Introduction
Colorectal cancer (CRC) is one of the most common
malignant tumor types in humans. The annual incidence of CRC
worldwide is >1,000,000 cases, which is greater than the
incidence of all other cancer types, with the exception of lung and
breast cancer (1). In 2011, there
were 310,244 new cases of CRC in China, accounting for 9.2% of all
new cases of cancer; additionally, there were 149,722 mortalities
due to CRC in 2011, accounting for 7.09% of all cancer-associated
mortalities (2). Evidence indicates
that the incidence of CRC has increased each year between 1998 and
2007 and has continued to increase thereafter (3). It has long been recognized that the
development of CRC is associated with the accumulation of certain
genetic mutations, including components of the epidermal growth
factor receptor (EGFR) signaling pathway (4). Evidence has also suggested that
mutations in KRAS proto-oncogene GTPase (KRAS) and B-Raf
proto-oncogene serine/threonine kinase (BRAF) are associated
with a worse patient prognosis in CRC (5). Therefore, detection of EGFR,
KRAS and BRAF mutations is important in studies of
CRC.
The term ‘multiple primary cancers’ refers to cases
in which independent primary malignant tumors occur simultaneously
or successively in one or multiple organs in the same individual.
Based on cancer registry records from between 1986 and 1995 at the
Cancer Institute Hospital of The Japanese Foundation for Cancer
Research (Tokyo, Japan), Ueno et al (6) reported that among 24,498 patients with
tumors, 1,281 (5.2%) had multiple primary cancers, and out of 1,587
cases of CRC, there were 142 (8.9%) cases of multiple primary
cancer. Therefore, increasing the understanding of multiple primary
cancers and CRCs, and strengthening the screening of patients for
whom CRC is suspected is expected to greatly reduce the rate of
misdiagnosis and missed diagnosis, provide novel strategies for
treatment and thus improve the prognosis for CRC patients.
The purpose of the present study was to investigate
the pathogenesis of cases of multiple primary cancer that included
≥1 CRC (MPCC) and provide evidence to aid the prevention and
treatment of CRC, including in cases of MPCC.
Subjects and methods
Patients
A total of 1,311 patients who received surgical
treatment for CRC at the Third Xiangya Hospital of Central South
University (Changsha, China) between August 2007 and August 2014
were included in this study. Patient data was obtained from medical
records and is presented in Table I.
All patients had signed informed consent forms and the study
received approval from Xiangya Hospital Ethics Committee. A
subgroup of these patients was confirmed by pathological and/or
cytological examinations to have MPCC.
 | Table I.Clinical epidemiological
characteristics of 1,311 colorectal cancer patients following
surgery. |
Table I.
Clinical epidemiological
characteristics of 1,311 colorectal cancer patients following
surgery.
| Variable | n | % |
|---|
| Sex |
|
|
| Male | 761 | 58.00 |
|
Female | 550 | 42.00 |
| Age, years |
|
|
| ≤35 |
63 | 4.80 |
|
36–59 | 600 | 45.77 |
|
≥60 |
648 | 49.43 |
| Pathological
type |
|
|
| Tubular
adenocarcinoma | 1,143 | 86.98 |
|
Mucinous adenocarcinoma |
89 |
6.77 |
|
Signet-ring cell
carcinoma |
6 |
0.46 |
|
Other |
76 |
5.79 |
| Lesion site |
|
|
|
Rectum |
669 | 50.11 |
| Left
side of the colon |
278 | 20.83 |
| Right
side of the colon |
388 | 29.06 |
Group inclusion and exclusion
criteria
CRC group
Patients were required to have pathologically
confirmed CRC and to previously have received surgical treatment at
the Third Xiangya Hospital. Patients with metastatic or recurrent
cancers, and those whose cancers were not pathologically confirmed,
were excluded.
CRC with other cancer (CCOC) group
Patients were selected according to the modification
of diagnostic criteria from Warren and Gates (7) in combination with clinical observations:
i) The patient must have multiple primary cancers including ≥1 CRC
and ≥1 primary cancer at another location; ii) each primary tumor
must be pathologically confirmed to be malignant and have its own
specific pathological morphology; iii) the possibility of the
subsequent tumors having arisen from the first primary tumor via
recurrence or metastasis must be excluded.
Multiple CRCs (MCC) group
Patients were selected according to the diagnostic
criteria of Lee et al (8) in
combination with clinical observations: i) The patient must have ≥2
primary cancers in the colon/rectum, with no primary tumors at
other sites, and each tumor must be pathologically confirmed to be
malignant; ii) cancer foci must be independent of each other, with
a transitional zone composed of heterotypic cell glands between
tumor foci and the normal intestinal wall; iii) the possibility of
metastasis, recurrence and submucosal diffusion of the primary
cancer must be excluded; iv) there must be no recurrence of
previous surgical anastomotic stoma, and new foci must be clearly
distinct from previous surgical incisions; v) patients must not
have been diagnosed with familial adenoma or enteropathic
arthritis-induced cancer.
DNA isolation and mutation assessment
Hematoxylin and eosin staining was implemented to
confirm that specimens contained >80% cancer cells, and areas
enriched with malignant cells were identified prior to DNA
extraction by two independent pathologists. DNA was extracted from
formalin-fixed, paraffin-embedded tissue specimens using a QIAamp
DNA FFPE Tissue Kit (Qiagen, Hilden, Germany) according to the
manufacturer's instructions and stored at −80°C until use.
Mutation hotspots in EGFR (L858R and L861Q),
KRAS (G12V, G13D and Q61R) and BRAF (V600E) were
detected. Polymerase chain reaction (PCR) amplification was
performed as follows: 1 min of initial denaturation at 95°C; 35
cycles of amplification consisting of 30 sec at 94°C, 40 sec at
57°C and 30 sec at 72°C, with a final additional elongation at 72°C
for 7 min. Used primers are as follows: EGFR L858R/L861Q
forward primer, 5′-CCAGGAACGTACTGGTGAAA-3′; EGFR L858R/L861Q
reverse primer, 5′-TGACCTAAAGCCACCTCCTT-3′; KRAS12/13
forward primer, 5′-TATAAGGCCTGCTGAAAATGACTG-3′; KRAS12/13
reverse primer, 5′-TATTCGTCCACAAAATGATTCTGA-3′; KRAS61 forward
primer, 5′-AATTGATGGAGAAACCTGTCTCTT-3′; KRAS61 reverse primer,
5′-TCCTCATGTACTGGTCCCTCATT-3′; BRAF V600E forward primer,
5′-CTTCATAATGCTTGCTCTGATAGG-3′; BRAF V600E reverse primer,
5′-GCATCTCAGGGCCAAAAATT-3′. Non-template control was included in
each batch during the experiment, and sequencing was performed
using ABI 3500xL Genetic Analyzer (Applied Biosystems, Carlsbad,
CA, USA).
Statistical analysis
The medical records of the overall population of
patients with CRC and the subset of patients with MPCC were
analyzed using SPSS 13.0 software (SPSS Inc., Chicago, IL, USA).
Numerical data were analyzed with the χ2 test.
Measurement data are presented as the mean ± standard deviation.
The two-sample t-test was used for comparisons between groups.
P<0.05 was considered to indicate a statistically significant
difference.
Results
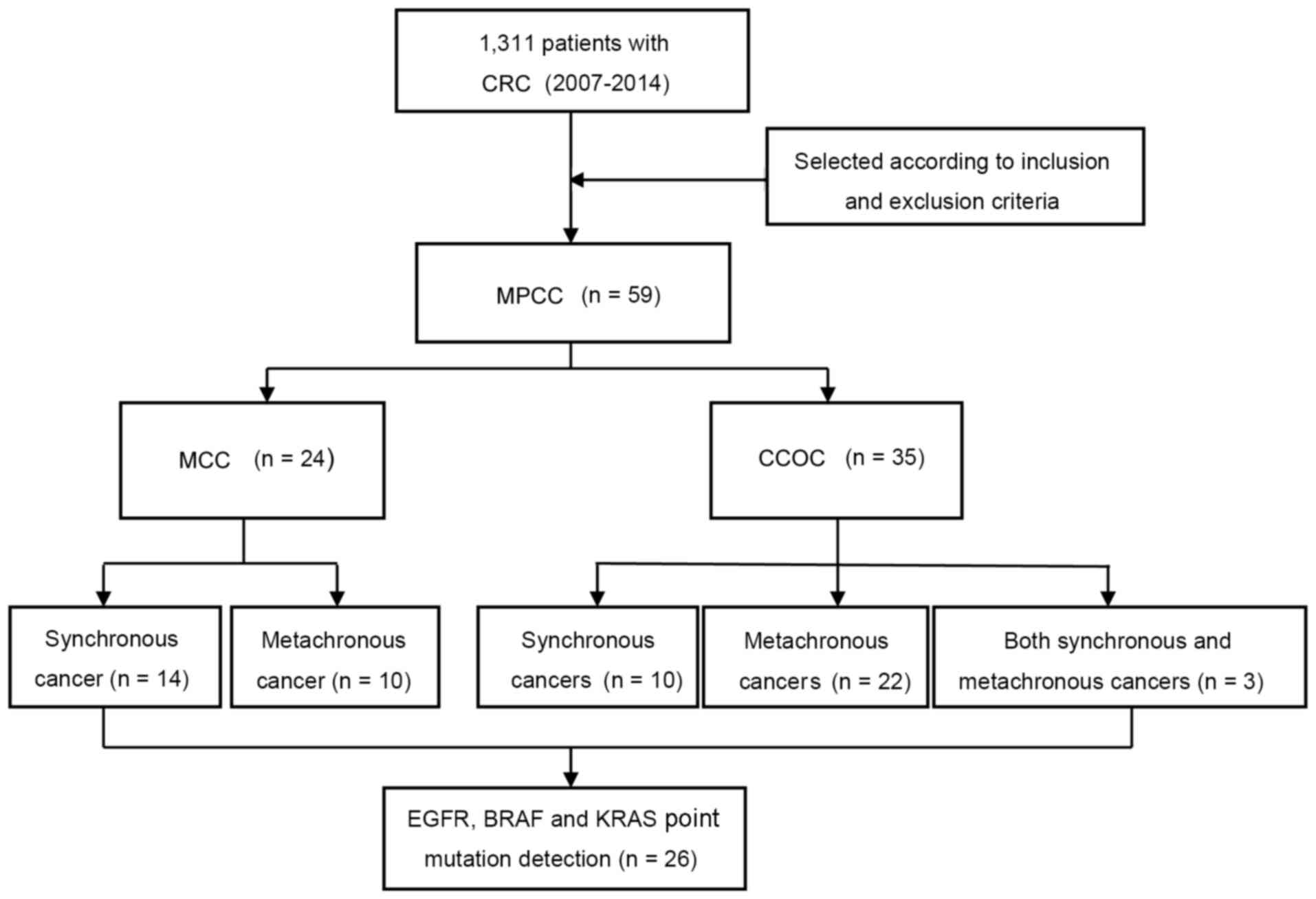
Patient selection
A flow diagram illustrating the selection of
patients in the study is presented in Fig. 1. A total of 1,311 patients underwent
surgery for CRC during the study period. Of these, 59 patients had
MPCC (including 35 with CCOC and 24 with MCC).
Clinical epidemiological
characteristics of CRC patients following surgery
The clinical epidemiological characteristics of the
1,311 patients who underwent CRC surgery are presented in Table I. The overall patient population
consisted of 761 males and 550 females (male:female ratio, 1.38:1),
with a mean age of 58.36±13.07 years (range, 20–91 years).
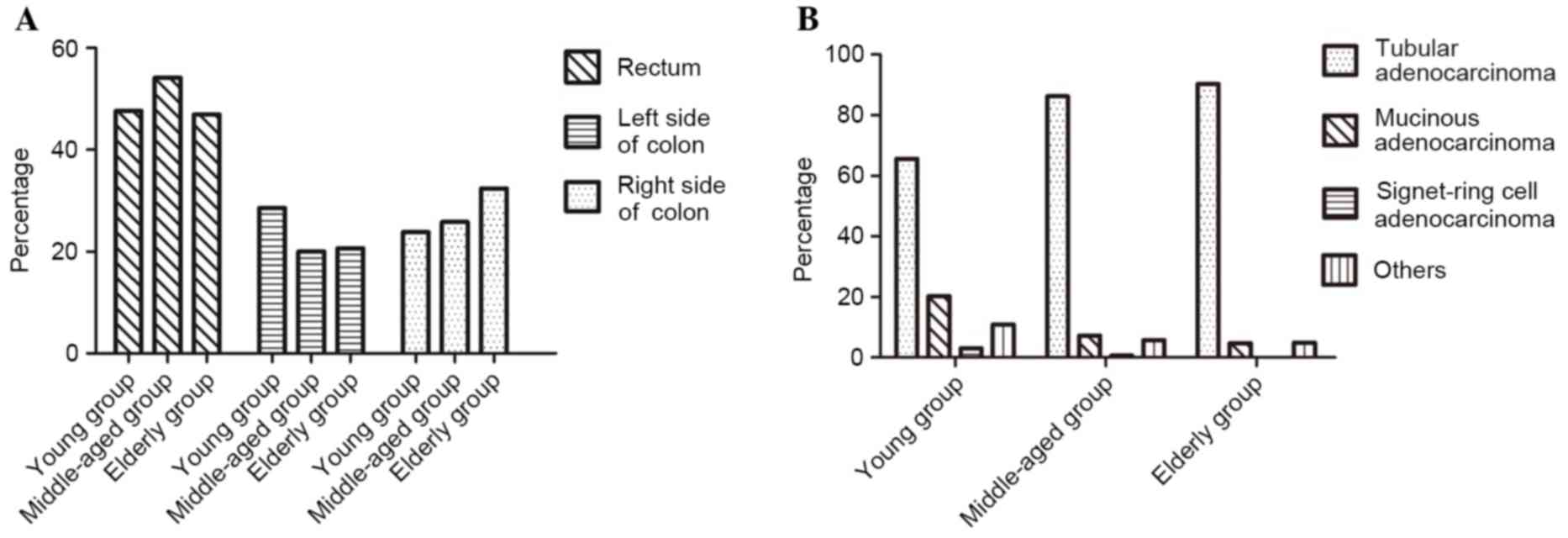
Patients were divided into three age groups: Young
(≤35 years), middle-aged (36–59 years), and elderly (≥60 years). In
the young group, 47.62% of patients had rectal cancer, 23.81% had
cancer of the right side of the colon, and 28.57% had cancer of the
left side of the colon. In the middle-aged group, 54.17% of
patients had rectal cancer, 20.00% had cancer of the left side of
the colon, and 25.83% had cancer of the right side of the colon. In
the elderly group, 46.91% of patients had rectal cancer, 20.68% had
cancer of the left side of the colon, and 32.41% had cancer of the
right side of the colon.
Among the total study population, 1,143 (86.98%)
patients had tubular adenocarcinoma, 89 (6.77%) had mucinous
adenocarcinoma, 6 (0.46%) had signet-ring cell cancer, and 76
(5.79%) had undifferentiated carcinoma or other cancer types. For
cases in which the tumors were of the same histological type, the
highest-level pathological diagnosis was included in the
statistics. Of the total 1,311 patients, 3 patients had different
pathological types between two CRC foci and therefore were
retrospectively included in the statistical analysis. A significant
difference in pathological type between age groups was identified
(P<0.05; Fig. 2).
Comparisons of age of onset, sex and
pathological types between patients with MPCC and CRC
There was a significant difference in the age of
onset between the 59 patients with MPCC and the 1,311 patients with
CRC (P<0.05); however, no significant difference was observed in
sex between them (P>0.05). Among the 1,311 patients with CRC,
318 (24.265%) had adenoma and 446 (34.02%) had polyp(s). By
comparison, 19 (30.20%) of the 59 patients with MPCC had adenoma
and 33 (55.93%) had polyps. There was no significant difference
between the CRC and MPCC cohorts with regard to the proportion of
patients with adenoma (P=0.166); however, a significant difference
was observed in the proportions of patients with polyp(s) (P=0.001;
Table II).
 | Table II.Comparison of 1,311 patients with CRC
and 59 patients with MPCC. |
Table II.
Comparison of 1,311 patients with CRC
and 59 patients with MPCC.
| Variable | MPCC | All CRC | P-value |
|---|
| Total, n | 59 | 1,311 | – |
| Age, years |
|
| 0.035 |
| Mean ±
SD | 62.11±11.74 | 58.36±13.07 |
|
|
Range | 40–81 | 20–91 |
|
| Sex |
|
| 0.747 |
|
Male | 33 | 761 |
|
|
Female | 26 | 550 |
|
| Complication |
|
|
|
|
Adenoma | 19 | 318 | 0.166 |
|
Polyp(s) | 33 | 446 | 0.001 |
Occurrence and clinical features of
patients with MPCC
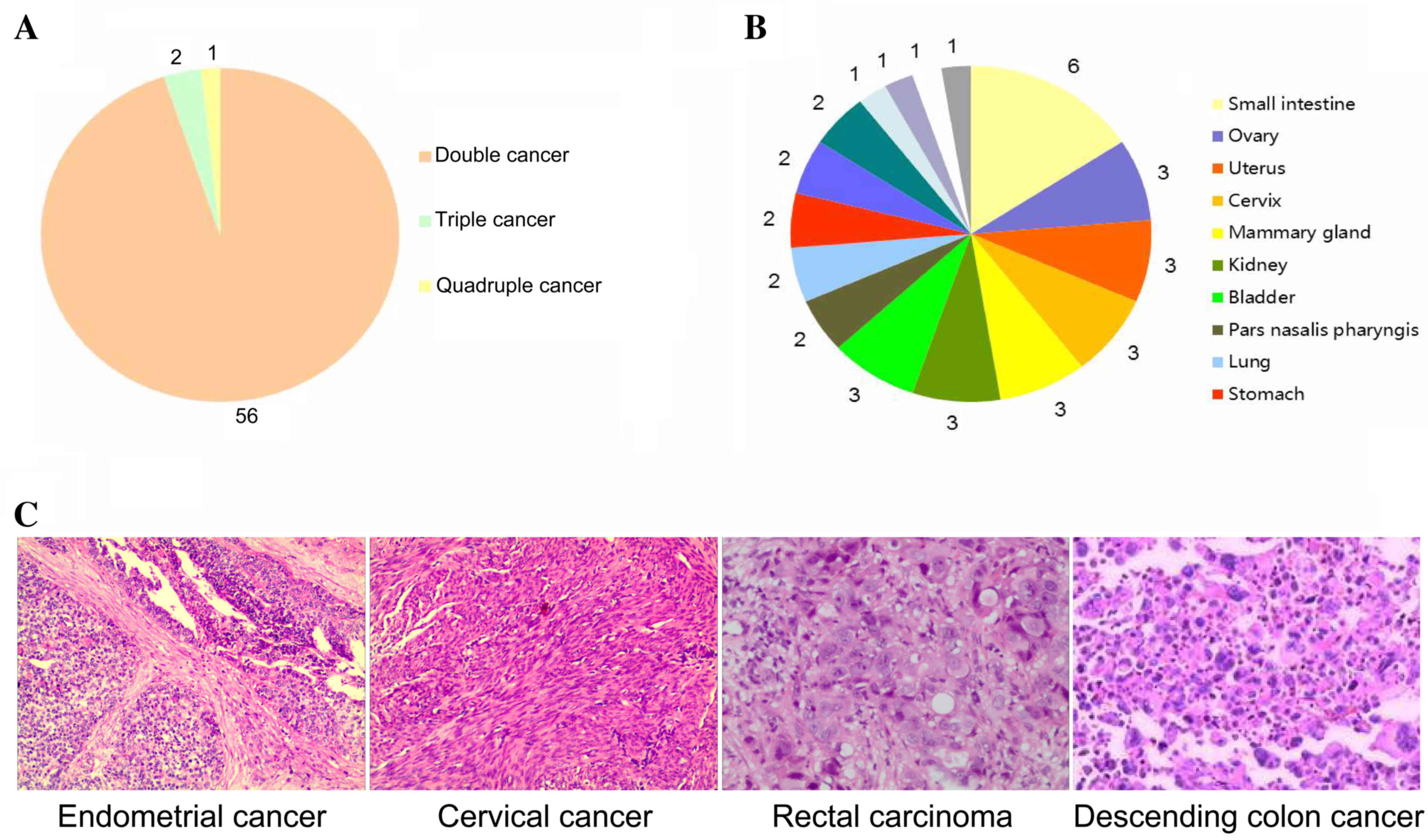
According to the inclusion criteria, 59 (4.50%)
patients, consisting of 33 (55.93%) males and 26 (44.07%) females
with a mean age of 62.11±11.74 years (range, 40–81 years) had MPCC.
Among these patients, 56 patients (94.92%) had double cancer, 2
(3.39%) had triple cancer, and 1 (1.69%) had quadruple cancer
(Fig. 3A).
There were 122 primary cancer foci
among the 59 patients with MPCC
These foci were located in the large intestine
[n=84; including the rectum (n=28), left side of the colon (n=24),
and right side of the colon (n=32)], small intestine (n=6), ovary
(n=3), uterus (n=3), cervix (n=3), mammary gland (n=3), kidney
(n=3), bladder (n=3), nasopharynx (n=2), lung (n=2), stomach (n=2),
ureter (n=2), prostate (n=2), esophagus (n=1), thyroid gland (n=1),
liver (n=1) and the left iliac fossa (n=1; Fig. 3B).
As well as the 59 pathologically confirmed primary
CRC foci (i.e. 1 per patient) included in the cohort, the 63
additional primary cancer foci were located in the digestive system
[n=35; including the large intestine (n=25), small intestine (n=6),
stomach (n=2), esophagus (n=1), and liver (n=1)], reproductive
system [n=14; including the mammary gland (n=3), ovary (n=3),
uterus (n=3), cervix (n=3), and prostate (n=2)], urinary system
[n=8; including the kidney (n=3), bladder (n=3), and ureter (n=2)],
respiratory system [n=4; including the nasopharynx (n=2), and lung
(n=2)], endocrine system (n=1) and hematological system (n=1).
Of the 59 patients with MPCC, 24 (1.83% of total CRC
cohort) patients had synchronous cancer, 32 (2.44% of total CRC
cohort) patients had metachronous cancer, and 3 (0.23% of total CRC
cohort) patients had both. There was 1 patient with quadruple
cancer, including both synchronous and metachronous cancers,
comprising 2 CRCs, 1 cervical cancer and 1 endometrial cancer
(Fig. 3C).
Among the 24 patients with synchronous cancer, 18
patients (75.00%) were diagnosed with a synchronous cancer
simultaneously with the diagnosis of CRC (before or during the CRC
surgery), and 2 patients were diagnosed with the second cancer ~1
month after surgery. A total of 6 patients (25.00%) in the
synchronous cancer group were misdiagnosed.
Among the 32 patients with metachronous cancer, the
mean disease onset interval (between two cancer diagnoses) was
49.25 months (range, 7 months to 20 years). For the 10 patients
with metachronous cancers in the MCC group, the mean disease onset
interval was 23.80 months (range, 7 months to 6 years). In the 22
patients with metachronous cancers in the CCOC group, the mean
disease onset interval was 60.86 months (range, 7 months to 20
years; Table III).
 | Table III.Intervals between onset of each
cancer in 32 patients with metachronous multiple primary cancers
including CRC. |
Table III.
Intervals between onset of each
cancer in 32 patients with metachronous multiple primary cancers
including CRC.
|
|
| Disease onset
interval, years |
|
|---|
|
|---|
| Group | Total, n | <1 | ≥1-<3 | ≥3-<5 | ≥5-<10 | ≥10 | Mean interval,
months |
|---|
| MCC | 10 | 5
(50) | 4
(40) | 0 (0) | 1 (10) | 0 (0) | 23.80 |
| CCOC | 22 | 5
(23) | 6
(27) | 4
(18) | 4 (18) | 3
(14) | 60.86 |
| Total | 32 | 10 (31) | 10 (31) | 4
(13) | 5 (16) | 3 (9) | 49.25 |
Detection of point mutations
The common CRC-associated point mutation loci of the
EGFR, KRAS and BRAF genes were analyzed in
available specimens from 26 patients with MPCC. Mutations of
KRAS G12V and in exon 21 of the EGFR gene (including
L858R and L861Q) were not detected. The incidence rates were 11.54%
for KRAS G13D, 3.85% for KRAS Q61R and 3.85% for
BRAF V600E (Table IV).
 | Table IV.Point mutations detected among 26
specimens from patients with multiple primary cancers including a
colorectal cancer. |
Table IV.
Point mutations detected among 26
specimens from patients with multiple primary cancers including a
colorectal cancer.
|
| Incidence of
mutation |
|---|
|
|---|
| Gene and mutation
locus | n | % |
|---|
| EGFR
L858R | 0 |
0.00 |
| EGFR
L861Q | 0 |
0.00 |
| KRAS
G12V | 0 |
0.00 |
| KRAS
G13D | 3 | 11.54 |
| KRAS
Q61R | 1 |
3.85 |
| BRAF
V600E | 1 |
3.85 |
Discussion
The incidence of CRC has increased in recent years,
and rectal cancers account for a larger proportion than colon
cancers (9). In the present study,
the lesions in middle-aged patients predominantly occurred in the
rectum, whereas, in elderly patients, lesions most commonly
occurred in the colon; cancer of the right side of the colon was
more common than the left side in elderly patients. These results
are consistent with previous reports (10,11).
Adenocarcinoma is the predominant type of CRC; with age, patients
possess an increasing risk of adenocarcinoma overall, whereas the
risk of signet-ring cell carcinoma or mucinous adenocarcinoma
decreases (12).
There is evidence that 17–19% of patients with new
tumors have previously experienced malignant tumors (13,14).
Multiple cancers of the head and neck are among the most
extensively studied of recent years (15,16). A
small number of studies have reported on multiple CRCs and other
multiple primary cancers. The results of the present study indicate
that the incidence of MPCC among CRC cases is 4.50%, which is
consistent with the incidence reported in a previous series of
studies (6,17–19). There
was a significant difference in the age of onset between the 59
patients with MPCC and the 1,311 patients with CRC (P<0.05). A
significant difference in the number of cases complicated by
polyp(s) was identified between the 59 patients with MPCC and the
overall population of 1,311 patients with CRC (P<0.05),
indicating that the occurrence of MPCC is associated with the
presence of polyp(s) (20,21).
Among the 59 patients with MPCC, the proportion of
males (n=33; 55.93%) was higher than that of females (n=26;
44.07%), which is similar to the incidence rates of single primary
CRC in males and females (22). Among
the patients with MPCC, the proportion with metachronous cancers
was greater than the proportion with synchronous cancers. Among
patients with MPCC, double cancer was the most common type, and
triple or greater multiples of cancers were rarely identified.
Metachronous cancers predominantly occurred within 1–3 years,
followed by within 5 years, after the diagnosis of CRC. In addition
to the 59 primary foci in the large intestine, the other primary
foci were mainly located in the digestive system, reproductive
system, urinary system and respiratory system. This is consistent
with the field cancerization theory (23); specifically, as the esophagus and
gastrointestinal tract are the passage through which food passes,
the lungs are the air channels, and the urinary system is the fluid
waste channel, all of these organs are particularly exposed to
carcinogens in food or air.
It is well known that the occurrence of cancer is
closely associated with the accumulation of gene mutations, and
patients with incipient cancer thus possess a high risk for
secondary cancer (24,25). In this study, common point mutation
loci of the EGFR, KRAS and BRAF genes in 26
specimens from patients with multiple cancers were analyzed. The
rates of incidence were 11.54% for KRAS G13D and 3.85% for
KRAS Q61R mutations, which were evidently lower than
previously reported rates of 30–60% (5,26,27). The incidence rate of BRAF V600E
mutation was 3.85%, which was also lower than previously reported
(12.44%) (26). There is evidence
that survival following surgery in patients who developed
metachronous MPCCs tended to be better than that of patients with a
single carcinoma (6). This suggests
that the mutation profile of MPCC is likely to be associated with
its prognosis. This hypothesis will be investigated further in a
larger study by this group.
The findings of the present study suggest that, for
patients with CRC, detailed medical records, physical examination
and associated auxiliary examinations are required, and
pathological examination of living tissue is necessary to determine
whether a new foci is a primary cancer, metastatic cancer or
recurrent cancer. Thus, treatment strategies can be developed with
the purpose of lengthening the patient's survival time and
improving their quality of life. Studies in patients with MPCC aid
the development of novel strategies for investigating the
occurrence and underlying mechanism of the development of this
disease, and identifying molecular targets for its treatment.
Acknowledgements
This study was supported by National Natural Science
Foundation of China (grant nos. 81301688, 81272192, 81572965); PhD
Programs Foundation of Ministry of Education of China (grant nos.
20130162110050 and 20130162120093); Natural Science Foundation of
Hunan Province (grant no. 2015JJ4053); Technology Project of Hunan
Province (grant no. 2012SK3229); Post-doctoral Foundation of
Central South University (grant no. 131425); 125 Talent Project/New
Xiangya Project of the Third Xiangya Hospital of Central South
University; the Fundamental Research Funds for the Central
Universities of Central South University (grant no.
2016zzts561).
Glossary
Abbreviations
Abbreviations:
|
CRC
|
colorectal cancer
|
|
MPCC
|
multiple primary cancers including ≥1
colorectal cancer
|
|
CCOC
|
colorectal cancer with other primary
cancer type
|
|
MCC
|
multiple CRCs and no other primary
cancer types
|
|
EGFR
|
epidermal growth factor receptor
|
|
KRAS
|
KRAS proto-oncogene GTPase
|
|
BRAF
|
B-Raf proto-oncogene serine/threonine
kinase
|
References
|
1
|
Ferlay J, Soerjomataram I, Dikshit R, Eser
S, Mathers C, Rebelo M, Parkin DM, Forman D and Bray F: Cancer
incidence and mortality worldwide: Sources, methods and major
patterns in GLOBOCAN 2012. Int J Cancer. 136:E359–E386. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen W, Zheng R, Zeng H, Zhang S and He J:
Annual report on status of cancer in China, 2011. Chin J Cancer
Res. 27:2–12. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dai Z, Zheng RS, Zou XN, Zhang SW, Zeng
HM, Li N and Chen WQ: Analysis and prediction of colorectal cancer
incidence trend in China. Zhonghua Yu Fang Yi Xue Za Zh.
46:598–603. 2012.(In Chinese).
|
|
4
|
Shen Y, Han X, Wang J, Wang S, Yang H, Lu
SH and Shi Y: Prognostic impact of mutation profiling in patients
with stage II and III colon cancer. Sci Rep. 6:243102016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kriegsmann M, Arens N, Endris V, Weichert
W and Kriegsmann J: Detection of KRAS NRAS and BRAF by mass
spectrometry-a sensitive, reliable, fast and cost-effective
technique. Diagn Pathol. 10:1322015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ueno M, Muto T, Oya M, Ota H, Azekura K
and Yamaguchi T: Multiple primary cancer: An experience at the
Cancer Institute Hospital with special reference to colorectal
cancer. Int J Clin Oncol. 8:162–167. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Warren S and Gates O: Carcinoma of
ceruminous gland. Am J Pathol. 17:821–826.3. 1941.PubMed/NCBI
|
|
8
|
Lee TK, Barringer M, Myers RT and Sterchi
JM: Multiple primary carcinomas of the colon and associated
extracolonic primary malignant tumors. Ann Surg. 195:501–507. 1982.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Li M and Gu J: Changing patterns of
colorectal cancer in China over a period of 20 years. World J
Gastroenterol. 11:4685–4688. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
McCashland TM, Brand R, Lyden E and de
Garmo P: CORI Research Project: Gender differences in colorectal
polyps and tumors. Am J Gastroenterol. 96:882–886. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lacopetta B: Are there two sides to
colorectal cancer? Int J Cancer. 101:403–408. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Stewart SL, Wike JM, Kato I, Lewis DR and
Michaud F: A population-based study of colorectal cancer histology
in the United States, 1998–2001. Cancer. 107 5 Suppl:S1128–S1141.
2006. View Article : Google Scholar
|
|
13
|
Morton LM, Swerdlow AJ, Schaapveld M,
Ramadan S, Hodgson DC, Radford J and van Leeuwen FE: Current
knowledge and future research directions in treatment-related
second primary malignancies. EJC Suppl. 12:S5–S17. 2014. View Article : Google Scholar
|
|
14
|
Morton LM, Onel K, Curtis RE, Hungate EA
and Armstrong GT: The rising incidence of second cancers: Patterns
of occurrence and identification of risk factors for children and
adults. Am Soc Clin Oncol Educ Book. e57–e67. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
da Silva SD, Morand GB, Alobaid FA, Hier
MP, Mlynarek AM, Alaoui-Jamali MA and Kowalski LP:
Epithelial-mesenchymal transition (EMT) markers have prognostic
impact in multiple primary oral squamous cell carcinoma. Clin Exp
Metastasis. 32:55–63. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jung YS, Lim J, Jung KW, Ryu J and Won YJ:
Metachronous second primary malignancies after head and neck cancer
in a Korean cohort (1993–2010). PLoS One. 10:e01341602015.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chen HS and Sheen-Chen SM: Synchronous and
‘early’ metachronous colorectal adenocarcinoma: Analysis of
prognosis and current trends. Dis Colon Rectum. 43:1093–1099. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Takeuchi H, Toda T, Nagasaki S, Kawano T,
Minamisono Y, Maehara Y and Sugimachi K: Synchronous multiple
colorectal adenocarcinomas. J Surg Oncol. 64:304–307. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bertolaccini L and Olivero G: Hereditary
non polyposis colorectal cancer (HNPCC). A clinical and genetic
entity. Minerva Chir. 57:63–72. 2002.PubMed/NCBI
|
|
20
|
Hodadoostan MK, Reza F, Elham M, Alizade
AH Mohammad, Molaie M, Mashaiekhy R, Doagoo SZ, Moosavy M, Malek FN
and Zali MR: Clinical and pathology characteristics of colorectal
polyps in Iranian population. Asian Pac J Cancer Prev. 11:557–560.
2010.PubMed/NCBI
|
|
21
|
Yoshida D, Kono S, Moore MA, Toyomura K,
Nagano J, Mizoue T, Mibu R, Tanaka M, Kakeji Y, Maehara Y, et al:
Colorectal polypectomy and risk of colorectal cancer by subsite:
The Fukuoka colorectal cancer study. Jpn J Clin Oncol. 37:597–602.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Papadopoulos V, Michalopoulos A, Baanis G,
Papapolychroniadis K, Paramythiotis D, Fotiadis P, Berovalis P and
Harlaftis N: Synchronous and metachronous colorectal carcinoma.
Tech Coloproctol. 8 Suppl 1:s97–s100. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Brown SR, Finan PJ, Hall NR and Bishop DT:
Incidence of DNA replication errors in patients with multiple
primary cancers. Dis Colon Rectum. 41:765–769. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wood LD, Parsons DW, Jones S, Lin J,
Sjöblom T, Leary RJ, Shen D, Boca SM, Barber T, Ptak J, et al: The
genomic landscapes of human breast and colorectal cancers. Science.
318:1108–1113. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liang YH, Shao YY, Chen HM, Lai CL, Lin
ZZ, Kuo RN, Cheng AL, Yeh KH and Lai MS: Young patients with
colorectal cancer have increased risk of second primary cancers.
Jpn J Clin Oncol. 45:1029–1035. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Negru S, Papadopoulou E, Apessos A,
Stanculeanu DL, Ciuleanu E, Volovat C, Croitoru A, Kakolyris S,
Aravantinos G, Ziras N, et al: KRAS, NRAS and BRAF mutations in
Greek and Romanian patients with colorectal cancer: A cohort study.
BMJ Open. 4:e0046522014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Haley L, Tseng LH, Zheng G, Dudley J,
Anderson DA, Azad NS, Gocke CD, Eshleman JR and Lin MT: Performance
characteristics of next-generation sequencing in clinical mutation
detection of colorectal cancers. Mod Pathol. 28:1390–1399. 2015.
View Article : Google Scholar : PubMed/NCBI
|