Introduction
Hepatocellular carcinoma (HCC) is the seventh most
commonly diagnosed cancer and the sixth leading cause of
cancer-associated mortality worldwide (1). It is generally more common in
non-Caucasian populations (1).
Chronic infection with hepatitis B virus (HBV) or hepatitis C virus
(HCV), alcoholic liver disease and non-alcoholic fatty liver
disease have been associated with the tumorigenesis of HCC
(2). HCC is an
inflammation-associated cancer that generally develops in the
background of chronic hepatitis, regardless of the triggering
etiology (3).
Inflammation-induced HCC is dependent on AKT
activation (4,5). AKT, also called protein kinase B, is a
serine/threonine kinase. Phosphorylated AKT (p-AKT), the active
form of AKT, influences a range of cellular functions, including
cell growth, proliferation, differentiation, motility, survival and
intracellular trafficking (6).
Previous studies have indicated that the increased
immunohistochemical expression of p-AKT is correlated with a poorer
prognosis in various types of cancer, including endometrial
carcinoma (7), renal cell carcinoma
(8), colorectal cancer (9), breast cancer (10), melanoma (11) and nasopharyngeal carcinoma (12). In HCC, the upregulation of AKT1, 2 or
3 has been demonstrated to be significantly associated with tumor
progression and a poor survival rate (13).
p-AKT may be a target for therapeutic regimens
aiming to reverse acquired resistance to sorafenib during the
treatment of patients with HCC (14–16).
Although p-AKT expression in tumor tissue (TU) was previously
explored (13), the role for p-AKT in
the adjacent non-neoplastic liver tissue (AN) remains unidentified.
The aim of the present study was to apply immunohistochemical
staining for p-AKT to clinical samples of TU and AN tissues, to
investigate the clinical significance in patients with HCC.
Patients and methods
Patients
Formalin-fixed and paraffin-embedded HCC TU and
paired AN samples were obtained from 202 patients that underwent
surgical tumor resection at Changhua Christian Hospital, (Changhua,
Taiwan) between July 2011 and November 2013. In the retrospective
the study, clinical data was obtained through chart review, thus,
patients lost in the follow-up period were excluded. All patients
received chemotherapy or radiotherapy prior to surgery. A tissue
microarray (TMA) was constructed from the TU and AN tissues. A TMA
block was made up of 96 tissue cores measuring 2 mm in diameter.
Approximately 250 consecutive sections (4-µm thick) could be cut
from a TMA block and used for immunohistochemical staining to
determine specific protein expression patterns for antibodies. All
patients were staged as per the American Joint Committee on Cancer
staging guidelines (17). Each
patient's clinical characteristics and outcomes were collected
until the event of patient mortality, censorship or loss of
follow-up. The Ethics Committee of the Institutional Review Board
of Changhua Christian Hospital approved all procedures of the
present study. Informed consents were obtained from all sample
donors in accordance with the Declaration of Helsinki.
The patients, including 56 females and 146 males,
were aged 29–81 years (mean ± standard deviation, 63.1±11.7).
Survival time was defined as period from the date of primary
surgery to the date of patient mortality or disease recurrence. Due
to the retrospective nature of the study, clinical data was
obtained through chart review, and some information was incomplete;
among the 202 HCC patients, HCV status was unknown for 8 and HBV
serum antigen status was unknown for 7. The median follow-up time
subsequent to surgery was 907 days; the median OS time of all
patients was 937 days. A total of 44 patients succumbed to HCC
during the study. On the basis of follow-up data, 8 patients
relapsed, with local recurrence.
Immunohistochemistry (IHC) and
scoring
IHC was used to detect p-AKT protein expression. The
IHC procedures were conducted as previously described (18), using an anti-p-AKT antibody
(sc-16646-R) purchased from Santa Cruz Biotechnology, Inc. (Dallas,
TX, USA). Negative controls were obtained by performing all IHC
steps without the primary antibody. The IHC staining intensities
were evaluated by a board-certified pathologist. Immunostaining
scores were defined as the cell staining intensity (nil, 0; weak,
1; moderate, 2; strong, 3) multiplied by the percentage of labeled
cells (0–100%), producing scores between 0–300. A score greater
than the mean was defined as ‘high’ immunostaining, whereas a score
less than or equal to the mean was categorised as ‘low’,
respectively for AN and TU tissues.
Statistical analysis
All statistics were performed with SPSS software
(version 18.0; SPSS, Inc., Chicago, IL, USA). χ2
analyses and paired t-tests were used to analyze the associations
between clinical characteristics and p-AKT expression. Survival
curves were plotted using the Kaplan-Meier method and variables
associated with survival were analyzed with Cox's proportional
hazards regression model. Statistical differences in survival data
were analyzed using the log-rank test. P<0.05 was considered to
indicate a statistically significant difference.
Results
p-AKT expression is higher in TU than
in AN
A total of 202 HCC patients were enrolled in the
present study. p-AKT expression was detected using IHC in 202 sets
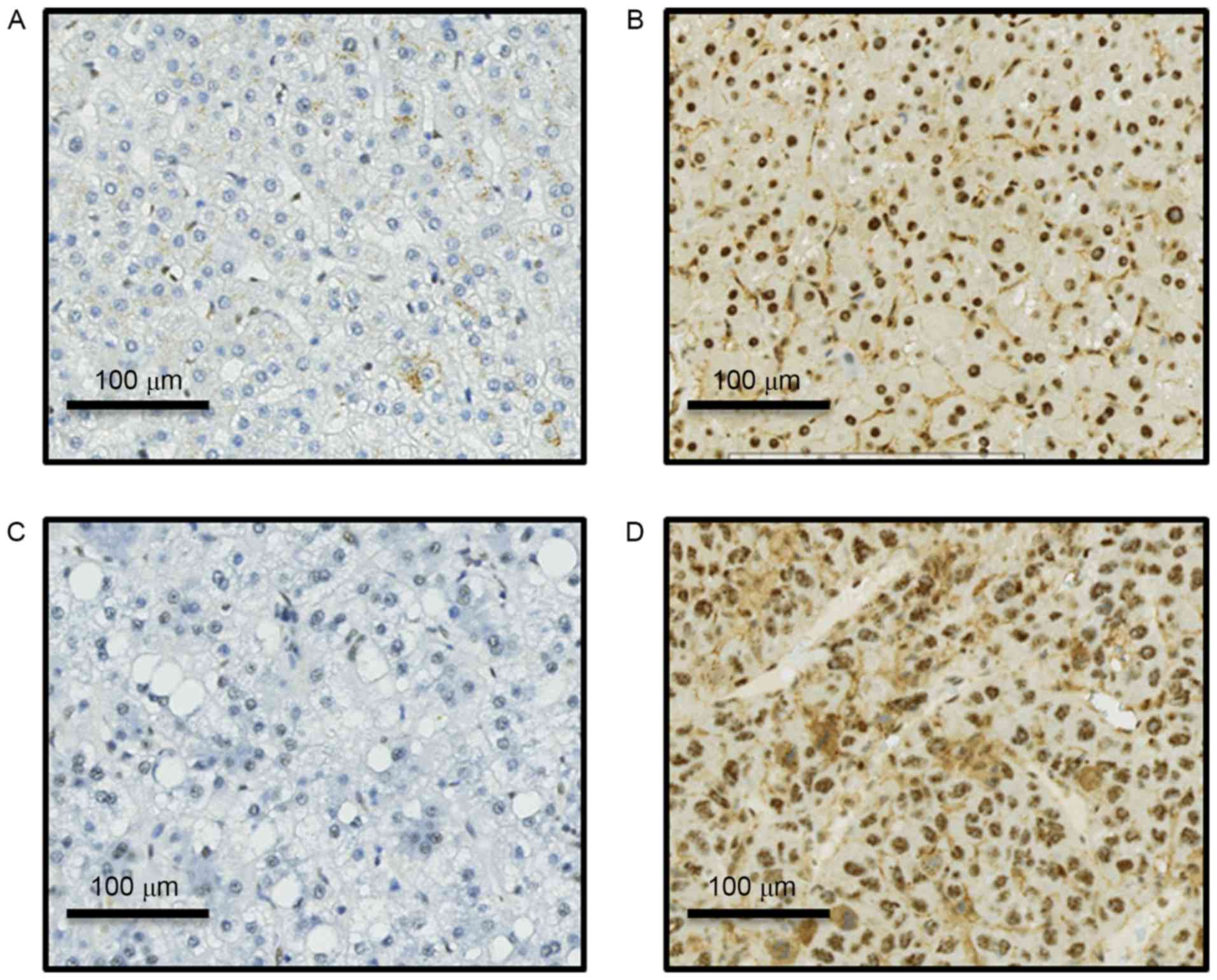
of paired TU and AN tissues (Fig. 1).
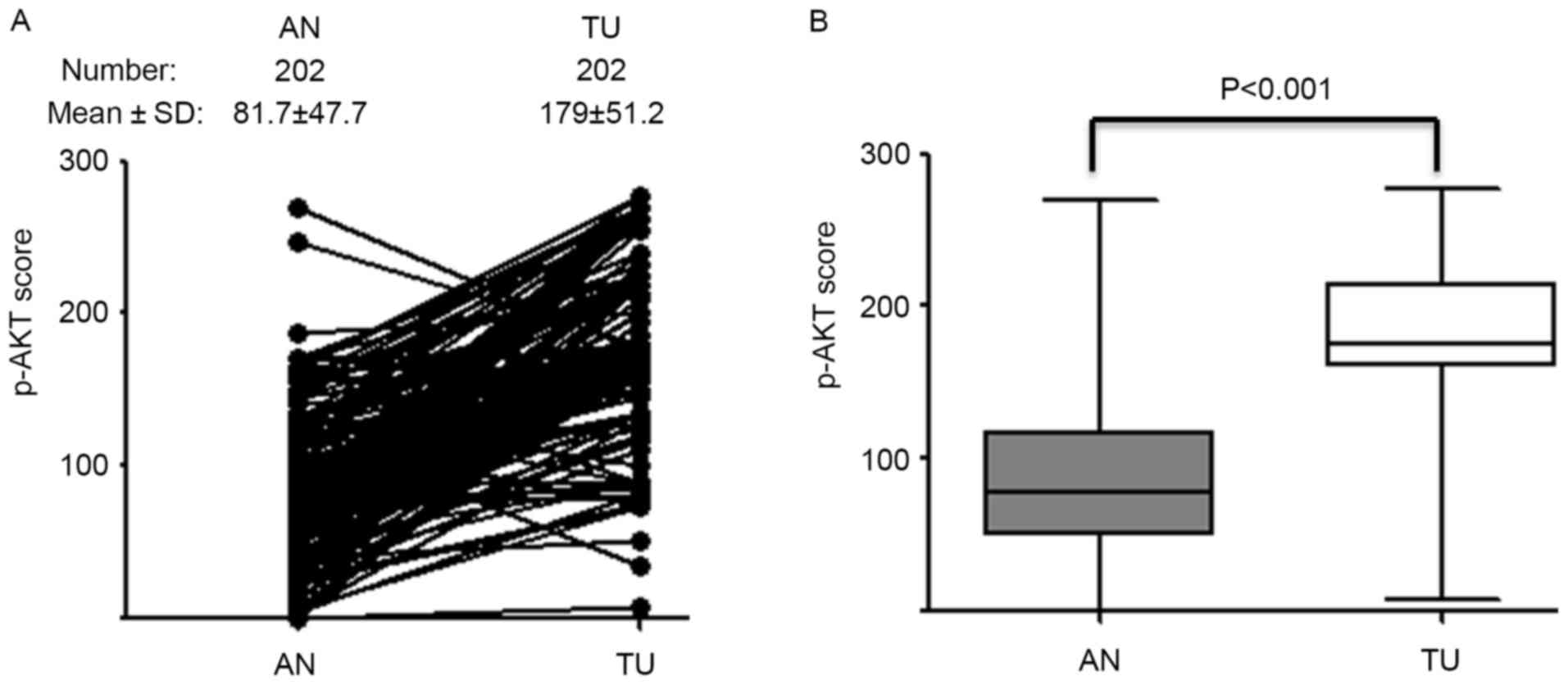
p-AKT expression level in TU tissue (p-AKT TU) was significantly
higher than in the paired AN tissue (p-AKT AN; P<0.001; Fig. 2). The mean IHC score was 179 for TU
and 81 for AN; these scores were used as cut-off values for high
and low expression in the respective groups.
p-AKT (AN) is positively associated
with hepatitis c virus infection
Statistical analysis was performed to verify whether
p-AKT (AN) and p-AKT (TU) were linked with clinicopathological
parameters including age, sex, differentiation grade, tumor stage,
HBV surface antigen and HCV status. Only HCV status was
significantly associated with p-AKT (AN); Patients with HCC that
exhibited HCV infection had a higher expression of p-AKT (AN) than
those without HCV infection (P=0.026; Table I). The results of the present study
suggest that the effect of HCV infection on p-AKT (AN) expression
was more evident than on p-AKT (TU).
 | Table I.Association of clinical parameters
with p-AKT expression of AN and TU tissue in hepatocellular
carcinoma patients. |
Table I.
Association of clinical parameters
with p-AKT expression of AN and TU tissue in hepatocellular
carcinoma patients.
|
|
| p-AKT (AN), n
(%) |
| p-AKT (TU), n
(%) |
|
|---|
|
|
|
|
|
|
|
|---|
| Variables | Total, n (%) | Low | High | P-value | Low | High | P-value |
|---|
| Total | 202 | 119 | 83 |
| 115 | 87 |
|
| Age, years |
|
|
| 0.424 |
|
| 0.764 |
|
<65 | 109 (54) | 67 (62) | 42 (38) |
| 61 (56) | 48 (44) |
|
| ≥65 | 93 (46) | 52 (56) | 41 (44) |
| 54 (58) | 39 (42) |
|
| Sex |
|
|
| 0.111 |
|
| 0.360 |
|
Female | 56 (28) | 28 (50) | 28 (50) |
| 29 (52) | 27 (48) |
|
| Male | 146 (72) | 91 (62) | 55 (38) |
| 86 (59) | 60 (41) |
|
| Differentiation |
|
|
| 0.590 |
|
| 0.164 |
| Well | 11 (5) | 8 (73) | 3 (27) |
| 9 (81) | 2 (19) |
|
|
Moderate | 101 (50) | 62 (61) | 39 (39) |
| 60 (59) | 41 (41) |
|
| Poor | 84 (42) | 46 (55) | 38 (45) |
| 44 (52) | 40 (48) |
|
|
Undifferentiated | 6 (3) | 3 (50) | 3 (50) |
| 2 (33) | 4 (67) |
|
| Stage |
|
|
| 0.938 |
|
| 0.369 |
| I,
II | 166 (82) | 98 (59) | 68 (41) |
| 97 (58) | 69 (42) |
|
| III,
IV | 36 (18) | 21 (58) | 15 (42) |
| 18 (50) | 18 (50) |
|
| Hepatitis B surface
antigen status |
|
|
| 0.386 |
|
| 0.818 |
|
Negative | 89 (44) | 55 (62) | 34 (38) |
| 51 (57) | 38 (43) |
|
|
Positive | 106 (52) | 59 (56) | 47 (44) |
| 59 (56) | 47 (44) |
|
|
Unknown | 7 (4) | 5 (71) | 2 (29) |
| 5 (71) | 2 (29) |
|
| Hepatitis C
virus |
|
|
| 0.026 |
|
| 0.520 |
|
Negative | 125 (62) | 82 (66) | 43 (34) |
| 73 (58) | 52 (42) |
|
|
Positive | 69 (34) | 34 (49) | 35 (51) |
| 37 (54) | 32 (44) |
|
|
Unknown | 8 (4) | 3 (38) | 5 (62) |
| 5 (62) | 3 (38) |
|
p-AKT (AN) is associated with OS and
RFS time in HCC patients
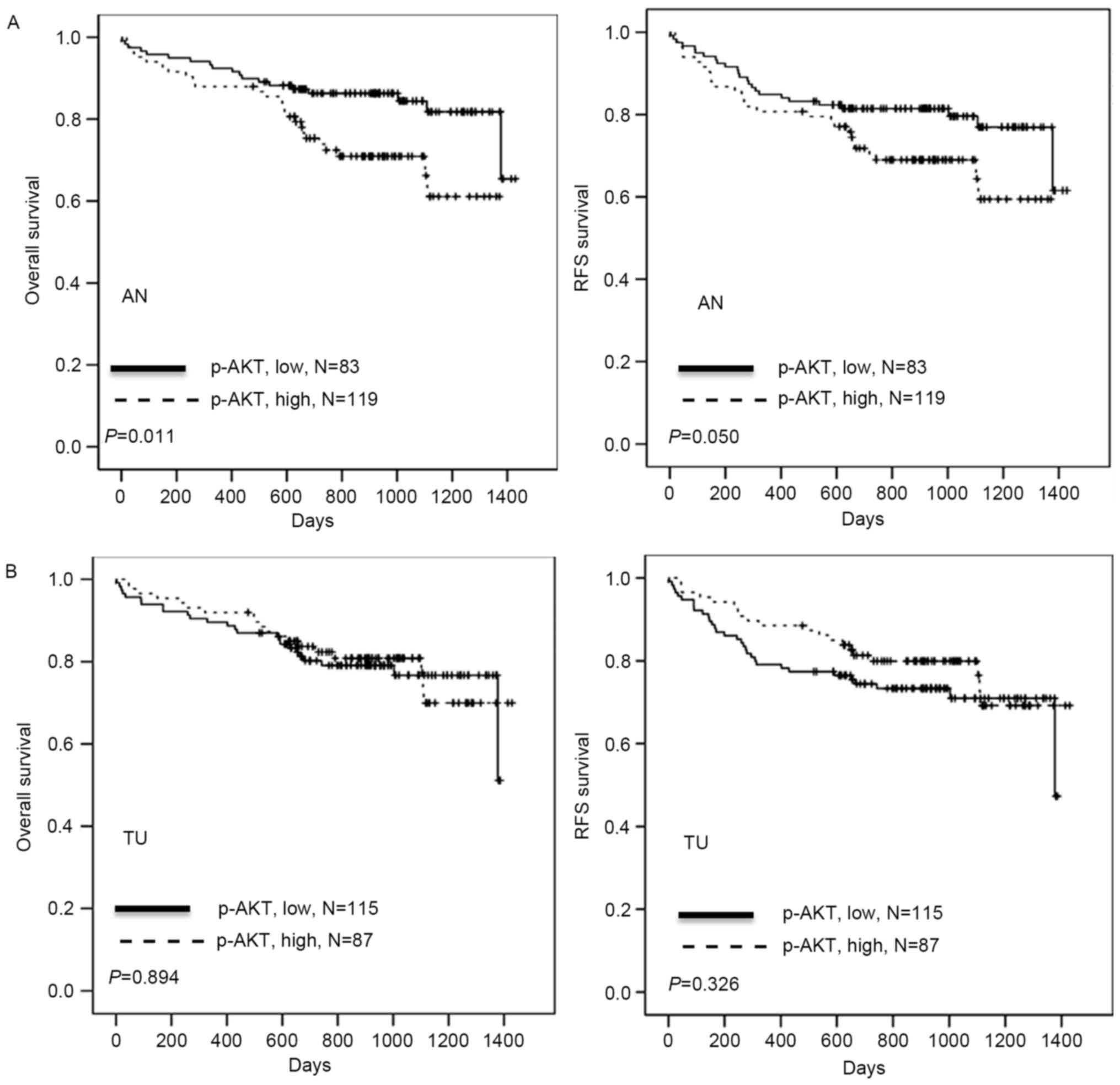
The association of p-AKT (AN) and
clinicopathological parameters, including age, sex,
differentiation, stage, HBV surface antigen, HCV, p-AKT (TU) and
p-AKT (AN), with patient survival time was investigated by
univariate analysis The full results are included in Table II. OS time was significantly
associated with stage (P<0.001) and p-AKT (AN) (P=0.011); RFS
was significantly associated with stage (P<0.001) and p-AKT (AN)
(P=0.050). It was then examined whether p-AKT (AN) expression was
associated with clinical outcomes in HCC patients. Kaplan-Meier
analysis demonstrated that patients with high p-AKT (AN) had
shorter OS and RFS periods when compared with patients with low
p-AKT (AN) (P=0.011 and P=0.050, respectively; Table II; Fig.
3), whereas p-AKT (TU) was not significantly associated with
survival time. Cox regression analysis indicated a prognostic
significance for p-AKT (AN) in OS and RFS in the study population
(P=0.011 and P=0.046, respectively; Table III). The hazard ratios for high
p-AKT (AN) were 2.192 for OS and 1.751 for RFS, respectively,
relative to low p-AKT (AN) (Table
III). Additionally, the hazard ratios for stage III/IV were
3.064 for OS and 3.536 for RFS, respectively, relative to stage
I/II (both P<0.001; Table III).
The results suggest that p-AKT (AN) expression may promote tumor
malignancy, resulting in poor outcomes for patients with HCC.
 | Table II.Univariate analysis of influences of
clinical characteristics, and p-AKT (AN) or (TU), on OS and RFS in
hepatocellular carcinoma patients. |
Table II.
Univariate analysis of influences of
clinical characteristics, and p-AKT (AN) or (TU), on OS and RFS in
hepatocellular carcinoma patients.
|
|
| OS |
| RFS |
|
|---|
|
|
|
|
|
|
|
|---|
|
Characteristics | Total, n | Median time
(days) | Rate (%) | Log-rank
P-value | Median time
(days) | Rate (%) | Log-rank
P-value |
|---|
| Age, years |
|
|
| 0.178 |
|
| 0.174 |
|
<65 | 109 | 923 | 81.7 |
| 912 | 78.0 |
|
|
≥65 | 93 | 874 | 74.2 |
| 874 | 69.9 |
|
| Sex |
|
|
| 0.635 |
|
| 0.445 |
|
Female | 56 | 838 | 76.8 |
| 838 | 71.4 |
|
|
Male | 146 | 910 | 78.8 |
| 905 | 75.3 |
|
|
Differentiation |
|
|
| 0.755 |
|
| 0.416 |
|
Well/Moderate | 112 | 884 | 78.6 |
| 879 | 75.9 |
|
|
Poor/Undifferentiated | 90 | 914 | 77.8 |
| 908 | 72.2 |
|
| Stage |
|
|
| <0.001 |
|
| <0.001 |
| I,
II | 165 | 923 | 82.4 |
| 921 | 80.0 |
|
| III,
IV | 36 | 685 | 58.3 |
| 630 | 47.2 |
|
| Hepatitis B surface
antigen |
|
|
| 0.917 |
|
| 0.365 |
|
Negative | 89 | 884 | 77.5 |
| 874 | 70.8 |
|
|
Positive | 106 | 916 | 78.3 |
| 946 | 76.4 |
|
| Hepatitis C
virus |
|
|
| 0.256 |
|
| 0.489 |
|
Negative | 125 | 907 | 76.0 |
| 904 | 72.8 |
|
|
Positive | 69 | 884 | 82.6 |
| 874 | 76.8 |
|
| p-AKT (TU) |
|
|
| 0.894 |
|
| 0.326 |
|
Low | 115 | 874 | 78.3 |
| 868 | 77.2 |
|
|
High | 87 | 912 | 78.2 |
| 912 | 77.0 |
|
| p-AKT (AN) |
|
|
| 0.011 |
|
| 0.050 |
|
Low | 119 | 923 | 84.0 |
| 917 | 79.0 |
|
|
High | 83 | 874 | 69.9 |
| 874 | 67.5 |
|
 | Table III.Cox regression analysis for the
influence of stage and p-AKT (AN) on OS and RFS time in
hepatocellular carcinoma patients. |
Table III.
Cox regression analysis for the
influence of stage and p-AKT (AN) on OS and RFS time in
hepatocellular carcinoma patients.
|
| OS | RFS |
|---|
|
|
|
|
|---|
| Variables | HR | 95% CI |
Unfavorable/favorable | P-value | HR | 95% CI |
Unfavorable/favorable | P-value |
|---|
| p-AKT (AN) | 2.192 | 1.193–4.026 | High/low | 0.011 | 1.751 | 1.009–3.039 | High/low | 0.046 |
| Stage | 3.064 | 1.637–5.733 | III, IV/I, II | <0.001 | 3.536 | 2.003–6.241 | III, IV/I, II | <0.001 |
Discussion
Based on the data of the present study,
post-resection patients with HCV-associated HCC exhibit higher
p-AKT (AN) expression than those without HCV infection. p-AKT (AN)
may be a predictor for prognosis and recurrence in HCC. These
results support a previous study in which patients positive for HCV
undergoing the resection of HCC experienced reduced OS and RFS
times relative to patients negative for HCV (19). HCV is a single-stranded,
positive-sense RNA virus of the Flaviviridae family; HCV-induced
HCC is expected to increase in the next two decades (20,21).
Examinations of the association between HCV and the
phosphatidylinositol-4,5-bisphosphate 3-kinase (PI3K)/AKT pathway
has revealed that the HCV-associated NS5A protein binds to PI3K,
consequently activating AKT and potentially contributing to the
development of HCC (22,23). One study identified that HCV rapidly
and transiently activated AKT in the early stage of infection via
the interaction between the HCV E2 envelope protein and its
co-receptors CD81 and claudin-1, with the effect of enhancing viral
entry into the cell (24).
Another study reported that cancer stem cells or
tumor-initiating cells that retain a stem cell-like phenotype,
along with the HCV-induced reprogramming of liver cells, may
contribute to hepatocarcinogenesis in an animal model (25). AKT serves an additional role in the
maintenance of stem-like characteristics, the mesenchymal phenotype
and the self-renewal of these cells via the AKT/Forkhead box
O/Bcl2-like 11 pathway (26).
Therefore, the observation that higher p-AKT (AN) may be an
independent prognostic factor for HCC may be due to HCV
infection.
In summary, the present study revealed that patients
with HCC with high levels of p-AKT (AN) expression exhibited a
relatively poor survival rate, and p-AKT (TU) was significantly
higher than p-AKT (AN). Curing HCV and inhibiting p-AKT may be
necessary to improve the outcome for patients with HCC.
Acknowledgements
The present study was supported by grant nos.
102-2321-B-750-001-MY3 and 103-2314-B-442-002-MY3 from the Ministry
of Science and Technology, Taiwan, and nos. RB15001 and RB16001
from Show Chwan Memorial Hospital, Taiwan.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
El-Serag HB: Hepatocellular carcinoma. N
Engl J Med. 365:1118–1127. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Berasain C, Castillo J, Perugorria MJ,
Latasa MU, Prieto J and Avila MA: Inflammation and liver cancer:
New molecular links. Ann N Y Acad Sci. 1155:206–221. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Leng J, Han C, Demetris AJ, Michalopoulos
GK and Wu T: Cyclooxygenase-2 promotes hepatocellular carcinoma
cell growth through Akt activation: Evidence for Akt inhibition in
celecoxib-induced apoptosis. Hepatology. 38:756–768. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yang Y, Guo Y, Tan S, Ke B, Tao J, Liu H,
Jiang J, Chen J, Chen G and Wu B: β-Arrestin1 enhances
hepatocellular carcinogenesis through inflammation-mediated Akt
signalling. Nat Commun. 6:73692015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vivanco I and Sawyers CL: The
phosphatidylinositol 3-Kinase AKT pathway in human cancer. Nat Rev
Cancer. 2:489–501. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Uegaki K, Kanamori Y, Kigawa J, Kawaguchi
W, Kaneko R, Naniwa J, Takahashi M, Shimada M, Oishi T, Itamochi H
and Terakawa N: PTEN-positive and phosphorylated-Akt-negative
expression is a predictor of survival for patients with advanced
endometrial carcinoma. Oncol Rep. 14:389–392. 2005.PubMed/NCBI
|
|
8
|
Hager M, Haufe H, Kemmerling R, Hitzl W,
Mikuz G, Moser PL and Kolbitsch C: Increased activated Akt
expression in renal cell carcinomas and prognosis. J Cell Mol Med.
13:2181–2188. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Malinowsky K, Nitsche U, Janssen KP, Bader
FG, Späth C, Drecoll E, Keller G, Höfler H, Slotta-Huspenina J and
Becker KF: Activation of the PI3 K/AKT pathway correlates with
prognosis in stage II colon cancer. Br J Cancer. 110:2081–2089.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tokunaga E, Kimura Y, Oki E, Ueda N,
Futatsugi M, Mashino K, Yamamoto M, Ikebe M, Kakeji Y, Baba H and
Maehara Y: Akt is frequently activated in HER2/neu-positive breast
cancers and associated with poor prognosis among hormone-treated
patients. Int J Cancer. 118:284–289. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dai DL, Martinka M and Li G: Prognostic
significance of activated Akt expression in melanoma: A
clinicopathologic study of 292 cases. J Clin Oncol. 23:1473–1482.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang W, Wen Q, Xu L, Xie G, Li J, Luo J,
Chu S, Shi L, Huang D, Li J and Fan S: Activation of Akt/mTOR
pathway is associated with poor prognosis of nasopharyngeal
carcinoma. PLoS One. 9:e1060982014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang Y, Guo X, Yang M, Yu L, Li Z and Lin
N: Identification of AKT kinases as unfavorable prognostic factors
for hepatocellular carcinoma by a combination of expression
profile, interaction network analysis and clinical validation. Mol
Biosyst. 10:215–222. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gedaly R, Angulo P, Chen C, Creasy KT,
Spear BT, Hundley J, Daily MF, Shah M and Evers BM: The role of
PI3K/mTOR inhibition in combination with sorafenib in
hepatocellular carcinoma treatment. Anticancer Res. 32:2531–2536.
2012.PubMed/NCBI
|
|
15
|
Simioni C, Martelli AM, Cani A,
Cetin-Atalay R, McCubrey JA, Capitani S and Neri LM: The AKT
inhibitor MK-2206 is cytotoxic in hepatocarcinoma cells displaying
hyperphosphorylated AKT-1 and synergizes with conventional
chemotherapy. Oncotarget. 4:1496–1506. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhai B, Hu F, Jiang X, Xu J, Zhao D, Liu
B, Pan S, Dong X, Tan G, Wei Z, et al: Inhibition of Akt reverses
the acquired resistance to sorafenib by switching protective
autophagy to autophagic cell death in hepatocellular carcinoma. Mol
Cancer Ther. 13:1589–1598. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Edge SB and Compton CC: The American joint
committee on cancer: The 7th edition of the AJCC cancer staging
manual and the future of TNM. Ann Surg Oncol. 17:1471–1474. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yu HC, Hung MH, Chen YL, Chu PY, Wang CY,
Chao TT, Liu CY, Shiau CW and Chen KF: Erlotinib derivative
inhibits hepatocellular carcinoma by targeting CIP2A to reactivate
protein phosphatase 2A. Cell Death Dis. 5:e13592014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ahmad SA, Bilimoria MM, Wang X, Izzo F,
Delrio P, Marra P, Baker TP, Porter GA, Ellis LM, Vauthey JN, et
al: Hepatitis B or C virus serology as a prognostic factor in
patients with hepatocellular carcinoma. J Gastrointest Surg.
5:468–476. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
de Oliveria Andrade LJ, D'Oliveira A, Melo
RC, De Souza EC, Silva Costa CA and Paraná R: Association between
hepatitis C and hepatocellular carcinoma. J Glob Infect Dis.
1:33–37. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Douam F, Ding Q and Ploss A: Recent
advances in understanding hepatitis C. F1000Res. 3(5): pii: F1000
Faculty Rev. –131. 2016.
|
|
22
|
Street A, Macdonald A, Crowder K and
Harris M: The Hepatitis C virus NS5A protein activates a
phosphoinositide 3-kinase-dependent survival signaling cascade. J
Biol Chem. 279:12232–12241. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Street A, Macdonald A, McCormick C and
Harris M: Hepatitis C virus NS5A-mediated activation of
phosphoinositide 3-kinase results in stabilization of cellular
beta-catenin and stimulation of beta-catenin-responsive
transcription. J Virol. 79:5006–5016. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Liu Z, Tian Y, Machida K, Lai MM, Luo G,
Foung SK and Ou JH: Transient activation of the PI3K-AKT pathway by
hepatitis C virus to enhance viral entry. J Biol Chem.
287:41922–41930. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ali N, Allam H, May R, Sureban SM, Bronze
MS, Bader T, Umar S, Anant S and Houchen CW: Hepatitis C
virus-induced cancer stem cell-like signatures in cell culture and
murine tumor xenografts. J Virol. 85:12292–12303. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gargini R, Cerliani JP, Escoll M, Antón IM
and Wandosell F: Cancer stem cell-like phenotype and survival are
coordinately regulated by Akt/FoxO/Bim pathway. Stem Cells.
33:646–660. 2015. View Article : Google Scholar : PubMed/NCBI
|