Introduction
Breast cancer is one of the most common types of
cancer among female malignancies, and has previously been
associated with high mortality worldwide (1). Primary breast cancer often occurs in the
twinned mammary gland, which accounts for 2–11% of female breast
tumors (2). Statistical data reveals
that numerous types of factor function in the recurrence and
metastasis of primary breast cancer subsequent to surgery (3). Primary breast tumor cells may
metastasize to a number of positions in the human body such as the
lung, bone and lymph node, a process involving a number of
biological processes including tumor cell proliferation, migration
and apoptosis (4,5). Surgery may be the best choice for
patients with primary cancer, which results in the necessary
administration of anesthesia. However, a possible association
between anesthetic techniques and primary breast cancer has been
reported (6).
Bupivacaine is a type of surgical local anesthetic,
and studies have demonstrated that the excessive administration of
bupivacaine results in central nervous system and cardiovascular
system poisoning (7,8). Bupivacaine has been wildly used in
clinical surgeries such as tonsillectomy, neuroleptanalgesia and
tumor resections. A low dose of bupivacaine yielded satisfactory
postoperative effects on female ovarian cancer resection, with
little influence on hemodynamics and postoperative adverse
reactions (9,10). Previous studies have demonstrated that
anesthesia during primary breast cancer surgery may influence
recurrence or metastasis (11). The
administration of bupivacaine has been examined in breast cancer
resection surgery. For example, the addition of 1 µg/kg
dexmedetomidine to 0.25% bupivacaine in paravertebral analgesia for
patients undergoing modified radical mastectomy surgery, for the
treatment of breast cancer, yielded no serious side effects
(12). However, the mechanism of
several types of anesthesia, including bupivacaine, on breast
cancer recurrence and metastasis remain unclear.
The abnormal expression of leucine rich repeat
containing 3B (LRRC3B) has been reported in numerous types of
cancer such as breast, colon and ovarian (13,14). An
increasing number of studies have mentioned the pivotal role of
LRRC3B in tumor development and progression. For instance, Kim
et al (15) reported that
LRRC3B was a tumor suppressor for gastric cancer. Furthermore,
LRRC3B was downregulated in a renal cell carcinoma line, which
suggests that LRRC3B could be involved in the process of
carcinogenesis as a tumor suppressor (13,16).
Additionally, abnormal expression of LRRC3B may serve as a useful
marker for diagnosis and prognosis in breast carcinoma (17). Despite numerous studies being focused
on the effect of LRRC3B expression in tumor pathogenesis, the
potential role of LRRC3B on breast cancer cell invasion
post-anesthesia has not been studied.
The present study used 2 types of breast cancer cell
lines to assess the effect and potential mechanism of LRRC3B
silencing on breast cancer cell invasion post-anesthesia. A number
of experimental methods were used to assess the effect of LRRC3B
silencing and bupivacaine on breast cancer cell invasion. The
present study aimed to investigate the potential role of LRRC3B on
breast cancer cell invasion post-anesthesia and may provide a
theoretical basis for the mechanism of LRRC3B in breast cancer cell
invasion following the administration of anesthetic.
Materials and methods
Cell culture and drug treatment
Human breast cancer MDA-MB-231 and MCF-7 cell lines
(American Type Culture Collection, Manassas, VA, USA) were cultured
in Dulbecco's modified Eagle's medium (DMEM; Sigma-Aldrich; Merck
KGaA, Darmstadt, Germany) containing 10% fetal bovine serum (FBS;
Hyclone, Logan, UT, USA), 100 U/ml penicillin and 100 U/ml
streptomycin (Invitrogen; Thermo Fisher Scientific Inc., Waltham,
MA, USA) at 37°C with 5% CO2.
Bupivacaine (Sigma-Aldrich; Merck KGaA) was diluted
in dimethyl sulfoxide (DMSO) to 10 mg/ml and stored at room
temperature with no exposure to light. Consequently, bupivacaine
was diluted to concentrations of 1, 10, 20, 50 and 100 µg/ml for
breast cancer cell treatment. The cells treated with DMSO only were
considered as the control group.
Small interfering RNA (siRNA)
transfection
The target sequence for LRRC3B specific siRNA was
purchased from Santa Cruz Biotechnology, Inc. (Dallas, TX, USA).
siRNA with no silencing sequence was transfected as control group.
Cell transfection was conducted with Lipofectamine® 2000
reagent (Invitrogen; Thermo Fisher Scientific, Inc.) according to
manufacturers protocol. G418 (Sigma-Aldrich; Merck KGaA) was used
for the stable LRRC3B transfectants selection (18).
Cellular invasion assay
For the cellular invasion ability assay, the
Matrigel method was used as previously described (19). The cells in each group previously
cultured for 48 h were incubated in serum-free DMEM medium
containing 10% FBS for 24 h at 37°C. The upper Transwell chamber
(Corning Incorporated, Corning, NY, USA) was covered with
serum-free DMEM supplemented with 50 mg/l Matrigel and air-dried at
4°C. Following the removal of the medium, 50 µl fresh serum-free
medium containing 10 g/l bovine serum albumin (Beijing Solarbio
Science and Technology Co., Ltd., Beijing, China) was added to the
upper chamber, and the cells were cultured for 30 min at 37°C.
Transwell inserts were subsequently added to the 24-well plates and
the plates were cultured with DMEM mixed with 10% FBS. MDA-MB-231
and MCF-7 cells (5×104 cells/well) in the Transwell
inserts were then suspended in serum-free DMEM. Subsequent to 48 h,
the Transwell inserts in each group were washed with PBS buffer to
remove the upper cells on the microporous membrane, subsequent to
fixing in ice-cold alcohol. Finally, the Transwell inserts from
each group were stained with 0.1% crystal violet for 30 min, and
washed with 33% acetic acid. The absorbance of the eluents was
observed at a wavelength of 570 nm using a microplate reader
(Bio-Rad Laboratories, Inc., Hercules, CA, USA). The Transwell
chambers in the control group were treated without Matrigel.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR) analysis
Total RNA was extracted from the breast cancer cells
and cultured for 48 h at 4°C using TRIzol Reagent (Invitrogen;
Thermo Fisher Scientific, Inc.) as previously described (20) and was treated with RNse-free Dnase I
(Promega Corporation, Madison, WI, USA). The concentration and
purity of the isolated RNA was measured with SMA 400 UV0VIS
(Merinton Instrument, Ltd., Shanghai, China). Purified RNA at a
density of 0.5 µg/µl with nuclease-free water was used for cDNA
synthesis with the PrimerScript 1st Strand cDNA Synthesis kit
(Invitrogen; Thermo Fisher Scientific, Inc.). The expression level
of LRRC3B in bupivacaine pre-treated MDA-MB-231 and MCF-7 cells
were detected in an Eppendorf Mastercycler (Brinkmann Instruments
Inc., Westbury, NY, USA) using the SYBR ExScript RT-qPCR kit
(Takara Biotechnology Co., Ltd., Dalian, China). LRRC3B expression
in cells without bupivacaine treatment served as negative controls.
The experiment was repeated three times. The total reaction system
of 20 µl volume was as follows: 1 µl cDNA, 10 µl SYBR Premix EX
Taq, 1 µl each of the primers (10 µM), and 7 µl double-distilled
H2O. The PCR program was performed using Taq DNA
polymerase (Roche Diagnostics, Basel, Switzerland) as follows:
Denaturation at 50°C for 2 min; 95°C for 10 min; 45 cycles at 95°C
for 10 sec; 60°C for 1 min. Melting curve analysis of the
amplification products was performed at the end of each PCR to
confirm that only 1 product was amplified and detected. Data were
analyzed according to the 2−ΔΔCq method (21) and were normalized to
glyceraldehyde-3-phosphate dehydrogenase (GAPDH) expression in each
sample. Primers used for targets amplification were as follows:
LRRC3B sense, 5′-GAGGTATTGGTTGGGTTTTG-3′, and anti-sense,
5′-AACCCAACTACCCACCTAA-3′; and GAP DH sense,
5′-TATGATGATATCAAGAGGGTAGT-3′, and anti-sense,
5′-TGTATCCAAACTCATTGTCATAC-3′.
Western blot analysis
The two types of breast cancer cells were lysed by
culturing for 48 h at 4°C in lysis buffer (Sigma-Aldrich; Merck
KGaA). The cells were then centrifuged at 300 × g for 10 min at
4°C. The supernatant was collected to determine the protein
concentration using a bicinchoninic acid assay kit (Pierce; Thermo
Fisher Scientific, Inc.). For western blotting (22), 30 µg cell lysate protein was separated
by 10% SDS-PAGE, subsequently the gels were transferred onto a
polyvinylidene difluoride (PVDF) membrane (EMD Millipore,
Billerica, MA, USA). The membrane was blocked in TBS and Tween-20
(TBST) containing 5% non-fat milk for 1 h. The membrane was then
incubated with anti-LRRC3B antibody (catalog no. HPA015568) and
anti-GAPDH antibody (1:100; catalog no. SAB2103104;, Sigma-Aldrich;
Merck KGaA), overnight at 4°C. The membrane was incubated with
horseradish peroxidase labeled anti-rabbit secondary antibody
(1:1,000; catalog no. 7054; Cell Signaling Technology, Danvers, MA,
USA) at room temperature for 1 h. The PVDF membrane was
subsequently washed with 1X TBST buffer for 10 min 3 times.
Detection was conducted with X-rays using the enhanced
chemiluminescence (ECL) reagent (GE Healthcare, Chalfont, UK).
GAPDH served as the internal control.
Statistical analysis
All experiments were conducted independently in
triplicate. All experimental data is presented as the mean ±
standard deviation and was performed using GraphPad Prism 5.0
software (GraphPad Software Inc., La Jolla, CA, USA). A post hoc
Tukey's test was used to calculate the differences between groups.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Expression of LRRC3B in breast cancer
cell lines
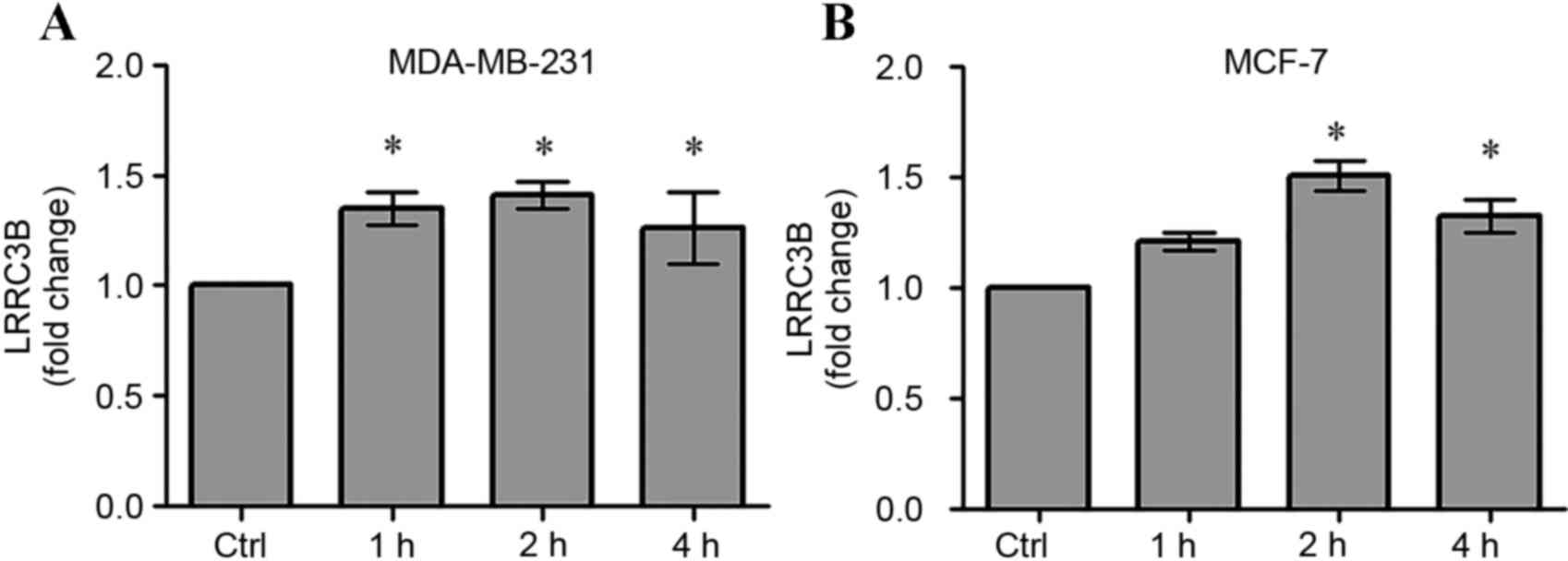
The expression of LRRC3B in each type of breast
cancer cell line was analyzed using RT-qPCR (Fig. 1). The results showed that the fold
change of LRRC3B significantly increased as time increased, up to 2
h, compared with the control in the MDA-MB-231 cell line, declining
slightly at 4 h (P<0.05, Fig. 1A).
The same tendency with respect to LRRC3B expression was exhibited
in the MCF-7 cell line (P<0.05, Fig.
1B). The aforementioned results suggested that LRRC3B was
overexpressed in the breast cancer cell lines.
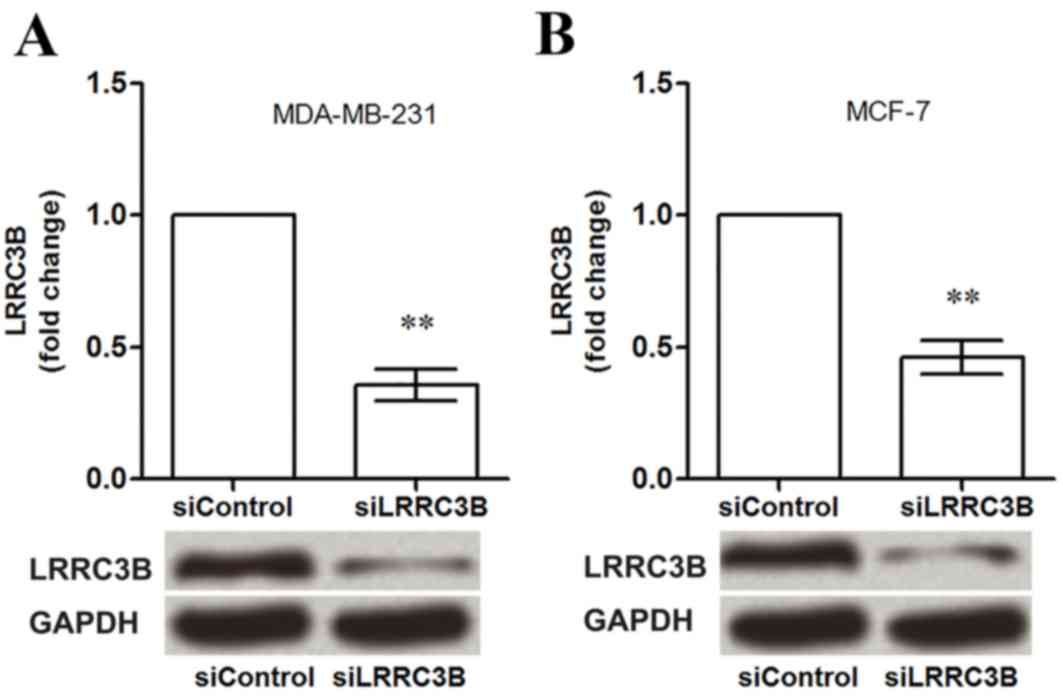
In addition, when the breast cancer MDA-MB-231 and
MCF-7 cell lines were transfected with siRNA-LRRC3B plasma, the
expression of LRRC3B was detected with western blotting (Fig. 2). The results suggested that LRRC3B
was downregulated in the MDA-MB-231 and MCF-7 cell lines.
Influence of siLRRC3B on protein
expression in breast cancer cells
RT-qPCR analysis showed that when the breast cancer
cells were transfected with a siLRRC3B vector, LRRC3B mRNA
expression in MDA-MB-231 and MCF-7 cells significantly decreased
compared with the controls (P<0.01; Fig. 2). A similar pattern of LRRC3B
expression was observed in the western blotting, suggesting that
LRRC3B silencing exerted an effect on LRRC3B expression in breast
cancer cells.
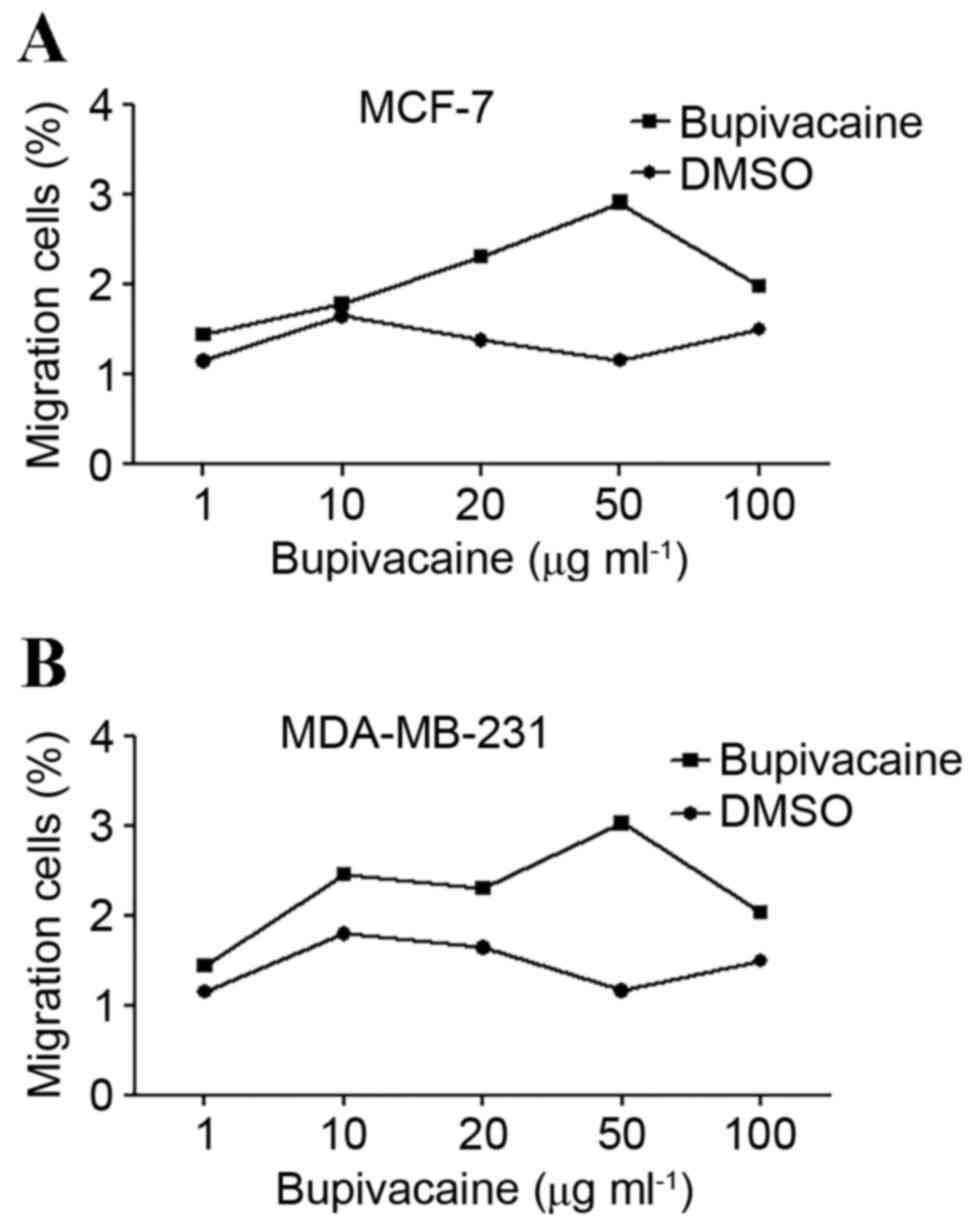
Effect of bupivacaine on breast cancer
cell invasion
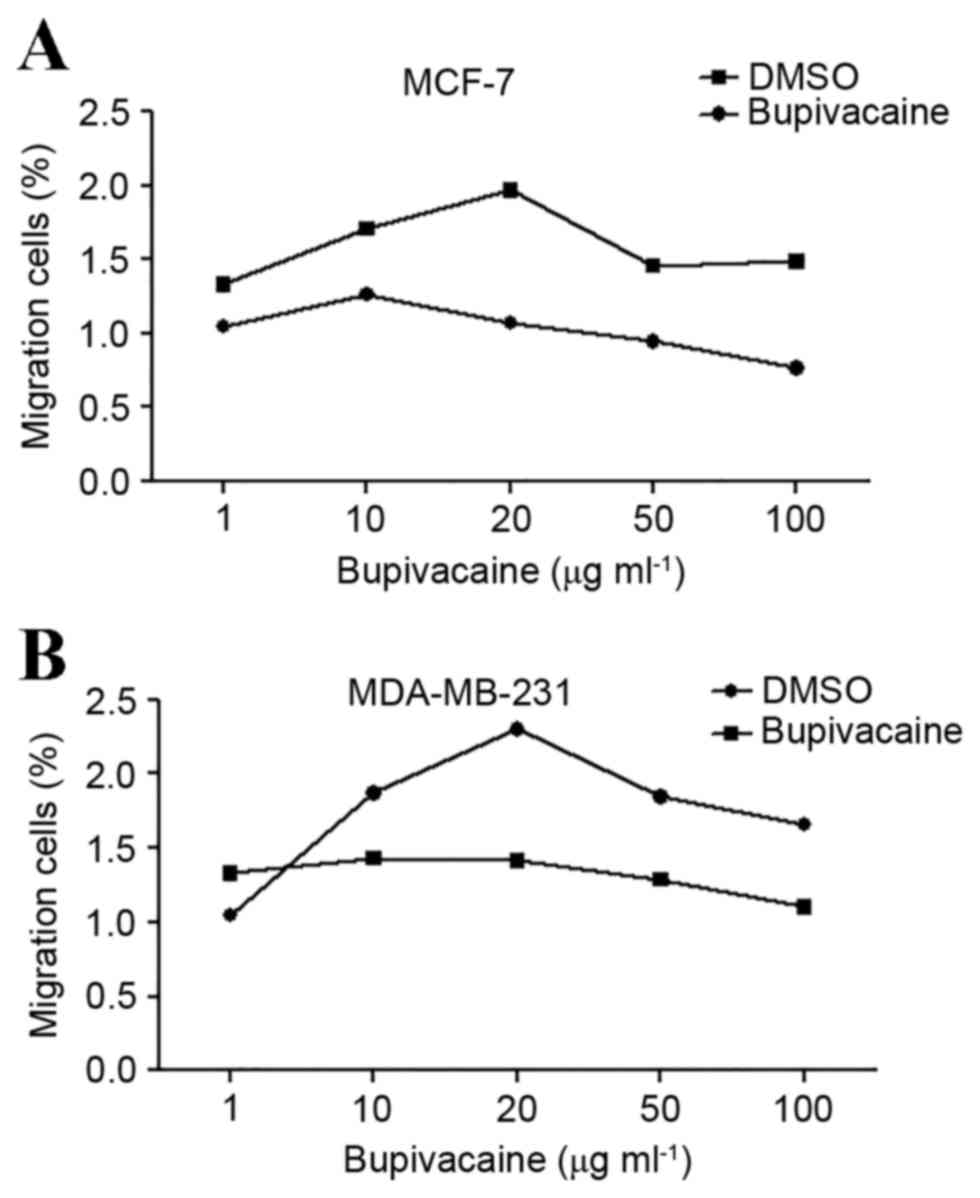
Transwell assay was used to assess the effect of
bupivacaine on breast cancer cell invasion (Fig. 3). Compared with the control DMSO
group, the percentage migrated MCF-7 cells increased as bupivacaine
concentration increased until 50 µg/ml and declined when
bupivacaine concentration exceeded 50 µg/ml (Fig. 3A). However, the effect of bupivacaine
at different concentrations on MDA-MB-231 cells was not the same as
the effect in MCF-7 cells, with the results revealing that the
concentration of bupivacaine that yielded the largest percentage
migrated cells was 50 µg/ml (Fig.
3B). This data suggested that 50 µg/ml bupivacaine promoted
breast cancer cell invasion in the 2 cell types.
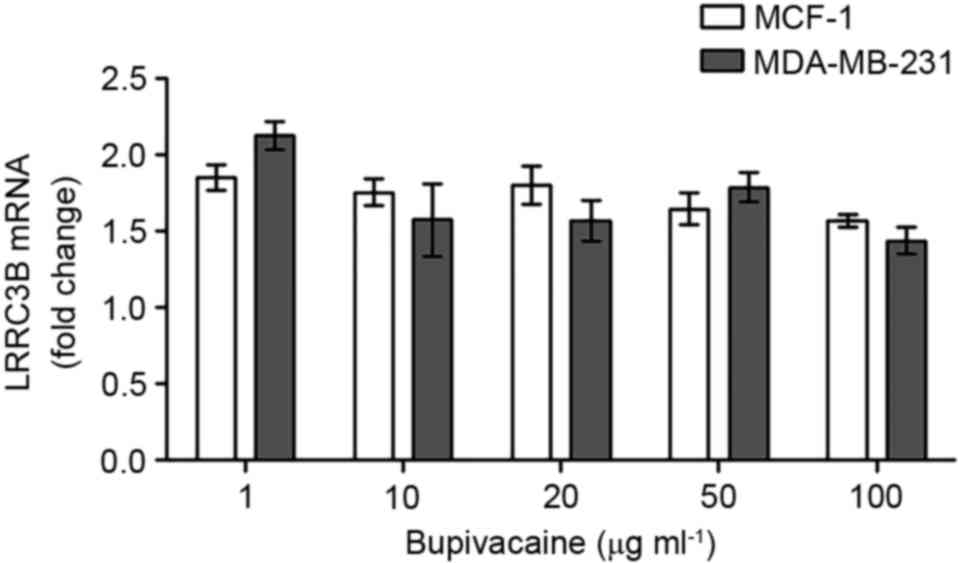
LRRC3B mRNA expression in breast
cancer cells exposed to bupivacaine
The mRNA expression of LRRC3B in breast cancer cells
post-anesthesia was measured using RT-qPCR analysis (Fig. 4). No significant difference was
indicated for LRRC3B expression in MCF-7 or MDA-MB-231 cells at a
variety of bupivacaine concentrations. However, the LRRC3B mRNA
expression reduced slightly at a high concentration (100 µg/ml) of
bupivacaine.
Effects of LRRC3B silencing on breast
cancer cells exposed to bupivacaine
When the breast cancer cells were transfected with
siLRRC3B plasma, the percentage migrated cells was highest at 20
µg/ml bupivacaine in MDA-MB-231 and MCF-7 cells (Fig. 5), indicating that LRRC3B silencing
suppresses bupivacaine-induced breast cancer cell invasion.
Discussion
Previous studies have reported that the
administration of anesthetics may serve pivotal roles in cancer
recurrence and metastasis during primary breast cancer surgery
(6,23). LRRC3B has been revealed to perform an
important role in numerous types of cancer, however, there were
previously no studies about the function of LRRC3B in breast cancer
recurrence and metastasis post-anesthesia. The present study
assessed the potential function of LRRC3B in breast cancer cell
invasion subsequent to being treated with the anesthetic
bupivacaine. The data showed that LRRC3B expression was inhibited
by bupivacaine application. However, when LRRC3B was silenced, the
effect of bupivacaine on breast cancer cell invasion was reversed,
indicating the role of LRRC3B in the suppression of
bupivacaine-induced breast cancer cell invasion.
The present study showed that LRRC3B expression
increased significantly in breast cancer MDA-MB-231 and MCF-7 cell
lines, but decreased significantly when the cells were transfected
with siRNA-LRRC3B (P<0.05). LRRC3B has been reported to be a
tumor suppressor for gastric cancer (24), and Tian et al (25) revealed the tumor suppressor role of
LRRC3B in colorectal cancer using a gene silencing method. The role
of LRRC3B in breast cancer has not been fully discussed, even in
primary breast cancer surgery. Based on the results of the present
study, LRRC3B overexpression was speculated to be associated with
breast cancer. However, the results showed that the application of
50 µg/ml bupivacaine yielded the maximum effect on breast cancer
cell invasion, suggesting that bupivacaine administration may be
associated with recurrence and metastasis in post-primary breast
cancer surgery (26). Therefore, the
present study investigated the association between bupivacaine and
LRRC3B expression in breast cancer cells.
In the present study, LRRC3B expression levels
decreased in breast cancer MDA-MB-231 and MCF-7 cells that were
treated with different concentrations of bupivacaine, indicating
that the administration of bupivacaine to breast cancer tumor cells
suppressed the expression of LRRC3B. A number of studies have
revealed that bupivacaine administration during cancer surgery
serves a crucial role in cancer recurrence and metastasis by
promoting cell migration (27,28). In
line with previous studies, the data of the present study showed
that 50 µg/ml bupivacaine yielded the maximum increase breast cell
invasion. However, this effect was inhibited by LRRC3B silencing
(Fig. 5). Jørgensen et al
(29) demonstrated that the
downregulation of LRRC3B inhibited the migration of breast cancer
cells (29). The present study
speculated, based on the aforementioned results, that LRRC3B
silencing may perform a protective role in preventing breast cancer
recurrence, post-bupivacaine, by suppressing cell invasion.
In conclusion, the data presented in the present
study suggests that LRRC3B silencing may serve a protective role by
preventing breast cancer recurrence and metastasis post-anesthesia
in vitro. LRRC3B downregulation suppressed the breast cancer
cell invasion caused by bupivacaine administration. The present
study may provide a theoretical basis for the mechanism of action
of LRRC3B and the clinical application of the gene in breast
cancer. However, additional experimental studies are required to
investigate the mechanism.
References
|
1
|
Mariotto AB, Noone AM, Howlader N, Cho H,
Keel GE, Garshell J, Woloshin S and Schwartz LM: Cancer survival:
An overview of measures, uses, and interpretation. J Natl Cancer
Inst Monogr. 49:145–186. 2014. View Article : Google Scholar
|
|
2
|
Senkus E, Kyriakides S, Ohno S,
Penault-Llorca F, Poortmans P, Rutgers E, Zackrisson S and Cardoso
F: ESMO Guidelines Committee: Primary breast cancer: ESMO clinical
practice guidelines for diagnosis, treatment and follow-up. Ann
Oncol. 26 Suppl 5:v8–v30. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Voogd AC, Nielsen M, Peterse JL,
Blichert-Toft M, Bartelink H, Overgaard M, van Tienhoven G,
Andersen KW, Sylvester RJ, van Dongen JA, et al: Differences in
risk factors for local and distant recurrence after
breast-conserving therapy or mastectomy for stage I and II breast
cancer: Pooled results of two large European randomized trials. J
Clin Oncol. 19:1688–1697. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Al-Sahaf O, Wang JH, Browne TJ, Cotter TG
and Redmond HP: Surgical injury enhances the expression of genes
that mediate breast cancer metastasis to the lung. Ann Surg.
252:1037–1043. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang Y, Klijn JG, Zhang Y, Sieuwerts AM,
Look MP, Yang F, Talantov D, Timmermans M, Meijer-van Gelder ME, Yu
J, et al: Gene-expression profiles to predict distant metastasis of
lymph-node-negative primary breast cancer. Lancet. 365:671–679.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Exadaktylos AK, Buggy DJ, Moriarty DC,
Mascha E and Sessler DI: Can anesthetic technique for primary
breast cancer surgery affect recurrence or metastasis?
Anesthesiology. 105:660–664. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Marwick PC, Levin AI and Coetzee AR:
Recurrence of cardiotoxicity after lipid rescue from
bupivacaine-induced cardiac arrest. Anesth Analg. 108:1344–1346.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lange DB, Schwartz D, DaRoza G and Gair R:
Use of intravenous lipid emulsion to reverse central nervous system
toxicity of an iatrogenic local anesthetic overdose in a patient on
peritoneal dialysis. Ann Pharmacother. 46:e372012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
de Oliveira GS Jr, Ahmad S, Schink JC,
Singh DK, Fitzgerald PC and McCarthy RJ: Intraoperative neuraxial
anesthesia but not postoperative neuraxial analgesia is associated
with increased relapse-free survival in ovarian cancer patients
after primary cytoreductive surgery. Reg Anesth Pain Med.
36:271–277. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lacassie HJ, Cartagena J, Brañes J, Assel
M and Echevarría GC: The relationship between neuraxial anesthesia
and advanced ovarian cancer-related outcomes in the chilean
population. Anesth Analg. 117:653–660. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ecimovic P, Murray D, Doran P and Buggy
DJ: Propofol and bupivacaine in breast cancer cell function in
vitro-role of the NET1 gene. Anticancer Res. 34:1321–1331.
2014.PubMed/NCBI
|
|
12
|
Mohamed SA, Fares KM, Mohamed AA and
Alieldin NH: Dexmedetomidine as an adjunctive analgesic with
bupivacaine in paravertebral analgesia for breast cancer surgery.
Pain Physician. 17:E589–E598. 2014.PubMed/NCBI
|
|
13
|
Haraldson K, Kashuba VI, Dmitriev AA,
Senchenko VN, Kudryavtseva AV, Pavlova TV, Braga EA, Pronina IV,
Kondratov AG, Rynditch AV, et al: LRRC3B gene is frequently
epigenetically inactivated in several epithelial malignancies and
inhibits cell growth and replication. Biochimie. 94:1151–1157.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kobe B and Kajava AV: The leucine-rich
repeat as a protein recognition motif. Curr Opin Struct Biol.
11:725–732. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kim M, Kim JH, Jang HR, Kim HM, Lee CW,
Noh SM, Song KS, Cho JS, Jeong HY, Hahn Y, et al: LRRC3B, encoding
a leucine-rich repeat-containing protein, is a putative tumor
suppressor gene in gastric cancer. Cancer Res. 68:7147–7155. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tian XQ, Zhang Y, Sun D, Zhao S, Xiong H
and Fang J: Epigenetic silencing of LRRC3B in colorectal cancer.
Scand J Gastroenterol. 44:79–84. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wang Y, Peng Y, Zhou Y and Zhong H: The
clinical value of LRRC3B gene expression and promoter
hypermethylation in breast carcinomas. Cell Biochem Biophys.
70:1035–1041. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
You Y, Yang W, Qin X, Wang F, Li H, Lin C,
Li W, Gu C, Zhang Y and Ran Y: ECRG4 acts as a tumor suppressor and
as a determinant of chemotherapy resistance in human nasopharyngeal
carcinoma. Cell Oncol (Dordr). 38:205–214. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li Y, Han N, Yin T, Huang L, Liu S, Liu D,
Xie C and Zhang M: Lentivirus-mediated Nox4 shRNA invasion and
angiogenesis and enhances radiosensitivity in human glioblastoma.
Oxid Med Cell Longev. 2014:5817322014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liang Z, Wu H, Reddy S, Zhu A, Wang S,
Blevins D, Yoon Y, Zhang Y and Shim H: Blockade of invasion and
metastasis of breast cancer cells via targeting CXCR4 with an
artificial microRNA. Biochem Biophys Res Commun. 363:542–546. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chow SE, Kao CH, Liu YT, Cheng ML, Yang
YW, Huang YK, Hsu CC and Wang JS: Resveratrol induced ER expansion
and ER caspase-mediated apoptosis in human nasopharyngeal carcinoma
cells. Apoptosis. 19:527–541. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Deegan CA, Murray D, Doran P, Moriarty DC,
Sessler DI, Mascha E, Kavanagh BP and Buggy DJ: Anesthetic
technique and the cytokine and matrix metalloproteinase response to
primary breast cancer surgery. Reg Anesth Pain Med. 35:490–495.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kim M, Kim JH, Jang HR, Kim HM, Lee CW,
Noh SM, Song KS, Cho JS, Jeong HY, Hahn Y, et al: LRRC3B, encoding
a leucine-rich repeat-containing protein, is a putative tumor
suppressor gene in gastric cancer. Cancer Res. 68:7147–7155. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Tian XQ, Zhang Y, Sun D, Zhao S, Xiong H
and Fang J: Epigenetic silencing of LRRC3B in colorectal cancer.
Scand J Gastroenterol. 44:79–84. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sessler DI, Ben-Eliyahu S, Mascha EJ,
Parat MO and Buggy DJ: Can regional analgesia reduce the risk of
recurrence after breast cancer? Methodology of a multicenter
randomized trial. Contemp Clin Trials. 29:517–526. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
de Leon-Casasola O, Parker B, Lema MJ,
Harrison P and Massey J: Postoperative epidural
bupivacaine-morphine therapy. Experience with 4,227 surgical cancer
patients. Anesthesiology. 81:368–375. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lee GW, Park H, Kim EJ, Cho YW, Kim GT,
Mun YJ, Choi EJ, Lee JS, Han J and Kang D: Reduction of breast
cancer cell migration via up-regulation of TASK-3 two-pore domain
K+ channel. Acta Physiol (Oxf). 204:513–524. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jørgensen JR, Juliusson B, Henriksen KF,
Hansen C, Knudsen S, Petersen TN, Blom N, Seiger A and Wahlberg LU:
Identification of novel genes regulated in the developing human
ventral mesencephalon. Exp Neurol. 198:427–473. 2006. View Article : Google Scholar : PubMed/NCBI
|