Introduction
Spinal tumors are relatively rare in clinical
practice (1–3). However, due to the complex anatomical
structure of the spine and the spinal cord, as well as large
vessels and vital organs around the spine, the risk of surgical
resection is relatively high. Therefore, subtotal resection has
become the major treatment options for spinal tumors. However, the
recurrence rate of subtotal resection is high, which in turn
reduces the treatment efficacy (4–7).
Over the past 20 years, with the development of
microsurgical technology, materials science, ergonomics and
computer technology, understanding of surgeons in regard to spinal
tumors has improved, and the treatment efficacy of spinal tumors
has also significantly increased (8,9). Through
retrospective studies of surgical approach, resection methods,
intraoperative bleeding control and spinal stability
reconstruction, the resection rate was found to be significantly
increased. By contrast, the complication, mortality and local
recurrence rates were significantly reduced (8–12).
The risk factors of recurrent spinal tumors and the
corresponding clinical treatment strategies involved have yet to be
reported. Therefore, the aim of the study was to investigate the
correlations between these risk factors.
Materials and methods
Subjects
Inclusion criteriafor the study were: Patients
received spinal cancer surgery more than 12 months before, quality
of life scale score was ≥70 points, patients received surgery or
biopsy, patients and their families voluntarily participated in the
study and signed informed consent, and patients with normal
function of major organs who showed no chemotherapy
contraindications. Exclusion criteria for the study were: Patients
combined with severe brain, heart, liver, renal and blood system
diseases, as well as pregnant and lactating women.
In total, 125 patients with spine tumors including
77 males and 48 females were selected from January, 2010 to
December, 2015. The ages ranged from 14 to 75 years with a median
age of 41 years. There were 32 cases of cervical spine tumors, 5
cases of cervical thoracic spinal tumors, 31 cases of thoracic
spine tumors, 34 cases of lumbosacral spine tumors, and 23 cases of
thoracolumbar sacral spine tumors. Ependymoma was found in 42
cases, astrocytoma in 30 cases, hemangioblastoma in 14 cases,
cavernous hemangioma in 7 cases, hamartoma in 6 cases, lipoma in 6
cases, dermoid cyst in 5 cases, metastatic tumor in 4 cases,
ganglion glioma in 4 cases, neuroma in 4 cases, and meningioma in 3
cases. None of the patients had any history of radiation
therapy.
Surgical methods
All 125 patients with spinal tumor were treated by
microsurgical resection of spinal tumor. Limb movement, body
surface sensation and anal sphincter function were monitored by the
intraoperative application of neural electrophysiological
equipment. The patients only underwent treatment with a high dose
of methylprednisolone combined with neurotrophic drug therapy.
Patients with limb movement disorders were treated with acupuncture
and rehabilitation training 1 week after operation. All the
patients were reviewed by nuclear magnetic resonance imaging to
check possible recurrence. The McCormick grading system was used to
evaluate the postoperative spinal cord function. Patients with
increased McCormick (1 grade or more) were treated as patients with
improvement, while patients with decreased McCormick (1 grade or
more) were treated as patients with deterioration.
Statistical analysis
Data were processed by SPSS 20.0 statistical
software (IBM, Armonk, NY, USA). Measurement data were expressed as
mean ± standard deviation, t-test was performed for comparisons
between groups, and data that did not fit the normal distribution
were processed using U test. Countable data were expressed as %,
comparisons between groups were performed using χ2, and
the on-recurrence survival rate was calculated by Kaplan-Meier
method. Multivariate analysis was performed by Logistic multiple
regression analysis. P<0.05 was considered to indicate a
statistically significant difference.
Results
Treatment efficacy
Of the 77 male patients, the proportion of patients
with thoracic and lumbosacral tumors was the largest, reaching
27.3% (21/77), followed by cervical, lumbosacral, thoracic and
cervicothoracic. Of the 48 female patients, the proportion of
patients with lumbosacral tumors was the largest, reaching 33.3%
(16/48), followed by the thoracic, cervical, thoracolumbar sacral
and cervicothoracic tumors (Table I).
Sixty-three cases showed improvement after operation, 50 cases were
stable, and deterioration was found in 12 cases. The improvement
rate of patients with cervical spine tumor, which reached 56.3%,
was the highest, followed by thoracic, lumbosacral, thoracic and
lumbosacral and cervicothoracic tumors (Table II). Postoperative symptoms included:
52 cases of sensory disturbance, 34 cases of pain, 30 cases of
inability to exercise, 26 cases of ataxia and 12 cases of sphincter
disorders (Table III).
 | Table I.Distribution of sex and tumor location
of 125 patients with spinal tumors [cases (%)]. |
Table I.
Distribution of sex and tumor location
of 125 patients with spinal tumors [cases (%)].
| Tumor locations | n | Male | Female |
|---|
| Cervical | 32 | 19 (24.7) | 13 (27.1) |
| Cervicothoracic | 5 | 3 (3.9) | 2 (4.2) |
| Thoracic | 31 | 16 (20.8) | 15 (31.3) |
| Lumbosacral | 34 | 18 (23.4) | 16 (33.3) |
| Thoracic and
lumbosacral | 23 | 21 (27.3) | 2 (4.2) |
| Total | 125 | 77 (100.0) | 48 (100.0) |
 | Table II.Correlation between tumor locations
and treatment outcomes in 125 patients [cases (%)]. |
Table II.
Correlation between tumor locations
and treatment outcomes in 125 patients [cases (%)].
| Tumor locations | n | Improvement | Stable | Deterioration |
|---|
| Cervical | 32 | 18 (56.3) | 11 (34.3) | 3 (9.4) |
| Cervicothoracic | 5 | 2
(40.0) | 2
(40.0) | 1 (20.0) |
| Thoracic | 31 | 16 (51.6) | 13 (41.9) | 2 (6.5) |
| Lumbosacral | 34 | 16 (47.1) | 14 (41.2) | 4 (11.7) |
| Thoracic and
lumbosacral | 23 | 11 (47.8) | 10 (43.5) | 2 (8.7) |
| Total | 125 | 63 (50.4) | 50 (40.0) | 12 (9.6) |
 | Table III.Correlation between tumor locations
and postoperative complications in 125 patients [cases (%)]. |
Table III.
Correlation between tumor locations
and postoperative complications in 125 patients [cases (%)].
| Tumor locations | n | Sensory
disturbance | Pain | Inability to
exercise | Ataxia | Aphincter
disorders |
|---|
| Cervical | 32 | 13 (40.6) | 7
(21.9) | 7
(21.9) | 6
(18.8) | 2 (6.3) |
| Cervicothoracic | 5 | 2
(40.0) | 1
(20.0) | 2
(40.0) | 1
(20.0) | 0 (0.0) |
| Thoracic | 31 | 12 (38.7) | 8
(25.8) | 7
(22.6) | 6
(19.4) | 4 (12.9) |
| Lumbosacral | 34 | 13 (38.2) | 10 (29.4) | 8
(23.5) | 8
(23.5) | 3 (8.8) |
| Thoracic and
lumbosacral | 23 | 12 (52.2) | 8
(34.8) | 6
(26.1) | 5
(21.7) | 3 (13.0) |
| Total | 125 | 52 (41.6) | 34 (27.2) | 30 (24.0) | 26 (20.8) | 12 (9.6) |
Correlation between tumor type and
surgical resection
With microsurgical resection, there were 72 cases
(57.6%) of total resection, 18 cases (14.4%) of subtotal resection,
23 cases (18.4%) of partial resection and 12 cases (9.6%) of
biopsy/decompression due to the existing of multiple lesions. Total
resection rate of neuroma was 100.0% (4/4), followed by
hematoblastoma 92.9% (13/14), cavernous hemangioma 85.7% (6/7),
ependymoma 83.3% (35/42), ganglion glioma 75.0% (3/4), meningioma
66.7% (2/3), dermoid cysts 40.0% (2/5), metastatic tumor 25.0%
(1/4), hamartoma 16.7% (1/6) and astrocytoma 16.7% (5/30) (Table IV).
 | Table IV.Correlation between pathological tumor
types and surgical resection [cases (%)]. |
Table IV.
Correlation between pathological tumor
types and surgical resection [cases (%)].
| Pathological
types | Total resection | Subtotal
resection | Partial
resection |
Biopsy/decompression | Total |
|---|
| Ependymoma | 35 (83.3) | 3 (7.1) | 2 (4.8) | 2 (4.8) | 42 |
| Astrocytoma | 5 (16.7) | 8 (26.7) | 14 (46.7) | 3 (10.0) | 30 |
| Hemangioblastoma | 13 (92.9) | 1 (7.1) | 0 (0.0) | 0 (0.0) | 14 |
| Cavernous
hemangioma | 6 (85.7) | 1 (14.3) | 0 (0.0) | 0 (0.0) | 7 |
| Hamartoma | 1 (16.7) | 1 (16.7) | 2 (33.3) | 2 (33.3) | 6 |
| Lipoma | 0 (0.0) | 0 (0.0) | 3 (50.0) | 3 (50.0) | 6 |
| Dermoid cysts | 2 (40.0) | 1 (20.0) | 1 (20.0) | 1 (20.0) | 5 |
| Metastatic tumor | 1 (25.0) | 1 (25.0) | 1 (25.0) | 1 (25.0) | 4 |
| Ganglion
glioma | 3 (75.0) | 1 (25.0) | 0 (0.0) | 0 (0.0) | 4 |
| Neuroma | 4 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 4 |
| Meningioma | 2 (66.7) | 1 (33.3) | 0 (0.0) | 0 (0.0) | 3 |
| Total | 72 (57.6) | 18 (14.4) | 23 (18.4) | 12 (9.6) | 125 |
Tumor recurrence
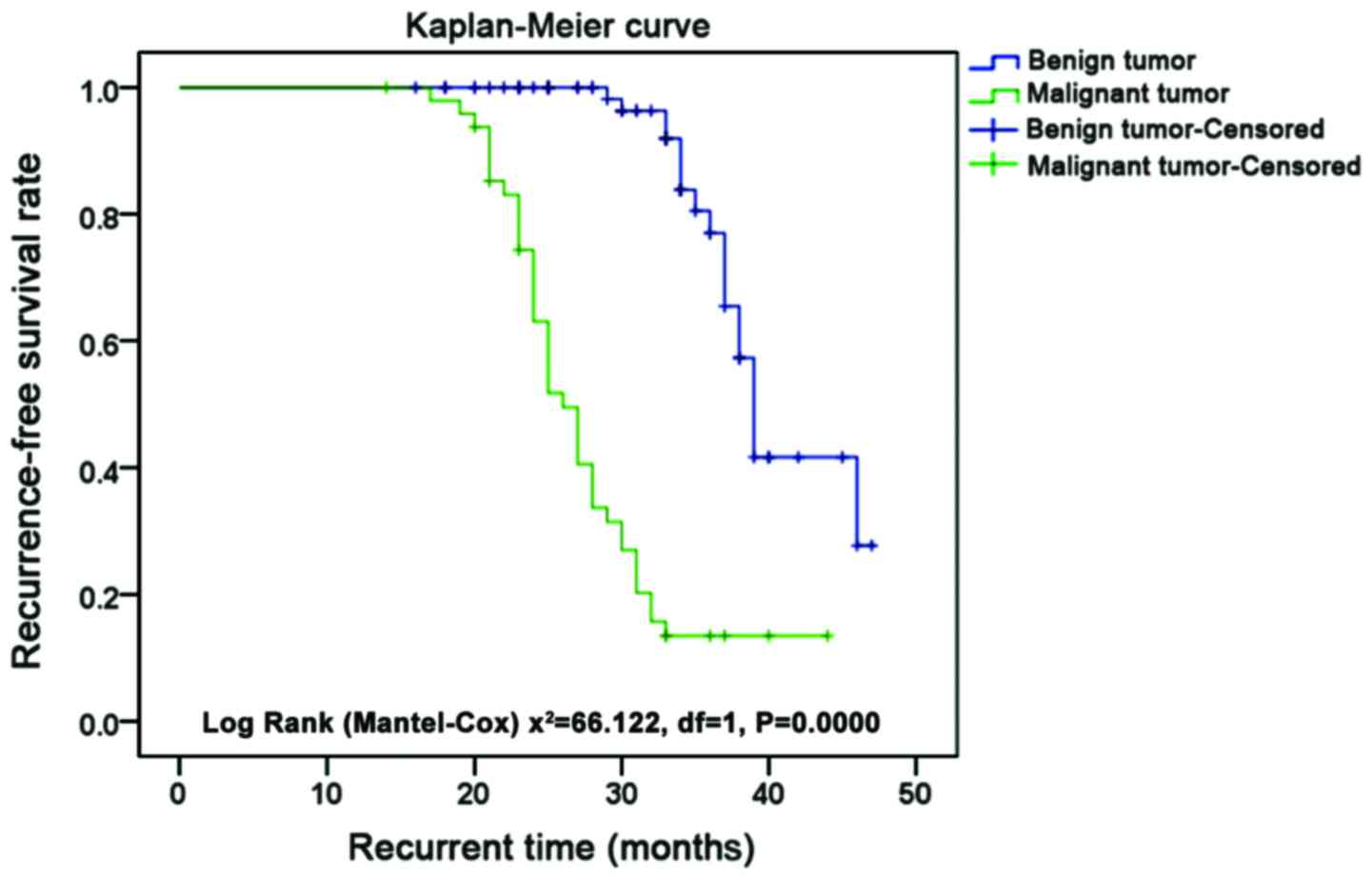
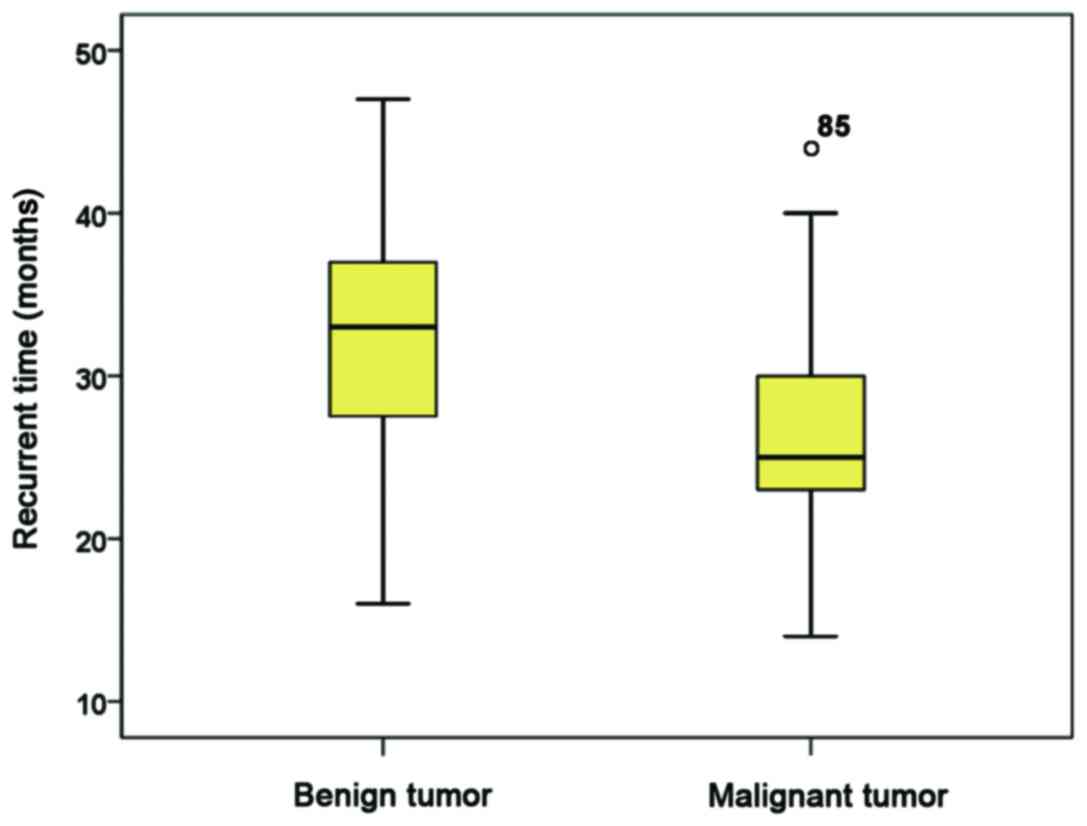
Of the 125 patients with spinal tumors, 57 (45.6%)
had tumor recurrence at different time points after surgery. The
mean recurrence time of 49 patients with malignant tumor was
27.49±6.09 months, while the recurrence time of 76 patients with
benign tumor was 40.62±4.34 months. Recurrence-free survival rate
of patients with benign tumor was significantly higher than that of
patients with malignant tumor (P<0.001). The recurrence-free
survival time of patients with malignant tumor was significantly
shorter than that of patients with benign tumor (P<0.001)
(Figs. 1 and 2). Thirty-six males and 21 females showed
recurrence, and no significant difference was found between sexes
(P=0.142). Recurrence was found in 18 cases of benign tumors
(23.7%) and 39 cases of malignant tumor (79.6%), and the results
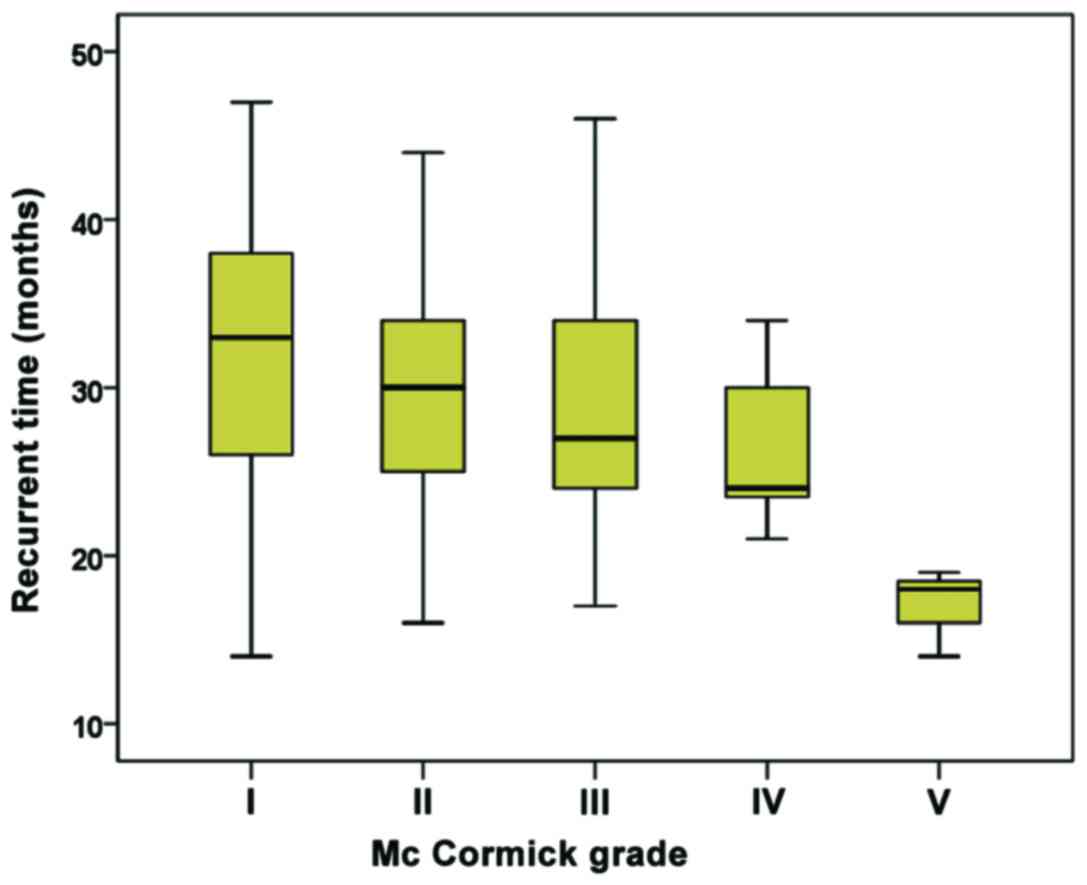
were significantly different (P<0.001). Among the patients with
recurrence, 17 cases had a McCormick grade of I or II (21.8%), 30
cases had a grade of III (81.1%), and 10 cases had a grade of VI
and V (100%), and the results showed significant differences
(P<0.001). Patients with higher McCormick grade showed a
significantly higher recurrence rate (P<0.001) (Fig. 3). Recurrence was found in 13 cases of
72 patients who received total resection and all patients receiving
partial resection and biopsy/decompression, significant difference
was found between them (P<0.001). Recurrence was found in 3
cases (42.9%) of patients below 25 years, 43 cases (45.3%) of
patients between 25 and 60 years, and 11 cases (47.8%) of patients
above 60 years, with the results showing no significant differences
were. No significant difference in recurrence time was found
between different age groups (Fig.
4). The comparisons of recurrence rate between patients with
different pathological tumor types are listed in Table V.
 | Table V.Comparisons of recurrence rate
between patients with different pathological backgrounds
(n=125). |
Table V.
Comparisons of recurrence rate
between patients with different pathological backgrounds
(n=125).
| Items | n | Recurrence | Non-recurrence | χ2
value | P-value |
|---|
| Sex |
|
|
| 0.113 | 0.142 |
|
Male | 77 | 36 (46.8) | 41 (53.2) |
|
|
|
Female | 48 | 21 (43.8) | 27 (56.3) |
|
|
| Age (years) |
|
|
| 0.069 | 0.241 |
|
<25 | 7 | 3 (42.9) | 4 (57.1) |
|
|
|
25–60 | 95 | 43 (45.3) | 52 (54.7) |
|
|
|
>60 | 23 | 11 (47.8) | 12 (52.2) |
|
|
| Tumor
properties |
|
|
| 37.543 | 0.000 |
|
Benign | 76 | 18 (23.7) | 58 (76.3) |
|
|
|
Malignant | 49 | 39 (79.6) | 10 (20.4) |
|
|
| Tumor
positions |
|
|
| 4.662 | 0.073 |
|
Cervical | 32 | 16 (50.0) | 16 (50.0) |
|
|
|
Cervicothoracic | 5 | 4 (80.0) | 1 (20.0) |
|
|
|
Thoracic | 31 | 13 (41.9) | 18 (58.1) |
|
|
|
Lumbosacral | 34 | 12 (35.3) | 22 (64.7) |
|
|
|
Thoracic and lumbosacral | 23 | 12 (52.2) | 11 (47.8) |
|
|
| McCormick
grades |
|
|
| 48.531 | 0.000 |
| I and
II | 78 | 17 (21.8) | 61 (78.2) |
|
|
|
III | 37 | 30 (81.1) | 7 (18.9) |
|
|
| IV and
V | 10 | 10 (100.0) | 0 (0.0) |
|
|
| Resection |
|
|
| 63.924 | 0.000 |
| Total
resection | 72 | 13 (18.1) | 59 (81.9) |
|
|
|
Subtotal resection | 18 | 9 (50.0) | 9 (50.0) |
|
|
| Partial
resection | 23 | 23 (100.0) | 0 (0.0) |
|
|
|
Biopsy/decompression | 12 | 12 (100.0) | 0 (0.0) |
|
|
Logistic regression analysis of total
surgical resection-related factors
Logistic regression analysis of total surgical
resection-related factors was carried out. Significant differences
in degree of resection were found between patients with different
tumor properties (Wald Chi-square value=32.429, potence ratio:
10.386, P<0.05), indicating that the total resection was
preferred for patients with benign tumors. Significant differences
in the degree of resection were found between patients with
different tumor positions (Wald Chi-square value=9.453, potence
ratio: 0.550, P<0.05), indicating that the total resection was
preferred for patients with thoracic and lumbosacral tumors.
Significant differences in the degree of resection were also found
between patients with different McCormick grades (Wald Chi-square
value=30.571, potence ratio: 7.442, P<0.05), indicating that the
total resection was preferred for patients with lower McCormick
grades. Significant differences in the degree of resection were
aslo found between patients with or without syringomyelia (Wald
Chi-square value= 9.781, potence ratio: 0.962, P<0.05),
indicating the total resection is preferred for patients without
syringomyelia. Significant differences in the degree of resection
were also found between patients with or without intramedullary
tumors (Wald Chi-square value=11.199, potence ratio: 1.167,
P<0.05), indicating that total resection was preferred for
patients without intramedullary tumors (Table VI).
 | Table VI.Logistic regression analysis of total
surgical resection-related factors. |
Table VI.
Logistic regression analysis of total
surgical resection-related factors.
|
|
|
|
|
|
|
| 95% confidence
interval |
|---|
|
|
|
|
|
|
|
|
|
|---|
| Variable | Coefficient | Standard
deviation | Wald Chi-square
value | Degree of
freedom | P-value | Potence ratio | Lower limit | Upper limit |
|---|
| Sex | 0.401 | 0.898 | 0.321 | 1 | 0.624 | 1.546 | 0.664 | 2.406 |
| Age | 0.32 | 0.677 | 0.312 | 1 | 0.841 | 0.998 | 0.435 | 2.458 |
| Tumor
properties | 2.663 | 0.66 | 32.429 | 1 | 0.027 | 10.386 | 4.674 | 24.764 |
| Tumor position | −0.275 | 0.348 | 9.453 | 1 | 0.009 | 0.550 | 0.456 | 0.711 |
| McCormick
grades | 2.33 | 0.613 | 30.571 | 1 | 0.007 | 7.442 | 3.672 | 16.184 |
| With or without
syringomyelia | 0.036 | 0.397 | 9.781 | 1 | 0.021 | 0.962 | 0.938 | 2.564 |
| With or without
intramedullary tumors | 1.167 | 0.58 | 11.199 | 1 | 0.011 | 1.167 | 0.707 | 2.184 |
Logistic regression analysis of risk
factors of spinal tumor recurrence
Logistic regression analysis of risk factors of
spinal tumor recurrence was carried out. Significant differences in
the tumor recurrence rate were found between patients with
different tumor properties (Wald Chi-square value=32.283, potence
ratio: 12.567, P<0.05), indicating that the tumor recurrence
rate was higher in patients with malignant tumors than that of
patients with malignant tumors. Significant differences in tumor
recurrence rate were found between patients with different tumor
positions (Wald Chi-square value=9.307, potence ratio: 0.665,
P<0.05), indicating that tumor recurrence rate was higher in
patients with cervical and thoracic and lumbosacral tumors than in
patient with other tumor positions. Significant differences in the
tumor recurrence rate were also found between patients with
different McCormick grades (Wald Chi-square value=30.425, potence
ratio: 9.005, P<0.05), suggesting that the tumor recurrence rate
was higher in patients with higher McCormick grades than in
patients with lower McCormick grades. Significant differences in
the tumor recurrence rate were found between patients with or
without total resection (Wald Chi-square value=9.634, potence
ratio: 1.164, P<0.05), indicating that the recurrence rate was
higher in patients with partial resection or biopsy/decompression
than in patients with total resection. In addition, significant
differences in the tumor recurrence rate were also found between
patients with or without intramedullary tumors (Wald Chi-square
value=11.053, potence ratio: 1.412, P<0.05), suggesting that the
recurrence rate was higher in patients with intramedullary tumors
than in patients without intramedullary tumors (Table VII).
 | Table VII.Logistic regression analysis of
recurrence-related factors. |
Table VII.
Logistic regression analysis of
recurrence-related factors.
|
|
|
|
|
|
|
| 95% confidence
interval |
|---|
|
|
|
|
|
|
|
|
|
|---|
| Variable | Coefficient | Standard
deviation | Wald χ2
value | Degree of
freedom | P-value | Potence ratio | Lower limit | Upper limit |
|---|
| Sex | 0.269 | 0.683 | 0.175 | 1 | 0.467 |
1.871 | 0.746 |
2.923 |
| Age | 0.188 | 0.462 | 0.166 | 1 | 0.684 |
1.207 | 0.488 |
2.987 |
| Tumor
properties | 2.531 | 0.445 | 32.283 | 1 | 0.000 | 12.567 | 5.249 | 30.088 |
| Tumor position | −0.407 | 0.133 | 9.307 | 1 | 0.002 |
0.665 | 0.512 |
0.864 |
| McCormick
grades | 2.198 | 0.398 | 30.425 | 1 | 0.000 |
9.005 | 4.124 | 19.663 |
| With or without
total resection | −0.096 | 0.182 | 9.634 | 1 | 0.024 |
1.164 | 1.053 |
3.115 |
| With or without
intramedullary tumors | 1.035 | 0.365 | 11.053 | 1 | 0.014 |
1.412 | 0.794 |
2.654 |
Discussion
The incidence rate of spinal tumors is approximately
6.6% to 8.8% (13), which is a low
level. However, spinal tumors have many pathological types and also
lack characteristic clinical manifestations at the early stage.
Thus, the treatment of spinal tumors is usually delayed, which in
turn affects prognosis (14,15). In recent years, with the advancement
of medical imaging technology, the early diagnosis of spinal tumors
has become possible. Combined with advances in microsurgical
techniques, robotic techniques and biomedical materials, the
surgical treatment of spinal tumors has been significantly improved
and the treatment efficacy significantly increased (16,17).
Therefore, how to further improve the efficacy of surgical
treatment, improve the long-term control rate of cancer, design a
reasonable treatment plan, and reduce surgical complications has
become a hot research field.
The majority of primary spinal tumors are malignant
tumors. However, the majority of surgical studies are usually
focused on the treatment of benign tumors, which may be explained
by the loss of surgical opportunities of malignant tumors and the
radioactive treatment-dominated treatment strategy. Surgical
treatment is the main treatment of spinal tumors, but the risk is
high and the incidence of postoperative complication is also high.
In addition, surgical operations may injure important blood vessels
and nerves, resulting in spinal cord ischemia or injury and the
postoperative recurrence of tumor (18). A retrospective study carried by
Klekamp (19) found that the total
resection rate of spinal tumors has been significantly improved in
the last 30 years. Approximately 61% of patients with spinal tumors
had neurological dysfunction after surgery, of which 41.5% were
reversible. The incidence of permanent neurological deficit is
approximately 19.5%, which is closely related to the experience of
surgeons and the state of the preoperative nervous system. Further
analysis revealed that patients with thoracic tumors, tumor
bleeding, malignancy and recurrent tumors usually had a higher risk
of permanent complications (19).
The cause of spinal tumor recurrence is complex
(20,21). Pathological grade of the tumor has a
significant effect on the recurrence rate of tumors and the
survival status of patients. Except for some of cases of
astrocytomas, recurrence is common in all malignant spinal tumors.
Therefore, radiation therapy is preferred for patients with
malignant spinal tumors (21). For
invasive spondyloma tumors, total tumor resection or subtotal
resection can effectively reduce the tumor recurrence rate. Effects
of the degree of tumor resection on the recurrence rate of
ependymoma have been very clear. Some studies have reported no
significant correlation between tumor resection and
progression-free survival in patients with astrocytomas, which may
be explained by the small sample size (22).
In this study, recurrence was found in 57 cases of
spinal tumors (45.6%) after surgery. The recurrence time was
shorter in patients with malignant tumors, and the recurrence rate
was also higher than that of benign tumors. Patients with higher
McCormick grades showed shorter recurrence time. This can be
explained by the factor that tumors with higher McCormick grades
are usually malignant tumors with a high invasion ability, causing
difficulties to total resection and subtotal resection. Logistic
regression analysis of total resection showed that total resection
should be the preferred treatment for patients with benign tumors,
thoracic and lumbosacral tumors and lower McCormick grades, as well
as patients without syringomyelia and intramedullary tumors.
Logistic regression analysis of recurrence-related factors showed
that the recurrence rate was higher in patients with malignant
tumors, cervical and thoracic and lumbosacral tumors, higher
McCormick grades and intramedullary tumors, and patients receiving
partial resection or biopsy/decompression treatment.
In summary, tumor properties, tumor locations,
McCormick grades, degrees of tumor resection and intramedullary
tumors are risk factors for the postoperative recurrence of spinal
tumors. Clinical assessment of these risk factors may be helpful in
selecting appropriate treatment strategies.
References
|
1
|
Hariri O, Takayanagi A, Miulli DE, Siddiqi
J and Vrionis F: Minimally invasive surgical techniques for
management of painful metastatic and primary spinal tumors. Cureus.
9:e11142017.PubMed/NCBI
|
|
2
|
Dea N, Gokaslan Z, Choi D and Fisher C:
Spine oncology-primary spine tumors. Neurosurgery. 80:S124–S130.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mechtler LL and Nandigam K: Spinal cord
tumors: New views and future directions. Neurol Clin. 31:241–268.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kato S, Murakami H, Demura S, Yoshioka K,
Kawahara N, Tomita K and Tsuchiya H: More than 10-year follow-up
after total en bloc spondylectomy for spinal tumors. Ann Surg
Oncol. 21:1330–1336. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tokuhashi Y, Uei H, Oshima M and Ajiro Y:
Scoring system for prediction of metastatic spine tumor prognosis.
World J Orthop. 5:262–271. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shi R, Wang PY, Li XY, Chen JX, Li Y,
Zhang XZ, Zhang CG, Jiang T, Li WB, Ding W, et al: Exosomal levels
of miRNA-21 from cerebrospinal fluids associated with poor
prognosis and tumor recurrence of glioma patients. Oncotarget.
6:26971–26981. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sun SQ, Cai C, Ravindra VM, Gamble P,
Yarbrough CK, Dacey RG, Dowling JL, Zipfel GJ, Wright NM, Santiago
P, et al: Simpson grade I–III resection of spinal atypical (World
Health Organization Grade II) meningiomas is associated with
symptom resolution and low recurrence. Neurosurgery. 76:739–746.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Karikari IO, Nimjee SM, Hodges TR, Cutrell
E, Hughes BD, Powers CJ, Mehta AI, Hardin C, Bagley CA, Isaacs RE,
et al: Impact of tumor histology on resectability and neurological
outcome in primary intramedullary spinal cord tumors: A
single-center experience with 102 patients. Neurosurgery. 76 Suppl
1:S4–S13. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Varga PP, Szövérfi Z, Fisher CG, Boriani
S, Gokaslan ZL, Dekutoski MB, Chou D, Quraishi NA, Reynolds JJ,
Luzzati A, et al: Surgical treatment of sacral chordoma: Prognostic
variables for local recurrence and overall survival. Eur Spine J.
24:1092–1101. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tang C, Hess K, Bishop AJ, Pan HY,
Christensen EN, Yang JN, Tannir N, Amini B, Tatsui C, Rhines L, et
al: Creation of a prognostic index for spine metastasis to stratify
survival in patients treated with spinal stereotactic radiosurgery:
Secondary analysis of mature prospective trials. Int J Radiat Oncol
Biol Phys. 93:118–125. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bishop AJ, Tao R, Rebueno NC, Christensen
EN, Allen PK, Wang XA, Amini B, Tannir NM, Tatsui CE, Rhines LD, et
al: Outcomes for spine stereotactic body radiation therapy and an
analysis of predictors of local recurrence. Int J Radiat Oncol Biol
Phys. 92:1016–1026. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Matamalas A, Gargallo A, Porcel JA, García
de Frutos A and Pellisé F: Cervical spine epithelioid
hemangioendothelioma: Case report. Eur Rev Med Pharmacol Sci. 18
Suppl 1:72–75. 2014.PubMed/NCBI
|
|
13
|
Vera-Bolanos E, Aldape K, Yuan Y, Wu J,
Wani K, Necesito-Reyes MJ, Colman H, Dhall G, Lieberman FS,
Metellus P, et al CERN Foundation, : Clinical course and
progression-free survival of adult intracranial and spinal
ependymoma patients. Neuro Oncol. 17:440–447. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Goldschlager T, Dea N, Boyd M, Reynolds J,
Patel S, Rhines LD, Mendel E, Pacheco M, Ramos E, Mattei TA, et al:
Giant cell tumors of the spine: Has denosumab changed the treatment
paradigm? J Neurosurg Spine. 22:526–533. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jahangiri A, Chin AT, Wagner JR, Kunwar S,
Ames C, Chou D, Barani I, Parsa AT, McDermott MW, Benet A, et al:
Factors predicting recurrence after resection of clival chordoma
using variable surgical approaches and radiation modalities.
Neurosurgery. 76:179–186. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Xu W, Li X, Huang W, Wang Y, Han S, Chen
S, Xu L, Yang X, Liu T and Xiao J: Factors affecting prognosis of
patients with giant cell tumors of the mobile spine: Retrospective
analysis of 102 patients in a single center. Ann Surg Oncol.
20:804–810. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Huang L, Chen K, Ye JC, Tang Y, Yang R,
Wang P and Shen HY: Modified total en bloc spondylectomy for
thoracolumbar spinal tumors via a single posterior approach. Eur
Spine J. 22:556–564. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ahmed R, Menezes AH, Awe OO and Torner JC:
Long-term disease and neurological outcomes in patients with
pediatric intramedullary spinal cord tumors. J Neurosurg Pediatr.
13:600–612. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Klekamp J: Treatment of intramedullary
tumors: Analysis of surgical morbidity and long-term results. J
Neurosurg Spine. 19:12–26. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Prejbeanu RI, Daliborca C Vlad, Dumitrascu
V, Vermesan D, Mioc M, Abbinante A and Cagiano R: Application of
acrylic spacers for long bone defects after tumoral resections. Eur
Rev Med Pharmacol Sci. 17:2366–2371. 2013.PubMed/NCBI
|
|
21
|
Oh MC, Kim JM, Kaur G, Safaee M, Sun MZ,
Singh A, Aranda D, Molinaro AM and Parsa AT: Prognosis by tumor
location in adults with spinal ependymomas. J Neurosurg Spine.
18:226–235. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nair S, Gobin YP, Leng LZ, Marcus JD,
Bilsky M, Laufer I and Patsalides A: Preoperative embolization of
hypervascular thoracic, lumbar, and sacral spinal column tumors:
Technique and outcomes from a single center. Interv Neuroradiol.
19:377–385. 2013. View Article : Google Scholar : PubMed/NCBI
|