boscá L and
Martin-Sanz P: Protection against Fas-induced liver apoptosis in
transgenic mice expressing cyclooxygenase 2 in hepatocytes.
Hepatology. 45:631–638. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nzeako UC, Guicciardi ME, Yoon JH, Bronk
SF and Gores GJ: COX-2 inhibits Fas-mediated apoptosis in
cholangiocarcinoma cells. Hepatology. 35:552–559. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Izhak L, Wildbaum G, Weinberg U, Shaked Y,
Alami J, Dumont D, Friedman B, Stein A and Karin N: Predominant
expression of CCL2 at the tumor site of prostate cancer patients
directs a selective loss of immunological tolerance to CCL2 that
could be amplified in a beneficial manner. J Immunol.
184:1092–1101. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lu Y, Cai Z, Galson DL, Xiao G, Liu Y,
George DE, Melhem MF, Yao Z and Zhang J: Monocyte chemotactic
protein-1 (MCP-1) acts as a paracrine and autocrine factor for
prostate cancer growth and invasion. Prostate. 66:1311–1318. 2006.
View Article : Google Scholar : PubMed/NCBI
|