Introduction
Carcinoma of the thyroid gland is the most common
malignant tumor of the endocrine system (1). Papillary thyroid cancer (PTC) is the
most common histological type of thyroid cancer, representing 80%
of all cases of thyroid cancer and 85% of cases of differentiated
thyroid cancer (2,3). PTC is 2.9–3.8 times more common in women
than in men (4), and is more common
in regions associated with a high dietary intake of iodine
(5). In the United States, the
incidence of PTC is 1.56–3.58/100,000 men and 4.9–10.96/100,000
women (4). PTC is usually associated
with a more positive prognosis than follicular thyroid cancer;
however, certain subtypes are more aggressive than others (5). Of the PTC subtypes, the tall-cell
variant (TCV) is among the most aggressive (6). The 2004 World Health Organization (WHO)
classification defined TCV as PTC containing ≥50% tall cells
(7). Other characteristics of TCV
include an eosinophilic tall cell cytoplasm and nuclear features
characteristic of PTC (7). However,
the molecular mechanisms that cause TCV differentiation are
unclear.
In recent years, B-raf proto-oncogene (BRAF)
mutation has been demonstrated to be the most common genetic
alteration in PTC (8). It is a
molecular marker associated with aggressive tumor behaviors,
including size, extra-thyroidal extension, multifocality, lymph
node metastasis, tumor recurrence and advanced disease stage
(9,10).
The rat sarcoma viral oncogene homolog (RAS)
genes, which include the isoforms HRAS, KRAS and
NRAS, are crucial effectors in a number of signaling
cascades. The mitogen activated protein kinase (MAPK) and the
phosphatidylinositol 3-kinase (PI3K) pathways, which mediate cell
differentiation, proliferation, and survival, are affected by
RAS genes (11,12). RAS activity is regulated by
GTP-bound hydrolysis, and any mutation that results in the
dysregulation of this hydrolysis results in aberrant MAPK and
PI3K/(RAC serine/threonine-protein kinase (Akt) signaling, which
are critical events in thyroid carcinogenesis (13).
HRAS is one of the most commonly mutated
genes in PTC, particularly in variants identified in follicular
(14–17) and Hurthle cells (18), reflecting its key regulatory
functions. The contribution made by HRAS to PTC progression
is poorly understood. Therefore, the present study aimed to
investigate the presence of somatic variants in HRAS
exhibited by patients with PTC as well as by healthy individuals,
and to investigate their association with PTC development. The
results of the present study provide an improved understanding of
PTC pathogenesis and may provide novel insight for the advancement
of PTC treatment.
Materials and methods
Study design and subjects
The present study involves the retrospective
investigation of tumor samples collected from patients with PTC who
underwent thyroidectomy at the Beijing Friendship Hospital, Capital
Medical University (Beijing, China) between January 2011 and
February 2016. A total of 139 PTC patients (106 females and 33
males), age (48.7±9.3) years old. The final diagnoses were made by
pathological examination of the specimens. The following inclusion
criteria were applied: i) No treatment for PTC prior to the
surgery; ii) the absence of any other type of malignant tumor; iii)
tumor size >0.5 cm; iv) no distant metastasis identified prior
to surgery; v) clear results from lymph node dissection; and vi)
sufficient DNA extractable from the tissue for analysis.
A total of 195 blood samples from asymptotic people
undergoing routine health examinations were acquired as healthy
controls. The following exclusion criteria were applied: i) Any
symptom of thyroid cancer, and ii) the identification of any
biochemical abnormality.
The present study was approved by the Clinical
Research Ethics Committee of Beijing Friendship Hospital, Capital
Medical University.
Pathological evaluation
Following surgery, formalin-fixed paraffin-embedded
(FFPE) tumor-rich tissue areas were dissected from unstained 4-µm
sections under the guidance of stained slides which was stained by
undiluted hematoxylin and eosin (Merck KGaA, Darmstadt, Germany)
for 330 sec at room temperature, with the tumor area marked under
the guidance of light microscope (original magnification ×200). All
histological slides were reviewed independently by experienced
pathologists specialized in thyroid pathology (from the Peking
University Third Hospital, Beijing, China). Diagnoses were
performed according to the WHO classification (7). The tumors were classified into
histological subtypes: Classic variant of papillary thyroid
carcinoma (CVPTC), follicular variant of papillary thyroid
carcinoma (FVPTC), and TCV.
DNA extraction
Tumor-rich areas were scraped from the paraffin
sections, added to 500 µl xylene (concentration ≥99.0%; Sinopharm
Chemical Reagent Co., Ltd., Shanghai, China), and centrifuged
27,400 × g at room temperature for 15 min. The supernatant was
discarded and 500 µl of anhydrous ethanol was used to disperse the
pellet prior to centrifugation twice more 27,400 × g at room
temperature for 10 min. The supernatant was discarded and 50 µl
acetone was used to disperse the pellet prior to further
centrifugation 27,400 × g at room temperature for 5 min. Subsequent
to air drying, the pellet was suspended in 309 µl DNA extraction
buffer (300 µl digestion buffer and 9 µl proteinase K;
E.Z.N.A® FFPE DNA Kit; Omega Bio-Tek, Inc., Rockville,
MD, USA), and incubated at 55°C for 3–5 h. The DNA was extracted
from the 195 control samples using Blood DNA kits (Tiangen Biotech
Co., Ltd., Beijing, China), according to the manufacturer's
instructions. The DNA concentration was determined by
spectrophotometric absorption (A) at 230, 260, and 280 nm, and the
DNA quality was evaluated by calculating the ratio of optical
density (OD) value at 260 and 280 nm or 260 and 230 nm measured by
a BioSpec-nano spectrophotometer (Shimadzu Corporation, Kyoto,
Japan).
Single-stranded conformational
polymorphism analysis (SSCP) and direct DNA sequencing for HRAS
mutations
SSCP analysis was performed to prescreen for
mutations in the HRAS and BRAF exons, in which
hotpoint mutations can be identified (19). Primers for SSCP-polymerase chain
reaction (PCR) were designed using the Primer 3.0 software (Premier
Biosoft International, Palo Alto, CA, USA; Table I. PCR was performed in a total volume
of 10 µl, consisting of 1 µl DNA solution (100 ng/µl), 0.5 units of
Platinum Taq DNA polymerase (Invitrogen; Thermo Fisher Scientific,
Inc., Waltham, MA, USA), 0.1 µCi [a-33P] deoxycytidine
triphosphate (ICN Biomedicals, Irvine, CA, USA; specific activity
of 3,000 Ci/mmol), 1–4 mmol/l MgCl2, 0.1–0.2 mmol/l
deoxynucleotide triphosphate, 0.2–0.4 mmol/l each primer, 10 mmol/l
Tris-HCl (pH 8.3) and 50 mmol/l KCl in a thermal cycler (Biometra
GmbH, Göttingen, Germany). The thermocycling conditions were as
follows: 95°C for 5 min, 37–40 cycles of 95°C for 50 sec, 45–54°C
for 60 sec and extension 72°C for 60 sec, and 72°C for 5 min.
Subsequent to PCR amplification, 10 µl PCR product was mixed with
20 µl loading buffer (0.02 M NaOH, 95% formamide, 20 mmol/l EDTA,
0.05% xylene cyanol, and 0.05% bromophenol blue) and denatured at
95°C for 10 min, prior to quenching on ice. A total of 5.5 µl
sample mixture was loaded onto a 12.5% polyacrylamide
non-denaturing gel containing 10% glycerol. Electrophoresis was
performed at 45 W for 3.5–4.5 h at room temperature with fan
cooling. Gels were performed silver staining according to our
previous study (20). Samples
exhibiting mobility shifts in SSCP analysis were re-amplified using
the same primers and PCR conditions as for SSCP analysis and
sequenced to determine the HRAS and BRAF genotypes
(Beijing Tianyi Huiyuan Co., Ltd., Beijing, China; Table I) (21).
 | Table I.Primers used for HRAS variant
screening in PTC. |
Table I.
Primers used for HRAS variant
screening in PTC.
| Gene (exon) | Forward sequence,
5′-3′ | Reverse sequence,
5′-3′ | Product size,
bp |
|---|
| HRAS
(1) |
cagtccttgctgcctggc |
atggttctggatcagctgga | 264 |
| HRAS
(2) |
cctgtctcctgcttcctctag |
tggcaaacacacacaggaag | 298 |
| BRAF
(15) |
aactcttcataatgcttgctctga |
agtaactcagcagcatctcagg | 251 |
Statistical analysis
χ2 test was used to identify the
association between HRAS and BRAF variants, the
different subtypes of PTC, and lymph node metastasis. All
statistical analyses were performed using SPSS 16.0 (SPSS, Inc.,
Chicago, IL, USA). P<0.05 was considered to indicate a
statistically significant difference.
Results
Subject characteristics
Table II presents the
clinical characteristics of the subjects. There were no differences
in age and sex between the 139 patients with PTC and the 195
healthy individuals. However, HRAS variants were more
frequent in patients with PTC compared with healthy individuals (37
vs. 26%, P=0.04).
 | Table II.Characteristics of the subjects. |
Table II.
Characteristics of the subjects.
| Variable | PTC samples, n
(%) | Control samples, n
(%) | P-value |
|---|
| Total | 139 | 195 |
|
| Age, years |
|
| 0.14 |
|
≤45 | 78 (56.1) | 126 (64.6) |
|
|
>45 | 61 (44.9) | 69 (35.4) |
|
| Sex |
|
| 0.25 |
|
Female | 106 (76.3) | 136 (69.7) |
|
|
Male | 33 (23.7) | 59 (30.3) |
|
| HRAS
variant | 51 (36.7) | 51 (26.2) | 0.04 |
Molecular analysis of HRAS and
BRAF
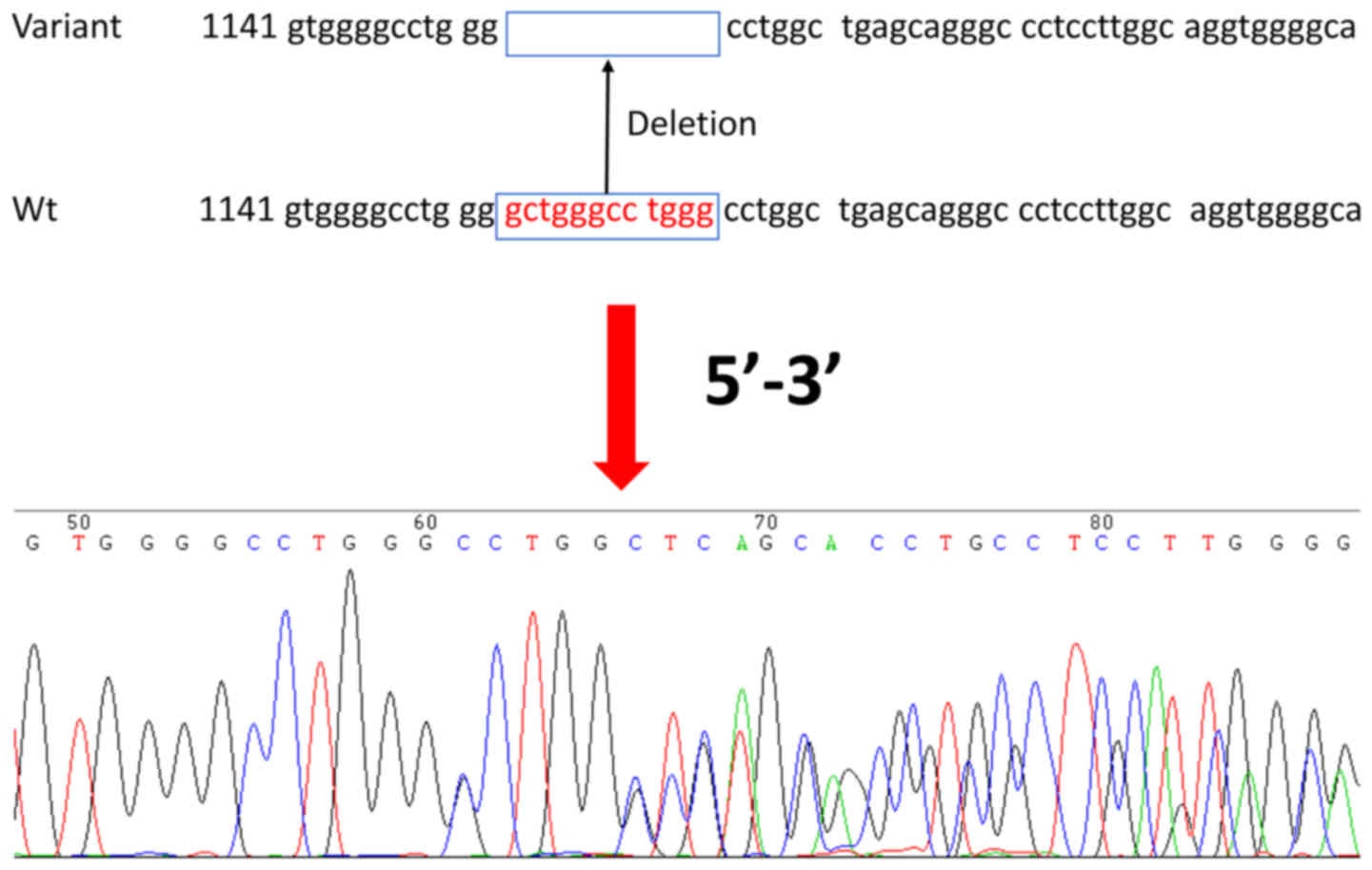
A novel variant of HRAS (IVS1-82del
gctgggcctggg; Fig. 1) was identified
to the best of our knowledge for the first time in PTC and adjacent
non-tumor tissue: 51/139 (37%) patients with PTC were heterozygous
for the IVS1-82del gctgggcctggg variant, compared with 51/195 (26%)
healthy controls (P=0.04; Table II).
The HRAS variant was not specific to PTC but occurred more
frequently in patients with PTC compared with healthy individuals.
The frequency of the HRAS variant did not differ among PTC
subtypes (P=0.95). There were no associations between the
HRAS variant and age, sex, tumor size, encapsulation,
multifocality/intrathyroidal spread, Tumor-Node-Metastasis stage
(22), thyroid nodule status,
Hashimoto history, BRAF mutation or PTC subtype (all
P>0.05; Table III). There were
significant differences in the number of BRAF mutations
among the different subtypes (P=0.041; Table IV). The presence of the BRAF V600E
mutant was not associated with that of the HRAS variant (P=0.196;
Table V).
 | Table III.Association of HRAS variant,
IVS1-82del gctgggcctggg, with clinical features in patients with
PTC. |
Table III.
Association of HRAS variant,
IVS1-82del gctgggcctggg, with clinical features in patients with
PTC.
|
|
| HRAS status,
n (%) |
|
|---|
|
|
|
|
|
|---|
| Variable | Patients with PTC,
n (%) | Wild-type | Variant | P-value |
|---|
| Total | 139 | 88 | 51 |
|
| Sex |
|
|
| 0.68 |
|
Female | 106 (76.3) | 66 (75.0) | 40 (78.4) |
|
|
Male | 33 (23.7) | 22 (25.0) | 11 (21.6) |
|
| Age, years |
|
|
| 0.11 |
|
≤45 | 78 (56.1) | 54 (31.4) | 24 (47.1) |
|
|
>45 | 61 (43.9) | 34 (68.6) | 27 (52.9) |
|
| Tumor size, mm |
|
|
| 0.11 |
|
≤10 | 79 (56.8) | 55 (62.5) | 24 (47.1) |
|
|
>10 | 60 (43.2) | 33 (37.5) | 27 (52.9) |
|
|
Encapsulation | 54 (38.9) | 32 (63.6) | 22 (53.1) | 0.47 |
|
Multifocality/intrathyroidal
spread | 32 (23.0) | 19 (21.6) | 13 (25.5) | 0.68 |
| Lymph
node metastasis | 66 (47.5) | 39 (44.3) | 27 (72.7) | 0.40 |
| TNM stage |
|
|
| 0.56 |
|
I/II | 99 (71.2) | 61 (69.3) | 38 (74.5) |
|
|
III/IV | 40 (28.8) | 27 (30.7) | 13 (25.5) |
|
|
Hashimoto's disease | 77 (55.3) | 51 (57.9) | 26 (50.9) | 0.49 |
| PTC subtype |
|
|
| 0.95 |
|
CVPTC | 34 (24.5) | 22 (25.0) | 12 (23.5) |
|
|
FVPTC | 36 (25.9) | 22 (25.0) | 14 (27.5) |
|
|
TCV | 69 (49.6) | 44 (50.0) | 25 (49.0) |
|
 | Table IV.BRAF V600E mutation occurrence
in different subtypes of papillary thyroid carcinoma. |
Table IV.
BRAF V600E mutation occurrence
in different subtypes of papillary thyroid carcinoma.
| Subtype | Mutation, n
(%) | Wild-type, n
(%) | χ2 | P-value |
|---|
| CVPTC | 25 (73.5) | 9 (26.4) |
| 0.041 |
| FVPTC | 24 (66.7) | 12 (33.3) | 6.390 |
|
| TCV | 60 (86.9) | 9 (13.0) |
|
|
 | Table V.Association between BRAF
mutation and the novel HRAS variant. |
Table V.
Association between BRAF
mutation and the novel HRAS variant.
|
|
HRAS−, n |
HRAS+, n | Total, n | χ2 | P-value |
|---|
|
BRAF− | 20 | 7 | 27 | 1.672 | 0.196 |
|
BRAF+ | 68 | 44 | 112 |
|
|
| Total | 88 | 51 | 139 |
|
|
Discussion
HRAS is one of the most commonly mutated
genes in thyroid cancer, particularly the follicular and Hurthle
cell subtypes. However, its contribution to PTC and the TCV is
poorly understood. Therefore, the present study aimed to
investigate the presence of somatic variants in HRAS in
patients with PTC and healthy controls, and to investigate their
association with PTC development. The results demonstrated that a
novel HRAS variant (IVS1-82del gctgggcctggg) could be
associated with PTC. Larger studies are required to assess the
distribution of this novel HRAS variant and to validate the
results of the present study.
PTC is the most common form of thyroid cancer
(2,3).
In the present study, the percentage of TCV samples harboring the
HRAS variant was 49.6%. The most common etiological factor
associated with onset of PTC is radiation; however, other factors,
including genetic susceptibility, have been demonstrated to be
associated with PTC development (23), as have predispositions such as
Hashimoto's thyroiditis (HT) (24).
HT has been recognized as a common autoimmune thyroid disorder
associated with various antibodies, including thyroid peroxidase
antibody (TPOAb) and thyroglobulin antibody (TgAb) (25). If patients present with diffuse goiter
(Graves disease), and their TPOAb and TgAb levels are
simultaneously increased, an HT diagnosis can be made. However, in
the present study, no significant association between HT and the
novel HRAS variant was identified.
Mutations associated with phenotypic susceptibility
are popular in oncology research; however, such research often
requires a large sample size to obtain reliable results.
Furthermore, the identification of novel variants often requires
DNA sequencing, which is an expensive technology with limited
availability in certain countries. The most commonly used method is
SSCP (26,27), which is an efficient and sensitive
technique used for the identification of single-base mutations.
Mutations in the genes of the RAS family
members are known to be associated with thyroid carcinogenesis;
RAS mutations have been identified in PTC, follicular
carcinoma, follicular adenoma, and medullary thyroid carcinoma
(17,28–32).
Previous studies have demonstrated that various types of thyroid
carcinoma, particularly FVPTC, harbor somatic mutations in
HRAS (15,16,33). The
HRAS gene is also often activated in urinary tract tumors
(34). The 81T>C polymorphism in
the HRAS gene is associated with increased risk of skin
(35), oral (36), bladder (37), and gastric (38) cancer. It has been demonstrated that
the 81T>C polymorphism, which increases protein expression
without changing its function, was associated with aneuploidy in
thyroid cancer (39). Previous
studies have reported that the frequency of RAS variants was
10–43% in PCT (40–43).
The BRAF V600E mutation has been demonstrated
to be the most common genetic alteration in PTC (8). BRAF is a member of the RAF
family and is involved in the MAPK pathway (28). Briefly, the MAPK cascade is initiated
upon RAS activation, which recruits BRAF to the
plasma membrane. The present study demonstrated that BRAF
mutations were more frequent in TCV than in other subtypes, and
that the HRAS variant occurred concomitantly with the
BRAF mutation in 31.6% of PTC samples (P=0.196). The
concomitant mutations are typically present in the CVPTC and TCV
subtypes (29.4 vs. 30.4%). This indicates that the concomitant
mutations may be associated with aggressive disease behavior and
poor prognosis; however, further studies are required to confirm
this.
Two different mechanisms may be responsible for the
carcinogenic effect of HRAS mutations: Modified protein
function or increased protein expression (43,44–46). As
RAS proteins are involved in cell differentiation, proliferation,
and survival, increased expression or activity of HRAS may
enhance these activities, which are associated with carcinogenesis.
Indeed, increased RAS activation leads to constitutive
activation of the downstream targets of RAS proteins, i.e., the
MAPK and PI3K/Akt signaling pathways (13). The novel HRAS variant
identified in the present study occurs at the 5′ end of the
sequence, which may affect the selective splicing of HRAS
and could be associated with tumor pathogenesis. However, the exact
effect of this variant on protein expression remains to be
determined.
Concomitant BRAF and RAS mutations may
allow simultaneous activation of the MAPK and PI3K/Akt signaling
pathways in cancer cells, providing a growth advantage (47,48).
Long-term follow-up revealed that patients with concomitant
mutations had a poorer response to treatment and reduced
disease-free survival times (49),
indicating that activation of the two genes may have a synergistic
effect on disease progression (50).
One previous study revealed no association between
HRAS variants and tumor biology (51), whereas other studies have reported
associations between HRAS variants and poorly differentiated
tumors (51,52). In the present study, HRAS
mutations were demonstrated to be associated with follicular
thyroid lesions (32). HRAS
has been demonstrated to be frequently mutated in Hurthle cells,
which are believed to represent a common metaplastic change in
damaged thyroid follicular epithelium (53). Hurthle cells can often develop into
Hurthle cell cancer, which is categorized as an oncocytic variant
of follicular carcinoma (54). The
present study did not include follicular carcinoma or Hurthle cell
cancer clinical cases; however, it is possible that the HRAS
variant arises from follicular or Hurthle cells in PTCs. In
addition, the results of the present study indicated that the novel
HRAS variant tends to occur in the TCV. Additional studies
are required to fully elucidate the role of the novel HRAS
variant in tumor biology.
The present study is limited by the number of
patients, retrospective nature, and constrained follow-up
information. Furthermore, the potential cellular mechanisms of
mutation functions in PTC were not determined. In conclusion, a
novel variant of HRAS (IVS1-82del gctgggcctggg) was
associated with PTC. Further studies are required to assess the
distribution of this novel HRAS variant and to validate the
results of the present study.
Acknowledgements
The authors would like to thank the team of
Professor Jian Huang for providing technical support. This study
was supported by a grant from the National Natural Science
Foundation of China (grant no. 81541132).
References
|
1
|
Hou P, Bojdani E and Xing M: Induction of
thyroid gene expression and radioiodine uptake in thyroid cancer
cells by targeting major signaling pathways. J Clin Endocrinol
Metab. 95:820–828. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ron E and Schneider AB: Thyroid
CancerCancer Epidemiology and Prevention. Schottenfeld D and
Fraumeni JF: Oxford University Press; New York: 2006, View Article : Google Scholar
|
|
3
|
Rahbari R, Zhang L and Kebebew E: Thyroid
cancer gender disparity. Future Oncol. 6:1771–1779. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Aschebrook-Kilfoy B, Ward MH, Sabra MM and
Devesa SS: Thyroid cancer incidence patterns in the United States
by histologic type, 1992–2006. Thyroid. 21:125–134. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Schneider DF and Chen H: New developments
in the diagnosis and treatment of thyroid cancer. CA Cancer J Clin.
63:374–394. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ghossein R and Livolsi VA: Papillary
thyroid carcinoma tall cell variant. Thyroid. 18:1179–1181. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Livolsi VA, Albores-Saavedra J, Asa SL,
Baloch ZW, Sobrinho-Simoes M, Wenig B, DeLellis RA, Cady B,
Mazzaferri EL, Hay I, et al: Papillary CarcinomaPathology and
Genetics: Tumours of Endocrine Organs. World Health Organization
Classification of Tumours. DeLellis RA, Lloyd RV, Heitz R and Eng
C: IARC Press; Lyon: 2004
|
|
8
|
Kim KB, Cabanillas ME, Lazar AJ, Williams
MD, Sanders DL, Ilagan JL, Nolop K, Lee RJ and Sherman SI: Clinical
responses to vemurafenib in patients with metastatic papillary
thyroid cancer harboring BRAF (V600E) mutation. Thyroid.
23:1277–1283. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Joo JY, Park JY, Yoon YH, Choi B, Kim JM,
Jo YS, Shong M and Koo BS: Prediction of occult central lymph node
metastasis in papillary thyroid carcinoma by preoperative BRAF
analysis using fine-needle aspiration biopsy: A prospective study.
J Clin Endocrinol Metab. 97:3996–4003. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kurtulmus N, Duren M, Ince U, Cengiz
Yakicier M, Peker O, Aydin O, Altiok E, Giray S and Azizlerli H:
BRAF (V600E) mutation in Turkish patients with papillary thyroid
cancer: Strong correlation with indicators of tumor aggressiveness.
Endocrine. 42:404–410. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Aksamitiene E, Kiyatkin A and Kholodenko
BN: Cross-talk between mitogenic Ras/MAPK and survival PI3K/Akt
pathways: A fine balance. Biochem Soc Trans. 40:139–146. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Xing M: Genetic alterations in the
phosphatidylinositol-3 kinase/Akt pathway in thyroid cancer.
Thyroid. 20:697–706. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nikiforov YE and Nikiforova MN: Molecular
genetics and diagnosis of thyroid cancer. Nat Rev Endocrinol.
7:569–580. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhu Z, Gandhi M, Nikiforova MN, Fischer AH
and Nikiforov YE: Molecular profile and clinical-pathologic
features of the follicular mutation of papillary thyroid carcinoma.
An unusually high prevalence of ras mutations. Am J Clin Pathol.
120:71–77. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Park JY, Kim WY, Hwang TS, Lee SS, Kim H,
Han HS, Lim SD, Kim WS, Yoo YB and Park KS: BRAF and RAS mutations
in follicular mutation of papillary thyroid carcinoma. Endocr
Pathol. 24:69–76. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rivera M, Ricarte-Filho J, Knauf J, Shaha
A, Tuttle M, Fagin JA and Ghossein RA: Molecular genotyping of
papillary thyroid carcinoma follicular mutation according to its
histological subtypes (encapsulated vs infiltrative) reveals
distinct BRAF and RAS mutation patterns. Mod Pathol. 23:1191–1200.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Adeniran AJ, Zhu Z, Gandhi M, Steward DL,
Fidler JP, Giordano TJ, Biddinger PW and Nikiforov YE: Correlation
between genetic alterations and microscopic features, clinical
manifestations and prognostic characteristics of thyroid papillary
carcinomas. Am J Surg Pathol. 30:216–222. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Liu RT, Hou CY, You HL, Huang CC,
Hock-Liew, Chou FF, Wang PW and Cheng JT: Selective occurrence of
ras mutations in benign and malignant thyroid follicular neoplasms
in Taiwan. Thyroid. 14:616–621. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Huang J, Pang J, Watanabe T, Ng HK and
Ohgaki H: Whole genome amplification for array comparative genomic
hybridization using DNA extracted from formalin-fixed,
paraffin-embedded histological sections. J Mol Diagn. 11:109–116.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huang J, Zhao YP, Li Q, Zhang JX, Wang Y
and Zhang B: Association of single nucleotide polymorphisms of NBS1
gene with genetic susceptibility to primary liver cancer in a
Chinese Han population. Prog Biochem Biophys. 39:678–686. 2012.
View Article : Google Scholar
|
|
21
|
Huang J, Grotzer MA, Watanabe T, Hewer E,
Pietsch T, Rutkowski S and Ohgaki H: Mutations in the Nijmegen
breakage syndrome gene in medulloblastomas. Clin Cancer Res.
14:4053–4058. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Qing W, Fang WY, Ye L, Shen LY, Zhang XF,
Fei XC, Chen X, Wang WQ, Li XY, Xiao JC and Ning G: Density of
tumor-associated macrophages correlates with lymph node metastasis
in papillary thyroid carcinoma. Thyroid. 22:905–910. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lloyd RV, Buehler D and Khanafshar E:
Papillary thyroid carcinoma mutation. Head Neck Pathol. 5:51–56.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Okayasu I, Fujiwara M, Hara Y, Tanaka Y
and Rose NR: Association of chronic lymphocytic thyroiditis and
thyroid papillary carcinoma. A study of surgical cases among
Japanese and white and African Americans. Cancer. 76:2312–2318.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hiromatsu Y, Satoh H and Amino N:
Hashimoto's thyroiditis: History and future outlook. Hormones
(Athens). 12:12–18. 2013.PubMed/NCBI
|
|
26
|
Long J, Wang Y, Li M, Tong WM, Jia JD and
Huang J: Correlation of TP53 mutations with HCV positivity in
hepatocarcinogenesis: Identification of a novel TP53 microindel in
hepatocellular carcinoma with HCV infection. Oncol Rep. 30:119–124.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Huang MD, Chen XF, Xu G, Wu QQ, Zhang JH,
Chen GF, Cai Y and Qi FZ: Genetic variation in the NBS1 gene is
associated with hepatic cancer risk in a Chinese population. DNA
Cell Biol. 31:678–682. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kimura ET, Nikiforova MN, Zhu Z, Knauf JA,
Nikiforov YE and Fagin JA: High prevalence of BRAF mutations in
thyroid cancer: Genetic evidence for constitutive activation of the
RET/PTC-RAS-BRAF signaling pathway in papillary thyroid carcinoma.
Cancer Res. 63:1454–1457. 2003.PubMed/NCBI
|
|
29
|
Soares P, Trovisco V, Rocha AS, Lima J,
Castro P, Preto A, Máximo V, Botelho T, Seruca R and
Sobrinho-Simões M: BRAF mutations and RET/PTC rearrangements are
alternative events in the etiopathogenesis of PTC. Oncogene.
22:4578–4580. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Frattini M, Ferrario C, Bressan P,
Balestra D, De Cecco L, Mondellini P, Bongarzone I, Collini P,
Gariboldi M, Pilotti S, et al: Alternative mutations of BRAF, RET
and NTRK1 are associated with similar but distinct gene expression
patterns in papillary thyroid cancer. Oncogene. 23:7436–7440. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Dockhorn-Dworniczak B, Caspari S, Schroder
S, Bocker W and Dworniczak B: Demonstration of activated oncogenes
of the ras family in human thyroid tumors using the polymerase
chain reaction. Verh Dtsch Ges Pathol. 74:415–418. 1990.PubMed/NCBI
|
|
32
|
Schulten HJ, Al-Maghrabi J, Al-Ghamdi K,
Salama S, Al-Muhayawi S, Chaudhary A, Hamour O, Abuzenadah A, Gari
M and Al-Qahtani M: Mutational screening of RET, HRAS, KRAS, NRAS,
BRAF, AKT1 and CTNNB1 in medullary thyroid carcinoma. Anticancer
Res. 31:4179–4183. 2011.PubMed/NCBI
|
|
33
|
Rivera M, Ricarte-Filho J, Tuttle RM,
Ganly I, Shaha A, Knauf J, Fagin J and Ghossein R: Molecular,
morphologic and outcome analysis of thyroid carcinomas according to
degree of extrathyroid extension. Thyroid. 20:1085–1093. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Fujita J, Yoshida O, Yuasa Y, Rhim JS,
Hatanaka M and Aaronson SA: Ha-ras oncogenes are activated by
somatic alterations in human urinary tract tumours. Nature.
309:464–466. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kreimer-Erlacher H, Seidl H, Back B, Kerl
H and Wolf P: High mutation frequency at Ha-ras exons 1–4 in
squamous cell carcinomas from PUVA-treated psoriasis patients.
Photochem Photobiol. 74:323–330. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Sathyan KM, Nalinakumari KR, Abraham T and
Kannan S: Influence of single nucleotide polymorphisms in H-Ras and
cyclin D1 genes on oral cancer susceptibility. Oral Oncol.
42:607–613. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Johne A, Roots I and Brockmoller J: A
single nucleotide polymorphism in the human H-ras proto-oncogene
determines the risk of urinary bladder cancer. Cancer Epidemiol
Biomarkers Prev. 12:68–70. 2003.PubMed/NCBI
|
|
38
|
Zhang Y, Jin M, Liu B, Ma X, Yao K, Li Q
and Chen K: Association between H-RAS T81C genetic polymorphism and
gastrointestinal cancer risk: A population based case-control study
in China. BMC Cancer. 8:2562008. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Castro P, Soares P, Gusmão L, Seruca R and
Sobrinho-Simoes M: H-RAS 81 polymorphism is significantly
associated with aneuploidy in follicular tumors of the thyroid.
Oncogene. 25:4620–4627. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Esapa CT, Johnson SJ, Kendall-Taylor P,
Lennard TW and Harris PE: Prevalence of Ras mutations in thyroid
neoplasia. Clin Endocrinol (Oxf). 50:529–535. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zhu Z, Gandhi M, Nikiforova MN, Fischer AH
and Nikiforov YE: Molecular profile and clinical-pathologic
features of the follicular variant of papillary thyroid carcinoma.
An unusually high prevalence of ras mutations. Am J Clin Pathol.
120:71–77. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Santarpia L, Myers JN, Sherman SI,
Trimarchi F, Clayman GL and El-Naggar AK: Genetic alterations in
the RAS/RAF/mitogen-activated protein kinase and
phosphatidylinositol 3-kinase/Akt signaling pathways in the
follicular variant of papillary thyroid carcinoma. Cancer.
116:2974–2983. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Khan MS, Pandith AA, Ul Hussain M, Iqbal
M, Khan NP, Wani KA, Masoodi SR and Mudassar S: Lack of mutational
events of RAS genes in sporadic thyroid cancer but high risk
associated with HRAS T81C single nucleotide polymorphism
(case-control study). Tumour Biol. 34:521–529. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Bos JL: ras oncogenes in human cancer: A
review. Cancer Res. 49:4682–4689. 1989.PubMed/NCBI
|
|
45
|
Bos JL: The ras gene family and human
carcinogenesis. Mutat Res. 195:255–271. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Hashimoto-Gotoh T, Kikuno R, Takahashi M
and Honkawa H: Possible role of the first intron of c-H-ras in gene
expression: anti-cancer elements in oncogenes. Anticancer Res.
8:851–859. 1988.PubMed/NCBI
|
|
47
|
Vasko V, Saji M, Hardy E, Kruhlak M, Larin
A, Savchenko V, Miyakawa M, Isozaki O, Murakami H, Tsushima T, et
al: Akt activation and localisation correlate with tumour invasion
and oncogene expression in thyroid cancer. J Med Genet. 41:161–170.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Janku F, Lee JJ, Tsimberidou AM, Hong DS,
Naing A, Falchook GS, Fu S, Luthra R, Garrido-Laguna I and Kurzrock
R: PIK3CA mutations frequently coexist with RAS and BRAF mutations
in patients with advanced cancers. PLoS One. 6:e227692011.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Zou M, Baitei EY, Alzahrani AS, BinHumaid
FS, Alkhafaji D, Al-Rijjal RA, Meyer BF and Shi Y: Concomitant RAS
RET/PTC, or BRAF mutations in advanced stage of papillary thyroid
carcinoma. Thyroid. 24:1256–1266. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Oliveira C, Velho S, Moutinho C, Ferreira
A, Preto A, Domingo E, Capelinha AF, Duval A, Hamelin R, Machado
JC, et al: KRAS and BRAF oncogenic mutations in MSS colorectal
carcinoma progression. Oncogene. 26:158–163. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Suarez HG, du Villard JA, Severino M,
Caillou B, Schlumberger M, Tubiana M, Parmentier C and Monier R:
Presence of mutations in all three ras genes in human thyroid
tumors. Oncogene. 5:565–570. 1990.PubMed/NCBI
|
|
52
|
Pilotti S, Collini P, Mariani L, Placucci
M, Bongarzone I, Vigneri P, Cipriani S, Falcetta F, Miceli R,
Pierotti MA and Rilke F: Insular carcinoma: A distinct de novo
entity among follicular carcinomas of the thyroid gland. Am J Surg
Pathol. 21:1466–1473. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Ganly I, Ricarte Filho J, Eng S, Ghossein
R, Morris LG, Liang Y, Socci N, Kannan K, Mo Q, Fagin JA and Chan
TA: Genomic dissection of Hurthle cell carcinoma reveals a unique
class of thyroid malignancy. J Clin Endocrinol Metab. 98:E962–E972.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
DeLellis RA, Lloyd RV and Heitz PU: World
Health Organization Classification of Tumors. Pathology and
Genetics: Tumors of Endocrine Organs. IARC Press; Lyon, France: pp.
69–72. 2004
|