Introduction
Nasopharyngeal carcinoma (NPC) is a common head and
neck cancer. Owing to its sensitivity to radiation, radiotherapy is
the most important method used to treat NPC (1,2). Since the
site where NPC occurs usually has limited space and the head and
facial nerve distribution is widespread, there are only limited
treatments for NPC.
Commonly used methods of treatment include surgery,
posterior implantation or implantation of radiation therapy as well
as stereotactic radiotherapy and external irradiation (3–5). Due to
the wide spread of nasopharyngeal mass, surgery, endovascular
grafting, implantation of radiotherapy and stereotactic
radiotherapy are often limited, which causes a high recurrence of
NPC. High-dose external irradiation is the main treatment for
patients with relapse, especially for those with large local masses
or a wide range attack when recurrence occurs (6,7). As
conventional radiotherapy can often lead to serious complications
and sequelae, including nasopharyngeal ulcers, hearing loss,
temporal lobe necrosis, radiation encephalopathy, posterior cranial
nerve injury and/or difficulty in mouth opening (7), in recent years we have continued to
explore new radiotherapy treatments that can reduce the incidence
of adverse reactions.
Three-dimensional conformal radiation therapy
(3D-CRT) is an advanced treatment technique that can irradiate the
target area through multiple fields (usually 5–7 fields) to align
the tumor with the radiation target through three-dimensional
directions. It makes the target dose distribution more reasonable
and reduces exposure to adjacent normal tissue (8). To the best of our knowlegde, few studies
have focused on the treatment of recurrent NPC by 3D-CRT.
Therefore, the aim of the present study is to analyze the efficacy
of 3D-CRT in the treatment of recurrent NPC and long-term adverse
effects after radiotherapy.
Materials and methods
Materials
Between May 2010 and June 2012, 141 patients with
NPC who had been diagnosed with local recurrence by biopsy and/or
computed tomography/magnetic resonance imaging (CT/MRI) imaging of
bone destruction or cranial nerve symptom progression received
3D-CRT treatment. The median relapse interval was 27.5 months
(range, 3–156 months). Chest X-ray, abdominal B-ultrasound, head
and neck CT/MRI, electrocardiogram, bone scan and oral, and other
tests were performed. Since July 2005, CT was replaced with MRI in
the head and neck exam (CT before July and MRI after July). PET/CT
examination was performed based on the physician's judgement
depending on the condition of the patient. No neck biopsy was
performed in 10 patients with recurrence in neck. All the patients
were re-staged according to the AJCC (5th edition, 1997).
Signed written informed consent was obtained from
patients enrolled in the study. The study was approved by the
Ethics Committee of the Nanchong Central Hospital (Nanchong,
China).
3D-CRT radiotherapy treatment
plan
The patients were placed in a supine position and
wore a thermoplastic mask. CT was performed from the head to 2 cm
below the clavicle, with a scanning layer of 3 mm and an enhanced
scan. From July 2005 onwards, the MRI/CT image was produced using
MasterPlan® version 1.5, Nucletron BV software analysis
and image fusion.
Gross tumor volume (GTV), such as GTV-P (planned
target area of primary tumor area) and GTV-N (unplanned target area
of primary tumor area), including masses visible on CT/MRI images
as well as clinical target volume (CTV), including CTV-P and CTV-N
received external radiation of 8–10 mm. If the mass was close to
the brain stem or spinal cord, the exposure of the radiation
boundary was smaller, with the smallest distance being 3 mm, to
protect the brain stem and spinal cord from receiving more than the
allowable tolerated dose. Cervical lymphatic drainage area did not
receive prophylactic irradiation. Considering the system and
positioning errors, 3 mm beyond CTV was considered as planning
target volume (PTV). Organs affected included brain stem, spinal
cord, optic nerve, optic chiasm, temporal lobe, pituitary,
temporomandibular joint, eyeball, crystal and parotid gland. The
dose received by affected organs was limited and individualized
based on the first dose of radiotherapy, but within the tolerances
specified by RTOG.
The treatment plan involved Plato®
preparation planning software system (RTS® version
2.6.4), using isocentric coplanar or non-coplanar techniques; the
isocenter is placed at the center of GTV-P. The irradiation of
primary focus and neck involved 5–9 coplanar static intensity
control technology. The prescribed doses were PTV-GTVnx, 70 Gy;
PTV-GTVnd, 64–66 Gy; PTV-GTVnd, 64–66 Gy; PTV-CTVnx60, 60–64 Gy;
PTV-CTVx50, 54 Gy; and PTV-CTVnd, 54 Gy; 31–32 times of
segmentation irradiation. The mean radiotherapy dose of 3D-CRT for
three groups of patients were 58/1.8–2 Gy, 62/1.8–2 Gy and 68/1.8–2
Gy respectively (single segmentation 2/1.8 Gy, once a day, 5
days/week). Five to seven coplanar irradiation fields were designed
and a medical accelerator and a multi-leaf grating were used.
Radiotherapy
Due to the absence of current standard chemotherapy
regimens for local recurrence of NPC, clinicians can consider
whether to prescribe a combined chemotherapy based on the overall
state of health of patients. In our study, 65 patients received 2–6
cycles of platinum-based monotherapy or combinations of
chemotherapy with neoadjuvant and/or concurrent adjuvant
chemotherapy.
Follow-up
Patients were enrolled in a weekly check up for
clinicians to evaluate the retraction of their lumps. Patients
administered chemotherapy received routine blood, liver and kidney
tests weekly. The patients were followed up every 3 months within 2
years after the treatment, every 6 months 3 years after the
treatment and every year 5 years after the treatment. Each follow
up included systemic examination, blood, VCA-IgA, VCA-EA, nose
pharyngeal fibrobronchoscopy, chest X-ray, abdominal B-ultrasound,
and head and neck MRI. Adverse reactions and sequelae were recorded
according to the RTOG/EORTC assessment of adverse reactions of
radiation therapy.
Statistical analysis
SPSS 19.0 software (IBM, Armonk, NY, USA) was used
for statistical analysis. The time at which a local region relapses
or shifts was calculated from the end of the 3D-CRT. Overall
survival (OS) was defined as the time between the diagnosis of
relapse and death or the last follow up. Locoregional
recurrence-free survival (LRRFS), disease-free survival (DFS) and
OS were calculated using the Kaplan-Meier method. The log-rank test
was used for univariate analysis of different prognostic factors.
The Cox regression model was used for multivariate analysis.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Comparison of the general clinical
situation of patients enrolled
The general clinical conditions of the patients were
compared, including age, sex, T stage, whether to receive
chemotherapy, time of recurrence and tumor invasion. The patient's
age ranged from 26 to 71 years with an average age of 45 years.
There was no statistically significant difference between the three
groups in general clinical baseline data (P>0.05) (Table I).
 | Table I.Comparison of the general clinical
situation of patients enrolled. |
Table I.
Comparison of the general clinical
situation of patients enrolled.
|
|
| Groups |
|
|
|---|
|
|
|
|
|
|
|---|
| Factors | No. | 58/1.8–2 Gy n=47 | 62/1.8–2 Gy n=47 | 68/1.8–2 Gy n=47 | χ2
value | P-value |
|---|
| Sex |
|
|
|
| 0.473 | 0.556 |
| Male | 70 | 26 | 24 | 20 |
|
|
|
Female | 71 | 21 | 23 | 27 |
|
|
| Age (years) |
|
|
|
| 0.102 | 0.732 |
| ≤50 | 68 | 24 | 21 | 23 |
|
|
|
>50 | 73 | 23 | 26 | 24 |
|
|
| T stage |
|
|
|
| 0.027 | 0.973 |
| T1 | 31 | 13 | 10 | 8 |
|
|
| T2 | 50 | 14 | 17 | 19 |
|
|
| T3 | 30 | 9 | 11 | 10 |
|
|
| T4 | 30 | 11 | 9 | 10 |
|
|
| Combined
chemotherapy |
| No | 87 | 27 | 32 | 28 |
|
|
| Yes | 54 | 20 | 15 | 19 |
|
|
| Nasopharyngeal
tumor | 55 | 19 | 22 | 14 | 0.483 | 0.567 |
| invasion to both
sides | 86 | 28 | 25 | 33 |
|
|
| Time of relapse |
|
|
|
| 0.465 | 0.587 |
| <24
months | 67 | 17 | 24 | 26 |
|
|
| 24-36
months | 28 | 8 | 9 | 11 |
|
|
| >36
months | 46 | 16 | 17 | 13 |
|
|
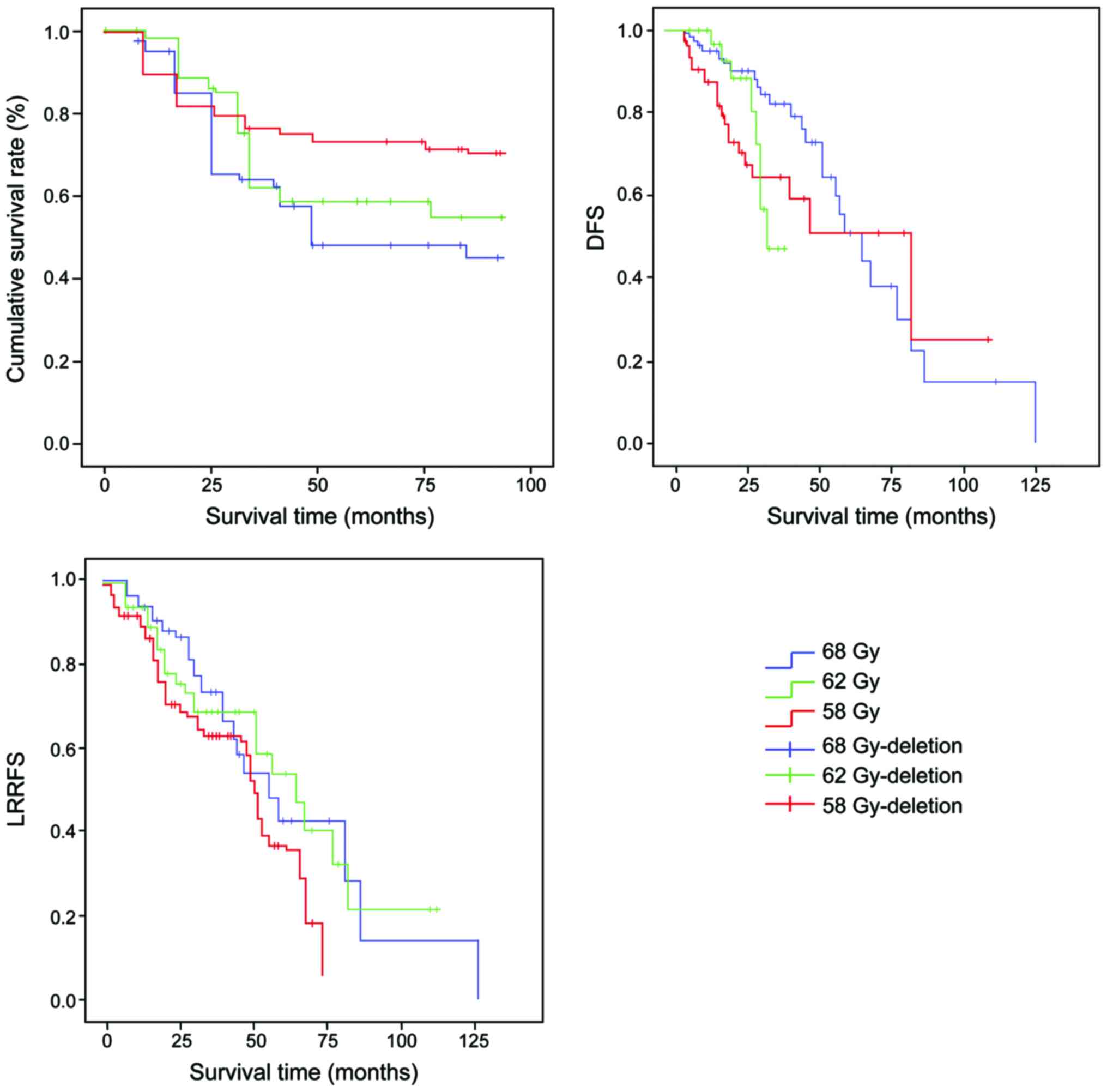
Survival prognosis
The prognosis of the three groups of patients were
analyzed. The OS, DFS and LRRFS of the 3 groups of patients were:
43.2 vs. 64.53 vs. 75%, 29.13 vs. 42.82 vs. 39.7%, 30.76 vs. 44.19
vs. 45.4%, respectively (Fig. 1).
Comparison of the incidence of adverse
reactions
Adverse reactions mainly included nasopharyngeal
ulcer, cranial nerve injury, mouth opening difficulties and hearing
loss. The overall adverse reaction rate of the 68/1.8–2 Gy group
was higher than that of the other two groups and the difference was
statistically significant (P<0.05) (Table II).
 | Table II.Comparison of adverse reaction
rate. |
Table II.
Comparison of adverse reaction
rate.
| Groups | Nasopharyngeal
ulcer | Cranial nerve
injury | Mouth opening
difficulties | Hearing loss |
|---|
| 58/1.8–2 Gy | 2 | 1 | 3 | 2 |
| 62/1.8–2 Gy | 0 | 1 | 2 | 4 |
| 68/1.8–2 Gy | 15 | 10 | 3 | 8 |
| χ2
value |
| 32.8 |
|
|
| P-value |
| 0.001 |
|
|
Univariate prognostic analysis
The prognostic factors of the patients were analyzed
by a univariate analysis. The prognostic factors included sex, age,
treatment regimen (with or without chemotherapy), total radiation
dose, primary T stage, recurrence T stage and recurrence interval.
The results showed that age ≥50 years of age was a risk factor for
poor prognosis (Tables III and
IV).
 | Table III.Univariate prognostic analysis. |
Table III.
Univariate prognostic analysis.
|
|
| OS | DFS | LFS |
|---|
|
|
|
|
|
|
|---|
| Factors | n | t | P-value | t | P-value | t | P-value |
|---|
| Sex |
|
| 0.387 |
| 0.583 |
| 0.387 |
| Male | 70 | 52.4±5.5 |
| 48.4±5.3 |
| 52.3±5.5 |
|
|
Female | 71 | 42.3±7.1 |
| 40.3±7.2 |
| 40.1±7.1 |
|
| Age (years) |
|
| 0.027 |
| 0.016 |
| 0.008 |
|
<50 | 68 | 64.2±7.3 |
| 60.3±6.6 |
| 62.4±7.1 |
|
|
≥50 | 73 | 55.4±7.2 |
| 38.7±4.5 |
| 38.6±5.2 |
|
| rT stage |
|
| 0.276 |
| 0.078 |
| 0.271 |
|
1+2 | 81 | 57.3±7.2 |
| 58.7±7.2 |
| 57.5±8.2 |
|
|
3+4 | 60 | 45.5±5.1 |
| 40.2±5.9 |
| 31.2±5.4 |
|
| Recurrence
time |
|
| 0.478 |
| 0.228 |
| 0.271 |
| <24
months | 67 | 57.6±7.1 |
| 55.1±6.7 |
| 57.3±7.2 |
|
| 24-36
months | 28 | 43.6±7.2 |
| 41.2±6.6 |
| 43.4±7.7 |
|
| >36
months | 46 | 44.9±8.1 |
| 39.7±7.1 |
| 41.7±7.2 |
|
| Radiation dose |
|
| 0.323 |
| 0.227 |
| 0.863 |
| <60
Gy | 47 | 47.3±5.5 |
| 57.2±9.1 |
| 49.3±5.5 |
|
| 62
Gy | 47 | 49.7±5.3 |
| 44.5±4.4 |
| 48.4±6.7 |
|
| 68
Gy | 47 | 48.3±4.3 |
| 46.5±4.3 |
| 48.1±5.3 |
|
 | Table IV.Multivariate prognostic analysis. |
Table IV.
Multivariate prognostic analysis.
|
|
|
|
|
|
|
| 95% CI Exp (B) |
|---|
|
|
|
|
|
|
|
|
|
|---|
| Factor | B | SE | WALD | df | Sig | Exp (B) | Lower | Upper |
|---|
| Age | 0.538 | 0.215 | 6.218 | 1 | 0.014 | 1.701 | 1.121 | 2.598 |
| T stage | 0.368 | 0.206 | 3.187 | 1 | 0.076 | 1.453 | 0.956 | 2.156 |
| Age | 0.494 | 0.207 | 5.721 | 1 | 0.016 | 1.635 | 1.004 | 2.448 |
| Age | 0.552 | 0.212 | 6.798 | 1 | 0.009 | 1.747 | 1.165 | 2.628 |
Discussion
Nasopharyngeal carcinoma, after a timely and
standardized radical radiotherapy or integrated radiotherapy and
chemotherapy, can lead to local and/or regional recurrence in
20–30% of patients. Local nasopharyngeal and skull-based recurrence
are the main reasons for the failure of local treatment of NPC
after radiotherapy (9–11). Retrospective studies have shown that
salvage therapy can improve survival in patients with a single
local recurrence (especially those with local recurrence of T1-2)
(12). For nasopharyngeal local
recurrence of T1-2, surgery or follow-up treatment is an effective
means of NPC (13). Some radiotherapy
centers reported treatment results showing that intraluminal or
interstitial brachytherapy was also feasible for patients with
local recurrence of NPC (14,15). Accordingly, Law et al (16) showed that, the use of 192Ir
interstitial particles DT50-55 Gy could lead to a 5-year local
control rate of 85% and moderate as well as severe complications
occurrence rate of 47%. Leung et al used high-dose rate of
intracavitary and external irradiation treatment for recurrent NPC
(17). The results showed that
although the high dose of radiation was strong enough to kill local
cancer cells, it could also cause local early recurrence due to
normal tissue damage and interstitial cell damage.
In the present study, the patients with NPC were
treated with different doses of radiation ranging from 58 to 68 Gy.
The results showed that the three groups of patients had 5-year OS,
DFS and regional recurrence-free survival rates as 43.2 vs. 64.53
vs. 75%, 29.13 vs. 42.82 vs. 39.7% and 30.76 vs. 44.19 vs. 45.4%.
The treatment effect of 62/1.8–2 Gy was similar to that of 68/1.8–2
Gy, but 68/1.8–2 Gy showed more adverse reactions than 62/1.8–2 Gy.
Therefore, we believe that 62/1.8–2 Gy can be used as a safe and
effective dose for 3D-CRT treatment of NPC. Age may be the main
prognostic risk factor for patients with NPC (18). Previous findings have shown that
radiation dose in the treatment of cancer may be positively
correlated with an increase in side effects. Chang et al
treated 35 patients with recurrent NPC using 3D-CRT (19). The results showed that the median
survival rates of radiotherapy after 1, 2 and 3 years were 54.9,
30.2 and 22.9%, respectively. Additionaly, long-term adverse
reactions included hearing loss and difficulty in mouth opening
compared to the conventional group, albeit no brain necrosis was
found. Our study further explored the dose and safety of
three-dimensional radiotherapy, and further determined 62/1.8–2 Gy
as a therapeutic dose with certain clinical applicability. Teo
et al reported that more than 900 patients with recurrences
showed better therapeutic effects when the radiation dose was ≥60
Gy (20). Those authors, however, did
not explore in-depth the radiation dose ≥60 Gy, and the DFS and OS
rates of patients. In this study, the 62 and 68 Gy radiation doses
were further categorized and explored because of differences in the
patient population and the number of patients enrolled in the
study. We found that 62/1.8–2 Gy was safer and more effective as a
three-dimensional radiotherapy dose and could lead to longer OS and
DFS.
In conclusion, we believe that the dose of 62/1.8–2
Gy of 3D-CRT is a safe, effective and adverse-reaction-tolerable
NPC treatment with good clinical values.
References
|
1
|
Lv X, Xia WX, Ke LR, Yang J, Qiu WZ, Yu
YH, Liang H, Huang XJ, Liu GY, Zeng Q, et al: Comparison of the
short-term efficacy between docetaxel plus carboplatin and
5-fluorouracil plus carboplatin in locoregionally advanced
nasopharyngeal carcinoma. Onco Targets Ther. 9:5123–5131. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zeng Q, Wang J, Lv X, Li J, Yin LJ, Xiang
YQ and Guo X: Induction chemotherapy followed by radiotherapy
versus concurrent chemoradiotherapy in elderly patients with
nasopharyngeal carcinoma: Finding from a propensity-matched
analysis. BMC Cancer. 16:6932016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ho S, Ip W, Chu S, Chan S, Lee B, Chan B,
Lee J, Flynn B, Ho W, Sin J, et al: Treatment regret in long-term
survivors of nasopharyngeal carcinoma treated with radical
radiotherapy. Clin Oncol (R Coll Radiol). 29:e472017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cao C, Luo J, Gao L, Yi J, Huang X, Li S,
Xiao J, Zhang Z and Xu G: Magnetic resonance imaging-detected
intracranial extension in the T4 classification nasopharyngeal
carcinoma with intensity-modulated radiotherapy. Cancer Res Treat.
49:518–525. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lu L, Li J, Zhao C, Xue W, Han F, Tao T,
Chang H, Jia W and Lu T: Prognostic efficacy of combining tumor
volume with Epstein-Barr virus DNA in patients treated with
intensity-modulated radiotherapy for nasopharyngeal carcinoma. Oral
Oncol. 60:18–24. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Maingon P, Blanchard P, Bidault F and
Calmels L: Radiotherapy for nasopharyngeal carcinoma. Cancer
Radiother. 20:S104–S109. 2016.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang D, Li YH, Fu J and Wang H: Diffusion
kurtosis imaging study on temporal lobe after nasopharyngeal
carcinoma radiotherapy. Brain Res. 1648:387–393. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nakahara S, Hanamoto A, Seo Y, Miyaguchi
S, Yamamoto Y, Tomiyama Y, Yoshii T, Takenaka Y, Yoshioka Y,
Isohashi F, et al: Chemoradiotherapy with weekly low-dose docetaxel
and cisplatin concurrent with radiation for patients with locally
advanced nasopharyngeal carcinoma, followed by adjuvant
chemotherapy for selected patients. Jpn J Clin Oncol. 46:903–910.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ma Q, Wu D, Zeng LL, Shen H, Hu D and Qiu
S: Radiation-induced functional connectivity alterations in
nasopharyngeal carcinoma patients with radiotherapy. Medicine
(Baltimore). 95:e42752016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Brown E, Owen R, Harden F, Mengersen K,
Oestreich K, Houghton W, Poulsen M, Harris S, Lin C and Porceddu S:
Head and neck adaptive radiotherapy: Predicting the time to replan.
Asia Pac J Clin Oncol. 12:460–467. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wu SX, Chua DT, Deng ML, Zhao C, Li FY,
Sham JS, Wang HY, Bao Y, Gao YH and Zeng ZF: Outcome of
fractionated stereotactic radiotherapy for 90 patients with locally
persistent and recurrent nasopharyngeal carcinoma. Int J Radiat
Oncol Biol Phys. 69:761–769. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wong FC, Tung SY, Leung TW, Sze WK, Wong
VY, Lui CM and Yuen KK OSK: Treatment results of high-dose-rate
remote afterloading brachytherapy for cervical cancer and
retrospective comparison of two regimens. Int J Radiat Oncol Biol
Phys. 55:1254–1264. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lu J, Cooper J and Lee A: Nasopharyngeal
Cancer: Multidisciplinary Management. Springer-Verlag; Berlin,
Heidelberg: pp. 253–265. 2010
|
|
14
|
Fee WE Jr, Moir MS, Choi EC and Goffinet
D: Nasopharyngectomy for recurrent nasopharyngeal cancer: A 2- to
17-year follow-up. Arch Otolaryngol Head Neck Surg. 128:280–284.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wei W: Cancer of the nasopharynx:
Functional surgical salvage. World J Surg. 27:844–848. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Law SC, Lam WK, Ng MF, Au SK, Mak WT and
Lau WH: Reirradiation of nasopharyngeal carcinoma with
intracavitary mold brachytherapy: An effective means of local
salvage. Int J Radiat Oncol Biol Phys. 54:1095–1113. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Leung TW, Tung SY, Sze WK, Sze WM, Wong VY
and Wong CS OSK: Salvage radiation therapy for locally recurrent
nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys.
48:1331–1338. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhang B, Mo Z, Du W, Wang Y, Liu L and Wei
Y: Intensity-modulated radiation therapy versus 2D-RT or 3D-CRT for
the treatment of nasopharyngeal carcinoma: A systematic review and
meta-analysis. Oral Oncol. 51:1041–1046. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chang JT, See LC, Liao CT, Ng SH, Wang CH,
Chen IH, Tsang NM, Tseng CK, Tang SG and Hong JH: Locally recurrent
nasopharyngeal carcinoma. Radiother Oncol. 54:135–142. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Teo PM, Kwan WH, Chan AT, Lee WY, King WW
and Mok CO: How successful is high-dose (> or = 60 Gy)
reirradiation using mainly external beams in salvaging local
failures of nasopharyngeal carcinoma? Int J Radiat Oncol Biol Phys.
40:897–913. 1998. View Article : Google Scholar : PubMed/NCBI
|