Introduction
Thoracic malignancies are the most common types of
cancer globally (1,2). One of the primary treatments for this
type of malignancy is radiotherapy (3). It is known that the fundamental
principle of radiotherapy is to deliver an accurate therapeutic
dose to the tumor tissue and avoid excessive radiation exposure to
the adjacent normal tissues, thus increasing local tumor control
probability (TCP) and decreasing normal tissue complication
probability (NTCP) (4).
Conventionally, thoracic radiotherapy is planned using
three-dimensional conformal radiotherapy (3D-CRT) and
intensity-modulated radiation therapy (IMRT) (3). Recently, volumetric-modulated arc
therapy (VMAT) has become a focus of studies worldwide due to its
increased delivery efficiency over 3D-CRT and IMRT (5); however, a number of studies have
reported controversial findings on the conformity of targets and
the protection of healthy structures in thoracic radiotherapy
(6–8).
This can be attributed to interpatient diversity and the
contrasting definition of the target in different radiotherapy
centers. The evaluation and comparison of the quality and efficacy
of distinct radiotherapy strategies remains challenging (9).
Staging of involved mediastinal lymph nodes (MLNs)
serves a function in determining the treatment strategy and overall
patient prognosis (10). In 1996, the
American Thoracic Society and American Joint Committee for Cancer
(AJCC) proposed a criterion to divide intrathoracic lymph nodes
(ITLN) into groups, nine categorized as MLNs and the other five
within the hilus and lobe of the lung group (11). The Union for International Cancer
Control and the International Association for the Study of Lung
Cancer also support this classification of ITLN (12,13);
however, the method to clearly recognize and localize MLNs, and to
distinguish them from adjacent structures remains a clinical
problem. In a clinical setting, current identification of MLNs
primarily involves 2D white-gray imaging, including computed
tomography (CT), magnetic resonance imaging (MRI) and positron
emission tomography-CT, which is inefficient at distinguishing MLNs
from blood vessels, muscles and soft tissues (14). The Chinese Visible Human (CVH) dataset
has been established by Third Military Medical University
(Chongqing, China) (15,16); thus, 3D reconstruction of high-quality
MLN images and thoracic structures has become possible. Images of
CVH dataset sections were captured in high structural and spatial
resolutions, and CVH images demonstrated advantages, including high
resolution, lack of deformation, high articulation and thinness of
section, compared with medical images. Thus, the CVH dataset has
been frequently used as a tool to construct 3D medical models to
discern miniscule structures; for example, 3D thorax models have
been reconstructed based on the CHV1 dataset as a learning tool for
interpreting human thoracic anatomy and virtual thoracic and
cardiovascular surgery for medical students and junior surgeons
(17). Furthermore, the CVH head
dataset has been used as a brain atlas for locating the subthalamic
nucleus prior to deep brain stimulation surgery (18). However, no 3D MLN models or similar
tools have been used in previous studies, to the best of our
knowledge.
It has been previously demonstrated that the modern
treatment planning system (TPS) is able to accurately predict the
patient dose (19); however, the
actual absorbed doses generally deviate from calculated doses in a
certain range. The accurate absorbed doses of regions of interest
(ROIs), including planning target volume (PTV) and organs at risk
(OARs), cannot be obtained from a patient receiving radiotherapy
(20,21). Therefore, a standard method is
required to measure the in vivo radiation doses, which may
be explored by a simulation. The present study attempts to improve
the plan evaluation and dosimetric measurement using a constructed
visual model.
In the present study, a 3D MLN digital model was
constructed based on the CVH dataset to use as a virtual tool to
assist in obtaining improved contours of lymph nodes, and to
optimize the plan in TPS and dosimetric measurement of the Chengdu
Dosimetric Phantom (CDP), a state-of-the-art heterogeneous phantom
(22). The CDP is a novel radiation
phantom of a person of medium-build and Chinese origin, with a
height of 170 cm and a weight of 65 kg (22). CDP was named by the International
Commission of Radiation Units and Measurements (report 48) and has
been accepted internationally (23).
Similar to other radiation phantoms, the CDP possesses a humanoid
shape (24). The CDP is composed of
the material with the same ratio of atomic elements as real human
bodies (25); therefore, it is
bioequivalent with human beings in irradiation, energy transfer and
radiation distribution, and is regarded as an avatar to assess
damage in reality (25). All of these
characteristics of the CDP can be combined with a 3D MLN model for
dosimetric measurement in thoracic radiotherapy.
The hypothesis of the present study was that the CVH
dataset and CDP phantom could be combined to build a 3D MLN model,
which could be used to test the quality of thoracic radiotherapy
plans. The results may provide implications for clinical
practice.
Materials and methods
Image segmentation of the CVH
dataset
The CVH female dataset (CVH2), available at
http://www.chinesevisiblehuman.com,
was selected for the 3D reconstruction of MLNs. The CVH2 cadaver
was 22 years old at mortality, 162 cm in height, 54 kg in weight
and free of organic lesions. The subject was sectioned in axial
planes, and high-resolution anatomic images were acquired. The
complete series of anatomical images constitute the CVH2, with each
slice 0.5 mm in thickness and a resolution of 3,072×2,048 pixels
(16). The high-resolution
cryosectional color photographic images were captured using a
high-definition digital camera. A total of 380 images of the
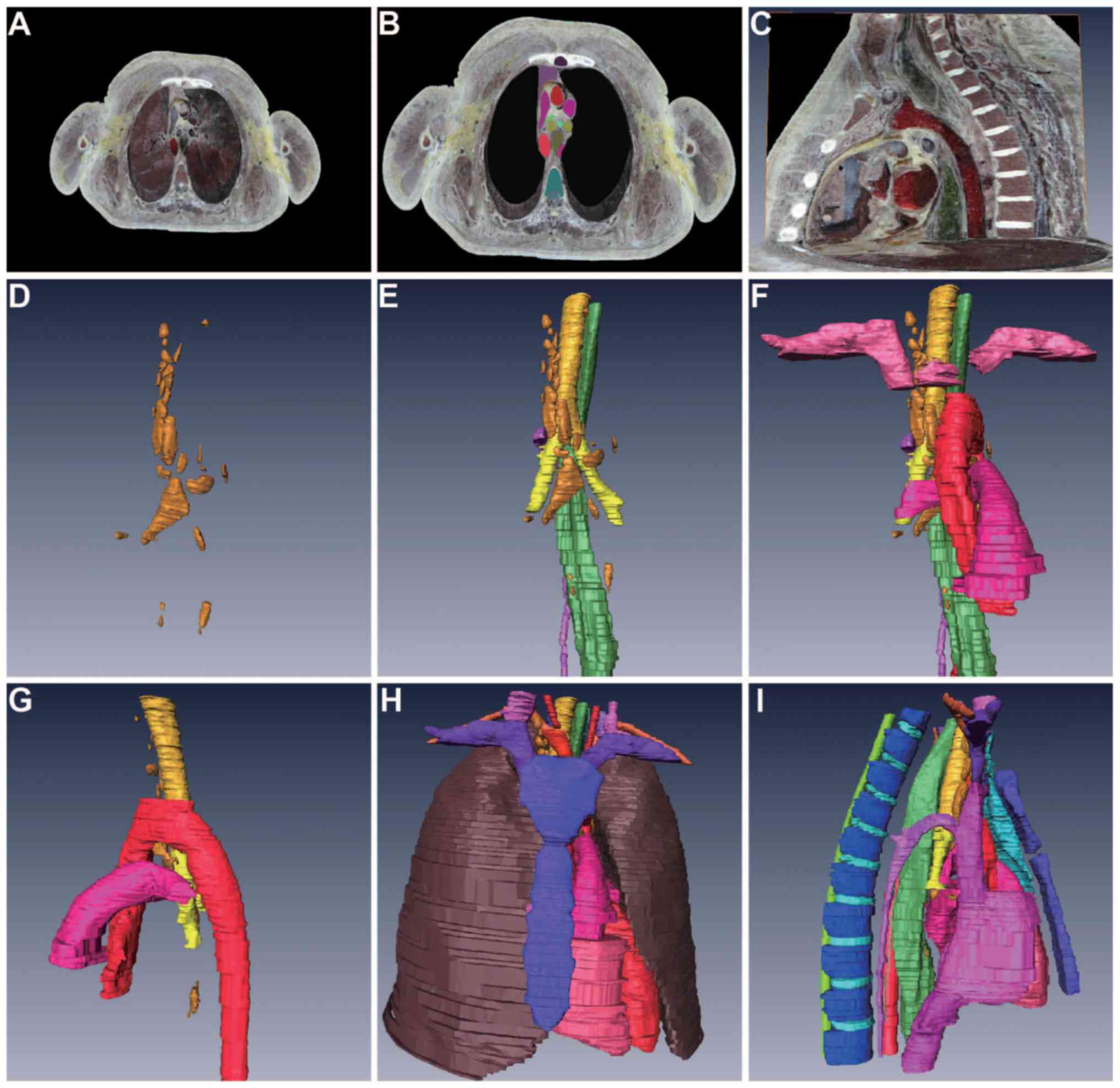
mediastinum (Fig. 1A) were imported
into the Photoshop CS software (version 3.0; Adobe Systems, Inc.,
Sam Jose, CA, USA) for editing, including contouring MLN stations.
An expert anatomist and a physician contoured and segmented the
1st-8th MLN stations on every layer manually, ranging from the
sternum to the thoracic vertebrae and from the supraclavicular area
to the bottom of the lungs. The adjacent MLN structures were also
contoured, including the esophagus, trachea, left and right
bronchi, thymus, sternum, thoracic duct and vertebrae, spinal cord,
thoracic great vessels and heart. Every structure was then awarded
different red, green and blue values and filled with different
colors (Fig. 1B). The layers were
established and input one by one in order to complete the 3D
reconstruction.
Surface and volume
reconstructions
Surface and volume reconstructions were performed as
previously described (17). Briefly,
the original images in PSD format were converted to PNG format with
Photoshop CS. The color images were converted to grayscale mode and
imported into the Amira program (version 5.2.2; Thermo Fisher
Scientific, Inc., Waltham, MA, USA). Threshold segmentation was
used to extract the data of different anatomical structures, and
then surface reconstruction was applied to gain the surface model
of these anatomical structures. As for volume reconstruction, the
original sectional images in PNG format were cut appropriately by
Photoshop CS and imported into the Amira program. According to the
‘Orthoslice’ and ‘Oblique Slice’ commands, random sections were
acquired through virtual cutting, including coronal and sagittal
planes, or in any angle or layer of the target structures. MATLAB
software (version 8.1; MathWorks, Natick, MA, USA) was used to
convert CVH images into the Digital Imaging and Communications in
Medicine (DICOM) format.
Image registration and fusion in
TPS
The CVH2 cadaver underwent imaging acquisition
procedures via a CT scan and standard radiological imaging. Chest
CT images were also obtained. The chest CT images and MLN images in
DICOM format were imported to the Eclipse™ TPS (version 8.3; Varian
Medical System. Inc., Palo Alto, CA, USA). Rigid alignment was
performed following the selection of four points on the bony
landmarks. The procedure was repeated automatically three to five
times in order to obtain the best fused images.
Formulation of the plan for thoracic
radiotherapy in a 3D MLN model
Fused images were transferred into Eclipse TPS for
radiotherapy plan formulation. One virtual simulated lung lesion
(SLL) was produced for each case in a 3D MLN model in Eclipse TPS.
A total of 10 cases of SLL were assigned at different spots of the
right lung. Gross tumor volume (GTVt), lymph nodes at the 2nd, 4th
and 7th stations (GTVn) and OARs (lungs, heart and spinal cord)
were contoured on the fused images. Planning GTVt (PGTV) and
clinical target volume (CTV) were obtained by 3-mm and 8-mm 3D
enlargement of the GTVt and GTVn, respectively. A dose of 66 Gy/33
F was administered to the CTV. The radiotherapy plan was created
for each case by three distinct technologies, including 3D-CRT with
three fields, IMRT with five fields and VMAT with a full arc
(range, 181–179°) based on the anisotropic analytical algorithm.
The VMAT fields used a dynamic multi-leaf collimator, and variable
dose rates and gantry speeds. Plan optimization was performed with
dose volume objectives in IMRT and a progressive resolution
optimizer in VMAT. Each plan should be created and confirmed by
three different radiotherapy physicists and accepted by three
different radiotherapy physicians. Dosimetric parameters in
dose-volume histograms (DVHs) are presented as the mean ± standard
deviation (SD).
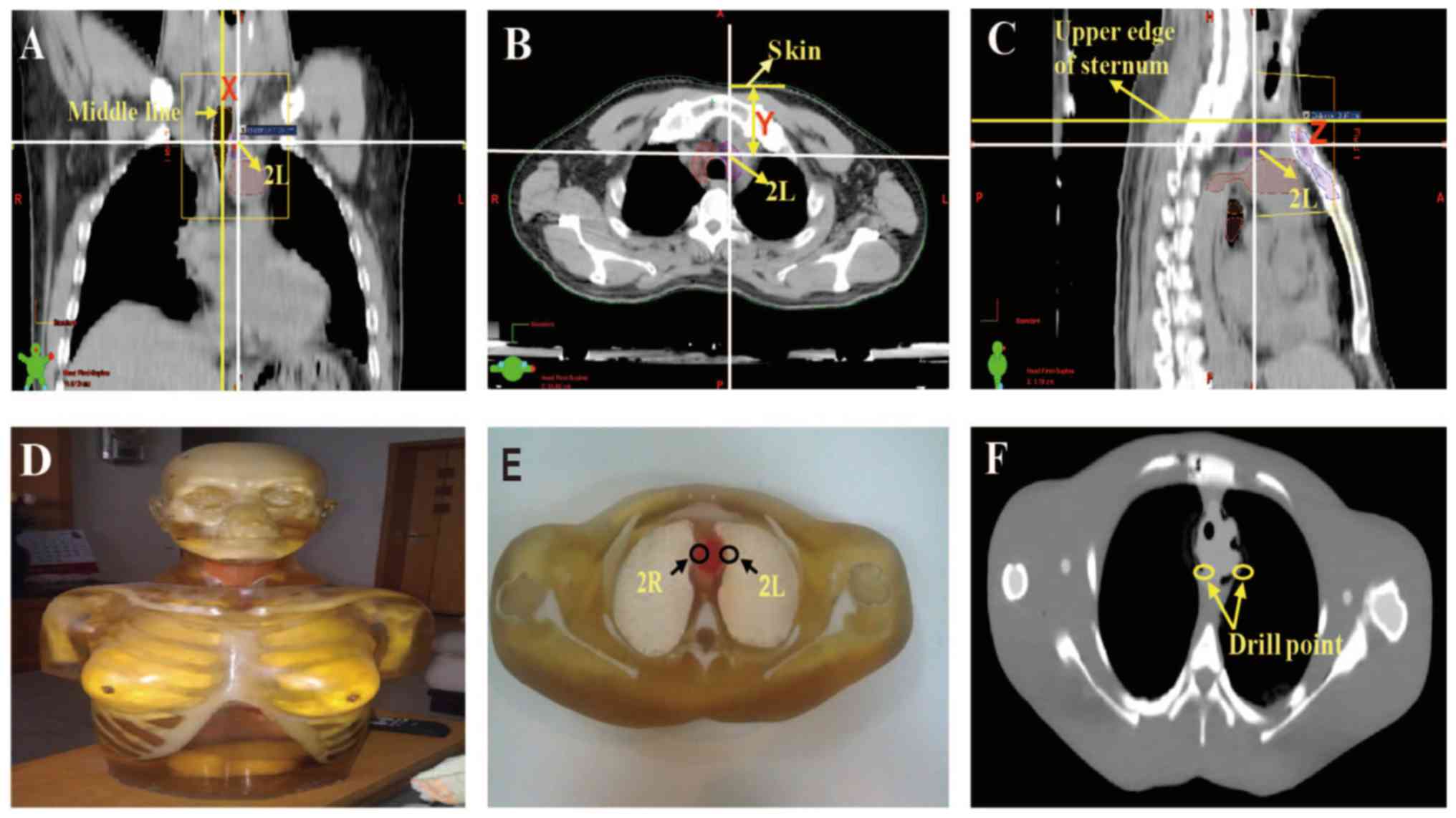
Drilling the CDP
To drill the MLN checkpoints onto the CDP model,
three distances were measured in the CT images of patients. To
avoid deviation in drilling the CDP due to different sizes of
female breasts, male patients were used to build the model for a
female dataset. Male patients had similar characteristics to those
of the medium CDP (170 cm in height and 65 kg in weight), whose
thoracic tumors were selected to measure X, Y and Z distances. In
the plane of the coronal section, the vertical distance (X) was
measured from the central point of specific MLNs to the middle
line. In the plane of the transverse section, the vertical distance
(Y) was measured from the central point of specific MLNs to the
surface skin. In the plane of the sagittal section, the vertical
distance (Z) was measured from the central point of specific MLNs
to the upper edge of the sternum. The mean X, Y and Z distances of
specific MLNs were calculated as the drilling points of ROIs. The
difference of X, Y and Z distances between the male patients and
female CDP were modified according to the proportion of Phantom
products. Drilling on the CDP was conducted at Chengdu Phantom,
Ltd. (Chengdu, China).
CT scan and plan design of CDP
model
The CDP was scanned with a CT simulator (Philips
Healthcare, Amsterdam, The Netherlands) with a slice thickness of 3
mm. The Phantom CT images and DICOM format MLN images were uploaded
to the MIM system (version 6.5.4; MIM Software Inc., Cleveland, OH,
USA) of elastic deformation. In the image registration interface of
the MIM system, two sets of images with the same position could be
automatically registered and fused with rigid alignment.
Multimodality fusion of primary and secondary images could be
aligned automatically to correct possible differences in the X-, Y-
and Z-axes. The procedure was repeated three to five times to
obtain the best fusion images. Fusion images were transferred into
the Eclipse TPS. Contours of the SLL, MLNs and OARs were copied
from 3D MLNs images to Phantom CT images for the plan design of
3D-CRT, IMRT and VMAT. The CTV concept was defined identical to
that aforementioned. To keep the dosimetric measurement of the
thermoluminescence dosimeter (TLD) in a linear range, CTV was dosed
at 100 cGy irradiation by a 6-MV X-ray.
Measurement of radiation dose
Following the alignment of central points in the
radiation field of the Phantom, any setup errors were corrected by
cone beam CT, and then TLDs using lithium fluoride rods (3×10 mm;
Chengdu Phantom Ltd) were plugged into drill points. TLDs are a
type of lithium fluoride material, and the energy corrections and
calibration were performed at the Center for Disease Control and
Prevention of Sichuan (Chengdu, China). Additionally, the Phantom
underwent 100 cGy irradiation from the Trilogy® system
linear accelerator (Varian Medical System, Inc.). The same
procedures were conducted for all three plans. The dosimetric
measurement of TLDs at 3 points of ROIs, including at the 2R and
7th MLN stations, and at SLL, was performed. All experiments were
repeated three times.
Statistical analysis
All the data and readings of TLDs are presented as
the mean ± SD. Differences between groups were statistically
analyzed using one-way analysis of variance (ANOVA) followed by a
Student-Newman-Keuls post-hoc test and unpaired Student's t-test in
SPSS version 18.0 (SPSS, Inc., Chicago, IL, USA). P<0.05 was
considered to indicate a statistically significant difference.
Results
3D reconstruction of MLNs and adjacent
structures
A 3D model of MLNs with surface and volume
reconstructions was formed. The esophagus, trachea, left and right
bronchi, thymus, sternum, thoracic duct and vertebrae, spinal cord,
thoracic great vessels and heart were also reconstructed (Fig. 1C). The chest was divided into eight
regions (11), which facilitated the
identification of MLN stations (Fig. 1D
and E). In the reconstructed 3D model of MLNs, MLN and adjacent
structures were depicted, including front- and right-sided views
(Fig. 1F and G). Additionally,
further details of adjacent structures were depicted, including the
lungs, sternum, esophagus, trachea, spinal cord, heart and great
vessels, with front- and left-sided views (Fig. 1H and I). The 9th MLN station and other
groups of the ITLN were not identified in CVH2.
Plan comparison in different
radiotherapy technologies
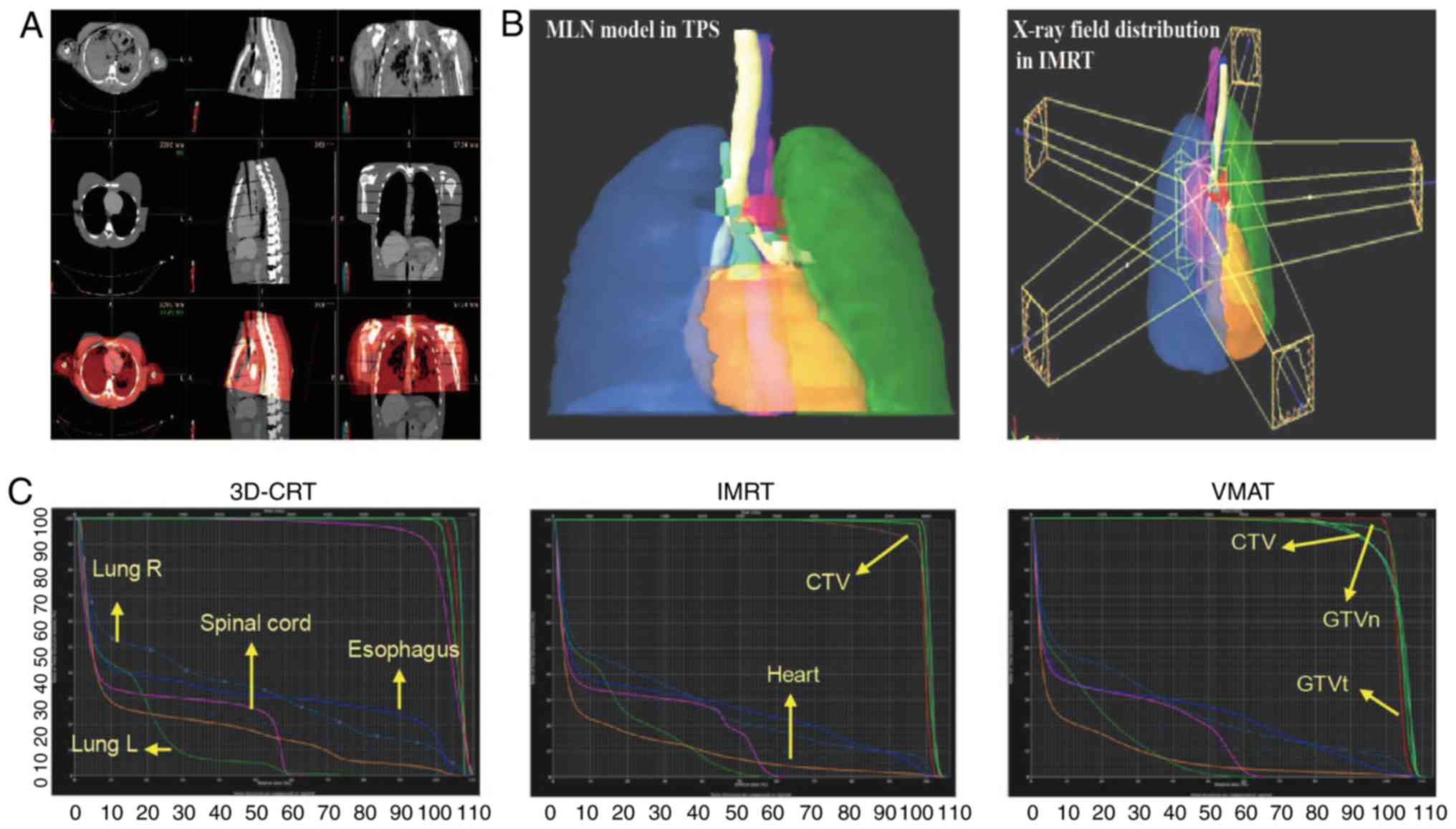
Following image registration and fusion in Eclipse
TPS, a successful match was obtained of the mediastinum, lungs,
backbone and OARs between the 3D MLN model and chest CT (Fig. 2A). In radiotherapy, contouring of MLNs
is generally based on the CT image set. The 3D MLN model with
high-resolution fusion photography could optimize the MLN contours.
The cadaver data for target delineation were much clearer than
chest CT, even if contrast agents were used in CT or MRI imaging,
due to the blood vessel perfusion imaging and high resolution
(15,16). The MLN model can improve the clarity
and resolution of CT images notably (Fig.
2B). The treatment plans of 3D-CRT, IMRT and VMAT were designed
in the Eclipse TPS.
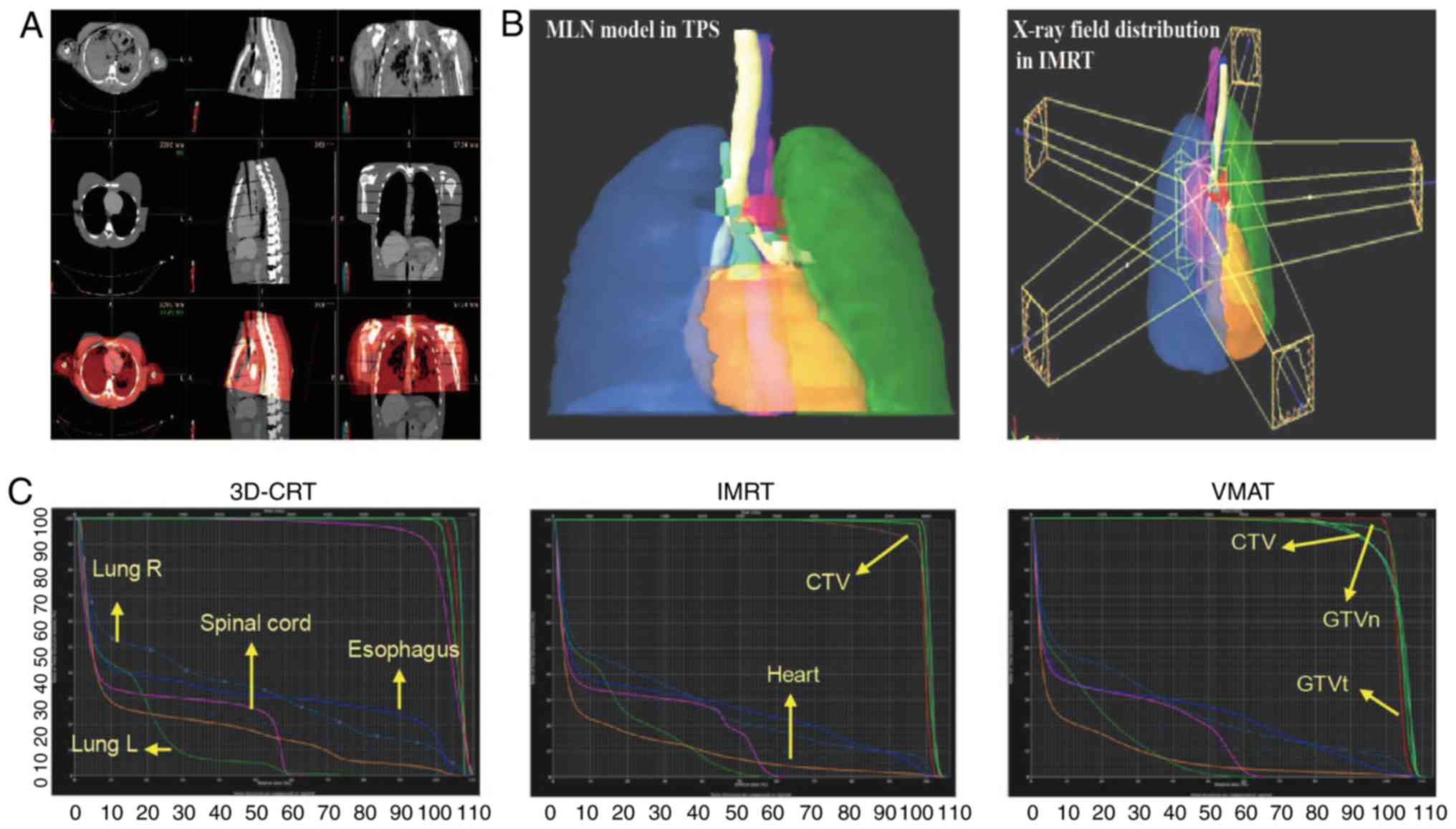 | Figure 2.Image registration and fusion, and
plan design for thoracic radiotherapy. (A) A 3D MLN model and
computed tomography images registered and fused automatically in
the Eclipse™ TPS. (B) A 3D MLN model in the Eclipse TPS. X-ray
field distribution of IMRT as a representative. (C) The dose volume
histogram of three plans in the fused MLN model (3D conformal
radiotherapy, IMRT and VMAT). The same color lines in different
panels represent the same regions of interest. MLN, mediastinal
lymph node; CTV, clinical target volume; GTVn, MLNs at the 2nd, 4th
and 7th stations; GTVt, gross tumor volume; IMRT,
intensity-modulated radiotherapy; TPS, treatment planning system;
3D, three-dimensional; VMAT, volumetric-modulated arc therapy;
3D-CRT, three-dimensional conformal radiotherapy. |
The dose of 2 percent target volume
(D2%), dose of 98 percent target volume
(D98%) and mean dose of target volume (Dmean)
of CTV in 3D-CRT were increased compared with those in IMRT and
VMAT. Compared with IMRT, there were no differences in
D2% and Dmean of CTV in VMAT, but differences
were identified in D98%. The volume of 20 Gy
(V20), volume of 30 Gy (V30) and mean lung
dose (MLD) of the lungs in IMRT were decreased compared with those
in 3D-CRT and VMAT. The V5 of the lungs in VMAT was
higher than that in 3D-CRT and IMRT. The maximum dose of the spinal
cord (DMax) was lowest in IMRT, and the heart dose
(V40) was lowest in VMRT.
Conformity index (CI;
CI=VRI/VTV) and homogeneity index (HI;
HI=DMax/RI) were also calculated as per The Radiation
Therapy Oncology Group definition (26,27). In
the present study, RI was the prescribed dose of PTV,
VRI was the volume of the RI, VTV was the
total volume of PTV and DMax was the maximum dose. The
CI in IMRT and VMAT was better than that in 3D-CRT, but there was
no difference in HI among the three radiotherapy plans. All these
comparisons were significantly different (P<0.05; Table I; Fig.
2C). Taken in combination, IMRT demonstrated significantly
higher values in CI, CTV coverage and OARs (lungs and spinal cord)
protection compared with 3D-CRT and VMAT (P<0.05).
 | Table I.Plan comparison of distinct
radiotherapy technologies (n=10). |
Table I.
Plan comparison of distinct
radiotherapy technologies (n=10).
|
|
|
|
| P-value |
|---|
|
|
|
|
|
|
|---|
| Parameters | 3D-CRTa | IMRTa | VMATa | 3D-CRT vs.
IMRT | 3D-CRT vs.
VMAT | IMRT vs. VMAT |
|---|
| D2% CTV,
cGy | 7177.6±86.1 | 7017.1±105.7 | 7024.9±94.2 | 0.001 | 0.001 | 0.863 |
| D98%
CTV, cGy | 6609.2±135.4 | 6452±33.7 | 6501.4±38.2 | 0.002 | 0.026 | 0.006 |
| Dmean
CTV, cGy | 6925.6±52.3 | 6838.1±64.5 | 6826.8±61.4 | 0.016 | 0.001 | 0.693 |
| V5 Double
Lungs, % | 46.52±6.5 | 50.26±2.5 | 58.78±4.8 | 0.107 | 0.002 | 0.001 |
| V20 Double
Lungs, % | 28.46±4.6 | 25.31±1.8 | 28.26±2.4 | 0.061 | 0.905 | 0.007 |
| V30 Double
Lungs, % | 23.69±3.2 | 18.1±1.0 | 18.99±0.6 | <0.001 | 0.002 | 0.036 |
| MLD, cGy | 1752.9±180.0 | 1529.9±62.5 | 1666.5±97.5 | 0.001 | 0.198 | 0.001 |
| DMax Spinal
Cord, cGy | 3816.5±46.7 | 3665.5±38.8 | 3761±38.7 | <0.001 | 0.009 | <0.001 |
| V40
Heart, % | 28.6±10.9 | 22.11±8.2 | 12.32±7.8 | 0.151 | 0.001 | 0.014 |
| CI | 1.72±0.25 | 1.07±0.08 | 1.11±0.06 | <0.001 | <0.001 | 0.241 |
| HI | 1.10±0.03 | 1.08±0.03 | 1.09±0.03 | 0.316 | 0.675 | 0.675 |
Location of MLNs and drilling the
radiation phantom
Among the 20 male patients with thoracic tumors in
Oncology Department, Xinqiao Hospital (Chongqing, China), there
were 9 cases of lung squamous cell carcinoma, 1 case of lung
adenosquamous carcinoma, 7 cases of small cell lung cancer, 1 case
of esophageal carcinoma and 2 cases of other tumor types. The
physical characteristics were as follows: Median age, 57 years;
median height, 169.4 cm; median weight, 66.6 kg; and median body
surface area, 1.80 m2. The vertical distances X
(Fig. 3A), Y (Fig. 3B) and Z (Fig. 3C) of the 2R, 2L, 4R, 4L and 7th MLN
stations were measured from their chest CT images (data not shown)
and the mean distances were calculated. The MLN ROIs were then
drilled into the CDP model (Figs.
3D-F). The drill points were 3×10 mm in size, which matched the
TLDs.
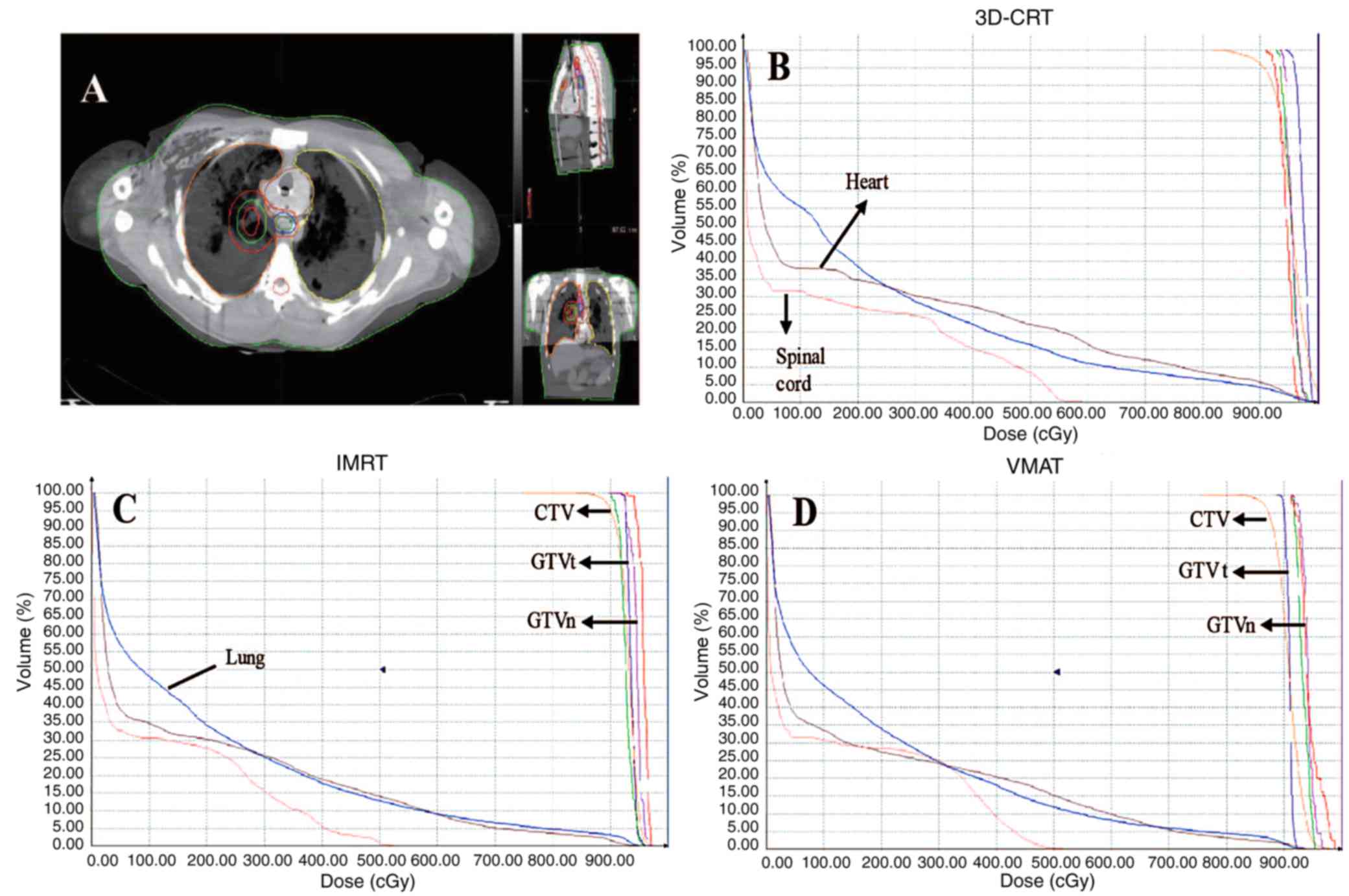
Dosimetric measurement in distinct
radiotherapy plans
The chest CT scan of the CDP demonstrated that each
drill point was clearly located in specific MLN stations. A
simulation model of the MLNs for thoracic radiotherapy was then
established (Fig. 4A). Since
dosimetric variation existed between actual absorbed and calculated
doses, the same dosimetric measurement was repeated among the
3D-CRT, IMRT and VMAT plans, and the dosimetric variation in
different ROIs was identified. In DVH, the doses (mean ± SD) of CTV
at 3 points were calculated (2R and 7th MLN stations, and SLL)
(Table II; Fig. 4B-D) and the dosimetric measurement of
TLDs was made for the three distinct radiotherapy technologies.
Through statistical analysis, bias was identified between measured
and calculated doses in three distinct plans (Table II). In combination, the measurement
doses were within ± 10% deviation, compared with calculated doses
at SLL, and at 2R and 7th MLN stations, indicating dosimetric bias
in the calculated doses (Table
II).
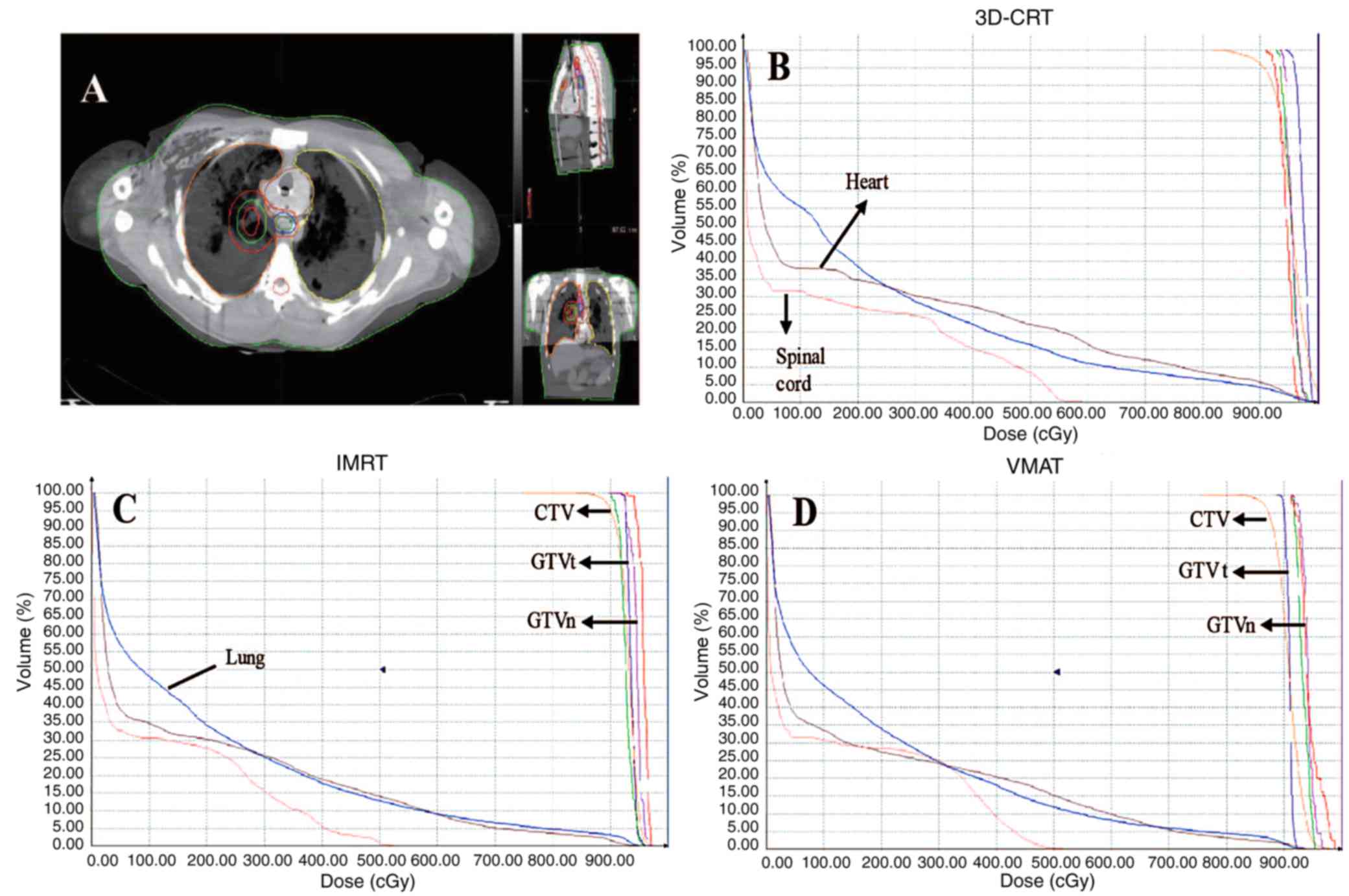 | Figure 4.Contours and DVH of three
radiotherapy plans in the MLN model. (A) Contours of MLNs,
simulated lung lesion and organs at risk on fused images in the MIM
system. (B) DVH of the 3D-CRT plan. (C) DVH of the IMRT plan. (D)
DVH of the VMAT plan. The same color lines in different panels
represent the same regions of interest. Note that the arrow for
GTVn is referring to the purple line in both (C) and (D) graphs.
DVH, dose-volume histogram; MLN, mediastinal lymph node; 3D-CRT,
three-dimensional conformal radiotherapy; IMRT, intensity-modulated
radiotherapy; VMAT, volumetric-modulated arc therapy; CTV, clinical
target volume; GTVn, MLNs at the 2nd, 4th and 7th stations; GTVt,
gross tumor volume. |
 | Table II.Comparison of measurement and
calculated doses in distinct radiotherapy technologies (n=5). |
Table II.
Comparison of measurement and
calculated doses in distinct radiotherapy technologies (n=5).
|
| 3D-CRT | IMRT | VMAT | Mean |
|---|
|
|
|
|
|
|
|---|
| ROIs | Measured, cGy | Calculated,
cGy | Difference, % | Measured, cGy | Calculated,
cGy | Difference, % | Measured, cGy | Calculated,
cGy | Difference, % | Difference, % |
|---|
| 2R MLNs | 93.2±1.6 | 90.2±1.1 | −3.32 | 102±3.3 | 96.0±0.8 | −6.98 | 101±1.7 | 92.8±1.0 | −9.59 | −6.75 |
| 7th MLNs | 85.4±2.3 | 90.7±1.1 | 5.84 | 86.7±0.7 | 92.6±1.1 | 6.37 | 85.7±1.1 | 92.1±0.7 | 6.95 | 6.39 |
| SLL | 97.8±3.6 | 92.7±0.9 | −5.50 | 107±1.1 | 93.6±0.7 | −14.32 | 96.6±1.4 | 89.9±0.6 | −7.49 | −9.10 |
Discussion
In thoracic malignancy, tumor, node, metastasis
(TNM) staging serves an important role in selecting the treatment
options and calculating the prognosis estimation (28). Weder (29) identified that the TNM staging system
was a vital reference for treatment and prognostic analysis in
thoracic malignancy. In the present study, the 3D MLN model,
observed by unaided eyes, was superior to the CT and MRI images in
terms of high definition, resolution and recognition. Although a
previous study reported reconstruction of thoracic structures
(17), to the best of our knowledge,
the present study is the first to construct a 3D MLN model based on
the CVH dataset. This model is a useful teaching tool, and it can
provide morphological data for imaging diagnosis, facilitating a
self-learning approach for the chest anatomy for medical students
and for navigating the thoracic cavity during surgery for junior
surgeons. The visualized MLN model can provide additional valuable
information and assist in the understanding of miniscule and
spatial structures, arousing a Student's interest in anatomy and
overcoming the teaching difficulty when there is a lack of human
cadavers; however, this function of the 3D MLN model is not the
focus of the present study and will not be discussed further.
The 3D MLN model can also function as a contouring
aid. The user can view single or multiple contours rendered on the
anatomical or CT scan images for CVH2; thus, the MLN model allows
the user to practice the contouring process of anatomical
structures and improve their ability to contour MLNs. The 3D MLN
digital model was used in combination with the chest CT, which is
based on a medium-build figure, to ensure uniform conditions in the
present study and prevent deviation due to the diversity of
patients. Image fusion between the 3D MLN model and chest CT was
performed; thus, it was easier to recognize MLNs and OARs on fused
images. There is also a possibility to simulate thoracic
radiotherapy in TPS and even dynamically visualize radiation fields
from different directions and angles in coplanar radiation. Based
on the standard evaluation model, a definite dosimetric deviation
and radiation plan can be determined for different thoracic
radiotherapy strategies. Without a 3D MLN model combined with the
standard chest CT images, a group of patients would have been
required to compare different plans, which would have raised the
issue of avoiding interpatient diversity and uncertain MLN
contours.
Furthermore, the 3D MLN model can be used for
dosimetric measurement in thoracic radiotherapy supported by CDP, a
humanoid-shaped bioequivalent material of Chinese individuals.
Since the CDP is based on a Chinese patient of a medium-build, it
ensured uniform conditions and prevented interpatient deviation in
the present study. The majority of commercially available
dosimetric devices in quality assurance, including the solid water
and delta 4 device, have homogeneous density throughout their
volume (30). There are also certain
heterogeneous phantoms, including the Rando® phantom
(31). By contrast, CDP is an
inhomogeneous phantom that has variable and varying densities
inside, similar to that of the real interior of a body. Therefore,
it could achieve a precise radiotherapy target volume, positioning
and release dose using modern radiation technology. Peng et
al (25) verified CDP as a good
avatar for humans via studying the tissue equivalent imaging.
Comparisons between the CT values of the CDP and humans
demonstrated a deviation of <5% (25). The current study is based on these
earlier reports, and brings CDP into preclinical research.
Eclipse TPS supports image registration and fusion
of the 3D MLN model and CDP CT images. Thus, CDP can be radiation
detector simulator with the use of TLDs. In the present study, four
sets of data of TLDs were tested, with the X-ray at 25, 50, 75 and
100 cGy, respectively. The measurement value linearly increased
with the increasing X-ray radiation (data not shown), indicating
that TLDs are an ideal tool to measure the actual dose of the
radiation phantom.
The current study demonstrated that different
radiation technologies have different dose-volume effects. IMRT
possessed improved V20, V30 and MLD of the
lungs with similar CTV coverage. Furthermore, the present study
indicated that there are dosimetric deviations between measured and
calculated doses. To the best of our knowledge, the current study
was the first to combine the 3D MLN model with the CDP model to
optimize the plan of thoracic radiotherapy. This newly built MLN
model could be an important tool in improving the effectiveness of
thoracic radiotherapy in future clinical studies. Similarly, the
present study lays the foundation for other ROI studies in
dosimetric phantoms and sets an example for radiotherapy studies of
other cancer types.
There is significant dose variation in the soft
tissue/skin, solid tissue/lung and soft tissue/bone, due to the
backscatter radiation from the interface in the treatment region
(32). Although modern TPS is
believed to have the ability to successfully predict the dose that
should be given to the patient, the actual absorbed doses generally
deviate from calculated doses in practice. In a study of
stereotactic lung radiotherapy, two heterogeneous phantoms were
conducted with targets of 1.5 and 4.0 cm. Dose distributions in the
simulated tumors delivered by different treatment plans were
measured with radiochromic film. The dosimetric inaccuracy ranged
from −3 to 4% (33). In another study
of dose distribution for VMAT applied to total marrow irradiation
in a human-like phantom, readings of TLDs demonstrated a dose
difference from −4.3 to 6.6% compared with the calculated dose
(34). To examine if there were
variations in different radiotherapy strategies, the dosimetric
measurement was repeated among the 3D-CRT, IMRT and VMAT plans in
the present study. Based on the standard evaluation model of CDP, a
definite dosimetric deviation can be determined for different
thoracic radiotherapy strategies, thus avoiding interpatient
diversity and uncertain MLNs contour. The deviation at SLL, and at
the 2R and 7th MLN stations was identified. A larger deviation was
demonstrated between measured and calculated doses, which may have
been caused by the different CTVs and linear accelerators.
Collectively, all these studies indicated that it is necessary to
apply dosimetric phantoms in clinical dosimetric monitoring.
There are certain limitations to the present study.
Firstly, the CDP was produced based on selected male patients of a
medium-build, due to the female patients being shorter and thinner
than the medium figure. Additionally, the present study was not
rigorous enough to design radiotherapy plans and measure the dose
in the same CDP. In addition, visual models were insufficient for
individualized radiotherapy plans of real-world patients. The depth
of thoracic cavity in the prone posture serves a critical role in
dose deposition, which means that the individualized radiotherapy
plans should be optimized with compensation of bioequivalent
material of CDP to realize an adjustable thickness. Furthermore, a
set of criteria is also required for using and evaluating 3D MLN
models and radiation phantoms in thoracic radiotherapy. More
detailed studies are required to further confirm the conclusions.
Since MIM has the function of deformable image registration in
internal structures between MLNs images and chest CT, MIM and
deformable registration could be used to extend this model to other
patients using an atlas-based approach.
In the future, a 3D movable virtual system or 4D
application could be used in the future for dosimetric monitoring
of novel radiotherapy techniques, including breath gating or target
tracking treatment, since 4D-radiotherapy is gaining popularity
(35).
In conclusion, clinical diagnosis and treatment may
greatly benefit from digital medical models for radiotherapy. The
3D MLN model in the present study can benefit plan optimization and
dosimetric measurement of thoracic radiotherapy, and when combined
with CDP, it may provide a tool for clinical dosimetric
monitoring.
Acknowledgements
The authors are grateful to The National Key
Research and Development Project (grant no. 2016YFC0106400), The
National Natural Science Foundation of China (grant no. 81272496),
The Natural Science Foundation of Chongqing (grant nos.
cstc2012jjA10096 and cstc2013kjrc-tdjs10011) and The Clinical
Foundation of Third Military Medical University (grant no.
2011XLC46) for financial support. In addition, the authors would
like to thank Professor Da-Quan Lin at Sichuan University (Chengdu,
Sichuan, China) for guidance in drilling the CDP and in the
dosimetric measurement of TLDs.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Allemani C, Weir HK, Carreira H, Harewood
R, Spika D, Wang XS, Bannon F, Ahn JV, Johnson CJ, Bonaventure A,
et al: Global surveillance of cancer survival 1995–2009: Analysis
of individual data for 25,676,887 patients from 279
population-based registries in 67 countries (CONCORD-2). Lancet.
385:977–1010. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Diwanji TP, Mohindra P, Vyfhuis M, Snider
JW III, Kalavagunta C, Mossahebi S, Yu J, Feigenberg S and Badiyan
SN: Advances in radiotherapy techniques and delivery for non-small
cell lung cancer: Benefits of intensity-modulated radiation
therapy, proton therapy, and stereotactic body radiation therapy.
Transl Lung Cancer Res. 6:131–147. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jensen I, Carl J, Lund B, Larsen EH and
Nielsen J: Radiobiological impact of reduced margins and treatment
technique for prostate cancer in terms of tumor control probability
(TCP) and normal tissue complication probability (NTCP). Med Dosim.
36:130–137. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Palma DA, Verbakel WF, Otto K and Senan S:
New developments in arc radiation therapy: A Review. Cancer Treat
Rev. 36:393–399. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chan OS, Lee MC, Hung AW, Chang AT, Yeung
RM and Lee AW: The superiority of hybrid-volumetric arc therapy
(VMAT) technique over double arcs VMAT and 3D-conformal technique
in the treatment of locally advanced non-small cell lung cancer-A
planning study. Radiother Oncol. 101:298–302. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rauschenbach BM, Mackowiak L and Malhotra
HK: A dosimetric comparison of three-dimensional conformal
radiotherapy, volumetric-modulated arc therapy, and dynamic
conformal arc therapy in the treatment of non-small cell lung
cancer using stereotactic body radiotherapy. J Appl Clin Med Phys.
15:48982014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wu Z, Xie C, Hu M, Han C, Yi J, Zhou Y,
Yuan H and Jin X: Dosimetric benefits of IMRT and VMAT in the
treatment of middle thoracic esophageal cancer: Is the conformal
radiotherapy still an alternative option? J Appl Clin Med Phys.
15:93–101. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bzdusek K, Friberger H, Eriksson K,
Hårdemark B, Robinson D and Kaus M: Development and evaluation of
an efficient approach to volumetric arc therapy planning. Med Phys.
36:2328–2339. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Heineman DJ, Daniels JM and Schreurs WH:
Clinical staging of NSCLC: Current evidence and implications for
adjuvant chemotherapy. Ther Adv Med Oncol. 9:599–609. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mountain CF and Dresler CM: Regional lymph
node classification for lung cancer staging. Chest. 111:1718–1723.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rusch VW, Asamura H, Watanabe H, Giroux
DJ, Rami-Porta R and Goldstraw P; Members of IASLC Staging
Committee, : The IASLC lung cancer staging project: A proposal for
a new international lymph node map in the forthcoming seventh
edition of the TNM classification for lung cancer. J Thorac Oncol.
4:568–577. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lababede O, Meziane M and Rice T: Seventh
edition of the cancer staging manual and stage grouping of lung
cancer: Quick reference chart and diagrams. Chest. 139:183–189.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shen G, Lan Y, Zhang K, Ren P and Jia Z:
Comparison of 18F-FDG PET/CT and DWI for detection of mediastinal
nodal metastasis in non-small cell lung cancer: A meta-analysis.
PLoS One. 12:e01731042017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang SX, Heng PA, Liu ZJ, Tan LW, Qiu MG,
Li QY, Liao RX, Li K, Cui GY, Guo YL, et al: Creation of the
Chinese visible human data set. Anat Rec B New Anat. 275:190–195.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang SX, Heng PA, Liu ZJ, Tan LW, Qiu MG,
Li QY, Liao RX, Li K, Cui GY, Guo YL, et al: The Chinese Visible
Human (CVH) datasets incorporate technical and imaging advances on
earlier digital human. J Anat. 204:165–173. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wu Y, Luo N, Tan L, Fang B, Li Y, Xie B,
Liu K, Chu C, Li M and Zhang S: Three-dimensional reconstruction of
thoracic structures: Based on chinese visible human. Comput and
Math Methods Med. 2013:7956502013. View Article : Google Scholar
|
|
18
|
Rong J, Wang Q, Liu K, Tan L, Ran X, Zhang
S, Li Q and Han Y: A new atlas localization approach for
subthalamic nucleus utilizing Chinese visible human head datasets.
PLoS One. 8:e572642013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Capelle L, Warkentin H, Mackenzie M,
Joseph K, Gabos Z, Pervez N, Tankel K, Chafe S, Amanie J, Ghosh S,
et al: Skin-sparing helical tomotherapy vs. 3D-conformal
radiotherapy for adjuvant breast radiotherapy: In Vivo, skin
dosimetry study. Int J Radiat Oncol Biol Phys. 83:e583–e590. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nazemi-Gelyan H, Hasanzadeh H, Makhdumi Y,
Abdollahi S, Akbari F, Varshoee-Tabrizi F, Almasrou H, Nikoofar A
and Rezaei-Tavirani M: Evaluation of organs at risk's dose in
external radiotherapy of brain tumors. Iran J Cancer Prev. 8:47–52.
2015.PubMed/NCBI
|
|
21
|
Adolfsson E, Gustafsson H, Lund E, Alm
Carlsson G, Olsson S and Carlsson Tedgren S: A system for remote
dosimetry audit of 3D-CRT, IMRT and VMAT based on lithium formate
dosimetry. Radiother Oncol. 113:279–282. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jiang X, Li T, Liu Y, Zhou L, Xu Y, Zhou X
and Gong Y: Planning analysis for locally advanced lung cancer:
Dosimetric and efficiency comparisons between intensity-modulated
radiotherapy (IMRT), single-arc/partial-arc volumetric modulated
arc therapy (SA/PA-VMAT). Radiat Oncol. 6:1402011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
ICRU report 48, phantoms and computational
models in therapy, diagnosis and protection. 1992.
|
|
24
|
Lehmann J, Stern RL, Levy J, Daly TP,
Siantar CL and Goldberg Z: Radiation phantom with humanoid shape
and adjustable thickness (RPHAT). Phys Med Biol. 49:N125–N129.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Peng G, Zeng Y, Luo T, Zhao F, Peng S, You
R, Tan H, Liu X and Wang J: Organ dose evaluation for multi-slice
spiral CT scans based on China Sichuan chest anthropomorphic
phantom measurements. Radiat Prot Dosimetry. 150:292–297. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Feuvret L, Noël G, Mazeron JJ and Bey P:
Conformity index: A review. Int J Radiat Oncol Biol Phys.
64:333–342. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ayata HB, Güden M, Ceylan C, Kücük N and
Engin K: Comparison of dose distributions and organs at risk (OAR)
doses in conventional tangential technique (CTT) and IMRT plans
with different numbers of beam in left-sided breast cancer. Rep
Pract Oncol Radiother. 16:95–102. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mountain CF: Revisions in the
international system for staging lung cancer. Chest. 111:1710–1717.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Weder W: Lung cancer: New
opportunities-changing algorithm in staging. Ann Oncol. 19 Suppl
7:vii28–vii30. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Gurjar OP, Mishra SP, Bhandari V, Pathak
P, Patel P and Shrivastav G: Radiation dose verification using real
tissue phantom in modern radiotherapy techniques. J Med Phys.
39:44–49. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yamazaki H, Iwama K, Nishimura T, Iwai Y,
Aibe N, Takenaka T, Miyake S, Tanaka E, Yoshida K, Oota Y, et al:
Comparison of calculated dose by helical tomotherapy treatment
planning machine and measured dose of radiophotoluminescence glass
dosimeter in lung lesions using Rando Phantom. Anticancer Res.
33:1679–1684. 2013.PubMed/NCBI
|
|
32
|
Kinhikar RA, Tambe CM, Patil K, Mandavkar
M, Deshpande DD, Gujjalanavar R, Yadav P and Budrukkar A:
Estimation of dose enhancement to soft tissue due to backscatter
radiation near metal interfaces during head and neck radiothearpy-A
phantom dosimetric study with radiochromic film. J Med Phys.
39:40–43. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Seppala J, Suilamo S, Kulmala J, Mali P
and Minn H: A dosimetric phantom study of dose accuracy and
build-up effects using IMRT and RapidArc in stereotactic
irradiation of lung tumours. Radiat Oncol. 7:792012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Surucu M, Yeginer M, Kavak GO, Fan J,
Radosevich JA and Aydogan B: Verification of dose distribution for
volumetric modulated arc therapy total marrow irradiation in a
humanlike phantom. Med Phys. 39:281–288. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Padmanaban S, Boopathy R, Kunjithapatham
B, Sukumar P and Nagarajan V: A phantom study on the effects of
target motion in non-gated kV-CBCT imaging. Australas Phys Eng Sci
Med. 33:59–64. 2010. View Article : Google Scholar : PubMed/NCBI
|