Introduction
Glioblastoma multiforme (GBM) is the most common
intracranial malignancy (1),
accounting for 15.6% of all primary brain tumors and 45.2% of
primary malignant brain tumors (1).
At present, the standard treatment of GBM involves surgery combined
with postoperative synchronous chemoradiotherapy and adjuvant
chemotherapy (2). Despite
improvements in minimally invasive surgical techniques and the use
of intensity modulated conformal radiotherapy (RT) and temozolomide
chemotherapy, the 5-year overall survival rate of GBM is still only
9.8% (3). Postoperative RT is the
most important adjuvant therapy for GBM as it can reduce the
likelihood of tumor recurrence (4).
However, RT is not always ideal because of poor glioma cell
radiosensitivity and an insufficient blood and oxygen supply to the
postoperative tumor area. In addition, the brain is a dose-limiting
organ for radiation, such that it is difficult to enhance the local
control of a tumor by increasing the radiation dose. Therefore,
methods to augment the radiosensitivity of GBM have emerged as an
important research topic. Furthermore, to improve the outcomes of
patients following traditional surgery and chemoradiotherapy,
studies investigating strategies to improve the survival rate of
GBM by targeted molecular therapy are urgently required.
Platelet-derived growth factor (PDGF) was first
identified in fibroblasts and smooth muscle cells and was
considered a powerful pro-mitotic agent (5,6) as it may
be physically separated from human platelets (7). The PDGF receptor (PDGFR) is a type of
tyrosine kinase receptor. PDGF and PDGFR have both been shown to be
overexpressed in glial tumor cell lines and tumor surgical samples,
and their increased expression has been correlated with a higher
tumor grade. In previous studies, analysis of the expression levels
of PDGF-A and PDGF-B, as well as their receptor PDGFR-β, in glioma
cells was performed through in situ hybridization and
immunohistochemical staining (8–10). Binding
of PDGF to PDGFR-β activates an intracellular signal transduction
pathway involving a cascade of mitogen-activated protein kinase
proteins and resulting in the proliferation of malignant cells
(11). In addition, PDGFR-β has been
closely related to tumor angiogenesis. During this process, new
extravascular blood vessels are covered by vascular smooth muscle
cells and adventitial cells, and the development of these cells
requires the activation of PDGFR. PDGF is also chemotactic and
causes these cells to concentrate around the neovascular networks
in order to stimulate their growth and promote tumor angiogenesis.
Furthermore, PDGF is able to induce the transcription and secretion
of vascular endothelial growth factor (VEGF), thereby promoting
tumor angiogenesis indirectly (12).
At present, a variety of clinical PDGFR tyrosine
kinase inhibitors are used to treat glioma. Imatinib has been shown
to enhance the radiosensitivity and chemosensitivity of gliomas,
inhibit glioma cell clone formation and arrest glioma cells in the
G0/G1 and G2/M phases (13,14). Holdhoff et al (15) observed glioma cell lines while
administering imatinib combined with RT, and observed that imatinib
was able to radiosensitize the cells and inhibit tyrosine
phosphorylation of numerous intracellular proteins in a
dose-dependent manner. Although it is known that PDGFR-β is the key
tyrosine kinase in the alteration of the radiosensitivity of glioma
cells (16), the downstream pathways
of such reactions require further elucidation. Imatinib is a
phenylaminopyrimidine derivative that selectively inhibits several
receptor tyrosine kinases thought to play a role in tumor
proliferation and progression. These include the oncogenic BCR-ABL
fusion protein found in leukemia cells, PDGFR and KIT, which is the
oncogenic product of the stem cell factor receptor gene c-Kit.
Other non-receptor tyrosine kinases, serine/threonine kinases and
growth factor receptors, including epidermal growth factor receptor
(EGFR) and fibroblast growth factor receptor, are at least two
orders of magnitude more resistant to imatinib than BCR-ABL and
PDGFR (17). These findings suggested
that the radiosensitizing effect of imatinib on gliomas may involve
the inhibition of multiple receptor tyrosine kinases, including
PDGFR and other non-receptor tyrosine kinases.
In order to investigate the effect of PDGFR-β on the
radiosensitivity of glioma, the present study used RNA interference
(RNAi) technology to silence PDGFR-β expression in C6 glioma cells,
and observed the proliferation, cell cycle distribution and
apoptosis of C6 glioma cells in vivo and in vitro.
Furthermore, the present study evaluated the possibility of
combining RNAi technology with RT to enhance the radiosensitivity
of gliomas, as well as the underlying molecular mechanisms.
Materials and methods
Ethics statement
This study was performed in strict accordance with
the recommendations in the Guide for the Care and Use of Laboratory
Animals of Central South University (Changsha, China). The protocol
was approved by the Committee on the Ethics of Animal Experiments
of Central South University (permit no. 2014033-2). Animals were
sacrificed by sodium pentobarbital anesthesia, and all efforts were
made to minimize suffering.
Cells and cell culture
C6 glioma cells were purchased from the cell center
of Xiangya Medical College, Central South University. The cells
were divided into three groups, as follows: i) Untreated C6 glioma
cells were designated the control group (CON); ii) C6 glioma cells
transfected with PDGFR-β-small interfering (si)RNA vector were
designated the knockdown group (KD); and iii) C6 glioma cells
transfected with the empty vector were designated the negative
control group (NC). CON, NC and KD cells were cultured in
Dulbecco's modified Eagle's medium (Hyclone; GE Healthcare Life
Sciences, Logan, UT, USA) supplemented with 10% heat-inactivated
fetal bovine serum (Hyclone; GE Healthcare Life Sciences), 50 U/ml
penicillin and 50 mg/ml streptomycin in a humidified atmosphere
containing 5% CO2 at 37°C.
Construction and transfection of the
RNAi-PDGFR-β vector
The 19-nucleotide siRNA targeting the rat PDGFR-β
gene with a high gene-silencing efficacy (sense, caG GTG GTG TTT
GAG GCT TAT; antisense, ATA AGC CTC AAA CAC CAC CTG) and the
negative control siRNA (sense, TTC TCC GAA CGT GTC ACG T;
antisense, ACG TGA CAC GTT CGG AGA A) were chemically synthesized
by Shanghai GeneChem Co., Ltd. (Shanghai, China). The short hairpin
(sh)RNA corresponding to the 6-nucleotide loop sequence (CTC GAG)
of the PDGFR-β-siRNA, and its negative control containing the
9-nucleotide loop sequence (TTC AAG AGA) flanked by sense and
antisense siRNA sequences, were synthesized by polymerase chain
reaction (PCR) as previously described (18). The PDGFR-β-shRNA was inserted
immediately into the shRNA expression system of the
pU6-vshRNA-UBI-GFP vector (Shanghai GeneChem Co., Ltd.) to generate
an RNAi-PDGFR-β vector, in which PDGFR-β shRNA was driven by the LV
promoter and green fluorescent protein (GFP) was the reporter gene.
All generated plasmids were identified by PCR and sequencing.
Detailed vector maps and sequence information are available on
request.
Transfection
For transfection, C6 glioma cells were seeded into
6-well plates at a concentration of 5×104 cells/well in
a humidified incubator containing 5% CO2 at 37°C. Upon
reaching 15% confluence, the cells were transfected with 10-µl
diluents containing 4×107 RNAi-PDGFR-β vector or
negative control vector, and were added to 890 µl enhancing
solution (REVG0002; Shanghai GeneChem Co., Ltd.) and 100-µl
polybrene (5 µl/ml) at a multiplicity of infection of 2. If there
were no obvious signs of cell toxicity, the medium was changed
after 24 h, and the cells were incubated for 2–3 days. GFP reporter
gene expression was observed by fluorescence microscopy; a
fluorescence rate of >80% suggested transfection success.
Western blot analysis
CON, NC and KD cells were homogenized in lysis
buffer [50 mM Tris (pH 7.5), 1% Nonidet P-40, 150 mM NaCl, 2 mM
EGTA, 1 mM Na3VO4, 100 mM NaF, 10 mM Na4P2O7,
1 mM phenylmethylsulfonyl fluoride, 10 g/ml aprotinin and 10 g/ml
leupeptin]. Protein lysates were centrifuged at 14,000 × g
for 10 min at 4°C, after which the total protein concentration was
determined using the BCA protein assay (Beijing Dingguo Changsheng
Biotechnology, Co., Ltd., Beijing, China). Cell lysates containing
50 µg protein were separated by 8% SDS-PAGE and transferred onto
polyvinylidene difluoride membranes (EMD Millipore, Billerica, MA,
USA). The membranes were blocked with 5% (wt/vol) skimmed milk, and
then probed with rabbit anti-rat PDGFR-β (dilution 1:10,000;
sc-358943; Santa Cruz Biotechnology, Inc., Dallas, TX, USA) and
β-actin (dilution 1:10,000; AP0060; Bioworld Technology, Inc., St.
Louis Park, MN, USA) monoclonal antibodies overnight at 4°C. The
membranes were then washed three times [with 50 mM Tris (pH 7.5),
0.5% Tween-20, 150 mM NaCl and 2 mM EGTA] and incubated with
horseradish peroxidase-conjugated goat anti-rabbit secondary
antibody (dilution 1:10,000; A0208; Beyotime Institute
Biotechnology, Haimen, China) for 1 h at room temperature, followed
by visualization using enhanced chemiluminescence (ECL) Western
blotting detection reagents (Beyotime Institute Biotechnology).
Protein band intensities were measured using ImageJ v1.45 software
(National Institutes of Health, Bethesda, MD, USA) and normalized
using the β-actin band intensity as the internal standard of the
total protein load.
Cell viability assay
CON, NC and KD cells were plated onto 96-well plates
at a density of 1×104/well, and the cell viability was
determined using MTT assays after 12, 24, 48 and 72 h. Briefly, 10
µl MTT (Beijing Dingguo Changsheng Biotechnology, Co., Ltd.) stock
solution (5 mg/ml) was added to each well, and the plates were
incubated at 37°C for 4 h. Subsequently, 150 µl DMSO was added to
each well. The plate was shaken on a rotary platform at room
temperature for 10 min, after which the optical density was
measured at 570 nm. Data are expressed as a percentage of the
control. Experiments were performed in triplicate and repeated at
least three times.
Colony formation assay
CON, NC and KD cells were plated onto 6-well plates
at a density of 1×103 cells/well and cultured in 5%
CO2 at 37°C for 12 days. The cells were exposed to
fractionated 6-MV X-rays (0, 2, 4, 6 or 8 Gy doses) at a dose rate
of 2.0 Gy/min using a Siemens PRIMUS™ Linear Accelerator (Siemens
Ltd., Malvern, PA, USA). Colonies were stained with 0.005% crystal
violet in methanol. Colony formation (≥50 cells) was counted under
an inverted Olympus microscope (Olympus Corporation, Tokyo, Japan).
Experiments were performed in triplicate and repeated thrice.
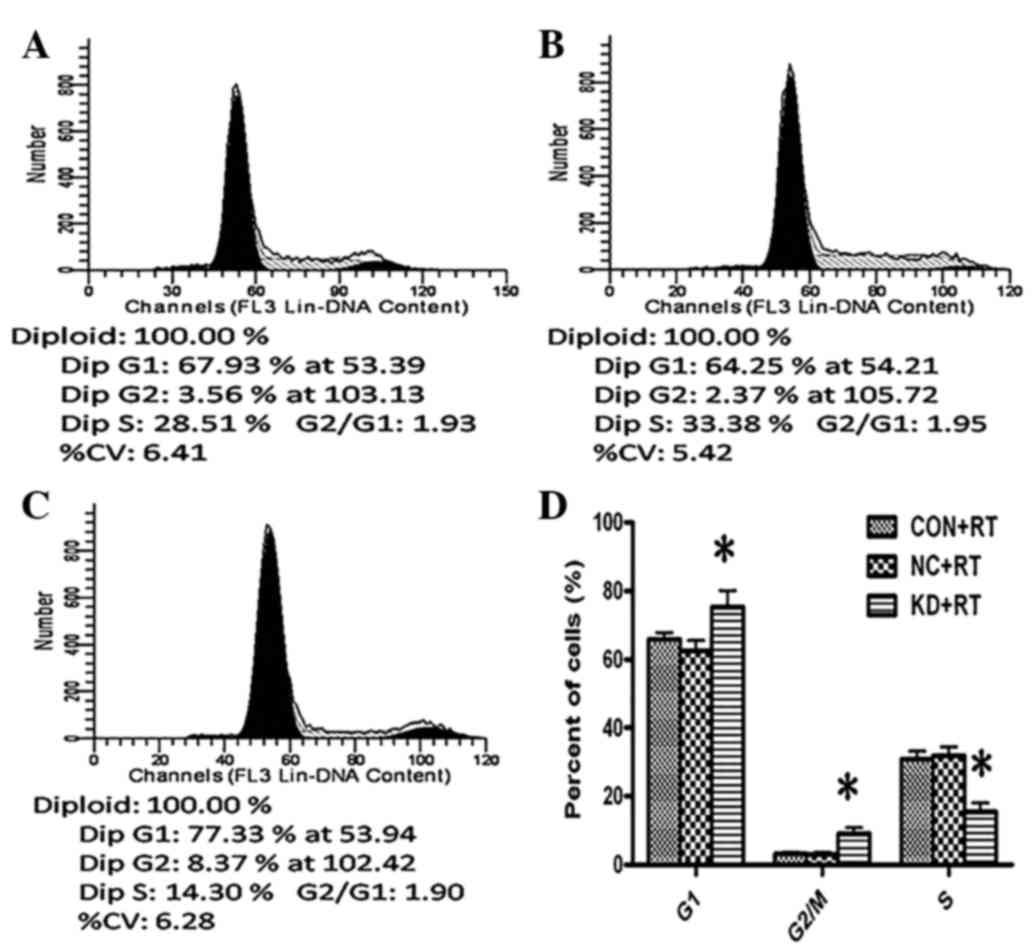
Cell cycle analysis
C6 glioma cells were divided into the CON+RT group,
NC+RT group (NC+RT) and KD+RT group. The cells were treated with a
radiation dose of 3 Gy at a dose rate of 2 Gy/min using a 6-MV
X-ray. Cells were trypsinized, washed with cold PBS and
re-suspended in PBS. Subsequently, the cells were fixed in 70%
ethanol for 30 min, after which 5 µl propidium iodide (final
concentration, 250 ng/ml; BD Biosciences, Franklin Lakes, NJ, USA)
was added to the mixture. Flow cytometry was performed to detect
and analyze changes in the cell cycle distribution using a FACScan
flow cytometer (BD Biosciences).
Xenografts and experimental
design
A total of 50 4-to-6-week-old female nude mice were
purchased from the Hunan Slack King of Laboratory Animal Co., Ltd.,
(Changsha, China). All mice were housed in the Unit for Laboratory
Animal Medicine, Xiangya Hospital (Changsha, China), with a 12-h
light/dark cycle, free access to water and a standard mouse diet.
The mice were divided into five groups of 10 mice each, as follows:
i) CON group, ii) NC group, iii) KD group, iv) RT group and vi)
KD+RT group. Cells (1×106) were injected subcutaneously
into the left side of the axillary rear position of the mice. The
CON and RT groups were injected with C6 cells only, the NC group
with C6 cells and empty vector, and the KD and KD+RT groups with C6
cells and the RNAi-PDGFR-β vector. When the tumor volume had
reached an average size of 150 mm3, the mice in the RT
and KD+RT groups were irradiated with a dose of 10-Gy radiation.
During radiation treatment, the entire mouse body was covered with
lead sheets, with the exception of the tumor area, so that only the
tumor was exposed to the radiation. After 2 days, four mice from
each group were sacrificed. Subcutaneous tumors were removed and
fixed in buffered formaldehyde for hematoxylin-eosin (H&E)
staining, immunohistochemical analysis and terminal
deoxynucleotidyl transferase dUTP nick end-labeling (TUNEL) assays.
Subcutaneous tumor growth of the remaining six mice in each group
was measured every 3 days using vernier calipers. Tumor volume was
calculated according to the equation: Volume (mm3) = 1 /
2 × (Rmax × Rmin2), where R is the tumor diameter. Mice
were sacrificed after 28 days.
H&E staining and
immunohistochemistry
Formalin-fixed paraffin-embedded tumors were cut
into 4-µm thick sections for H&E and immunohistochemical
analysis. H&E was performed using standard histological
techniques. Immunohistochemical analysis was conducted in
accordance with the manufacturer's protocol. Briefly, the tissue
sections were incubated with one of the following antibodies:
Rabbit anti-mouse PDGFR-β polyclonal antibody (dilution 1:100;
sc-358943; Santa Cruz Biotechnology, Inc.), rabbit anti-mouse Ki-67
monoclonal antibody (dilution 1:400; ab16667; Abcam, Cambridge,
UK), rabbit anti-mouse cyclin B1 polyclonal antibody (dilution
1:100; sc-752; Santa Cruz Biotechnology, Inc.) and rabbit
anti-mouse VEGF polyclonal antibody (dilution 1:400; ab51745;
Abcam). Cyclin B1 and Ki-67 were expressed in the nuclei of tumor
cells, PDGFR-β was expressed in the cytomembrane and VEGF was
expressed in the cytoplasm. Positively stained cells were counted
in five randomly selected fields.
Cell apoptosis by TUNEL
To detect apoptotic cells in subcutaneous tumors,
TUNEL assays were performed using a commercial apoptosis detection
kit (KGA 105; Nanjing KeyGen Biotech Co., Ltd., Nanjing, China),
according to the manufacturer's protocol. TUNEL-positive cells
displayed compaction or segregation of the nuclear chromatin, or
nuclei that were broken up into discrete fragments. Positively
stained cells were counted in five representative fields. The
apoptosis index was calculated according to the following formula:
Apoptosis index (%) = number of TUNEL-positive cells / total cell
count × 100.
Statistical analysis
The experimental data were analyzed using SPSS
version 17.0 (SPSS, Inc., Chicago, IL, USA) and quantitative data
are presented as the mean ± standard deviation. Two groups were
compared using the Student's t-test and multiple groups were
compared using one-way analysis of variance followed by post-hoc
tests such as the least significant difference test. The results of
the TUNEL and immunohistochemical assays were compared using the
χ2 test. P<0.05 was considered to indicate a
statistically significant difference.
Results
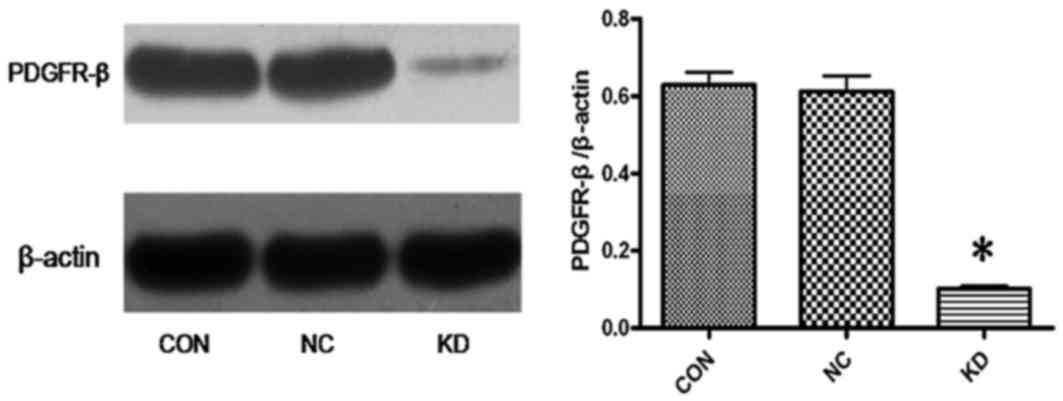
PDGFR-β-shRNA downregulates PDGFR-β
expression in C6 glioma cells
As shown in Fig. 1,
western blotting was used to assess the expression levels of
PDGFR-β in the CON, NC and KD group C6 cells. The density ratio of
PDGFR-β/β-actin was 0.6298±0.555 in the Con group, 0.6125±0.696 in
the NC group and 0.1020±0.0126 in the KD group. There were
significant differences in the protein expression levels of PDGFR-β
between the KD group and the CON and NC groups (P=0.0001). These
results suggest that RNAi-PDGFR-β significantly inhibits PDGFR-β
expression in glioma cells.
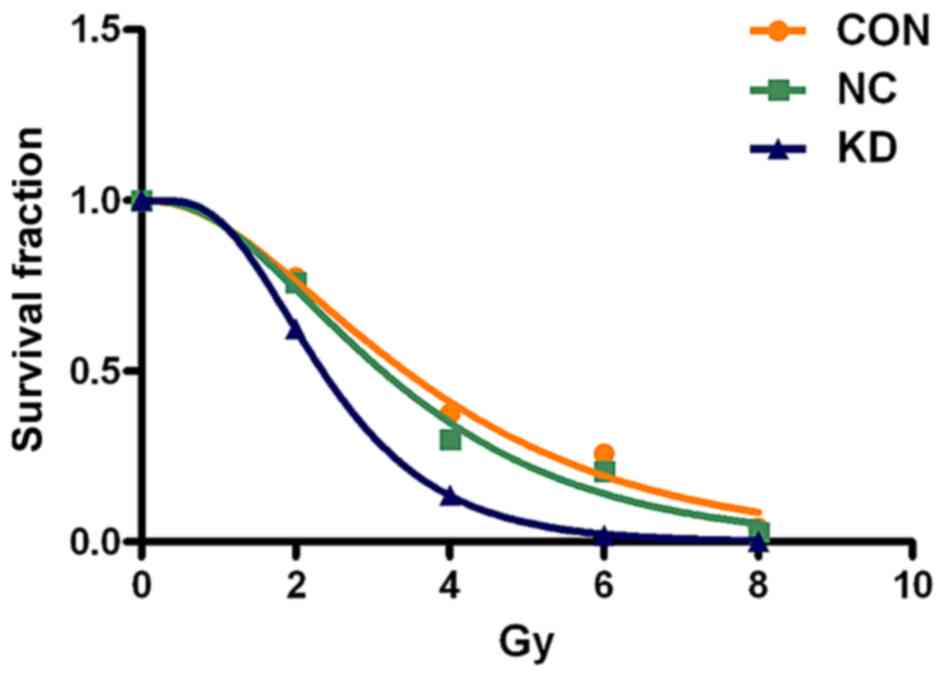
PDGFR-β-specific shRNA enhances the
radiosensitivity of C6 glioma cells in vitro
In order to investigate the radiosensitivity of the
KD cells, a clonogenic survival assay was performed (Fig. 2) and quantified by determination of
the radiobiological parameters (Table
I). Clone formation assays indicated that the mean lethal dose
(D0) of radiation in the KD+RT group was decreased from
2.391 to 1.091 Gy compared with the RT group, and the
radiosensitization ratio was 2.192. These results suggest that
RNAi-PDGFR-β specifically increases the level of radiation-induced
C6 glioma cell death and enhances the radiosensitivity of C6 glioma
cells in vitro.
 | Table I.Radiobiological parameters of NC and
KD C6 glioma cells combined with radiotherapy. |
Table I.
Radiobiological parameters of NC and
KD C6 glioma cells combined with radiotherapy.
| Group | K | N | D0 | Dq | SER (KD vs.
CON) | SER (KD vs.
NC) | R2 |
|---|
| CON | 0.4183 | 2.543 | 2.391 | 1.805 | – | – | 0.988 |
| NC | 0.4968 | 2.920 | 2.013 | 1.771 | – | – | 0.988 |
| KD | 0.9164 | 5.616 |
1.091 | 1.813 | 2.192 | 1.845 | 1.000 |
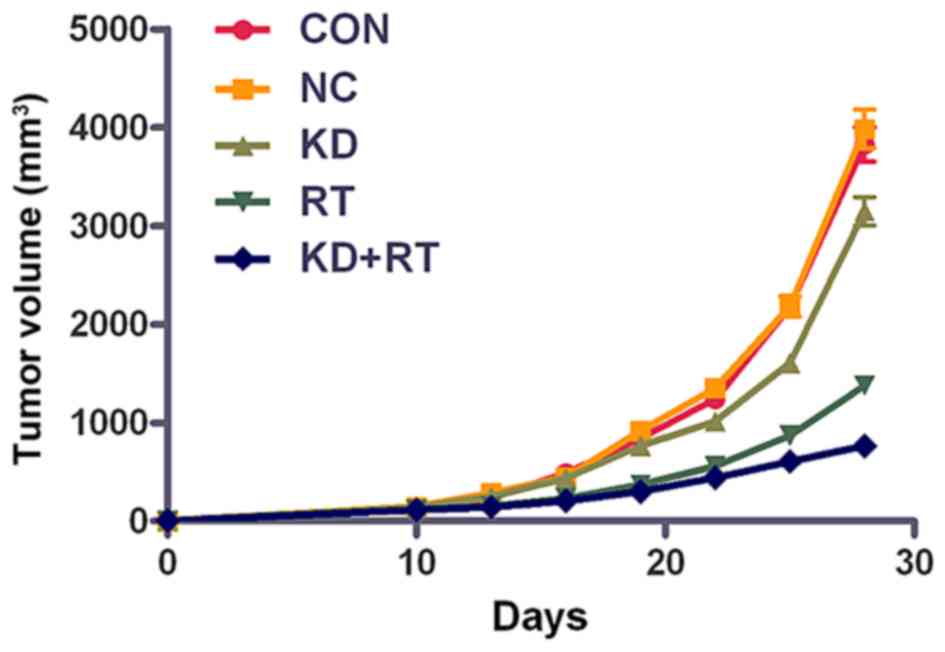
PDGFR-β-specific shRNA enhances the
radiosensitivity of C6 glioma cell xenografts
To further examine the effects of RNAi-PDGFR-β,
in vivo experiments with C6 cell xenograft tumors were
conducted. An in vivo radiation dose of 10 Gy was used to
simplify the assessment of the effects following treatment. No
significant differences were observed in the tumor volumes between
the CON and NC groups; however, the tumor volume of the KD group
was significantly smaller compared with the CON and NC groups after
28 days (P=0.02; Fig. 3). The tumor
volumes in the RT and KD+RT groups were significantly smaller
compared with those in the CON, NC and KD groups at 28 days
(P=0.0001; Fig. 3). In addition, the
tumor volume in the KD+RT group was significantly smaller than the
RT group at 28 days (P=0.0001; Fig.
3). These results suggest that RNAi-PDGFR-β specifically
enhances the radiosensitivity of C6 glioma cell xenografts in
vivo.
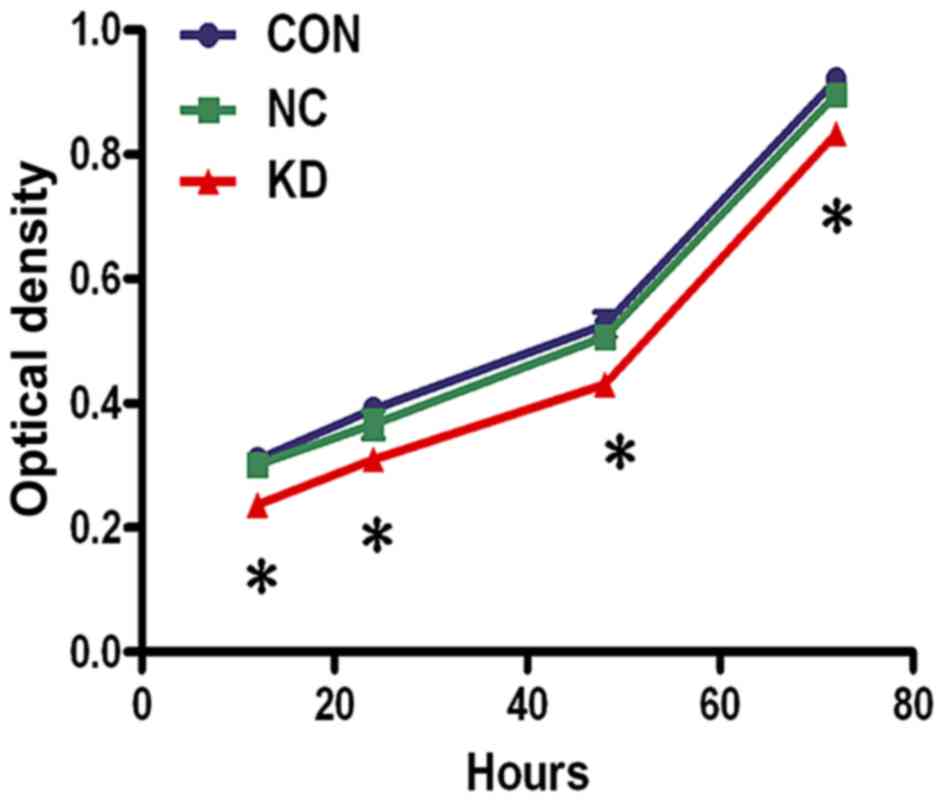
PDGFR-β-specific shRNA reduces the
viability of C6 glioma cells
To investigate the effect of PDGFR-β-specific shRNA
on C6 glioma cell viability, MTT assays were performed. The results
demonstrated that the KD cells had a significantly reduced
viability compared with the CON and NC cells at 12 (all P=0.04), 24
(P=0.04 vs. CON; P=0.03 vs. NC), 48 (P=0.03 vs. CON; P=0.04 vs. NC)
and 72 h (all P=0.04) (Fig. 4).
PDGFR-β silencing causes cell cycle
arrest in the G1 and G2/M phases
Cell cycle profiles were determined by flow
cytometry. The fractions of KD+RT group cells in the G1 and G2/M
phases were significantly increased by 9.47 and 5.88%,
respectively, compared with those in the CON+RT group (G1 phase,
P=0.02; G2/M phase, P=0.00; Fig. 5).
Furthermore, the fraction of KD+RT group cells in the S phase was
significantly decreased by 15.34% compared with the CON and NC
groups (all P=0.001; Fig. 5). These
results suggest that the knockdown of PDGFR-β expression enhances
radiation-induced cell cycle arrest in the G1 and G2/M phases.
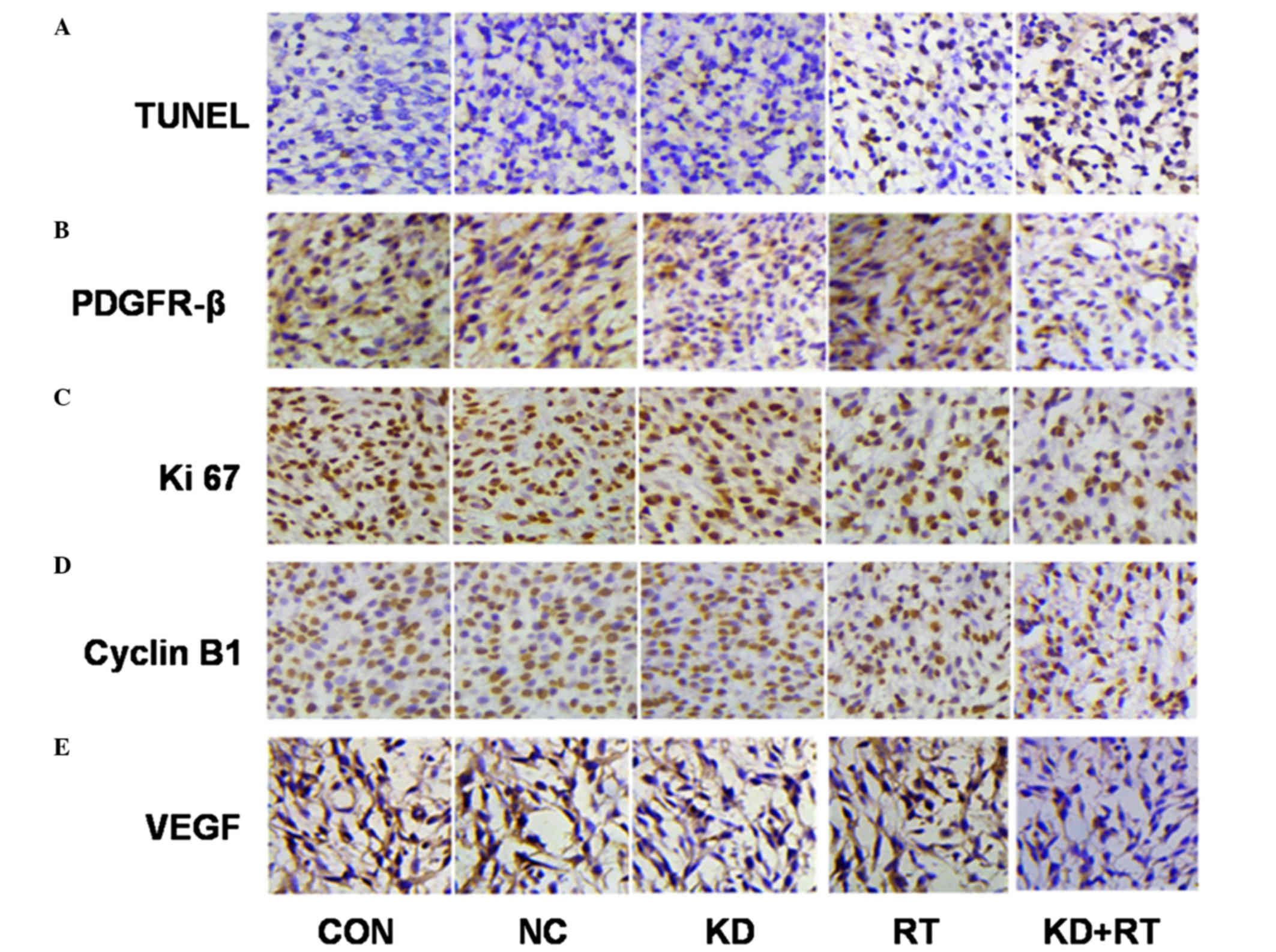
Immunohistochemical analysis of
xenograft sections for PDGFR-β expression
PDGFR-β was expressed in all groups examined,
although the degree of expression varied widely among the groups.
Immunohistochemical analysis showed that the expression of PDGFR-β
in the KD and RT groups was significantly reduced compared with the
CON and NC groups (KD vs. CON and NC, P=0.01; RT vs. CON and NC,
P=0.03; Fig. 6 and Table II). Furthermore, the expression of
PDGFR-β in the KD+RT group was significantly lower compared with
the KD and RT groups (all P=0.001; Fig.
6 and Table II).
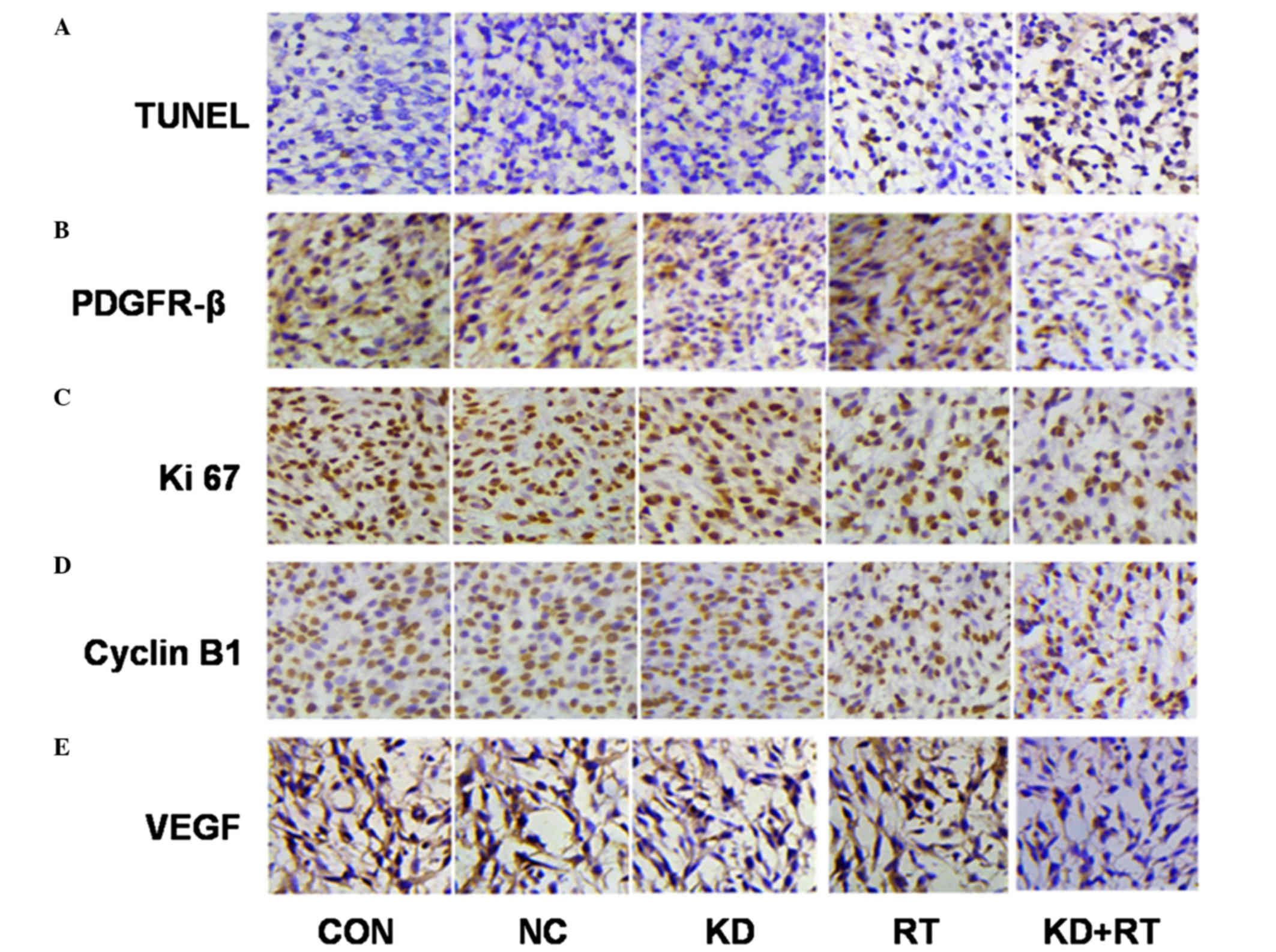 | Figure 6.TUNEL assay and expression of
PDGFR-β, Ki-67, VEGF and cyclin B1 in C6 cell xenografts using
immunohistochemistry (magnification, ×400). (A) Radiation and
PDGFR-β-specific shRNA induced cell apoptosis in C6 cell
xenografts. Positive apoptotic cells were identified as brown, with
a brownish/black nuclear stain. (B) The expression of PDGFR-β in C6
cells in vivo. Positive PDGFR-β expression was identified by
a brown cytoplasm/membrane stain. (C) The expression of Ki-67 in C6
cells in vivo. Positive Ki-67 expression was identified by a
brown nuclear stain. (D) The expression of cyclin B1 in C6 cells
in vivo. Positive cyclin B1 expression was identified by a
brown nuclear stain. (E) The expression of VEGF in C6 cells in
vivo. Positive VEGF expression was identified as a brown
cytoplasmic stain. TUNEL, terminal deoxynucleotidyl transferase
dUTP nick end-labeling; PDGFR-β, platelet-derived growth factor
receptor-β; VEGF, vascular endothelial growth factor; CON, control
C6 cells; NC, negative control C6 cells; KD, PDGFR-β-knockdown C6
cells; RT, radiotherapy. |
 | Table II.AI and expression of PDGFR-β, Ki-67,
cyclin B1 and VEGF in C6 cell xenografts. |
Table II.
AI and expression of PDGFR-β, Ki-67,
cyclin B1 and VEGF in C6 cell xenografts.
| Group | AI (%) | PDGFR-β (%) | Ki-67 (%) | Cyclin B1 (%) | VEGF (%) |
|---|
| CON | 2.77 | 53.28 | 81.75 | 55.38 | 55.33 |
| NC | 3.02 | 54.62 | 78.88 | 65.27 | 54.78 |
| KD | 5.12 | 30.83 | 77.89 | 54.25 | 46.36 |
| RT | 28.4 | 37.38 | 57.23 | 35.45 | 59.24 |
| KD+RT | 48.2a | 17.33a | 41.38a | 27.23a | 25.43 |
| χ2 | 112.52 | 42.33 | 57.64 | 26.81 | 28.87 |
Immunohistochemical analysis of
xenograft sections for Ki-67 and cyclin B1 expression
Immunohistochemical analysis indicated that the
expression of Ki-67 in the KD group was marginally lower than its
expression level in the CON group, although the difference was not
significant (P=0.29). The expression of Ki-67 in the RT and KD+RT
groups was significantly lower compared with the CON, NC and KD
groups (P<0.0001), and the expression of Ki-67 in the KD+RT
group was significantly lower compared with that in the RT group
(P<0.0001). PDGFR-β-specific shRNA did not affect the expression
of cyclin B1 in C6 cell xenografts, although the expression of
cyclin B1 was reduced in the RT group (P=0.26 vs. CON). The
expression of cyclin B1 in the RT and KD+RT groups was lower
compared with the CON, NC and KD groups (all P=0.0003). The
expression of cyclin B1 in the KD+RT group was significantly lower
than that in the RT group (P=0.0002; Fig.
6 and Table II).
TUNEL analysis of cell apoptosis in C6
glioma cell xenografts
TUNEL analysis showed that there were no significant
differences in the apoptosis indexes of C6 glioma cell xenografts
among the CON, NC and KD groups (P=0.06). The apoptosis indexes of
the RT and KD+RT groups were significantly higher than those of the
CON, NC and KD groups (all P<0.0001). The apoptosis index of the
KD+RT group was significantly higher than that of the RT group
(P=0.01; Fig. 6 and Table II.). These results suggest that
radiation and PDGFR-β-specific shRNA induces cell apoptosis in C6
glioma cell xenografts.
Immunohistochemical analysis of
xenograft sections for VEGF
Immunohistochemical analysis of C6 cell xenograft
tissues demonstrated exposure of C6 cell xenografts to RT resulted
in a slight increase in VEGF expression (P=0.24), and suggested
there was a radiation-induced increase in VEGF protein levels. The
expression of VEGF in the KD group was lower compared with the CON
and NC groups (all P=0.01). The expression of VEGF in the KD+RT
group was significantly lower compared with the RT group (P=0.01).
This finding indicates that, when KD cells are irradiated, VEGF
levels are reduced as compared with the irradiation alone control.
Therefore, PDGFR-β-specific shRNA reduced the radiation-stimulated
increase in VEGF protein expression levels.
Discussion
Targeted molecular therapy is a novel therapeutic
strategy for GBM (18). In previous
studies, targeting of PDGFR using selected inhibitors achieved some
success in the treatment of gliomas. However, the molecular
mechanisms remain unclear. The present study demonstrated that
PDGFR-β-specific shRNA enhanced the radiosensitivity of C6 glioma
cells in vivo and in vitro, and that the molecular
mechanisms involved promoting radiation-induced arrest of C6 glioma
cells in the G1 and G2/M phases and reducing the expression levels
of Ki-67, cyclin B1 and VEGF. These results suggested that PDGFR-β
may be used a target for enhancement of the radiosensitivity of
GBM.
Generally, it is thought that the G2 and M phases
are the most sensitive to radiation therapy, followed by the G1
phase, while the S phase is the least sensitive to RT (19). Radiation is able to cause M phase
delay, as well as cell cycle arrest in the G0/1 and G2/M phases
(20). Cyclin B1, which is closely
associated with mitosis, is not expressed in normal brain tissue or
is expressed at extremely low levels; however, it has been shown to
be overexpressed in glial tumors and its upregulation was
correlated with a higher tumor grade (21). Cyclin B1 plays an important role in
accelerating cell cycle progression and regulating the
transformation of the G2/M phase. To date, studies have reported
that excessive cyclin B1 expression is able to cause radiation
resistance, while decreased cyclin B1 expression is able to enhance
G2/M phase arrest and increase radiosensitivity (22,23). Ren
et al (13) reported that the
PDGFR inhibitor, imatinib, was able to inhibit glioma cell colony
formation and to cause the arrest of glioma cells in the G0/G1 and
G2/M phases, with a concomitant reduction of the number of cells in
the S phase. The present study demonstrated that PDGFR-β-specific
shRNA caused C6 cells to arrest in the G0/G1 and G2/M phases.
Furthermore, the positive expression rates of cyclin B1 in the RT
and KD+RT groups were significantly reduced compared with the other
groups. In addition, the expression levels of cyclin B1 in the
KD+RT group were reduced to a greater extent compared with the RT
group. These results suggested that PDGFR-β-targeted therapy
combined with RT was able to reduce the expression of cyclin B1,
thereby blocking cells in the G2/M period and increasing the
radiosensitivity of the cells.
Apoptosis is regulated by the programmed cell death
gene and is the main form of tumor cell death induced by radiation
therapy (24). The present study
demonstrated that the apoptosis index of the KD+RT group was higher
than the other three groups, and that this group had the most
TUNEL-positive cells. These results indicated that inhibition of
PDGFR-β expression by RNAi combined with RT was able to enhance
apoptosis compared with RT alone, suggesting that RNAi of PDGFR-β
might enhance the tumor radiosensitivity of C6 gliomas.
Ki-67 is a nuclear antigen associated with cell
proliferation. The expression levels of Ki-67 have been correlated
with glioma grading and prognosis (25). Lafuente et al (26) reported that the expression of Ki-67
was correlated with the expression of PDGFR-β, suggesting that
PDGFR-β overexpression may promote cell proliferation. In the
present study, expression of Ki-67 was inhibited in the RT and
KD+RT groups, and the lowest number of positive tumor nuclei was
found in the combined treatment group. These results indicated that
PDGFR-β-specific shRNA combined with RT may inhibit cell
proliferation, leading to a greater antitumor effect than RT
alone.
Previous studies have shown that anti-angiogenesis
strategies combined with RT are able to increase the radiation
sensitivity and improve the efficacy of RT (27,28). GBM
is a typical tumor that is rich in blood vessels, and its processes
of development, invasion and metastasis depend on angiogenesis,
which is closely related to PDGF and VEGF signaling pathways
(29). When tumor cells release
PDGF-activated PDGFR-β, it is able to induce endothelial cells and
smooth muscle cells to proliferate and migrate, stimulating the
formation of new blood vessels, which has a direct role in tumor
angiogenesis. In addition, abnormal expression of PDGF stimulates
VEGF secretion via autocrine and paracrine signaling, which
indirectly promotes tumor angiogenesis (30). VEGF is the most effective factor in
promoting vascular growth, as it induces endothelial cell
proliferation and the formation of blood vessels, and also
increases the permeability of blood vessels. In a previous study,
upregulation of VEGF resulted in the resistance of tumors to
radiation (27). PDGFR-β is highly
expressed in vascular endothelial cells and around microvasculature
in glioma, and it is closely related to the formation of blood
vessels (31). In the present study,
as compared with the control and empty vector groups, reduced
expression of VEGF was seen in the KD and KD+RT groups, although
the expression of VEGF was increased in the RT group.
PDGFR-β-specific shRNA combined with RT was able to reduce the
expression of VEGF, and thus affect tumor angiogenesis, while
radiation alone induced increased expression of VEGF. Gorski et
al (32) reported that the level
of VEGF expression increased following RT, which is consistent with
our immunohistochemical results.
The present study demonstrated that PDGFR-β-specific
shRNA inhibits the proliferation of C6 cells in vitro and
in vivo. RT combined with RNAi-PDGFR-β displayed synergistic
antitumor effects on C6 glioma cells in vitro and in
vivo. The molecular mechanism of the radiosensitizing effect of
RNAi-PDGFR-β is involved in cell cycle arrest, cell apoptosis and
anti-angiogensis. A single therapeutic target is often not
effective; thus, multiple target treatments should be adopted.
Omuro (33) reported that the results
of single-target drugs targeting EGFR, VEGFR and PDGFR in malignant
gliomas (glioblastomas and anaplastic forms of astrocytomas,
oligodendrogliomas and oligoastrocytomas) have been disappointing.
Multi-targeting drugs or combinations of two or more
single-targeting drugs should to be used to overcome the resistance
of malignant glioma.
In conclusion, the present study demonstrated that
PDGFR-β-specific shRNA downregulated the expression of PDGFR-β at
the protein level and enhanced the radiosensitivity of C6 cells
in vivo and in vitro. The molecular mechanism of the
enhancement of radiosensitivity by RNAi-PDGFR-β may involve cell
apoptosis, cell cycle arrest and anti-angiogenesis. Therefore,
PDGFR-β may be an appropriate target for selectively enhancing the
radiosensitivity of glioblastoma.
Acknowledgements
The present study was supported by the Hunan
Province Science and Technology Program (grant no. 2011SK3223) and
the Hunan Provincial Natural Science Foundation of China (grant no.
2012JJ5043).
References
|
1
|
Ostrom QT, Gittleman H, Farah P, Ondracek
A, Chen Y, Wolinsky Y, Stroup NE, Kruchko C and Barnholtz-Sloan JS:
CBTRUS statistical report: Primary brain and central nervous system
tumors diagnosed in the United States in 2006–2010. Neuro Oncol. 15
Suppl 2:ii1–ii56. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Stupp R, Hegi ME, Mason WP, van den Bent
MJ, Taphoorn MJ, Janzer RC, Ludwin SK, Allgeier A, Fisher B,
Belanger K, et al European Organisation for Research and Treatment
of Cancer Brain Tumour and Radiation Oncology Groups; National
Cancer Institute of Canada Clinical Trials Group. Effects of
radiotherapy with concomitant and adjuvant temozolomide versus
radiotherapy alone on survival in glioblastoma in a randomised
phase III study, : 5-year analysis of the EORTC-NCIC trial. Lancet
Oncol. 10:459–466. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stupp R, Mason WP, van den Bent MJ, Weller
M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn
U, et al: Radiotherapy plus concomitant and adjuvant temozolomide
for glioblastoma. N Engl J Med. 352:987–996. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nakagawa K, Aoki Y, Fujimaki T, Tago M,
Terahara A, Karasawa K, Sakata K, Sasaki Y, Matsutani M and Akanuma
A: High-dose conformal radiotherapy influenced the pattern of
failure but did not improve survival in glioblastoma multiforme.
Int J Radiat Oncol Biol Phys. 40:1141–1149. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kohler N and Lipton A: Platelets as a
source of fibroblast growth-promoting activity. Exp Cell Res.
87:297–301. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ross R, Glomset J, Kariya B and Harker L:
A platelet-dependent serum factor that stimulates the proliferation
of arterial smooth muscle cells in vitro. Proc Natl Acad Sci USA.
71:pp. 1207–1210. 1974; View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Heldin CH, Westermark B and Wasteson A:
Platelet-derived growth factor: Purification and partial
characterization. Proc Natl Acad Sci USA. 76:pp. 3722–3726. 1979;
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hermansson M, Nistér M, Betsholtz C,
Heldin CH, Westermark B and Funa K: Endothelial cell hyperplasia in
human glioblastoma: Coexpression of mRNA for platelet-derived
growth factor (PDGF) B chain and PDGF receptor suggests autocrine
growth stimulation. Proc Natl Acad Sci USA. 85:pp. 7748–7752. 1988;
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Maxwell M, Naber SP, Wolfe HJ,
Galanopoulos T, Hedley-Whyte ET, Black PM and Antoniades HN:
Coexpression of platelet-derived growth factor (PDGF) and
PDGF-receptor genes by primary human astrocytomas may contribute to
their development and maintenance. J Clin Invest. 86:131–140. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Plate KH, Breier G, Farrell CL and Risau
W: Platelet-derived growth factor receptor-beta is induced during
tumor development and upregulated during tumor progression in
endothelial cells in human gliomas. Lab Invest. 67:529–534.
1992.PubMed/NCBI
|
|
11
|
Chen D, Li Y, Mei Y, Geng W, Yang J, Hong
Q, Feng Z, Cai G, Zhu H, Shi S, et al: miR-34a regulates mesangial
cell proliferation via the PDGFR-β/Ras-MAPK signaling pathway. Cell
Mol Life Sci. 71:4027–4042. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nazarenko I, Hede SM, He X, Hedrén A,
Thompson J, Lindström MS and Nistér M: PDGF and PDGF receptors in
glioma. Ups J Med Sci. 117:99–112. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ren H, Tan X, Dong Y, Giese A, Chou TC,
Rainov N and Yang B: Differential effect of imatinib and synergism
of combination treatment with chemotherapeutic agents in malignant
glioma cells. Basic Clin Pharmacol Toxicol. 104:241–252. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Russell JS, Brady K, Burgan WE, Cerra MA,
Oswald KA, Camphausen K and Tofilon PJ: Gleevec-mediated inhibition
of Rad51 expression and enhancement of tumor cell radiosensitivity.
Cancer Res. 63:7377–7383. 2003.PubMed/NCBI
|
|
15
|
Holdhoff M, Kreuzer KA, Appelt C, Scholz
R, Na IK, Hildebrandt B, Riess H, Jordan A, Schmidt CA, van Etten
RA, et al: Imatinib mesylate radiosensitizes human glioblastoma
cells through inhibition of platelet-derived growth factor
receptor. Blood Cells Mol Dis. 34:181–185. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ranza E, Bertolotti A, Facoetti A,
Mariotti L, Pasi F, Ottolenghi A and Nano R: Influence of imatinib
mesylate on radiosensitivity of astrocytoma cells. Anticancer Res.
29:4575–4578. 2009.PubMed/NCBI
|
|
17
|
Savage DG and Antman KH: Imatinib
mesylate-a new oral targeted therapy. N Engl J Med. 346:683–693.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chen SW, Zhang XR, Wang CZ, Chen WZ, Xie
WF and Chen YX: RNA interference targeting the platelet-derived
growth factor receptor beta subunit ameliorates experimental
hepatic fibrosis in rats. Liver Int. 2008. View Article : Google Scholar
|
|
19
|
Reardon DA, Desjardins A, Vredenburgh JJ,
Herndon JE II, Coan A, Gururangan S, Peters KB, McLendon R,
Sathornsumetee S, Rich JN, et al: Phase II study of Gleevec plus
hydroxyurea in adults with progressive or recurrent low-grade
glioma. Cancer. 118:4759–67. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Biade S, Stobbe CC and Chapman JD: The
intrinsic radiosensitivity of some human tumor cells throughout
their cell cycles. Radiat Res. 147:416–421. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen H, Huang Q, Dong J, Zhai DZ, Wang AD
and Lan Q: Overexpression of CDC2/CyclinB1 in gliomas, and CDC2
depletion inhibits proliferation of human glioma cells in vitro and
in vivo. BMC Cancer. 8:292008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
He J, Li J, Ye C, Zhou L, Zhu J, Wang J,
Mizota A, Furusawa Y and Zhou G: Cell cycle suspension: A novel
process lurking in G2 arrest. Cell Cycle. 10:1468–1476. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Maity A, Hwang A, Janss A, Phillips P,
McKenna WG and Muschel RJ: Delayed cyclin B1 expression during the
G2 arrest following DNA damage. Oncogene. 13:1647–1657.
1996.PubMed/NCBI
|
|
24
|
Silva MF, Khokhar AR, Qureshi MZ and
Farooqi AA: Ionizing radiations induce apoptosis in TRAIL resistant
cancer cells: in vivo and in vitro analysis. Asian Pac J Cancer
Prev. 15:1905–1907. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Takano S, Ishikawa E, Sakamoto N, Matsuda
M, Akutsu H, Noguchi M, Kato Y, Yamamoto T and Matsumura A:
Immunohistochemistry on IDH 1/2, ATRX, p53 and Ki-67 substitute
molecular genetic testing and predict patient prognosis in grade
III adult diffuse gliomas. Brain Tumor Pathol. 33:107–116. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lafuente JV, Adán B, Alkiza K, Garibi JM,
Rossi M and Cruz-Sánchez FF: Expression of vascular endothelial
growth factor (VEGF) and platelet-derived growth factor
receptor-beta (PDGFR-beta) in human gliomas. J Mol Neurosci.
13:177–185. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Fenton BM, Paoni SF and Ding I:
Pathophysiological effects of vascular endothelial growth factor
receptor-2-blocking antibody plus fractionated radiotherapy on
murine mammary tumors. Cancer Res. 64:5712–5719. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Shannon AM and Williams KJ:
Antiangiogenics and radiotherapy. J Pharm Pharmacol. 60:1029–1036.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jain RK: Normalization of tumor
vasculature: An emerging concept in antiangiogenic therapy.
Science. 307:58–62. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Cohen-Jonathan Moyal E: Angiogenic
inhibitors and radiotherapy: From the concept to the clinical
trial. Cancer Radiother. 13:562–567. 2009.(In French). PubMed/NCBI
|
|
31
|
Raymond E: PDGFR inhibition in brain
tumours-oft expectation fails where most it promises. Eur J Cancer.
45:2236–2238. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Gorski DH, Beckett MA, Jaskowiak NT,
Calvin DP, Mauceri HJ, Salloum RM, Seetharam S, Koons A, Hari DM,
Kufe DW and Weichselbaum RR: Blockage of the vascular endothelial
growth factor stress response increases the antitumor effects of
ionizing radiation. Cancer Res. 59:3374–3378. 1999.PubMed/NCBI
|
|
33
|
Omuro AM: Exploring multi-targeting
strategies for the treatment of gliomas. Curr Opin Investig Drugs.
9:1287–1295. 2008.PubMed/NCBI
|