Introduction
At present, lung cancer has the highest incidence
among all types of cancers around the world, which is also the
leading cause of death of cancer patients (1). Non-small cell lung cancer (NSCLC)
accounts for the majority of lung cancers. The prognosis of
patients with lung cancer is still poor, and the 5-year survival
rate after diagnosis is <16% (2).
According to NCCN guidelines, the postoperative 5-year survival
rate of Stage-I NSCLC patients for whom the radiotherapy and
chemotherapy were not recommended after operation is only about
61.3%, and there are still a considerable number of patients who
die within 5 years due to the local tumor recurrence or distant
metastasis (3). Douillard et
al conducted the large-scale clinical study and found that the
postoperative adjuvant chemotherapy was helpful for the improvement
of survival rate of some lung cancer patients with a high risk of
recurrence and metastasis (4).
Therefore, screening the high-risk patients through evaluating the
related factors to the prognosis of NSCLC patients, and providing
adjuvant therapy in time are of great clinical importance in
improving the 5-year survival rate of patients with early-stage
NSCLC.
The new type of candidate tumor suppressor gene, Ras
association domain family gene 1A (RASSF1A), is a kind of
newly-discovered gene with speculated tumor-suppressing function,
located in 3p21.3. This gene is expressed in the normal tissues,
but there is a higher rate of expression loss in lung cancer and
other tumors. It is found in the study that the lung cancer cell
line A549 without the expression of RASSF1A after being transfected
with this gene can reduce the cell clonal formation, inhibit the
anchorage-independent growth, slow down the growth rate of
transplanted tumor inoculated to nude mice and significantly reduce
the pulmonary metastasis capacity of A549 cells (5,6).
As a key member in long-lived proteins, SIRT6 is
closely related to the tumor formation and progression, which is
also significantly associated with the survival rate of cancer
patients. Studies have shown that SIRT6 shows a significant
anticancer effect in lung cancer, especially in NSCLC. In NSCLC
tissue and cell lines, mRNA and protein expression levels in SIRT6
are generally decreased (7). Further
studies have shown that SIRT6 can inhibit the proliferation of
NSCLC cells by inhibiting Twist1 (7).
This study aimed to detect the expressions of
RASSF1A and SIRT6 in NSCLC tissues and normal lung tissues by
immunohistochemical method, and investigated its relationship with
clinicopathological features and prognosis of NSCLC patients.
Materials and methods
Patients and sample source
In total 122 NSCLC patients (NSCLC group) in the
Chinese Medicine Hospital of Linyi City from January to December
2011 were selected, including 89 males and 33 females aged 33–76
years with an average age of (59.83±8.94) years; none of the cases
received radiotherapy or chemotherapy before operation, which was
confirmed pathologically. According to the TNM staging criteria
revised by UICC (Union for International Cancer Control) in 2009,
there were 48 cases in Stage I, 33 cases in Stage II and 41 cases
in Stage III. According to the WHO classification standards of lung
cancer, there were 65 cases of squamous carcinoma, 42 cases of
adenocarcinoma and 15 cases of adenosquamous carcinoma. There were
76 cases of high and moderate differentiation and 46 cases of low
differentiation, and there were 62 cases of lymph node metastasis
and 60 cases of non-lymph node metastasis. Another 122 cases of
normal lung tissues (normal group) without infiltration of cancer
cells confirmed by H&E staining were collected from the same
patients. The follow-up was from February 1, 2011 to January 31,
2016, and the survival period was calculated from the date of
surgery to the expiration date of follow-up, or to the date of
death due to recurrence and metastasis. The application of samples
was approved by the Ethics Committee of the Chinese Medicine
Hospital of Linyi City and signed written informed consent was
obtained from patients or their families.
Methods
The samples were fixed with 10% neutral formalin
immediately after surgical excision, followed by conventional
paraffin embedding and serial section. The section thickness was 5
µm. Conventional immunohistochemical Super Pic Ture™ Polymer
(Biosharp, Hefei, China) two-step method was used for detection
according to the instructions. The high-pressure high-temperature
thermal remediation was used for antigen retrieval. Rabbit
polyclonal RASSF1A antibody (dilution, 1:100; cat. no. ab180801)
and rabbit polyclonal SIRT6 antibody (dilution, 1:100; cat. no.
ab135566) and secondary goat anti-rabbit (HRP) IgG antibody
(dilution, 1:2,000; cat. no. ab6721) were all purchased from Abcam
(Cambridge, MA, USA). Diaminobenzidine (DAB) chromogenic kit was
purchased from Fuzhou Maixin Biotech. Co., Ltd., (Fuzhou, China).
The known positive sections were used as the positive control and
PBS as the negative control, instead of the primary antibody.
Judgement of results
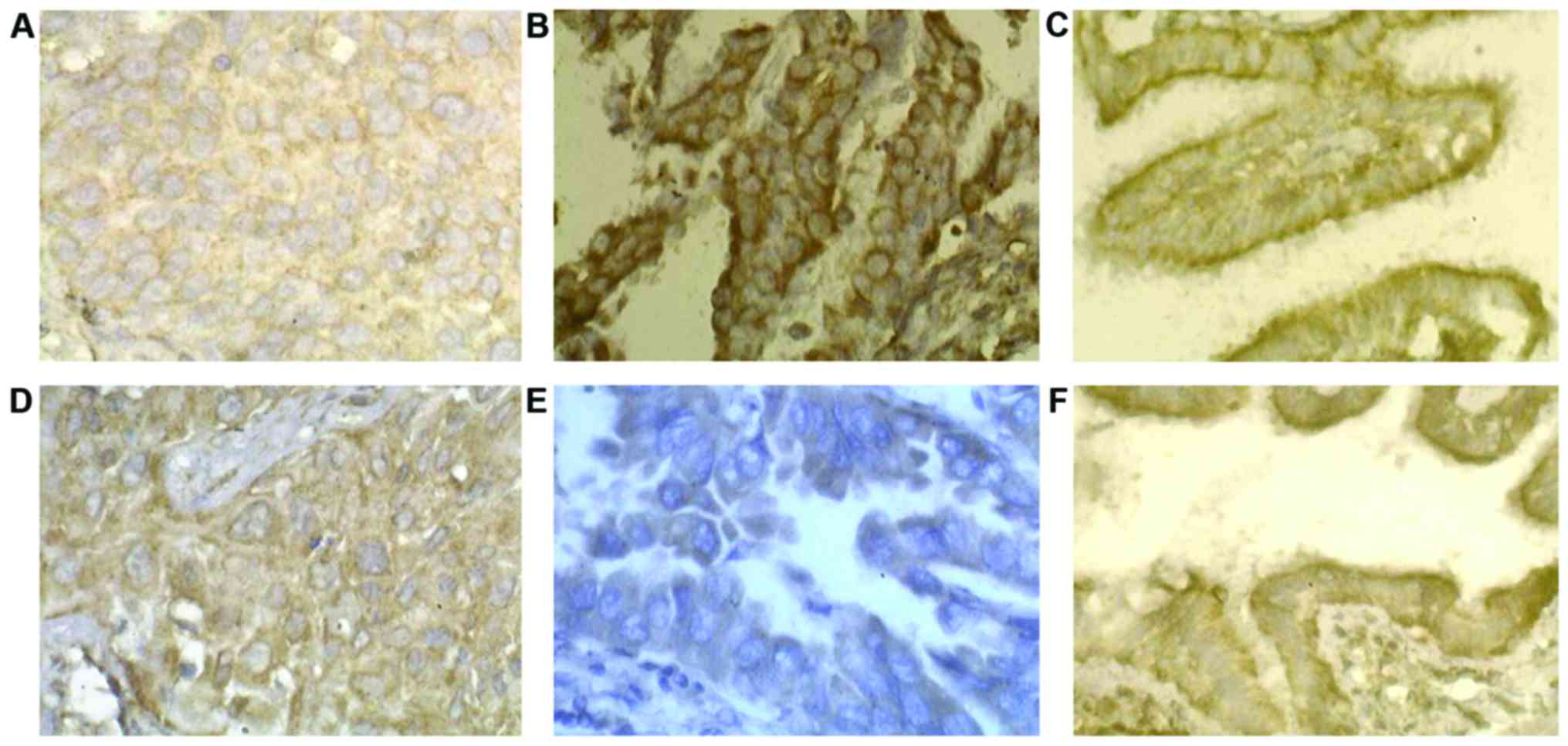
RASSF1A protein was mainly expressed on the membrane
structure of cells. Positive SIRT6 was mainly expressed on the cell
membrane and partially in the cytoplasm. The assessment and
analysis were conducted according to the percentage of staining
cells and staining degree: 10 high-power fields (×400) were
randomly observed for each case, and 100 cells were counted in each
field; the positive cell rate = positive cell count/observed cell
count × 100%. Scoring standards of positive cell rate: ≤10% for 0
point, 11–25% for 1 point, 26–50% for 2 points, 51–75% for 3
points, and >75% for 4 points. Staining degree: yellow, 1 point;
brown yellow, 2 points; and dark brown 3 points; the scores of
positive cell rate and staining degree were multiplied to obtain
the final score: 0 point for negative (−), 1–4 points for weakly
positive (+), 5–8 points for moderately positive (++) and 9–12
points for strongly positive (+++). In the analysis, (−) and (+)
were recognized as the low expression, and (++) and (+++) were
recognized as the high expression.
Statistical analysis
SPSS 18.0 software (SPSS, Inc., Chicago, IL, USA)
was used for data processing. The χ2 test was used for
intergroup comparison of enumeration data. Spearman rank
correlation was used for the correlation analysis. Kaplan-Meier
analysis was used for survival data, the survival curves were
drawn, and the differences were detected by log-rank test. COX risk
model was used for analysis of prognostic factors. P<0.05
suggested that the difference was statistically significant.
Results
Comparison of the positive expression
of RASSF1A and SIRT6 between the two groups
The positive expression rates of RASSF1A and SIRT6
in NSCLC group were lower than those in the normal group
(P<0.01) (Table I). In both
groups, RASSF1A was mainly expressed on membrane structure (cell or
nuclear membrane) and SIRT6 was expressed on the cell membrane; the
positive expression of RASSF1A and SIRT6 was high expressioned in
the normal group (Fig. 1).
 | Table I.Comparison of positive expressions of
RASSF1A and SIRT6 between two groups. |
Table I.
Comparison of positive expressions of
RASSF1A and SIRT6 between two groups.
| Group | n | RASSF1A (%) | SIRT6 (%) |
|---|
| NSCLC | 122 | 68 (55.74) | 64 (52.46) |
| NOR | 122 | 103 (84.43) | 101 (82.49) |
| χ2 |
| 23,746 | 25,537 |
Relationship between expressions of
RASSF1A and SIRT6 and clinicopathological features of patients in
NSCLC group
The differences in expression intensity of RASSF1A
and SIRT6 had no statistical significance between genders, ages,
smoking habits, tumor sites and maximum tumor diameters. The
differences in expression intensity of RASSF1A in NSCLC tissues had
statistical significance under different pathological patterns of
the tumor, tumor differentiation degrees and lymph node metastases.
The differences in expression intensity of SIRT6 in NSCLC tissues
had statistical significance under the tumor differentiation
degrees, TNM stages and lymph node metastases (Table II).
 | Table II.Comparison of the expressions of
RASSF1A and SIRT6 between different clinicopathological
characteristic groups of NSCLC. |
Table II.
Comparison of the expressions of
RASSF1A and SIRT6 between different clinicopathological
characteristic groups of NSCLC.
|
|
| RASSF1A | SIRT6 |
|---|
|
|
|
|
|
|---|
| Pathological
characteristic | n | Low expression
(%) | χ2 | Low expression
(%) | χ2 |
|---|
| Sex |
|
| 0.121 |
| 0.537 |
| Male | 89 | 45 (50.56) |
| 54 (60.67) |
|
|
Female | 33 | 17 (51.51) |
| 18 (54.55) |
|
| Age (years) |
|
| 0.345 |
| 0.592 |
| ≤60 | 57 | 31 (54.38) |
| 35 (61.40) |
|
|
>60 | 65 | 32 (49.23) |
| 36 (55.38) |
|
| Smoking |
|
| 0.297 |
| 0.103 |
| Yes | 93 | 48 (51.61) |
| 55 (59.14) |
|
| No | 29 | 16 (55.17) |
| 17 (58.62) |
|
| Tumor site |
|
| 0.134 |
| 0.212 |
| Left | 49 | 25 (51.02) |
| 27 (55.10) |
|
|
Right | 73 | 37 (50.68) |
| 42 (57.53) |
|
| Tumor size (cm) |
|
| 0.023 |
| 0.247 |
| ≤3 | 55 | 28 (50.90) |
| 30 (54.55) |
|
|
>3 | 67 | 34 (50.75) |
| 35 (52.24) |
|
| Pathological
type |
|
| 9.862 |
| 0.751 |
|
Adenocarcinoma | 42 | 13 (30.95) |
| 22 (52.38) |
|
| Squamous
carcinoma | 65 | 38 (58.46) |
| 39 (60.00) |
|
|
Adenosquamous carcinoma | 15 | 11 (73.33) |
| 10 (66.67) |
|
|
Differentiation |
|
| 6.138 |
| 4.619 |
|
High-medium | 76 | 30 (39.47) |
| 36 (47.37) |
|
|
Low | 46 | 32 (69.57) |
| 34 (73.91) |
|
| TNM |
|
| 2.125 |
| 8.176 |
| Stage
I | 48 | 22 (45.83) |
| 22 (45.83) |
|
| Stage
II–III | 74 | 42 (56.76) |
| 49 (66.22) |
|
| Lymph node
metastasis |
|
| 5.739 |
| 5.177 |
|
Yes | 62 | 37 (59.68) |
| 42 (67.74) |
|
| No | 60 | 24 (40.00) |
| 26 (43.33) |
|
Analysis of correlation between
expression of RASSF1A and SIRT6 in NSCLC group
There was a positive correlation between expression
of RASSF1A and SIRT6 in NSCLC group (r=0.532, P<0.01) (Table III).
 | Table III.Correlation of the expression of
RASSF1A and SIRT6 in NSCLC. |
Table III.
Correlation of the expression of
RASSF1A and SIRT6 in NSCLC.
|
| SIRT6 |
|---|
|
|
|
|---|
| RASSF1A | Low expression | High
expression | Total |
|---|
| Low expression | 55 | 12 | 67 |
| High
expression | 18 | 37 | 55 |
| Total | 73 | 49 | 122 |
The relationship between the
expression of RASSF1A and SIRT6 and the prognosis of patients with
NSCLC
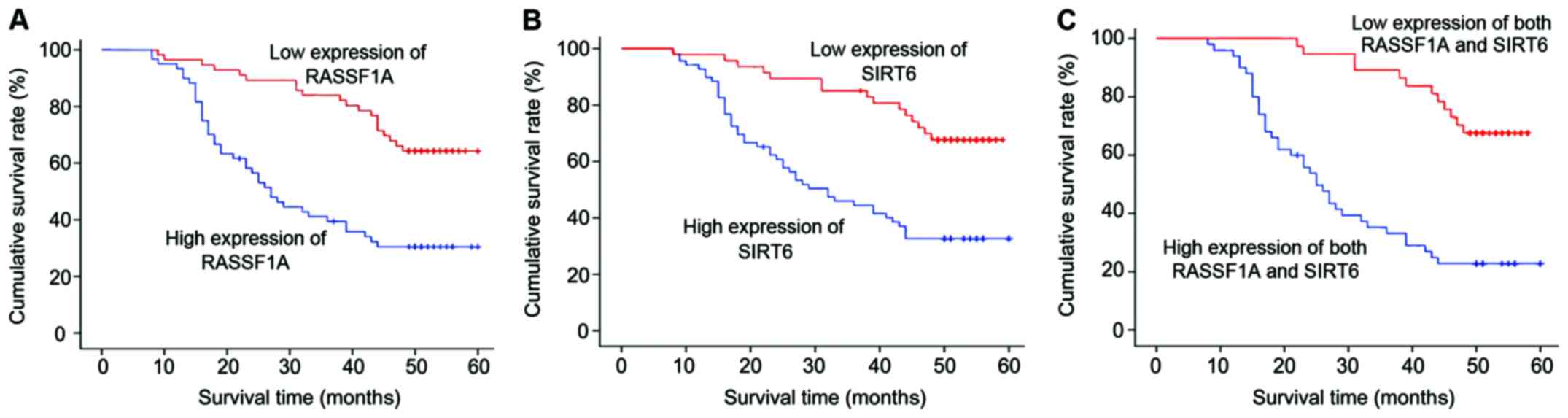
A total of 122 NSCLC patients were followed up for
1–60 months with the median time of 44 months, and 3 cases were
lost to follow-up. The 3-year survival rates of patients with
high-expression RASSF1A and low-expression RASSF1A were 83.82%
(57/68) and 40.74% (22/54), respectively; and the difference had
statistical significance (log-rank χ2=18,992, P<0.01)
(Fig. 2A). The 3-year survival rates
of patients with high-expression of SIRT6 and low-expression of
SIRT6 were 85.71% (42/49) and 45.20% (33/73), respectively; and the
difference had statistical significance (log-rank
χ2=16,680, P<0.01) (Fig.
2B). The 3-year survival rates of patients with high-expression
RASSF1A and high-expression of SIRT6, and patients with
low-expression of RASSF1A and low-expression of SIRT6 were 89.19%
(33/37) and 34.55% (19/55), respectively; and the difference had
statistical significance (log-rank χ2=24,385, P<0.01)
(Fig. 2C).
Multivariate COX regression model
analysis
COX proportional hazard regression model was used
for analysis with the gender (male=1, female=2), age, pathological
pattern, tumor differentiation degree, maximum tumor diameter,
whether there was lymph node metastasis (yes=1, no=2) and whether
RASSF1A and SIRT6 were lowly expressed (yes = 1, no = 2) as
independent variables and the survival time as dependent variable.
The results showed that the low expressions of RASSF1A and SIRT6
and lymph node metastasis were the risk factors affecting the
prognosis of NSCLC patients (Table
IV).
 | Table IV.COX proportional hazards model for
various factors related to prognosis in patients with NSCLC. |
Table IV.
COX proportional hazards model for
various factors related to prognosis in patients with NSCLC.
| Variable | β | SE | Wald
χ2 | P-value | RR | RR 95% CI |
|---|
| Age | −0.131 | 0.252 | 0.147 | 0.673 | 0.859 | 0.541–1.515 |
| Sex | 0.014 | 0.364 | 2.005 | 0.172 | 1.716 | 0.883–3.248 |
|
Differentiation | 0.459 | 0.372 | 0.018 | 0.947 | 0.978 | 0.495–1.897 |
| Lymph node
metastasis | 1.411 | 0.327 | 20.523 | <0.001 | 4.012 | 2.372–7.586 |
| Pathological
type | −0.119 | 0.245 | 0.566 | 0.517 | 0.914 | 0.613–1.317 |
| Tumor size | −0.034 | 0.236 | 0.047 | 0.796 | 0.885 | 0.512–1.526 |
| Common low
expression | 1.314 | 0.362 | 19.021 | <0.001 | 3.872 | 1.971–6.315 |
Discussion
RASSF1A is a relatively unique molecule in the RAS
family. The expression of RASSF1A is usually reduced in the
development process of malignant tumors (8). The in vitro studies have also
shown that RASSF1A can inhibit the proliferation, survival,
invasion and metastasis of tumor cells (9–11). Chen
et al knocked out the RASSF1A genes in non-tumor cells in
bronchus via RNA interference, and found that the decreased
expression of RASSF1A could promote cell migration and invasion
(12). Huang et al found that
the expression quantity of RASSF1A in lung cancer was significantly
decreased with the increase of lung cancer infiltration (13), and the expression loss of RASSF1A was
significantly associated with the high stage, high infiltration,
poor differentiation and high proliferation index of lung cancer,
and the proliferation and growth of A549 cells with RASSF1A
overexpression were significantly decreased (14–16).
Pastuszak-Lewandoska et al studied and showed that 64 out of
112 cases of primary NSCLC had no expression or low expression of
RASSF1A, which was consistent with the results of this study
(17).
In this study, RASSF1A was highly expressed in
normal lung tissues and significantly decreased in NSCLC tissues,
and its expression intensity was different under different
pathological patterns of tumor, tumor differentiation degrees and
lymph node metastases (17). The
positive expression of SIRT6 has the function of inhibiting tumor
metastasis (18); the decreased
expression or expression loss of SIRT6 and the decreased cell
adhesion cause the infiltrative growth of cells to the peripheral
region (7,19,20); once
the necessary conditions for metastasis are obtained, cells can get
out of the primary lesion, followed by invasion and metastasis.
In recent years, the studies on lung cancer and
breast cancer, papillary thyroid carcinoma, bladder, prostate,
colorectal and nasopharyngeal cancer have confirmed that the
decreased expression of SIRT6 was significantly correlated with the
tumor differentiation, invasion and metastasis (21–25). In
this study, SIRT6 expression was significantly decreased in most of
the NSCLC tissues, and its expression intensity was different in
different TNM stages, tumor differentiation degrees and lymph node
metastases. The results of this study showed that the high or low
expressions of RASSF1A and SIRT6 occur easily in patients with
adenosquamous carcinoma, poor differentiation, high stage and lymph
node metastasis, and the low expressions of RASSF1A and SIRT6 are
the risk factors of poor prognosis of NSCLC patients. The
expression of RASSF1A and SIRT6 in NSCLC tissues have a better
correlation and consistency, suggesting that RASSF1A and SIRT6 play
similar roles in the signal transduction pathway promoting the
occurrence and infiltration of the tumor.
The low or no expression of RASSF1A in lung cancer
may be mainly caused by the low acetylation of histones, and the
significantly low expression of RASSF1A can be seen in lung cancer
cell lines treated with histone deacetylase inhibitors. The low
expression of RASSF1A can promote the migration and infiltration of
bronchial epithelial cells, which activates the
phosphatidylinositol 3-kinase (PI3K)-Akt signaling pathway mainly
through the activation of serine/threonine protein kinase (Akt).
Thaler et al found that RASSF1A deletion could promote
tumorigenesis and tumor cell growth, and promote the occurrence of
Akt signaling pathway in breast cancer cells (26). Romano et al proposed that
RASSF1A plays an important role in the migration and budding of
endothelial cells and the formation of blood capillaries, and its
partial mechanism is the inhibition of Ras/ROCK signaling pathway
(27).
Thus, it can be seen that the expression loss of
RASSF1A may be one of the features of lung cancer cell
infiltration, and its mechanism may be related to the activation of
PI3K/Akt signaling pathway. Studies have also found that SIRT6 has
an effect on tumor cell proliferation through mediating the
activation effect of epidermal growth factor receptor on PI3K/Akt
(28). SIRT6 inhibits the
proliferation and infiltration of NSCLC cells, which is realized
possibly by downregulating the expression of Raf/MEK/ERK. When Raf
genes are knocked out, the proliferation and infiltration
capabilities of NSCLC cells are significantly decreased. It was
observed that RASSF1A and SIRT6, to a certain extent, have the same
effects in the signal transduction pathway of tumor occurrence and
development.
References
|
1
|
Leong D, Rai R, Nguyen B, Lee A and Yip D:
Advances in adjuvant systemic therapy for non-small-cell lung
cancer. World J Clin Oncol. 5:633–645. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jing W, Li N, Wang Y, Liu X, Liao S, Chai
H and Tu J: The prognostic significance of long noncoding RNAs in
non-small cell lung cancer: A meta-analysis. Oncotarget.
8:3957–3968. 2016.
|
|
3
|
Ettinger DS, Wood DE, Akerley W, Bazhenova
LA, Borghaei H, Camidge DR, Cheney RT, Chirieac LR, DAmico TA,
Dilling TJ, et al: NCCN guidelines insights: Non-small cell lung
cancer, version 4.2016. J Natl Compr Canc Netw. 14:255–264. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Douillard JY, Lehur PA, Vignoud J,
Blottière H, Maurel C, Thedrez P, Kremer M and Le Mevel B:
Monoclonal antibodies specific immunotherapy of gastrointestinal
tumors. Hybridoma. 5 Suppl 1:S139–S149. 1986.PubMed/NCBI
|
|
5
|
Dallol A, Agathanggelou A, Tommasi S,
Pfeifer GP, Maher ER and Latif F: Involvement of the RASSF1A
tumor suppressor gene in controlling cell migration. Cancer Res.
65:7653–7659. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Deng ZH, Zhou JH, Cao HQ, Sheng M and Weng
JF: Proliferation inhibition of human lung adenocarcinoma cell line
A549 transfected by RASSF1A gene. J Cent South Univ (Med
Sci). 30:193–196. 2005.
|
|
7
|
Han Z, Liu L, Liu Y and Li S: Sirtuin
SIRT6 suppresses cell proliferation through inhibition of Twist1
expression in non-small cell lung cancer. Int J Clin Exp Pathol.
7:4774–4781. 2014.PubMed/NCBI
|
|
8
|
Fukatsu A, Ishiguro F, Tanaka I, Kudo T,
Nakagawa K, Shinjo K, Kondo Y, Fujii M, Hasegawa Y, Tomizawa K, et
al: RASSF3 downregulation increases malignant phenotypes of
non-small cell lung cancer. Lung Cancer. 83:23–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Avruch J, Praskova M, Ortiz-Vega S, Liu M
and Zhang XF: Nore1 and RASSF1 regulation of cell proliferation and
of the MST1/2 kinases. Methods Enzymol. 407:290–310. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dubois F, Keller M, Calvayrac O, Soncin F,
Hoa L, Hergovich A, Parrini MC, Mazières J, Vaisse-Lesteven M,
Camonis J, et al: RASSF1A suppresses the invasion and metastatic
potential of human non-small cell lung cancer cells by inhibiting
YAP activation through the GEF-H1/RhoB pathway. Cancer Res.
76:1627–1640. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Whang YM, Park KH, Jung HY, Jo UH and Kim
YH: Microtubule-damaging agents enhance RASSF1A-induced cell death
in lung cancer cell lines. Cancer. 115:1253–1266. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen K, Li BK, Xu K, Xu A, Liu C, Zheng S,
Xu Y, Jia C, Liu Q, Li Η, et al: Effect of stable DNA
methyltransferase 3b knockdown on proliferation and apoptosis in
bladder cancer cells in vitro. Nan Fang Yi Ke Da Xue Xue Bao.
35:1524–1529. 2015.(In Chinese). PubMed/NCBI
|
|
13
|
Huang YZ, Wu W, Wu K, Xu XN and Tang WR:
Association of RASSF1A promoter methylation with lung cancer risk:
A meta-analysis. Asian Pac J Cancer Prev. 15:10325–10328. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Fu L and Zhang S: RASSF1A promotes
apoptosis and suppresses the proliferation of ovarian cancer cells.
Int J Mol Med. 33:1153–1160. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ko E, Lee BB, Kim Y, Lee EJ, Cho EY, Han
J, Shim YM, Park J and Kim DH: Association of RASSF1A and p63 with
poor recurrence-free survival in node-negative stage I–II non-small
cell lung cancer. Clin Cancer Res. 19:1204–1212. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dittfeld C, Richter AM, Steinmann K,
Klagge-Ulonska A and Dammann RH: The SARAH domain of RASSF1A and
its tumor suppressor function. Mol Biol Int. 2012:1967152012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Pastuszak-Lewandoska D, Kordiak J,
Migdalska-Sęk M, Czarnecka KH, Antczak A, Górski P, Nawrot E,
Kiszałkiewicz JM, Domańska D and Brzeziańska-Lasota E: Quantitative
analysis of mRNA expression levels and DNA methylation profiles of
three neighboring genes: FUS1, NPRL2/G21 and
RASSF1A in non-small cell lung cancer patients. Respir Res.
16:762015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bai L, Lin G, Sun L, Liu Y, Huang X, Cao
C, Guo Y and Xie C: Upregulation of SIRT6 predicts poor prognosis
and promotes metastasis of non-small cell lung cancer via the
ERK1/2/MMP9 pathway. Oncotarget. 7:40377–40386. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Azuma Y, Yokobori T, Mogi A, Altan B,
Yajima T, Kosaka T, Onozato R, Yamaki E, Asao T, Nishiyama M, et
al: SIRT6 expression is associated with poor prognosis and
chemosensitivity in patients with non-small cell lung cancer. J
Surg Oncol. 112:231–237. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Cai Y, Sheng ZY and Liang SX:
Radiosensitization effect of overexpression of adenovirus-mediated
SIRT6 on A549 non-small cell lung cancer cells. Asian Pac J Cancer
Prev. 15:7297–7301. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bae JS, Park SH, Jamiyandorj U, Kim KM,
Noh SJ, Kim JR, Park HJ, Kwon KS, Jung SH, Park HS, et al:
CK2α/CSNK2A1 phosphorylates SIRT6 and is involved in the
progression of breast carcinoma and predicts shorter survival of
diagnosed patients. Am J Pathol. 186:3297–3315. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bhardwaj A and Das S: SIRT6 deacetylates
PKM2 to suppress its nuclear localization and oncogenic functions.
Proc Natl Acad Sci USA. 113:E538–E547. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Demir IE, Ceyhan GO and Friess H:
Epigenomic therapies: The potential of targeting SIRT6 for the
treatment of pancreatic cancer. Expert Opin Ther Targets. 21:1–3.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lee N, Ryu HG, Kwon JH, Kim DK, Kim SR,
Wang HJ, Kim KT and Choi KY: SIRT6 depletion suppresses tumor
growth by promoting cellular senescence induced by DNA damage in
HCC. PLoS One. 11:e01658352016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wolf K and Strand S: Assessing the histone
deacetylase activity of SIRT6 in primary murine hepatocytes via
proximity ligation assay. Methods Mol Biol. 1510:149–158. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Thaler S, Hähnel PS, Schad A, Dammann R
and Schuler M: RASSF1A mediates p21Cip1/Waf1-dependent
cell cycle arrest and senescence through modulation of the
Raf-MEK-ERK pathway and inhibition of Akt. Cancer Res.
69:1748–1757. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Romano D, Matallanas D, Weitsman G,
Preisinger C, Ng T and Kolch W: Proapoptotic kinase MST2
coordinates signaling crosstalk between RASSF1A, Raf-1, and Akt.
Cancer Res. 70:1195–1203. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Sundaresan NR, Vasudevan P, Zhong L, Kim
G, Samant S, Parekh V, Pillai VB, Ravindra PV, Gupta M, Jeevanandam
V, et al: The sirtuin SIRT6 blocks IGF-Akt signaling and
development of cardiac hypertrophy by targeting c-Jun. Nat Med.
18:1643–1650. 2012. View
Article : Google Scholar : PubMed/NCBI
|