Introduction
Pancreatic cancer is the eighth-leading cause of
cancer associated mortality in males and the ninth-leading cause in
females worldwide (1). Pancreatic
cancer has a rapid disease progression that is accompanied by the
absence of specific symptoms, which largely precludes early
diagnosis and curative treatment (2,3). The vast
majority of patients with pancreatic cancer are not diagnosed until
their cancer has metastasized, and so surgical treatment is the
only curative treatment. However, due to this late diagnosis the
majority of patients present in an advanced stage, and only a
minority (10–20%) of these patients are amenable to surgical
intervention (4,5). Even when diagnosed early enough to be
potentially resectable, the prognosis of invasive pancreatic cancer
is poor. Due to its high recurrence rate, post-operative patients
with pancreatic cancer require adjuvant chemotherapy with or
without radiotherapy, which provides a 5-year patient survival rate
of 15–25% (6).
Galectin-9 (Gal-9) is a tandem-repeat type galectin
with 2 carbohydrate-recognition domains (CRDs), and it was first
identified as an eosinophil chemoattractant and activation factor
(7–10). Similarly to other galectins, Gal-9
performs a role in cell aggregation and adhesion and in the
apoptosis of tumor cells (10,11). Gal-9
can enhance antitumor immunity through the initial CRD-independent
maturation of dendritic cells and the subsequent induction of
Th1-mediated antitumor immunity (12). In addition, treatment with recombinant
Gal-9 prolonged survival in a murine melanoma model, not only by
increasing the numbers of CD8 cytotoxic T cells (CTLs) but also by
increasing the number of natural killer (NK) cells and macrophages
(13).
Previous studies have uncovered additional
mechanisms by which T cell immunoglobulin mucin-3, a receptor for
Gal-9, negatively regulates T cell responses by promoting CD8+ T
cell exhaustion and inducing the expansion of myeloid-derived
suppressor cells (14,15). Therefore, Gal-9 augments antitumor
immunity by inducing a subset of macrophages and dendritic cells
and activating tumor-specific CTLs and NK cells.
Recombinant Gal-9 induced apoptosis in various T
cell leukemic cell lines in a dose-dependent and functional
CRD-dependent manner (16,17). Additionally, several in vitro
and in vivo studies have also indicated that Gal-9 inhibits
the growth of multiple myeloma (18)
and chronic myeloid leukemia (19).
In hematologic malignancies, Gal-9 suppresses cellular
proliferation and tumor growth in vitro and in vivo.
However, in solid malignancies, the antitumor effect of Gal-9
remains unknown. Previously, it was reported that Gal-9 inhibits
the growth of hepatocellular carcinoma and cholangiocarcinoma via
apoptosis in vitro and in vivo (20,21).
However, less is known regarding the antitumor
effects of Gal-9 on pancreatic cancer cells or the microRNAs
(miRNAs) that are associated with these effects. The present study
therefore evaluated the effects of Gal-9 on the growth of two
pancreatic cancer cell lines, its mechanism of action, and the
miRNAs that are associated with the antitumor effect of Gal-9 on
pancreatic cancer cells.
Materials and methods
Cell lines and culture
The human pancreatic cancer PK-1 and PK-9 cell lines
were obtained from the RIKEN cell bank (Ibarkai, Japan) and
passaged in our laboratory for <6 months. The 2 cell lines were
authenticated by the cell bank using short tandem repeat polymerase
chain reaction. PK-1 and PK-9 cells were grown in RPMI 1640
supplemented with 10% fetal bovine serum and 100 mg/l of
penicillin-streptomycin in a humidified atmosphere with 5%
CO2 at 37°C.
Chemicals and reagents
Recombinant mutant forms of human Gal-9 that lack
linker peptides were expressed and purified as described in one of
our previous studies (22). A cell
counting kit (CCK-8) was purchased from Dojindo Molecular
Technologies, Inc. (Kumamoto, Japan), and all other chemicals were
obtained from Sigma-Aldrich (Merck KGaA, Darmstadt, Germany).
Cell proliferation assay
A total of 5×103 cells were seeded in 100
µl of culture medium supplemented with 10% FBS into each well of a
96-well microplate and incubated at 37°C overnight. Following 24 h,
cells were treated with 0.1, 0.3 or 1.0 µM of Gal-9 and the cells
were cultured at 37°C for an additional 48 h. A total of 10 µl
CCK-8 reagent was added to each well and the plates were incubated
at 37°C for 3 h. The absorbance of each well was measured at 450 nm
using an auto-microplate reader.
ELISA assay for apoptosis
Caspase-cleaved keratin 18 (CCK18) was evaluated
using M30 Apoptosense ELISA kits obtained from PEVIVA AB (Bromma,
Sweden) (23). Each cell line (cell
density, 5×103 cells) was seeded into 96-well plates and
cultured in 100 µl of culture medium for 24 h. Cells were then
treated with 0.3 µM of Gal-9. The procedures of the assays were
performed according to the manufacturer's protocol. The amounts of
antigen in the control and treated samples were calculated by
interpolation of a standard curve.
Gel electrophoresis and western
blotting
PK-1 cells (1.0×106/dish) were seeded in
100-mm culture dishes and cultured at 37°C for 24 h. Gal-9 was
subsequently added, and the cells were cultured at 37°C for an
additional 48 h. Cells were washed twice in PBS and lysed using a
protease inhibitor cocktail (Proprep, Complete protease inhibitor
mixture; Intron Biotechnology, Inc., Seongnam, Korea). Protein
concentration was quantified using a NanoDrop 2000
fluorospectrometer (Thermo Fisher Scientific, Inc., Waltham, MA,
USA). Whole-cell lysates (10 µg) were separated using SDS-PAGE on
10% Tris-glycine gradient gels (24),
and the proteins were transferred to nitrocellulose membranes.
Subsequent to blocking with a solution containing 5% non-fat milk
powder in TBS/Tween-20 at 37°C for 1 h, the membranes were
incubated with primary antibodies at 4°C overnight and incubated
with horseradish peroxidase (HRP) -conjugated secondary antibodies
at 4°C for 1 h (25). The antibodies
used were: Anti-β-actin monoclonal antibody (dilution, 1:3,000;
cat. no. A5441; Sigma-Aldrich; Merck KGaA), cyclin D1 (dilution,
1:1,000; cat. no. RB-9041; Thermo Fisher Scientific Inc.), cyclin E
(dilution, 1:1,000; cat. no. 870P1605B; Thermo Fisher Scientific,
Inc.), Cdk (cyclin dependent kinase) 6 (dilution, 1:1,000; cat. no.
sc-177; Santa Cruz Biotechnology, Inc., Dallax, TX, USA), Cdk4
(dilution, 1:1,000; cat. no. sc-749; Santa Cruz Biotechnology,
Inc.), Cdk2 (dilution, 1:2,000; cat. no. sc-163; Santa Cruz
Biotechnology, Inc.) and secondary horseradish peroxidase-linked
anti-mouse (dilution, 1:2,000; cat no. 7076; Cell Signaling
Technology, Inc., Danvers, MA, USA) and anti-rabbit Immunoglobulin
G antibodies (dilution, 1:2,000; cat, no. 7074; Cell Signaling
Technology, Inc.).
Immunoreactive proteins were visualized using an
enhanced chemiluminescence detection system (Perkin Elmer Inc.,
Waltham, MA, USA) on X-ray film.
Antibody arrays of apoptosis-related
proteins
A Human Apoptosis Antibody Array kit (R&D
Systems, Inc., Minneapolis, MN, USA) was used according to the
manufacturer's protocol.
Antibody arrays of phosphorylated
receptor tyrosine kinase (p-RTK)
Human phospho-RTK was assayed using Human
Phospho-RTK Array kits (R&D Systems, Inc.), according to the
manufacturer's protocol. Each array membrane was exposed to X-ray
film using a chemiluminescence detection system (Perkin-Elmer
Co.).
Analysis of miRNA arrays
Total RNA was extracted from tumor samples using
miRNeasy Mini kits (Qiagen GmbH, Hilden, Germany) according to the
manufacturer's protocol. RNA samples typically demonstrated
A260/280 ratios between 1.9 and 2.1 when assayed
on an Agilent 2100 Bioanalyzer (Agilent Technologies, Inc., Santa
Clara, CA, USA). PK-1 cells were cultured at 37°C with or without
0.3 µM Gal-9 for 24 h, with 5 replicates per sample. Following RNA
measurement with an RNA 6000 Nano kit (Agilent Technologies, Inc.),
the samples were labeled using a miRCURY LNMä microRNA Array
Hi-Power Labeling kit (Exiqon A/S, Vedbaek, Denmark) and were
hybridized to a human miRNA Oligo chip (v.21.0; Toray Industries).
The chips were scanned with a 3-D Gene Scanner 3000 (Toray
Industries, Inc., Tokyo, Japan), and the results were analyzed with
3D-Gene extraction version 1.2 software (Toray Industries, Inc.,
Tokyo, Japan). Differences in miRNA expression between
Gal-9-treated and control samples were assessed by analyzing the
raw data using GeneSpringGX v. 10.0 (Agilent Technologies, Inc). On
the raw data that were above the background level, quantile
normalization was performed. Differentially expressed miRNAs were
determined using the Mann-Whitney U test. False discovery rate was
computed with Benjamini_Hochberg method (26) as the correction for multiple testing.
Hierarchical clustering was performed using the farthest neighbor
method with the absolute uncentered Pearson's correlation
coefficient as a metric. A heat map was produced with the relative
expression intensity for each miRNA, in which the base-2 logarithm
of the intensity was median-centered for each row.
Statistical analysis
All statistical analyses were performed using JMP
9.0 software (SAS Institute, Cary, NC, USA). Paired analysis
between groups was performed using t-tests. P<0.05 was
considered to indicate a statistically significant difference.
Results
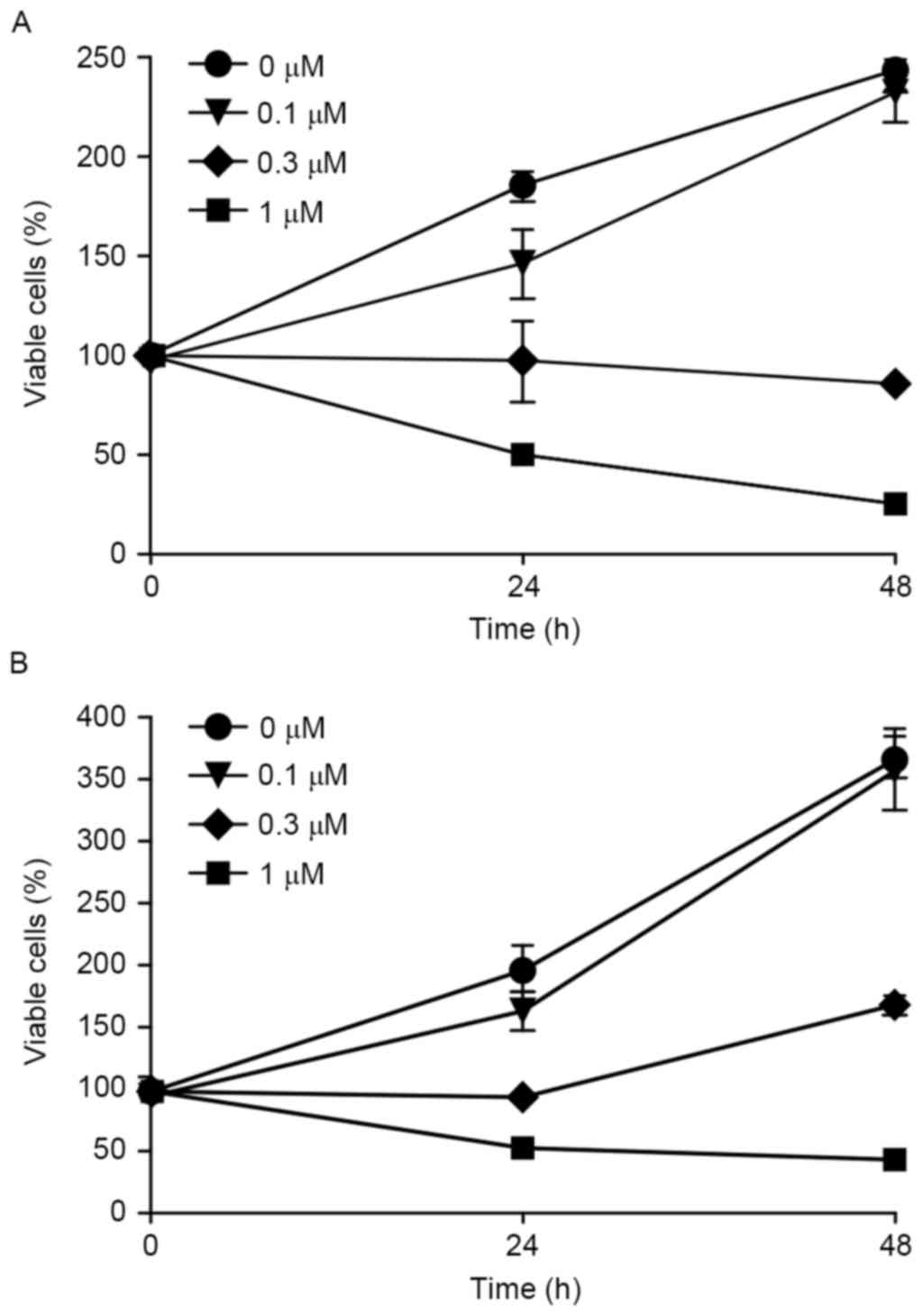
Gal-9 suppresses the proliferation of
human pancreatic cancer cells
To evaluate the effect of Gal-9 on the growth
activity of human pancreatic cells in vitro, the present
study examined the effect of Gal-9 on the proliferation of the
pancreatic cancer PK-1 and PK-9 cell lines. Cells were grown in 10%
FBS and treated with 0.1, 0.3 or 1.0 µM Gal-9 or without Gal-9 (as
a control) for 48 h. Gal-9 demonstrated strong, dose-dependent
inhibition of cellular proliferation the two pancreatic cancer cell
lines (Fig. 1).
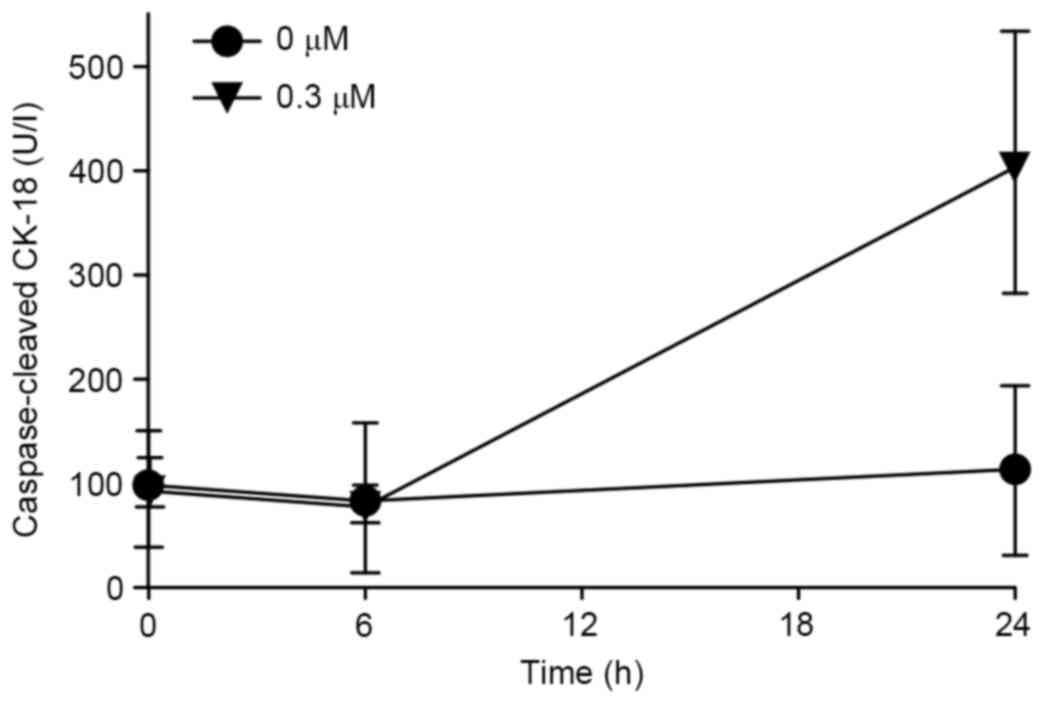
Gal-9 induces apoptosis to suppresses
cellular proliferation of pancreatic cancer
To clarify the mechanism of the inhibitory effect of
Gal-9 on cancer cell growth, the present study first examined the
induction of apoptosis by Gal-9. CCK18 was evaluated by ELISA to
confirm whether apoptosis was involved in Gal-9-induced cell death.
Gal-9 increased the levels of CCK18 in the two pancreatic cancer
cell lines (Fig. 2).
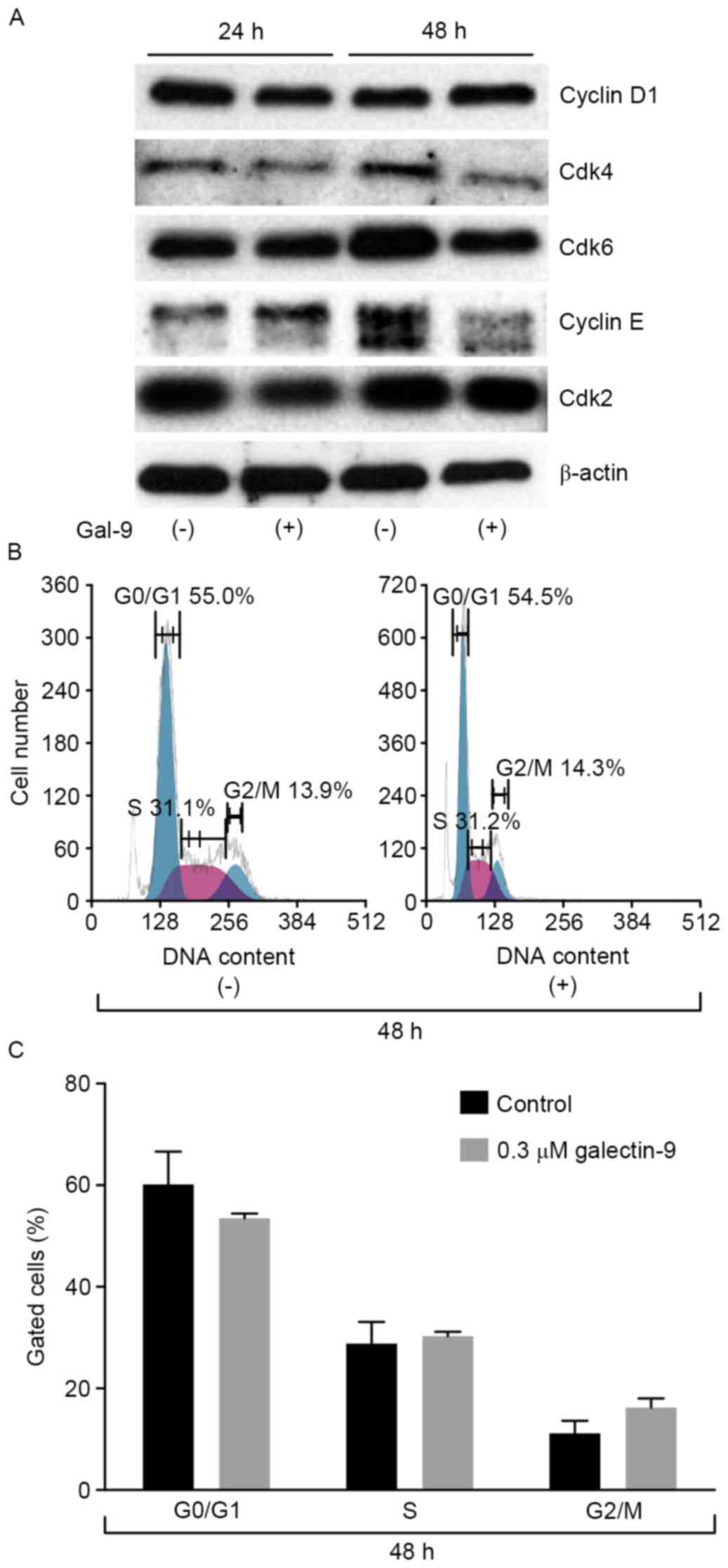
The effects of Gal-9 on the cell cycle
in PK-1
The effects of Gal-9 on the expression of various
cell-cycle-related molecules in PK-1 cells were evaluated using
western blot analysis. Cells were treated with 0 or 0.3 µM Gal-9
for 24–48 h. Assays for the expression of proteins associated with
the G0-to-G1 transition demonstrated that
cyclin E and Cdk4 were slightly decreased 48 h after the addition
of 0.3 µM of Gal-9 (Fig. 3A). The
expression of other proteins, including cyclin D1, Cdk2 and Cdk6
were not changed compared with the control.
Next, a flow cytometric analysis of the cell cycle
was performed to evaluate the contribution of Gal-9 to cell cycle
arrest during the suppression of pancreatic cancer cellular
proliferation. PK-1 cells were treated with 0.3 µM Gal-9. In
contrast to the expression levels of cyclin E and Cdk4, which
decreased, Gal-9 did not alter the cell cycle of PK-1 cells
(Fig. 3B and C). These results
suggest that Gal-9 suppresses cell growth through tumor cell
apoptosis but not through cell cycle arrest.
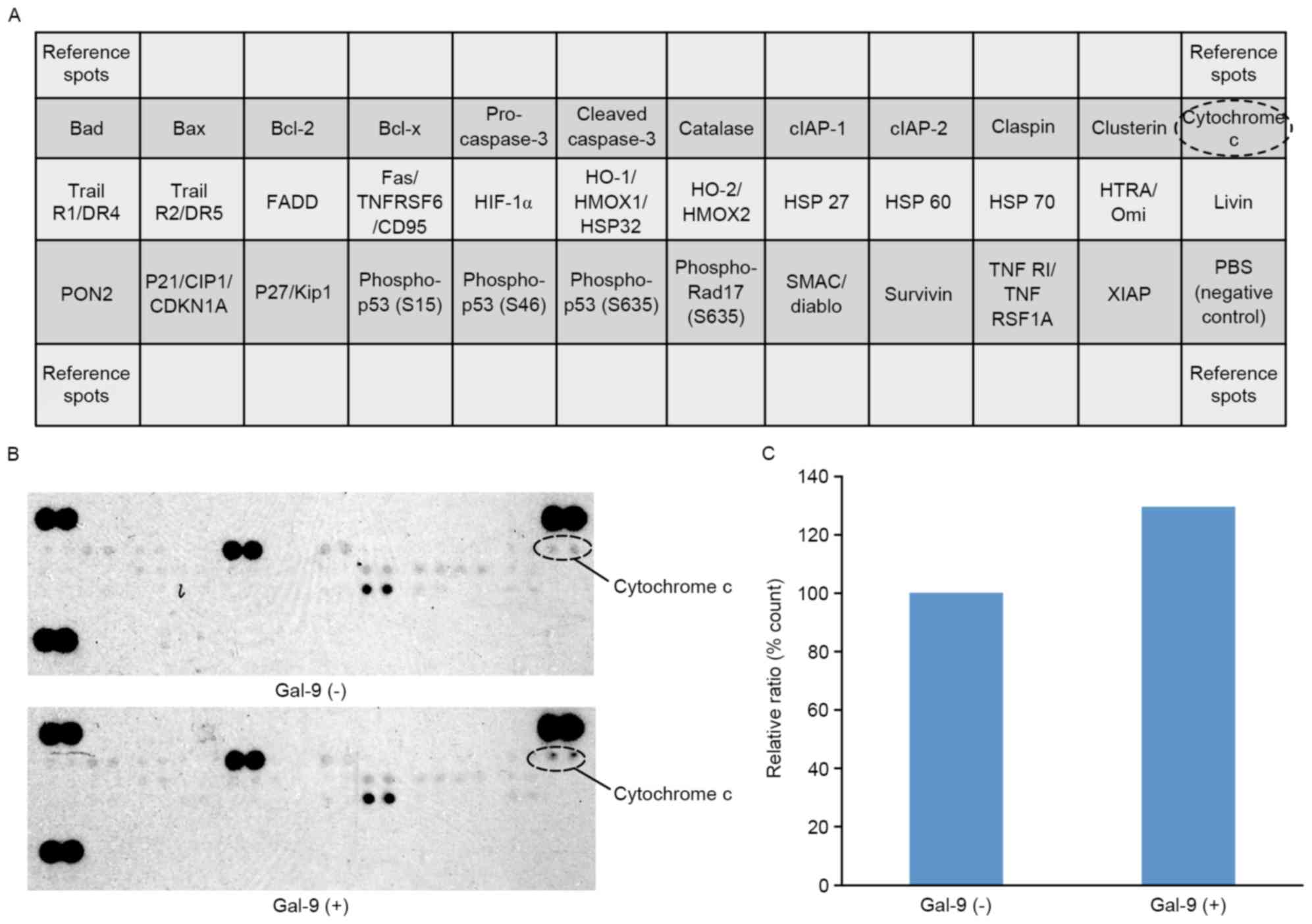
The effects of Gal-9 on
apoptosis-associated proteins in PK-1 cells
The present study used an apoptosis array system to
identify apoptosis proteins that were associated with the antitumor
effect of Gal-9. An antibody array enabled the screening of 35
apoptosis-associated proteins in PK-1 cells in the presence and
absence of Gal-9 (Fig. 4A). Gal-9
increased the expression levels of cytochrome c (Fig. 4B). Densitometry analysis demonstrated
that the intensity of cytochrome c spots from Gal-9-treated cells
relative to untreated cells was 129.7% (Fig. 4C).
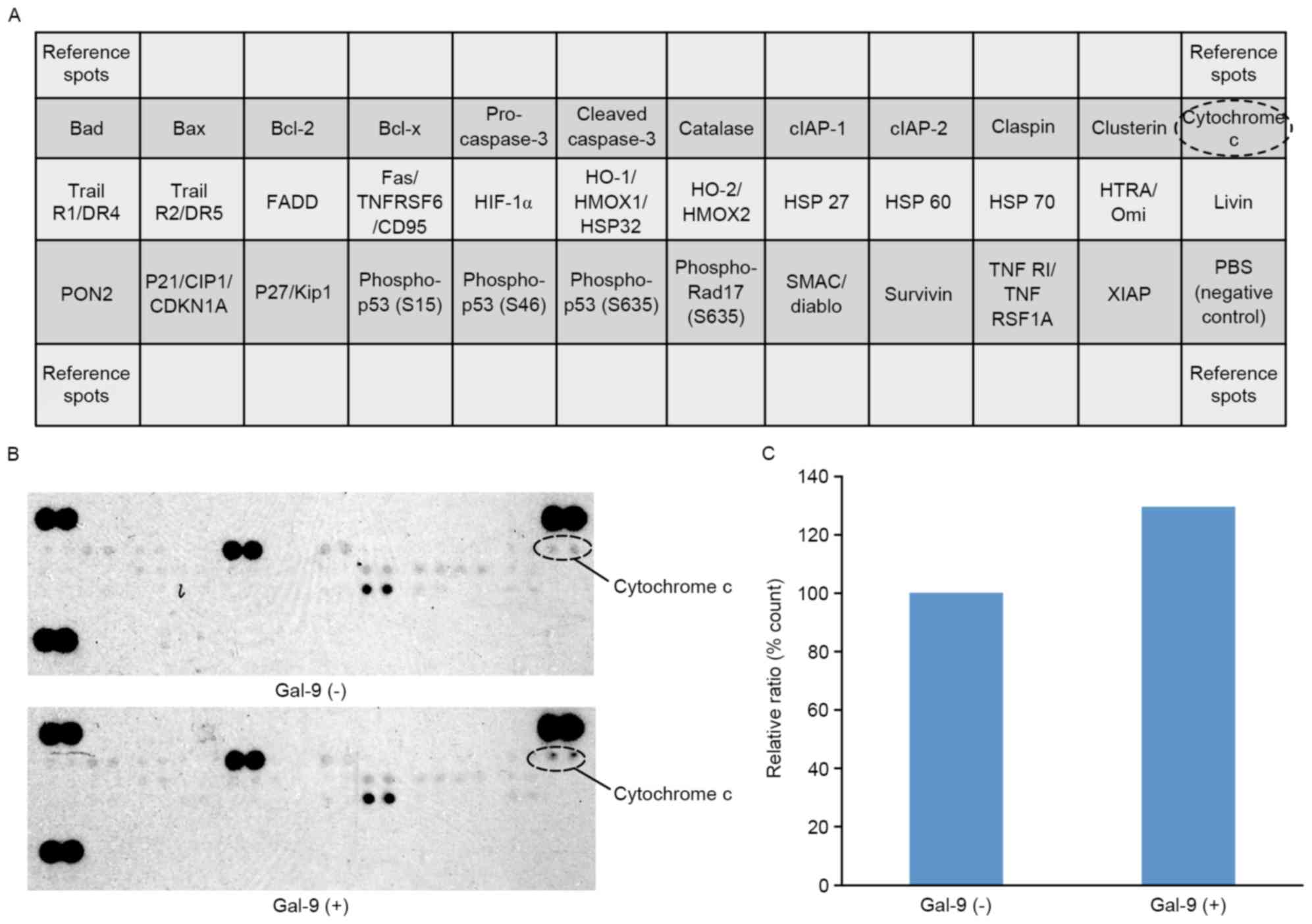 | Figure 4.The effects of Gal-9 on
apoptosis-related proteins in PK-1 cells. (A) Template showing the
locations of tyrosine kinase antibodies spotted onto a human
apoptosis array. (B) Representative expression of various
apoptosis-related proteins in PK-1 cells treated with or without
Gal-9. (C) Densitometry analysis demonstrated that the intensity of
cytochrome c spots from Gal-9-treated cells relative to untreated
cells was 129.7%. Gal-9, galectin-9; Bad, Bcl-2 associated death
promotor; Bax, Bcl-2 associated × protein; Bcl-2, B-cell lymphoma
2; Bcl-x, B cell lymphoma-extra-large; clAP, cellular inhibitor of
apoptosis protein; Trail R1/DR4, Trail receptor 1/death receptor 4;
FADD, Fas associated via death domain; TNFRSF6/CD95, tumor necrosis
factor receptor superfamily member 6/cluster of differentiation 95;
HIF-1α, hypoxia-inducible factor-1α; HO-1/HMOX1/HSP32, heme
oxygenase-1/heme oxygenase (decycling) 1/heat shock protein 32;
PON2, paraoxonase 2; P21/CIP1/CDKN1A, cyclin-dependent kinase
inhibitor 1A; SMAC, second mitochondria-derived activator of
caspases; TNF R1, tumor necrosis factor receptor 1; TNFRSF1A, TNF
receptor superfamily member 1A; XIAP, X-linked inhibitor of
apoptosis protein. |
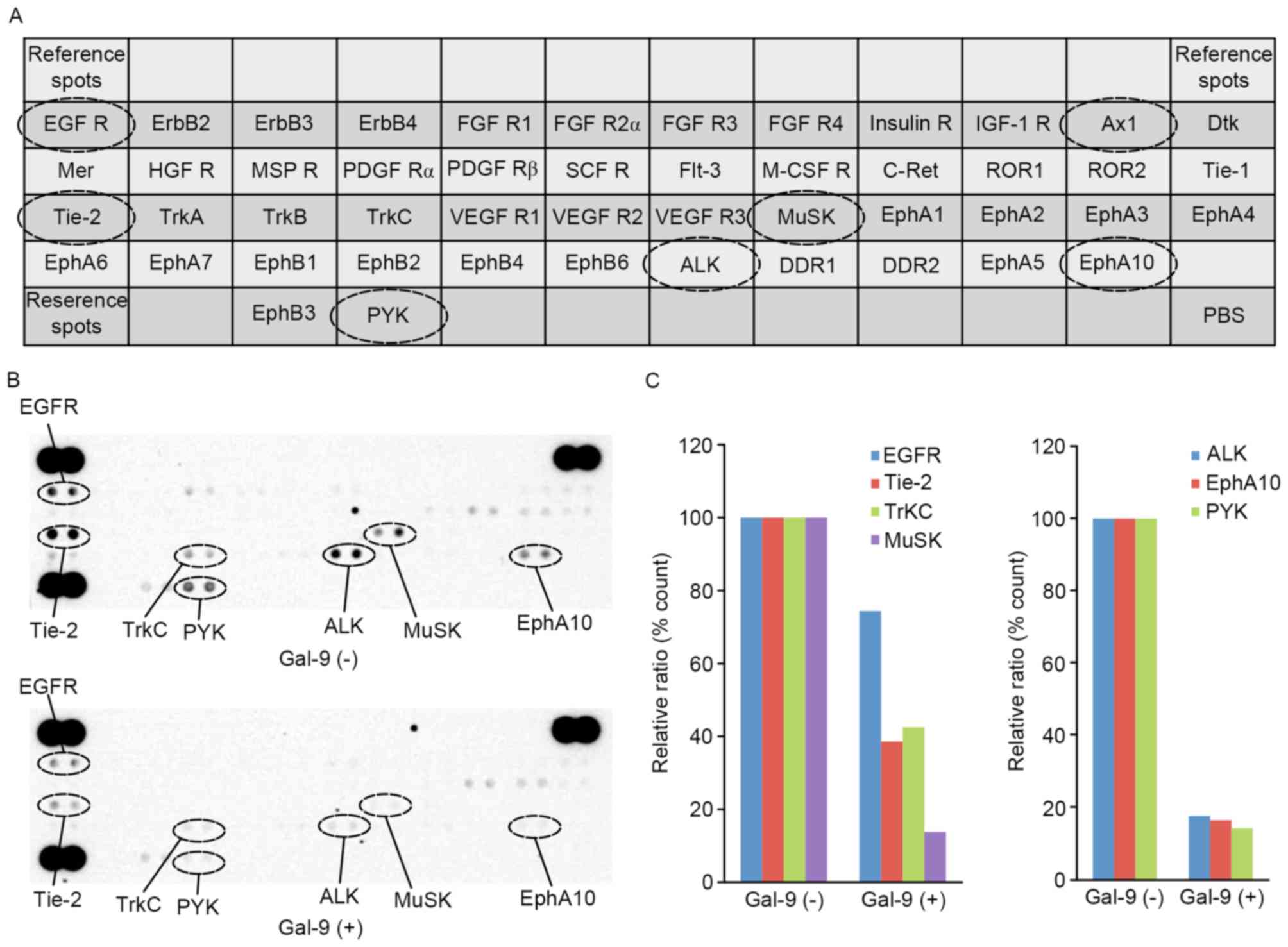
Effects of Gal-9 on p-RTKs in
PK-1
The present study used a p-RTK array system to
identify key RTKs that were associated with the antitumor effect of
Gal-9. An antibody array enabled the screening of 49 activated RTKs
in PK-1 cells in the presence and absence of Gal-9 (Fig. 5A). Gal-9 reduced the expression levels
of phosphorylated epidermal growth factor receptor (p-EGFR) and
phosphorylated tyrosine kinase with immunoglobulin-like and
EGF-like domains 2 (p-Tie-2), and it also reduced the expression of
tropomyosin receptor kinase C (TrKC), muscle-Specific Kinase
(MuSK), anaplastic lymphoma kinase (ALK), erythropoietin-producing
human hepatocellular carcinoma cell (EphA10) and receptor-like
tyrosine kinase (RYK) (Fig. 5B).
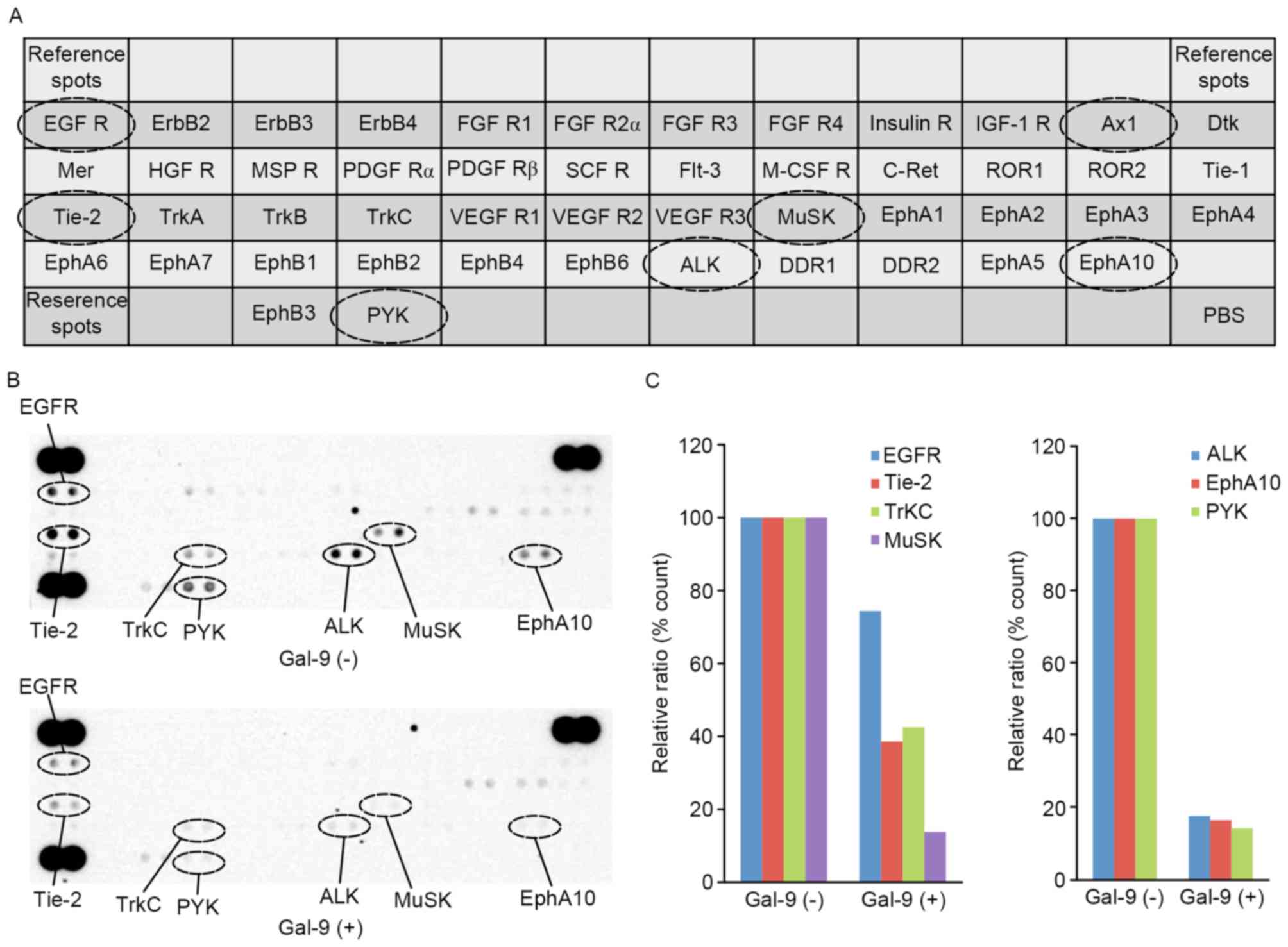 | Figure 5.The effects of Gal-9 on pRTKs in PK-1
cells. (A) Template showing the locations of tyrosine kinase
antibodies spotted onto a human pRTK array. (B) Representative
expression of various phosphorylated tyrosine kinase receptors in
PK-1 cells treated with or without Gal-9. (C) Densitometry analysis
demonstrated that the intensities of p-EGFR, p-Tie-2, p-TrKC,
p-MuSK, p-ALK, p-EphA10 and p-RYK spots from Gal-9-treated cells
relative to untreated cells were 74.4, 38.6, 42.5, 13.8, 17.7, 16.5
and 14.3%, respectively. Gal-9, galectin-9; pRTK, phospho-receptor
tyrosine kinase; p-EGFR, phosphor-epidermal growth factor; p-Tie-2,
phospho-tyrosine kinase with immunoglobulin-like and EGF-like
domains-2; p-TrKC, phospho-tropomyosin receptor kinase C; p-MuSK,
phospho-muscle-specific kinase; p-ALK, phospho-anaplasic tyrosine
kinase; p-EphA10, phospho-erythropoietin-producing human
hepatocellular receptors 10; p-RYK, phosphor-receptor-like tyrosine
kinase; ErbB2, human epidermal growth factor 2; FGF R1, fibroblast
growth factor receptor 1; IGF-1R, insulin-like growth factor 1
receptor; Ax1, tyrosine-protein kinase receptor UFO; Dtk, Dtk
receptor tyrosine kinase; Mer, Mer receptor tyrosine kinase; HGFR,
hepatocellular growth factor receptor; MSP R,
macrophage-stimulating protein receptor; PDGF Rα, platelet-derived
growth factor receptor α; SCF R, stem cell factor receptor; Flt-3,
Fms-like tyrosine kinase 3; M-CSF R, monocyte colony stimulating
factor; C-Ret, C-Te receptor tyrosine kinase; ROR1, receptor
tyrosine kinase-like orphan receptor 1; Tie-1, tyrosine kinase with
immunoglobulin-like and EGF-like domains-1; Trk, tropomyosin
receptor kinase; VEGF R1, vascular endothelial growth factor
receptor 1; Musk, muscle-specific kinase; EphA1,
erythropoietin-producing human hepatocellular receptor A1; ALK,
anaplasic tyrosine kinase; DDR1, discoidin domain receptor 1. |
Densitometry analysis demonstrated that the
intensities of p-EGFR, p-Tie-2, p-TrKC, p-MuSK, p-ALK, p-EphA10 and
p-RYK spots from Gal-9-treated cells relative to untreated cells
were 74.4, 38.6, 42.5, 13.8, 17.7, 16.5 and 14.3%, respectively
(Fig. 5C).
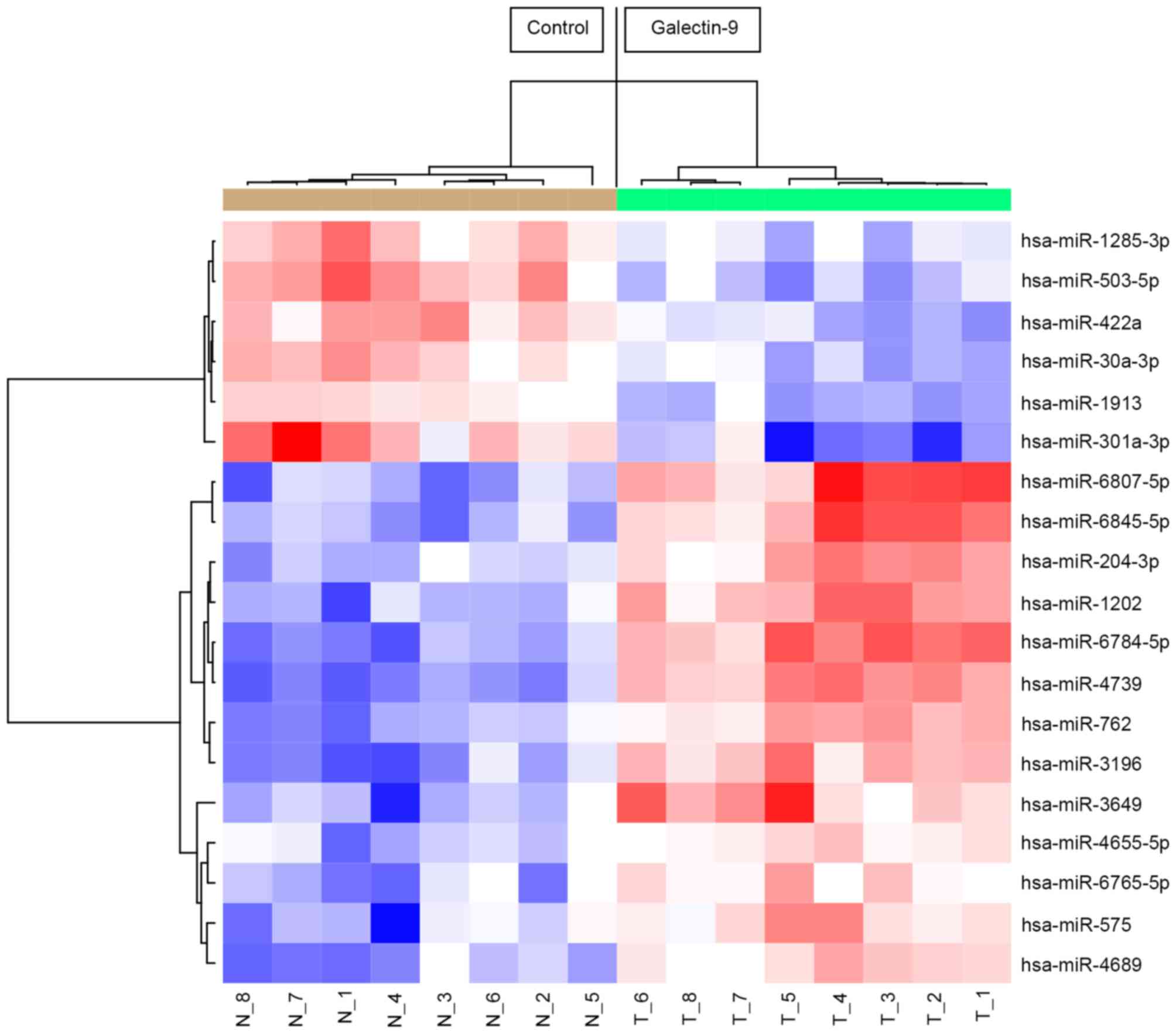
The effects of Gal-9 on the in vitro
miRNA expression of cells treated with and without Gal-9
Using a custom microarray platform, the present
study analyzed the in vitro expression levels of 2,555 miRNA
probes in tumorous tissues that were treated with and without
Gal-9. In PK-1 cells treated with Gal-9, there were 13 upregulated
and 6 downregulated miRNAs among the 2,555 miRNAs (Table I).
 | Table I.Statistical results and chromosomal
locations of miRNAs in PK-1 cells treated with and without
Gal-9. |
Table I.
Statistical results and chromosomal
locations of miRNAs in PK-1 cells treated with and without
Gal-9.
| miRNA | Fold-change
(treated/non-treated) | P-value | FDR | Chromosomal
localization |
|---|
| Upregulated |
|
hsa-miR-6807-5p | 2.27 | 0.00016 | 0.0045 | 19 |
|
hsa-miR-6784-5p | 2.25 | 0.00016 | 0.0045 | 17 |
|
hsa-miR-4739 | 2.18 | 0.00016 | 0.0045 | 17 |
|
hsa-miR-6845-5p | 2.04 | 0.00016 | 0.0045 | 8 |
|
hsa-miR-3196 | 1.91 | 0.00016 | 0.0045 | 20 |
|
hsa-miR-3649 | 1.88 | 0.00016 | 0.0045 | 12 |
|
hsa-miR-1202 | 1.88 | 0.00016 | 0.0045 | 6 |
|
hsa-miR-762 | 1.72 | 0.00016 | 0.0045 | 16 |
|
hsa-miR-204-3p | 1.67 | 0.00016 | 0.0045 | 9q21.12 |
|
hsa-miR-4689 | 1.63 | 0.00016 | 0.0045 | 1 |
|
hsa-miR-575 | 1.55 | 0.00031 | 0.0071 | 4q21.22 |
|
hsa-miR-6765-5p | 1.46 | 0.00031 | 0.0071 | 14 |
|
hsa-miR-4655-5p | 1.33 | 0.00016 | 0.0045 | 7 |
| Downregulated |
|
hsa-miR-301a-3p | 0.46 | 0.00031 | 0.0071 | 17q22 |
|
hsa-miR-503-5p | 0.56 | 0.00016 | 0.0045 | Xq26.3 |
|
hsa-miR-422a | 0.63 | 0.00016 | 0.0045 | 15q22.31 |
|
hsa-miR-30a-3p | 0.66 | 0.00031 | 0.0071 | 6q13 |
|
hsa-miR-1913 | 0.68 | 0.00016 | 0.0045 | 6 |
|
hsa-miR-1285-3p | 0.69 | 0.00016 | 0.0045 | 7q21-q22 |
Unsupervised hierarchical clustering analysis using
Pearson's correlation demonstrated that in vivo, tumorous
tissues treated with Gal-9 clustered together and separated from
untreated cell lines (Fig. 6).
Discussion
Pancreatic cancer has the worst 5-year survival rate
of all malignancies due to its aggressive progression and
resistance to therapy. Worldwide, the incidence of all types of
pancreatic cancer ranges between 1 and 10 cases per 100,000
individuals, and it is generally higher in developed countries and
among men (1). However, there is no
effective screening tool to detect asymptomatic premalignant or
early malignant tumors, and >90% of patients who receive a
diagnosis of pancreatic cancer die from the disease (27). Thus, there is strong demand for new
curative approaches to pancreatic cancer therapy.
The present data revealed that Gal-9 suppressed the
cellular proliferation and tumor growth of human pancreatic cancer
cell lines in vitro. The antitumor effect of Gal-9 in T cell
hemostasis, cell aggregation and metastasis is well known (14,15).
Previous findings suggest that Gal-9 inhibits the proliferation of
hematologic malignancies, including multiple myeloma (18) and chronic myeloid leukemia (19), and significantly retards the tumor
growth of myeloma xenografts in mice (18). Cell surface-associated Gal-9 triggered
the aggregation of melanoma cells, indicative of Gal-9-mediated
cellular adhesion and inhibition of cell detachment (28). In hematologic malignancies, Gal-9 may
suppress cellular proliferation and tumor growth in vitro
and in vivo. On the other hand, in solid malignancies,
breast cancer cell lines with high levels of endogenous Gal-9 had a
strong tendency to aggregate, whereas cells with low levels of
Gal-9 did not (29). Importantly,
ectopic expression of endogenous Gal-9 and treatment with
recombinant Gal-9 triggered the formation of tight cellular
clusters (28,29). Therefore, Gal-9 directly suppresses
cellular proliferation and tumor growth and has therapeutic
potential for several solid tumors.
Recombinant Gal-9 induces apoptosis and cell death
through an apoptotic signaling pathway (18,19). Such
apoptotic signaling was caspase-dependent and was induced by
activation of the mitogen activated protein kinases, c-Jun
N-terminal kinases and p38 in multiple myeloma cells (18). In addition, Gal-9 induced the
proapoptotic Bcl-2 family member Noxa via activation of
transcription factor 3, leading to the death of chromic myeloma
cells (19). Various hematological
malignancies are sensitive to apoptotic elimination by recombinant
Gal-9. Cleavage of cytokeratin 18 (CK18) occurs as an early event
during apoptosis following activation of apoptosis executioners,
particularly effector caspases (30).
However, CK18 remains intact during other types of cell death,
including autophagy or necrosis (30). Several studies have made use of this
phenomenon to detect cellular apoptosis at its early phase
(31–33). Our data suggested that Gal-9 increases
the levels of CCK18 in human pancreatic cancer cell lines.
Additionally, using an apoptosis array, the present study revealed
that the expression of cytochrome c was increased in Gal-9-treated
pancreatic cancer cell lines. Cytochrome c release from damaged
mitochondria is an early event in the intrinsic apoptosis pathway
and contributes to caspase-9 activation. The present data suggest
that Gal-9 may induce the apoptosis of pancreatic cancer cell lines
in the intrinsic apoptosis pathway through caspase-dependent and
caspase-independent pathways.
A previous study demonstrated that Gal-9 suppresses
cellular proliferation and tumor growth in hepatocellular carcinoma
and cholangiocarcinoma by inducing apoptosis but not cell cycle
arrest (20,21). Although the expression levels of
certain cell cycle-related proteins (Cdk4 and cyclin E) decreased
48 h after the addition of Gal-9, flow cytometry demonstrated that
Gal-9 did not affect PK-1 pancreatic cancer cells at the G0-to-G1
transition in vitro. These data suggest that the antitumor
effect of Gal-9 may not be associated with the reduction of various
cell cycle-related proteins.
Since the discovery of these proteins, RTKs have
been investigated as key regulators of the proliferation,
differentiation and metastasis of cancer cells (34). Gal-9 reduced the expression levels of
p-EGFR and phosphorylated Tie-2, TrKC, MuSK, ALK, EphA10 and RYK,
according to the pRTK array. The EGFR family and their ligands are
frequently overexpressed in pancreatic cancer (35), and EGFR activity correlates with the
prognosis of the patient (36).
The miRNAs that are associated with the antitumor
effects of Gal-9 were assessed using miRNA expression arrays.
miRNAs are small, endogenous, non-coding siRNAs that are 21–30
nucleotides in length and that modulate the expression of various
target genes at the post-transcriptional and translational levels
(37). miRNAs take part in
fundamental molecular processes associated with pancreatic cancer
initiation and progression, including the cell cycle, DNA repair,
apoptosis, invasion and metastasis (38). Cluster analyses clearly demonstrated
that Gal-9 treatment affected the extent of miRNA expression in
pancreatic cancer cell lines. The present study identified 19
miRNAs that were differentially expressed in the cluster. These
miRNAs are potential candidates to gauge the effectiveness of Gal-9
treatment, and provide clues regarding the molecular basis of the
anti-cancer effects of Gal-9, particularly those mediated by
miRNAs. Notably, miR301a was downregulated in a Gal-9-treated
pancreatic cancer cell line. The overexpression of miR-301a has
been previously demonstrated in pancreatic tumor tissue (39), hepatocellular carcinoma (40) and breast cancer (41). Additionally, miR-301a acts as a
nuclear factor-κB activator in pancreatic cancer (42) and promotes proliferation and invasion
in breast cancer. Thus, the present data suggest that miR-301a may
be a candidate target for new therapeutic approaches to pancreatic
cancer.
In conclusion, our results reveal that Gal-9
inhibits human pancreatic cancer cellular proliferation, possibly
by inducing apoptosis through cytochrome c release, which is
associated with the alteration of miRNAs. These findings suggest
that Gal-9 may be a new therapeutic agent for the treatment of
pancreatic cancer.
Acknowledgements
The authors would like to thank Ms. Kana Ogawa, Ms.
Kayo Endo, Ms. Fuyuko Kokado, Ms. Keiko Fujikawa and Ms. Noriko
Murao for providing technical assistance.
Glossary
Abbreviations
Abbreviations:
|
Gal-9
|
Galectin-9
|
|
CRDs
|
carbohydrate-recognition domains
|
|
CTLs
|
cytotoxic T cells
|
|
NK cells
|
natural killer cells
|
|
miRNAs
|
microRNAs
|
|
CCK-8
|
cell counting kit
|
|
CCK18
|
Caspase-cleaved keratin 18
|
|
phospho-RTK
|
phosphorylated receptor tyrosine
kinases
|
|
EGFR
|
epidermal growth factor receptor
|
|
CRDs
|
carbohydrate-recognition domains
|
|
Tie-2
|
tyrosine kinase with
immunoglobulin-like and EGF-like domains 2
|
|
TrKC
|
tropomyosin receptor kinase C
|
|
MuSK
|
muscle-Specific Kinase
|
|
ALK
|
anaplastic lymphoma kinase
|
|
Eph
|
erythropoietin-producing human
hepatocellular carcinoma cell
|
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Stathis A and Moore MJ: Advanced
pancreatic carcinoma: Current treatment and future challenges. Nat
Rev Clin Oncol. 7:163–172. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schneider G, Siveke JT, Eckel F and Schmid
RM: Pancreatic cancer: Basic and clinical aspects.
Gastroenterology. 128:1606–1625. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gudjonsson B: Pancreatic cancer: Survival,
errors and evidence. Eur J Gastroenterol Hepatol. 21:1379–1382.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wray CJ, Ahmad SA, Matthews JB and Lowy
AM: Surgery for pancreatic cancer: Recent controversies and current
practice. Gastroenterology. 128:1626–1641. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Loos M, Kleeff J, Friess H and Büchler MW:
Surgical treatment of pancreatic cancer. Ann NY Acad Sci.
1138:169–180. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Matsumoto R, Matsumoto H, Seki M, Hata M,
Asano Y, Kanegasaki S, Stevens RL and Hirashima M: Human ecalectin,
a variant of human galectin-9, is a novel eosinophil
chemoattractant produced by T lymphocytes. J Biol Chem.
273:16976–16984. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Matsushita N, Nishi N, Seki M, Matsumoto
R, Kuwabara I, Liu FT, Hata Y, Nakamura T and Hirashima M:
Requirement of divalent galactoside-binding activity of
ecalectin/galectin-9 for eosinophil chemoattraction. J Biol Chem.
275:8355–8360. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Matsumoto R, Hirashima M, Kita H and
Gleich GJ: Biological activities of ecalectin: A novel
eosinophil-activating factor. J Immunol. 168:1961–1967. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Saita N, Goto E, Yamamoto T, Cho I,
Tsumori K, Kohrogi H, Maruo K, Ono T, Takeya M, Kashio Y, et al:
Association of galectin-9 with eosinophil apoptosis. Int Arch
Allergy Immunol. 128:42–50. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Asakura H, Kashio Y, Nakamura K, Seki M,
Dai S, Shirato Y, Abedin MJ, Yoshida N, Nishi N, Imaizumi T, et al:
Selective eosinophil adhesion to fibroblast via IFN-gamma-induced
galectin-9. J Immunol. 169:5912–5918. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dai S, Nakagawa R, Itoh A, Murakami H,
Kashio Y, Abe H, Katoh S, Kontani K, Kihara M, Zhang SL, et al:
Galectin-9 induces maturation of human monocyte-derived dendritic
cells. J Immunol. 175:2974–2981. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nobumoto A, Oomizu S, Arikawa T, Katoh S,
Nagahara K, Miyake M, Nishi N, Takeshita K, Niki T, Yamauchi A and
Hirashima M: Galectin-9 expands unique macrophages exhibiting
plasmacytoid dendritic cell-like phenotypes that activate NK cells
in tumor-bearing mice. Clin Immunol. 130:322–330. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wiersma VR, de Bruyn M, Helfrich W and
Bremer E: Therapeutic potential of Galectin-9 in human disease. Med
Res Rev. 33 Suppl 1:E102–E126. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fujihara S, Mori H, Kobara H, Rafiq K,
Niki T, Hirashima M and Masaki T: Galectin-9 in cancer therapy.
Recent Pat Endocr Metab Immune Drug Discov. 7:130–137. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kashio Y, Nakamura K, Abedin MJ, Seki M,
Nishi N, Yoshida N, Nakamura T and Hirashima M: Galectin-9 induces
apoptosis through the calcium-calpain-caspase-1 pathway. J Immunol.
170:3631–3636. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lu LH, Nakagawa R, Kashio Y, Ito A, Shoji
H, Nishi N, Hirashima M, Yamauchi A and Nakamura T:
Characterization of galectin-9-induced death of Jurkat T cells. J
Biochem. 141:157–172. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kobayashi T, Kuroda J, Ashihara E, Oomizu
S, Terui Y, Taniyama A, Adachi S, Takagi T, Yamamoto M, Sasaki N,
et al: Galectin-9 exhibits anti-myeloma activity through JNK and
p38 MAP kinase pathways. Leukemia. 24:843–850. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kuroda J, Yamamoto M, Nagoshi H, Kobayashi
T, Sasaki N, Shimura Y, Horiike S, Kimura S, Yamauchi A, Hirashima
M and Taniwaki M: Targeting activating transcription factor 3 by
Galectin-9 induces apoptosis and overcomes various types of
treatment resistance in chronic myelogenous leukemia. Mol Cancer
Res. 8:994–1001. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Fujita K, Iwama H, Sakamoto T, Okura R,
Kobayashi K, Takano J, Katsura A, Tatsuta M, Maeda E, Mimura S, et
al: Galectin-9 suppresses the growth of hepatocellular carcinoma
via apoptosis in vitro and in vivo. Int J Oncol. 46:2419–2430.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kobayashi K, Morishita A, Iwama H, Fujita
K, Okura R, Fujihara S, Yamashita T, Fujimori T, Kato K, Kamada H,
et al: Galectin-9 suppresses cholangiocarcinoma cell proliferation
by inducing apoptosis but not cell cycle arrest. Oncol Rep.
34:1761–1770. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nishi N, Itoh A, Fujiyama A, Yoshida N,
Araya S, Hirashima M, Shoji H and Nakamura T: Development of highly
stable galectins: Truncation of the linker peptide confers
protease-resistance on tandem-repeat type galectins. FEBS Lett.
579:2058–2064. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Schutte B, Henfling M, Kölgen W, Bouman M,
Meex S, Leers MP, Nap M, Björklund V, Björklund P, Björklund B, et
al: Keratin 8/18 breakdown and reorganization during apoptosis. Exp
Cell Res. 297:11–26. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Laemmli UK: Cleavage of structural
proteins during the assembly of the head of bacteriophage T4.
Nature. 227:680–685. 1970. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Towbin H, Staehelin T and Gordon J:
Electrophoretic transfer of proteins from polyacrylamide gels to
nitrocellulose sheets: Procedure and some applications. Proc Natl
Acad Sci USA. 76:pp. 4350–4354. 1979; View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Benjamini Y and Hochberg Y: Controlling
the false discovery rate: A practical and powerful approach to
multiple testing. J Roval Statis Soc. 57:289–300. 1995.
|
|
27
|
Ryan DP, Hong TS and Bardeesy N:
Pancreatic adenocarcinoma. N Engl J Med. 371:1039–1049. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kageshita T, Kashio Y, Yamauchi A, Seki M,
Abedin MJ, Nishi N, Shoji H, Nakamura T, Ono T and Hirashima M:
Possible role of galectin-9 in cell aggregation and apoptosis of
human melanoma cell lines and its clinical significance. Int J
Cancer. 99:809–816. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Irie A, Yamauchi A, Kontani K, Kihara M,
Liu D, Shirato Y, Seki M, Nishi N, Nakamura T, Yokomise H and
Hirashima M: Galectin-9 as a prognostic factor with antimetastatic
potential in breast cancer. Clin Cancer Res. 11:2962–2968. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kramer G, Erdal H, Mertens HJ, Nap M,
Mauermann J, Steiner G, Marberger M, Bivén K, Shoshan MC and Linder
S: Differentiation between cell death modes using measurements of
different soluble forms of extracellular cytokeratin 18. Cancer
Res. 64:1751–1756. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Linder S: Cytokeratin markers come of age.
Tumour Biol. 28:189–195. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Cummings J, Ranson M, Butt F, Moore D and
Dive C: Qualification of M30 and M65 ELISAs as surrogate biomarkers
of cell death: Long term antigen stability in cancer patient
plasma. Cancer Chemother Pharmacol. 60:921–924. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Scott LC, Evans TR, Cassidy J, Harden S,
Paul J, Ullah R, O'Brien V and Brown R: Cytokeratin 18 in plasma of
patients with gastrointestinal adenocarcinoma as a biomarker of
tumour response. Br J Cancer. 101:410–417. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Morishita A, Gong J and Masaki T:
Targeting receptor tyrosine kinases in gastric cancer. World J
Gastroenterol. 20:4536–4545. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Cohenuram M and Saif MW: Epidermal growth
factor receptor inhibition strategies in pancreatic cancer: Past,
present and the future. JOP. 8:4–15. 2007.PubMed/NCBI
|
|
36
|
Ueda S, Ogata S, Tsuda H, Kawarabayashi N,
Kimura M, Sugiura Y, Tamai S, Matsubara O, Hatsuse K and Mochizuki
H: The correlation between cytoplasmic overexpression of epidermal
growth factor receptor and tumor aggressiveness: Poor prognosis in
patients with pancreatic ductal adenocarcinoma. Pancreas. 29:e1–e8.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Morishita A and Masaki T: miRNA in
hepatocellular carcinoma. Hepatol Res. 45:128–141. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Marin-Muller C, Li D, Bharadwaj U, Li M,
Chen C, Hodges SE, Fisher WE, Mo Q, Hung MC and Yao Q: A
tumorigenic factor Interactome connected through tumor suppressor
MicroRNA-198 in human pancreatic cancer. Clin Cancer Res.
19:5901–5913. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Lee EJ, Gusev Y, Jiang J, Nuovo GJ, Lerner
MR, Frankel WL, Morgan DL, Postier RG, Brackett DJ and Schmittgen
TD: Expression profiling identifies microRNA signature in
pancreatic cancer. Int J Cancer. 120:1046–1054. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Jiang J, Gusev Y, Aderca I, Mettler TA,
Nagorney DM, Brackett DJ, Roberts LR and Schmittgen TD: Association
of MicroRNA expression in hepatocellular carcinomas with hepatitis
infection, cirrhosis, and patient survival. Clin Cancer Res.
14:419–427. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Shi W, Gerster K, Alajez NM, Tsang J,
Waldron L, Pintilie M, Hui AB, Sykes J, P'ng C, Miller N, et al:
MicroRNA-301 mediates proliferation and invasion in human breast
cancer. Cancer Res. 71:2926–2937. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Lu Z and Li Y, Takwi A, Li B, Zhang J,
Conklin DJ, Young KH, Martin R and Li Y: miR-301a as an NF-κB
activator in pancreatic cancer cells. EMBO J. 30:57–67. 2011.
View Article : Google Scholar : PubMed/NCBI
|