Introduction
Since laparoscopic-assisted distal gastrectomy was
first reported by Kitano et al (1), the effectiveness for laparoscopic distal
gastrectomy in the treatment of early gastric cancer has been
established in several clinical studies (2–6). Moreover,
in the past 15 years, totally laparoscopic distal gastrectomy
(TLDG), in which all surgical procedures including lymph node
dissection, gastric resection, and anastomosis are performed in a
wide laparoscopic visual field, has been developed due to
improvements in laparoscopic devices and techniques (7–18).
Therefore, we introduced TLDG with Roux-en-Y reconstruction or
Billroth-I (B-I) reconstruction in 2013. Antecolic Roux-en-Y
reconstruction with antiperistaltic gastrojejunostomy was used when
the remnant stomach was small or the first portion of the duodenum
was short (8,11,16,17). On
the other hand, B-I reconstruction was used when the tension in the
gastroduodenostomy was low.
Since intracorporeal delta-shaped B-I
reconstruction, in which a functional end-to-end gastroduodenostomy
was performed using endoscopic linear staplers, was first described
by Kanaya et al, this technique has been accepted worldwide
(7,9–15,17,18).
However, the disadvantage of this procedure is the higher cost
because it requires many linear stapler cartridges (7,9,10,12).
Furthermore, Noshiro et al reported that one knotted suture
was added on the greater curvature side of the closed entry hole
for the stapler to prevent not only anastomotic leakage but also
intraabdominal abscess around the anastomosis (15).
V-Loc 180 Wound Closure device (Covidien, Mansfield,
MA, USA) consists of a barbed unidirectional absorbable thread with
a needle at one end and a loop at the other end. This design causes
the tissues to adhere at many points without the need to tie
surgical knots (19,20). Here, to reduce the number of linear
stapler cartridges used in the intracorporeal delta-shaped
gastroduodenostomy, we present a single-layer entire-thickness
suturing technique for the stapler entry hole using 3-0 V-Loc 180
(VLOCL0604; taper point, 1/2 circle/26 mm; length, 15 cm). In
addition, to prevent both anastomotic leakage and intraabdominal
abscess around the anastomosis, we describe our initial experience
combining the application of additional knotted sutures of 3-0
Prolene (Ethicon Endo-Surgery, Cincinnati, OH, USA).
Materials and methods
From June 2013 to February 2017, 20 patients
underwent TLDG with delta-shaped gastroduodenostomy with the
combined application of 3-0 V-Loc 180 of 15 cm in length and 3-0
Prolene at Otori Stomach and Intestines Hospital. The indication
for TLDG at our institution is T1N0M0 gastric cancer, according to
the Japanese classification of gastric carcinoma (21), that is located in the middle or lower
third of the stomach and is not a candidate for endoscopic
submucosal dissection. B-I reconstruction was performed when the
tension in the gastroduodenostomy was low.
Patients were placed in the modified lithotomy
position. The operator stood between the patient's legs, with the
first assistant operating the laparoscope on the left side and the
second assistant on the right side. After five trocars were placed
in the upper abdomen including the umbilicus and a Nathanson's
retractor was inserted from just below the xiphoid process to
elevate the round ligament and the lateral segment of the liver,
lymphadenectomy based on the Japanese treatment guidelines was
performed under a pneumoperitoneum (22). The duodenal bulb was transected in a
posteroanterior direction using one endoscopic linear stapler
during lymphadenectomy. Proximal gastric resection with reference
to preoperative endoscopic marking was carried out (23), and the specimen was removed through
the extended umbilical wound using a large plastic bag.
Pneumoperitoneum was re-established before the reconstruction.
A small hole was made on the greater curvature side
of the remnant stomach and the posterior side of the duodenum. A
45-mm linear stapler was introduced through a left lower port, with
one jaw in each hole. The stapler was closed and fired to attach
the posterior walls of the remnant stomach and the duodenum
together. After confirming that there was no bleeding in the
intraluminal anastomotic line, the entry hole for the stapler was
closed by the single-layer entire-thickness suturing technique
using a knotless barbed suture combined with the application of
additional knotted sutures.
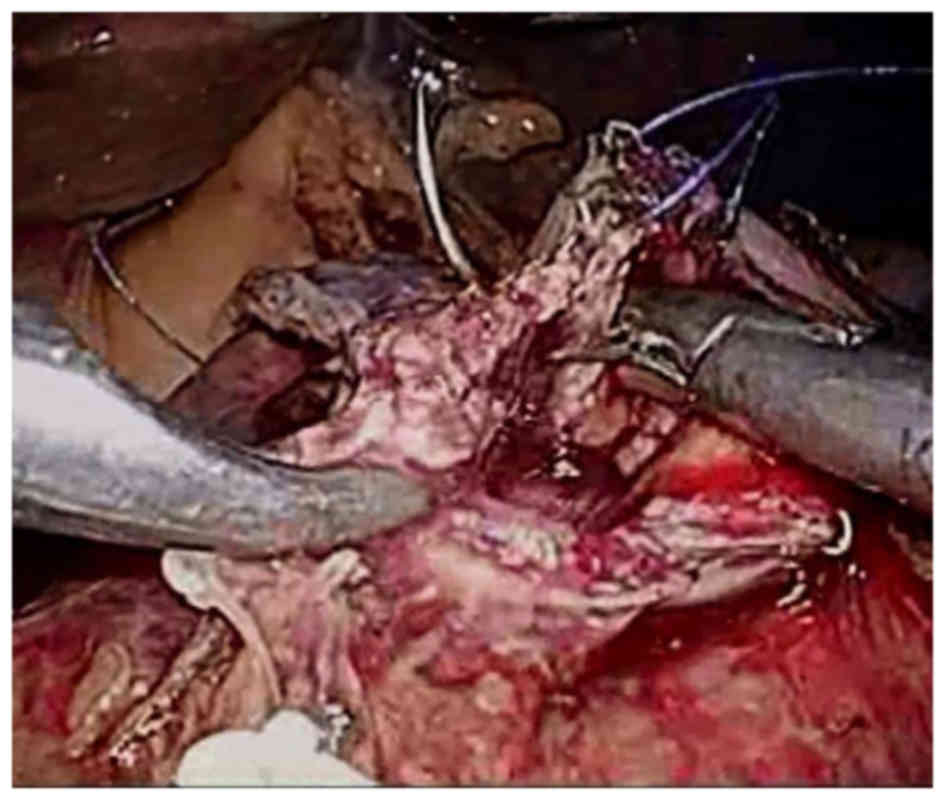
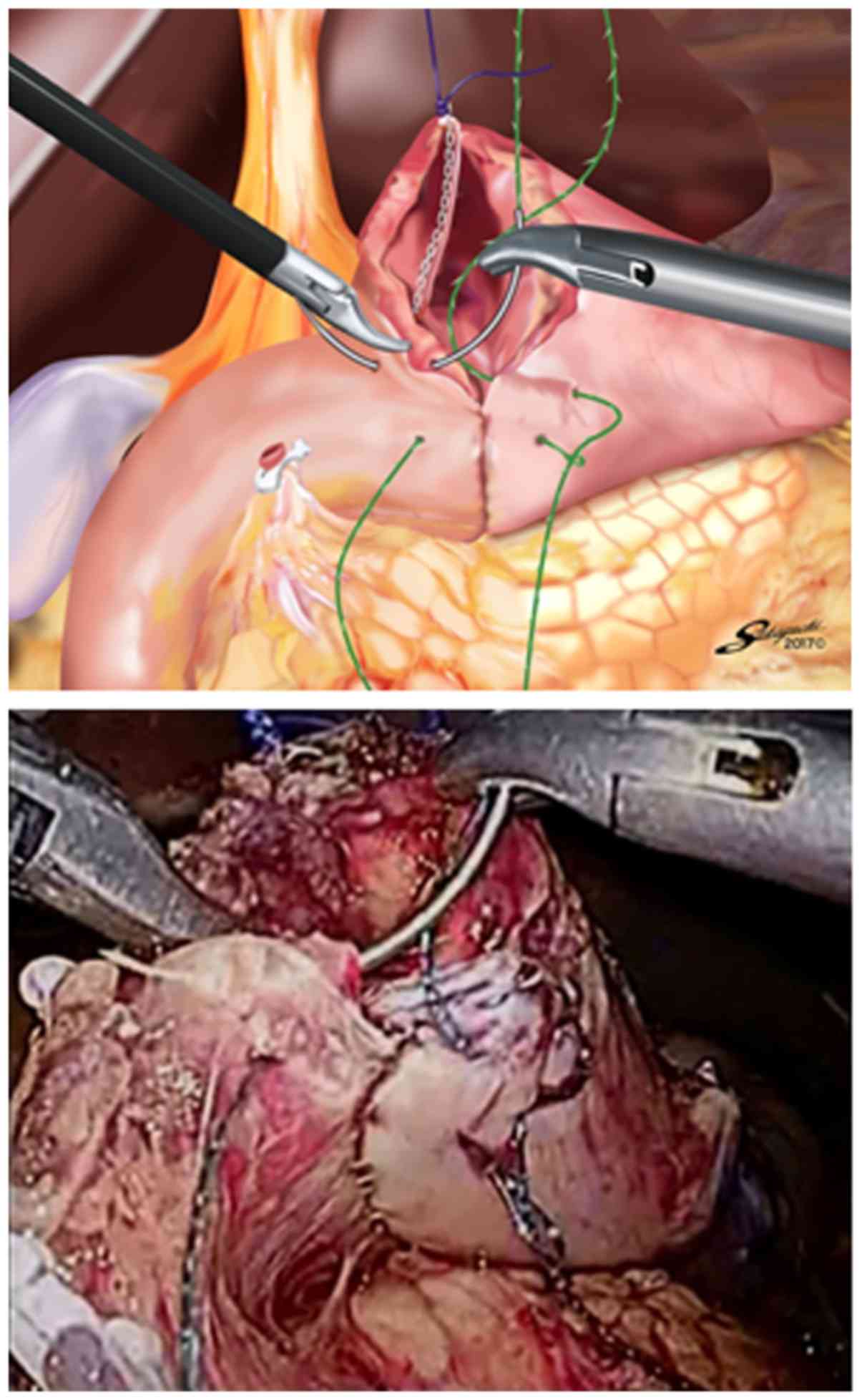
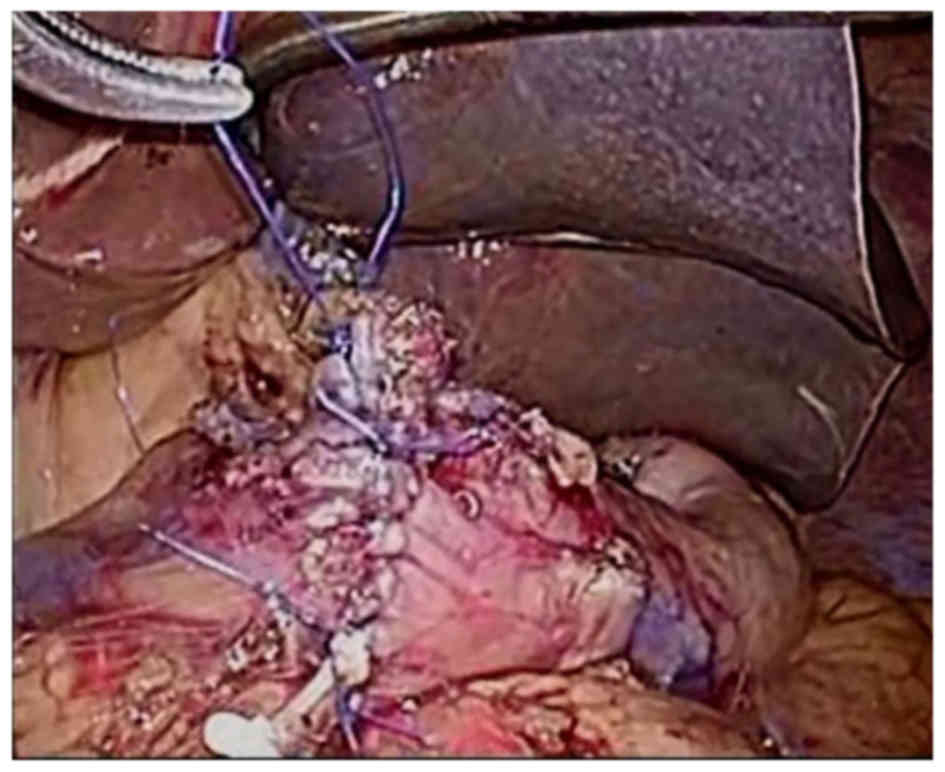
An entire-thickness suture with 3-0 Prolene was
placed on the lesser curvature side of the entry hole using the
extracorporeal slip knot technique (Roeder's knot) (Fig. 1). After creating a good view of the
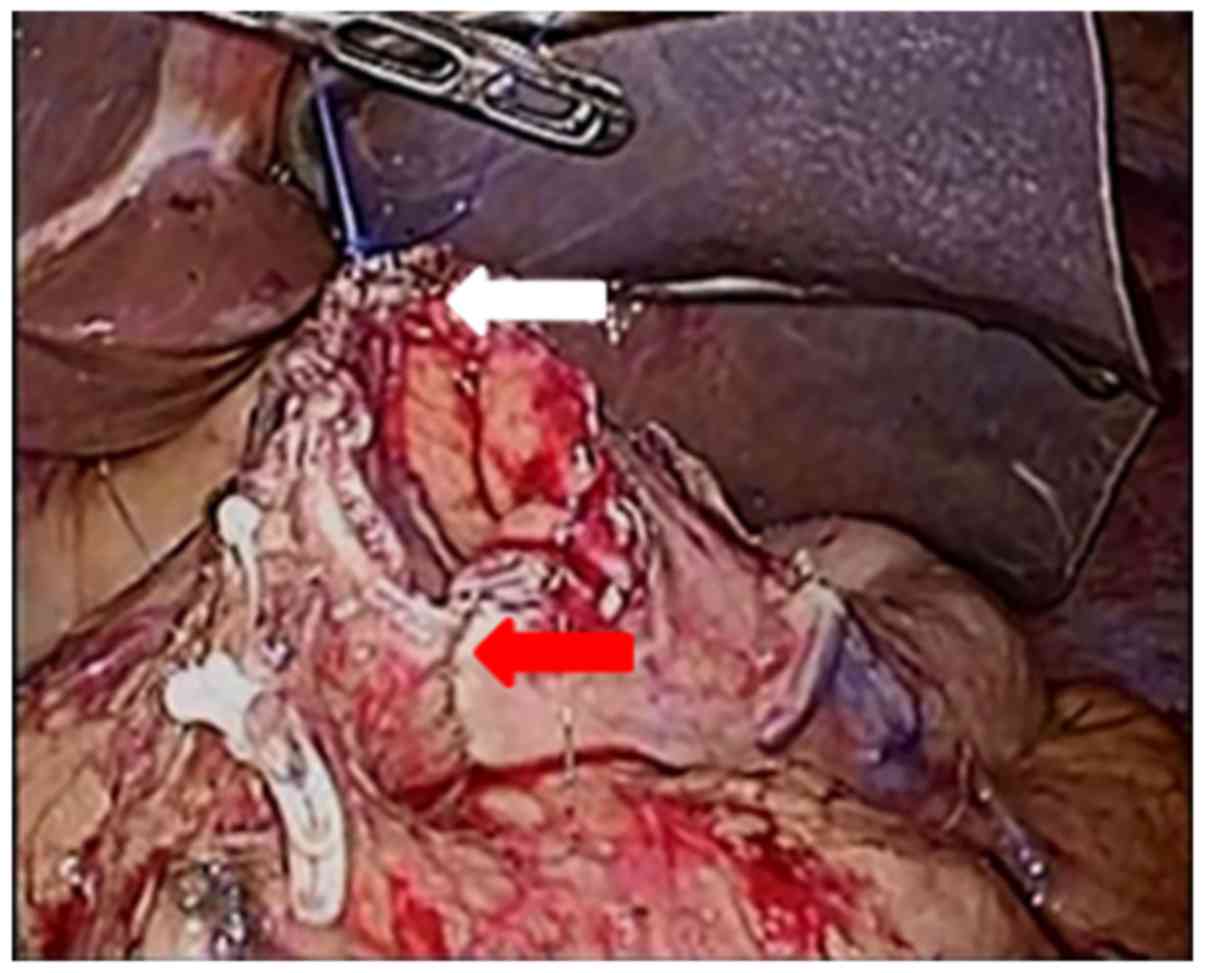
greater curvature side by retracting this knotted suture toward the
ventral side (Fig. 2), continuous
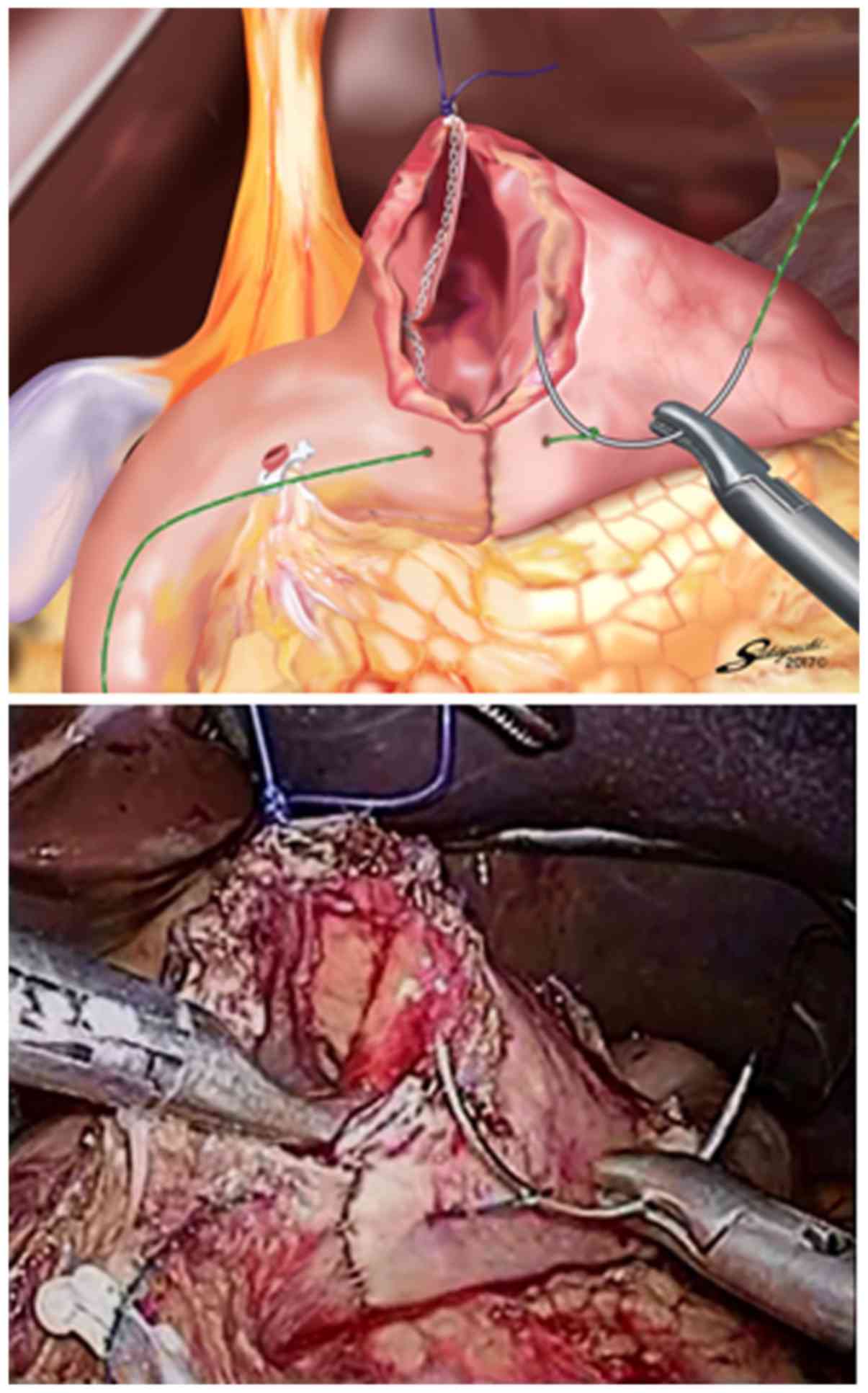
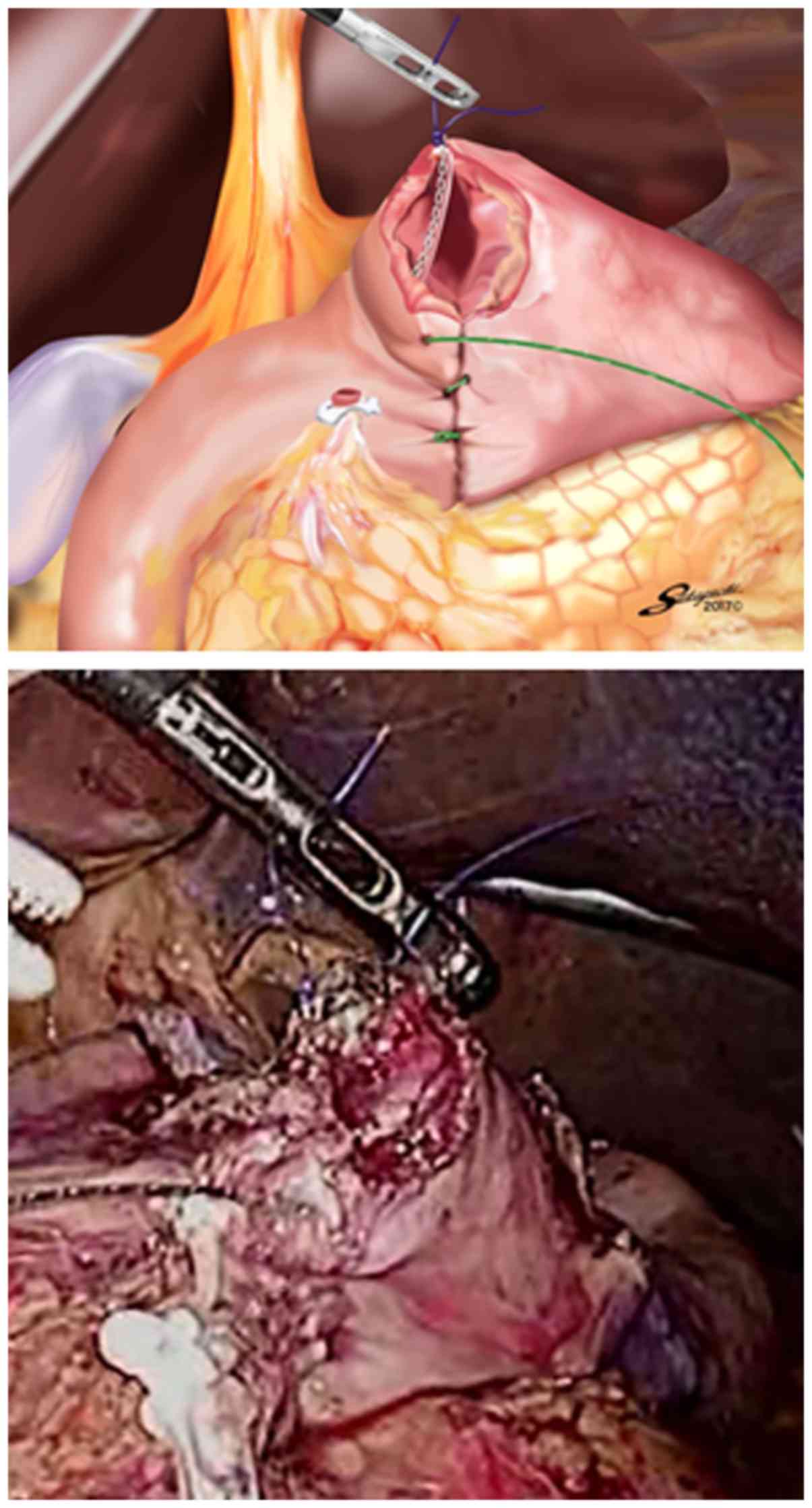
suturing with a 15-cm 3-0 V-Loc 180 device was carried out from the
greater curvature side to the lesser curvature side. The first
entire-thickness stitch was positively placed on the greater
curvature side, and the needle was passed through the loop
(Fig. 3). The second and third
stitches were made between the seromuscular layer of the remnant
stomach and the entire-thickness layer of the duodenum, with the
duodenal mucosa being sutured as minutely as possible (Figs. 4 and 5)
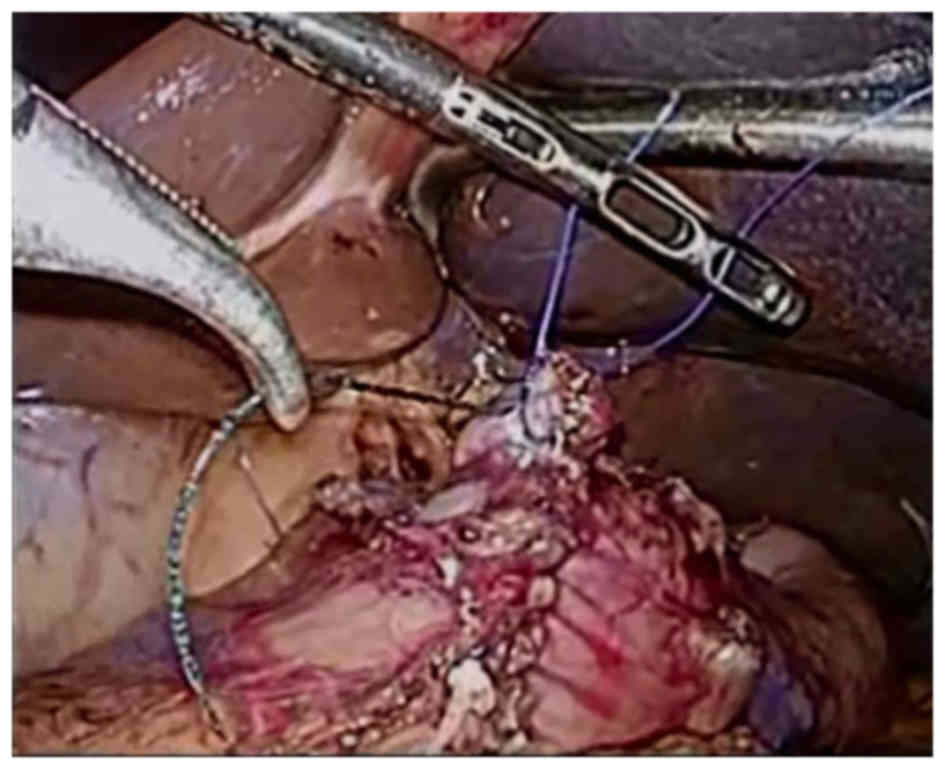
to avoid extroversion of the mucosa of the alimentary tract near
the greater curvature side (Fig. 6).
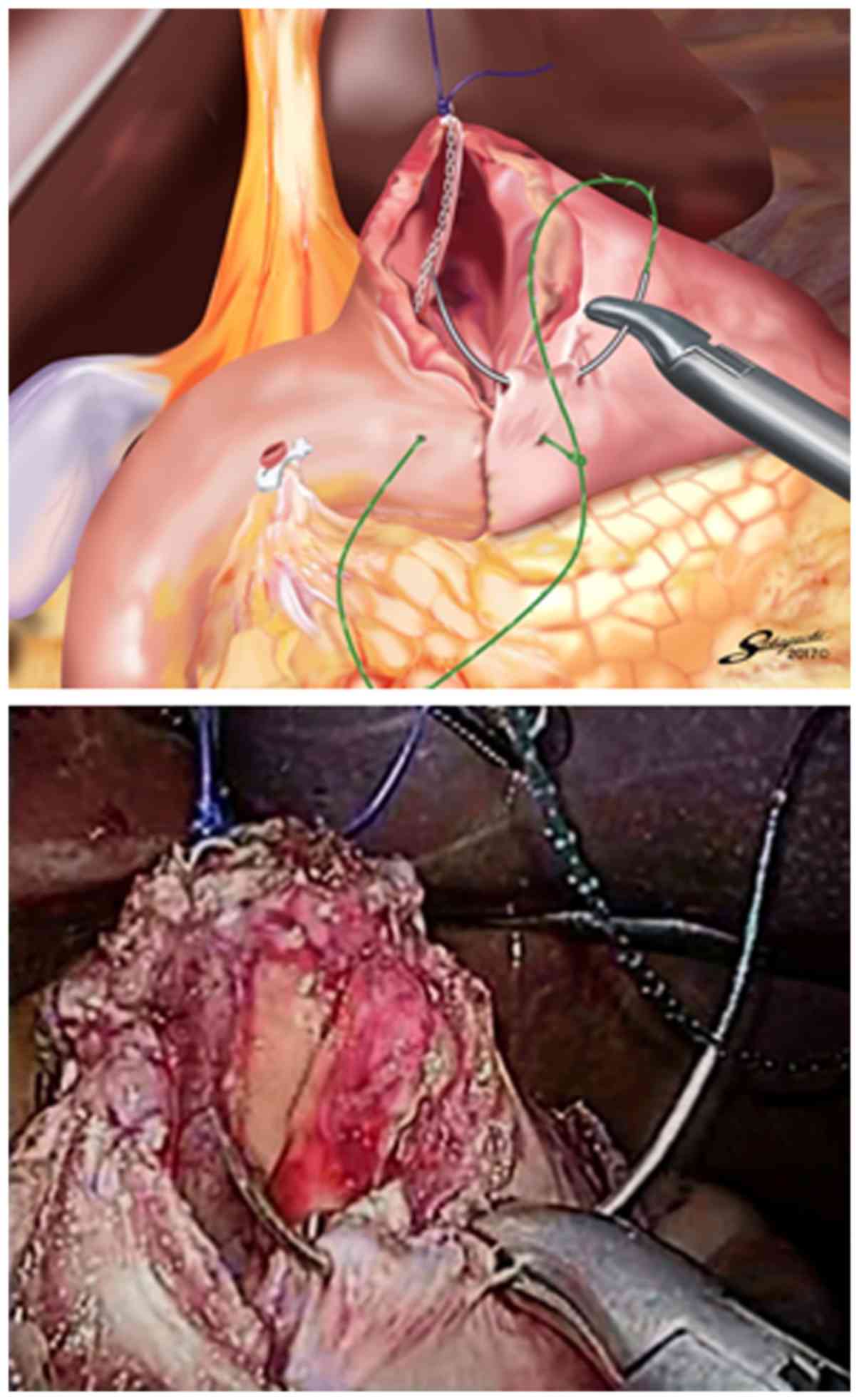
Thereafter, single-layer entire-thickness continuous suturing was
performed until the suture crossed over the knotted suture on the
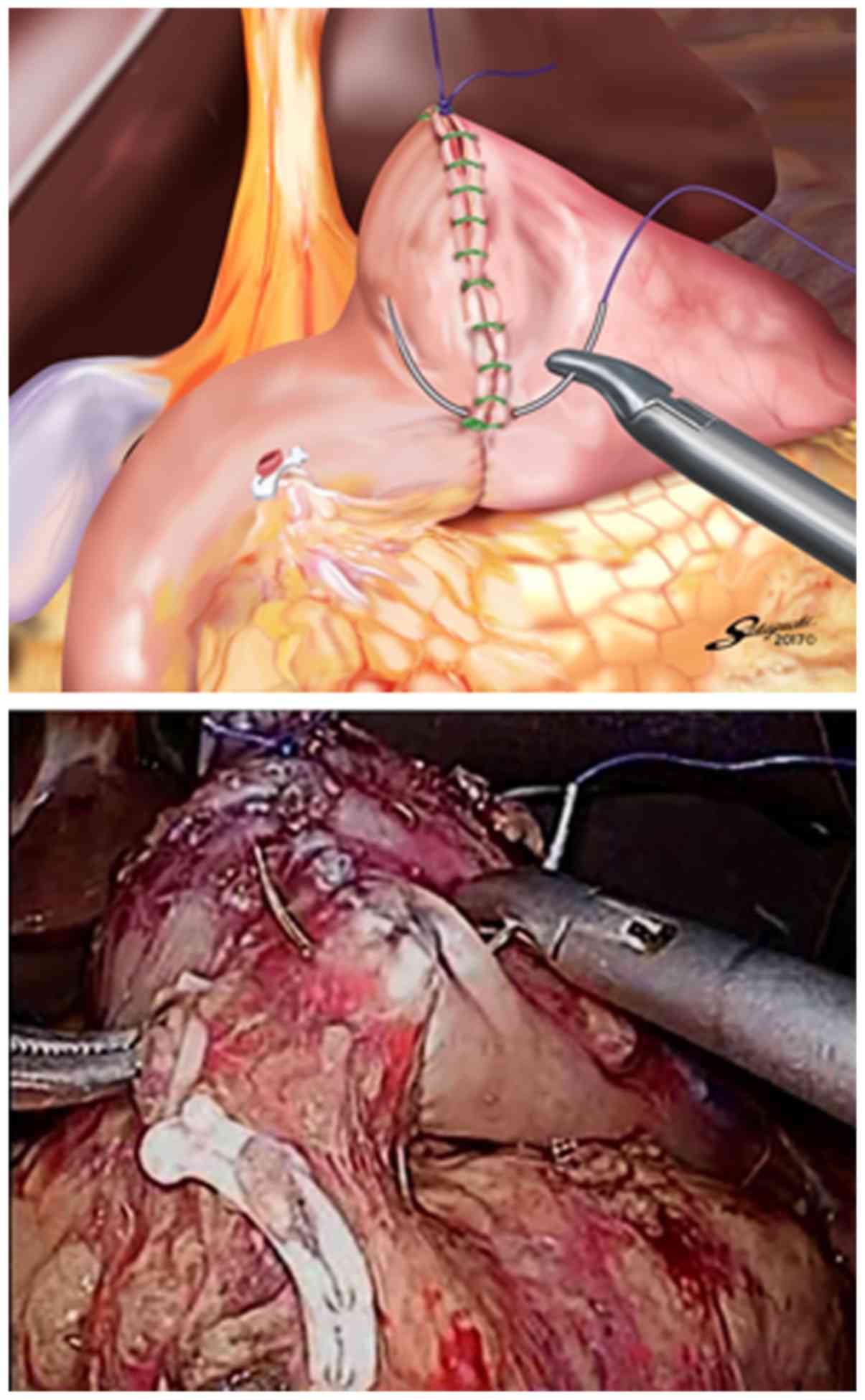
lesser curvature side (Fig. 7). The
suture end was then cut simply, as short as possible, without the
need for a knot. Routinely, one or two entire-thickness knotted
sutures with 3-0 Prolene were added at the site near the greater
curvature side to reinforce this site and avoid loosening of the
3-0 V-Loc 180 (Fig. 8). Similar
additional sutures were made on the site with a broad pitch. The
intracorporeal B-I reconstruction was then accomplished (Fig. 9).
Results
Patient characteristics and operative outcomes are
shown in Table I. In all patients (13
men and 7 women), TLDG with this reconstruction technique was
successfully performed without any intraoperative complications.
The mean patient age was 64.4±7.8 years (45–77 years), and the mean
body mass index was 21.6±1.8 kg/m2 (19.3–24.6
kg/m2). The mean operation time was 249±23 min (205–273
min), and the mean estimated blood loss was 22.5±4.6 ml (20–30 ml).
The mean number of linear stapler cartridges used intraoperatively
was 4.4±0.5 (4–5). The overall mean suturing time of the
stapler entry hole was 14.8±1.6 min (12.0–18.1 min). The mean
suturing time involving the 3-0 V-Loc 180 was 9.4±1.6 min (7.4–13.0
min), and the mean number of additional knotted sutures placed was
2.9±0.9 (2–4). According to the postoperative
complications related to the anastomosis, neither anastomotic
leakage nor intraabdominal abscess around the anastomosis, were
encountered. However, in one patient, anastomotic hemorrhage at the
vertex of the V-shaped staple line requiring endoscopic hemostasis
occurred on postoperative day 1, which was categorized as grade
IIIa according to the Clavien-Dindo classification (24). There were no other complications,
including anastomotic stenosis, pancreatic fistula, and intestinal
obstruction. The mean postoperative hospital stay was 13.8±1.5 days
(12–17 days). Fig. 10 is a typical
upper gastrointestinal fluoroscopic image on postoperative day 3
that shows no anastomotic leakage and stenosis.
 | Table I.Patient characteristics and
outcomes. |
Table I.
Patient characteristics and
outcomes.
| Characteristics and
outcomes | Data |
|---|
| Cases, n | 20 |
| Age, years | 64.4±7.8 |
| Sex, n |
|
| Male | 13 |
|
Female | 7 |
| BMI,
kg/m2 | 21.6±1.8 |
| Operative time,
min | 249±23 |
| Blood loss, ml | 22.5±4.6 |
| Linear stapler
cartridges used, n | 4.4±0.5 |
| Overall suturing
time, min | 14.8±1.6 |
| V-Loc suturing time,
min | 9.4±1.6 |
| Additional knotted
sutures, n | 2.9±0.9 |
| Postoperative
hospital stay, d | 13.8±1.5 |
| Postoperative
complications, n |
|
|
Anastomotic leakage | 0 |
|
Intraabdominal abscess | 0 |
|
Anastomotic hemorrhage | 1 |
|
Anastomotic stenosis | 0 |
|
Pancreatic fistula | 0 |
|
Intestinal obstruction | 0 |
Discussion
To securely perform TLDG for gastric cancer,
establishment of safe and reproducible intracorporeal
reconstruction is essential in addition to precise lymph node
dissection and accurate proximal gastric resection. In B-I
reconstruction for TLDG, the delta-shaped gastroduodenostomy using
only endoscopic linear staplers has been accepted worldwide due to
its safety and simplicity (7,9–15,17,18), but
the disadvantage of this technique is its higher cost (7,9,10,12). On
the other hand, some authors have reported the efficacy of the
knotless barbed unidirectional absorbable suture in
gastrointestinal reconstruction (25–29), and
especially, Nemecek et al stated that single-layer
entire-thickness sutures of the alimentary tract with 3-0 V-Loc 180
had higher bursting pressures than those with 3-0 monofilament in a
cadaver study (27). Therefore, to
reduce the number of linear stapler cartridges used in the
delta-shaped gastroduodenostomy, a single-layer entire-thickness
continuous suturing technique for the stapler entry hole using a
15-cm-long 3-0 V-Loc 180 device was applied because it was not only
effective for gastrointestinal reconstruction but also easy to
handle in the abdominal cavity. In this patient series, no linear
stapler cartridges were used to close the entry hole.
Noshiro et al reported that among the initial
71 patients undergoing delta-shaped gastroduodenostomy using linear
staplers, 6 experienced anastomotic leakage and 2 developed
intraabdominal abscess around the anastomosis, and in all of these
patients, the affected site was the greater curvature side of the
closed entry hole for the stapler (15). They indicated two possible reasons for
these complications. First, the procedure for closing the greater
curvature side of the entry hole was uncertain because this site
tended to roll backward behind the linear stapler. Next, the
extroverted gastroduodenostomy sometimes directly contacted the
pancreatic head after infrapyloric lymph node dissection, and so
even minimal leakage of pancreatic juice might be activated by the
attachment of mucosa of the alimentary tract. They added one
knotted suture on the greater curvature side of the closed entry
hole in the last 71 patients and neither anastomotic leakage nor
intraabdominal abscess around the anastomosis occurred among these
patients. Thus, to stabilize the outcomes of the delta-shaped
gastroduodenostomy with 3-0 V-Loc 180, we standardized the
procedure by adding knotted 3-0 Prolene sutures using the
extracorporeal slip knot technique (Roeder's knot). The steps of
this procedure include; i) retracting the knotted 3-0 Prolene
suture on the lesser curvature side toward the ventral side to
create a good view of the greater curvature side of the entry hole
for the stapler; ii) performing single-layer entire-thickness
continuous suturing of the entry hole using 3-0 V-Loc 180 from the
greater curvature side to the lesser curvature side; iii) placing
the second and third stitches of 3-0 V-Loc 180 between the
seromuscular layer of the remnant stomach and the entire-thickness
layer of the duodenum by suturing the duodenal mucosa as minutely
as possible to avoid extroversion of mucosa of the alimentary tract
near the greater curvature side; iv) routinely adding one or two
entire-thickness knotted sutures with 3-0 Prolene at the site near
the greater curvature side to reinforce this site and avoid
loosening of the 3-0 V-Loc 180; and v) placing similar additional
knotted sutures on the site with a broad pitch. In this patient
series, this reconstruction procedure resulted in no incidences of
anastomotic leakage or intraabdominal abscess around the
anastomosis. These results were comparable to those of the last 71
patients reported by Noshiro et al.
The knotless barbed suture is assumed to make
intracorporeal digestive anastomoses easier to perform because it
does not require any knots and the tension is self-maintained
during the running suture, with no need for continuous traction
(28). In addition, the
extracorporeal knotted suturing technique such as Roeder's knot
could be carried out more easily than the intracorporeal ligation
technique. Therefore, it is considered that a single-layer suturing
technique for the stapler entry hole using 3-0 V-Loc 180 combined
with the application of additional knotted sutures of 3-0 Prolene
is not difficult to master for the gastrointestinal surgeons.
Although there is a concern that the free tail of
the barbed suture might cause intestinal obstruction (30–32), this
complication was not encountered in this series. For this reason,
it could be considered that we cut the suture end as short as
possible and the free tail located at the lesser curvature side of
the closed entry hole was covered by the liver.
In conclusion, it is suggested that a single-layer
entire-thickness suturing technique for the stapler entry hole
using 3-0 V-Loc 180 with a length of 15 cm combined with the
application of additional knotted sutures of 3-0 Prolene can be one
option for delta-shaped gastroduodenostomy in TLDG due to its
cost-effectiveness and feasibility. Examination of a larger number
of patients needs to be performed to draw a conclusion on the
utility of this reconstruction technique.
Glossary
Abbreviations
Abbreviations:
|
BI
|
Billroth-I
|
|
TLDG
|
totally laparoscopic distal
gastrectomy
|
References
|
1
|
Kitano S, Iso Y, Moriyama M and Sugimachi
K: Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc
Endosc. 4:146–148. 1994.PubMed/NCBI
|
|
2
|
Adachi Y, Shiraishi N, Shiromizu A, Bandoh
T, Aramaki M and Kitano S: Laparoscopy-assisted Billroth I
gastrectomy compared with conventional open gastrectomy. Arch Surg.
135:806–810. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kitano S, Shiraishi N, Fujii K, Yasuda K,
Inomota M and Adachi Y: A randomized controlled trial comparing
open vs. laparoscopy-assisted distal gastrectomy for the treatment
of early gastric cancer: An interim report. Surgery. 131(1 Suppl):
S306–S311. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hayashi H, Ochiai T, Shimada H and Gunji
Y: Prospective randomized study of open versus laparoscopy-assisted
distal gastrectomy with extraperigastric lymph node dissection for
early gastric cancer. Surg Endosc. 19:1172–1176. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Naka T, Ishikura T, Shibata S, Yamaguchi
Y, Ishiguro M, Yurugi E, Nishidoi H, Kudoh H, Murakami S and
Tsujitani S: Laparoscopy-assisted and open distal gastrectomies for
early gastric cancer at a general hospital in Japan.
Hepatogastroenterology. 52:293–297. 2005.PubMed/NCBI
|
|
6
|
Kim YW, Baik YH, Yun YH, Nam BH, Kim DH,
Choi IJ and Bae JM: Improved quality of life outcomes after
laparoscopy-assisted distal gastrectomy for early gastric cancer:
Results of a prospective randomized clinical trial. Ann Surg.
248:721–727. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe
H, Katayama T, Wada Y and Ohtoshi M: Delta-shaped anastomosis in
totally laparoscopic Billroth I gastrectomy: New technique of
intraabdominal gastroduodenostomy. J Am Coll Surg. 195:284–287.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Takaori K, Nomura E, Mabuchi H, Lee SW,
Agui T, Miyamoto Y, Iwamoto M, Watanabe H and Tanigawa N: A secure
technique of intracorporeal Roux-Y reconstruction after
laparoscopic distal gastrectomy. Am J Surg. 189:178–183. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kim JJ, Song KY, Chin HM, Kim W, Jeon HM,
Park CH and Park SM: Totally laparoscopic gastrectomy with various
types of intracorporeal anastomosis using laparoscopic linear
staplers: Preliminary experience. Surg Endosc. 22:436–442. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Song KY, Park CH, Kang HC, Kim JJ, Park
SM, Jun KH, Chin HM and Hur H: Is totally laparoscopic gastrectomy
less invasive than laparoscopy-assisted gastrectomy?: Prospective,
multicenter study. J Gastrointest Surg. 12:1015–1021. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ikeda O, Sakaguchi Y, Aoki Y, Harimoto N,
Taomoto J, Masuda T, Ohga T, Adachi E, Toh Y, Okamura T and Baba H:
Advantages of totally laparoscopic distal gastrectomy over
laparoscopically assisted distal gastrectomy for gastric cancer.
Surg Endosc. 23:2374–2379. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kanaya S, Kawamura Y, Kawada H, Iwasaki H,
Gomi T, Satoh S and Uyama I: The delta-shaped anastomosis in
laparoscopic distal gastrectomy: Analysis of the initial 100
consecutive procedures of intracorporeal gastroduodenostomy.
Gastric Cancer. 14:365–371. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim MG, Kawada H and Kim BS, Kim TH, Kim
KC, Yook JH and Kim BS: A totally laparoscopic distal gastrectomy
with gastroduodenostomy (TLDG) for early surgical outcomes in hjgh
BMI patients. Surg Endosc. 25:1076–1082. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kinoshita T, Shibasaki H, Oshiro T,
Ooshiro M, Okazumi S and Katoh R: Comparison of
laparoscopy-assisted and total laparoscopic Billroth-I gastrectomy
for gastric cancer: A report of short-term outcomes. Surg Endosc.
25:1395–1401. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Noshiro H, Iwasaki H, Miyasaka Y,
Kobayashi K, Masatsugu T, Akashi M and Ikeda O: An additional
suture secures against pitfalls in delta-shaped gastroduodenostomy
after laparoscopic distal gastrectomy. Gastric Cancer. 14:385–389.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bouras G, Lee SW, Nomura E, Tokuhara T,
Nitta T, Yoshinaka R, Tsunemi S and Tanigawa N: Surgical outcomes
from laparoscopic distal gastrectomy and Roux-en-Y reconstruction:
Evolution in a totally intracorporeal technique. Surg Laparosc
Endosc Percutan Tech. 21:37–41. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lee SW, Tanigawa N, Nomura E, Tokuhara T,
Kawai M, Yokoyama K, Hiramatsu M, Okuda J and Uchiyama K: Benefits
of intracorporeal gastrointestinal anastomosis following
laparoscopic distal gastrectomy. World J Surg Oncol. 10:2672012.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Matsuhashi N, Yamaguchi K, Okumura N,
Tanahashi T, Matsui S, Imai H, Tanaka Y, Takahashi T, Osada S and
Yoshida K: The technical outcomes of delta-shaped anastomosis in
laparoscopic distal gastrectomy: A single-center safety and
feasible study. Surg Endosc. 31:1257–1263. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Alessandri F, Remorgida V, Venturini PL
and Ferrero S: Unidirectional barbed suture versus continuous
suture with intracorporeal knots in laparoscopic myomectomy: A
randomized study. J Minim Invasive Gynecol. 17:725–729. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shah HN, Nayyar R, Rajamahanty S and Hemal
AK: Prospective evaluation of unidirectional barbed suture for
various indications in surgeon-controlled robotic reconstructive
urologic surgery: Wake Forest University experience. Int Urol
Nephrol. 44:775–785. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Japanese Gastric Cancer Association, .
Japanese classification of gastric carcinoma: 3rd English edition.
Gastric Cancer. 14:101–112. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Japanese Gastric Cancer Association, .
Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric
Cancer. 20:1–19. 2017. View Article : Google Scholar
|
|
23
|
Tokuhara T, Nakata E, Tenjo T, Kawai I,
Satoi S, Inoue K, Araki M, Ueda H and Higashi C: A novel option for
preoperative endoscopic marking with India ink in totally
laparoscopic distal gastrectomy for gastric cancer: A useful
technique considering the morphological characteristics of the
stomach. Mol Clin Oncol. 6:483–486. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dindo D, Demartines N and Clavien PA:
Classification of surgical complications: A new proposal with
evaluation in a cohort of 6336 patients and results of a survey.
Ann Surg. 240:205–213. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lee SW, Nomura E, Tokuhara T, Kawai M,
Matsuhashi N, Yokoyama K, Fujioka H, Hiramatsu M, Okuda J and
Uchiyama K: Laparoscopic technique and initial experience with
knotless, unidirectional barbed suture closure for
staple-conseving, delta-shaped gastroduodenostomy after distal
gastrectomy. J Am Coll Surg. 213:e39–e45. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tyner RP, Clifton GT and Fenton SJ:
Hand-sewn gastrojejunostomy using knotless unidirectional barbed
absorbable suture during laparoscopic gastric bypass. Surg Endosc.
27:1360–1366. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Nemecek E, Negrin L, Beran C, Nemecek R
and Hollinsky C: The application of the V-Loc closure device for
gastrointestinal sutures: A preliminary study. Surg Endosc.
27:3830–3834. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Facy O, De Blasi V, Goergen M, Arru L, De
Magistris L and Azagra JS: Laparoscopic gastrointestinal
anastomoses using knotless barbed sutures are safe and
reproducible: A single-center experience with 201 patients. Surg
Endosc. 27:3841–3845. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Costantino F, Dente M, Perrin P, Sarhan FA
and Keller P: Barbed unidirectional V-Loc 180 suture in
laparoscopic Roux-en-Y gastric bypass: A study comparing
unidirectional barbed monofilament and multifilament absorbable
suture. Surg Endosc. 27:3846–3851. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Thubert T, Pourcher G and Deffieux X:
Small bowel volvulus following peritoneal closure using absorbable
knotless device during laparoscopic sacral colpopexy. Int
Urogynecol J. 22:761–763. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Donnellan NM and Mansuria SM: Small bowel
obstruction resulting from laparoscopic vaginal cuff closure with a
barbed suture. J Minim Invasive Gynecol. 18:528–530. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Buchs NC, Ostermann S, Hauser J, Roche B,
Iselin CE and Morel P: Intestinal obstruction following use of
laparoscopic barbed suture: A new complication with new material?
Minim Invasive Ther Allied Technol. 21:369–371. 2012. View Article : Google Scholar : PubMed/NCBI
|