Introduction
Mediastinal and intra-abdominal lymphadenopathies
may present with numerous benign or malignant conditions. Benign
lymph node enlargement may occur as a response to certain
infections, including tuberculosis and fungal infection, as well as
several less common diseases, including Castleman's disease and
Wegener's granulomatosis. Malignant lymphadenopathy may occur in
primary lymphatic diseases such as Hodgkin's lymphoma (HL) and
non-Hodgkin's lymphoma (NHL), as well as in other types of
malignancy that have metastasized to regional lymph nodes,
including lung, esophageal, breast and pancreatic carcinomas
(1,2).
Advanced imaging methods, including computed
tomography (CT), magnetic resonance imaging and positron emission
tomography-computed tomography (PET-CT), serve important roles in
identifying enlarged lymph nodes during the staging workup for
lymphoproliferative disorders; however, they may be limited in
their ability to differentiate between inflammatory/reactive
processes and malignancy (3–5). Thus, tissue obtained percutaneously or
surgically is critical to providing a pathological diagnosis,
including insight into the possible disease origin. Laparoscopic
lymph node biopsy and image-guided needle biopsy (IGNB) have been
applied to obtain tissue from enlarged lymph nodes; however, these
are invasive and expensive procedures. Endoscopic ultrasound (EUS)
has emerged as a novel imaging modality (3,5). A
fine-needle aspiration (FNA) biopsy coupled with EUS allows for the
sampling of the target lesion with ultrasound guidance in real
time, providing minimally invasive access to the lymph nodes within
the abdomen and mediastinum (6,7). Compared
with IGNB, EUS-FNA exhibits increased accuracy for the sampling of
anatomically challenging sites, including those close to major
blood vessels, which is useful for avoiding injury to the adjacent
tissue (7). In addition, EUS-FNA
allows access to deep-seated lymph nodes and the sampling of small
lesions (<25 mm), which overcomes the limitations of sampling
through other techniques (8).
Previous studies have demonstrated that, for diagnosing mediastinal
and intra-abdominal lymphadenopathies, EUS-FNA exhibits a
sensitivity of 79–98.3%, a specificity of 98–100%, a positive
predictive value (PPV) of 98–100%, a negative predictive value
(NPV) of 62–98.4% and an accuracy of 84–99.4% (9,10).
The aim of the present study was to evaluate the
efficacy and safety of EUS-FNA for the diagnosis of mediastinal and
intra-abdominal lymphadenopathies of unknown origin.
Patients and methods
Patients
The present retrospective study included 154
patients with mediastinal and intra-abdominal lymphadenopathies
that were suspected to be malignant based on imaging data. All
patients underwent EUS-FNA at Tongji Hospital (Wuhan, China)
between February 2010 and March 2015. The present study was
approved by The Ethics Committee of Tongji Hospital and informed
consent was obtained from each patient or their legally authorized
representative. The following data were collected from the hospital
medical record system: Age, sex, EUS findings, EUS-FNA findings,
procedure-associated complications and follow-up results.
EUS-FNA procedure
EUS-FNA was performed under deep sedation according
to the principles of ‘monitored anesthesia care’ (11). The patients were anaesthetized with
the intravenous administration of Propofol (2 ml/kg). All patients
received oxygen during the procedure and their blood pressure and
heart rate were monitored.
The EUS-FNA examinations were conducted using an
Olympus linear echoendoscope (GF-UCT 240, GF-UCT 260; Olympus
Corporation, Tokyo, Japan) platform with the Aloka Processor
Alpha-5 (Hitachi, Ltd., Tokyo, Japan). An endosonographer with
>5 years of EUS experience, performing >150 EUS–FNAs per
year, performed EUS-FNA in the present study. A 22-gauge EchoTip
Ultra needle (Cook Endoscopy; Cook Medical Inc., Bloomington, IN,
USA) was advanced into lesions with real-time EUS visualization.
The endosonographer maneuvered the needle back and forth 20 times
within the lesion, applying minimal negative pressure by pulling
the needle stylet slowly and continuously. If no specimen was
obtained, continuous suction was applied with a 5–10 ml syringe in
order to obtain a specimen. Samples were then prepared for
histological and cytological examinations. The specimens were
expelled from a needle in three steps: i) pushing the stylet into
the needle; ii) flushing the needle with 0.1 ml saline; and iii)
filling the needle with 2 ml of air. The core tissue was put into
the container filled with formaldehyde for histological
examination. The fragment of the specimen was put on the glass
slide, and another glass slide was used to smear for cytological
examinations. In suspected cases of lymphoma, additional samples
were obtained for flow cytometry (FCM).
FCM
FCM was performed on a FACScan analyzer (BD
Biosciences, Franklin Lakes, NJ, USA) using standard procedures
(12,13). The cells were stained with selected
monoclonal antibodies as required (30 min at room temperature),
from the following: Immunoglobulin κ and λ light chains (cat no.
560950, 1:5; cat no. 562054, 1:5; BD Biosciences, Franklin Lakes,
NJ, USA), cluster of differentiation CD2 (cat no. 555327; 1:5; BD
Biosciences), CD3 (cat no. 552127; 1:5; BD Biosciences), CD4 (cat
no. 561842; 1:20; BD Biosciences), CD5 (cat no. 555353; 1:5; BD
Biosciences), CD8 (cat no. 557085; 1:5; BD Biosciences), CDl0 (cat
no. 561002; 1:5; BD Biosciences), CDllc (cat no. 560999; 1:5; BD
Biosciences), CDl9 (cat no. 555413; 1:5; BD Biosciences), CD20 (cat
no. 560961; 1:5; BD Biosciences), CD23 (cat no. 561146; 1:20; BD
Biosciences), CD25(cat no. 560990; 1:5; BD Biosciences), CD38 (cat
no. 555462; 1:5; BD Biosciences), FMC-7 (cat no. 340919; 1:5; BD
Biosciences)-a normal B-cell antigen expressed on mature human B
cell and it is used in during immunophenotypic analysis and
differential diagnosis of lymphomas and leukemias (14), major histocompatibility complex (cat
no. ab63567; 1:10; Abcam, Cambridge, MA, USA), class II-DR (HLA-DR)
(cat no. 560896; 1:5; BD Biosciences), CD30 (cat no. 555829; 1:5;
BD Biosciences), CD45 (cat no. 340953; 1:5; BD Biosciences), CDl03
(cat no. 563883; 1:20; BD Biosciences), CDl38 (cat no. 564605;
1:20; BD Biosciences), ki-67 (cat no. 612472; 1:5; BD Biosciences),
Bcl-2 (cat no. 562679; 1:20; BD Biosciences), CDl6 (cat no. 565421;
1:20; BD Biosciences), CD56 (cat no. 565140; 1:20; BD Biosciences),
CD57 (cat no. 560845; 1:20; BD Biosciences), CD94 (cat no. 562361;
1:20; BD Biosciences), CDl61 (cat no. 551138; 1:5; BD Biosciences),
CDl58a/h (cat no. 564319; 1:20; BD Biosciences), CDl58b (cat no.
566053; 1:20; BD Biosciences), CDl58e (cat no. 564103; 1:20; BD
Biosciences), T-cell receptor (TCR)ab (cat no. 563826; 1:20; BD
Biosciences), and TCRrd (cat no. 564157; 1:5; BD Biosciences).
Follow up
The final diagnosis was typically based on the
pathological report obtained from surgery. However, if the patient
did not undergo surgery, a 9 month follow-up was performed
(15). Final diagnosis was classified
as either: i) Malignant lymphadenopathy: EUS-FNA cytology and/or
pathology results revealed malignant cells that were confirmed by
specific immunohistochemical stains or supported with FCM results;
or ii) benign lymphadenopathy: Absence of typical malignant cell
morphology with no further signs of malignancy, i.e. the lesions
exhibited regression or no further progression at follow-up, as
previously described (9,16).
Statistical analysis
EUS-FNA-associated parameters, including the
sensitivity, specificity, PPV, NPV and accuracy were evaluated by
comparing EUS-FNA results with the final diagnoses. Continuous
variables are reported as the mean ± standard deviation and
categorical variables are reported as percentages. Student's
t-tests were used to compare continuous variables and categorical
variables were compared using χ2-tests. A two-tailed
P-value of <0.05 was considered to indicate a statistically
significant difference. All data were processed and analyzed using
SPSS (version 19; IBM Corp., Armonk, NY, USA).
Results
Final diagnoses
A total of 154 patients (105 male, 49 female) were
included in the present study. The mean patient age was 49.1 years
(22–68 years). The success rate for obtaining pathological material
by EUS-FNA was 87.0% (134/154) and adequate cytology samples were
obtained in all cases. The mean number of needle passes was 2.9
(range, 1–6). For the 52 patients suspected to be presenting with
lymphoma, the EUS-FNA samples were evaluated by cytology, pathology
and FCM studies. Overall, a definitive diagnosis was obtained for
153 of the 154 patients (including 31 from surgical pathology and
122 from follow-up). A total of 100 patients were determined to
exhibit malignant lymphadenopathy, including 80 cases of
metastasis, 19 cases of lymphoma and 1 case of myeloid leukemia.
The remaining 53 cases were determined to be benign, including 27
cases of a non-specific inflammatory condition, 21 cases of
tuberculosis and 5 cases of Castleman's disease.
Patient and lesion
characteristics
As presented in Table
I, the incidence of malignant lymphadenopathy in the present
study cohort was significantly increased in males compared with
females (P=0.011). The observed mean age for patients with
malignancy was 55±11.9 years compared with 43±16.8 years for the
benign lymphadenopathy (P=0.0001). Other factors associated with
malignancy included the location and size of the enlarged lymph
node. The mean size of a malignant lymph node was 33.9±15.8 mm,
compared with 24.8±13.8 mm for a benign lymph node (P=0.011). In
particular, the celiac axis lymphadenopathy was a clear indicator
of malignancy (23.0% in malignancy vs. 3.8% in benign
lymphadenopathy; P=0.039). However, the echo-features of lymph
nodes as assessed during EUS were not significantly different
between malignant and benign cases (P=0.153); therefore, this may
not be useful in diagnosing malignancy.
 | Table I.Patient and lesion characteristics of
malignant and benign lymphadenopathy. |
Table I.
Patient and lesion characteristics of
malignant and benign lymphadenopathy.
| Patient
characteristics | Malignant
lymphadenopathy (n=100) | Benign
lymphadenopathy (n=53) | P-value |
|---|
| Sex, n |
|
| 0.0110a |
| Male | 75 | 29 |
|
|
Female | 25 | 24 |
|
| Age,
yearsb | 55±11.9 | 43±16.8 | 0.0001a |
| Lesion
locationc |
|
|
|
|
Peripancreas | 32 (32.0) | 21 (39.6) | 0.3750 |
| Around
the celiac axis | 23 (23.0) | 2 (3.8) | 0.0020a |
| Hepatic
portal | 5 (5.0) | 8 (15.1) | 0.0630 |
|
Mediastinum | 40 (40.0) | 22 (41.5) | 0.8640 |
| Endoscopic
ultrasound characteristics |
|
|
|
| Size,
mmb | 33.9±15.8 | 24.8±13.8 | 0.0110a |
| Sharp
marginc | 85 (85.0) | 40 (75.5) | 0.1470 |
|
Fusionc | 23 (23.0) | 9 (17.0) | 0.3840 |
|
Echogenic focusc | 25 (25.0) | 15 (28.3) | 0.6580 |
|
Homogeneous
echogenicityc | 46 (46.0) | 22 (41.5) | 0.5950 |
|
Malignant
echo-featuresc,d | 40 (75.5) | 81 (81.0) | 0.1530 |
As presented in Table
II, it was demonstrated that EUS-FNA may be useful in assessing
lymphadenopathy resulting from metastasis and lymphoma in the
celiac axis, mediastinum, peripancreatic and hepatic portal areas.
Malignant lymph nodes observed in the celiac axis were more likely
to have resulted from lymphoma (42.1%; 8/19 cases) than metastasis
(18.8%; 15/80 cases; P=0.039). In contrast, malignant lymph nodes
observed in the mediastinum were more likely to have been caused by
metastasis (47.5%; 38/80 cases) than lymphoma (10.5%; 2/19 cases;
P=0.004). EUS-FNA data revealed that the mean size of metastatic
lymph nodes was 35.6±16.4 mm, whereas it was 27.2±11.2 mm for
lymphoma (P=0.011). Furthermore, lesion fusion was observed in
47.4% of lymphoma cases and 17.5% of metastasis cases (P=0.013).
Homogeneous echogenicity was observed in 40.0% of the cases of
metastasis and 73.7% of the cases of lymphoma (P=0.011). Thus,
these results suggested a potential role for EUS-FNA in
distinguishing cases of lymphoma from metastasis in the celiac axis
and mediastinum.
 | Table II.Patient and lesion characteristics of
metastasis and lymphoma. |
Table II.
Patient and lesion characteristics of
metastasis and lymphoma.
| Patient
characteristics | Metastasis
(n=80) | Lymphoma
(n=19) | P-value |
|---|
| Sex, n |
|
| 0.2420 |
|
Male | 62 | 12 |
|
|
Female | 18 | 7 |
|
| Age,
yearsa | 54.9±11.9 | 55.4±12.8 | 0.8950 |
| Lesion
locationb |
|
|
|
|
Peripancreas | 23 (28.8) | 9 (47.4) | 0.2800 |
| Around
the celiac axis | 15 (18.8) | 8 (42.1) | 0.0390c |
| Hepatic
portal | 5 (6.3) | 0 (0.0) | 0.5800 |
|
Mediastinum | 38 (47.5) | 2 (10.5) | 0.0040c |
| Endoscopic
ultrasound characteristics |
|
|
|
| Size,
mma | 35.6±16.4 | 27.2±11.2 | 0.0110c |
| Sharp
marginb | 66 (82.5) | 19 (100.0) | 0.0650 |
|
Fusionb | 14 (17.5) | 9 (47.4) | 0.0130c |
|
Echogenic focusb | 24 (30.0) | 1 (5.3) | 0.0370c |
|
Homogeneous
echogenicityb | 32 (40.0) | 14 (73.7) | 0.0110c |
Efficacy of EUS-FNA for identifying
malignant lymphadenopathy
Among 100 patients diagnosed with malignant
lymphadenopathy, the sensitivity, specificity, PPV, NPV and
accuracy of EUS-FNA for malignant lymphadenopathy were 86.0, 100.0,
100.0, 79.1 and 90.8%, respectively (Table III).
 | Table III.Efficacy of endoscopic
ultrasound-guided fine-needle aspiration. |
Table III.
Efficacy of endoscopic
ultrasound-guided fine-needle aspiration.
|
| Metric, % |
|---|
|
|
|
|---|
| Condition | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|
| Malignant
lymphadenopathy | 86.0 | 100.0 | 100.0 | 79.1 | 90.8 |
|
Metastasis | 87.5 | 100.0 | 100.0 | 87.9 | 93.5 |
|
Lymphoma | 84.2 | 100.0 | 100.0 | 91.7 | 94.2 |
| Benign
lymphadenopathy | 58.5 | 100.0 | 100.0 | 81.9 | 85.6 |
|
Tuberculosis | 38.1 | 100.0 | 100.0 | 91.7 | 92.2 |
|
Nonspecific reactive
lymphadenopathy | 100.0 | 77.7 | 54.2 | 100.0 | 82.4 |
The predominant cause for lymphadenopathy was
metastasis (52.3%; 80/154). The application of EUS-FNA generated a
correct diagnosis for 70 patients, including squamous cell
carcinoma (n=28), adenocarcinoma (n=32), neuroendocrine tumor (n=7)
and undifferentiated carcinoma (n=3). Among them, 30 patients had a
history of tumors and the recurrence of malignancy was confirmed by
EUS−FNA. Notably, the remaining 40 patients had no history of
malignancy and no primary lesion had been detected prior to
EUS-FNA. Thus, additional examination, including PET-CT, was
applied to investigate the tumor origin following EUS−FNA; primary
lesions were successfully identified in 35/40 patients. The
sensitivity, specificity, PPV, NPV and accuracy of EUS-FNA for
metastasis were 87.5, 100.0, 100.0, 87.9 and 93.5%,
respectively.
Of the 52 patients suspected to be presenting with
lymphoma, 19 patients were confirmed, including 10 patients with
diffuse large B-cell lymphomas (DLBCL), 2 patients with HL, 1
patient with T-cell lymphoma and 7 patients with B-cell NHL (B-NHL)
without further subclassifications.
The cytological findings included 9 true-positive
cases and 3 false-positive cases. Benign lymphadenopathy due to
nonspecific inflammatory reaction was the final diagnosis in the 3
false-positive cases, which was determined by follow-up. The
sensitivity, specificity, PPV, NPV and accuracy of EUS-FNA combined
with cytology for lymphoma were 47.4, 90.9, 75.0, 75.0 and 75.0%,
respectively (Table IV).
 | Table IV.Efficacy of EUS-FNA in the
identification of lymphoma. |
Table IV.
Efficacy of EUS-FNA in the
identification of lymphoma.
|
|
| Final diagnoses,
n |
|
|
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|---|
| Method | n | Lymphoma | Non-lymphoma | Sensitivity, % | Specificity, % | PPV, % | NPV, % | Accuracy, % |
|---|
| EUS-FNA with flow
cytometry | 52 |
|
| 84.2 | 100.0 | 100.0 | 91.7 | 94.2 |
|
Lymphoma |
| 16 | 0 |
|
|
|
|
|
|
Non-lymphoma |
| 3 | 33 |
|
|
|
|
|
| EUS-FNA with
cytology | 52 |
|
| 47.4 | 90.9 | 75.0 | 75.0 | 75.0 |
|
Lymphoma |
| 9 | 3 |
|
|
|
|
|
|
Non-lymphoma |
| 10 | 30 |
|
|
|
|
|
| EUS-FNA with
pathology | 52 |
|
| 15.8 | 100.0 | 100.0 | 67.3 | 69.2 |
|
Lymphoma |
| 3 | 0 |
|
|
|
|
|
|
Non-lymphoma |
| 16 | 33 |
|
|
|
|
|
Pathology via EUS-FNA provided adequate tissue
samples for 84.2% of patients. Notably, the pathology analysis was
not sufficient to diagnose 16 cases with malignant lesions,
although there was no false-positive result. Only 3 patients were
diagnosed correctly (2 cases with DLBCL and 1 case without definite
subclassification). The sensitivity, specificity, PPV, NPV and
accuracy of EUS-FNA combined with pathology for lymphoma were 15.8,
100.0, 100.0, 67.3 and 69.2%, respectively.
The combined analysis of EUS-FNA and FCM contributed
to the correct diagnosis of 16 patients with B-NHL through
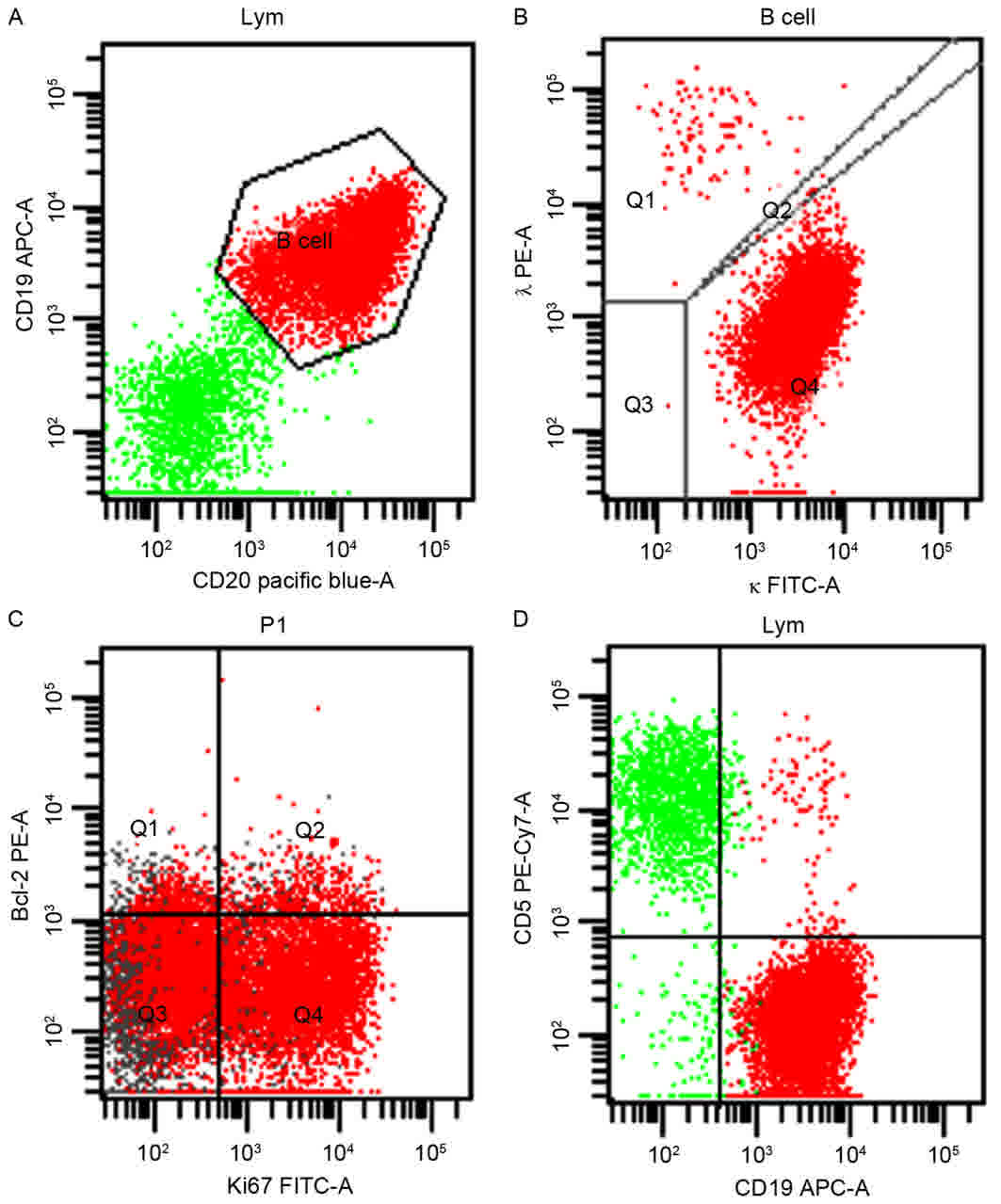
detecting light-chain restriction expression (Fig. 1). A total of 8 lymphomas were further
subtyped as DLBCL due to the detection of CD3, CD5, CD10, Bcl-2 and
CD20 expression by FCM (Fig. 1).
There were no false-positive cases. The combined EUS-FNA and FCM
method was not able to determine 2 cases of HL or 1 case of T-cell
lymphoma, which were ultimately diagnosed with excisional biopsies.
The sensitivity, specificity, PPV, NPV and accuracy of EUS-FNA
combined with FCM assessing lymphoma were 84.2, 100.0, 100.0, 91.7
and 94.2%, respectively. Thus, the efficacy of the combined
analysis is markedly higher than cytology (P<0.001) or pathology
(P=0.001) alone (data not shown).
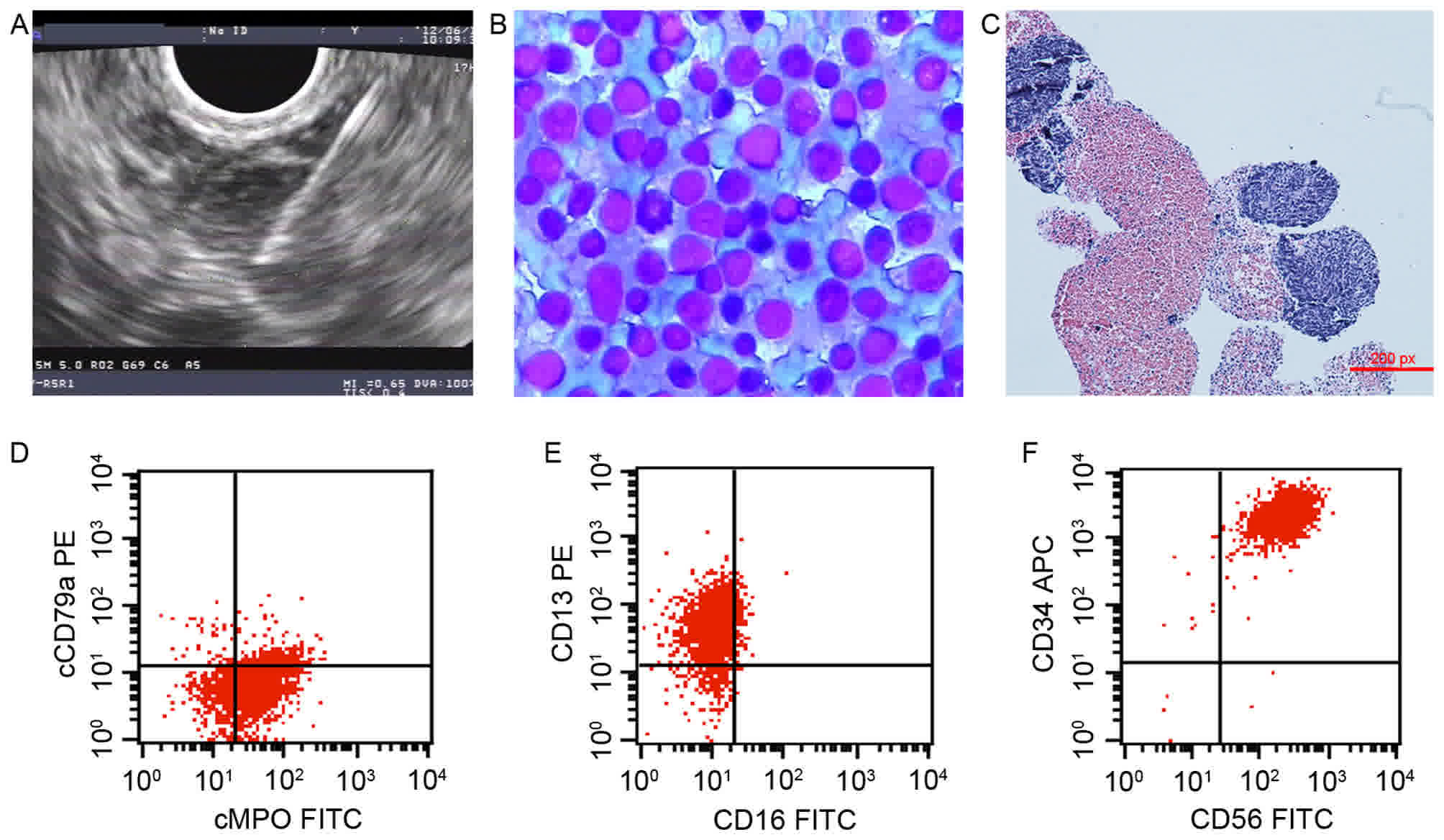
In one atypical case, a 16-year-old male experienced
intermittent abdominal pain for 6 months in the absence of fever.
Laboratory investigations were performed on peripheral blood
counts, whereas a CT scan revealed retroperitoneal lymphadenopathy.
EUS-FNA was therefore recommended to evaluate the enlarged lymph
nodes (Fig. 2). Although cytology
supported the diagnosis of NHL based on immature lymphocyte
proliferation and atypical small, round cells, a definitive
conclusion could not be drawn. A subsequent FCM investigation
highlighted the presence of abnormal cells with a characteristic
phenotype of malignant myeloid origin, which expressed CD117, CD56,
CD34, CD13, CD33 and HLA-DR, partially expressed CD19, cMPO, CD11c
and CD15, and did not express CD3, CD4, CD8, CD5, CD20, CD23, κ, λ,
cCD79a, cCD3 or CD16 (Fig. 2). The
patient underwent a bone marrow biopsy and the diagnosis of acute
myeloid leukemia was confirmed.
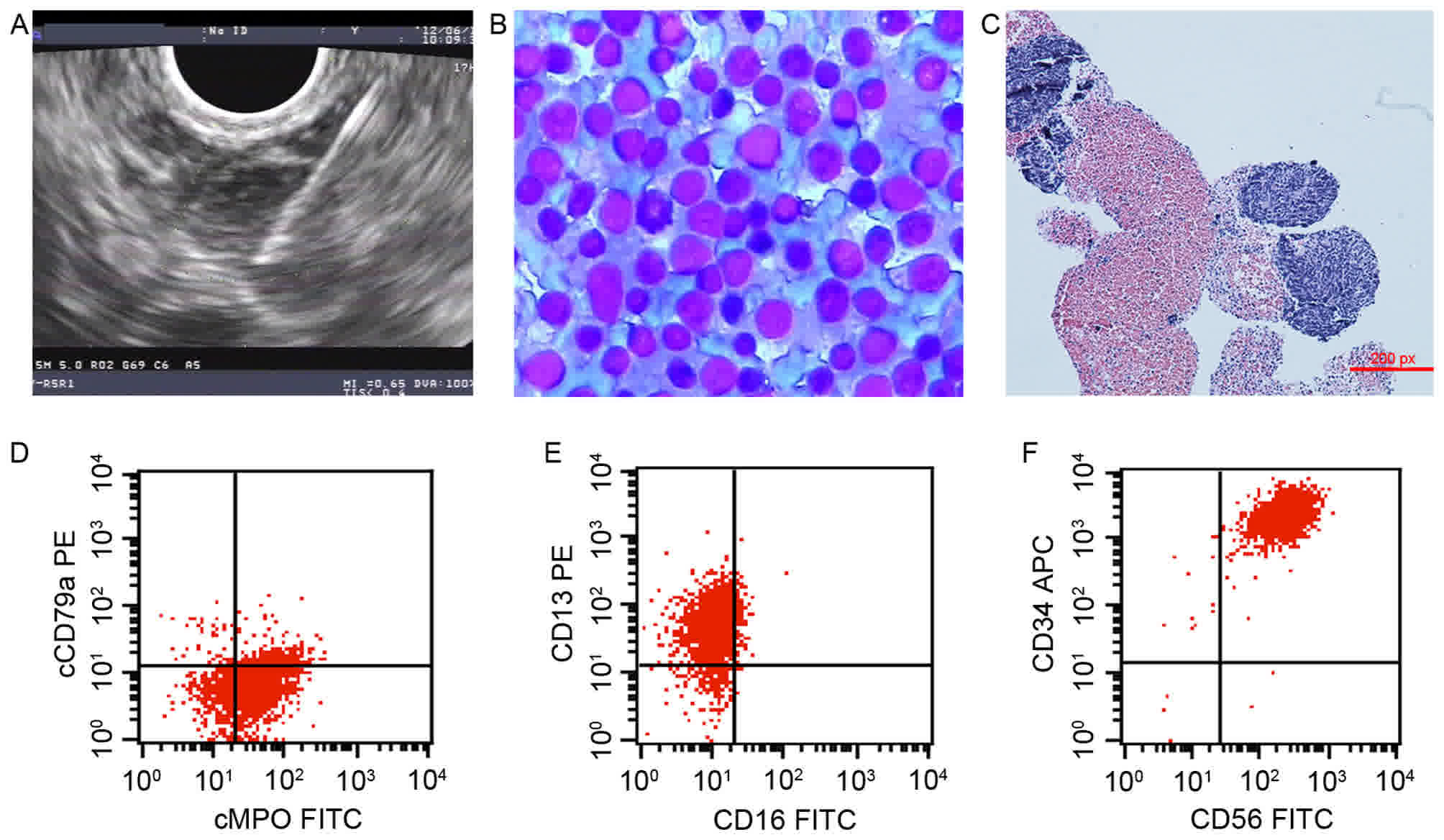 | Figure 2.A case of myeloid leukemia accompanied
by extramedullary infiltration, diagnosed using EUS-FNA combined
with FCM. (A) EUS image of retroperitoneal lymphadenopathy; EUS-FNA
was performed using a 22-gauge needle. (B) Cytology identified the
active proliferation of immature lymphocytes, suspected to be
non-Hodgkin's lymphoma (Liu's stain; magnification, ×400). (C)
Pathology revealed small, round cells (hematoxylin and eosin stain;
magnification, ×100). (D) A FCM scatter plot with cCD79a/cMPO
revealed cCD79a−/cMPO+ cells, which suggested
that the abnormal cells were derived from the myeloid hematopoietic
cells. (E) A FCM scatter plot for CD13/CD16 revealed
CD13+/CD16− cells, which suggested that the
abnormal cells were derived from granulocytes. (F) FCM scatter plot
for CD34/CD56 revealed CD13+/CD16+ cells,
which suggested the abnormal cells were precursors. APC,
allophycocyanin; PE, phycoerythrin; FITC, fluorescein
isothiocyanate; EUS-FNA, endoscopic ultrasound-guided fine-needle
aspiration; CD, cluster of differentiation; FCM, flow cytometry;
cMPO, myeloperoxidase on the cell membrane. |
Efficacy of EUS-FNA for benign
lymphadenopathy
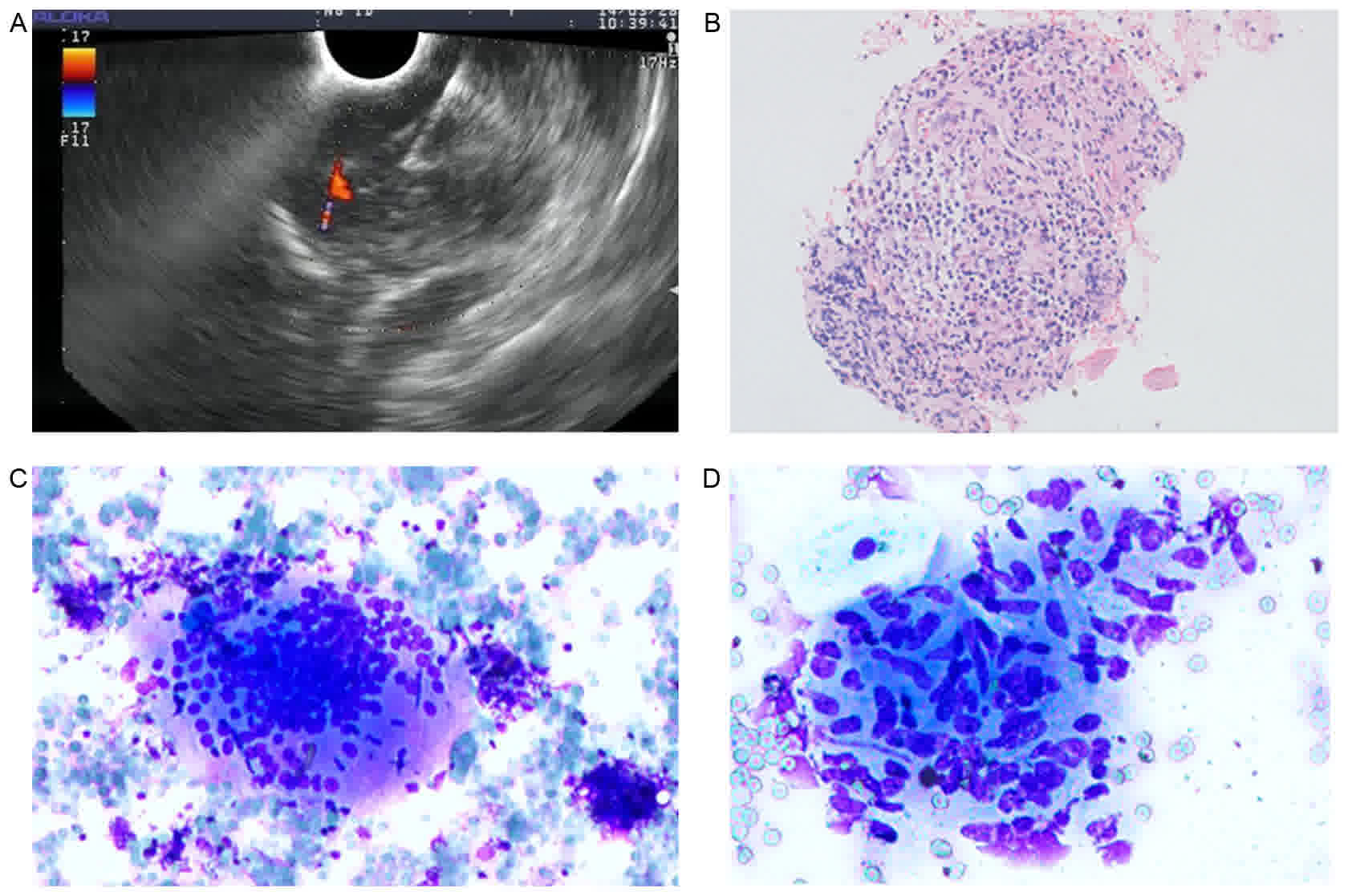
For the patients with benign lymphadenopathy, the
median follow-up period was 10.2 months (range 9–48 months). The
sensitivity, specificity, PPV, NPV and accuracy of EUS-FNA for
benign lymphadenopathy were 58.5, 100.0, 100.0, 81.9 and 85.6%,
respectively. Tuberculosis (n=21) was the most common etiology,
with the exception of a nonspecific inflammatory condition (n=27).
The diagnosis of tuberculosis in 8 patients depended on the
histological identification of granulomatous lymphadenitis without
acid-fast bacilli (Fig. 3). The
sensitivity, specificity, PPV, NPV and accuracy of EUS-FNA
assessing tuberculosis were 38.1, 100.0, 100.0, 91.7 and 92.2%,
respectively.
Complications
None of the patients experienced any severe peri- or
post-procedural complications, as previously defined (17), including hemorrhage or infection.
Discussion
EUS-FNA may influence patient management, as a
doctor will give patients different advice according to the results
of EUS-FNA. For example if the results show benign disease, the
doctor may suggest follow-up or conservative treatment. However, if
the results indicate malignant disease, the doctor may suggest
aggressive treatment. The diagnostic ability of EUS-FNA in regards
to lymphadenopathies is well established (3,18). The
present retrospective study of 154 patients is one of the largest
studies conducted on the topic, to the best of our knowledge. The
data collected suggest that EUS-FNA is an efficient and safe method
for assessing mediastinal and intra-abdominal lymphadenopathies of
unknown origin. In the present study, 65.4% of the enlarged lymph
nodes were determined to be malignant. Elderly and male patients
were identified to possess an increased risk of malignant disease
and, in addition, lymphadenopathy in the region of the celiac axis
was more likely to be caused by malignant disease. Echo-features
are an important assessment during EUS; however, criteria for their
assessment to predict malignant lymph node invasion have yet to be
established. Although Catalano et al (19) suggested that a number of
echo-features, including hypoechoic, sharp borders, rounded contour
and size >10 mm, were associated with malignancy, the
conclusions were not supported by similar studies (20,21). The
results of the present study did not indicate an association
between echo-features and malignant lymphadenopathy; however, the
size of malignant lymph nodes were significantly increased compared
with benign lymph nodes.
Taking into consideration the anatomical and
technical challenges associated with accessing the intra-abdomen or
mediastinum, the application of EUS-FNA may benefit the patients
with lymph node metastasis or lymphoma more than others (15). In the present study, an increased
proportion of the enlarged lymph nodes located in the mediastinum
were metastatic lymph nodes, whereas enlarged lymph nodes caused by
lymphoma were predominantly located around the celiac axis. In
addition, metastatic lymph nodes were larger and exhibited
echogenic focus, whereas enlarged lymph nodes caused by lymphoma
were characterized by lesion fusion and homogeneous echogenicity.
These results may provide insight into conducting a differential
diagnosis between metastatic lymph nodes and lymphoma in the
clinical work-up.
Patients with benign lymphadenopathies do not
require intensive treatment; typically, routine patient follow-up
is sufficient, depending on the nature of the pathology. By
contrast, the patients diagnosed with malignancy require the
determination of tumor origin and are subsequently referred for
surgical resection when possible, chemo/radiation therapy and/or
appropriate palliative care (4,20). PET-CT
is considered to be a valuable predictive and prognostic tool for
patients with malignancy; however, its sensitivity and NPV are poor
(22), and the biopsy result remains
the key in guiding the clinician's management choice (17). Consistent with a previous study by
Dewitt et al (23), the
present study demonstrated that EUS-FNA improved the detection of
the postoperative recurrence of malignancy, potentially allowing
for cancer staging to be performed prior to surgery.
FCM technology allows for the assessment of abnormal
cell phenotypes and thus improves the sensitivity, specificity and
accuracy of EUS-FNA in diagnosing primary or recurrent lymphoma
(1,24,25). In
the present study, FCM was performed on samples from 52 patients
with suspicions of lymphoma. The sensitivity, specificity, PPV, NPV
and accuracy of EUS-FNA combined with FCM for lymphoma were 84.2,
100, 100, 91.7 and 94.2%, respectively. The overall efficacy was
markedly increased compared with pathological and cytological
analyses.
Another advantage of the combined EUS-FNA and FCM
analysis is that it typically provides a sufficient specimen to
allow further lymphoma subtyping, so that patients may be given the
appropriate therapy (26). Consistent
with a previous study on subtyping B-NHL (3), the present study demonstrated that
EUS-FNA in combination with FCM markedly improved the diagnosis
efficiency in cases of deep-seated lymphoma; 84.2% of the patients
with lymphoma were diagnosed with B-NHL, and this method correctly
subtyped 50% of B-NHL cases.
There are several limitations for EUS-FNA as an
independent tool to provide a definitive diagnosis of lymphoma.
Firstly, the diagnosis of HL requires integration of
cytomorphology, immunophenotypical and clinical features, and thus
may continue to require open biopsies for diagnosis and
classification (12). In the present
study, 2 cases of HL were ultimately diagnosed using excisional
biopsy. Secondly, the diagnosis of T cell lymphomas could not be
performed with FCM due to the lack of specific antibodies for
detection (12,13). T cell lymphoma rarely occurs in the
gastrointestinal tract, mediastinum or retroperitoneum (27); the present study identified only 1
case of T cell lymphoma, which was eventually determined by open
biopsy. Third, given the reliance on adequate material for FCM
analysis, the quality of sampling requires further improvement. A
total of ≥3 passes from several angles of the lymph nodes may be
necessary to obtain adequate samples (12). In addition, avoiding necrotic tissue
and blood contamination during sampling is critical.
In the present study, a rare case of myeloid
leukemia with extramedullary leukemic cell infiltration was
identified. The patient presented with abdominal pain in the
absence of typical myeloid leukemia symptoms, including fever,
anemia, bleeding and infection. Although malignant myeloid
precursor cells have been demonstrated to infiltrate and
proliferate in multiple organ systems (28), limited methods are available to
confirm diagnosis. To the best of our knowledge, the present study
is the first to demonstrate that EUS-FNA combined with FCM was able
to determine the characteristic phenotype of malignant myeloid
origin of abnormal cells from the enlarged lymph nodes. This
approach may be routinely applied to investigate cases of
myeloproliferative neoplasms with unusual clinical
manifestations.
For benign lymphadenopathy, extra-pulmonary
tuberculosis was the most common etiology besides a nonspecific
inflammatory condition in the present study (21 cases). EUS-FNA
appeared to be an efficient method for obtaining pathological
samples and distinguishing between tuberculosis-induced necrosis
and necrosis resulting from malignancy. The diagnostic accuracy in
the cohort from the present study was 92.2%; however, the detailed
diagnostic criteria for extra-pulmonary tuberculosis based on
EUS-FNA require further study and documentation (2,29,30).
The present study had certain limitations. It was a
retrospective study, and surgical pathology was not available for
the majority of patients at the time of diagnosis. However,
clinical follow-ups were performed for ≥9 months.
In conclusion, EUS-FNA is associated with high
diagnostic accuracy and low complication rates for evaluating cases
of mediastinal and intra-abdominal malignant lymphadenopathy.
EUS-FNA in combination with FCM as a minimally invasive and highly
sensitive tool should be routinely performed to determine lymphoma,
in addition to examining enlarged celiac axis lymph nodes in
elderly males, who exhibit an increased risk of malignancy based on
the data of the present study.
Acknowledgements
The authors wish to thank all the staff at the
Digestive Endoscopy Center of Tongji Hospital (Wuhan, China) for
providing the clinical data.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Author's contributions
JW and BC conceived the study and prepared a draft
manuscript. QC and XW assisted with data collection and
modification of the manuscript. YW and WH were operational
assistants of EUS-FNA and assisted with data collection. All
authors contributed to the study design and commented on the
manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by The Ethics
Committee of Tongji Hospital and informed consent was obtained from
each patient or their legally authorized representative.
Consent for publication
Informed consent was obtained from each patient or
their legally authorized representative.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Pugh JL, Jhala NC, Eloubeidi MA, Chhieng
DC, Eltoum IA, Crowe DR, Varadarajulu S and Jhala DN: Diagnosis of
deep-seated lymphoma and leukemia by endoscopic ultrasound-guided
fine-needle aspiration biopsy. Am J Clin Pathol. 125:703–709. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Puri R, Vilmann P, Sud R, Kumar M, Taneja
S, Verma K and Kaushik N: Endoscopic ultrasound-guided fine-needle
aspiration cytology in the evaluation of suspected tuberculosis in
patients with isolated mediastinal lymphadenopathy. Endoscopy.
42:462–467. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nakahara O, Yamao K, Bhatia V, Sawaki A,
Mizuno N, Takagi T, Shimizu Y, Koshikawa T, Yatabe Y and Baba H:
Usefulness of endoscopic ultrasound-guided fine needle aspiration
(EUS-FNA) for undiagnosed intra-abdominal lymphadenopathy. J
Gastroenterol. 44:562–567. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hussain T, Salamat A, Farooq MA, Hassan F
and Hafeez M: Indications for endoscopic ultrasound and diagnosis
on fine-needle aspiration and cytology. J Coll Physicians Surg Pak.
19:223–227. 2009.PubMed/NCBI
|
|
5
|
Larsen SS, Vilmann P, Krasnik K, Dirksen
A, Clementsen P, Skov BG, Jacobsen GK, Lassen U, Eigtved A,
Berthelsen AK, et al: A comparison of endoscopic ultrasound guided
biopsy and positron emission tomography with integrated computed
tomography in lung cancer staging. Curr Health Sci J. 35:5–12.
2009.PubMed/NCBI
|
|
6
|
Strand DS, Jeffus SK, Sauer BG, Wang AY,
Stelow EB and Shami VM: EUS-guided 22-gauge fine-needle aspiration
versus core biopsy needle in the evaluation of solid pancreatic
neoplasms. Diagn Cytopathol. 42:751–758. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mehmood S, Loya A and Yusuf MA: Clinical
utility of endoscopic ultrasound-guided fine-needle aspiration in
the diagnosis of mediastinal and intra-abdominal lymphadenopathy.
Acta Cytol. 57:436–442. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jhala NC, Jhala D, Eltoum I, Vickers SM,
Wilcox CM, Chhieng DC and Eloubeidi MA: Endoscopic
ultrasound-guided fine-needle aspiration biopsy: A powerful tool to
obtain samples from small lesions. Cancer. 102:239–246. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chen VK and Eloubeidi MA: Endoscopic
ultrasound-guided fine needle aspiration is superior to lymph node
echofeatures: A prospective evaluation of mediastinal and
peri-intestinal lymphadenopathy. Am J Gastroenterol. 99:628–633.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Devereaux BM, Leblanc JK, Yousif E, Kesler
K, Brooks J, Mathur P, Sandler A, Chappo J, Lehman GA, Sherman S,
et al: Clinical utility of EUS-guided fine-needle aspiration of
mediastinal masses in the absence of known pulmonary malignancy.
Gastrointest Endosc. 56:397–401. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sato M, Shirakami G and Fukuda K:
Comparison of general anesthesia and monitored anesthesia care in
patients undergoing breast cancer surgery using a combination of
ultrasound-guided thoracic paravertebral block and local
infiltration anesthesia: A retrospective study. J Anesth.
30:244–251. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Meda BA, Buss DH, Woodruff RD, Cappellari
JO, Rainer RO, Powell BL and Geisinger KR: Diagnosis and
subclassification of primary and recurrent lymphoma. The usefulness
and limitations of combined fine-needle aspiration cytomorphology
and flow cytometry. Am J Clin Pathol. 113:688–699. 2000.PubMed/NCBI
|
|
13
|
Young NA, Al-Saleem TI, Ehya H and Smith
MR: Utilization of fine-needle aspiration cytology and flow
cytometry in the diagnosis and subclassification of primary and
recurrent lymphoma. Cancer. 84:252–261. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Deans JP and Polyak MJ: FMC7 is an epitope
of CD20. Blood. 111(2492–2493): 24942008.
|
|
15
|
Jamil LH, Kashani A, Scimeca D, Ghabril M,
Gross SA, Gill KR, Hasan MK, Woodward TA, Wallace MB and Raimondo
M: Can endoscopic ultrasound distinguish between mediastinal benign
lymph nodes and those involved by sarcoidosis, lymphoma, or
metastasis? Dig Dis Sci. 59:2191–2198. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nguyen TQ, Kalade A, Prasad S, Desmond P,
Wright G, Hart D, Conron M and Chen RY: Endoscopic ultrasound
guided fine needle aspiration (EUS-FNA) of mediastinal lesions. ANZ
J Surg. 81:75–78. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
ASGE Standards of Practice Committee, .
Early DS, Acosta RD, Chandrasekhara V, Chathadi KV, Decker GA,
Evans JA, Fanelli RD, Fisher DA, Fonkalsrud L, et al: Adverse
events associated with EUS and EUS with FNA. Gastrointest Endosc.
77:839–843. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yasuda I, Tsurumi H, Omar S, Iwashita T,
Kojima Y, Yamada T, Sawada M, Takami T, Moriwaki H and Soehendra N:
Endoscopic ultrasound-guided fine-needle aspiration biopsy for
lymphadenopathy of unknown origin. Endoscopy. 38:919–924. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Catalano MF, Sivak MJ Jr, Rice T, Gragg LA
and Van Dam J: Endosonographic features predictive of lymph node
metastasis. Gastrointest Endosc. 40:442–446. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kanamori A, Hirooka Y, Itoh A, Hashimoto
S, Kawashima H, Hara K, Uchida H, Goto J, Ohmiya N, Niwa Y and Goto
H: Usefulness of contrast-enhanced endoscopic ultrasonography in
the differentiation between malignant and benign lymphadenopathy.
Am J Gastroenterol. 101:45–51. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Song HJ, Kim JO, Eun SH, Cho YD, Jung IS,
Cheon YK, Moon JH, Lee JS, Lee MS, Shim CS, et al: Endoscopic
ultrasonograpic findings of benign mediastinal and abdominal
lymphadenopathy confirmed by EUS-guided fine needle aspiration. Gut
Liver. 1:68–73. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
De Potter T, Flamen P, Van Cutsem E,
Penninckx F, Filez L, Bormans G, Maes A and Mortelmans L:
Whole-body PET with FDG for the diagnosis of recurrent gastric
cancer. Eur J Nucl Med Mol Imaging. 29:525–529. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dewitt J, Ghorai S, Kahi C, Leblanc J,
McHenry L, Chappo J, Cramer H, McGreevy K, Chriswell M and Sherman
S: EUS-FNA of recurrent postoperative extraluminal and metastatic
malignancy. Gastrointest Endosc. 58:542–548. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ribeiro A, Vazquez-Sequeiros E, Wiersema
LM, Wang KK, Clain JE and Wiersema MJ: EUS-guided fine-needle
aspiration combined with flow cytometry and immunocytochemistry in
the diagnosis of lymphoma. Gastrointest Endosc. 53:485–491. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Nunez AL, Jhala NC, Carroll AJ, Mikhail
FM, Reddy VV, Xian RR and Jhala DN: Endoscopic ultrasound and
endobronchial ultrasound-guided fine-needle aspiration of
deep-seated lymphadenopathy: Analysis of 1338 cases. Cytojournal.
9:142012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kwong YL: Predicting the outcome in
non-Hodgkin lymphoma with molecular markers. Br J Haematol.
137:273–287. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zinzani PL, Colecchia A, Festi D,
Magagnoli M, Larocca A, Ascani S, Bendandi M, Orcioni GF,
Gherlinzoni F, Albertini P, et al: Ultrasound-guided core-needle
biopsy is effective in the initial diagnosis of lymphoma patients.
Haematologica. 83:989–992. 1998.PubMed/NCBI
|
|
28
|
Neiman RS, Barcos M, Berard C, Bonner H,
Mann R, Rydell RE and Bennett JM: Granulocytic sarcoma: A
clinicopathologic study of 61 biopsied cases. Cancer. 48:1426–1437.
1981. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Bhandarkar DS, Shah RS, Katara AN, Shankar
M, Chandiramani VA and Udwadia TE: Laparoscopic biopsy in patients
with abdominal lymphadenopathy. J Minim Access Surg. 3:14–18. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Puri R, Mangla R, Eloubeidi M, Vilmann P,
Thandassery R and Sud R: Diagnostic yield of EUS-guided FNA and
cytology in suspected tubercular intra-abdominal lymphadenopathy.
Gastrointest Endosc. 75:1005–1010. 2012. View Article : Google Scholar : PubMed/NCBI
|