Introduction
Breast cancer is the second most common type of
cancer globally. Although the majority of patients have a good
outcome, the morbidity rate is increasing rapidly. In 2017, an
estimated 252,710 females and 2,470 males will be diagnosed with
invasive breast cancer, and ~40,610 females and 460 males are
expected to succumb to the disease (1). In China, female breast cancer was the
most prevalent cancer in 2011, with the 5-year prevalence estimate
reaching 1.02 million (2).
In the investigation of breast cancer, an excessive
intake of dietary fat, obesity and diabetes have been found to be
associated with cancer development (3). Free fatty acids (FFAs) act as substrates
in energy metabolism and mediators in signal transduction, and are
stored as lipid droplets (LDs) in hepatocytes and supply energy
under poor conditions (4,5). A growing number of in vitro cell
culture, animal cancer model and epidemiological studies, and
clinical studies in human subjects, have provided evidence to
support the effects of FFAs on cancer since almost 40 years ago
(6–9).
Unsaturated FFAs stimulated the proliferation of human breast
cancer cells, whereas saturated FFAs inhibited cell proliferation
and increased apoptosis (8). The high
dietary intake of n-3 polyunsaturated fatty acids (PUFAs) shows a
protective association with cancer risk (9); however, n-6 PUFAs are associated with an
increased risk for the development of breast cancer (6,10). The
mechanism of PUFAs remains unclear.
Autophagy has gained attention recently as an
essential contributor to human disease. The term ‘autophagy’ is
derived from Greek, meaning ‘self-eat’. As the only mechanism to
degrade large structures such as organelles and protein aggregates,
it has a double-edged role in human health and metabolism (11). In addition to its ability to promote
cancer by allowing cells to survive under conditions of metabolic
and genotoxic stress, excessive autophagy may paradoxically lead to
cell death (12). Successful
completion of the complex process of autophagy requires the
coordinated function of a number of proteins and complexes at
different steps, and tight regulation of each step by upstream
modulators aids in fine-tuning the autophagic process (13,14).
Autophagy is considered to promote cancer by
allowing cells to survive under conditions of metabolic and
genotoxic stress, and is additionally associated with cancer cell
death induced by autophagic lysosome features (15). At present, no study has identified an
association between autophagy and FFA-induced breast cancer cell
metabolism. In the present study, we created high FFA condition by
using two types of FFA to assess the effect of FFAs on human breast
cancer MDA-MB-231 cells and identify a possible role of
autophagy.
Materials and methods
Cell culture and reagents
Human breast cancer MDA-MB-231 cells were cultured
in high-glucose Dulbecco's modified Eagle's medium (DMEM; HyClone;
GE Healthcare Life Sciences, Logan, UT, USA) containing 10% fetal
bovine serum (FBS) (ScienCell Research Laboratories, Inc.,
Carlsbad, CA, USA) and 1% penicillin/streptomycin (Invitrogen;
Thermo Fisher Scientific, Inc., Waltham, MA, USA) at 37°C in a
humidified atmosphere containing 5% CO2. Palmitate acid
(PA) and oleic acid (OA) were purchased from Sigma-Aldrich (Merck
KGaA, Darmstadt, Germany), and essentially fatty acid-free bovine
serum albumin (BSA) was obtained from Roche Applied Science
(Penzberg, Germany). The stock solutions of fatty acids bound to 5%
BSA were prepared as follows. The corresponding fatty acid was
dissolved in a small amount of ethanol in a 37°C water bath, and
then mixed with 5% fatty acid-free BSA to obtain a 10 mM fatty acid
stock solution. Subsequent to being adjusted to pH 7.4, the
solution was filtered through a 0.45 µm filter. Finally, the
solutions were subpackaged and stored at −20°C; equal ethanol and
BSA were prepared as a control. The fatty acid stock solutions were
then diluted in culture medium to obtain various concentrations of
working solution, 0.25, 0.50 and 0.75 mmol/l; the control was
always selected with the maximum concentration of BSA (0.25%). The
antibody against LC3 (M152-3) was purchased from (Medical and
Biological Laboratories, Nagoya, Japan), whereas the anti-β-actin
antibody (cat. no. 37008H10D10), horse anti-mouse IgG (cat. no.
7076) and goat anti-rabbit IgG (cat. no. 7074) antibodies were
purchased from Cell Signaling Technology, Inc. (Danvers, MA, USA).
LC3 and β-actin were diluted in 5% BSA with a ratio of 1:500,
whereas the anti-mouse IgG and the anti-rabbit IgG were diluted
with the ratio of 1:20,000 fresh before use. Bafliomycin A1 (BFA)
and 3-methyladenine (3-MA) were purchased from Sigma-Aldrich (Merck
KGaA). Rapamycin was purchased from MedChem Express (Monmouth
Junction, NJ, USA).
Proliferation assay
The MTT assay was used to evaluate cell
proliferation. MTT (Amresco, LLC, Solon, OH, USA) was dissolved in
ddH2O at a concentration of 5 mg/ml, filtered through a
0.22 µm filter, and stored at 4°C. Cells were seeded at a density
of 5,000 cells/well in 96-well plate and cultured in stand medium
at 37°C for at least 12 h until all cells were adhered. Then cells
were treated with different concentrations of culture medium
containing FFAs (0.25, 0.50 and 0.75 mmol/l) with 5% BSA or
FFA-free BSA for 24 h. For the proliferation assay, 20 µl MTT was
added into each well. An ELISA plate reader (BioTek Instruments,
Inc., Winooski, VT, USA) was used to measure the optical density at
490 nm.
TUNEL assay
The TUNEL assay was performed using an In
Situ Cell Death Detection kit (Roche Diagnostics, Basel,
Switzerland), according to the manufacturer's instructions. Cells
were seeded at a density of 2×105 cells/well in 24-well
plate and cultured in DMEM without FBS at 37°C for at least 12 h
until all cells were adhered. Subsequently, the cells were treated
with various concentrations of culture medium containing FFAs (0.25
and 0.50 mmol/l) with 5% BSA or FFA-free BSA for 24 h at 37°C.
Cells were fixed with 4% paraformaldehyde for 1 h at room
temperature. Then 0.2% TrionX-100 was used as a permeabilisation
solution for 20 min at 4°C prior to TUNEL reagent (enzyme solution,
label solution=1:9) and DAPI (100 ng/ml) were respectively used for
60 min and 10 min at 37°C to stain the nucleus. Finally, three
fields of view were randomly selected and images (magnification,
×400) were captured using the Olympus Fluo View FV1000 Confocal
Microscope (Olympus, Tokyo, Japan).
Wound healing assay
MDA-MB-231 cells were grown to confluent monolayers
on 6-well plates and a pipette tip (200 µl) was used to create
linear scratch wounds. Mitomycin C (Amresco, LLC) was used to
inhibit cell proliferation. Wound images were captured using a
digital camera mounted on a light microscope (magnification, ×200).
The wound gap widths were measured using ImageJ software (National
Institutes of Health, Bethesda, MD, USA).
Transwell assay
The upper chamber of each 8.0-µm pore size Transwell
apparatus (Corning Inc., Corning, NY, USA) was coated with Matrigel
(BD Biosciences, San Jose, CA, USA). MDA-MB-231 cells were added to
the upper chamber at a density of 2×106 cells/ml (100
µl/chamber) and incubated for 24 h, followed by removal of the
cells that remained in the top chamber with cotton swabs. Cells
that penetrated to the lower membrane surface were fixed in 4%
paraformaldehyde, stained with crystal violet, and counted under a
light microscope (magnification, ×400).
shRNA transfection
The autophagy protein 5 (ATG5) shRNA and a
non-specific shRNA (mock or control) were purchased from GeneChem,
Inc. (Daejeon, Korea). According to the manufacturer's
instructions, the transfections were performed at ~60% confluency
using Lipofectamine 2000 (Invitrogen; Thermo Fisher Scientific,
Inc.). For each transfection reaction, 4 µg shRNA was used for the
preparation of the shRNA-transfection complexes at room temperature
for 20 min. The transfections were performed in 293T cells.
Targeted MDA-MB-231 cell transfection was then performed using
obtained virus fluid from 293T cells under the addition of 1 µg/µl
polybrene for 24 h. Subsequent to incubation, the transfection
complexes were removed and replaced with their corresponding media
with puromycin. The transfection efficiency was determined by
western blotting. Successfully transfected MDA-MB-231 cells were
used for subsequent experiments one week after amplification.
Western blotting
Cells were collected with lysis buffer (Cell
Signaling Technology, Inc.) subsequent to being washed three times
with ice-cold PBS. Protein concentrations were determined using the
BCA assay (Sigma-Aldrich; Merck KGaA). Lysates were boiled in SDS
loading buffer for 10 min after cleared by centrifugation (12,000 ×
g, 10 min, 4°C). Immunoblotting was performed using 15% SDS-PAGE,
transferred to a nitrocellulose membrane and detected using
specific primary antibodies (LC3 and β-actin at 4°C overnight). The
immunocomplexes were incubated with the appropriate
fluorescein-conjugated horse anti-mouse IgG or the goat anti-rabbit
IgG antibody (1 h at room temperature) and detected using ECL. In
addition, 100 µg protein was loaded per well. The ECL visualization
reagent was purchased romm Cell Signaling Technology, Inc. and
mixed fresh prior to use.
Statistical analysis
Results are expressed as the mean ± standard error
of the mean. The quantification of the relative increase in protein
expression was performed using National Institutes of Health Scion
Image software and was normalized with the control protein
expression in each experiment. The values were representative of at
least three independent experiments. Differences between mean
values were examined using the paired Student's t-test. P<0.05
was considered to indicate a statistically significant
difference.
Results
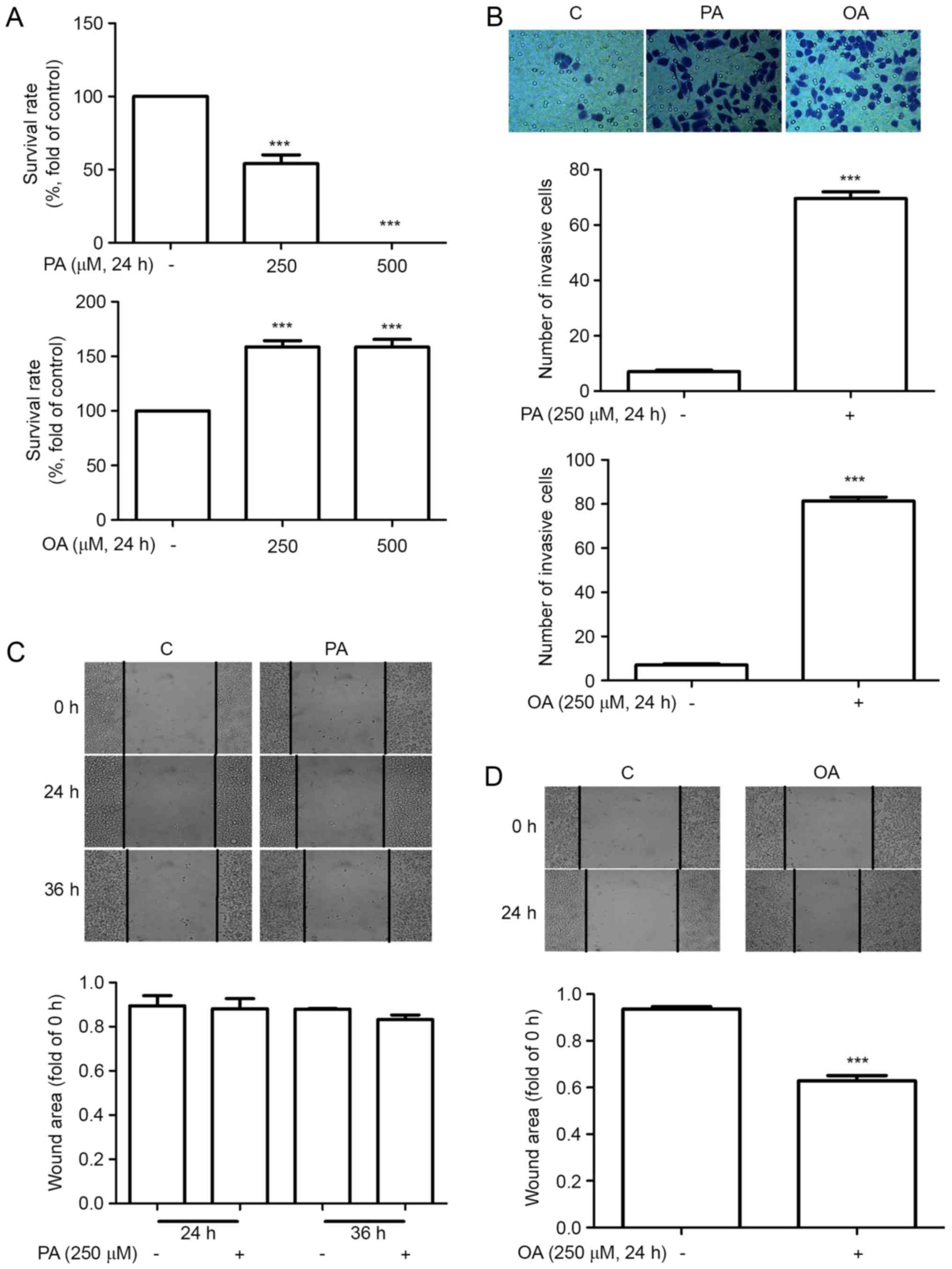
Different effects of PA and OA on
MDA-MB-231 cell growth
To investigate the effects of FFAs on cancer cell
proliferation, MDA-MB-231 cells were incubated in 250 µM
BSA-bounded PA/OA for 24 h. MTT and TUNEL assays were performed to
measure cell proliferation and apoptosis. As demonstrated in
Figs. 1 and 2, OA enhanced MDA-MB-231 cell proliferation
while PA enhanced apoptosis. The effects of FFAs on MDA-MB-231 cell
migration and invasion were then investigated using wound healing
and Transwell assays. Mitomycin C was administered to inhibit cell
proliferation, and it was determined that the relative wound area
and the number of invading cells was significantly increased in
cells that had been treated with OA for 24 h. The invading cells
were also significantly increased in cells treated with PA for 24
h. However, no evident migration was observed in cells treated with
PA for 24 or 36 h.
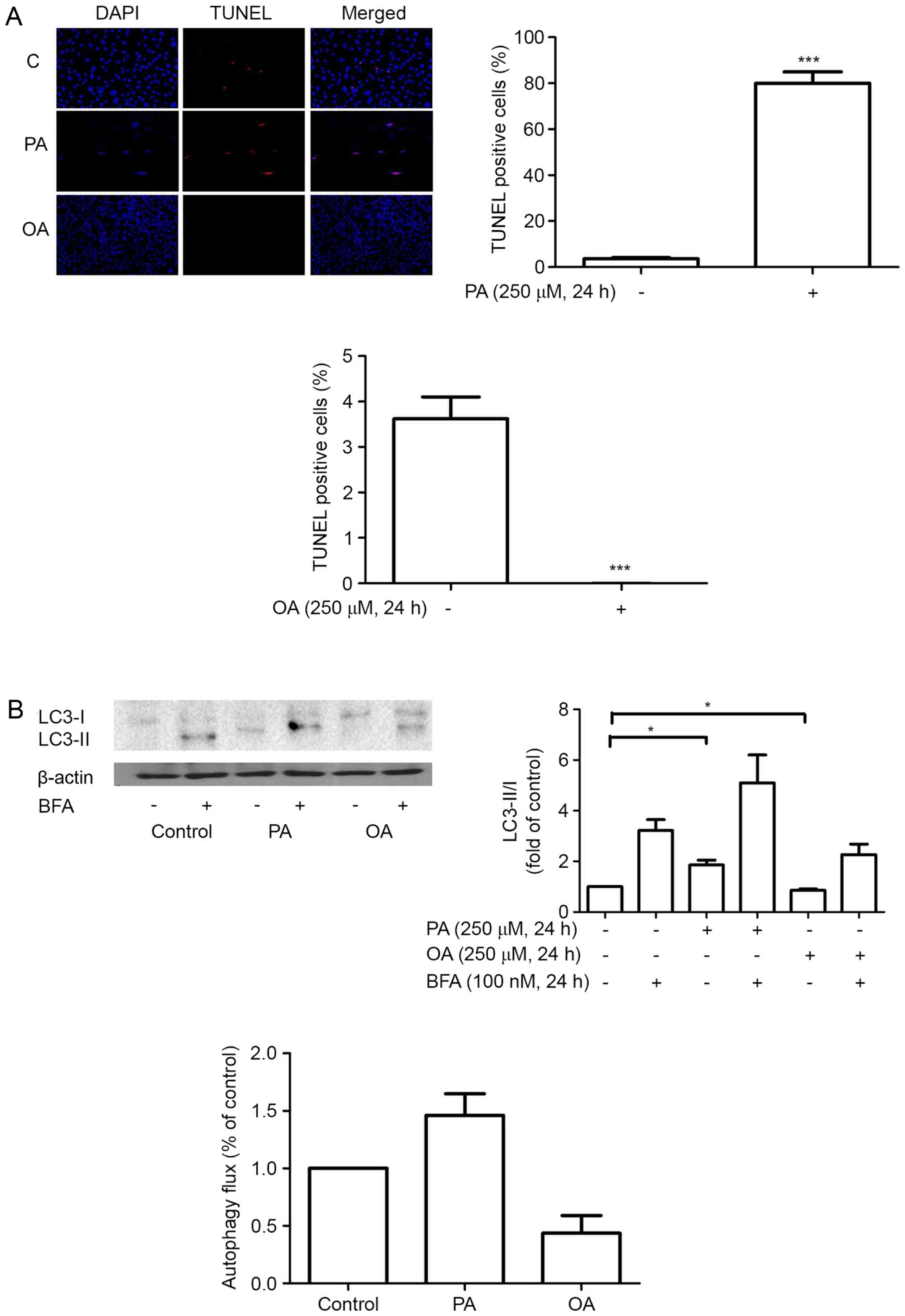
Effects of FFAs on autophagy
As a specific marker for autophagy, LC3 is widely
used to monitor autophagy. The present study detected autophagy
through western blot analysis for LC3. When autophagy is induced,
the cytosolic form of LC3, LC3-I, is processed to the lipidated and
autophagosome-associated form, LC3-II (11,13). In
the present study, treatment with PA led to an increased LC3II/I
ratio in MDA-MB-231 cells, while treatment with OA led to a
decrease. To conclusively establish the autophagy flux, LC3-II/I
levels were determined using BFA, a type of inhibitor that inhibits
the autolysosomal degradation step. The present result showed a
rise of autophagy flux subsequent to treatment with PA and a
concurrent decrease in OA (Fig. 2B).
Therefore, the present study hypothesized that PA induced autophagy
while OA inhibited autophagy in MDA-MB-231 cells.
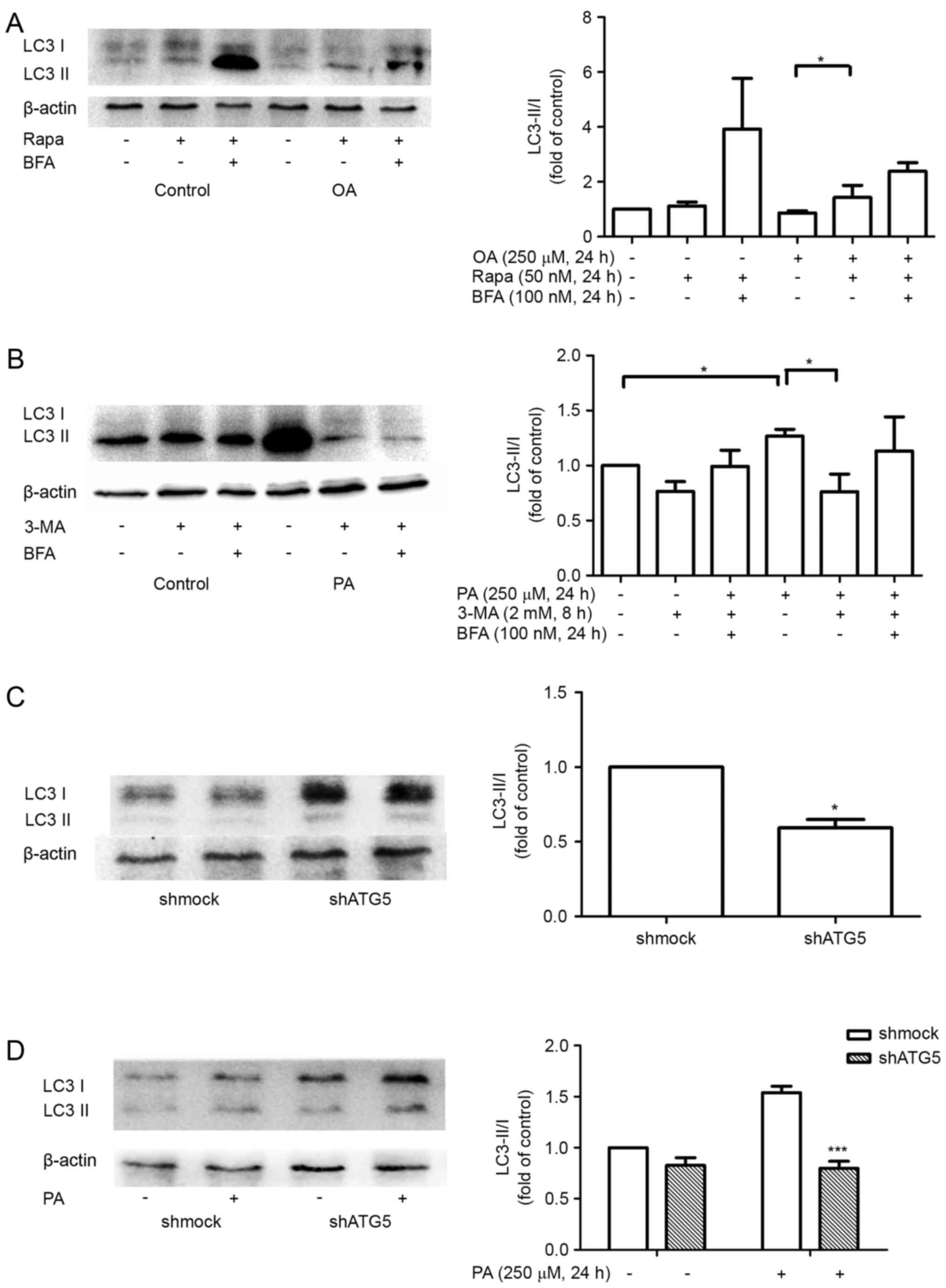
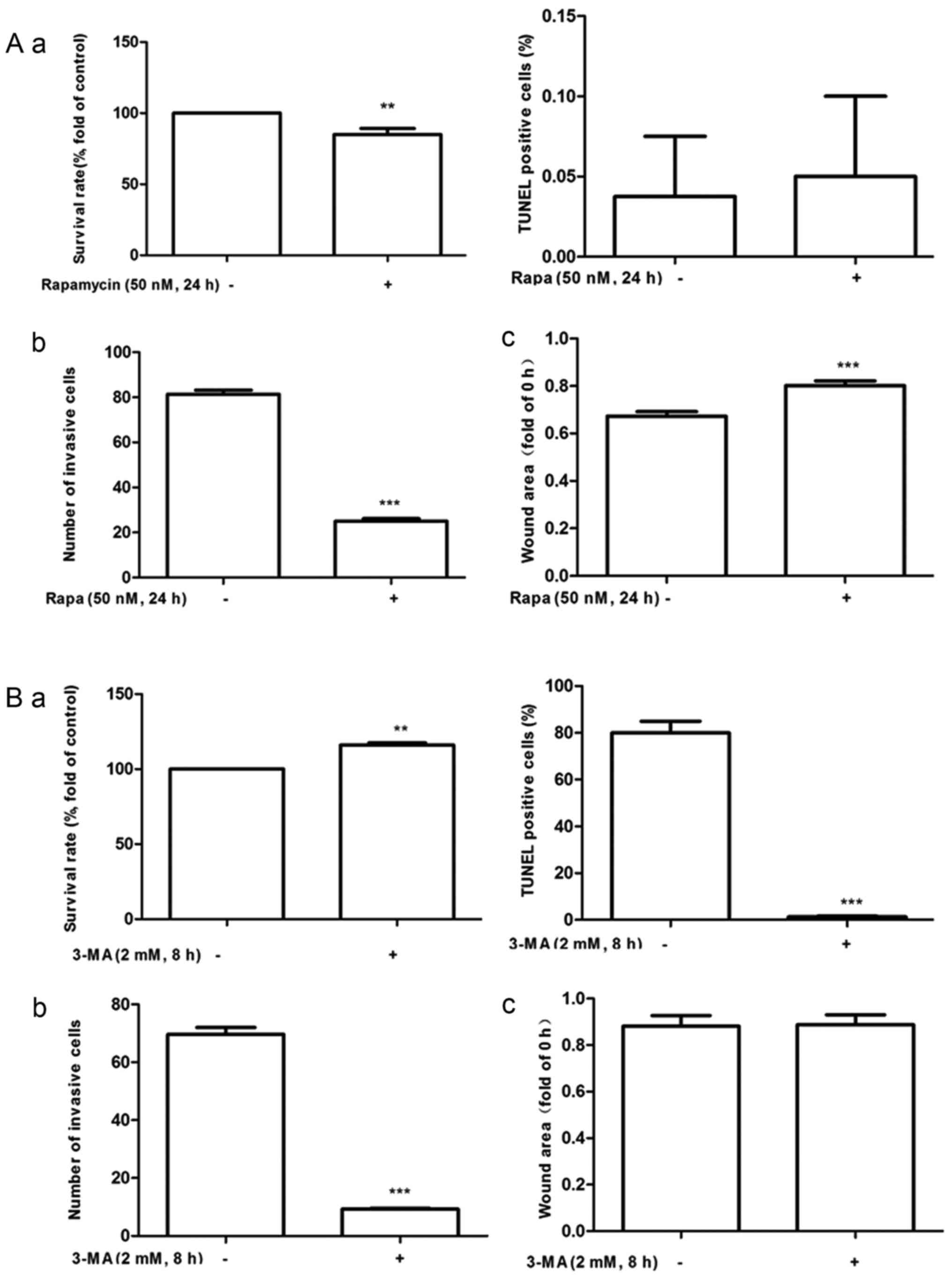
Autophagy mediated the effect of FFAs
on proliferation, migration and invasion in MDA-MB-231 cells
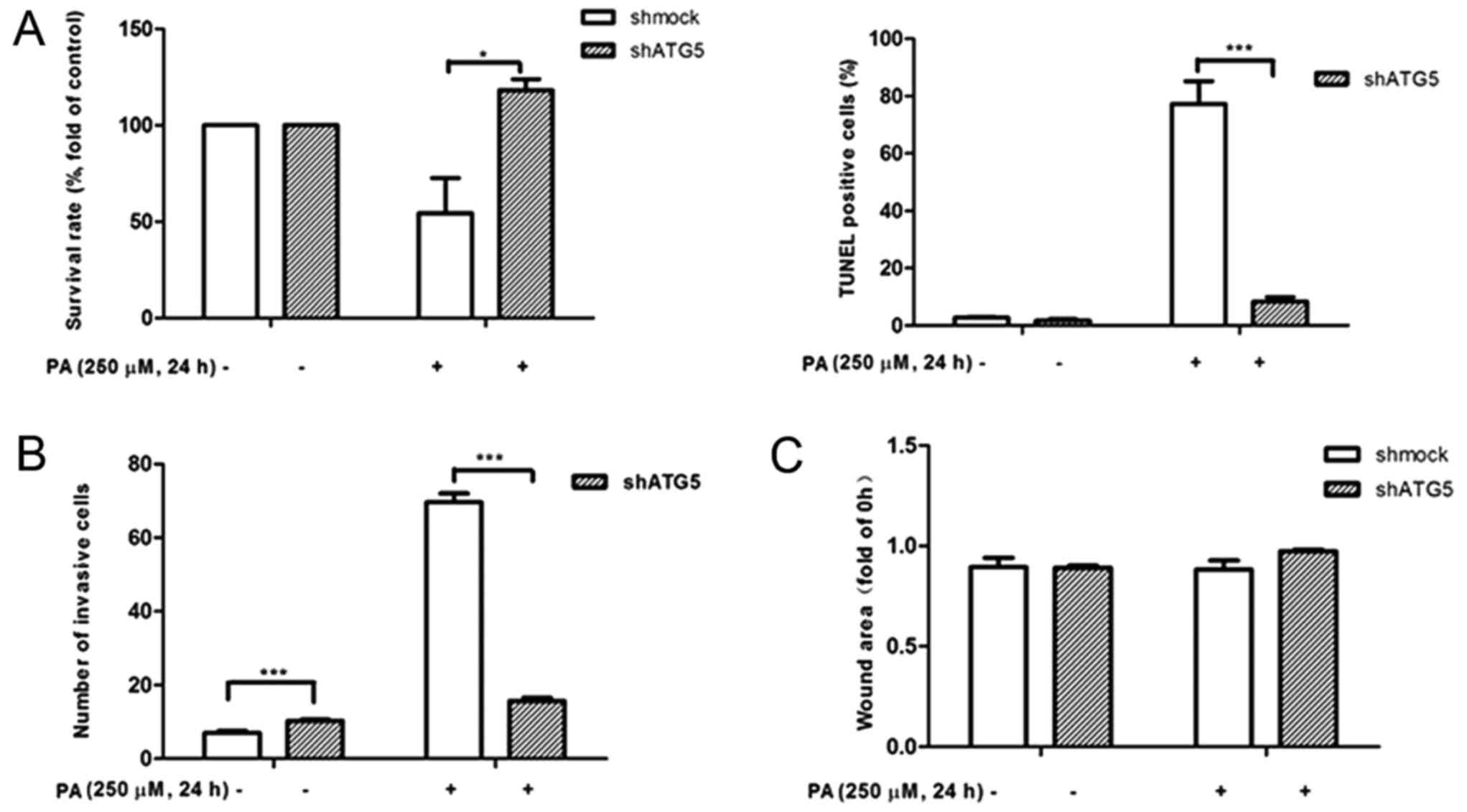
To confirm the functional consequences of autophagy
on MDA-MB-231 cell growth, migration and invasion, MDA-MB-231 cells
were incubated with autophagy inhibitor or inducer as well as PA or
OA for 24 h. It was confirmed that PA induced autophagy could be
mitigated by 3-MA pretreatment (Fig.
3B) while OA-induced autophagy inhibition could be promoted by
treatment with rapamycin (Fig. 3A).
Cell growth, migration, and invasion were then assessed by MTT,
TUNEL, wound healing, and Transwell assays, respectively. The
results demonstrated that the autophagy inhibitor 3-MA
significantly increased PA-induced cell proliferation (Fig. 4A), reduced the number of invading
cells (Fig. 4B) and suppressed cell
apoptosis (Fig. 5B). At the same
time, autophagy inducer rapamycin significantly reduced OA induced
cell proliferation (Fig. 4A), reduced
the number of invading cells (Fig.
4B) and suppressed wound closure (Fig. 5A).
shRNA against ATG5, which is known to initiate the
formation of the autophagosome, was transfected into MDA-MB-231
cells. Western blot analysis confirmed that inhibition of ATG5
expression could attenuate PA-induced LC3-II accumulation in
MDA-MB-231 cells (Fig. 3C and D). As
depicted in Figs. 4A and B, and
5B, consistent with the exposure to
3-MA, silencing of ATG5 by treatment with PA caused a increase in
cell proliferation, and decrease in cell apoptosis and invasion
after 24 h.
Discussion
Previous studies have reported accumulating evidence
of metabolic reorganization during cancer development. Tumor cells
gain a survival or growth advantage by adapting their metabolism to
respond to environmental stress, the best-known aspect of which is
the Warburg effect (16,17). Understanding the metabolic differences
between normal and tumor cells could provide the opportunity to
design selective personalized therapy against breast cancer and
other cancers (18). However, the
metabolism of cancer cells is complex and involves various rewiring
of the metabolic pathways that occurs during malignant
transformation. The data presented in the present study
demonstrated that PA promotes MDA-MB-231 cell apoptosis and
invasion while OA promotes proliferation, migration and invasion.
Although FFA levels are generally elevated in breast cancer
patients (19,20), the role of FFA in health and disease
in humans has been minimally investigated and understood.
It has been shown that autophagy may be induced by
multiple stimuli, including nutrient deprivation, serum starvation,
metabolic stress, radiation and anticancer drugs, in multiple
cancer cells (21,22). This has provided insight into the
adaptation process for cells, which either allows tolerance of
adverse conditions or triggers cell suicide mechanisms (23). Basal autophagy is essential to
maintain cellular homeostasis and genomic integrity by degrading
the aged or malfunctioning organelles and damaged or misfolded
proteins (11,24). It has been shown that autophagy is
frequently upregulated in tumors in response to therapy and may
protect the tumors during cancer development, but promote cell
survival during cancer progression (22). However, the role of autophagy in
cancer remains controversial, as it may suppress tumors during
cancer development and promote cell survival during cancer
progression (25).
In the present study, it was found that LC3-II
accumulated in PA-treated MDA-MB-231 cells; this effect was
enhanced in the presence of BFA and was blocked by 3-MA. Inhibition
of ATG5 expression attenuated PA-induced LC3-II accumulation. The
present results also determined that pretreatment with the
autophagy inhibitor 3-MA significantly mitigated cell apoptosis and
invasion, suggesting that high PA-induced MDA-MB-231 cell apoptosis
and invasion are mediated by promoting autophagy. By contrast,
LC3-II decreased in OA-treated MDA-MB-231 cells and was restored
using rapamycin, which significantly reduced cell growth, migration
and invasion, indicating that high OA-induced MDA-MB-231 cell
proliferation, migration and invasion are mediated by inhibiting
autophagy.
In summary, to the best of our knowledge, the
present findings revealed that the difference between PA and
OA-induced growth, migration and invasion of MDA-MB-231 cells is
mediated by autophagy for the first time. This indicates the
potential therapeutic importance of lipid regulation on human
breast cancer.
Acknowledgements
The authors would like to thank Professor Lei Wei
(Department of Pathology and Pathophysiology, Wuhan University
School of Basal Medical School) for the gift of the MDA-MB-231 cell
line.
References
|
1
|
American Cancer Society: Cancer Facts and
Figures 2017. American Cancer Society; Atlanta, GA: 2017
|
|
2
|
Zheng R, Zeng H, Zhang S, Chen T and Chen
W: National estimates of cancer prevalence in China. Cancer Lett.
370:33–38. 2011. View Article : Google Scholar
|
|
3
|
Wolf I, Sadetzki S, Catane R, Karasik A
and Kaufman B: Diabetes mellitus and breast cancer. Lancet Oncol.
6:103–111. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nomura DK, Long JZ, Niessen S, Hoover HS,
Ng SW and Cravatt BF: Monoacylglycerol lipase regulates a fatty
acid network that promotes cancer pathogenesis. Cell. 140:49–61.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Przybytkowski E, Joly E, Nolan CJ, Hardy
S, Francoeur AM, Langelier Y and Prentki M: Upregulation of
cellular triacylglycerol-free fatty acid cycling by oleate is
associated with long-term serum-free survival of human breast
cancer cells. Biochem Cell Biol. 85:301–310. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cantrill RC and Huang YS: Fatty acids and
cancer. Nutrition. 14:235–237. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Patterson RE, Flatt SW, Newman VA,
Natarajan L, Rock CL, Thomson CA, Caan BJ, Parker BA and Pierce JP:
Marine fatty acid intake is associated with breast cancer
prognosis. J Nutr. 141:201–206. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ford JH: Saturated fatty acid metabolism
is key link between cell division, cancer, and senescence in
cellular and whole organism aging. Age (Dordr). 32:231–237. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Patterson RE, Flatt SW, Newman VA,
Natarajan L, Rock CL, Thomson CA, Caan BJ, Parker BA and Pierce JP:
Marine fatty acid intake is associated with breast cancer
prognosis. J Nutr. 141:201–206. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Abel S, Riedel S and Gelderblom WC:
Dietary PUFA and cancer. Proc Nutr Soc. 73:361–367. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rabinowitz JD and White E: Autophagy and
metabolism. Science. 330:1344–1348. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mizushima N, Levine B, Cuervo AM and
Klionsky DJ: Autophagy fights disease through cellular
self-digestion. Nature. 451:1069–1075. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shi Z, Li CY, Zhao S, Yu Y, An N, Liu YX,
Wu CF, Yue BS and Bao JK: A systems biology analysis of autophagy
in cancer therapy. Cancer Lett. 337:149–160. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zarzynska JM: The importance of autophagy
regulation in breast cancer development and treatment. Biomed Res
Int. 2014:7103452014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mizushima N, Levine B, Cuervo AM and
Klionsky DJ: Autophagy fights disease through cellular
self-digestion. Nature. 451:1069–1075. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li S, Zhou T, Li C, Dai Z, Che D, Yao Y,
Li L, Ma J, Yang X and Gao G: High metastaticgastric and breast
cancer cells consume oleic acid in an AMPK dependent manner. PLoS
One. 9:e973302014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kim S, Lee Y and Koo JS: Differential
expression of lipid metabolism-related proteins in different breast
cancer subtypes. PLoS One. 10:e01194732015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
DeBerardinis RJ and Thompson CB: Cellular
metabolism and disease: What do metabolic outliers teach us? Cell.
148:1132–1144. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lv ZH, Ma P, Luo W, Xiong H, Han L, Li SW,
Zhou X and Tu JC: Association between serum free fatty acid levels
and possible related factors in patients with type 2 diabetes
mellitus and acute myocardial infarction. BMC Cardiovasc Disord.
14:1592014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lv W and Yang T: Identification of
possible biomarkers for breast cancer from free fatty acid profiles
determined by GC-MS and multivariate statistical analysis. Clin
Biochem. 45:127–133. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen YR, Tsou B, Hu S, Ma H, Liu X, Yen Y
and Ann DK: Autophagy induction causes a synthetic lethal
sensitization to ribonucleotide reductase inhibition in breast
cancer cells. Oncotarget. 7:1984–1999. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Huang YH, Yang PM, Chuah QY, Lee YJ, Hsieh
YF, Peng CW and Chiu SJ: Autophagy promotes radiation-induced
senescence but inhibits bystander effects in human breast cancer
cells. Autophagy. 10:1212–1228. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wang L, Yao L, Zheng YZ, Xu Q, Liu XP, Hu
X, Wang P and Shao ZM: Expression of autophagy-related proteins
ATG5 and FIP200 predicts favorable disease-free survival in
patients with breast cancer. Biochem Biophys Res Commun.
458:816–822. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Eng CH and Abraham RT: The autophagy
conundrum in cancer: Influence of tumorigenic metabolic
reprogramming. Oncogene. 30:4687–4696. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Boyer-Guittaut M, Poillet L, Liang Q,
Bôle-Richard E, Ouyang X, Benavides GA, Chakrama FZ, Fraichard A,
Darley-Usmar VM, Despouy G, et al: The role of GABARAPL1/GEC1 in
autophagic flux and mitochondrial quality control in MDA-MB-436
breast cancer cells. Autophagy. 10:986–1003. 2014. View Article : Google Scholar : PubMed/NCBI
|