Introduction
Gastric cancer has become the 3rd leading cause for
cancer death in the world (1), and
ranks 1st in all malignant tumors in China. Most of the gastric
cancer patients have been diagnosed as the adenocarcinoma type.
Currently, pathogenesis of gastric cancer remains unknown due to
the heterogeneity in histological and pathological features of
gastric cancer, and the diagnostic rate in an early stage is
relatively low; nowadays, resection has been used as the preferred
option for treatment of gastric adenocarcinoma without distant
metastasis (1,2). According to the literature, it is
reported that tumor diameter, regional lymphatic metastasis,
vascular invasion, pTNM stage and surgical method are major factors
affecting the prognosis of gastric cancer patients (3–5). To
investigate the clinicopathologic factors associated with the
long-term survival of gastric cancer patients after surgery, and to
assess the prognosis and guide the treatment, we evaluated the
prognosis and the related factors of 298 gastric adenocarcinoma
patients without distant metastasis who underwent D2 resection for
gastric cancer in Shandong Provincial Hospital.
Patients and methods
General materials
Between January, 2005 and January, 2012, a total of
321 patients were admitted to the Gastrointestinal Surgery
Department of Shandong Provincial Hospital Affiliated to Shandong
University for D2 resection for gastric cancer, in which there were
23 patients with distant metastasis who were diagnosed as
non-adenocarcinoma in postoperative pathological examination. The
remaining 298 patients were confirmed as the gastric adenocarcinoma
within stage I to III (M0), and those patients with their perfect
clinicopathologic material and follow-up material were enrolled as
the subjects in this study. In the participants, there were 201
males and 97 females with a sex ratio of 2.1:1.0; the age ranged
from 23 to 83 years with an average of 61 years. All participants
were confirmed as non-distant metastasis patients through
examinations of ultrasonic B, computed tomography [CT; or magnetic
resonance imaging (MRI)] and surgical exploration. This study was
approved by the Ethics Committee of Shandong Provincial Hospital
Affiliated to Shandong University. Signed written informed consents
were obtained from the patients.
Material collection and follow-up
After surgery, follow-up was carried out as
out-patient review in combination with call visit or mail. In
addition, we collected the material of patients, including sex,
age, income, tissue differentiation, tumor diameter, regional
lymphatic metastasis, vascular invasion and pTNM stages. With month
as unit and death as outcome event, statistics on survival time of
patients were collected, while the material of patients was deleted
for missing cases or other causes of death. The follow-up ended in
January, 2017.
Statistical analysis
SPSS 22.0 (IBM, Armonk, NY, USA) was used for data
analysis. Chi-square test was performed for enumeration data,
postoperative survival rate was calculated using Kaplan-Meier
survival curve and significance testing was carried out using
log-rank method through one-way analysis of variance (ANOVA).
Variables with statistical significance (P<0.1) in one-way ANOVA
were incorporated into the Cox regression model for multivariate
analysis.
Results
Survival of patients
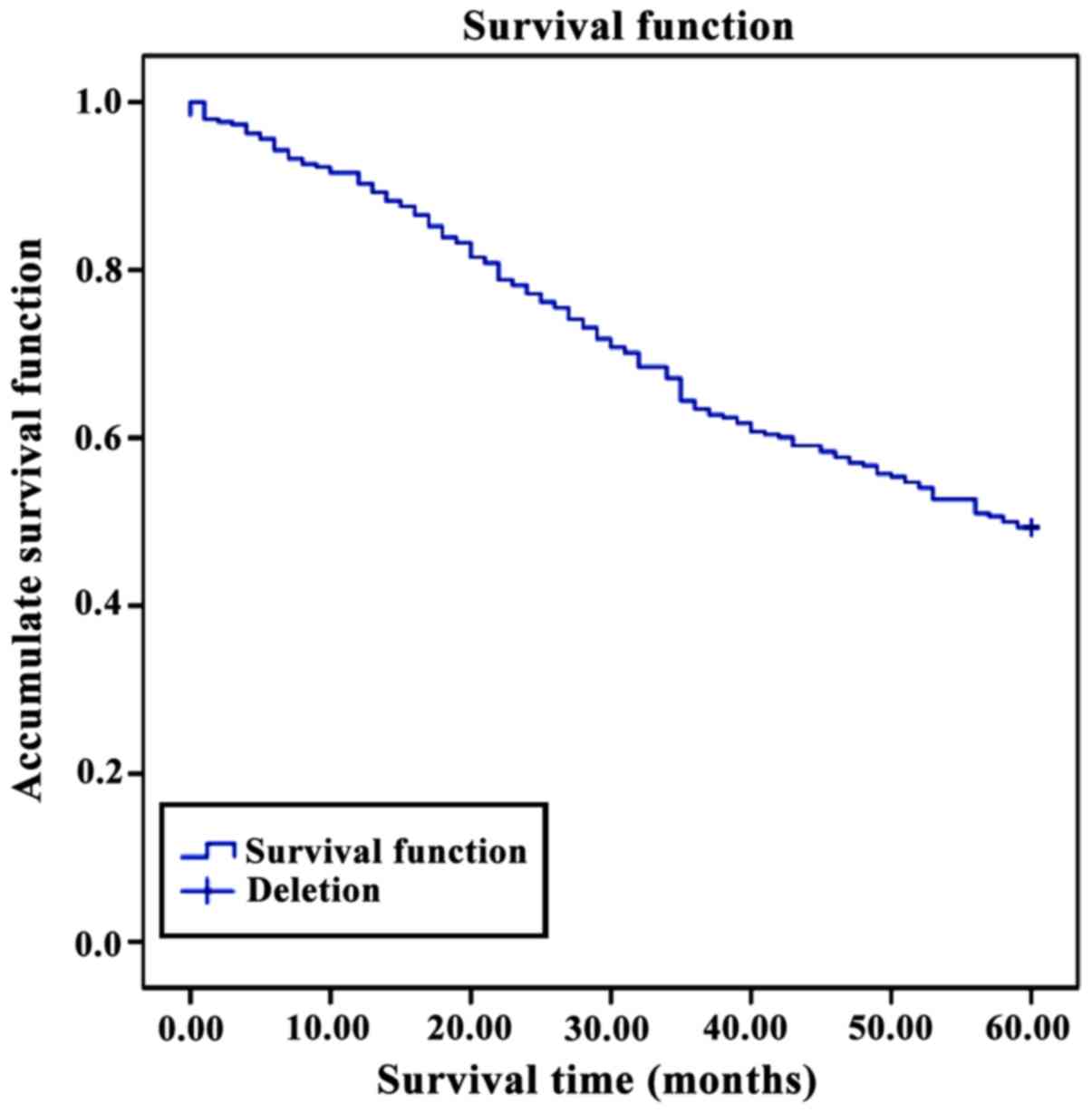
Of the 298 patients who received D2 resection for
gastric cancer, there were 2 patients who died in perioperative
period and 13 patients were lost to follow-up or died of other
causes, and the follow-up rate was 94.96%. The follow-up was for 60
months. The median survival time was 38 months, while the 5-year
accumulate survival rate was 49.3% (Fig.
1).
One-way ANOVA of prognostic factors on
gastric cancer
Comparisons of tumor position, regional lymphatic
metastasis, vascular invasion, pTNM stage and 5-year survival rate
showed that the differences had statistical significance
(P<0.05), suggesting that those are the factors affecting the
prognosis of M0 gastric adenocarcinoma. However, sex, age, tissue
differentiation and position of tumor posed no significant effects
on the 5-year survival rate of patients (P>0.05), and the
prognosis of M0 gastric adenocarcinoma (Table I).
 | Table I.Clinicopathological material and
5-year survival rate of 298 patients with no distant
metastasis. |
Table I.
Clinicopathological material and
5-year survival rate of 298 patients with no distant
metastasis.
| Clinicopathological
material | n | 5-year survival
rate | χ2
value | P-value |
|---|
| Age (years) |
|
| 3.95 | 0.138 |
| ≤40 | 26 | 30.8 |
|
|
| >40
and ≤60 | 107 | 50.5 |
|
|
|
>60 | 165 | 51.5 |
|
|
| Sex |
|
| 0.906 | 0.341 |
| Male | 201 | 51.2 |
|
|
|
Female | 97 | 45.4 |
|
|
| Differentiation |
|
| 2.58 | 0.108 |
| Non- or
low-differentiation | 166 | 45.2 |
|
|
| Mid- or
high-differentiation | 132 | 54.5 |
|
|
| Tumor position |
|
| 5.44 | 0.066 |
|
Upper | 54 | 38.9 |
|
|
|
Median | 69 | 43.5 |
|
|
|
Lower | 175 | 54.9 |
|
|
| Tumor diameter
(cm) |
|
| 4.84 | 0.028 |
| ≤5 | 119 | 57.1 |
|
|
|
>5 | 179 | 44.147 |
|
|
| Regional lymphatic
metastasis |
|
| 17.39 | <0.01 |
| None | 73 | 64.4 |
|
|
|
Perigastric metastasis | 108 | 54.6 |
|
|
|
Metastasis outside
stomach | 118 | 35.0 |
|
|
| Vascular
invasion |
|
| 4.34 | 0.037 |
| Yes | 68 | 38.2 |
|
|
| No | 230 | 52.6 |
|
|
| pTNM stages |
|
| 33.65 | <0.01 |
| Stage
I | 46 | 78.2 |
|
|
| Stage
II | 108 | 58.3 |
|
|
| Stage
III | 144 | 33.3 |
|
|
Multivariate analysis of Cox
regression model
Factors that were identified with effect on
prognosis of gastric adenocarcinoma patients with no distant
metastasis in one-way ANOVA (P<0.1) received further
multivariate analysis of Cox regression model, and the results
showed that tumor position, regional lymphatic metastasis, vascular
invasion and pTNM stages are the independent risk factors affecting
the gastric adenocarcinoma without distant metastasis (P<0.05).
One-way ANOVA revealed the correlation between the tumor diameter
and the prognosis of patients with M0 gastric adenocarcinoma, but
this correlation showed no statistical significance in analysis of
the final multivariate models (Table
II).
 | Table II.Multivariate analysis of the factors
affecting the prognosis of 298 patients with distant
metastasis. |
Table II.
Multivariate analysis of the factors
affecting the prognosis of 298 patients with distant
metastasis.
| Variate | Estimated value | Standard error | Wald value | P-value | Odds ratio | 95% confidential
interval |
|---|
| Tumor position | 1.21 | 0.56 | 6.24 | 0.016 | 3.91 | 1.96–5.26 |
| Regional lymphatic
metastasis (n) | 1.65 | 0.38 | 5.21 | 0.042 | 3.12 | 2.21–8.36 |
| Vascular
metastasis | 1.29 | 0.24 | 11.45 | 0.021 | 3.52 | 2.36–7.56 |
| pTNM stages | 1.09 | 0.15 | 18.37 | 0.009 | 4.25 | 1.19–8.95 |
Discussion
Gastric cancer is one of the major causes in
cancer-related death in China, while the adenocarcinoma occupies
over 95% in malignant tumors in the stomach. Thus, how to increase
the postoperative survival rate in gastric adenocarcinoma patients
has become one of the primary targets in clinical research. Various
factors affect the prognosis of gastric adenocarcinoma, in which
pTNM stage is one of the most important factors (6). Precise pathological staging is conducive
to assessment of prognosis and guidance of treatment. Currently,
among the patients with gastric adenocarcinoma in an early stage,
5-year survival rate reaches over 90%, and improvement in survival
and prognosis of patients with gastric adenocarcinoma in stage I,
II or III (M0) can tremendously increase the overall survival rate
of gastric cancer patients (7). In
this study, we investigated the correlation between the
pathological parameters (including sex, age, tumor position,
differentiation of tumor, tumor diameter, regional lymphatic
metastasis and vascular invasion) and the survival time of gastric
cancer patients through retrospective analysis of 298 patients with
gastric adenocarcinoma in stage I, II or III (M0) who received the
D2 resection for gastric cancer.
The analysis of clinicopathological features of M0
gastric adenocarcinoma patients showed that the sex ratio of
patients was 2.1:1.0, but the comparison of 5-year survival rate in
patients revealed no statistically significant difference,
suggesting that the difference in sex does not affect the prognosis
of patients. As for the age of onset, young patients (age ≤40
years) occupied 8.7%, which coincide with the description in
previous studies (8). Among young
patients undergoing D2 resection for gastric cancer, the 5-year
survival rate was only 30.7%, <50.5% in middle-aged patients (41
to 60 years) and 51.5% in elder patients (age >60 years).
Comparison of prognosis among patients in different age showed no
statistically significant difference (P=0.138). In this study,
patients with gastric adenocarcinoma in non- or low-differentiation
slightly overweighed those in moderate- or high-differentiation;
among the young and middle-aged patients, most of them were with
gastric adenocarcinoma in low- or non-differentiation, and were in
stage III or above at the time of diagnosis due to the high
malignancy and rapid progression. However, young patients are
usually without other severe organic diseases and are tolerant to
surgery. Thus, despite of the higher 5-year survival rate among the
gastric adenocarcinoma patients in moderate- or
high-differentiation, one-way ANOVA showed no statistically
significant difference (P>0.05).
In this study, the proportion of patients with
tumors in upper parts of stomach was relatively low, and their
5-year survival rate (38.9%) was inferior to those with tumor in
middle or lower parts of stomach. While in the patients with tumor
in lower part of stomach, the 5-year survival rate was 54.9%,
significantly higher than that in the patients with tumor in upper
part of the stomach. Petrelli et al (9) reported tumors in upper 1/3 region of
stomach can increase the risk of tumor-related death, suggesting
that the position of tumor is a key prognostic factor (9). In this study, the results of one-way
ANOVA showed P=0.066, slightly >0.05, but multivariate analysis
suggested that the position of tumor is an independent risk factor.
Also, analysis of results showed that patients with tumors in the
upper region of stomach are more susceptible to regional lymphatic
metastasis, which conforms to the results of previous studies in
other countries (9,10). Studies have shown that regional
lymphatic metastasis is one of the key risk factors leading to the
postoperative recurrence and death of patients with gastric
adenocarcinoma (11), which could
serve as not only the prognostic indicator for development and
outcome of patients, but also important evidence for stipulating
the adjuvant therapy and follow-up procedure after surgery.
Clinically, during the extraction and examination of lymph nodes,
it is quite difficult to evaluate the quantity of lymph nodes if
there is fusion of metastatic lymph nodes (12). In this study, all participants
underwent standard D2 resection, and after lymph node dissection,
>20 lymph nodes would be obtained for biopsy, thereby confirming
the regional lymphatic metastasis based on the statistics, which
could also maximally reduce the bias in stages caused by uneven
quantity of lymph nodes (13). Nitti
et al (14) carried out a
study involving 277 patients with lymphatic metastasis, and the
results showed that the quantity of metastatic lymph nodes in
gastric cancer patients is an effective prognostic factor, which is
consistent with the results of our study. With 5 cm as a critical
point, we divided the patients in gastric adenocarcinoma of stage
T1-3 into the large-diameter group (>5 cm) and small-diameter
group (≤5 cm) and the 5-year survival rates of these two groups
were 44.2 and 57.1%. One-way ANOVA of these results showed
P<0.05, suggesting that the difference had statistical
significance, but analysis in Cox regression models suggested no
statistically significant differences in comparisons of tumor
diameter and survival of patients. Hence, the diameter of tumor is
not an independent risk factor affecting the prognosis of patients
with gastric adenocarcinoma. Kunisaki et al (15) reported that the tumor diameter can be
used as an independent risk factor affecting the prognosis of
gastric adenocarcinoma patients depending on the infiltration of
the tumors, while in gastric adenocarcinoma, the range of tumor
infiltration to the adjacent organs is considered as the major
factor influencing the prognosis of patients (15).
pTNM stage serves as the crucial reference for
choice of clinical treatment strategy and assessment of prognosis
for gastric adenocarcinoma (16). In
late 2016, the American Joint Committee on Cancer (AJCC) released
the TNM staging system for gastric cancer (8th edition), with which
physicians can stipulate more rational therapeutic procedure and
assess the efficacy of the procedure in a scientific way, and the
new edition of TNM staging system is conducive to increase
precision of assessment of prognosis (17). Tokunaga et al (18,19), and
the multivariate analysis in this study indicated that pTNM stage
is one of the most important indicators influencing the
postoperative prognosis of gastric adenocarcinoma patients after D2
resection. In the 298 participants, there were 68 cases with
positive signs of vascular invasion, significantly lower than 230
cases with negative signs. Among those with positive signs, the
5-year survival rate was significantly lower, and the multivariate
analysis suggested that vascular invasion is an independent risk
factor of survival and prognosis of gastric adenocarcinoma
(20). Besides, a significant
correlation was identified with the vascular invasion and the poor
prognosis of gastric adenocarcinoma (11,21).
In conclusion, the one-way ANOVA and multivariate
analysis of Cox regression models suggested that pTNM stage, tumor
position, regional lymphatic metastasis and vascular invasion are
the independent risk factors affecting the prognosis of gastric
adenocarcinoma patients with non-distant metastasis. Thus,
comprehensive assessment of patient's condition and prophylactic
and therapeutic measures should be taken to increase the survival
rate of gastric adenocarcinoma patients.
References
|
1
|
Nam S, Chung JW and Yang JY: WNT5A
correlates with clinicopathological characteristics in gastric
cancer: A meta-analysis. Cell Physiol Biochem. 41:33–40. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wang J, Liu J, Zhang G and Kong D:
Individualized proximal margin correlates with outcomes in gastric
cancers with radical gastrectomy. Tumour Biol.
39:10104283177110322017.PubMed/NCBI
|
|
3
|
Kim DH, Kim SM, Choi MG, Sohn TS, Bae JM
and Kim S: Multiple primary malignancies in patients with multiple
early gastric cancer. J Gastric Cancer. 17:154–161. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Son T, Kwon IG, Lee JH, Choi YY, Kim HI,
Cheong JH, Noh SH and Hyung WJ: Impact of splenic hilar lymph node
metastasis on prognosis in patients with advanced gastric cancer.
Oncotarget. Jun 28–2017.(Epub ahead of print).
|
|
5
|
Gui R, Tang H, Gao M, Liu J, Huang R, Zhao
G, Ma J, Yi M, Liu F and Fu Y: Impact of perioperative blood
transfusion on survival of patients undergoing laparoscopic
gastrectomy for gastric cancer. J BUON. 22:396–402. 2017.PubMed/NCBI
|
|
6
|
Yu B and Xie J: Identifying therapeutic
targets in gastric cancer: The current status and future direction.
Acta Biochim Biophys Sin (Shanghai). 48:90–96. 2016.PubMed/NCBI
|
|
7
|
Spychała A, Nowaczyk P and Murawa D:
Comparison of lymphatic system staging classifications in patients
with gastric cancer. Pol Przegl Chir. 87:551–557. 2015.PubMed/NCBI
|
|
8
|
Qiu MZ, Wang ZQ, Zhang DS, Luo HY, Zhou
ZW, Wang FH, Li YH, Jiang WQ and Xu RH: Clinicopathological
characteristics and prognostic analysis of gastric cancer in the
young adult in China. Tumour Biol. 32:509–514. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Petrelli F, Ghidini M, Barni S,
Steccanella F, Sgroi G, Passalacqua R and Tomasello G: Prognostic
role of primary tumor location in non-metastatic gastric cancer: A
systematic review and meta-analysis of 50 studies. Ann Surg Oncol.
24:2655–2668. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Costa LB, Toneto MG and Moreira LF: Do
proximal and distal gastric tumours behave differently? Arq Bras
Cir Dig. 29:232–235. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ahmad R, Setia N, Schmidt BH, Hong TS, Wo
JY, Kwak EL, Rattner DW, Lauwers GY and Mullen JT: Predictors of
lymph node metastasis in western early gastric cancer. J
Gastrointest Surg. 20:531–538. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lee JH, Kang JW, Nam BH, Cho GS, Hyung WJ,
Kim MC, Lee HJ, Ryu KW, Ryu SW, Shin DW, et al: Correlation between
lymph node count and survival and a reappraisal of lymph node ratio
as a predictor of survival in gastric cancer: A multi-institutional
cohort study. Eur J Surg Oncol. 43:432–439. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim JJ, Song KY, Hur H, Hur JI, Park SM
and Park CH: Lymph node micrometastasis in node negative early
gastric cancer. Eur J Surg Oncol. 35:409–414. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nitti D, Marchet A, Olivieri M, Ambrosi A,
Mencarelli R, Belluco C and Lise M: Ratio between metastatic and
examined lymph nodes is an independent prognostic factor after D2
resection for gastric cancer: Analysis of a large European
monoinstitutional experience. Ann Surg Oncol. 10:1077–1085. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kunisaki C, Makino H, Takagawa R, Oshima
T, Nagano Y, Kosaka T, Ono HA, Otsuka Y, Akiyama H, Ichikawa Y, et
al: Tumor diameter as a prognostic factor in patients with gastric
cancer. Ann Surg Oncol. 15:1959–1967. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ren K, Liu QQ, An ZF, Zhang DP and Chen
XH: MiR-144 functions as tumor suppressor by targeting PIM1 in
gastric cancer. Eur Rev Med Pharmacol Sci. 21:3028–3037.
2017.PubMed/NCBI
|
|
17
|
Sano T, Coit DG, Kim HH, Roviello F,
Kassab P, Wittekind C, Yamamoto Y and Ohashi Y: Proposal of a new
stage grouping of gastric cancer for TNM classification:
International Gastric Cancer Association staging project. Gastric
Cancer. 20:217–225. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tokunaga M, Ito S, Yoshikawa T, Nunobe S,
Fukagawa T, Misawa K, Cho H, Katai H, Sano T and Terashima M:
Prognostic factors for survival in patients with pT1 N+
or T2-3 N0 gastric cancer in Japan. Br J Surg. 104:885–890. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wen T, Wang Z, Li Y, Li Z, Che X, Fan Y,
Wang S, Qu J, Yang X, Hou K, et al: A Four-Factor immunoscore
system that predicts clinical outcome for stage II/III gastric
cancer. Cancer Immunol Res. 5:524–534. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wang Z, Zhang X, Hu J, Zeng W and Zhou Z:
Clinicopathological features and outcomes in patients undergoing
radical resection for early gastric cancer with signet ring cell
histology. J Visc Surg. 152:357–361. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li P, He HQ, Zhu CM, Ling YH, Hu WM, Zhang
XK, Luo RZ, Yun JP, Xie D, Li YF, et al: The prognostic
significance of lymphovascular invasion in patients with resectable
gastric cancer: A large retrospective study from Southern China.
BMC Cancer. 15:3702015. View Article : Google Scholar : PubMed/NCBI
|