Introduction
Carotid body tumor (CBT) is a rare disease derived
from carotid body paraganglion cells. The characteristic feature of
this tumor is a rich vascular network in its contents and capsules
supplied by many feeding arteries (1). As the risk of complications such as
cranial nerve paralysis increases as the tumor grows, surgical
resection is recommended for all CBTs in otherwise healthy patients
(2,3).
Moreover, there is a small but definite risk of malignancies for
all paragangliomas (4–7). Molecular biological study has so far
revealed that this tumor has various types of gene alterations such
as point mutations in the SDH gene family (2,8,9). A total of 10 to 35% of patients with CBT
are estimated to harbor a hereditary predisposition and SDHD is the
most common mutation, followed by SDHB and then SDHC (2). In one review, it was reported that SDH
germ-line mutations are present in 31% of patients with head and
neck paragangliomas (10). The
concept of the ‘hereditary paraganglioma-pheochromocytoma syndrome’
has arisen to describe familial paraganglioma patients, which
includes CBT patients with a family history and gene alterations
(11–13).
The low incidence rate of this tumor and absence of
a registration and study system has prevented detailed research to
be performed to clarify the present status of this tumor in Japan.
Also the status of SDHx gene mutations was not obvious because of
genetic testing was not performed for these patients. We organized
a study group, which we call the Japan Carotid Body Tumor Research
Group (JCBTRG), and initiated a survey of the patients with CBT in
Japan. The goal of our study is to reveal the overall aspects of
gene alteration patterns, such as those present in the SDH gene
family, among patients in Japan. Initially, we began with a survey
of the status of patients throughout Japan. Here we report the
characteristic features of CBT patients in Japan unveiled from our
studies.
Patients and methods
All procedures followed were in accordance with the
ethical standards of the responsible committee on human
experimentation (institutional and national) and with the Helsinki
Declaration of 1975, as revised in 2008.
The study design was a multi-institutional
retrospective review of medical records. Research protocols were
assessed and accepted by the institutional research boards of
individual institutions.
We sent the research format for cases of CBT to 635
authorized institutions that had specialists who were members of
the Japan Otolaryngology Society. A total of 316 responses were
sent back to the research bureau at Iwate Medical University and
150 patients were registered from 25 institutions in our study.
There were 204 hospitals or institutions that did not have CBT
patients for 20 years. Information on the CBT patients was
summarized and analyzed. The analyzed items were gender, age,
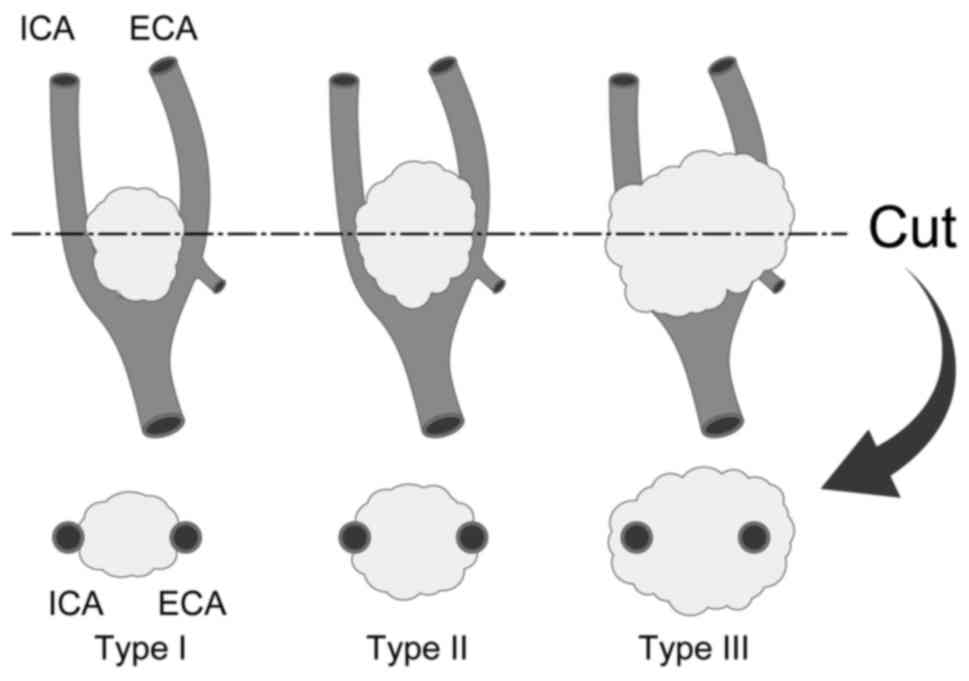
family history, size, Shamblin classification (Fig. 1) (1),
location of the patients, operation time of extirpation surgery,
amount of blood loss, preoperative embolization of the feeding
arteries and resection and repair of the carotid arteries.
Statistical analyses were carried out using Students' t-test.
Results
From 1995 to 2015, 399 patients with CBT were
referred to 112 institutions. In summary, 194 patients underwent
surgery and 205 patients were under follow-up without surgery.
Patients with CBT from these institutions were registered in our
study and we obtained 150 summarized patient records from 25
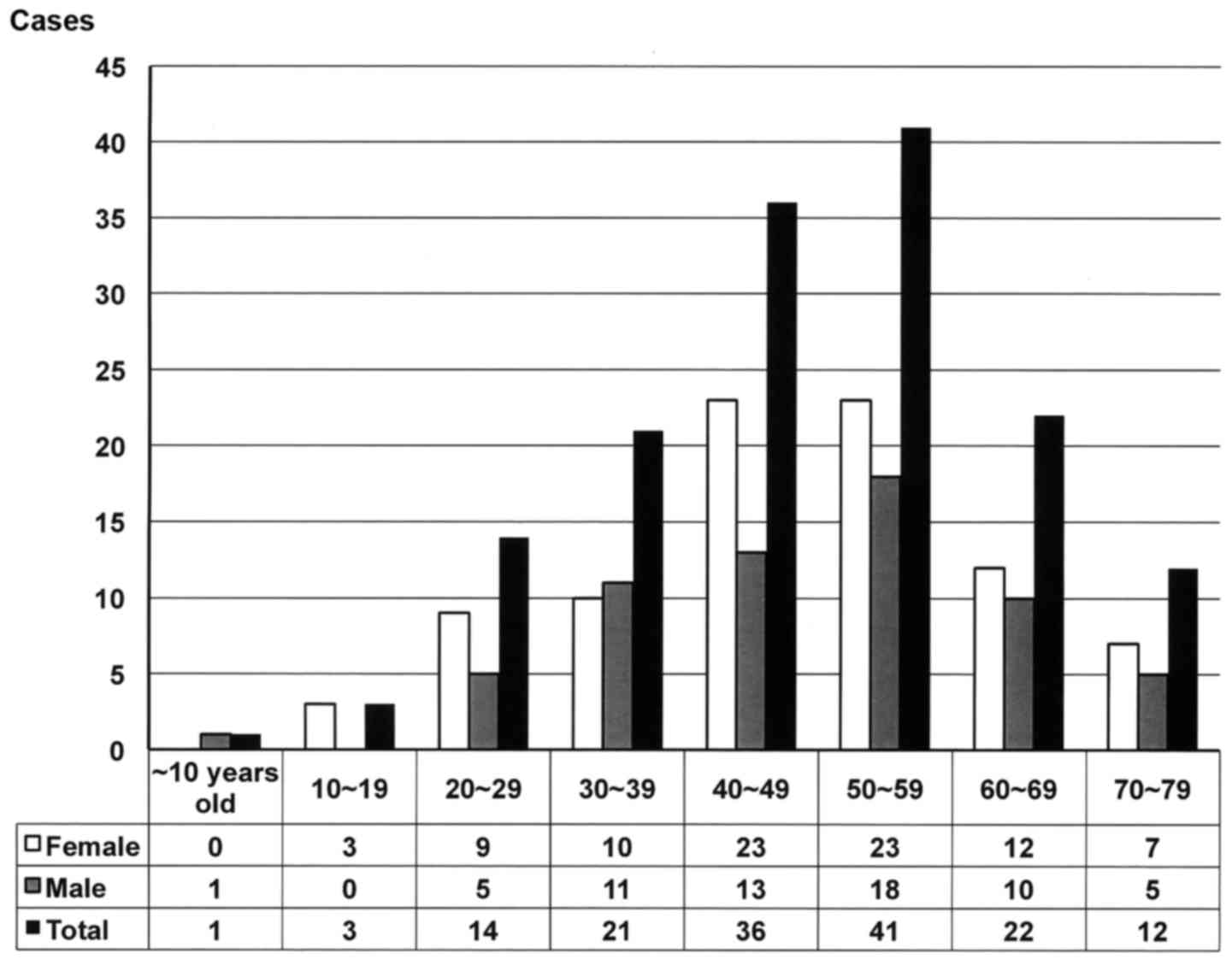
institutions. There were 87 females and 63 males and their mean and
median age were 48.0 years old and 49 years old, respectively,
ranging from 8 to 78 years old (Fig.
2). Fifty to 60 year old patients were the most dominant
throughout all age groups followed by 40 to 50 year old patients.
There was an 8 year old patient as well. As for gender, female
patients were dominant in almost every age group. Fifteen patients
had bilateral CBTs resulting in 165 CBTs.
The chief complaints of the patients with CBT are
shown in Table I. Neck tumors were
the most frequent chief complaint in these patients and 125
patients (83.3%) complained of neck tumors. The second chief
complaint was an incidental recognition of the tumor by some
modalities such as CT scan or MRI (14 patients, 9.3%). There were
some patients who complained of hoarseness (3 patients, 2.0%),
pharyngeal discomfort (2 patients, 1.3%) dysphagia, hearing loss,
numbness of the body, or chest discomfort. Four patients (2.7%)
complained of pain. The mean and median suffering period was 46.1
months and 10.5 months, respectively, ranging from 0 months to 480
months.
 | Table I.Chief complaint in the 150 patients
with carotid body tumors. |
Table I.
Chief complaint in the 150 patients
with carotid body tumors.
| Complaint type | Number of the
patients | Percentage of total
patients (%) |
|---|
| Neck tumor | 125 | 83.3 |
| Incidental
recognition | 14 | 9.3 |
| Pain | 4 | 2.7 |
| Hoarseness | 3 | 2.0 |
| Pharyngeal
discomfort | 1 | 0.6 |
| Dysphagia | 1 | 0.6 |
| Hearing loss | 1 | 0.6 |
| Numbness of the
body | 1 | 0.6 |
| Chest discomfort | 1 | 0.6 |
Eighteen patients had a family history of
paragangliomas (Table II). There
were 10 male and 8 female patients. Five patients had fathers who
had a type of paraganglioma; namely, CBT, vagal paraganglioma, or
pheochromocytoma (Cases 1, 3, 5, 6 and 12) and the other 4 patients
had a father who was expected to have a type of paraganglioma
(Cases 2, 10, 14 and 17). Two patients had a brother and a sister
with paragangliomas and two patients had a brother and a sister who
were assumed to have paragangliomas. A patient had sons with
paragangliomas and two patients had a daughter with CBT. Two
patients had bilateral CBTs.
 | Table II.Family history of patients with
CBT. |
Table II.
Family history of patients with
CBT.
| Case no. | Age (years) | Gender | Family members | Comments |
|---|
| 1 | 30 | Male | Father: CBT+vagal
paraganglioma Aunt: CBT |
|
| 2 | 23 | Female | Father: Renal tumor
(pheochromocytoma?) |
|
| 3 | 40 | Female | Father:
Pheochromocytoma elder brother: Pheochromocytoma |
|
| 4 | 56 | Female | Younger brother:
Vagal paraganglioma |
|
| 5 | 40 | Male | Father: CBT elder
brother: CBT |
|
| 6 | 45 | Male | Father: CBT younger
brother: CBT | Bilateral CBTs |
| 7 | 72 | Male | Sons: CBT |
|
| 8 | 49 | Male | Daughter: CBT |
|
| 9 | 53 | Male | Elder sister: Glomus
tumor paternal cousin: Glomus tumor |
|
| 10 | 48 | Female | Father: Bilateral
tumor of the neck(CBT?) |
|
| 11 | 37 | Male | Details unknown |
|
| 12 | 29 | Female | Father: CBT |
|
| 13 | 56 | Male | Daughter: CBT |
|
| 14 | 51 | Male | Father: Details
unknown |
|
| 15 | 59 | Male | Younger sister:
Details unknown | Bilateral CBTs |
| 16 | 58 | Female | Elder brother:
Details unknown |
|
| 17 | 42 | Female | Father: Details
unknown |
|
| 18 | 19 | Female | Grandmother: Details
unknown |
|
Seven patients had metastases that included the
lymph nodes in 5 patients and the lung in 3 patients. As for other
paragangliomas, 4 patients had pheochromocytomas, two of which were
malignant. Two of these patients had a family history. Three
patients had glomus tumors and 2 patients had mediastinal
paragangliomas. One patient had von Hippel Lindau disease.
Although the survey covered all prefectures, there
were some tendencies that indicated the frequency of CBT was
dependent on the area where the patients lived or the hospitals to
which they were referred. Table III
shows the frequencies of CBT patients according to the institutions
to which they were referred. There were 28 prefectures that had no
patient with CBT registered in our study. The other 19 prefectures
had more than one patient registered to our study. One-third of the
patients (57 patients) were located in the Tokyo area where medical
institutions were gathered. Fifteen patients were registered from
Aichi and Hyogo. Eleven and ten patients were from Iwate and
Miyagi, respectively. Nine patients were from Hokkaido and
Nagasaki, respectively.
 | Table III.Location of patients with carotid body
tumors in Japan. |
Table III.
Location of patients with carotid body
tumors in Japan.
| Prefecture | Male | Female | Total |
|---|
| Hokkaido | 4 | 5 | 9 |
| Iwate | 3 | 8 | 11 |
| Miyagi | 5 | 5 | 10 |
| Fukushima | 0 | 1 | 1 |
| Saitama | 0 | 3 | 3 |
| Chiba | 0 | 1 | 1 |
| Tokyo | 20 | 37 | 57 |
| Kanagawa | 2 | 0 | 2 |
| Niigata | 2 | 2 | 4 |
| Fukui | 1 | 0 | 1 |
| Aichi | 6 | 9 | 15 |
| Mie | 1 | 2 | 3 |
| Hyougo | 7 | 8 | 15 |
| Nara | 0 | 2 | 2 |
| Hiroshima | 0 | 2 | 2 |
| Fukuoka | 1 | 0 | 1 |
| Nagasaki | 7 | 2 | 9 |
| Kumamoto | 2 | 0 | 2 |
| Okinawa | 2 | 0 | 2 |
| Total no. of
patients | 63 | 87 | 150 |
Ninety-four patients underwent surgery and 6
patients underwent radiation therapy. The other patients remained
under observation because of the patients' choice or physicians'
recommendation. The treatment choice of these patients depended on
the institutions to which they were referred.
Among the 94 patients including 4 patients with
bilateral CBTs who underwent surgery to remove a CBT, 23 patients
had tumors classified as Shamblin type I, 59 had type II and 12 had
type III (Table IV). Classification
of tumors from four patients were not recorded nor undone. The
feeding arteries of 76 tumors were preoperatively embolized before
resection of the CBT (Table IV). The
average tumor size in diameter was 26.3 mm in Shamblin type I
tumors, 37.3 mm in type II tumors and 36.7 mm in type III
tumors.
 | Table IV.Shamblin classification. |
Table IV.
Shamblin classification.
| A, Size in diameter
(mm) |
|---|
|
|---|
|
| Shamblin
classification |
|
|---|
|
|
|
|
|---|
| Variable | I | II | III | Average |
|---|
| Mean | 26.3 | 37.3 | 36.7 | 34.6 |
| Median | 24.5 | 38.0 | 35.5 | 35.0 |
|
| B, Preoperative
embolization (n) |
|
|
| Shamblin
classification |
|
|
|
|
|
|
Variable | I | II | III | Total |
|
| + | 19 | 48 | 9 | 76 |
| − | 4 | 11 | 3 | 18 |
| Total (n) | 23 | 59 | 12 | 94 |
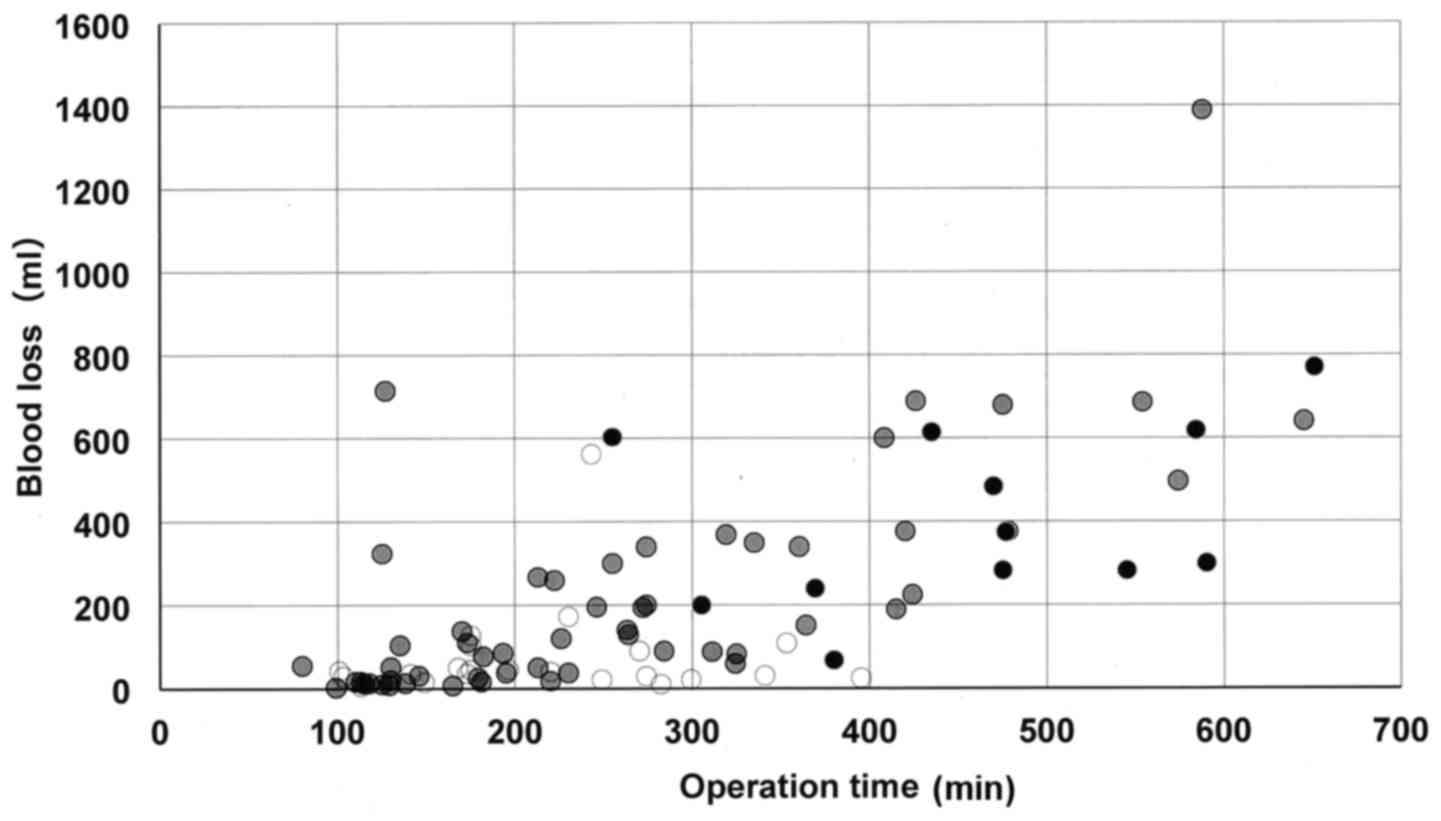
We analyzed the relationship between operation time
of the surgery and the amount of blood loss. Fig. 3 shows the result of the analysis. The
calculated coefficient correlation was 0.69 for all patients.
According to Shamblin classification, mean operation time of the
surgery and the mean amount of blood loss were 229 min and 77.8 ml
in Shamblin I, 262 min and 229 ml in Shamblin II, 461 min and 404
ml in Shamblin III, respectively. As for operation time, there were
significant differences between Shamblin I and II (P=0.016) and
Shamblin I and III (P<0.001) (Table
V). While as for the amount of blood loss, there were
significant differences between Shamblin I and III (P<0.001) and
Shamblin II and III (P<0.001) (Table
V).
 | Table V.Blood loss and operation time by
Shamblin classification. |
Table V.
Blood loss and operation time by
Shamblin classification.
| Variable | Shamblin I | Shamblin II | Shamblin III | P-value |
|---|
| Mean blood loss
(ml) | 78 | 229 | 404 | I vs.
II: 0.016 |
|
|
|
|
| II vs. III:
0.082 |
|
|
|
|
| I vs. III:
<0.001 |
| Mean operation time
(min) | 229 | 262 | 461 | I vs. II: 0.40 |
|
|
|
|
| II vs. III:
<0.001 |
|
|
|
|
| I vs. III:
<0.001 |
Table VI shows the
main feeding arteries of 78 tumors detected by carotid
arteriography. Most frequent feeding artery was the ascending
pharyngeal artery followed by the superior thyroid artery and the
occipital artery. It is noteworthy that in some patients, feeding
artery was derived from external carotid artery (n=7) and internal
carotid artery (n=1).
 | Table VI.Main feeding arteries of carotid body
tumors. |
Table VI.
Main feeding arteries of carotid body
tumors.
| Feeding artery | Number of the
patients (%) |
|---|
| Ascending
pharyngeal artery | 50 (64.1) |
| Superior thyroid
artery | 18 (23.1) |
| Occipital
artery | 17 (21.8) |
| External carotid
artery | 7 (9.0) |
| Lingual artery | 6 (7.7) |
| Posterior auricular
artery | 4 (5.1) |
| Facial artery | 2 (2.6) |
| Ascending palatine
artery | 2 (2.6) |
| Superficial
temporal artery | 1 (1.3) |
| Common carotid
artery | 1 (1.3) |
| Internal carotid
artery | 1 (1.3) |
When the patients underwent preoperative
embolization, mean operation time of the surgery and the mean
amount of blood loss were 240 min and 55.9 ml in Shamblin I, 255
min and 178 ml in Shamblin II, 468 min and 406 ml in Shamblin III,
respectively. While the patients did not undergo preoperative
embolization, mean operation time of the surgery and the mean
amount of blood loss were 181 min and 171 ml in Shamblin I, 290 min
and 468 ml in Shamblin II, 440 min and 396 ml in Shamblin III,
respectively. As for the amount of blood loss, there was a
significant difference between the patients with preoperative
embolization and those without that in Shamblin I and II tumors
(Table VII, P=0.038 and P=0.0011,
respectively).
 | Table VII.Operation time and blood loss during
surgery with or without preoperative embolization. |
Table VII.
Operation time and blood loss during
surgery with or without preoperative embolization.
| A, Operation
time |
|---|
|
|---|
| Shamblin
classification | Total time
(min) | Embolization
(−) | Embolization
(+) | P-value |
|---|
| I | 229±97 | 240±102 | 181±38 | 0.317 |
| II | 262±138 | 255±123 | 290±183 | 0.496 |
| III | 461±115 | 468±104 | 440±139 | 0.524 |
|
| B, Blood loss
during surgery |
|
| Shamblin
classification | Total quantity
(ml) | Embolization
(−) | Embolization
(+) | P-value |
|
| I | 78±114 | 56±45 | 171±226 | 0.038 |
| II | 229±271 | 178±206 | 468±387 | 0.0011 |
| III | 404±203 | 406±218 | 396±147 | 0.623 |
Patients with Shamblin I tumor underwent no
resection of carotid artery. Twenty-one out of 59 patients with
Shamblin II tumor underwent resection of external carotid artery
(ECA) and 2 patients underwent reconstruction of internal carotid
artery (ICA), while all 12 patients with Shamblin III tumor
underwent resection of ECA and 10 patients underwent reconstruction
of ICA (Table VIII).
 | Table VIII.Damage and repair to the carotid
arteries. |
Table VIII.
Damage and repair to the carotid
arteries.
| Variable | Shamblin I | Shamblin II | Shamblin III | Total |
|---|
| Number of
patients | 23 | 59 | 12 | 94 |
| Resection of
ECA | 0 | 21 | 12 | 33 (33.7%) |
| Reconstruction
of | 0 | 2 | 10 | 12 (12.2%) |
| ICA |
|
|
|
|
Fifty-five (56%) patients who underwent surgery
exhibited some postoperative complications (Table IX). The most frequent complication
was vagal nerve paralysis, including recurrent nerve palsy in 22
(23%) patients, followed by hypoglossal nerve paralysis in 18
(19%). Thirteen patients exhibited two or more nerve paralysis
episodes; the most frequent combination was that of vagal and
hypoglossal nerve paralysis. Most of these complications were
transient, but a patient underwent phonosurgery afterwards. There
was no mortality in this cohort of patients after surgery.
 | Table IX.Postoperative complications following
carotid body tumor surgery. |
Table IX.
Postoperative complications following
carotid body tumor surgery.
| Postoperative
complication | Total number | Embolization
(−) | Embolization
(+) |
|---|
| X paralysis | 22 | 4 | 18 |
| XII paralysis | 18 | 5 | 13 |
| First bite
syndrome | 10 | 0 | 10 |
| Horner
syndrome | 7 | 0 | 7 |
| IX paralysis | 6 | 1 | 5 |
| VII marginal branch
paralysis | 4 | 0 | 4 |
| Dysphagia | 4 | 0 | 4 |
| XI paralysis | 1 | 0 | 1 |
| Hypertension | 1 | 1 | 0 |
| Orthostatic
hypotension | 1 | 0 | 1 |
| Tunnel vision | 1 | 1 | 0 |
| Vertigo | 1 | 0 | 1 |
| Carotid artery
stenosis | 1 | 0 | 1 |
| Cerebral
infarction | 1 | 1 | 0 |
| Total no. of
cases | 55 out of 94
patients | 9 out of 18
patients | 46 out of 76
patients |
Discussion
As it is well known that CBTs are very rare,
detailed features of this tumor have not been clarified in Japan.
One of the reasons is that there has been no registration and study
system until we organized the study group JCBTRG and initiated the
survey of patients with CBT. By recruiting CBT patients to our
survey from 635 authorized institutions for specialists of the
Japan Otolaryngology Society, we could include CBT patients from
throughout Japan as a whole even if some of the patients were not
registered in our research system.
In accordance with our expectations, the number of
female CBT patients was more than that of male patients. Although
Shamblin's reports showed that the number of male patients was
twice as many as that of female patients (1), most reports have shown that the number
of female patients was more than that of male patients (3,13–16).
The most common chief complaint in our patients was
neck tumors and 83.3% of the patients complained of a neck tumor.
As expected, their suffering periods were relatively long compared
to those of other neck tumors, especially malignant ones. The
longest suffering period was 40 years, indicating CBT has a
characteristic feature of being a slow growing neck mass because
most CBTs are benign. As some patients showed paralysis of the
vagal nerve, which led to symptoms such as hoarseness and
dysphagia, physicians must treat CBT neck tumors when they
recognize vagal nerve paralysis as a differential diagnosis.
Eighteen patients (12%) had a family history of some
kind of paraganglioma. This frequency was compatible with previous
reports (12,17,18).
Perhaps on-going analysis of gene mutations and clarification of
gene mutation status could lead to recognition of more family
members in Japanese CBT patients. In fact, a father and a daughter
from Miyagi prefecture had the same mutation in the SDHD gene
(18). Similar results were reported
from Korea and China (19,20).
Seven patients (4.7%) had metastases of CBT and
their tumor was diagnosed as a malignant CBT. This frequency was
compatible with previous reports (4–7,21). It is well known that, as
histopathological examination cannot distinguish a malignant tumor
by morphological features in microscopic findings, malignancy or
not is diagnosed by metastatic activity, namely clinical findings.
The necessity of surgical resection depends on this aspect of tumor
malignancy if it is not frequent. Head and neck surgeons must
consider surgical resection of CBT once a patient is referred to
our hospital.
The uneven distribution of the CBT patients is
perhaps reflected in the uneven distribution of the population and
medical institutions in Japan. Tokyo is the capital city of Japan
and her population is over 10,000,000. However, as Japan has a
population of approximately 120,000,000, it is not reasonable to
expect that one-third of the CBT patients would be from the Tokyo
area. Maybe the number of medical institutions also influenced the
majority of patients being from the Tokyo area. Although Aichi and
Hyogo have reasonable population sizes for the number of CBT
patients, Iwate, Miyagi and Nagasaki have smaller populations,
which were not reasonable for the number of their CBT patients. As
we previously reported (18), CBT
patients in Miyagi and Iwate (next to Miyagi) have the possibility
of having the same gene alterations. These results indicated the
possibility that some gene alterations penetrated into other areas
in Japan such as Miyagi, Iwate and Nagasaki. Further investigation
is needed to clarify the gene alterations of CBT patients in these
high incidence areas.
As the characteristic feature of this tumor is a
rich vascular network in its contents and capsules supplied by many
feeding arteries, surgeons must be extremely careful to resect CBT
because careless procedures result in vessel damage and much blood
loss, especially damage of carotid artery lead to reconstruction of
it. Preoperative angiography revealed that the most frequent
feeding artery was the ascending pharyngeal artery followed by the
occipital artery and the superior thyroid artery. Our result
indicated that the direct feeding arteries derived from external
carotid artery were relatively common, if not so many, in CBT
patients (9%, 7 out of 78 tumors, Table
VI). Perhaps these direct feeding arteries from carotid
arteries were ringleaders for much blood loss in surgery. As we
head and neck surgeons experienced few cases of extra-branches from
carotid artery during neck surgery, especially neck dissection,
these frequent direct branches from carotid arteries could reflect
embryonic origin of branches of hereditary paraganglioma patients.
As there have been few studies to report the distribution of
feeding arteries into CBT, this study give the light for head and
neck surgeons and interventional radiologists to deal with feeding
arteries of CBT.
As our expectations, time of the surgery and the
amount of blood loss depended on Shamblin classification. Shamblin
III tumors took more time and blood loss than Shamblin II and I
tumors during their resection surgery, while Shamblin II tumors
took more time and blood loss than Shamblin I tumors (Table IV). Although effect of preoperative
embolization to reduce the amount of blood loss was seen in
Shamblin I and II tumors, effectiveness for reduction of time of
the surgery was not obvious in our series of patients (Table V), As same results were reported by
Power et al (22), it would be
common that the reduction of operative time is difficult by
preoperative embolization in CBT surgery. It could also be likely
that the variety of embolization technique and interventional
radiologists made the evaluation difficult. Multi-institutional
study using standard technique must be needed to clarify the effect
of preoperative embolization for accurate evaluation of the
procedures.
As Shamblin III tumor surrounded ECA and ICA,
resection surgery for these tumors needed resection these arteries
to some extent. Actually all patients with Shamblin III tumor
underwent resection of ECA and 83% of these patients (10 out of 12)
underwent reconstruction of ICA in our series. Although same
results were reported by some authors (23), there were few reports which mentioned
about the correlation of ICA reconstruction and Shamblin III tumor.
Our results indicated that preparation of reconstruction surgery of
ICA must be needed to perform resection of Shamblin III CBTs.
As we performed a survey of the status of patients
throughout Japan, we can report the characteristic features of CBT
patients in Japan as found in our studies. There were some
high-incidence areas of CBT such as Miyagi, Iwate, and Nagasaki,
perhaps reflecting the prevalence of patients with a familial
history of paraganglioma with some gene alterations. Among the 94
patients who underwent surgery to remove a CBT, 23 patients
presented with tumors classified as Shamblin type I, 59 with type
II, and 12 with type III. The most frequent feeding artery of these
CBTs was the ascending pharyngeal artery. Preoperative embolization
of these feeding arteries was effective to reduce blood loss, but
not the operation time of Shamblin type I and II tumors.
Acknowledgements
This work was supported by a Grant-in-aid for JSPS
KAKENHI (grant no. 26462619). The abstract of the present study was
published in J Clin Oncol 35 (Suppl 15): e17574, 2017.
References
|
1
|
Shamblin WR, ReMine WH, Sheps SG and
Harrison EG Jr: Carotid body tumor (Chemodectoma),
Clinicopathologic analysis of ninety cases. Am J Surg. 122:732–739.
1971. View Article : Google Scholar
|
|
2
|
Fruhmann J, Geigl JB, Konstantiniuk P and
Cohnert TU: Paraganglioma of the carotid body: Treatment strategy
and SDH-gene mutations. Eur Vasc Endovasc Surg. 45:431–436. 2013.
View Article : Google Scholar
|
|
3
|
Sajid MS, Hamilton G and Baker DM: A
multicenter review of carotid body tumor management. Eur J Vasc
Endovasc Surg. 34:127–130. 2007. View Article : Google Scholar
|
|
4
|
Lee JH, Barich F, Karnell LH, Robinson RA,
Zhen WK, Gantz BJ and Hoffman HT; American College of Surgeons
Commission on Cancer, ; American Cancer Society, : National cancer
data base report on malignant paragangliomas of the head and neck.
Cancer. 94:730–737. 2002. View Article : Google Scholar
|
|
5
|
Zhang WC, Cheng JP, Li Q, Zhang L, Wang XD
and Anniko M: Clinical and pathological analysis of malignant
carotid body tumor: A report of nine cases. Acta Otolaryngol.
129:1320–1325. 2009. View Article : Google Scholar
|
|
6
|
Hall TC, Renwick P and Stafford ND:
Recurrent familial malignant carotid body tumour presenting with
lymph node metastasis: Case report and review of diagnosis and
management of familial carotid body tumours. J Laryngol Otol.
124:1344–1346. 2010. View Article : Google Scholar
|
|
7
|
Nishijima H, Asakage T and Sugasawa M:
Malignant carotid body tumor with systemic metastases. Ann Otol
Rhinol Lalyngol. 120:381–385. 2011. View Article : Google Scholar
|
|
8
|
Offergeld C, Brase C, Yaremchuk S, Mader
I, Rischke HC, Gläsker S, Schmid KW, Wiech T, Preuss SF, Suárez C,
et al: Head and neck paragangliomas: Clinical and molecular genetic
classification. Clinics(Sao Paulo). 67 Suppl 1:S19–S28. 2012.
View Article : Google Scholar
|
|
9
|
Burnichon N, Rohmer V, Amar L, Herman P,
Leboulleux S, Darrouzet V, Niccoli P, Gaillard D, Chabrier G,
Chabolle F, et al: The succinate dehydrogenase genetic testing in a
large prospective series of patients with Paragangliomas. J Clin
Endocrinol Metab. 94:2817–2827. 2009. View Article : Google Scholar
|
|
10
|
Neumann HP, Erlic Z, Boedeker CC, Rybicki
LA, Robleda M, Hermsen M, Schiavi F, Falcioni M, Kwok P, Bauters C,
et al: Clinical predictors for germline mutations. in head and neck
paraganglioma patients: Cost reduction strategy in genetic
diagnostic process as fall-out. Cancer Res. 69:3650–3656. 2009.
View Article : Google Scholar
|
|
11
|
Astuti D, Latif F, Dallolv A, Dahia PL,
Douglas F, George E, Sköldberg F, Husebye ES, Eng C and Maher ER:
Gene mutations in the succinate dehydrogenase subunit SDHB cause
susceptibility to familial pheochromocytoma and to familial
paraganglioma. Am J Hum Genet. 69:49–54. 2001. View Article : Google Scholar
|
|
12
|
Kirmani S and Young WF: Hereditary
Paraganglioma-Pheochromocytoma Syndromes. Gene Reviews = Source
GeneReviews® [Internet]. Adam MP, Ardinger HH, Pagon RA,
Wallace SE, Bean LJH, Mefford HC, Stephens K, Amemiya A and
Ledbetter N: University of Washington; Seattle: 2008 Nov 6–2014
|
|
13
|
Unlü Y, Becit N, Ceviz M and Koçak H:
Management of carotid body tumors and familial paragangliomas:
Review of 30 years' experience. Ann Vasc Surg. 23:616–620. 2009.
View Article : Google Scholar
|
|
14
|
O'Neill S, O'Donnell M, Harkin D, Loughrey
M, Lee B and Blair P: A 22-year northern Irish experience of
carotid body tumours. Ulster Med J. 80:133–140. 2011.
|
|
15
|
Nazari I, Moghaddam FA, Zamani MM and
Salimi J: Clinical characteristics and remedies in 45 Iranians with
carotid body tumors. Acta Med Iran. 50:339–343. 2012.
|
|
16
|
Luna-Ortiz K, Rascon-Ortiz M,
Villavicencio-Valencia V, Granados-Garcia M and Herrera-Gomez A:
Carotid body tumors: Review of a 20-year experience. Oral Oncol.
41:56–61. 2005. View Article : Google Scholar
|
|
17
|
Sridhara SK, Yener M, Hnna EY, Rich T,
Jimenez C and Kupferman ME: Genetic testing in head and neck
paraganglioma: Who, what and why? J Neurol Surg B Skull Base.
74:236–240. 2013. View Article : Google Scholar
|
|
18
|
Ogawa K, Shiga K, Saijo S, Ogawa T, Kimura
N and Horii A: A novel G106D alteration of the SDHD gene in a
pedigree with familial paraganglioma. Am J Med Genet A.
140:2441–2446. 2006. View Article : Google Scholar
|
|
19
|
Kim ES, Kim SY, Mo EY, Jang DK, Moon SD
and Han JH: Novel germline SDHD mutation in a patient with
recurrent familial carotid body tumor and concomitant
pheochromocytoma. Head neck. 36:E131–E135. 2014. View Article : Google Scholar
|
|
20
|
Wang CP, Chen TC, Chang YL, Ko JY, Yang
TL, Lo FY, Hu YL, Chen PL, Wu CC and Lou PJ: Common genetic
mutations in the start codon of the SDH subunit D gene among
Chinese families with familial head and neck paragangliomas. Oral
Oncol. 48:125–129. 2012. View Article : Google Scholar
|
|
21
|
Kupferman ME and Hanna EY: Paragangliomas
of the head and neck. Curr Oncol Rep. 10:156–161. 2008. View Article : Google Scholar
|
|
22
|
Power AH, Bower TC, Kasperbauer J, Link
MJ, Oderich G, Cloft H, Young WF Jr and Gloviczki P: Impact of
preoperative embolization on outcomes of carotid body tumor
resections. J Vasc Surg. 56:979–989. 2012. View Article : Google Scholar
|
|
23
|
Torrealba JI, Valdés F, Krämer AH, Mertens
R, Bergoeing M and Mariné L: Management of carotid bifurcation
tumors: 30-year experience. Ann Vasc Surg. 34:200–205. 2016.
View Article : Google Scholar
|