Introduction
The function of the larynx includes deglutition,
phonation and facilitates respiration. Laryngeal carcinoma is a
common malignant tumor that is primarily treated by surgical
resection (1). The patient's stress
level after surgical resection (in addition to side effects of
radiotherapy and chemotherapy) is increased due in part to the
close association between the structure and function
characteristics of larynx and hosts nutritional status. Patients,
while under the body's high metabolic status after surgery, can
often develop varying degrees of eating disorders and a relative
malnutrition state that can negatively impact the patient's quality
of life (2,3). To prevent or reverse the postoperative
nutritional problems, attention directed to nutritional support
therapies may have a great significance in order to prolong the
patient's survival time and reduce the mortality rate (4). A Hospital to Home (H2H) nutrition
management model is an individualized nutrition management strategy
proposed by the clinical nutrition department in West China
Hospital of Sichuan University (Chengdu, China), with the objective
to extend nutritional therapy from hospital to discharge and
transform a single treatment approach into therapeutic regimen with
multiple models. The purpose of this investigation is to determine
the effectiveness of a H2H nutrition management model on the
postoperative clinical outcome of patients with surgically treated
laryngeal carcinoma.
Materials and methods
Eighty-six patients with laryngeal carcinoma
admitted to Weifang People's Hospital (Shandong, China) from
October 2014 to September 2015, were selected for possible study
inclusion. Inclusion criteria: Patients with a confirmed diagnosis
of laryngeal carcinoma by computed tomography (CT) or magnetic
resonance imaging (MRI) who did not receive radiotherapy or
chemotherapy before operation; who underwent surgical resection;
who had an expected survival period of more than 3 months; and who
had signed an informed consent. Patients were excluded if they had
abnormal coagulation function, or obnubilation or a communication
barrier. Patients were randomly divided (using a random number
table) into either an observation (n=43) or control group (n=43)
and demographic data were recorded.
All the patients were treated with surgery; the
nutritional status was comprehensively evaluated before treatment,
and an early nutritional screening was conducted. The control group
received routine nutritional support therapy after surgery; the
nasogastric tube was indwelt before operation and enteral
nutritional support was given at 48 h postoperative; patients were
given a gradual increase of Nutrison Fibre (Nutricia Pharmaceutical
Co., Ltd., Wuxi, China) by continuous micro-pumping (pump speed as
50–100 ml/h); nutritional support was given to patients after the
caloric requirement was calculated according to 20–30 kcal/(kg·day)
standard within the 1st to 3rd day of nutritional therapy, and the
total volume was increased to 2,000 ml from the 4th day. Nutrient
solution temperature was maintained at 37°C by infusion thermostat,
and gastric juice was pumped back every 5 h and observed; when the
gastric juice volume was more than 200 ml, the pumping was stopped
temporarily. The nutrient solution infusion volume was gradually
decreased when patients could take food by mouth, and the total
calorie intake was no less than 25 kcal/(kg·day).
The observation group was treated with the H2H
nutrition management model; the individualized therapeutic regimen
was formulated according to the results of nutritional screening
before surgery: i) Preoperative nutritional support therapy:
Nutritional education was performed for patients and their
families; for patients with well nutrition or mild malnutrition,
glucose and electrolyte infusion were taken before surgery, and for
patients with moderate to severe malnutrition, parenteral
nutritional support was administered; ii) postoperative nutritional
therapy during hospitalization: Early enteral nutritional support
was taken, within 24 h after operation, and the specific methods
were the same as those in the control group; and iii) nutrition
therapy outside the hospital: Patients were maintained with
nutritional support by continuous nutritional therapy until 6 weeks
after discharge.
Before surgery, patients orally ingested 2 g
lactulose and 1 g mannitol on an empty stomach; lactulose and
mannitol with the same grams were injected into nutritive canal on
the 1st, 7th and 14th postoperative day, and the total urine of
patients was collected within 6 h, adding dimethylbenzene, and then
storing it at −20°C, before analysis. The samples were thawed,
centrifuged 3,650 × g for 5 min; and the protein and ions were
removed. To the supernatant was added acetonitrile, mixing
uniformly, and then centrifuging at 1,050 × g for 10 min. Protein
and ion were removed, and the supernatant was isolated. The
lactulose and mannitol were respectively prepared for the samples
with concentrations of 1,000, 500, 200, 100 and 50 mg/l by
ultrapure water, and detected by the high-performance liquid
chromatography differential detection method. The concentration of
lactulose and mannitol was calculated in accordance with standard
curve computational formula, and the ratio of lactulose to mannitol
(L/M) was calculated.
Venous blood (5 ml) was collected before operation
and on the 1st, 7th and 14th postoperative day and centrifuged
2,750 × g for 20 min for 20 min; supernatant was collected and
stored at −20°C. The serum orexin-A level of patients was
determined by enzyme-linked immunosorbent assay (ELISA), using kits
(Shanghai Jiang Lai Biotechnology Co., Ltd., Shanghai, China)
according to the manufacturer's instructions. At postoperative 3
months, 10 ml fasting peripheral venous blood was used to determine
levels of hemoglobin (Hb), albumin (Alb), prealbumin (PAB) and
transferrin (TRF) using a fully automatic biochemical analyzer.
All patients were followed-up for 1 year, and the
readmission rates and mortality rates were recorded; all patients
were regularly re-examined in the out-patient department; patients
in the observation group were followed up by WeChat network
platform, mobile APP, telephone and family visit. A home visit was
performed for patients treated with home parenteral nutritional
support by community physicians every week.
The total urine was collected within 6 h after
patients orally ingested the lactulose and mannitol before
operation and on the 1st, 7th and 14th postoperative day, and L/M
was detected by the high-performance liquid chromatography
differential detection method and recorded; 5 ml venous blood was
analyzed before surgery and on the 1st, 7th and 14th postoperative
day and serum orexin-A level of patients was determined by
ELISA.
At postoperative 3 months, 10 ml fasting peripheral
venous blood was analyzed for levels of Hb, Alb, PAB and TRF using
a fully automatic biochemical analyzer. The nutritional status of
patients in the two groups was evaluated by PG-SGA quantitation,
and the grade standards were: i) Good nutrition, PG-SGA score ≤1
point; ii) mild/moderate malnutrition, 2 points ≤ PG-SGA score ≤8
points; and iii) severe malnutrition, PG-SGA score ≥9 points.
At postoperative 6 months, the quality of life of
patients was assessed by Quality of Life Questionnaire-Core 30
(QLQ-C30) (5), and the scoring was
respectively completed from 5 dimensions, including body function,
role function, cognitive function, emotional function and social
function; the original score was converted into centesimal system
by linear formula; the higher score correlated to a higher quality
of life.
The hospitalization time, hospitalization cost and
incidence rate of postoperative complication of patients were
determine after the one year follow-up and the readmission rate and
mortality rate of patients in the two groups were compared.
Data were processed using SPSS 19.0 (SPSS, Inc.,
Chicago, IL, USA). Measurements were expressed as mean ± standard
deviation (mean ± SD), and t-test was utilized; enumeration data
were expressed by ratio and Chi-square test was utilized. P<0.05
was considered to indicate a statistically significant
difference.
Results
The demographic data of patients between the two
groups was not statistically different (p>0.05) (Table I). Before operation, and on the 1st,
7th and 14th postoperative day, L/M in the observation group were
0.41±0.12, 0.95±0.23, 0.73±0.14 and 0.54±0.13, respectively, and
were 0.42±0.11, 0.96±0.24, 0.85±0.15 and 0.76±0.14 in the control
group; before operation and on postoperative 1st, 7th and 14th day,
orexin-A levels in the observation group were 8.32±2.14,
16.86±4.28, 13.47±3.26 and 10.63±1.08 ng/l, respectively, and were
8.67±2.34, 17.24±4.35, 16.49±3.42 and 13.63±1.39 ng/l in the
control group; L/M and orexin-A levels of patients in the two
groups on the 1st postoperative day were significantly higher than
those before operation, which were decreased from the 7th and 14th
postoperative day, but higher than those before operation
(p<0.05); there were no statistical differences between the two
groups before operation and on the 1st postoperative day
(p>0.05), and the indexes in the observation group were
significantly decreased than those in the control group on the 7th
and 14th postoperative day (Figs. 1
and 2).
 | Table I.Comparison of baseline data of
patients between the two groups. |
Table I.
Comparison of baseline data of
patients between the two groups.
| Items | Control group
(n=43) | Observation group
(n=43) | t/χ2 | P-value |
|---|
| Sex
(male/female) | 24/19 | 21/22 | 0.420 | 0.517 |
| Age (years) | 45–76 | 45–75 |
|
|
| Average age
(years) | 55.76±6.43 | 56.03±6.56 | 0.193 | 0.847 |
| Operation time
(min) | 203.54±61.17 | 204.43±61.36 | 0.067 | 0.947 |
| Tumor staging (n,
%) |
| I–II | 23 (53.49) | 21 (48.84) | 0.186 | 0.666 |
|
III–IV | 20 (46.51) | 22 (51.16) | 0.186 | 0.666 |
| Operation mode (n,
%) |
| Partial
laryngectomy | 17 (39.53) | 15 (34.88) | 0.199 | 0.655 |
| Total
laryngectomy | 26 (60.47) | 28 (63.12) | 0.199 | 0.655 |
The serum Hb, Alb, TRF and PAB of patients between
the two groups at 3 months postoperative were compared (Table II). Alb and Hb of patients in the
observation group were significantly lower (p<0.05) than those
in the control group, the levels of TRF and PAB in the observation
group were significantly higher (p<0.05) than those in the
control group (p<0.05).
 | Table II.Comparison of postoperative serum
nutritional indexes of patients between the two groups. |
Table II.
Comparison of postoperative serum
nutritional indexes of patients between the two groups.
| Groups | Case | Hb (g/l) | Alb (g/l) | PAB (g/l) | TRF (g/l) |
|---|
| Observation | 43 | 93.43±5.38 | 38.52±3.59 | 0.26±0.09 | 1.76±0.34 |
| Control | 43 | 96.57±5.76 | 41.41±3.63 | 0.18±0.06 | 1.38±0.47 |
| t-test |
| 2.612 | 3.712 | 4.850 | 4.296 |
| P-value |
| 0.011 | <0.001 | <0.001 | <0.001 |
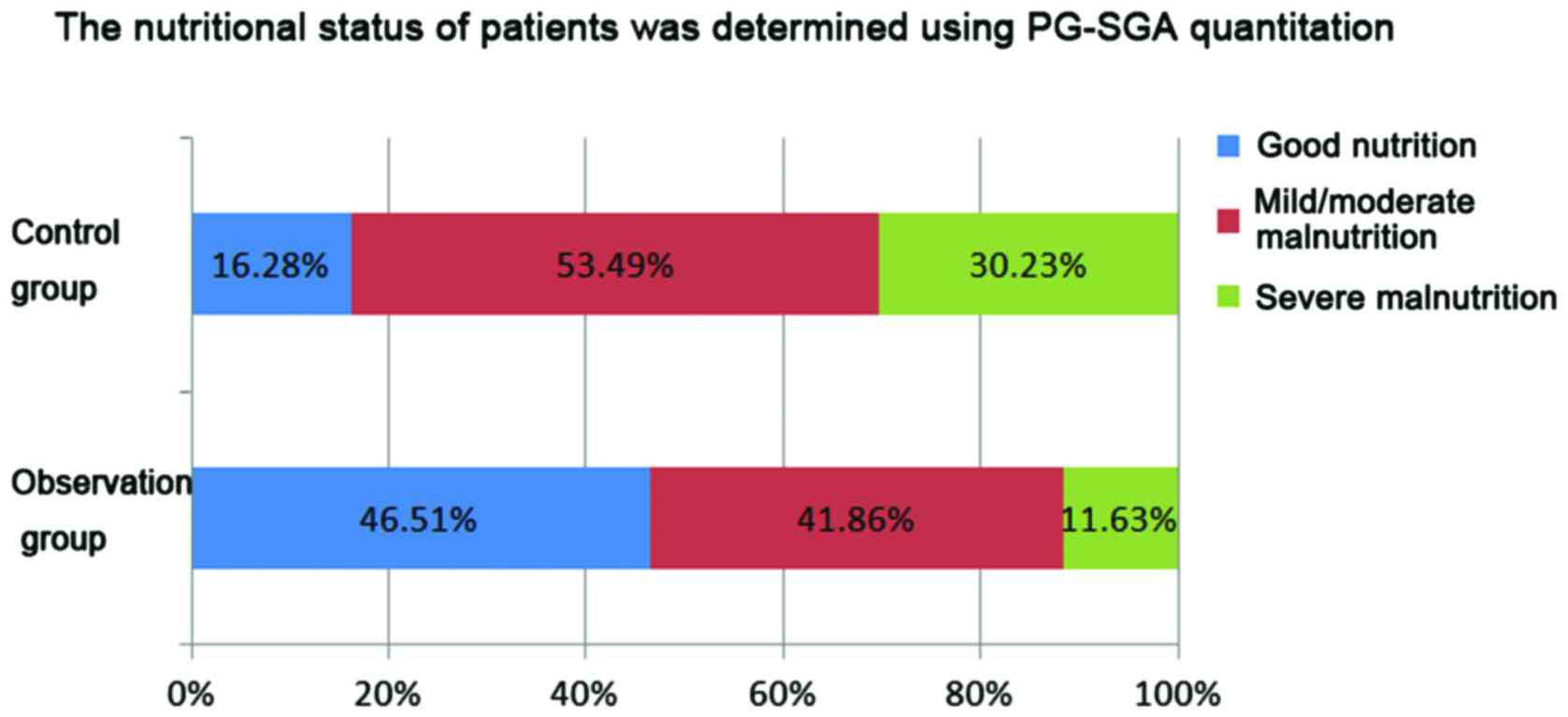
The nutritional status of patients was determined
using PG-SGA quantitation (Fig. 3).
The mild/moderate and severe malnutrition rates in the observation
group were 41.86% (18/43) and 11.63% (5/43), respectively, which
were 53.49% (23/43) and 30.23% (13/43) in the control group; the
malnutrition rates were significantly lower in the observation
group than those in the control group (p<0.05).
The incidence rate of postoperative complication,
hospitalization time and hospitalization cost of patients in the
two groups were compared (Table
III). There were no statistical differences in comparison of
hospitalization time and hospitalization cost of patients between
the two groups (p>0.05), and the incidence rate of postoperative
complication in the observation group was significantly lower than
that in the control group (p<0.05).
 | Table III.Therapeutic effects of patients in the
two groups. |
Table III.
Therapeutic effects of patients in the
two groups.
| Groups | Case | Hospitalization time
(days) | Hospitalization cost
(thousand RMB) | Postoperative
complication (n, %) |
|---|
| Observation | 43 | 11.82±3.23 | 2.73±1.24 | 3 (6.98) |
| Control | 43 | 12.14±3.24 | 2.65±1.38 | 12 (27.91) |
| t/χ2 |
| 0.459 | 0.283 | 5.174 |
| P-value |
| 0.647 | 0.778 | 0.023 |
The readmission rate and mortality rate of patients
in the two groups after one-year follow-up were compared (Table IV). The readmission rate and
mortality rate in the observation group (9.30 and 6.97%) were
significantly lower (p<0.05) than the control group (34.88 and
30.23%).
 | Table IV.Comparison of adverse reactions of
patients between the two groups (n, %). |
Table IV.
Comparison of adverse reactions of
patients between the two groups (n, %).
| Groups | Case | Readmission rate | Mortality rate |
|---|
| Observation | 43 | 4 (9.30) | 3 (6.98) |
| Control | 43 | 15 (34.88) | 13 (30.23) |
| χ2 |
| 6.756 | 6.223 |
| P-value |
| 0.009 | 0.012 |
The quality of life of patients between the two
groups after one-year follow-up (deceased patients were excluded)
were compared (Table V). Each
dimension score of quality of life in the observation group was
significantly higher (p<0.05) than the control group.
 | Table V.Comparisons of quality of life of
patients between the two groups. |
Table V.
Comparisons of quality of life of
patients between the two groups.
| Groups | Case | Body function | Role function | Cognitive
function | Emotional
function | Emotional
function |
|---|
| Observation | 40 | 91.62±3.23 | 92.73±1.24 | 88.72±3.23 | 72.73±3.24 | 87.73±5.44 |
| Control | 30 | 83.74±3.24 | 84.65±1.38 | 80.34±3.24 | 64.65±3.38 | 82.65±6.38 |
| t/χ2 |
| 10.088 | 25.704 | 10.728 | 10.136 | 3.590 |
| P-value |
| <0.001 | <0.001 | <0.001 | 0.001 | 0.001 |
Discussion
Laryngeal carcinoma is one of the most common
malignant tumors in otorhinolaryngology head and neck surgery,
accounting for 1 to 5% of systemic tumor, and its incidence rate is
increasing (6). Approximately, 30 to
90% of cancer patients will be malnourished (the malnutrition rate
in patients with laryngeal carcinoma is higher than in those with
other cancers) and ~20% of patients with cancer will be deceased
due to malnutrition and related complications (7). Multiple factors can lead to malnutrition
in patients with laryngeal carcinoma, including therapy, tumor load
and psychological factors (8).
Generally, patients with laryngeal carcinoma cannot eat food by
mouth for about two weeks after surgery. From surgery, the
integrity of laryngeal physiological function can be damaged which
can cause partial or total loss of its protective effects, leading
to dysphagia. In addition, the host caloric needs can be increased
by blood loss during and after surgery, pain and other stress
responses, resulting in a loss of appetite, gastrointestinal
symptoms and oral infections. These factors of an increased caloric
need and a decreased dietary caloric intake can lead to weight loss
and reduced subcutaneous fat, thus inducing or aggravating
malnutrition (9,10).
Nutritional oncology is an area of combined
nutrition theory and methods for the prevention (can accurately
evaluate nutritional status of patients with cancer to diagnose
malnutrition early in the disease/treatment process) and treatment
(provide appropriate nutritional support therapy) of cancer
patients) (11). Most of the
traditional nutritional therapies focus on the nutritional status
of patients only during hospitalization after surgery, and often
neglect the nutritional status of the patients outside the
hospital. After discharge of patients with laryngeal carcinoma,
anorexia, nausea, vomiting and other symptoms often occur after
postoperative radiotherapy and chemotherapy, and in particular,
metabolic disorders caused by cachexia can appear in patients with
advanced laryngeal carcinoma; therefore, it is necessary to improve
the nutrition maintenance therapy of patients once outside the
hospital (12–14). The H2H nutrition management model is a
comprehensive treatment model with the patient at the center with
continuous nutrition therapy for that patient from hospitalization
to outside the hospital; the model uses a team approach involved by
many medical disciplines (specialist physician, nutritionist,
community physician, nurse and patient's family), which can improve
patient compliance with nutritional therapy and minimize or
ameliorate the status of malnutrition in patients. The results of
this study showed the readmission and mortality rate in the
observation group were distinctly lower than those in the control
group (p<0.05), which demonstrates the validity of improved
patient outcomes with the implementation of the H2H nutrition
management model.
The results of this study showed that orexin-A
levels and L/M of patients in the two groups on the 1st
postoperative day were significantly higher than those before
operation, and decreased from postoperative 7th and 14th day, but
higher than those before operation (p<0.05); there were no
statistical differences between the two groups before operation and
on postoperative 1st day (p>0.05), and the indexes in the
observation group were significantly decreased over the control
group on the 7th and 14th postoperative day (p<0.05); the
increase of L/M reveals that the tight junction of intestinal
mucosa is incomplete, permeability is increased, and intestinal
barrier function is damaged (15,16); the
possible causes include: i) Intestinal secretory immunoglobulin A
content in patients treated by surgery is decreased; ii) intestinal
colonization resistance is reduced and iii) the normal intestinal
function is inhibited. Many inflammatory mediators can be activated
by the stress response of surgical trauma; for example the
gastrointestinal mucosal barrier can be damaged by interleukin (IL)
and tumor necrosis factor-α (TNF-α) and an excess amount of NO
production, that is induced by TNF-α, can cause microcirculation
congestion resulting in damage to the integrity of intestinal
membrane barrier (17). Early enteral
nutritional support during hospitalization, and continuous
parenteral nutritional support after discharge, can provide the
necessary fuel for the host to repair the injury of intestinal
epithelium and effectively protect the chemical barrier of
intestinal mucosa; this recovery of the intestinal barrier function
is gradual and aids in amelioration of the patients' malnourished
status (18). Orexin-A, is a
neuropeptide that can regulate the body's energy metabolism and
improve appetite (14). The related
experiment reveals that neuron of appetite function can be
inhibited by orexin-A, which can excite hypothalamic NPY/cocaine-
and amphetamine-regulated transcript peptide neuron, thus promoting
the increase of body's food intake and weight (15). The increased expression level of
orexin-A caused by postoperative fasting will promote the patient's
appetite and with the support of postoperative enteral nutrition,
especially early nutritional support, food intake is increased and
the body's energy metabolism is improved, thereby gradually
downregulating orexin-A expression to the normal level.
The results of this study indicated that the
incidence rate of postoperative complication in the observation
group was significantly lower than that in the control group
(p<0.05). It appears that early enteral nutritional support can
effectively reduce bacterial endotoxin translocation, stimulate
secretion of digestive juice and gastrointestinal hormones, promote
normal gastrointestinal peristalsis, and effectively avoid severe
consumption of high catabolism caused by prolonged postoperative
fasting, allowing the host metabolic state to return to the normal
(early recovery of preoperative nutritional status and improved
body's negative nitrogen balance) and prevent the occurrence of
postoperative complications caused by malnutrition (19). Results from this investigation noted
that between the two groups, serum Alb and Hb of patients in the
observation group were significantly lower than those in the
control group, and the levels of TRF and PAB in the observation
group were significantly higher than the control group, suggesting
that the nutritional level of patients intervened by the H2H
nutrition management model is significantly ameliorated, thus
reducing the incidence rate of malnutrition.
Currently, PG-SGA evaluation is utilized for
patients with laryngeal carcinoma to screen for malnutrition risk.
Advantages of this tool is that it can quantitatively evaluate
patient's nutritional status from measurement of upper limb muscle
circumference, triceps skinfold thickness, maximum circumferential
diameter of crus, grip strength of non-handedness and body mass
index (BMI) (20). By adopting the
H2H nutrition management model, PG-SGA evaluation showed that
malnutrition rates were significantly lower in the observation
group than the control group, and each dimension score of quality
of life in the observation group was distinctly higher than the
control group (p<0.05). It should be emphasized that the
nutritional therapy of patients administered by the H2H nutrition
management model is not static after hospital discharge; a
continuous and individualized nutritional support therapy is
implemented for patients through PG-SGA evaluation; the follow-up
is regularly conducted, and the intake, body weight change, and
effect of nutritional support therapy, of patients are observed; in
addition, effective psychological counseling is also important to
manage the patients with depression, self-abasement and other
social barriers, in order to improve patients' quality of life.
In conclusion, the H2H nutrition management model
can ameliorate the postoperative malnutritional status of patients
with laryngeal carcinoma, reduce the incidence rate of malnutrition
and postoperative complication and improve the postoperative
quality of life of patients, thus promoting an effective and
rational utilization of medical resources.
References
|
1
|
Li L, Xu Y and Wang B: Liriodenine induces
the apoptosis of human laryngocarcinoma cells via the upregulation
of p53 expression. Oncol Lett. 9:1121–1127. 2015.PubMed/NCBI
|
|
2
|
Li P, Zhang J, Sun G and Li H: Assessment
of quality of life for laryngeal cancer patients after
laryngectomy. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi.
28:1648–1651. 2014.(In Chinese). PubMed/NCBI
|
|
3
|
Kaya E, Cingi C, Pınarbaşlı Ö, Gürbüz MK,
Çaklı H, İncesulu A, Özüdoğru E and Keçik C: Health-related quality
of life in laryngeal cancer patients. J Med Updates. 4:29–36. 2014.
View Article : Google Scholar
|
|
4
|
Shivappa N, Hébert JR, Polesel J,
Zucchetto A, Crispo A, Montella M, Franceschi S, Rossi M, La
Vecchia C and Serraino D: Inflammatory potential of diet and risk
for hepatocellular cancer in a case-control study from Italy. Br J
Nutr. 115:324–331. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bedard G, Zeng L, Zhang L, Lauzon N,
Holden L, Tsao M, Danjoux C, Barnes E, Sahgal A, Poon M, et al:
Minimal important differences in the EORTC QLQ-C30 in patients with
advanced cancer. Asia Pac J Clin Oncol. 10:109–117. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Agra IM, Ferlito A, Takes RP, Silver CE,
Olsen KD, Stoeckli SJ, Strojan P, Rodrigo JP, Filho Gonçalves J,
Genden EM, et al: Diagnosis and treatment of recurrent laryngeal
cancer following initial nonsurgical therapy. Head Neck.
34:727–735. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen Y, Liu BL, Shang B, Chen AS, Liu SQ,
Sun W, Yin HZ, Yin JQ and Su Q: Nutrition support in surgical
patients with colorectal cancer. World J Gastroenterol.
17:1779–1786. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shpata V, Prendushi X, Kreka M, Kola I,
Kurti F and Ohri I: Malnutrition at the time of surgery affects
negatively the clinical outcome of critically ill patients with
gastrointestinal cancer. Med Arch. 68:263–267. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lu W, Xiong N, Lyu Z and Xu W: Effect of
peer education on postoperative rehabilitation of patients with
laryngeal cancer. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi.
49:632–636. 2014.(In Chinese). PubMed/NCBI
|
|
10
|
Langius JAE, Twisk J, Kampman M, Doornaert
P, Kramer MH, Weijs PJ and Leemans CR: Prediction model to predict
critical weight loss in patients with head and neck cancer during
(chemo)radiotherapy. Oral Oncol. 52:91–96. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Omlin A, Blum D, Wierecky J, Haile SR,
Ottery FD and Strasser F: Nutrition impact symptoms in advanced
cancer patients: Frequency and specific interventions, a
case-control study. J Cachexia Sarcopenia Muscle. 4:55–61. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Skóra T, Nowak-Sadzikowska J,
Mucha-Małecka A, Szyszka-Charewicz B, Jakubowicz J and Gliński B:
Postoperative irradiation in patients with pT3-4N0 laryngeal
cancer: Results and prognostic factors. Eur Arch Otorhinolaryngol.
272:673–679. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cotogni P: Enteral versus parenteral
nutrition in cancer patients: Evidences and controversies. Ann
Palliat Med. 5:42–49. 2016.PubMed/NCBI
|
|
14
|
Leonard CS and Kukkonen JP:
Orexin/hypocretin receptor signalling: A functional perspective. Br
J Pharmacol. 171:294–313. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Messina G, Dalia C, Tafuri D, Monda V,
Palmieri F, Dato A, Russo A, De Blasio S, Messina A, De Luca V, et
al: Orexin-A controls sympathetic activity and eating behavior.
Front Psychol. 5:9972014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Earley ZM, Akhtar S, Green SJ, Naqib A,
Khan O, Cannon AR, Hammer AM, Morris NL, Li X, Eberhardt JM, et al:
Burn injury alters the intestinal microbiome and increases gut
permeability and bacterial translocation. PLoS One.
10:e01299962015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Siplivyĭ VA, Grinchenko SV, Gorgol' NI,
Dotsenko VV and Evtushenko AV: Pathomorphological peculiarities of
hemomicrocirculatory bed of the small and large intestine in acute
peritoniti. Klin Khirurgiia. 29:61–63. 2014.
|
|
18
|
Xu XD, Sun YS, Shao QS, Hu JF, Qian ZY,
Zhou YL and Ye ZY: Effect of early enteral nutrition supplemented
with glutamine on postoperative intestinal mucosal barrier function
in patients with gastric carcinoma. Zhonghua Wei Chang Wai Ke Za
Zhi. 14:436–439. 2011.(In Chinese). PubMed/NCBI
|
|
19
|
Li NM, Liu F, Lv FY and Zhang QW:
Influencing factors and interventional strategies for early enteral
nutrition after gastric carcinoma surgery. J Cancer Res Ther.
12:689–692. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Um MH, Choi MY, Lee SM, Lee IJ, Lee CG and
Park YK: Intensive nutritional counseling improves PG-SGA scores
and nutritional symptoms during and after radiotherapy in Korean
cancer patients. Support Care Cancer. 22:2997–3005. 2014.
View Article : Google Scholar : PubMed/NCBI
|