Introduction
Colorectal cancer is the fourth most common type of
cancer in males and the third most common type of cancer in females
worldwide, and in numerous developed countries it is the second
leading cause of cancer-associated mortality (1). In addition, colon cancer is a major
cause of mortality in Japan (2). An
aging population and an increased life expectancy worldwide have
led to an increased incidence rate of colorectal cancer in elderly
patients, for whom treatment is often complicated (3).
The predicted mortality and type of radical surgery
should be taken into consideration when considering surgical
options for elderly patients, since elderly patients have an
increased number of preoperative risk factors compared with younger
patients. Therefore, minimally invasive surgery with a limited
number of risk factors is important for elderly patients.
Single-incision laparoscopic surgery (SILS) is a more recent
innovation proposed to further the outcomes of multi-port
laparoscopy (4). SILS was first
reported in 1999 for cholecystectomy and then applied to colorectal
resection in previous studies (4–6). SILS has
been successfully used as a method for colectomy (7). However, the feasibility of SILS in
elderly patients with colon cancer has not been previously
demonstrated, to the best of our knowledge. The purpose of the
present retrospective study was to elucidate the feasibility of
SILS for elderly patients.
Materials and methods
Patient information
Between January 2011 and December 2014, 100 patients
underwent SILS for the treatment of colon cancer at Yao Municipal
Hospital (Yao, Osaka, Japan). The present study reports the results
of a retrospective case controlled study of these 100 patients who
underwent elective surgical intervention for the treatment of colon
cancer. The elderly group consisted of 56 patients who were ≥70
years (elderly group; mean age, 76.6 years). The control group
consisted of 44 patients, all <70 years (mean age, 61.4
years).
All procedures were performed by colorectal surgeons
who were experienced in multi-port laparoscopic surgery or standard
laparoscopic surgery (8). Data on
patient demographics, body mass index (BMI), American Society of
Anesthesiologists physical status (ASA-PS) classification (9), Onodera's prognostic nutritional index
(PNI) (10), tumor location, tumor
size, personal history of surgery, surgery duration, estimated
blood loss, number of lymph nodes harvested, length of the resected
margin, conversion into open surgery, insertion of an additional
port, perioperative complications, morbidity and the length of
hospital stay were compared between the elderly and control groups.
Onodera et al (10) first
reported the validity of Onodera's PNI to predict the prognosis of
189 gastrointestinal surgical patients. Onodera's PNI is an
equation which takes into account the levels of serum albumin and
total lymphocyte count. Onodera's PNI can be applied rapidly in a
large number of patients. Validation of Onodera's PNI has been
applied for patients with colon cancer (11).
Surgical technique
The surgery was performed as described in a previous
study (12). Under general
anesthesia, the patient was placed in the modified lithotomy
position. A wound protector (Lap protector LP™; Hakkou Shoji,
Chikuma, Nagano, Japan) was inserted through a 30-mm transumbilical
incision. A single port access device (EZ-access™, Hakkou Shoji)
was then mounted to the wound protector and three 5-mm ports were
placed (Fig. 1). The surgical
procedures and instruments used were the same as those used for
standard laparoscopic surgery with a flexible 5-mm scope (Olympus
Medical Systems Corp., Tokyo, Japan).
An additional incision or trocar port was placed if
necessary, in order to complete the procedure, and conversion into
open laparotomy was maintained as an option. The decision to use an
additional trocar or to convert into open laparotomy was subject to
the opinion of the surgeon performing the procedure. For
lymphadenectomy, a complete mesocolic excision (CME) with central
vascular ligation (CVL) was performed. The final incision was
extended to a length comparable with the size of the specimen.
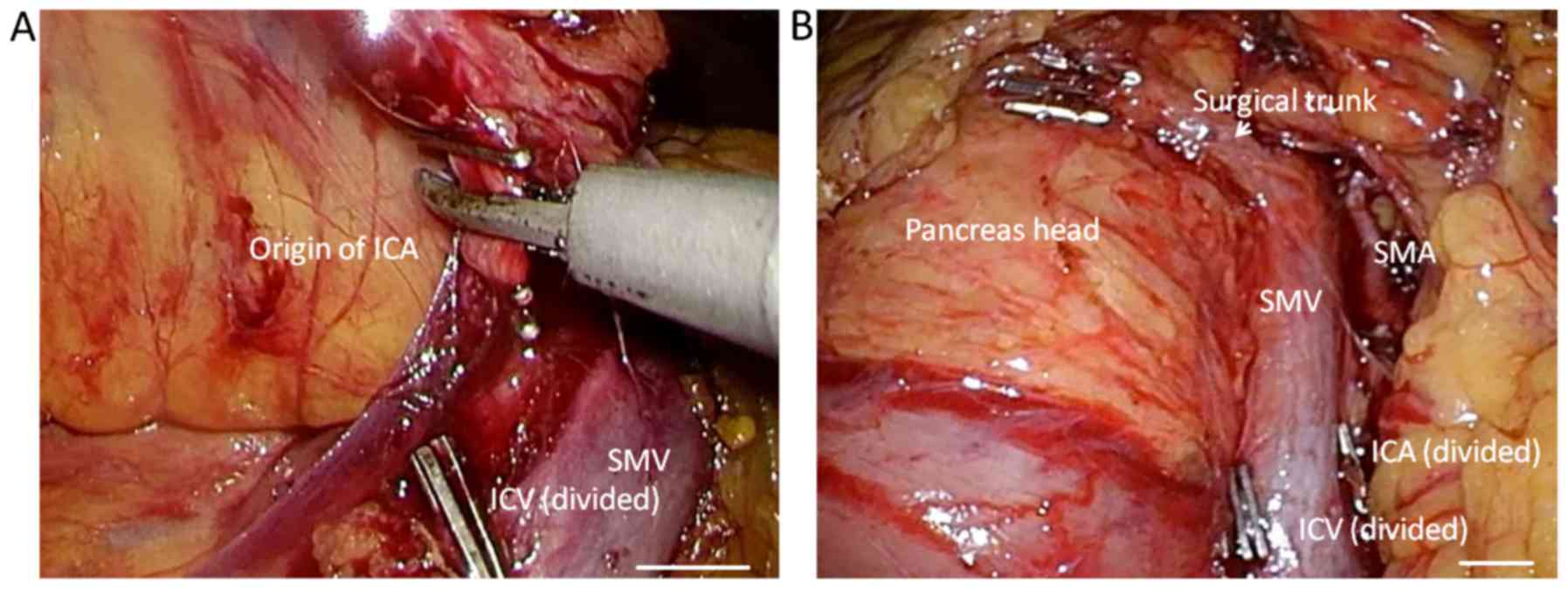
Right hemicolectomy
For the right hemicolectomy, the patient was placed
in the Trendelenburg semi-left lateral position. The surgeon and
camera operator stood on the left side of the patient. The
procedure was performed via an inferior approach, with the initial
peritoneal dissection occurring between the mesoileum and the
retroperitoneum. Following mesocolic plane resection, the duodenum
and pancreas were sufficiently exposed, and the ileocolic, right
colic (if necessary) and middle colic vessels were ligated and
dissected between clips at their origin to allow CME and CVL
(Fig. 2). Subsequent to the
dissection of the greater omentum, the hepatic flexure was
mobilized. The specimen was retrieved via the transumbilical
incision, and an extracorporeal functional end-to-end anastomosis
was subsequently performed.
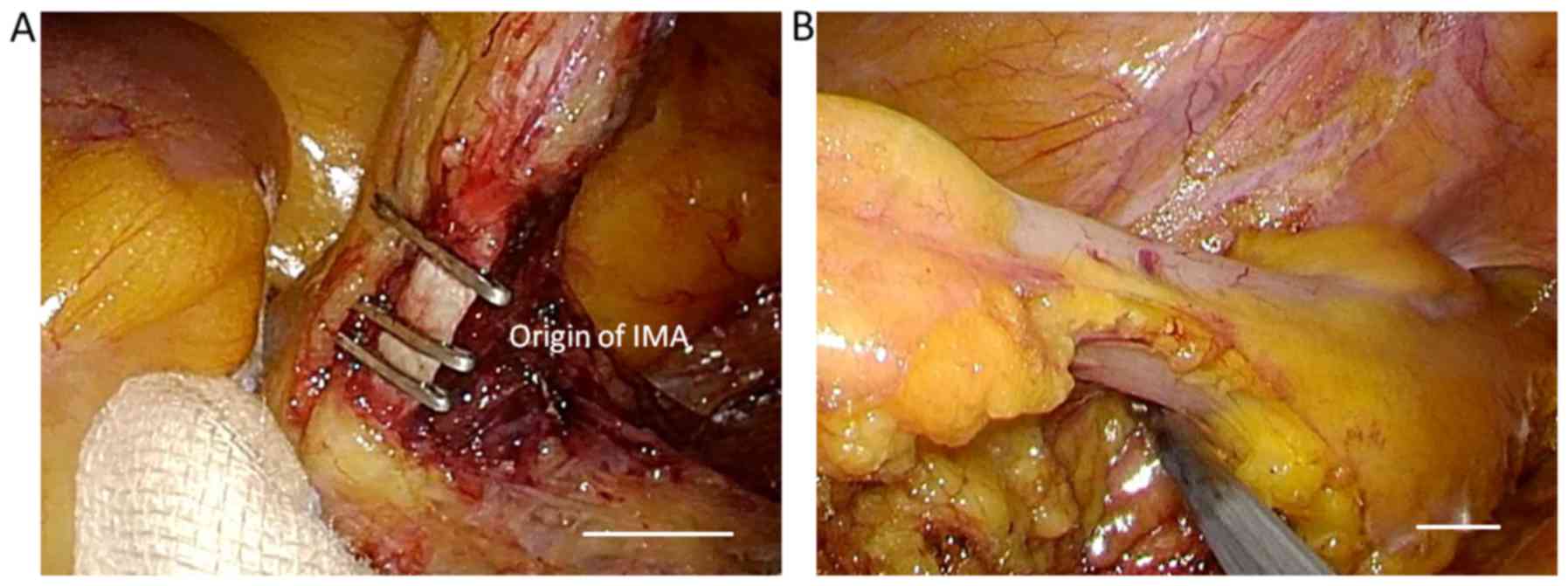
Sigmoidectomy and anterior
resection
The patient was placed in the Trendelenburg
semi-right lateral position. The surgeon and camera operator stood
on the right side of the patient. The procedure was performed via a
standard medial-to-lateral approach. The inferior mesenteric artery
and the inferior mesenteric vein were skeletonized, clipped, and
divided for CME and CVL (Fig. 3).
Surgeons then dissected downwards from the mesenteric window to the
pelvis. The sigmoid colon up to the splenic flexure was then
mobilized. The descending colon and sigmoid colon was pulled
anteromedially to ensure preservation of the left ureter and
gonadal vessels. The fat surrounding the rectum for >50 mm
distal to the lesion was dissected and subsequently transected
normally using an endoscopic linear stapler (Endo GIA™; Covidien
LLC, Mansfield, MA, USA) with a purple cartridge inserted from the
umbilical port with a 12-mm EZ Link (Hakko Co. Ltd., Nagano,
Japan). The specimen was retrieved through the umbilical incision,
and the double stapling technique was applied for anastomosis.
Statistical analysis
Statistical analysis was performed using SPSS
software (version 14.0; SPSS, Inc., Chicago, IL, USA). All
variables were evaluated using a χ2 test or Student's
t-test, as appropriate. P<0.05 was considered to indicate a
statistically significant difference.
Results
In the elderly patient group and the control group,
the primary tumor sites included the cecum (n=7; n=4), ascending
colon (n=24; n=6), descending colon (n=1; n=2), sigmoid colon
(n=14; n=27) and the rectosigmoid colon (n=10; n=5), respectively
(Table I). The primary tumor location
in the elderly group was more frequently in the right colon. In the
control group, the primary tumor location was more frequently in
the left colon.
 | Table I.Characteristics of patients with colon
cancer. |
Table I.
Characteristics of patients with colon
cancer.
|
| Total | Right | Left |
|---|
|
|
|
|
|
|---|
| Characteristics | Elderly, n=56 | Control, n=44 | P-value | Elderly, n=31 | Control, n=10 | P-value | Elderly, n=25 | Control, n=34 | P-value |
|---|
| Age, years | 76.6±4.7 | 61.4±7.2 | <0.05 | 77.5±7.9 | 62.1±5.6 | 0.56 | 75.4±7.7 | 61.2±7.6 | 0.30 |
| Sex, n |
|
|
|
|
|
|
|
|
|
| Male | 27 | 21 | 0.86 | 13 | 5 | 0.41 | 14 | 16 | 0.60 |
|
Female | 29 | 23 |
| 18 | 5 |
| 11 | 18 |
|
| BMI,
kg/m2 | 22.8±3.7 | 23.2±4.0 | 0.32 | 23.3±3.0 | 23.2±2.0 | 0.99 | 22.1±2.3 | 23.2±4.4 | 0.60 |
| ASA physical
status |
|
|
|
|
|
|
|
|
|
| 1 | 5 | 6 | 0.42 | 3 | 2 | 0.58 | 2 | 5 | <0.05 |
| 2 | 43 | 35 |
| 25 | 8 |
| 18 | 26 |
|
| 3 | 8 | 3 |
| 3 | 0 |
| 5 | 3 |
|
| Prior surgery, n | 20 | 13 | 0.73 | 11 | 4 | 0.67 | 9 | 9 | 0.67 |
| Onodera's PNI | 38.3 | 49.8 |
| 37.5 | 49.5 | <0.05 | 39.2 | 49.9 | <0.05 |
| Tumor location,
n |
|
|
|
|
|
|
|
|
|
|
Cecum | 6 | 4 |
|
|
|
|
|
|
|
|
Ascending colon | 25 | 6 |
|
|
|
|
|
|
|
|
Transvers colon | 0 | 0 | <0.05 |
|
|
|
|
|
|
|
Descending colon | 1 | 2 |
|
|
|
|
|
|
|
| Sigmoid
colon | 14 | 27 |
|
|
|
|
|
|
|
|
Rectosigmoid colon | 10 | 5 |
|
|
|
|
|
|
|
The median BMI of the elderly and control groups
were 22.8±3.7 and 23.2±4.0 kg/m2, respectively. The sex
distribution (P=0.86), history of prior surgery (20 vs. 13;
P=0.73), and ASA-PS (P=0.42) were not significantly different
between the groups. Renal function, respiratory function and
cardiac function were poorer in the elderly group compared with the
control group; however, no significant differences were
identified.
Onodera's PNI was significantly decreased in the
elderly compared with the control group (38.3 vs. 49.8; P<0.05).
For 1 patient (1.8%) in the elderly group, surgery was converted
into laparotomy, since it was not possible to make free working
space in the abdominal cavity due to bone deformities caused by
spondylocase. The remaining 99 patients underwent curative
colectomy without conversion into multi-port laparoscopic surgery
or open surgery. In the elderly group, 31 patients underwent right
hemicolectomy and 25 underwent sigmoid colectomy and anterior
resection. In the control group, 10 patients underwent right
hemicolectomy and 34 underwent sigmoid colectomy and anterior
resection. The mean skin incision length in the elderly and control
group was 34.0±5.9 and 35.5±6.8 mm, respectively. The mean surgical
duration in the elderly and control group was 219.5±73.5 and
201.4±76.5 min, respectively, and blood loss was 32.2±74.5 and
36.1±90.2 ml, respectively. The mean number of harvested lymph
nodes in the elderly and control group was 21.8±24.3 and 22.5±11.3,
respectively. No intraoperative complications occurred in either
group.
Postoperative complications included an anastomotic
leak, wound infection, pneumonia, deep vein thrombosis, dysuria,
ileus and urinary tract infections. Postoperative complications
occurred in 6 cases (10.7%) in the elderly group and 3 cases
(6.81%) in the control group. In the elderly group, 14 patients
(25.0%) were >80 years old; however, serious complications were
not observed in these patients, and delirium was not observed in
any patient from either group. The time until the first production
of feces following surgery in the elderly and control group was
4.11±4.60 and 3.80±1.40 days, respectively. The patients were
discharged following a mean period of 9.60±12.5 and 7.30±3.0 days
postoperatively in the elderly and control groups, respectively
(Table II). No mortality occurred in
any patient from either group, and there was no readmission within
30 days postoperatively. Regarding oncological features, the number
of resected lymph nodes and resection margins and tumor size did
not differ significantly between the elderly and control groups.
There were also no recurrences in either group <1 year following
surgery, according to follow-up physical examinations every 3
months and computed tomography scans performed every 6 months.
 | Table II.Surgical outcomes. |
Table II.
Surgical outcomes.
|
| Total | Right | Left |
|---|
|
|
|
|
|
|---|
| Surgical
feature | Elderly, n=56 | Control, n=44 | P-value | Elderly, n=31 | Control, n=10 | P-value | Elderly, n=25 | Control, n=34 | P-value |
|---|
| Surgical duration,
min | 219.5±73.5 | 201.4±76.5 | 0.43 | 221.3±23.5 | 209.7±63.3 | 0.89 | 217.2±23.6 | 199.2±80.6 | 0.68 |
| Estimated blood
loss, ml | 32.18±74.5 | 36.07±90.2 | 0.10 | 47.0±10.6 | 77.2±15.2 | 0.50 | 14.4±34.5 | 24.8±64.0 | 0.46 |
| Final incision,
mm | 34.0±5.9 | 35.5±6.8 | 0.16 | 34.2±3.5 | 37.2±9.1 | 0.80 | 33.8±3.5 | 35.1±6.2 | 0.83 |
| Conversion of
laparotomy, n | 1 | 0 | – | 0 | 0 | – | 1 | 0 | – |
| Additional trocars
required, n | 1 | 0 | – | 0 | 0 | – | 1 | 0 | – |
| Length of hospital
stay, days | 9.6±12.5 | 7.3±3.0 | 0.23 | 7.7±9.4 | 6.1±0.8 | 0.62 | 12.0±15.6 | 7.6±3.2 | 0.12 |
| Days until feces
following surgery | 4.11±4.6 | 3.8±1.4 | 0.71 | 4.0±4.2 | 3.9±0.8 | 0.94 | 4.2±5.1 | 3.8±1.6 | 0.65 |
| Complications,
n | 6 | 3 |
| 3 | 0 |
| 3 | 3 |
|
| Wound
infection | 1 | 0 |
| 1 | 0 |
| 0 | 0 |
|
|
Anastomotic leakage | 1 | 1 |
| 0 | 0 |
| 1 | 1 |
|
|
Ileus | 1 | 1 | 0.78 | 0 | 0 | – | 1 | 1 | 0.94 |
|
Urinary | 1 | 1 |
| 0 | 0 |
| 1 | 1 |
|
| Other |
|
Pneumonia | 1 | 0 |
| 1 | 0 |
| 0 | 0 |
|
|
Thrombosis | 1 | 0 |
| 1 | 0 |
| 0 | 0 |
|
| Readmission within
30 days of surgery, n | 0 | 1 | – | 0 | 0 | – | 0 | 1 | – |
| Harvested lymph
nodes, n | 21.8±24.3 | 22.5±11.3 | 0.87 | 22.8±2.5 | 28.8±1.7 | 0.51 | 20.7±2.3 | 20.8±8.8 | 0.98 |
| Margin of the
specimen, mm |
| PM | 100.7±128.2 | 90.6±73.4 | 0.64 | 132.7±15.8 | 154.3±11.8 | 0.71 | 62.3±7.3 | 73.2±4.3 | 0.48 |
| DM | 83.1±101.7 | 69.3±38.6 | 0.41 | 94.7±11.8 | 58.4±12.8 | 0.37 | 69.2±7.9 | 72.3±4.3 | 0.85 |
| Tumor size, mm | 44.1±50.5 | 36.4±27.2 | 0.37 | 47.1±54.7 | 45.4±31.7 | 0.93 | 40.6±46.0 | 33.9±25.9 | 0.49 |
Discussion
Currently, numerous surgeons have adopted
laparoscopic techniques. The oncological safety of laparoscopic
colectomy in patients with cancer has been demonstrated in
randomized trials (13). As a result,
laparoscopic surgery has steadily become a safe and practical
treatment option even for malignant diseases of the colon and
rectum.
The number of elderly patients with colorectal
cancer requiring surgery is increasing annually, due to an increase
in life expectancy and therefore an increasingly elderly
population. According to the census figures in 2010, the average
lifespan is 79.64 years for males and 86.39 years for females in
Japan (14). The proportion of
elderly individuals who are ≥70 years in Japan is 16.4%, and this
number is increasing (15). The
number of cases of elderly patients requiring surgery is expected
to increase. It is clear that, as patients age, there is an
associated increase in comorbid conditions that often complicate
the perioperative management of elderly patients who undergo major
surgery.
The most important part of surgical practices for
the treatment of elderly patients with a malignant disease is to
balance the invasiveness of treatment and radical cure, which are
often conflicting. Highly invasive surgery can only be performed in
patients with a high tolerability. Previous studies indicate that
lymph node dissection is less common in elderly patients and that
there is a tendency to avoid invasive surgery in elderly patients
(16,17). However, to the best of our knowledge,
there is no reported difference in cancer aggressiveness between
younger patients and elderly patients. Previous reports indicate
that radical surgery for elderly patients with colorectal cancer
can improve the prognosis (18) and
that radical surgery should be performed for elderly patients as it
is for younger patients, provided that the main organs are
functional (19).
A previous study demonstrated that multi-port
laparoscopic-assisted colectomy in elderly patients is safe and
feasible (6), and has numerous
benefits over open colectomy since it appears to be less
physiologically stressful compared with conventional open
laparotomy. Multi-port laparoscopic assisted colectomy should be
considered as the preferred surgical approach in the management of
numerous colorectal diseases for appropriately selected elderly
patients (6).
At Yao Municipal Hospital, it is considered that
less-invasive surgery should be performed in elderly patients as
often as possible while aiming for a radical cure and considering
the functional decline of the main organs. As a result, the authors
introduced a multi-port laparoscope-assisted surgery in 2009 in the
Department of Surgery. Furthermore, according to the theory of
reduced-port surgery (20–23), single-incision laparoscopic colectomy
(SILC) was introduced to Yao Municipal Hospital in July 2013 with
the aim of providing a less-invasive surgical technique.
Reduced port surgery aims to decrease the size and
number of ports to preserve the view afforded by the laparoscope
while making the surgery less invasive. Previous studies have
successfully discussed the advantages of decreasing the number of
laparoscopic ports, including improved cosmetic results, decreased
postoperative pain and shorter recovery period; however, there is a
technical complexity to decreased number of ports, including
instrument crowding and insufficient counter traction (20–23).
SILS as a treatment for colon cancer has been
preliminary described by Bucher et al (6), and through additional case reports and
small case series (24–27). Previously, Papaconstantinou et
al (28) described that, when
compared with established laparoscopic techniques, SILC can improve
patient recovery through a decrease in early postoperative pain and
shorter length of hospital stay. However, other than the cosmetic
advantage, the benefits of SILS are controversial.
In the present study, no statistically significant
differences were identified between the short-term outcomes for the
elderly and control groups of patients with colon cancer who
underwent SILS. To the best of our knowledge, the present study is
the first reported case-controlled study investigating colon cancer
and it involved elderly patients (mean age, 76.6 years).
The present study demonstrated that the short-term
outcomes of SILS in elderly (≥70 years) and younger (<70 years)
patients are equivalent (Table II).
The overall rate of morbidity and the number of cases with
postoperative complications were almost equivalent in the two
groups, and the length of hospital stay and the time until first
passing of feces subsequent to surgery did not differ significantly
between the two groups.
It has been reported that Onodera's PNI may be used
as a prognostic factor of colorectal cancer (11). In the present study, Onodera's PNI
score in the elderly patient group was significant lower compared
with the control group (38.3 vs. 49.8; P<0.05), whereas the
frequency of postoperative complications was similar between the
two groups. The results of the present study suggested that SILS in
elderly patients is equivalent to that for younger patients.
With regard to the oncological quality of the
surgery, the number of resected lymph nodes and resection margins
did not differ significantly between the elderly and control
groups. The mean number of removed lymph nodes was between 20.7
(elderly group) and 28.8 (control group), which is consistent with
what has been revealed in other studies (28,29). The
total surgical conversion rate for the 100 patients with colon
cancer was 1.0%, which is consistent with previous studies
(29,30). Therefore, radical surgery may be
performed for elderly patients as it is for younger patients, which
may improve prognosis (17).
The single-incision laparoscopic approach used in
the present study may have contributed to these low complication
rates, and the results of the present study demonstrate that age
alone should not be considered a reason to withhold surgical
treatment from elderly patients regarding morbidity and
mortality.
The results of the present study indicate that SILS
is oncologically feasible, and that a curative procedure for
elderly patients with colon cancer is equivalent to that for
younger patients. These results are consistent with those of
previous studies in the general population. Therefore, it is
considered that these results justify the use of SILS in the
routine treatment of elderly patients with colon cancer.
References
|
1
|
Center MM, Jemal A and Ward E:
International trends in colorectal cancer incidence rates. Cancer
Epidemiol Biomarkers Prev. 18:1688–1694. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
World Cancer Research Fund and American
Institute for Cancer Research Food, Nutrition, Physical Activity
and the Prevention of Cancer, . A Global Perspective. Washington,
DC: American Institute for Cancer Research; 2007
|
|
3
|
Fiscon V, Portale G, Migliorini G and
Frigo F: Laparoscopic resection of colorectal cancer in elderly
patients. Tumori. 96:704–708. 2010.PubMed/NCBI
|
|
4
|
Piskun G and Rajpal S: Transumbilical
laparoscopic cholecystectomy utilizes no incisions outside the
umbilicus. J Laparoendosc Adv Surg Tech A. 9:361–364. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Remzi FH, Kirat HT, Kaouk JH and Geisler
DP: Single-port laparoscopy in colorectal surgery. Colorectal Dis.
10:823–826. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bucher P, Pugin F and Morel P: Single port
access laparoscopic right hemicolectomy. Int J Colorectal Dis.
23:1013–1016. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jacob BP and Salky B; Laparoscopic
colectomy for colon adenocarcinoma, : An 11-year retrospective
review with 5-year survival rates. Surg Endosc. 19:643–649. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hinoi T, Kawaguchi Y, Hattori M, Okajima
M, Ohdan H, Yamamoto S, Hasegawa H, Horie H, Murata K, Yamaguchi S,
et al: Laparoscopic versus open surgery for colorectal cancer in
elderly patients: A multicenter matched case-control study. Ann
Surg Oncol. 22:2040–2250. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Saklad M: Grading of patients for surgical
procedures. Anesthesiol. 2:281–284. 1941. View Article : Google Scholar
|
|
10
|
Onodera T, Goseki N and Kosaki G:
Prognostic nutritional index in gastrointestinal surgery of
malnourished cancer patients. Nippon Geka Gakkai Zasshi.
85:1001–1005. 1984.(In Japanese). PubMed/NCBI
|
|
11
|
Nozoe T, Kohno M, Iguchi T, Mori E, Maeda
T, Matsukuma A and Ezaki T: The prognostic nutritional index can be
a prognostic indicator in colorectal carcinoma. Surg Today.
42:532–535. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tokuoka M, Ide Y, Takeda M, Hashimoto Y,
Matsuyama J, Yokoyama S, Morimoto T, Fukushima Y, Nomura T, Kodama
K and Sasaki Y: Single-incision Plus one port laparoscopic total
mesorectal excision and bilateral pelvic node dissection for
advanced rectal cancer-a medial umbilical ligament approach. Int
Surg. 100:417–422. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lacy AM, García-Valdecasas JC, Delgado S,
Castells A, Taurá P, Piqué JM and Visa J: Laparoscopy-assisted
colectomy versus open colectomy for treatment of non-metastatic
colon cancer: A randomaised trial. Lancet. 359:2224–2229. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Index mundi. http://www.indexmundi.com/facts/japan/life-expectancy-at-birthAugust
17–2016
|
|
15
|
POPULATION AND HOUSEHOLDS OF JAPAN 2010.
http://www.stat.go.jp/english/data/kokusei/2010/poj/mokuji.htmAugust
17–2016
|
|
16
|
Satou S, Yoneda K, Ogata J, Mori M, Wada
T, Sakamoto N, Majima A, Katou K, Aoki T and Koyanagi Y:
Clinicopathological feature and prognosis of colorectal cancer in
elderly-people (75 or more years old). Journal of Japan Society of
Coloproctology. 56:41–47. 2003. View Article : Google Scholar
|
|
17
|
Fujii S, Ishibe A, Ota M, Watanabe K,
Watanabe J, Tatsumi K, Yamagishi S, Ichikawa Y, Ohki S, et al:
Short-term and long-term outcomes of colorectal cancer surgery in
elderly patients (80 years or more) and measures for improving
treatment results. Nippon Daicho Komonbyo Gakkai Zasshi.
66:221–228. 2013.(In Japanese). View Article : Google Scholar
|
|
18
|
Man-I M, Nishisho I, Mishima H, Yagyu T,
Kikkawa N and Tsujinaka T: Risk factors of postoperative
complication and prognostic factors in aged patients with
resectable colorectal carcinomas by using multivariate analysis.
Jpn J Gastroenterol Surg. 35:590–597. 2002. View Article : Google Scholar
|
|
19
|
Nakamura T, Mitomi H, Onozato W, Sato T,
Ikeda A, Naito M, Ogura N, Kamata H, Ooki A and Watanabe M:
Oncological outcomes of laparoscopic surgery in elderly patients
with colon cancer: A comparison of patients 64 years or with those
75 years or older. Hepatogastroenterology. 58:1200–1204. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chen WT, Chang SC, Chiang HC, Lo WY, Jeng
LB, Wu C and Ke TW: Single-incision laparoscopic versus
conventional laparoscopic right hemicolectomy: A comparison of
short-term surgical results. Surg Endosc. 25:1887–1892. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Champagne BJ, Lee EC, Leblanc F, Stein SL
and Delaney CP: Single-incision vs straight laparoscopic segmental
colectomy: A case-controlled study. Dis Colon Rectum. 54:183–186.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Champagne BJ, Papaconstantinou HT, Parmar
SS, Nagle DA, Young-Fadok TM, Lee EC and Delaney CP:
Single-incision versus standard multiport laparoscopic colectomy: A
multicenter, case-controlled comparison. Ann Surg. 255:66–69. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Poon JT, Cheung CW, Fan JK, Lo OS and Law
WL: Single-incision versus conventional laparoscopic colectomy for
colonic neoplasm: A randomized, controlled trial. Surg Endosc.
26:2729–2734. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Takemasa I, Sekimoto M, Ikeda M, Mizushima
T, Yamamoto H, Doki Y and Mori M: Transumbilical single-incision
laparoscopic surgery for sigmoid colon cancer. Surg Endosc.
24:23212010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ramos-Valadez DI, Patel CB, Ragupathi M,
Pickron T Bartley and Haas EM: Single incision laparoscopic right
hemicolectomy: Safety and feasibility in a series of consecutive
cases. Surg Endosc. 24:2613–2616. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hirano Y, Hattori M, Kitamura H, Maeda K,
Douden K and Hashizume Y: Hybrid single-incision laparoscopic
sigmoidectomy: The effective use of small incision. J Laparoendosc
Adv Surg Tech A. 21:625–627. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Katsuno G, Fukunaga M, Nagakari K,
Yoshikawa S, Ouchi M and Hirasaki Y: Single-incision laparoscopic
colectomy for colon cancer: Early experience with 31 cases. Dis
Colon Rectum. 54:705–710. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Papaconstantinou HT, Sharp N and Thomas
JS: Single-incision laparoscopic right colectomy: A case-matched
comparison with standard laparoscopic and hand-assisted
laparoscopic techniques. J Am Coll Surg. 213:72–82. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Keller DS, Flores-Gonzalez JR, Ibarra S
and Haas EM: Review of 500 single incision laparoscopic colorectal
surgery cases - Lessons learned. World J Gastroenterol. 22:659–667.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Veldkamp R, Gholghesaei M, Bonjer HJ,
Meijer DW, Buunen M, Jeekel J, Anderberg B, Cuesta MA, Cuschierl A,
Fingerhut A, et al: Laparoscopic resection of colon Cancer:
consensus of the European Association of Endoscopic Surgery (EAES).
Surg Endosc. 18:1163–1185. 2004. View Article : Google Scholar : PubMed/NCBI
|