Introduction
In the treatment of malignant bone tumors around
joints it is essential to perform a complete resection of tumor
segments and to strive for the functional reconstruction of the
joint (1). Various preoperative
assessments such as computed tomography (CT) and magnetic resonance
imaging (MRI) are important references for guiding surgical margins
(2). Allogeneic joint
transplantations and artificial joints are both used in joint
functional reconstructions (3). One
of the main challenges for surgeons is finding an appropriate
replacement for large bone segment defects after tumor resection.
The establishment of a digital image inventory based on bone
analysis technology and available in a computer-assisted navigation
system will aid in matching the necessary surgical resection
margins to appropriate allogeneic bone specimens, significantly
improving the outcome of such procedures (4,5).
Accordingly, this study aims at analyzing the value of a
computer-assisted navigation system based on CT images for bone
reconstruction after malignant tumor resection in the knee.
Patients and methods
Participant selection
Forty-five patients diagnosed with malignant bone
tumors around the knee joint, at Linyi People's Hospital, were
continuously recruited for this study starting October 2014 and
lasting until October 2015. All the participants had limb salvage
indications, an expected life expectancy longer than 12 months, and
accompanying complete clinical data. This study was approved by the
Ethics Committee of Linyi People's Hospital. Signed written
informed consents were obtained from the patients. All participants
signed informed consent forms. In addition, none of the patients
enrolled presented knee osteoarthritis, rheumatoid diseases or
tumor metastasis. A total of 29 male and 16 female patients
participated, their average age was of 52.6±13.5 years with a range
of 38–72; 24 patients had a lesion on the left knee and 21
presented a right knee lesion. In terms of tumor location, 22 cases
had a distal femur tumor, and 23 cases a proximal tibia tumor.
According to pathology results 24 patients had osteosarcoma, 16
chondrosarcoma, and 5 Ewing's sarcoma. Finally, there were 20
patients with Enneking stage I and 25 with stage II; and the tumor
diameter range was 0.5–15.5 cm, with an average of 7.2±3.4 cm.
Study methods
The same team participating in surgery and nursing
of the patients completed this study. X-ray, CT and MRI
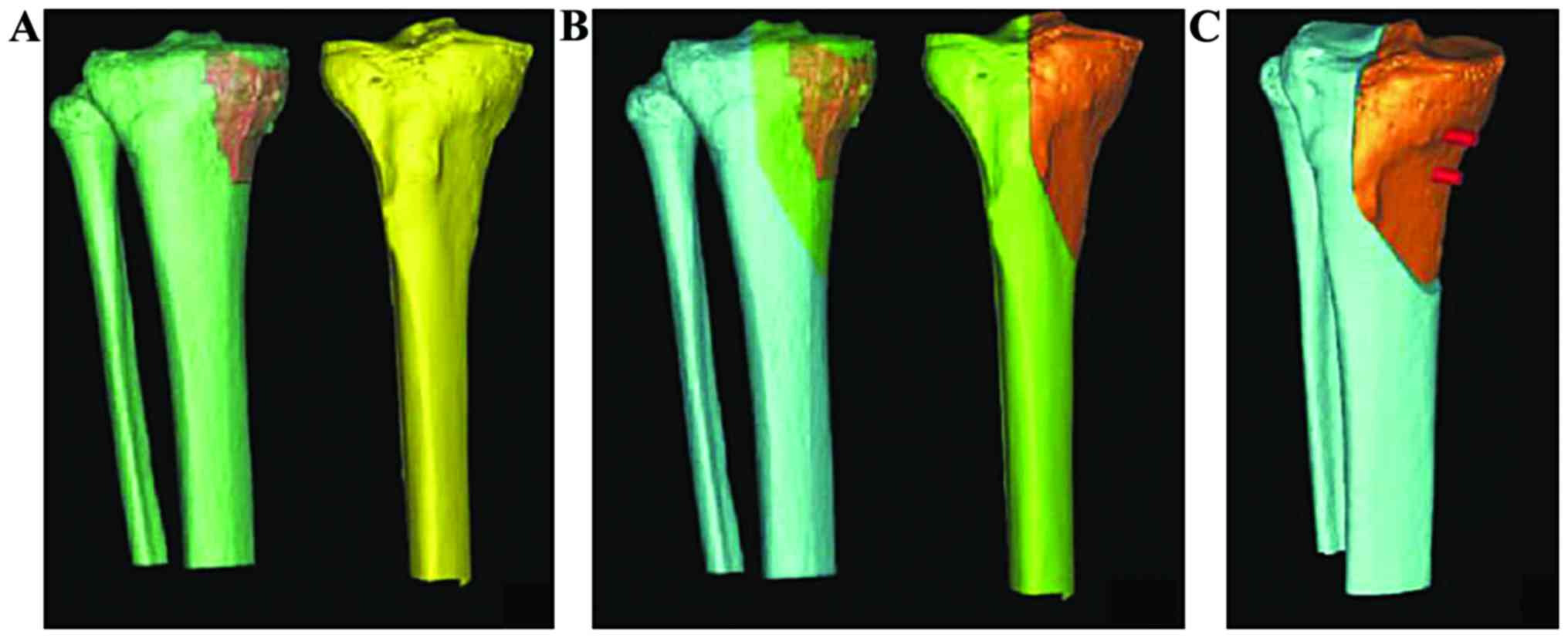
examinations were performed before surgery. The original image data
were saved as Dicom files, and analyzed with the Mimics 10.01
imported software (Materialise, Leuven, Belgium). Six CT tumor
three-dimensional images were reconstructed and a precise osteotomy
3D solid model site was built up via image fusion technology
(Fig. 1). The available bone marrow
resources at the Xijing Hospital of the Fourth Military Medical
University were recovered. Bone and cartilage tissues around the
knee (such as upper and lower femur, and upper and lower tibia)
were scanned via a 64-slice CT. Heterogeneity information such as
the length, width, height and three-dimensional image of each
specimen was stored in the Dicom format. At the same time,
articular surface and specific bone markers were used to establish
a digital bone bank. After that, tumor CT images were compared with
the allogeneic bone and joint data to make the necessary
measurements and to choose an optimal bone match. Mimics software
version 16.0 (Media Cybernetics, Inc., Rockville, MD, USA) was used
to simulate cleaning, compounding the lesion site, precisely
calculating the range of tumor resection and allogeneic bone
osteotomy.
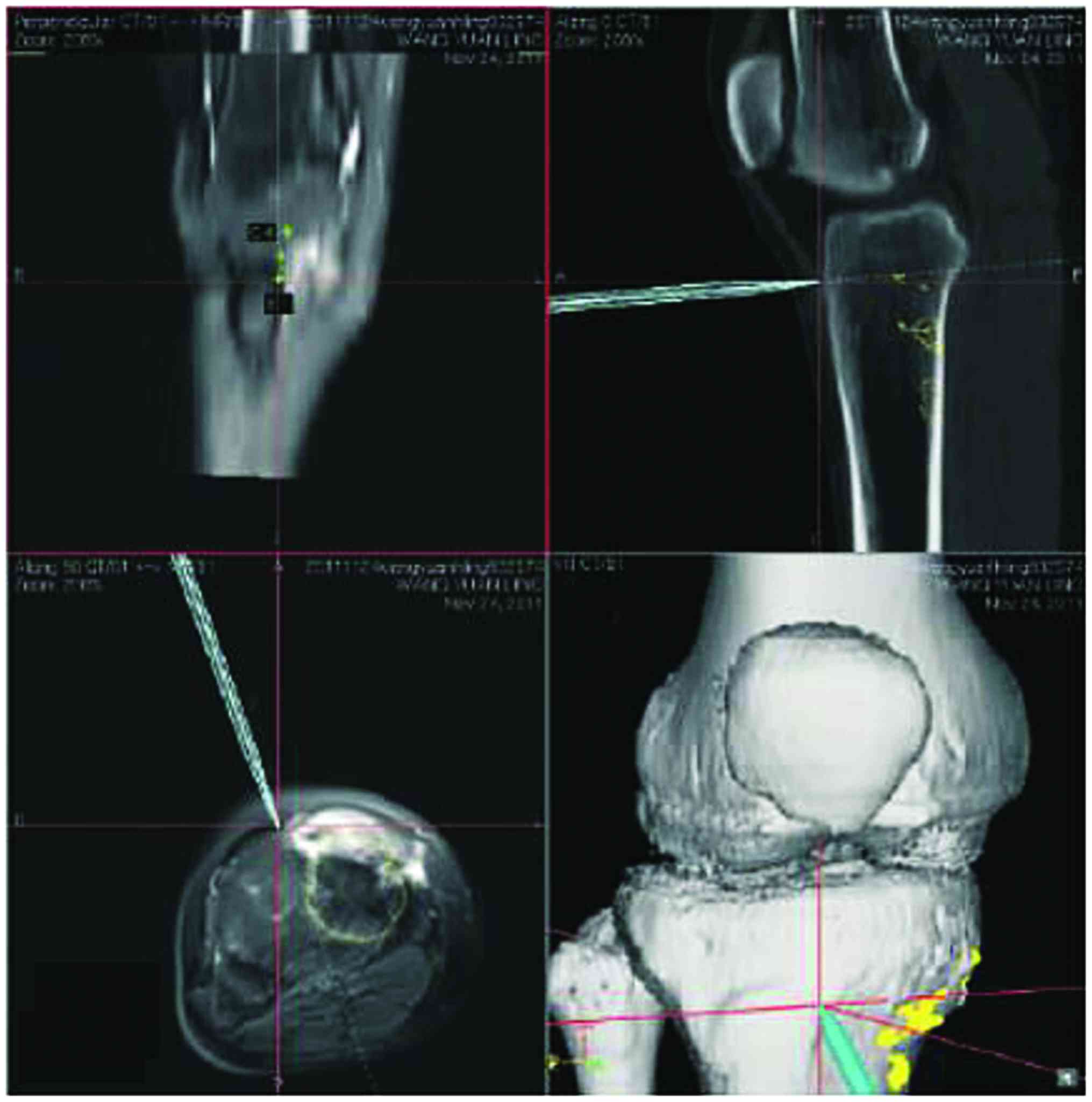
Bone tumor and allogeneic bone image data were
transmitted to the navigation system II-Cart (Stryker, Kalamazoo,
MI, USA). Image fusion technique was used to construct the
three-dimensional model of the surgical site and to mark the
preoperative design of the osteotomy region on the 3D solid model
(Fig. 2). The corresponding location
and internal fixation position of allogeneic bone and joint were
determined according to the osteotomy range. Three to five
registration points were marked on the three-dimensional model
based on the surgical approach and exposed range. A tracker was
installed during surgery to reveal the registration points, which
matched anatomical markers with corresponding sites on the
three-dimensional model and guided the procedure. After the
registration, the tumor was resected according to the preoperative
plan, the allogeneic bone was prepared and the bone defect was
filled based on the navigator's guidance, ensuring the pairing of
osteotomy and articular surface. The location of internal fixation
was determined via the navigation system instructions; lower limb
line and joint angle were corrected until satisfactory.
Follow-up indicators
The success rate of osteotomy and pairing, average
osteotomy time, pairing time, mean error of anatomical registration
point, average error of tumor resection and allogeneic bone pairing
were all calculated. Postoperative complications, tumor recurrence
and survival rates, allogeneic bone healing time and knee joint
functionality MSTS scores were evaluated after surgery.
Statistical analysis
The SPSS 20.0 statistical software (SPSS Inc.,
Chicago, IL, USA) was used for statistical analysis. Data were
expressed as mean ± standard deviation (SD), comparison between
groups was tested via independent sample t-test, and results were
expressed as number or percentages (%). Comparison between groups
was done via χ2 test or Fisher's exact test. P<0.05
was considered to indicate a statistically significant
diference.
Results
All patients underwent a successful osteotomy and
allogeneic bone pairing. The osteotomy time ranged from 25 to 72
min with an average of 46.8±12.3 min, and the pairing time ranged
from 18 to 45 min with an average of 32.5±9.8 min. The
intraoperative anatomical registration points were satisfactorily
paired with the virtual 3D CT images. The registration error ranged
from 0.16 to 0.58 mm, with an average of only 0.36±0.09 mm. The
tumor resection area and allogeneic osteoarticular osteotomy region
were satisfactorily paired with an error ranging from 0.05 to 0.36
mm or 0.11±0.03 mm on average. There were no unequal limb or joint
deformities after operation. The postoperative follow-up was
carried out for 8.5 to 22.5 months, with a mean of 11.6±3.9 months.
While 5 cases (11.1%) had tumor recurrence, the survival rate
during the follow-up period was 95.6% (43/45). There were no
statistically significant differences in the length of resection,
the size of incision margin, the osteotomy or matching durations or
the registration or pairing errors between the allogeneic bone and
the target defect (p>0.05) (Table
I). Additionally, the healing time of allogeneic and host bones
ranged from 3.6 to 8.2 months with an average of 5.5±1.2 months,
there were no flexible internal fixations, fractures or joint
collapses. The knee joint functionality MSTS score ranged from 18.2
to 28.9 points (with an average of 25.5±6.6 points) until the end
of the follow-up period.
 | Table I.Data of osteotomy range and allogeneic
bone pairing comparisons. |
Table I.
Data of osteotomy range and allogeneic
bone pairing comparisons.
| Group | Cases | Tumor resection
length (cm) | Margin negative rate
(cases, %) | Osteotomy duration
(min) | Pairing time
(min) | Registration error
(mm) | Pairing error
(mm) |
|---|
| Tumor recurrence | 5 | 11.6±3.5 | 4
(80.0) | 49.2±16.7 | 34.6±12.3 | 0.39±0.12 | 0.12±0.05 |
| Tumor
non-recurrence | 40 | 12.2±3.9 | 38 (95.0) | 45.6±18.2 | 31.9±11.5 | 0.34±0.11 | 0.10±0.04 |
| t/χ2 |
| 0.256 | – | 0.462 | 0.269 | 0.362 | 0.126 |
| P-value |
| 0.824 | 1.000 | 0.659 | 0.854 | 0.768 | 0.923 |
Discussion
The common complications of limb salvage surgery are
prosthesis loosening, dislocation, allogeneic nonunion, rejection
reaction, internal fixation fracture and infection (6). Allogeneic bone graft implantation
increases the biomechanical strength compared with prosthesis
(7), and also provides good articular
surfaces and muscle, ligament and joint capsule attachment points
(8). In general, a shorter time to
bone healing means there is a higher probability of better
stability and functionality of the joint (9). Many studies have proved that this method
has better short-term and long-term clinical results and fewer
complications (10,11). Our study results are no exception.
The right selection of an allogeneic bone joint,
especially the structure of the bone graft material is key to the
success of the surgery. We took advantage of an established
comprehensive digital bone bank library, combined with preoperative
computer-simulated tumor resection and residual joint defect
correction ranges, to choose the best pairing bone segment. The 3D
information obtained by processing CT images of the bone defects
aided in skeletal bone dressing and calculating the location and
direction of internal fixation parameters. Intraoperative,
real-time monitoring and the use of a computer-assisted navigation
system allow surgeons to improve operation accuracy, accomplishing
individual reconstruction requirements (12,13). This
study also analyzed data comparing parameters of tumor resection
length, margin of incision, osteotomy and pairing durations,
registration and pairing errors between allogeneic bone and bone
defect in a group of patients who presented tumor recurrences and
another that did not. The differences among groups were not
statistically significant, suggesting that the computer-assisted
navigation system for tumor resection, allogeneic bone pairing and
joint reconstruction is not a technical factor affecting the tumor
recurrence rate in the long run. The tumor biological
characteristics and individual differences probably account for
recurrence rate differences among patients (14), the specific mechanism remains to be
analyzed.
China has established dozens of standardized bone
banks, where the sources, preparation and preservation methods of
allogeneic bones are guaranteed (15,16). The
technology of computer-assisted navigation has been well tested in
neurosurgery, oral and maxillofacial deformity correction,
artificial joint selection, prosthesis implantation and other
medical practices (17,18).
The evaluation of the cases reviewed in this study
show that a computer-assisted navigation system for bone
reconstruction after malignant bone tumor resection results in a
high osteotomy accuracy and pairing success rate, achieves
appropriate post-reconstruction posterior limb function levels,
carries only a small risk of complications, and is therefore a safe
and effective approach. Due to the small sample size and the less
than desirable follow-up period of our study, further clinical
studies are needed to validate our results.
References
|
1
|
Zhang P, Feng F, Cai Q, Yao W, Gao S, Wang
J and Wang X: Effects of metaphyseal bone tumor removal with
preservation of the epiphysis and knee arthroplasty. Exp Ther Med.
8:567–572. 2014.PubMed/NCBI
|
|
2
|
Wong KC and Kumta SM: Joint-preserving
tumor resection and reconstruction using image-guided computer
navigation. Clin Orthop Relat Res. 471:762–773. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Rabitsch K, Maurer-Ertl W, Pirker-Frühauf
U, Lovse T, Windhager R and Leithner A: Reconstruction of the
distal radius following tumour resection using an osteoarticular
allograft. Sarcoma. 2013:3187672013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wong KC and Kumta SM: Use of computer
navigation in orthopedic oncology. Curr Surg Rep. 2:472014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Aponte-Tinao L, Ritacco LE, Ayerza MA,
Muscolo DL, Albergo JI and Farfalli GL: Does intraoperative
navigation assistance improve bone tumor resection and allograft
reconstruction results? Clin Orthop Relat Res. 473:796–804. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nakamura T, Matsumine A, Uchida A, Kawai
A, Nishida Y, Kunisada T, Araki N, Sugiura H, Tomita M, Yokouchi M,
et al: Clinical outcomes of kyocera modular limb salvage system
after resection of bone sarcoma of the distal part of the femur:
The Japanese Musculoskeletal Oncology Group Study. Int Orthop.
38:825–830. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ogilvie CM, Crawford EA, Hosalkar HS, King
JJ and Lackman RD: Long-term results for limb salvage with
osteoarticular allograft reconstruction. Clin Orthop Relat Res.
467:2685–2690. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fan H, Guo Z, Wang Z, Li J and Li X:
Surgical technique: Unicondylar osteoallograft prosthesis composite
in tumor limb salvage surgery. Clin Orthop Relat Res.
470:3577–3586. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gharedaghi M, Peivandi MT, Mazloomi M,
Shoorin HR, Hasani M, Seyf P and Khazaee F: Evaluation of clinical
results and complications of structural allograft reconstruction
after bone tumor surgery. Arch Bone Jt Surg. 4:236–242.
2016.PubMed/NCBI
|
|
10
|
Aponte-Tinao LA, Ayerza MA, Muscolo DL and
Farfalli GL: Allograft reconstruction for the treatment of
musculoskeletal tumors of the upper extremity. Sarcoma.
2013:9254132013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Teunis T, Nota SP, Hornicek FJ, Schwab JH
and Lozano-Calderón SA: Outcome after reconstruction of the
proximal humerus for tumor resection: A systematic review. Clin
Orthop Relat Res. 472:2245–2253. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wong KC and Kumta SM: Computer-assisted
tumor surgery in malignant bone tumors. Clin Orthop Relat Res.
471:750–761. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Meijer MF, Stevens M, Boerboom AL, Bulstra
SK and Reininga IH: The influence of computer-assisted surgery on
rotational, coronal and sagittal alignment in revision total knee
arthroplasty. BMC Musculoskelet Disord. 15:942014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ding HW, Yu GW, Tu Q, Liu B, Shen JJ, Wang
H and Wang YJ: Computer-aided resection and endoprosthesis design
for the management of malignant bone tumors around the knee:
Outcomes of 12 cases. BMC Musculoskelet Disord. 14:332013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang W, Bi WZ, Yang J, Han G and Jia JP:
Pelvic reconstruction with allogeneic bone graft after tumor
resection. Acta Ortop Bras. 21:150–154. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cheng B, Lu SL and Fu XB: Regenerative
medicine in China: Main progress in different fields. Mil Med Res.
3:242016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ort R, Metzler P, Kruse AL, Matthews F,
Zemann W, Grätz KW and Luebbers HT: The reliability of a
three-dimensional photo system (3dMDface) based evaluation of the
face in cleft lip infants. Plast Surg Int.
2012:1380902012.PubMed/NCBI
|
|
18
|
Al Eissa S, Al-Habib AF and Jahangiri FR:
Computer-assisted navigation during an anterior-posterior en bloc
resection of a sacral tumor. Cureus. 7:e3732015.PubMed/NCBI
|