Introduction
Doxorubicin (DOX) is an effective chemotherapeutic
agent that is widely used to treat numerous types of neoplasms.
However, serious cardiotoxic side effects, which may cause
arrhythmia and heart failure, limit its clinical application
(1–4).
Multiple mechanisms are involved in DOX cardiotoxicity, including
lipid peroxidation and decreased glutathione levels (5), calcium overloading and mitochondrial
dysfunction via increases in mitochondrial calcium and the
generation of reactive oxygen species (ROS) (6,7). Increased
oxidative stress and an antioxidant deficit serve key roles in
DOX-induced cardiotoxicity. Previous data suggests that the
dysregulation of calcium handling and mitochondrial function
contribute to DOX-induced cardiotoxicity (8). Multiple cardioprotective drugs may be
combined to eliminate its cardiotoxicity or reduce doses to an
acceptable level are expected to increase its efficacy (8). The majority of these attempts produced
beneficial effects, but the search for more effective strategies
against DOX-induced complications achieved little success (6). Therefore, additional adjuvant drugs are
co-administered with DOX to patients with neoplastic diseases to
reduce DOX-induced cardiotoxicity or enhance its therapeutic
effects (8).
Berberine (Ber) is an isoquinoline alkaloid that was
originally extracted from the traditional Chinese plant Coptis
chinensis (Huang Lian), and is an established treatment for
diarrhoea in traditional Chinese medicine (9). Ber exhibits a wide range of
pharmacological activities, including: Antioxidant properties to
attenuate reactive oxygen species (ROS) formation in various
tissues; anti-diabetic; anti-hyperlipidaemic; anti-inflammatory;
anti-tumour; and cardio-protective effects (9,10). We
hypothesized that the antioxidant and cardio-protective effects of
Ber may exhibit protective effects against DOX-induced
cardiomyopathy. The present experimental study investigated the
possible protective effects of Ber against acute DOX-induced
cardiotoxicity induced in a rat model. The effect of Ber on changes
in known indicators of cardiotoxicity and oxidative stress
including serum creatine kinase (CK), creatine kinase isoenzyme
(CK-MB) activities and serum and myocardial superoxide dismutase
(SOD), malondialdehyde (MDA) and catalase (CAT) contents was
investigated. The present study may support the utility of Ber as a
safe, clinically-approved drug in the treatment of cancer.
Materials and methods
Drugs and chemicals
DOX was provided by Lingnan Pharmaceutical, Ltd.
(Guangzhou, China). Ber was provided by Acros Organics (Geel,
Belgium). Fluo3-AM was purchased from Sigma-Aldrich; Merck KGaA
(Darmstadt, Germany). MDA, CAT and SOD assay kits were purchased
from Nanjing Jiancheng Bioengineering Institute (Nanjing, China).
CK and CK-MB assay kits were purchased from Sysmex Corporation
(Kobe, Japan). Rhodamine (Rh-123) and Rhod-2-acetoxymethyl
(rhod-2-AM) were purchased from Molecular Probes; Thermo Fisher
Scientific, Inc., (Waltham, MA, USA). The working solutions of
Harris Haematoxylin and eosin were purchased from Baso Diagnostics
Inc. Zhuhai (New Taipei City, Taiwan).
Animals and treatments
All experiments were performed in compliance with
the Guide for the Care and Use of Laboratory Animals (11) and were reviewed and approved by the
Ethics Committee for the Use of Experimental Animals at Hebei
Medical University (Shijiazhuang, China). Sprague-Dawley (SD) rats
weighing 200–250 g were obtained from the medical laboratory of
Hebei Medical University. The animals were acclimated to the
laboratory environment for 1 week in standard experimental
conditions (12 h light:12 h dark schedule) and allowed access to
food and water ad libitum. Animal experiments were performed
in accordance with the National Institutes of Health guidelines for
the experimental use of animals (11). Rats were randomly assigned to the
following five groups of 10 animals each: Water-treated (control)
group, DOX-treated group and DOX plus Ber treatment at doses of 5,
10 and 20 mg/kg. The control and DOX groups received distilled
water orally for 10 consecutive days. Ber was administered at the
aforementioned doses orally once daily for 10 consecutive days. The
dosing volume was 1 ml/100 g body weight. All rats were
intraperitoneally injected with a single dose of DOX 20 mg/kg on
day 8, with the exception of the control group. The selected dose
was based on our previous study (12).
Sample collection and biochemical
assays
All rats were anaesthetized 48 h after DOX
injection, and blood samples were collected prior to sacrifice.
Serum was separated for CK and CK-MB assays. The heart was quickly
isolated, blotted dry on filter paper, and weighed. The heart was
cut and prepared for histopathological examination, and one part
was prepared as 10% homogenates in ice-cold saline for the
determination of MDA, CAT activity and SOD contents. The total
protein content was detected with a bicinchoninic acid protein
Assay kit (Pierce, Thermo Fisher Scientific Inc.), and the
activities of MDA, CAT and SOD in the cardiac tissue were expressed
as units/mg protein.
Histopathological examinations
To analyse the histopathologic changes of the
cardiac tissue, one part of the heart was fixed in 10% buffered
formalin, embedded in paraffin and dehydrated in an ascending
series of ethanol (70, 80, 96, and 100%). Tissue samples were
embedded in paraffin and cut into 5-µm thick slices. The sections
were stained at room temperature with haematoxylin working solution
and 1% eosin (H&E) for 2 min respectively for histological
analysis under a light microscope (magnification, ×200, Olympus
BX-50; Olympus Corporation, Tokyo, Japan).
General toxicity observation
A total of 10 animals were used to determine
mortality in each group. The humane endpoints were a weight loss
above 15% of initial weight or animal in a state of prostration.
General conditions, mortality and body weight of the animals were
observed daily until the end of the experiment. Fluid accumulation
in the abdominal cavity was assessed at the end of the experiment
subsequent to abdominal opening and scored on a graded scale of 0
to 3+, where: 0, none; 1+, mild;
2+, moderate; and 3+, severe (13).
Acute isolation of cardiac
myocytes
Single cardiac myocytes were enzymatically isolated
from adult male rat hearts as described previously (14). Briefly, SD rats (200–250 g) were
anaesthetized using pentobarbital sodium (50 mg/kg,
intraperitoneally). The hearts were rapidly excised, mounted
through the aorta, and perfused on a modified Langendorff apparatus
with a calcium-free Tyrode solution at 37°C, followed by 0.6%
collagenase II in a Ca-free Tyrode solution to digest the heart.
Isolated ventricular myocytes were maintained in Krebs solution.
All experiments were performed within 6 h of ventricular myocyte
isolation.
Measurement of cytosolic calcium
concentration [Ca2+]i
Isolated myocytes were prepared as aforementioned
and loaded with 20 µmol/l membrane-permeable Fluo3-AM working
solution containing 0.03% pluronic F-127 at 37°C for 60 min. The
cells were superfused with fresh Tyrode solution three times at
25°C to allow de-esterification of Fluo3-AM. Cells were mounted in
a chamber on the stage of an inverted microscope. Only cells with a
rod shape and visible striations were used. Fluo3-AM fluorescence
in cells was excited at 488 nm, and fluorescence emission was
recorded at 530 nm using a photomultiplier. The fluorescence signal
was detected using a confocal laser scanning system (Leica TCS-SP
II; Leica Microsystems GmbH, Germany). Calcium measurement is
represented as relative fluorescence intensity
((FI-FI0)/FI0, %; FI0: Control;
FI: Administration of drugs). Cells were perfused with normal
Tyrode solution for 2 min and perfused with Tyrode solution
containing Ber for 15 min. A total of 50–100 images were scanned
from each cell, and the data were analysed by a confocal laser
microscopic system (Leica TCS SP2, Mannheim, Germany).
Mitochondrial Ca2+
concentration and membrane potential measurements
The mitochondrial membrane potential
(ΔΨm) was visualized in cardiomyocytes stained with the
fluorescent probe Rh-123. Myocytes were incubated with 0.5 µM
Rh-123 for 10 min at 37°C. Rh-123 fluorescence was detected at the
emission wavelength of 490 nm, and the green emission fluorescence
was excited at 530 nm to analyse ΔΨm. The mitochondrial
Ca2+ concentration [(Ca2+)m] was
measured using the Ca2+-sensing dye rhod-2-AM in loaded
cells. Myocytes were exposed to 10 µM rhod-2 acetoxymethyl ester
for 120 min at 4°C, and transferred to 37°C for an additional 30
min in the Tyrode solution (14).
Rhod-2 fluorescence was excited via excitation at 540 nm, and a 570
nm bandpass barrier filter was used to analyse
[Ca2+]m. The fluorescence signal was detected
using a confocal laser scanning system mentioned before. Regions of
rod-shaped cardiomyocytes were outlined/highlighted to represent
changes in fluorescence intensity over time, and the intensity of
the selected region of the image was analysed using a confocal
laser microscopic system. The fluorescence intensity was normalized
to the initial value (F0) recorded in normal Tyrode
solution in each experiment, and the density ratio represented the
relative fluorescence: (FI-FI0)/FI0 ×100,
where FI0 represents the control and FI represents the
drug-treated groups. Rat cardiomyocytes were treated with 0.1 or 1
µM Ber for 20 min and exposed to 1 µM DOX for 15 min, which is the
minimum time required for effective changes in
[Ca2+]m and ΔΨm (15).
Statistical analysis
All data are presented as the mean ± standard
deviation. Statistical tests were conducted using Microsoft Excel
2010 (version number, 14.0.4760.1000; Microsoft Corporation,
Redmond, WA, USA) and SPSS for windows (version 11.0; SPSS Inc.,
Chicago, IL, USA). Following a one-way analysis of variance,
quantitative data were analysed with post hoc contrasts by Fisher's
least significant difference test. A chi-squared test was used to
analyse the difference of the injury severity scores of the heart
among the various treatment groups. P<0.05 was considered to
indicate a statistically significant difference.
Results
Effects of Ber on animal body weight
and survival in DOX-induced cardiotoxicity
DOX treatment for two days reduced rat body weight
compared with the control group (235±35 vs. 266±15 g; P<0.01).
Treatment with 5, 10 and 20 mg/kg Ber exerted no marked increment
effects on body weight (231±36, 226±16 and 253±54 g, respectively;
P>0.05 vs. DOX alone). There was no significant difference in
the heart weight/body weight ratio between the five groups (3.0±0.4
mg/g in the control group vs. 3.1±0.3 mg/g in DOX treatment and
2.8±0.5, 3.3±0.3 and 2.9±0.3 mg/g in the Ber 5, 10, and 20 mg/kg
groups, respectively).
Effects of Ber on general toxicity in
DOX-induced cardiotoxicity
A total of 2 rats in the DOX-only treated group
succumbed 2 days following DOX injection. No mortality was observed
in the Ber+DOX-treated groups. All surviving rats in the DOX-only
treated group appeared weak, with scruffy fur and developed a
light-yellow tinge. These animals exhibited a significant decrease
in body weight compared to the Ber+DOX-treated groups. Notably,
these animals developed congestive heart failure, which manifested
as marked ascites during necropsy. The hallmark gross pathological
changes in DOX-only treated rats were excessive amounts of
pericardial, pleural and peritoneal fluids. The maximum ascites
volume exhibited by a single animal in DOX-only treated group was
11.5 ml. Compared with DOX alone (2.9±1.8%), the percentage of mean
maximum ascites volume to animal body weight were decreased
obviously in 5, 10 and 20 mg/kg Ber+DOX-treated groups (1.8±0.9,
1.0±0.1 and 1.4±1.1%: P<0.05, respectively). The effusion
intensity score was severe in 100% of the DOX-only treated animals
compared with 20–30% severe scores in the Ber+DOX groups (Table I).
 | Table I.Effect of Ber on DOX-induced
abdominal, pleural and pericardial effusion intensity scores in
surviving rats. |
Table I.
Effect of Ber on DOX-induced
abdominal, pleural and pericardial effusion intensity scores in
surviving rats.
|
|
| Effusion intensity
score |
|---|
|
|
|
|
|---|
|
|
| 0 | + | ++ | +++ |
|---|
|
|
|
|
|
|
|
|---|
| Group | n | N | % | N | % | N | % | N | % |
|---|
| Con | 10 | 10 | 100 | 0 | 0 | 0 | 0 | 0 | 0 |
| DOX | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 100a |
| Ber (5 mg/kg) | 10 | 0 | 0 | 4 | 40 | 3 | 30 | 3 | 30a,b |
| Ber (10 mg/kg) | 10 | 1 | 10 | 4 | 40 | 2 | 20 | 3 | 30a,b |
| Ber (20 mg/kg) | 10 | 1 | 10 | 5 | 50 | 2 | 33.3 | 2 | 20a,b |
Ber alleviates DOX-induced oxidative
damage
Serum CK-MB and CK levels are widely used as
clinical markers for oxidative stress, which indicate myocardial
injury (Table II). Oxidative stress
was evident in the cardiac myocytes of the DOX groups, with
significant increases in serum CK and CK-MB levels compared with
the control (P<0.01), and Ber treatment attenuated these
increases in a dose-dependent manner (P<0.05). CK and CK-MB
values in the Ber 10 and 20 mg/kg groups were almost equivalent to
control levels. Serum and heart tissues of DOX-only treated rats
revealed a significant increase in MDA and decreased CAT and SOD
contents compared to the control group. MDA, CAT and SOD
concentrations recovered markedly in the Ber+DOX groups compared to
the DOX-only group. However, 5 mg/kg Ber did not prevent the
DOX-induced increase in cardiac enzymes (Tables II and III).
 | Table II.Serum levels of CAT, SOD, MDA, CK,
and CK-MB activities following acute DOX intoxication and
protective activity by Ber. |
Table II.
Serum levels of CAT, SOD, MDA, CK,
and CK-MB activities following acute DOX intoxication and
protective activity by Ber.
| Group | n | CAT (U/ml) | SOD (U/ml) | MDA (mmol/ml) | CK (U/l) | CK-MB (U/l) |
|---|
| Con | 10 |
29.72±11.68 |
41.35±3.60 |
40.42±6.73 |
727±261 |
1,843±659 |
| DOX | 8 |
19.79±4.53a |
23.41±12.10b |
55.37±6.20b |
1,426±540b |
3,404±939b |
| Ber (5 mg/kg) | 10 |
28.53±7.72d |
36.44±9.65c |
46.93±7.90c |
1,069±366a |
2,694±571a |
| Ber (10 mg/kg) | 10 |
25.70±5.16c |
44.76±3.02a,d |
47.98±8.81c |
991±271c |
2,395±618c |
| Ber (20 mg/kg) | 10 |
27.51±10.20c |
41.51±3.77d |
40.47±18.21c |
792±378c |
2,123±865c |
 | Table III.Effect of Ber on peroxidative
alterations induced by acute DOX intoxication in rat cardiac
tissue. |
Table III.
Effect of Ber on peroxidative
alterations induced by acute DOX intoxication in rat cardiac
tissue.
| Group | n | CAT (U/mg
prot) | SOD (U/mg
prot) | MDA (nmol/mg
prot) |
|---|
| Con | 10 |
52.0±4.5 |
54.3±8.5 |
28.73±3.94 |
| DOX | 8 |
37.9±13.4b |
42.1±6.2b |
42.59±4.93b |
| Ber (5 mg/kg) | 10 |
48.3±9.9 |
46.15±7.25a |
42.50±7.22b |
| Ber (10 mg/kg) | 10 |
52.6±1.7d |
49.32±7.12c |
35.41±5.38a,d |
| Ber (20 mg/kg) | 10 |
52.9±2.6c |
50.97±6.77d |
33.00±1.15b,d |
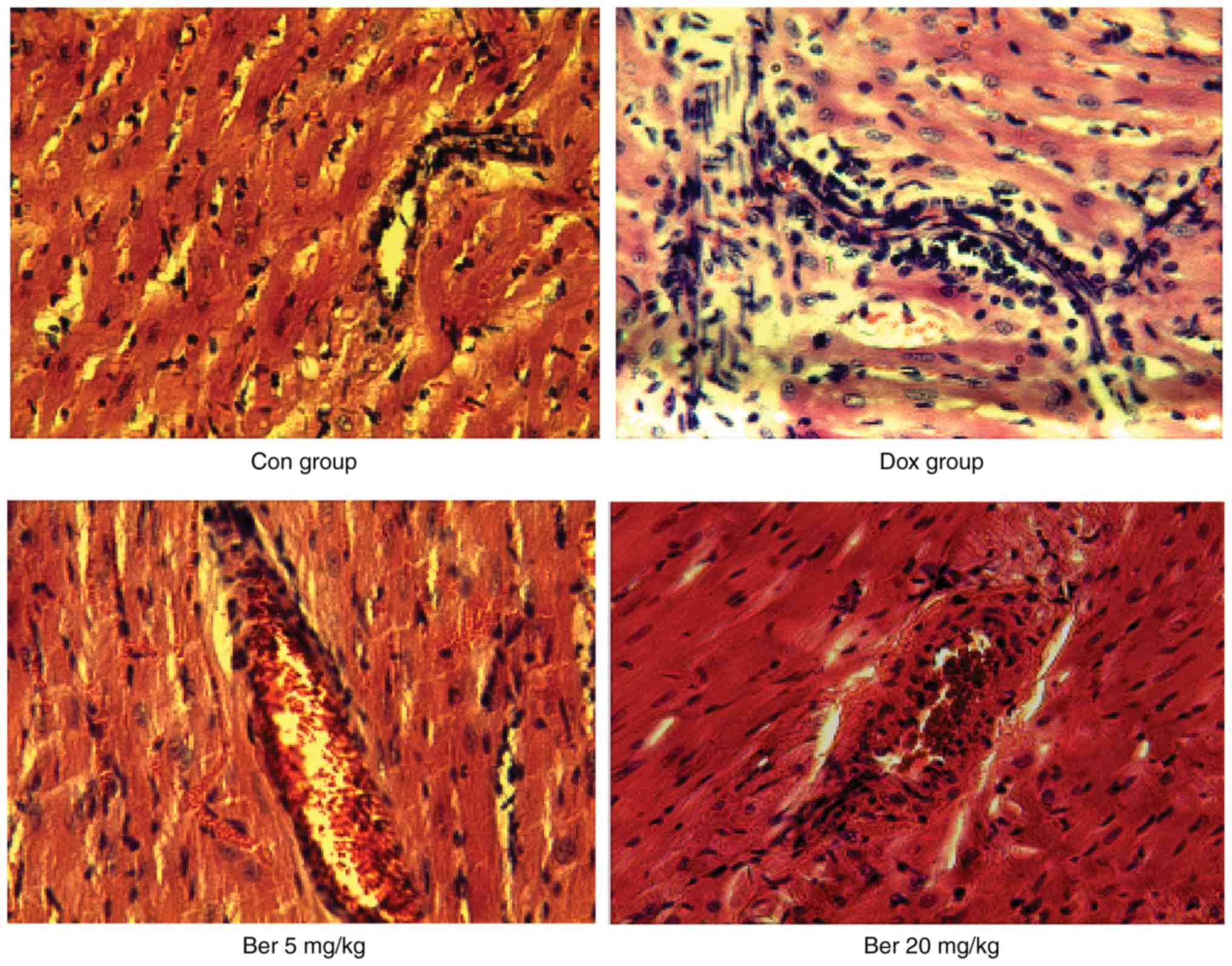
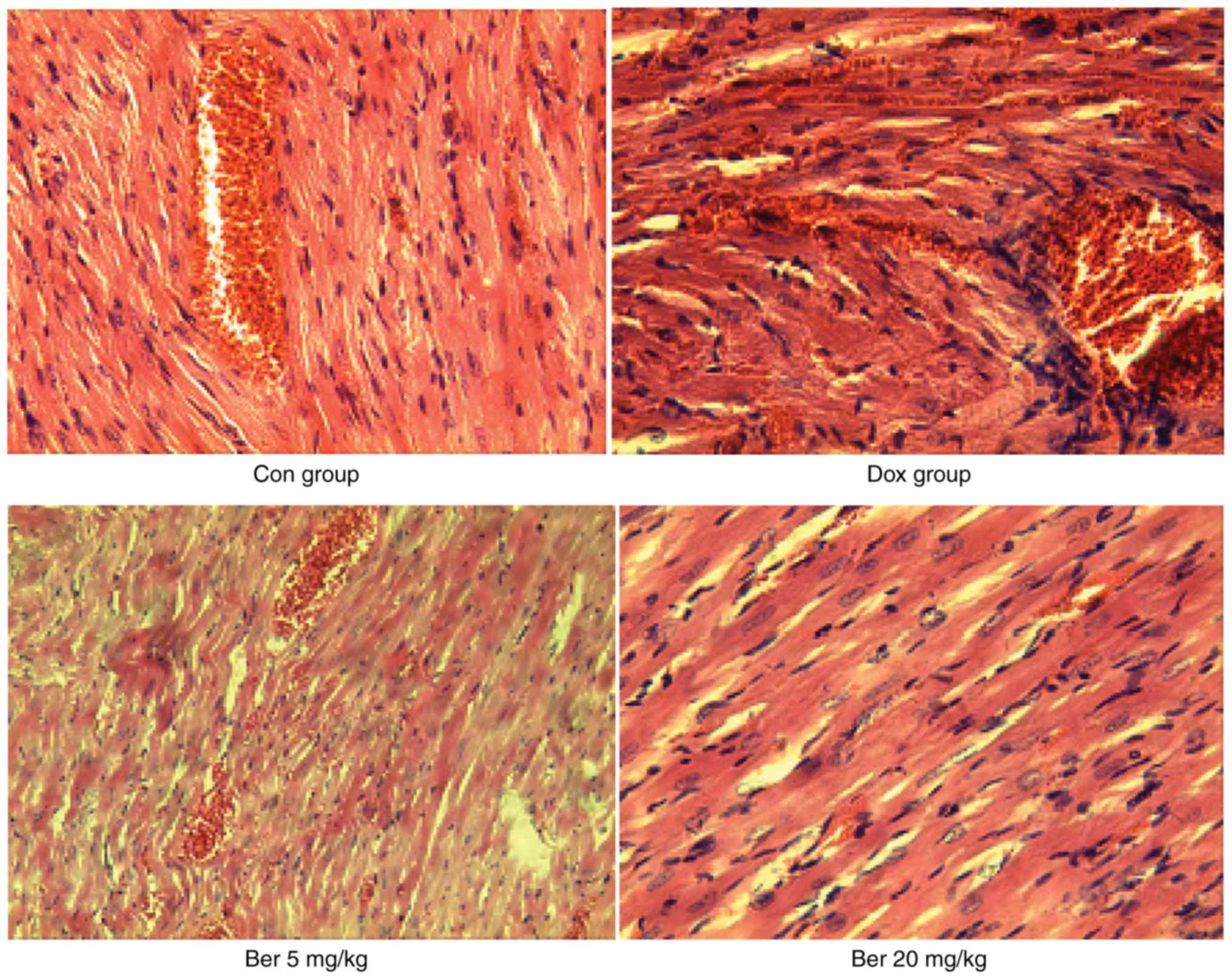
Histopathological examination
DOX-induced cardiotoxicity was additionally assessed
using H&E-stained sections. Heart tissue from the control
groups exhibited regular cell distribution and normal myocardium
architecture. Histological examination of cardiac sections using
H&E stain revealed that DOX induced cardiomyocyte cytoplasmic
vacuolization, interstitial oedema and inflammatory cell
infiltration. Myocardial lesions were attenuated in the Ber+DOX
groups compared to the DOX-alone group (Figs. 1 and 2).
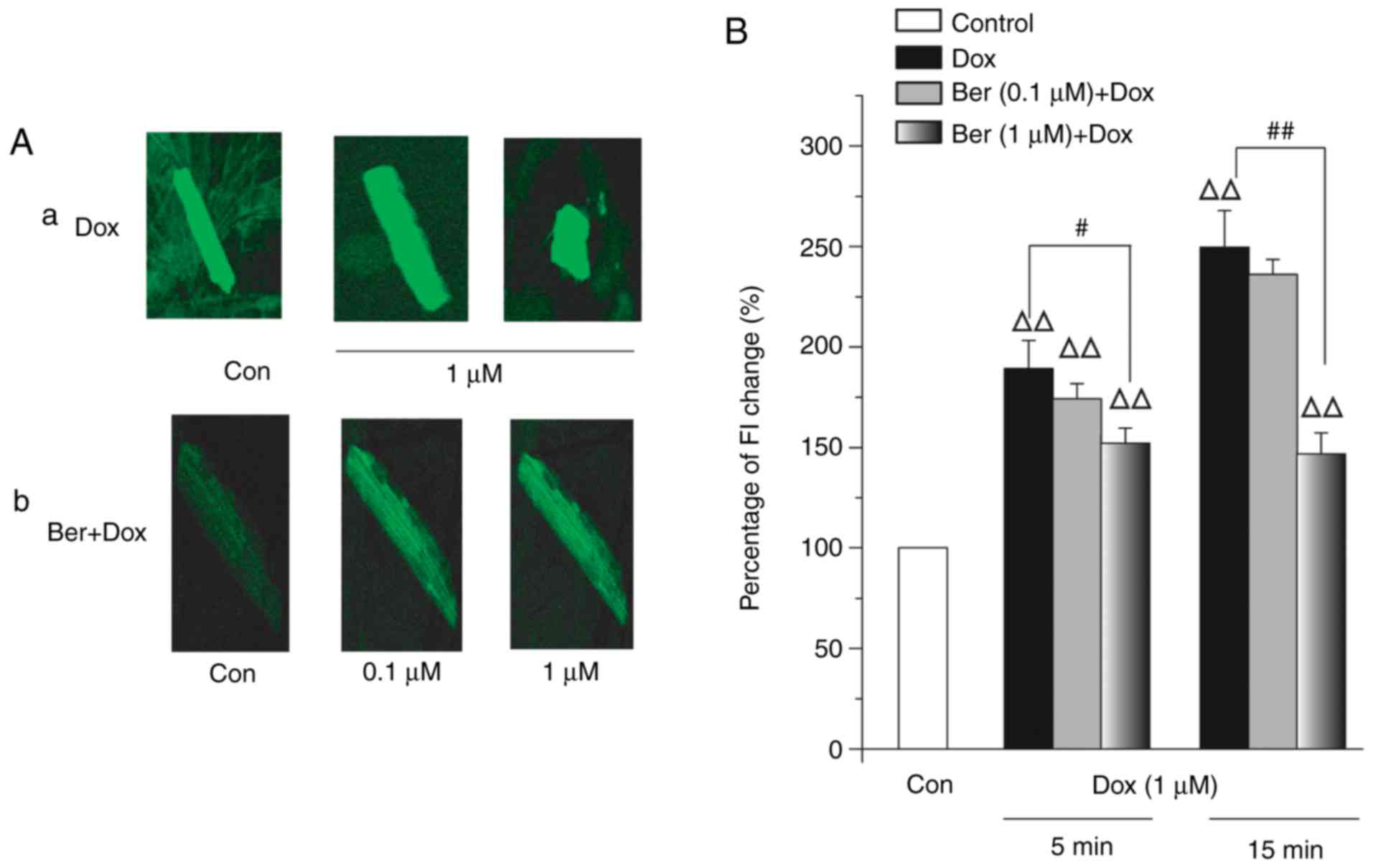
Effect of Ber on the DOX-induced
increase in [Ca2+]i
[Ca2+]i is critically
important in the contraction and relaxation of cardiomyocytes
(14). DOX-induced alterations in
Ca2+ homeostasis is one possible mechanism of
cardiotoxicity (15). Therefore, the
effect of DOX on [Ca2+]i in isolated
cardiomyocytes was examined using changes in the fluorescence
intensity of cardiomyocytes loaded with Fluo-3 AM. Fig. 3A demonstrates the effects of 1 µM DOX
on the increase in basal Fluo-3 fluorescence in the presence or
absence of 1 µM Ber in rat cardiomyocytes. Treatment of
cardiomyocytes with 1 µM DOX markedly increased
[Ca2+]i levels, and the cardiomyocytes
gradually became ‘rounded’ into a contracture state in 15 min
(Fig. 3A-a). However, the
cardiomyocytes treated with Ber did not become rounded (Fig. 3A-b). Fig.
3B summarizes the quantitative data. DOX (1 µM) increased
[Ca2+]i levels to 186.6±18.3% at 5 min and
252.1±11.1% at 15 min DOX, and the extent of the increase in
[Ca2+]i at 15 min was significantly >5 min
(P<0.05). Pre-treatment with 1 µM Ber significantly attenuated
the 1 µM DOX-induced elevation of [Ca2+]i to
150.6±4.7% at 5 min and 164.2±10.8% at 15 min. These results
demonstrated that DOX increased [Ca2+]i and
that Ber attenuated this increase.
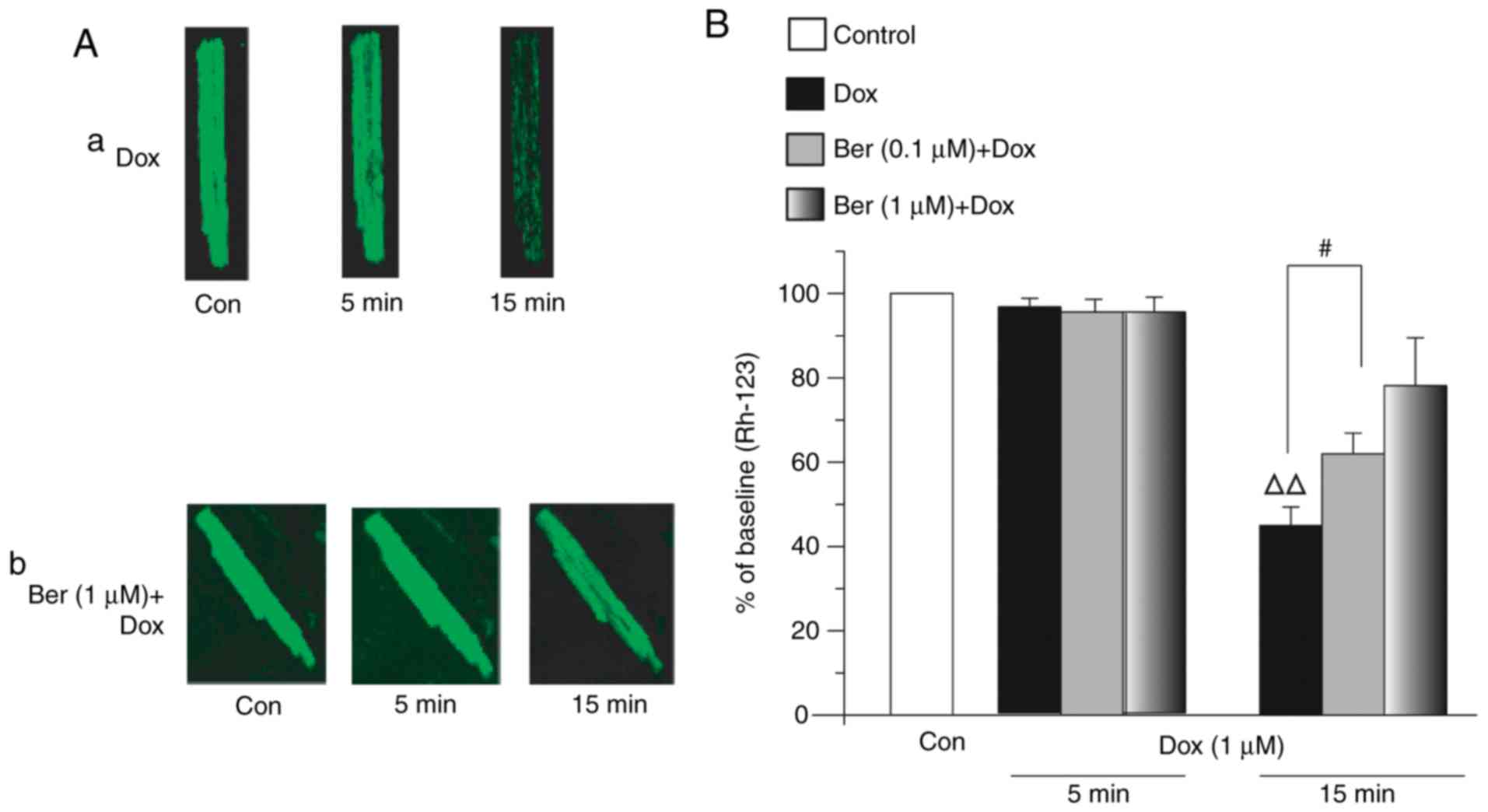
Effects of Ber on DOX-induced
ΔΨm
Mitochondria are involved in the maintenance of
Ca2+ homeostasis primarily due to their capacity to
buffer cytosolic Ca2+ (14,15).
ΔΨm is the central factor that controls the accumulation
of Ca2+ within the mitochondrial matrix, cell
respiration and ATP synthesis (14).
The measurement of ΔΨm is a powerful tool for evaluating
mitochondrial damage using the fluorescent probe Rhodamine 123
(Rh-123). Mitochondrial fluorescence intensity correlates
quantitatively with changes in ΔΨm (14). Therefore, the effects of DOX on
ΔΨm in rat ventricular myocytes were examined by
evaluating ΔΨm in cardiomyocytes using the Rh-123
staining assay. The corresponding changes in Rh-123 fluorescence
intensity in cardiomyocytes were measured 5 and 15 min following
perfusion of 1 µM DOX. Fig. 4A-a
indicates the confocal images of ΔΨm following cell
treatment for 15 min with 1 µM DOX. The results revealed that DOX
induced a marked decrease in mitochondrial membrane potential.
However, the pre-treatment of myocytes with 1 µM Ber significantly
restored the DOX-induced reduction in ΔΨm (P<0.05,
Fig. 4B) and attenuated the
DOX-induced decrease in Rh-123 fluorescence intensity (Fig. 4A-b). These results demonstrated that
Ber prevented the DOX-induced loss of the mitochondrial membrane
potential.
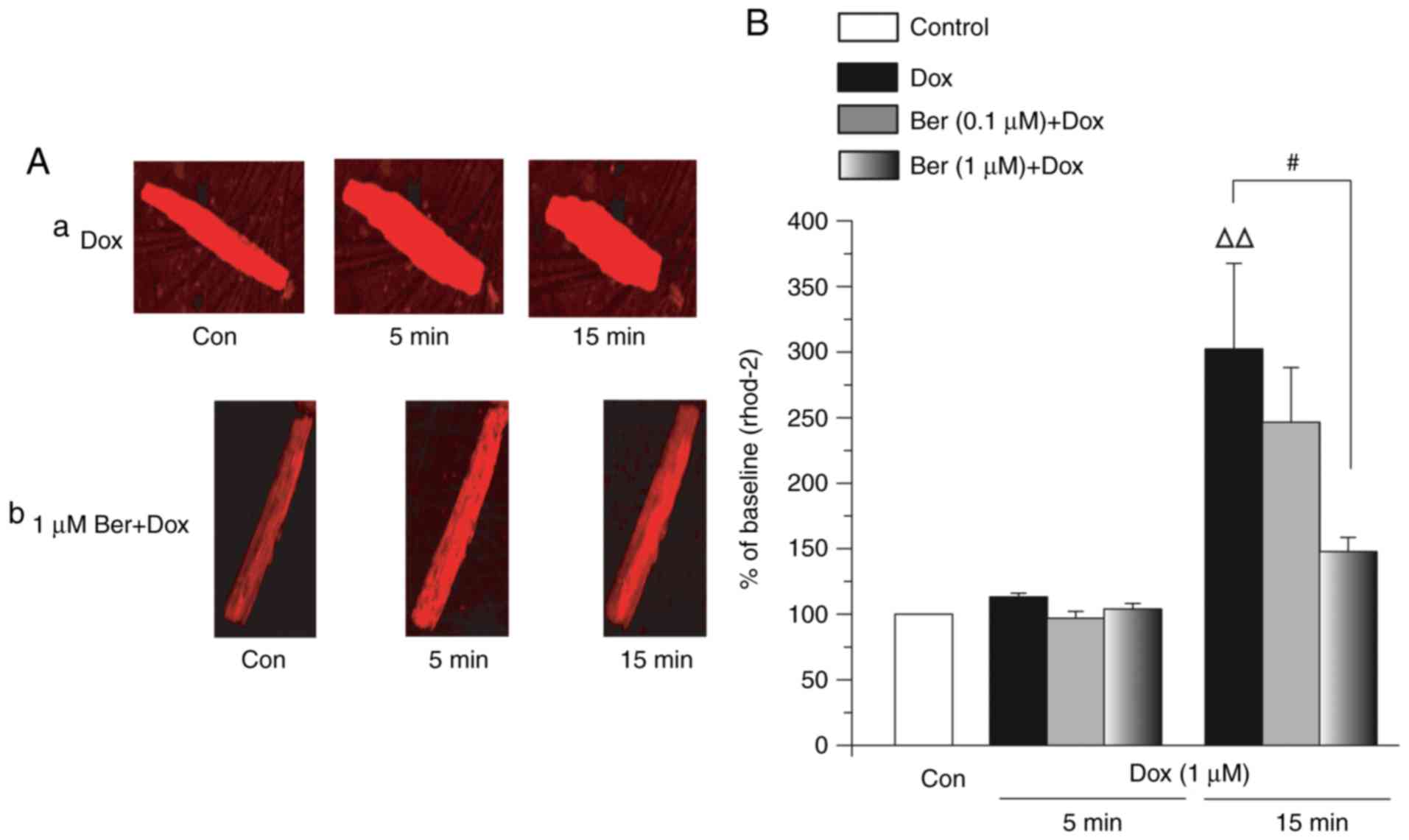
Effects of Ber on DOX-induced
[Ca2+]m overload
Ca2+ overload in mitochondria may lead to
mitochondrial dysfunction and be an important determinant of
myocyte toxicity (14). Whether Ber
attenuated the rise in DOX-induced [Ca2+]m
overload was investigated. Fig. 5A
demonstrates confocal images of rat ventricular myocytes loaded
with Rhod-2 in the presence or absence of 1 µM DOX or 1 µM DOX+1 µM
Ber. The resting [Ca2+]m in intact cells was
low, as revealed by the dim baseline signal of Rhod-2 fluorescence.
Treatment with 1 µM DOX significantly elevated
[Ca2+]m (Fig.
5A-a). Cells exhibited a high intensity of Rhod-2 fluorescence
in the presence of 1 µM DOX, and this fluorescence gradually
increased. However, pre-incubation with 1 µM Ber markedly decreased
the intensity of the DOX-induced rise in Rhod-2 fluorescence
(Fig. 5A-b). Fig. 5B suggests that Rhod-2 fluorescence
following 15 min of exposure to 1 µM DOX was 303.2±65.1% of the
baseline (P<0.001). Pre-incubation of 1 µM Ber apparently
lowered the 1 µM DOX-induced rise in Rhod-2 fluorescence, which was
reduced to 119.3±20.2% of the baseline (P<0.05). These data
indicate that the application of Ber prior to DOX treatment
prevented the elevation in mitochondrial Ca2+ overload
induced by DOX alone, and enabled normal mitochondrial
function.
Discussion
DOX is one of the most effective anti-tumour
antibiotics, and novel methods to reduce or prevent the cardiotoxic
side effects of DOX are expected. DOX-induced cardiotoxicity
manifests as acute effects (atrial and ventricular dysrhythmias)
that vary from transient electrocardiographic abnormalities to
dose-dependent cardiomyopathy and congestive heart failure
(15,16). A previous study of DOX cardiotoxicity
demonstrated that the single high-dose model is widely used since
it manifests certain characteristics of DOX-induced cardiotoxicity,
which is equivalent to a single high-dose injection in patients
with cancer (17).
Ber hydrochloride is an effective antioxidant and
free radical scavenger that prevents ROS formation and exerts
protective effects on cardiac, hepatic and renal functions
(18,19). Our previous study also demonstrated
that Ber exhibited a protective effect on DOX-induced acute
hepatorenal toxicity in rats (12).
Whether Ber exerts a protective effect against DOX-induced cardiac
injury is unknown. A number of cardioprotective agents, including
dexrazoxane, amifostine and probucol, are of limited value in
counteracting DOX cardiotoxicity and improving its clinical utility
(20,21). However, these scavengers exhibit
clinical disadvantages, including a diminished anti-tumour effect
and failure to protect the heart against DOX-induced injury in
clinical settings. Tong et al (22) revealed that Ber treatment potentiated
the sensitivity of cancer cells to DOX. Patil et al
(23) also demonstrated that Ber
suppressed tumour growth via the induction of apoptosis and cell
cycle arrest in cancer cells. Taken together, based on these data,
we hypothesized that combining DOX with Ber as a novel strategy for
tumour therapy would not only increase the effect of DOX, but also
prevent the cardiotoxicity induced by DOX. The present study
investigated the mechanism of the protective effects of Ber against
DOX-induced cardiotoxicity in rats. A rat model of DOX-induced
cardiotoxicity was developed in vivo and in vitro to
determine the potential protective action of Ber against the
cardiotoxic effects of DOX. The doses of Ber used in vivo
were those that has exhibited the maximum cardio-protective effect
in preliminary optimisation experiments (data not shown). Also,
this result is consistent with a previous study that indicated that
Ber demonstrated significant protective effects on heart tissue at
10 mg/kg in rats (24).
The data from the present study demonstrated that
DOX administration was accompanied by a high mortality compared
with the control group. Surviving animals suffered from an
excessive degree of pericardial, pleural and peritoneal effusion,
which indicated severe cardiac injury. The ability of Ber to
protect against DOX-induced high mortality and effusion intensity
score was considered an early sign of cardio-protection (25). Ber also attenuated DOX-induced
histopathological and ultrastructural deteriorations. These data
indicate that Ber is a potential protective agent against DOX
injury. Oxidative damage and antioxidant deficiencies in
cardiomyocytes are widely implicated as a primary cause for
DOX-induced cardiac toxicity (1,15), and
these factors were utilized in the present study to examine the
oxidant/antioxidant status of the rats. We used the single
high-dose model and investigated whether Ber protected the heart
from acute DOX toxicity. The current data demonstrated that cardiac
and serum levels of MDA, CK and CK-MB were significantly elevated,
and that the activities of the cardiac antioxidant enzymes CAT and
SOD were significantly reduced, following DOX administration
compared to the control group. These data clearly indicate a status
of overt oxidative stress. Ber significantly decreased the
DOX-associated elevation of serum MDA, CK and CK-MB activities,
which are classical biomarkers of cardiotoxicity (4). It is well-known that the expression
levels of B-type natriuretic peptide (BNP) and troponins are
specific and sensitive indicators for cardiac damage (20). However, in the present study, severe
cardiac damage induced by doxorubicin was observed, manifested by
marked ascites and notable symptom of congestive heart failure.
Since it was sufficient to analyse the cardiotoxicity by detecting
CK and CK-MB levels in serum, it was not necessary to measure the
expression levels of BNP and troponins. Nevertheless, means of
measuring the expressions of BDP and troponins will be included in
future studies, for full clarification of the protective mechanism
of Ber on DOX-induced cardiotoxicity. The activities of CAT and SOD
were significantly elevated in BER+DOX-treated groups compared with
DOX-only administration in rats. These data are consistent with the
current understanding of elevated cardiac lipid peroxidation
accompanied by deteriorating antioxidant status was evident in the
DOX-only treated rats. Ber pre-treatment significantly alleviated
the oxidative stress in the DOX group, and Ber therapy completely
prevented the biochemical and histopathological deteriorations
caused by DOX These results suggest that Ber therapy during DOX
treatment for cancer significantly protected the heart against
DOX-induced injury. These data are in agreement with a study by
Chen et al (12) and Hao et
al (26). The initial damage of
DOX-induced cardiotoxicity is likely oxidative in nature as it
undergoes a one-electron reduction, resulting in the corresponding
semiquinone, to form free radicals and superoxide radicals
(27).
Oxidative damage to the cardiac mitochondria and
cardiomyocyte is a cornerstone of DOX-induced cardiotoxicity, but a
previous study suggested calcium overload as an additional
important mechanism of DOX-induced cardiotoxicity (28). Previous studies have demonstrated that
DOX opened sarcoplasmic reticulum calcium release channels and
increased the maximal amount of calcium release (29,30),
inhibited Na+-Ca2+ exchange (31) or activated the L-type cardiac calcium
channel (32). DOX may lead to
calcium overload in cardiac cells, causing inadequate contraction
and impairing mitochondrial calcium homeostasis, which alters
energy metabolism and the generation of ROS (33) and may trigger the calcium-dependent
mitochondrial permeability transition via opening of the
permeability transition pores (14,15). The
opening of these pores induces the release of cytochrome c, which
is a critical step for apoptosis (34,35).
Mitochondria are key targets for anthracycline cardiotoxicity
(36,37), and may also be crucial for effective
cardio-protection. The decrease in ΔΨm reduced the
capacity for Ca2+ influx into mitochondria, as
ΔΨm primarily drives mitochondrial calcium uptake
(38). Therefore, the present study
investigated intracellular calcium and mitochondrial calcium in
cardiac myocytes following DOX treatment, and examined whether the
protective effect of Ber on DOX-induced Ca2+ overload
was associated with ΔΨm depolarization. The results
demonstrated that the high local [Ca2+]i
level produced by DOX caused mitochondrial Ca2+ overload
and a decrease in ΔΨm, which may alter cardiac
metabolism and lead to cardiomyocyte death. Incubation with Ber for
1 h significantly reduced mitochondrial Ca2+ overload
and significantly elevated cardiac energy metabolism. Ber treatment
significantly suppressed the DOX-induced increase in
[Ca2+]i. These results demonstrate that Ber
inhibited the DOX-induced acute modifications in calcium
homeostasis in cardiomyocytes, and suggest a protective role of Ber
against DOX-induced cardiotoxicity. A previous study demonstrated
that Ber may also attenuate DOX-induced cardiomyocyte apoptosis by
inhibiting caspase-3 activation, adenosine 5′-monophosphate
activated protein kinase α and tumour protein 53 phosphorylation
(39). Ber is a potential candidate
agent for co-administration with DOX to ameliorate its
cardiotoxicity. Additional studies are required to thoroughly
evaluate the potential protective effect of Ber in DOX-induced
cardiotoxicity.
Acknowledgements
The authors would like to thank Professor Lian-Shan
Zhang (Department of Pathology, Hebei Medical University,
Shijiazhuang, China) for her help in histopathological analysis of
the cardiac tissues.
Funding
The present study was supported by the Natural
Science Foundation of China (grant nos. 81273600, 81302773 and
81773828) and the Natural Science Foundation of Hebei Province
(grant nos. C2011206145, H2014206319 and H2018206297).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SWS and CX conceived and designed the study. YZ, CX,
ZXW, YZW, XYC, HCG, KRX, KXW, and PJ performed the experiments. CX,
YZ, YZW, and SWS wrote the paper. SWS and CX reviewed and edited
the manuscript. All authors read and approved the manuscript.
Ethics approval and consent to
participate
All experiments were performed in compliance with
the Guide for the Care and Use of Laboratory Animals and were
reviewed and approved by the Ethics Committee for the Use of
Experimental Animals at Hebei Medical University (Shijiazhuang,
China).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
DOX
|
doxorubicin
|
|
Ber
|
berberine
|
|
ROS
|
reactive oxygen radical species
|
|
ΔΨm
|
mitochondrial membrane potential
|
|
CK
|
creatine kinase
|
|
CK-MB
|
creatine kinase isoenzyme
|
|
MDA
|
malondialdehyde
|
|
SOD
|
superoxide dismutase
|
|
CAT
|
catalase
|
References
|
1
|
Duggan ST and Keating GM: Pegylated
liposomal doxorubicin: A review of its use in metastatic breast
cancer, ovarian cancer, multiple myeloma and AIDS-related Kaposi's
sarcoma. Drugs. 71:2531–2558. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cortés-Funes H and Coronado C: Role of
anthracyclines in the era of targeted therapy. Cardiovasc Toxicol.
7:56–60. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Minotti G, Menna P, Salvatorelli E, Cairo
G and Gianni L: Anthracyclines: Molecular advances and
pharmacologic developments in antitumor activity and
cardiotoxicity. Pharmacol Rev. 56:185–229. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhang YY, Yi M and Huang YP: Oxymatrine
ameliorates doxorubicin-induced cardiotoxicity in rats. Cell
Physiol Biochem. 43:626–635. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bordoni A, Biagi P and Hrelia S: The
impairment of essential fatty acid metabolism as a key factor in
doxorubicin-induced damage in cultured rat cardiomyocytes. Biochim
Biophys Acta. 1440:100–106. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chatterjee K, Zhang J, Honbo N and
Karliner JS: Doxorubicin cardiomyopathy. Cardiology. 115:155–162.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Christiansen S: Clinical management of
doxorubicin-induced heart failure. J Cardiovasc Surg (Torino).
52:133–138. 2011.PubMed/NCBI
|
|
8
|
Ludke AR, Al-Shudiefat AA, Dhingra S,
Jassal DS and Singal PK: A concise description of cardioprotective
strategies in doxorubicin-induced cardiotoxicity. Can J Physiol
Pharmacol. 87:756–763. 2009.PubMed/NCBI
|
|
9
|
Tan HL, Chan KG, Pusparajah P, Duangjai A,
Saokaew S, Mehmood Khan T, Lee LH and Goh BH: Rhizoma coptidis: A
potential cardiovascular protective agent. Front Pharmacol.
7:362.eCollection 20162016. View Article : Google Scholar
|
|
10
|
Tabeshpour J, Imenshahidi M and
Hosseinzadeh H: A review of the effects of Berberis vulgaris and
its major component, berberine, in metabolic syndrome. Iran J Basic
Med Sci. 20:557–568. 2017.PubMed/NCBI
|
|
11
|
National Research Council (US) Committee
for the Update of the Guide for the Care and Use of Laboratory
Animals = Guide for the Care and Use of Laboratory Animals. 8th.
Washington (DC): National Academies Press (US); 2011
|
|
12
|
Chen X, Zhang Y, Zhu Z, Liu H, Guo H,
Xiong C, Xie K, Zhang X and Su S: Protective effect of berberine on
doxorubicin induced acute hepatorenal toxicity in rats. Mol Med
Rep. 13:3953–3960. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kelishomi RB, Ejtemaeemehr S, Tavangar SM,
Rahimian R, Mobarakeh JI and Dehpour AR: Morphine is protective
against doxorubicin-induced cardiotoxicity in rat. Toxicology.
243:96–104. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xiong C, Li JX, Guo HC, Zhang LN, Guo W,
Meng J and Wang YL: The H1-H2 domain of the
α1 isoform of Na+-K+-ATPase is involved in ouabain toxicity in rat
ventricular myocytes. Toxicol Appl Pharmacol. 262:32–42. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Asensio-López MC, Soler F, Pascual-Figal
D, Fernández-Belda F and Lax A: Doxorubicin-induced oxidative
stress: The protective effect of nicorandil on HL-1 cardiomyocytes.
PLoS One. 12:e01728032017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jain D, Ahmad T, Cairo M and Aronow W:
Cardiotoxicity of cancer chemotherapy: Identification, prevention
and treatment. Ann Transl Med. 5:3482017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li T, Danelisen I and Singal PK: Early
changes in myocardial antioxidant enzymes in rats treated with
adriamycin. Mol Cell Biochem. 232:19–26. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lee IA, Hyun YJ and Kim DH: Berberine
ameliorates TNBS-induced colitis by inhibiting lipid peroxidation,
enterobacterial growth and NF-κB activation. Eur J Pharmacol.
648:162–170. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li P, Ren J, Duan C, Lin C and Liu J:
Effects of four components of Rhizoma Corydalis on anoxia and
peroxidation injuries in neonatal cardiomyocytes. Zhongguo Zhong
Yao Za Zhi. 35:84–88. 2010.(In Chinese). PubMed/NCBI
|
|
20
|
Che FF, Liu Y and Xu CG: Schisandrin B
prevents doxorubicin-induced cardiotoxicity in rabbits. Sichuan Da
Xue Xue Bao Yi Xue Ban. 41:24–28. 2010.(In Chinese). PubMed/NCBI
|
|
21
|
Li T and Singal PK: Adriamycin-induced
early changes in myocardial antioxidant enzymes and their
modulation by probucol. Circulation. 102:2105–2110. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tong N, Zhang J, Chen Y, Li Z, Luo Y, Zuo
H and Zhao X: Berberine sensitizes mutliple human cancer cells to
the anticancer effects of doxorubicin in vitro. Oncol Lett.
3:1263–1267. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Patil JB, Kim J and Jayaprakasha GK:
Berberine induces apoptosis in breast cancer cells (MCF-7) through
mitochondrial-dependent pathway. Eur J Pharmacol. 645:70–78. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang YJ, Yang SH, Li MH, Iqbal J,
Bourantas CV, Mi QY, Yu YH, Li JJ, Zhao SL, Tian NL and Chen SL:
Berberine attenuates adverse left ventricular remodeling and
cardiac dysfunction after acute myocardial infarction in rats: Role
of autophagy. Clin Exp Pharmacol Physiol. 41:995–1002. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Takemura G and Fujiwara H:
Doxorubicin-induced cardiomyopathy from the cardiotoxic mechanisms
to management. Prog Cardiovasc Dis. 49:330–352. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hao G, Yu Y, Gu B, Xing Y and Xue M:
Protective effects of berberine against doxorubicin-induced
cardiotoxicity in rats by inhibiting metabolism of doxorubicin.
Xenobiotica. 45:1024–1029. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang S, Konorev EA, Kotamraju S, Joseph J,
Kalivendi S and Kalyanaraman B: Doxorubicin induces apoptosis in
normal and tumor cells via distinctly different mechanisms.
Intermediacy of H(2)O(2)- and p53-dependent pathways. J Biol Chem.
279:25535–25543. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Solem LE, Henry TR and Wallace KB:
Disruption of mitochondrial calcium homeostasis following chronic
doxorubicin administration. Toxicol Appl Pharmacol. 129:214–222.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zorzato F, Sarviati G, Facchinetti T and
Volpe P: Doxorubicin induces calcium release from terminal
cisternae of skeletal muscle. A study on isolated sarcoplasmic
reticulum and chemically skinned fibers. J Biol Chem.
260:7349–7355. 1985.PubMed/NCBI
|
|
30
|
Kim DH, Landry AB III, Lee YS and Katz AM:
Doxorubicin-induced calcium release from sarcoplasmic reticulum
vesicles. J Moll Cell Cardiol. 21:433–436. 1989. View Article : Google Scholar
|
|
31
|
Caroni P, Villani F and Carafoli E: The
cardiotoxic antibiotic doxorubicin inhibits the Na+/Ca2+ exchange
of dog heart sarcolemmal vesicles. FEBS Lett. 130:184–186. 1981.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Keung EC, Toll L, Ellis M and Jensen RA:
L-type cardiac calcium channels in doxorubicin cardiomyopathy in
rats morphological, biochemical, and functional correlations. J
Clin Invest. 87:2108–2113. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Przygodzki T, Sokal A and Bryszewska M:
Calcium ionophore A23187 action on cardiac myocytes is accompanied
by enhanced production of reactive oxygen species. Biochim Biophys
Acta. 1740:481–488. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Petrosillo G, Ruggiero FM, Pistolese M and
Paradies G: Ca2+-induced reactive oxygen species production
promotes cytochrome c release from rat liver mitochondria via
mitochondrial permeability transition (MPT)-dependent and
MPT-independent mechanisms: Role of cardiolipin. J Biol Chem.
279:53103–53108. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Waring P: Redox active calcium ion
channels and cell death. Arch Biochem Biophys. 434:33–42. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Li L, Takemura G, Li Y, Miyata S, Esaki M,
Okada H, Kanamori H, Khai NC, Maruyama R, Ogino A, et al:
Preventive effect of erythropoietin on cardiac dysfunction in
Doxorubicin-induced cardiomyopathy. Circulation. 113:535–543. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yeh YC, Lai HC, Ting CT, Lee WL, Wang LC,
Wang KY, Lai HC and Liu TJ: Protection by doxycycline against
doxorubicin-induced oxidative stress and apoptosis in mouse testes.
Biochem Pharmacol. 74:969–980. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Rahn CA, Bombick DW and Doolittle DJ:
Assessment of mitochondrial membrane potential as an indicator of
cytotoxicity. Fundam Appl Toxicol. 16:435–448. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Lv X, Yu X, Wang Y, Wang F, Li H, Wang Y,
Lu D, Qi R and Wang H: Berberine inhibits doxorubicin-triggered
cardiomyocyte apoptosis via attenuating mitochondrial dysfunction
and increasing Bcl-2 expression. PLoS One. 7:e473512012. View Article : Google Scholar : PubMed/NCBI
|