Introduction
Head and neck squamous cell carcinoma (HNSCC) is one
of the most common malignant tumor in the world, which occurs in
upper respiratory and upper digestive tract. HNSCC includes cancer
of the lip, oral cavity, pharynx, larynx, hypopharynx, salivary
gland, nose, head and facial soft tissue, and thyroid (1). In recent years, the incidence of HNSCC
has been increasing (2). Management
strategies for HNSCC are varied, including surgery, radiotherapy,
chemotherapy, biological therapy and traditional Chinese medicine
(3). Despite the integrated
application of these therapies, the 5-year survival rate of HNSCC
has not increased substantially in recent years (4). However, the combination of surgery,
radiotherapy and chemotherapy can severely reduce the quality of
life of patients with the disease (5).
Compared with normal cells, cancer cells with rapid
growth exhibit a higher demand for iron (6). Generally, the expression of transferrin
receptor 1 (TfR1) is higher in cancer cells compared with normal
cells, which allows cancer cells to absorb iron from transferrin at
a higher rate (7), and this results
in selectively increased iron chelation (8). Previous studies have shown that iron
chelators confer anti-tumor activity as they can chelate metal ions
(2,9).
Di-2-pyridylketone thiosemicarbazone (DpT) is an
iron chelator with good anti-tumor activity and selectivity
(10–12), which was first reported by Yuan et
al (13).
Di-2-pyridylketone-4,4,-dimethyl-3-thiosemicarbazone (Dp44mT), one
of the most effective chelators of the DpT family, has been shown
to exhibit a substantial inhibitory effect in transplanted tumors
in mice (14)
Di-2-pyridylketone-4-cyclohexyl-4-methyl-3-thiosemicarbazone (DpC)
is a second-generation iron chelator. DpC exhibits a synergistic
effect with chemotherapy on mouse lung tumors and a potential
independent antitumor activity (8).
In comparison to the first-generation iron chelator Dp44mT, DpC
exhibits advantages in the treatment of tumors (3). At present, there are a limited number of
studies on the anti-tumor activity of DpC and Dp44mT in HNSCC. The
present study aims to clarify the anti-tumor effect of DpC and
Dp44mT on several HNSCC cell lines in vitro, and investigate
the mechanisms involved.
Materials and methods
Chemical regents
DpC, Dp44mT and dimethyl sulfoxide (DMSO) were
obtained from Sigma-Aldrich (Merck KGaA, Darmstadt, Germany). DpC
and Dp44mT were dissolved in DMSO (final concentration, 20 mM) and
stored at −20°C. Cell counting kit-8 was purchased from Dojindo
Molecular Technologies, Inc. (Kumamoto, Japan). The Annexin
V-Propidium Iodide (PI) Double Staining assay kit was used for
apoptosis detection by flow cytometry (Hangzhou Lianke
Biotechnology Co., Ltd., Zhejiang, China). Antibodies against
GAPDH, phosphorylated (p)-serine-protein kinase ATM (ATM),
p-serine/threonine-protein kinase Chk1 (Chk-1),
p-serine/threonine-protein kinase ATR (ATR), p-Chk-2, poly
(ADP-ribose) polymerase, p-histone H2AX, breast cancer type 1
susceptibility protein (BRCA1), p-tumor protein P53 (P53) were all
obtained from Cell Signaling Technology, Inc. (Danvers, MA,
USA).
Cell culture
The HNSCC Cal-27, SCC-9 and FaDu cell lines were
cultured in Dulbecco's modified Eagle's Medium (DMEM; HyClone;)
with 10% fetal bovine serum (Gibco; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA) in 37°C at 5% CO2. The cells in the
logarithmic phase of growth were used in the experiment.
Cytotoxicity test
FaDu, Cal-27 and SCC-9 cells (1×103) in
the logarithmic growth phase were seeded into wells in a 96-well
plate. A range of concentrations of DpC (0, 1, 5, 10 and 50 µM) and
Dp44mT (0, 1, 5, 10 and 50 µM) were added to the cells for
treatment for 24 h. Next, 10 µl/well CCK-8 reagent was added to
96-well plates, which were incubated at 37°C for 1 h, then the
optical density (OD) values were detected using a microplate reader
at a wavelength of 450 nm. The experiment was repeated three times
independently. The effect of DpC and Dp44mT on cell activity was
measured by normalizing the OD value of the experimental group to
the OD value of the control group (0 nM), and the concentration
required to inhibit viability by 50% (IC50) was
calculated.
Flow cytometry analysis
FaDu, Cal-27 and SCC-9 HNSCC cells in the
logarithmic growth phase were treated with a range of
concentrations of DpC (0, 2.5, 5 and 7.5 µM) and Dp44mT (0, 2.5, 5
and 7.5 µM) for 24 h and the cells were collected. The adherent
cells and supernatant were washed with precooled PBS twice, and
then the cells were resuspended with 500 µl 1X Binding buffer. Next
5 µl Annexin V-fluorescein isothiocyanate (Annexin V-FITC) and 10
µl propidium iodide were added for staining at room temperature for
15 min. All the regents used in this experiment were contained in
the Annexin V/PI kit. A flow cytometer was used to detect the
levels of cell apoptosis. The software CellQuest Pro (BD
Biosciences, San Jose, CA, USA) was used for the analysis.
Hoechst staining
The Cal-27 cells in the logarithmic growth phase
were collected and seeded into 6-well plates, and the cells were
treated with a range of concentrations of DpC (0, 2.5, 5 and 7.5
µM) at 37°C for 24 h. The cells were then washed once with PBS, and
1 ml Hoechst staining solution was added per well (Beyotime
Institute of Biotechnology, Jiangsu, China). The cells were
incubated in the dark for 30 min and then washed twice with PBS.
The cells were then observed with a fluorescent microscope (×40).
The staining results were quantified using Image Studio v3.1
software (LI-COR Biosciences, Lincoln, NE, USA)
Western blot analysis
Cal-27 HNSCC cells in the logarithmic growth phase
were treated with DpC (0, 2.5, 5 and 7.5 µM) for 24 h. Next, the
cells were collected, and the total protein was extracted. Cells
were harvested and lysed in the protein lysate buffer (Beyotime
Institute of Biotechnology). A bicinchoninic acid assay (Pierce™
BCA Protein Assay kit; cat. no. 23225; Thermo Fisher Scientific,
Inc.) was used to determine the protein concentration. The protein
sample used per lane was 25 µg. Lysates were resolved by SDS-PAGE
on a 10% gel. The proteins were transferred onto the PVDF membrane
by electrophoresis and electrotransfer. Following incubation with
the blocking solution (5% non-fat milk powder) at room temperature
for 2 h, the primary antibodies against GAPDH, p-ATM, p-Chk-1,
p-ATR p-Chk-2, PARP, p-histone H2A.X, BRCA1 and p-P53 were added,
and the membrane was incubated at 4°C overnight. The samples were
washed with TBST three times, and the secondary antibody
[IRDye® 800CW Donkey anti-rabbit IgG (cat. no.
925-32213; LI-COR Biosciences; 1:10,000)] was added for incubation
for 1 h. The membranes were visualized using the Odyssey CLx
Infrared Imaging system (LI-COR Biosciences, Lincoln, NE, USA). And
the western blotting bands were quantified using Image Studio v3.1
software.
Statistical analysis
SPSS v17.0 software (SPSS, Inc., Chicago, IL, USA)
was used for statistical analysis. Data between two groups were
compared using unpaired t-test, and multiple groups were compared
using one way-analysis of variance, post-hoc analysis was performed
with the Tukey test. P<0.05 was considered to indicate a
statistically significant difference.
Results
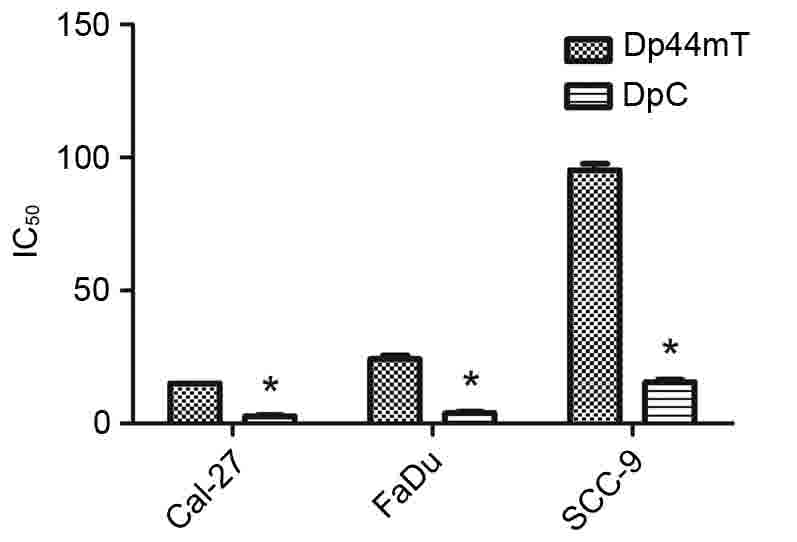
Proliferation of HNSCC cells is
efficiently inhibited by DpC and Dp44mT
To evaluate the effect of DpC and Dp44mT on the
proliferation of HNSCC cell lines in vitro, a cell viability
test was performed using the CCK-8 method (Fig. 1). Gradient concentrations of DpC (0,
1, 5, 10 and 50 µM) and Dp44mT (0, 1, 5, 10 and 50 µM) were used to
treat the FaDu, Cal-27, SCC-9 HNSCC cell lines for 24 h. The
results demonstrated that DpC and Dp44mT had an anti-proliferative
effect on HNSCC cells, and the effect was concentration-dependent.
The IC50 values at 24 h were assessed, and the values
are as follows: FaDu Dp44mT, 24.37 µM and DpC, 3.93 µM; Cal-27
Dp44mT, 15.15 µM and DpC, 2.79 µM; and SCC-9 Dp44mT, 95.36 µM and
DpC, 15.61 µM. The results of the present study indicated the
anti-proliferative effect of DpC was stronger compared with Dp44mT
in HNSCC cells, and that the IC50 of Cal-27 cells was
the lowest for treatment with DpC and Dp44mT, indicating that
Cal-27 cells were the most sensitive to DpC and Dp44mT.
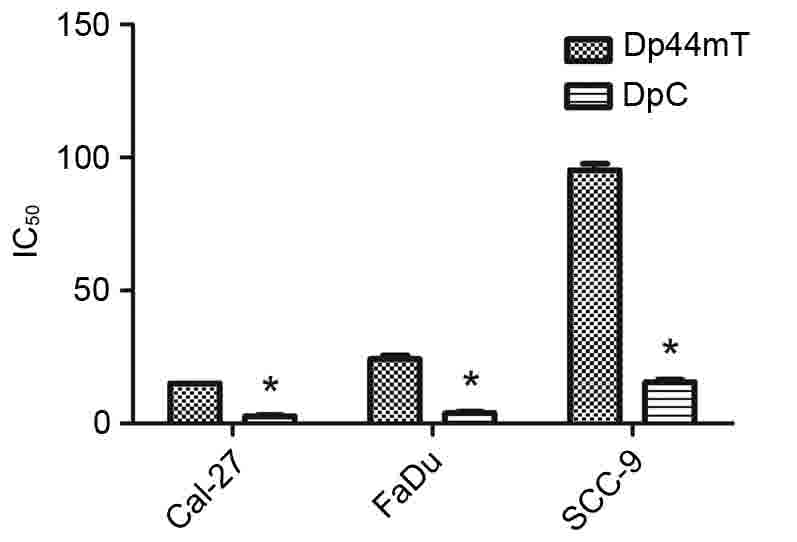 | Figure 1.Dp44mT and DpC inhibit the viability
of Cal-27, FaDu and SCC-9 cells. The Cal-27, SCC-9 and FaDu HNSCC
cell lines were treated with a range of concentrations of DpC (0,
1, 5, 10 and 50 µM) and Dp44mT (0, 1, 5, 10 and 50 µM) for 24 h,
and the viability of these cell lines were subsequently assessed.
The IC50 values at 24 h were assessed, and it was
indicated the anti-proliferative effect of DpC was stronger
compared with Dp44mT in HNSCC cells. *P<0.001 vs. Dp44mT.
Dp44mT, di-2-pyridylketone-4,4,-dimethyl-3-thiosemicarbazone; DpC,
di-2-pyridylketone-4-cyclohexyl-4-methyl-3-thiosemicarbazone;
HNSCC, head and neck squamous cell carcinoma; IC50,
half-maximal inhibitory concentration. |
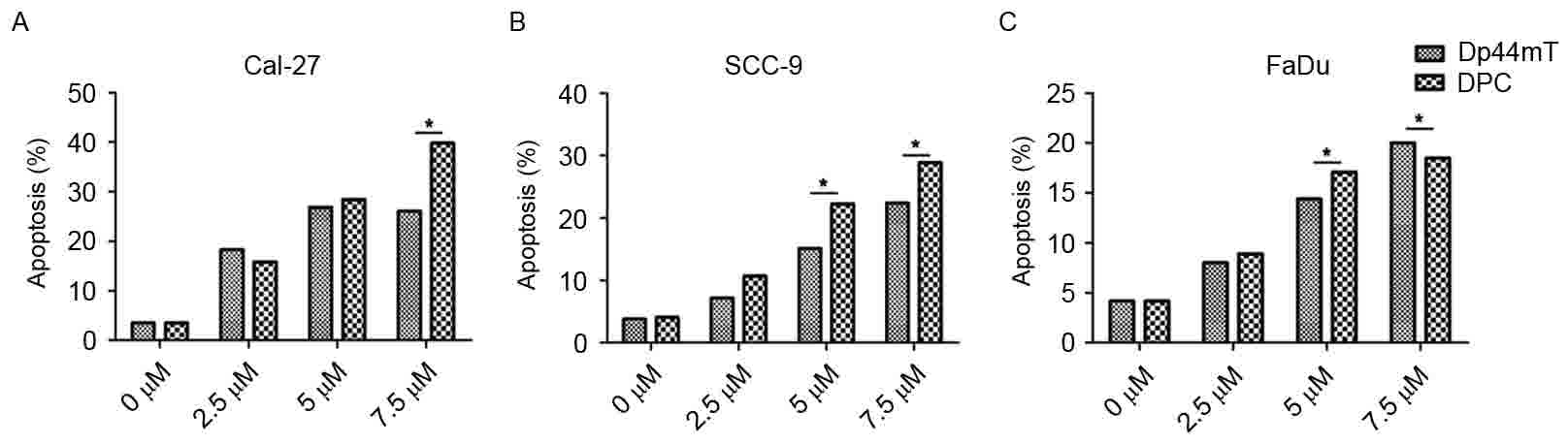
Apoptosis of HNSCC cells is
efficiently induced by DpC and Dp44mT
To determine the effect of DpC and Dp44mT on the
apoptosis of HNSCC cells in vitro, flow cytometry was
performed to detect the proportion of cells in early apoptosis and
late apoptosis were included (Fig.
2). Gradient concentration of DpC (0, 1, 5, 10 and 50 µM) and
Dp44mT (0, 1, 5, 10 and 50 µM) were used to treat HNSCC Cal-27,
SCC-9 and FaDu cell lines for 24 h. The results revealed that the
percentage of apoptotic cells increased with the increase of the
concentration of DpC and Dp44mT, and the effect was
concentration-dependent (Fig. 2). The
percentages of apoptotic cells for 0, 1, 5, 10, 50 µM Dp44mT
treatment were as follows: Cal-27, 3.5, 18.3, 26.8 and 26.1%
(Fig. 2A); SCC-9, 3.8, 7.2, 15.1 and
22.4% (Fig. 2B); FaDu, 4.2, 8.0, 14.4
and 20.0%, respectively (Fig. 2C).
The percentages of apoptotic cells for 0, 1, 5, 10, 50 µM DpC
treatment were as follows: Cal-27, 3.5, 15.8, 28.4, 39.8% (Fig. 2A); SCC-9, 4.1, 10.7, 22.3 and 28.9%
(Fig. 2B); FaDu, 4.2, 8.9, 17.1 and
18.5%, respectively (Fig. 2C). These
findings indicated DpC and Dp44mT were able to promote the
apoptosis of HNSCC cells. The effect of DpC on the apoptosis of
HNSCC cells was greater compared with Dp44mT, and Cal-27 was the
most sensitive cell line to DpC and Dp44mT treatment.
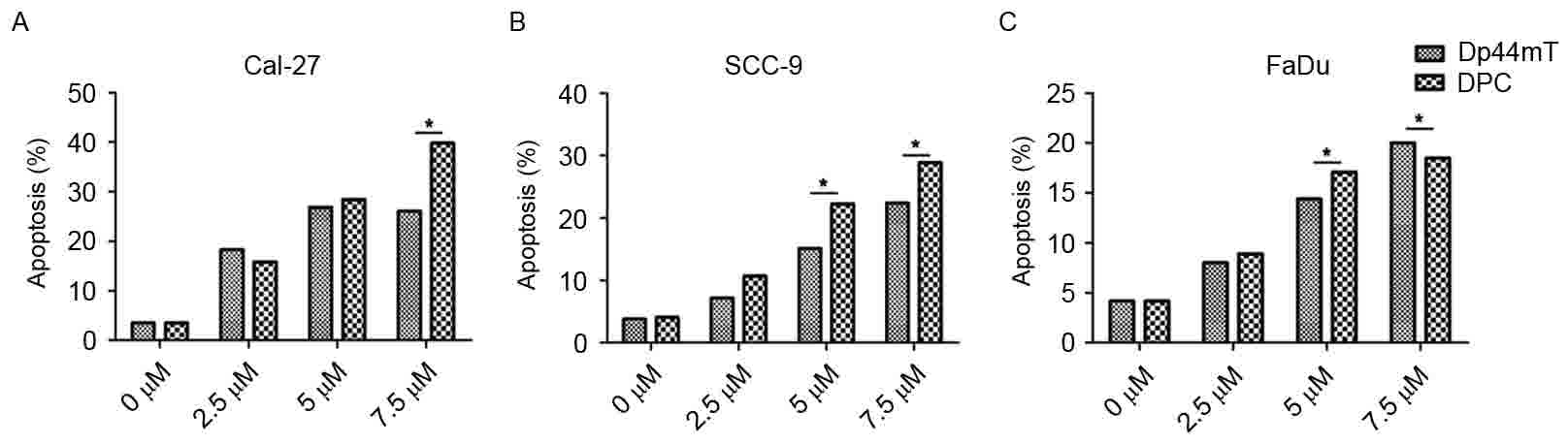 | Figure 2.Dp44mT and DpC promote the apoptosis
of Cal-27, FaDu and SCC-9 cells. DpC (0, 1, 5, 10 and 50 µM) and
Dp44mT (0, 1, 5, 10 and 50 µM) were used to treat Cal-27, SCC-9 and
FaDu HNSCC cells for 24 h. (A) The apoptotic rate of the Cal-27
cells when treated with DpC (0, 1, 5, 10 and 50 µM) and Dp44mT (0,
1, 5, 10 and 50 µM). (B) The apoptotic rate of the SCC-9 cells when
treated with DpC (0, 1, 5, 10 and 50 µM) and Dp44mT (0, 1, 5, 10
and 50 µM). (C) The apoptotic rate of the FaDu cells when treated
with DpC (0, 1, 5, 10 and 50 µM) and Dp44mT (0, 1, 5, 10 and 50
µM). The apoptotic rate of the cells increased with the increase of
the concentration of DpC and Dp44mT, indicating that DpC and Dp44mT
are able to promote the apoptosis of HNSCC cells. The effect of DpC
on the apoptosis of HNSCC cells was stronger compared with Dp44mT.
*P<0.001. Dp44mT,
di-2-pyridylketone-4,4,-dimethyl-3-thiosemicarbazone; DpC,
di-2-pyridylketone-4-cyclohexyl-4-methyl-3-thiosemicarbazone;
HNSCC, head and neck squamous cell carcinoma. |
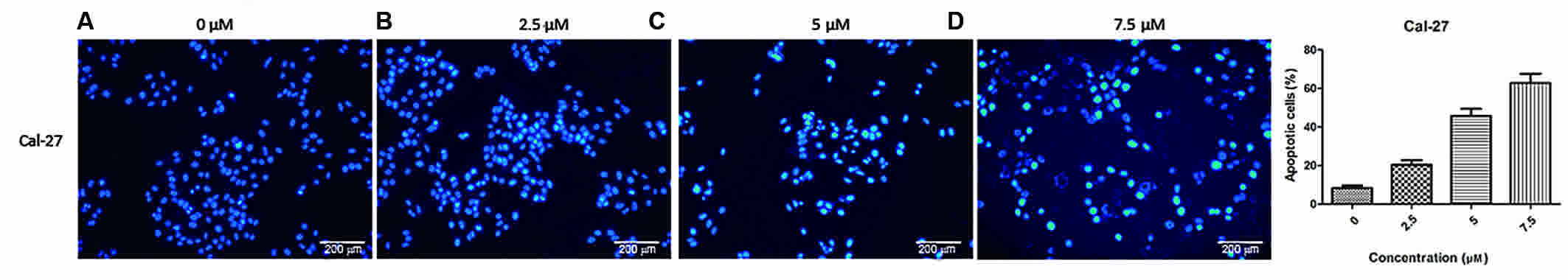
Nuclear damage in Cal-2 cells7
increased with the increase of DpC drug concentration
Flow cytometric analysis revealed a significant
increase in apoptosis upon treatment with increasing drug
concentrations. Compared with the first-generation iron-chelating
agent Dp44mT, DpC had a more marked effect on the regulation of
proliferation and apoptosis of HNSCC cell lines, particularly in
Cal-27 cells. In order to confirm this result, the changes in
nuclear morphology in Cal-27 cell line mediated by DpC treatment
was examined by Hoechst staining (Fig.
3). The Cal-27 cell line was observed to be the more sensitive
cell line to DpC. Hoechst is a specific fluorescent DNA probe,
which can be combined with DNA in living cells. The nucleus
exhibits a bright blue fluorescence when excited by ultraviolet
light and viewed with a fluorescence microscope. This experiment
revealed that with increasing concentrations of DpC (0, 2.5, 5 and
7.5 µM) treatment, the proportion of nuclei with bright blue
fluorescence decreased significantly.
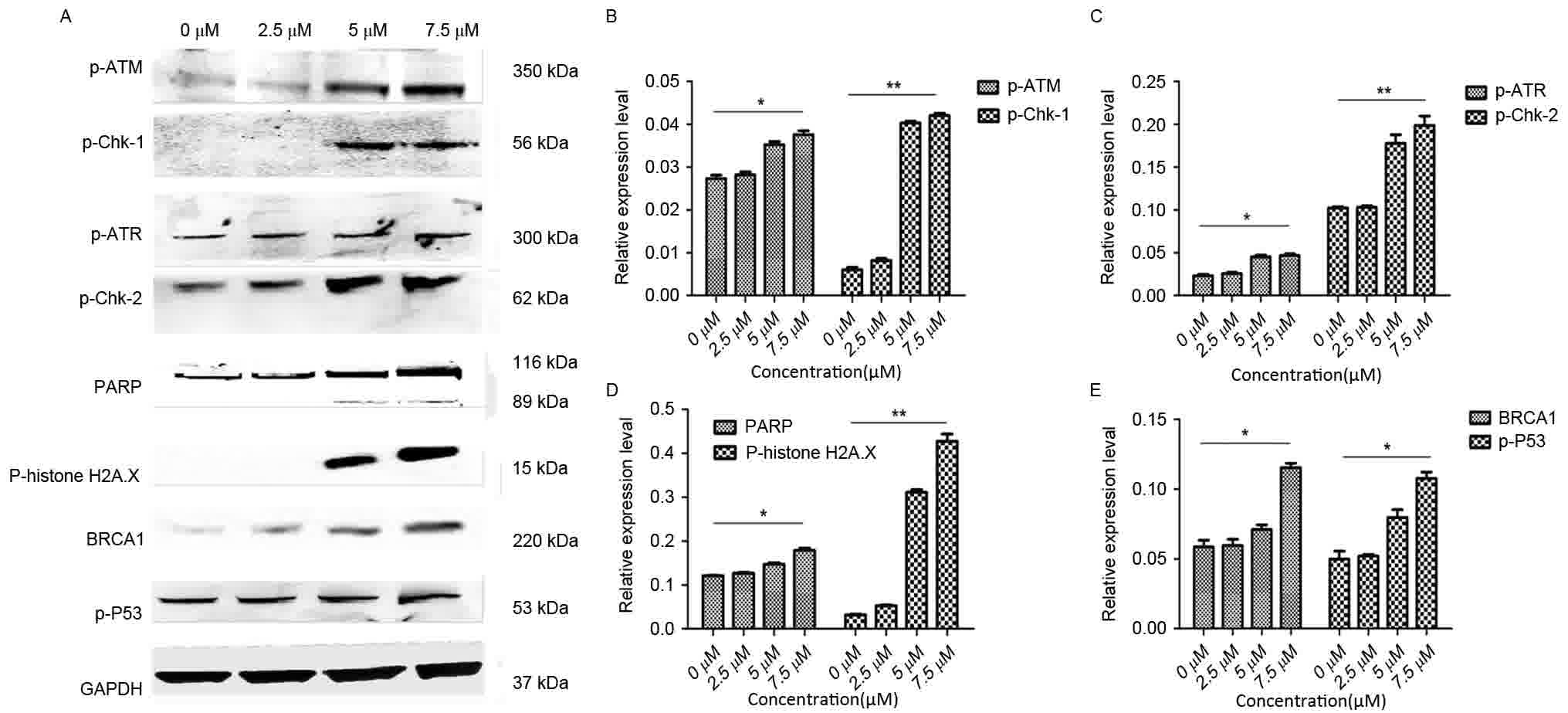
Expression of proteins associated with
DNA damage was upregulated in Cal-27 following treatment with
DpC
As aforementioned, DpC has an important role in
regulating proliferation and apoptosis of HNSCC cells. Therefore,
the expression of several important proteins in the DNA damage
pathway associated with proliferation and apoptosis may also change
accordingly. Western blot analysis was performed to detect the
expression of proteins that are associated with DNA damage
(Fig. 4). GAPDH was used as a loading
control. Cal-27 cells were treated with an increasing concentration
of DpC (0, 2.5, 5 and 7.5 µM). It as observed that PARP, a protein
that in involved in the monitoring of DNA damage, was upregulated
as the concentration of DpC increased. Furthermore, the levels of
p-ATM and p-ATR proteins were upregulated, and it was hypothesized
that ATM and ATR carried out DNA damage repair in two ways after
DNA damage has occurred. Which resulted in increased expression of
p-histone H2AX and BRCA1 (15). In
addition, the expression of p-Chk-1, p-Chk-2 and p-P53 were also
upregulated.
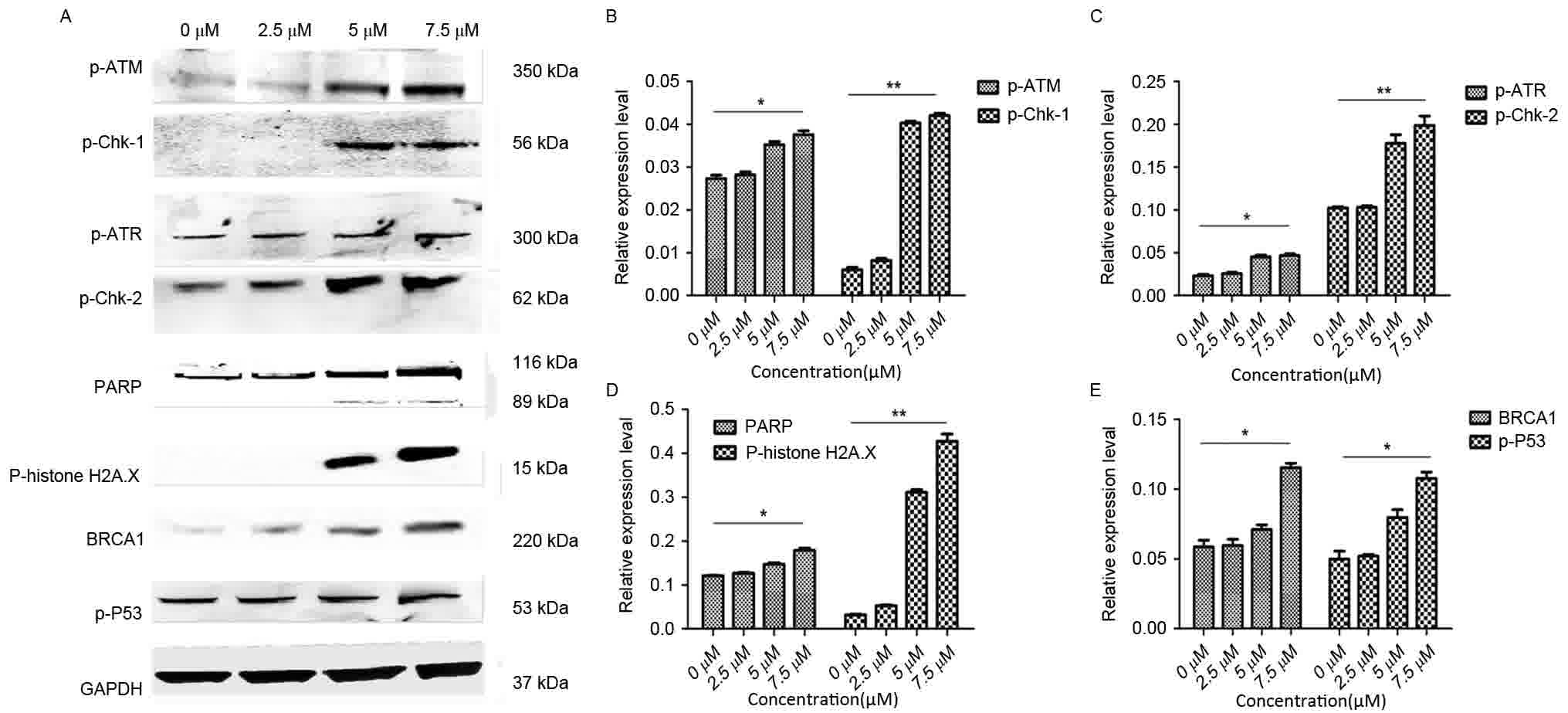 | Figure 4.Changes in the expression of proteins
in the DNA-damage-associated pathway following DpC treatment in
Cal-27 cells. (A) Western blot analysis was performed to detect the
expression of the indicated proteins, and GAPDH was used as a
loading control. Cal-27 cells treated with a range of
concentrations of DpC (0, 2.5, 5 and 7.5 µM). (B) Statistical view
of western blot analysis for p-ATM and p-Chk-1. (C) Statistical
views of western blot analysis for p-ATR and p-Chk-2. (D)
Statistical views of western blot analysis for PARP and p-histone
H2A.X. (E) Statistical views of western blot analysis for BRCA1 and
p-P53. As the concentration of DpC increased, the expression of (B)
p-ATM, (C) p-ATR, (D) PARP, (E) BRCA1 and p-P53 also increased.
*P<0.05; **P<0.01. DpC,
di-2-pyridylketone-4-cyclohexyl-4-methyl-3-thiosemicarbazone; p-,
phosphorylated; PARP, poly (ADP-ribose) polymerase; BRCA1, breast
cancer type 1 susceptibility protein; P53, tumor protein P53. |
Discussion
Thiosemicarbazone compounds with antitumor activity
were initially identified by Hamre et al (16) in 1950. The DpT group of compounds,
which includes Dp44mT and DpC, were derived from an analysis of
structural activity associations over a period of 20 years and were
derived from assessment of the pyridoxal isonicotinoyl hydrazone
analogue group of agents (17–20). Since
the derivation of DpT compounds, numerous types of biological
activity, including antiviral, antibacterial, antitumor,
anti-leprosy, anti-tubercular and anti-malarial activities, were
reported in multiple studies (21–25). The
N1NH(CS)N4H structure is the key active structure, and
is necessary for the biological activity of the compound. Due to
the presence of N, S and other elements, and the C=N group,
thiosemicarbazones readily form stable complexes with a variety of
metal ions. The biological activity of thiosemicarbazones was
markedly enhanced following the formation of complexes,
particularly in terms of anticancer and anti-HIV activity (26). Compared with
3-aminopyridine-2-carboxaldehyde thiosemicarbazone (3-AP), the
double-ketone thiosemicarbazone compounds, DpTs, are better ferrous
ion chelating agents, which are able to inhibit tumor occurrence
and development by chelating iron required for tumor growth
(10). Compared with the commonly
used iron chelator 3-aminopyridine-2-carboxaldehyde
thiosemicarbazone (3-AP), DpTs possess significantly higher
antitumor activity and selectivity. As DpTs are more selective
compounds, they also lack the side effects that are caused by 3-AP,
which include methemoglobinemia and hypoxia (27). As a first-generation DpT drug, Dp44mT
was reported to effectively inhibit breast and lung cancer cells by
Lovejoy et al (28). Kovacevic
et al (29) demonstrated that
the second-generation DpT drug DpC exhibited a superior antitumor
activity in pancreatic cancer cells compared with Dp44mT.
In the present study, DpC and Dp44mT efficiently
inhibited the proliferation of HNSCC cell lines in vitro and
induced apoptosis in these cells. DpC was able to effectively
inhibit proliferation and induce the apoptosis of HNSCC cells, and
the effects were greater compared with the first-generation DpT,
Dp44mT. These antitumor functions may be mediated via the
regulation of the expression of DNA damage signaling
pathway-associated proteins p-ATM, Chk-1, p-ATR, p-Chk-2, PARP,
p-histone, H2A.X, BRCA1 and p-P53.
The DNA-damage signaling pathway is closely
associated with the occurrence and development of HNSCC. DNA damage
is caused by DNA modifications that can initiate apoptosis, induce
DNA double-strand breaks (DSBs) and block DNA replication, which
can cause DSBs (30). It has been
widely reported that ATM, ATR, nibrin, meiotic recombination 11
homolog 1, Rad50, PARP, histone H2AX, BRCA1, topoisomerase
IIβ-binding protein 1, p-Chk-1, p-Chk-2, and p-P53 are involved in
the repair of DNA damage (31). ATM
is primarily activated by DSBs, whereas ATR is primarily activated
by blocks in DNA replication (15).
Chen et al (32) reported that iron mediates the
production of reactive oxygen species, which leads to oxidative
damage of DNA (32). Iron chelators
are able to repair oxidative damage to DNA in cells by chelating
excessive iron normal cells (33).
However, iron is also an essential element required for cellular
metabolism. When iron is required for the growth of tumor cells, it
may also initiate DNA oxidative damage to the tumor cells (34). Therefore, it can be inferred that DpC
is able to inhibit the proliferation of HNSCC cells and induce
apoptosis by regulating the DNA-damage-signaling pathway, which is
closely associated with the occurrence and development of
HNSCC.
To elucidate the association between DNA damage
signaling pathways and antitumor effects of DpC in HNSCC, the HNSCC
cell line Cal-27 was incubated with a range of concentrations of
DpC, and the changes in protein expression levels of the DNA damage
signaling pathway were analyzed. It was also observed that the
expression of PARP, a protein involved in the monitoring of DNA
damage, was upregulated as the concentration of DpC increased. In
addition, the levels of p-ATM and p-ATR proteins were also
upregulated as the concentration of DpC increased, and the
expression of ATM and ATR was hypothesized to be induced once DNA
damage occurred. Furthermore, p-Chk-1 and p-Chk-2 were also
upregulated as the concentration of DpC increased, leading to
increased expression of p-histone H2AX and BRCA1, and the cascade
of pro-apoptotic genes was activated (35). In addition, the expression of P53 was
also upregulated, although the role of P53 in the process requires
further investigation. The results of the present study revealed
that the DNA-damage signaling pathway is closely associated with
the occurrence and development of HNSCC, and DpC is able to cause
DSBs and induce arrest of DNA replication in tumor cells.
Studies have reported that iron chelators are able
to upregulate the expression of N-Myc downstream regulated 1, which
is considered to be an iron-regulated metastasis suppressor
(36,37). Dp44mT and DpC were revealed to
selectively activate the lysosomal apoptotic pathway in cancer
cells by sequestration of redox-active copper, indicating that
treatment with these compounds may represent a novel generalized
strategy for chemotherapeutic intervention against cancer (28,38).
Conventional radiotherapy and chemotherapy cause
damage to normal tissues and organs. Despite the development of
novel chemotherapeutic agents and technologies for radiotherapy,
the side effects of these treatments remain (39). The present study confirmed that DpC is
able to effectively inhibit the proliferation and induce the
apoptosis of HNSCC cells, indicating that DpC may be an effective
drug for the treatment of HNSCC, and that in the future, DpC may be
used for the clinical treatment of HNSCC patients.
Acknowledgements
The present study was supported by a grant from the
National Natural Science Foundation of China (grant no.
81372880).
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
D'Cruz A, Lin T, Anand AK, Atmakusuma D,
Calaguas MJ, Chitapanarux I, Cho BC, Goh BC, Guo Y, Hsieh WS, et
al: Consensus recommendations for management of head and neck
cancer in Asian countries: A review of international guidelines.
Oral Oncol. 49:872–877. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Quach P, Gutierrez E, Basha MT, Kalinowski
DS, Sharpe PC, Lovejoy DB, Bernhardt PV, Jansson PJ and Richardson
DR: Methemoglobin formation by triapine,
di-2-pyridylketone-4,4-dimethyl-3-thiosemicarbazone (Dp44mT), and
other anticancer thiosemicarbazones: Identification of novel
thiosemicarbazones and therapeutics that prevent this effect. Mol
Pharmacol. 82:105–114. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Molinolo AA, Amornphimoltham P, Squarize
CH, Castilho RM, Patel V and Gutkind JS: Dysregulated molecular
networks in head and neck carcinogenesis. Oral Oncol. 45:324–334.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bian X, Xu ZG, Lu CM, Tang PZ and Luo J:
Cancer and surgica l treatment impact the qua lity of life in
patients w ith head and neck cancer. Zhonghua Er Bi Yan Hou Tou
Jing Wai Ke Za Zhi. 40:606–610. 2005.(In Chinese). PubMed/NCBI
|
|
6
|
Padmanabhan H, Brookes MJ and Iqbal T:
Iron and colorectal cancer: Evidence from in vitro and animal
studies. Nutr Rev. 73:308–317. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Miljuš G, Malenković V, Đukanovic B,
Kolundžić N and Nedić O: IGFBP-3/transferrin/transferrin receptor 1
complexes as principal mediators of IGFBP-3 delivery to colon cells
in non-cancer and cancer tissues. Exp Mol Pathol. 98:431–438. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dragset MS, Poce G, Alfonso S,
Padilla-Benavides T, Ioerger TR, Kaneko T, Sacchettini JC, Biava M,
Parish T, Argüello JM, et al: A novel antimycobacterial compound
acts as an intracellular iron chelator. Antimicrob Agents
Chemother. 59:2256–2264. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fang BA, Kovačević Ž, Park KC, Kalinowski
DS, Jansson PJ, Lane DJ, Sahni S and Richardson DR: Molecular
functions of the iron-regulated metastasis suppressor, NDRG1, and
its potential as a molecular target for cancer therapy. Biochim
Biophys Acta. 1845:1–19. 2014.PubMed/NCBI
|
|
10
|
Richardson DR, Sharpe PC, Lovejoy DB,
Senaratne D, Kalinowski DS, Islam M and Bernhardt PV: Dipyridyl
thiosemicarbazone chelators with potent and selective antitumor
activity form iron complexes with redox activity. J Med Chem.
49:6510–6521. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jansson PJ, Kalinowski DS, Lane DJ,
Kovacevic Z, Seebacher NA, Fouani L, Sahni S, Merlot AM and
Richardson DR: The renaissance of polypharmacology in the
development of anti-cancer therapeutics: Inhibition of the ‘Triad
of Death’ in cancer by Di-2-pyridylketone thiosemicarbazones.
Pharmacol Res. 100:255–260. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yu Y, Suryo Rahmanto Y and Richardson DR:
Bp44mT: An orally active iron chelator of the thiosemicarbazone
class with potent anti-tumour efficacy. Br J Pharmacol.
165:148–166. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yuan J, Lovejoy DB and Richardson DR:
Novel di-2-pyridyl-derived iron chelators with marked and selective
antitumor activity: In vitro and in vivo assessment. Blood.
104:1450–1458. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Whitnall M, Howard J, Ponka P and
Richardson DR: A class of iron chelators with a wide spectrum of
potent antitumor activity that overcomes resistance to
chemotherapeutics. Proc Natl Acad Sci USA. 103:14901–14906. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tanaka T, Huang X, Jorgensen E, Traganos
F, Darzynkiewicz Z and Albino AP: ATM activation accompanies
histone H2AX phosphorylation in A549 cells upon exposure to tobacco
smoke. BMC Cell Biol. 8:262007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hamre D, Bernstein J and Donovick R: The
chemotherapy of experimental tuberculosis. II. Thiosemicarbazones
and analogues in experimental tuberculosis in the mouse. J
Bacteriol. 59:675–860. 1950.PubMed/NCBI
|
|
17
|
Richardson DR, Tran EH and Ponka P: The
potential of iron chelators of the pyridoxal isonicotinoyl
hydrazone class as effective antiproliferative agents. Blood.
86:4295–4306. 1995.PubMed/NCBI
|
|
18
|
Richardson DR and Milnes K: The potential
of iron chelators of the pyridoxal isonicotinoyl hydrazone class as
effective antiproliferative agents II: The mechanism of action of
ligands derived from salicylaldehyde benzoyl hydrazone and
2-hydroxy-1-naphthylaldehyde benzoyl hydrazone. Blood.
89:3025–3038. 1997.PubMed/NCBI
|
|
19
|
Darnell G and Richardson DR: The potential
of iron chelators of the pyridoxal isonicotinoyl hydrazone class as
effective antiproliferative agents III: The effect of the ligands
on molecular targets involved in proliferation. Blood. 94:781–792.
1999.PubMed/NCBI
|
|
20
|
Gao J and Richardson DR: The potential of
iron chelators of the pyridoxal isonicotinoyl hydrazone class as
effective antiproliferative agents, IV: The mechanisms involved in
inhibiting cell-cycle progression. Blood. 98:842–850. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Pahontu E, Julea F, Rosu T, Purcarea V,
Chumakov Y, Petrenco P and Gulea A: Antibacterial, antifungal and
in vitro antileukaemia activity of metal complexes with
thiosemicarbazones. J Cell Mol Med. 19:865–878. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhu TH, Cao SW and Yu YY: Synthesis,
characterization and biological evaluation of paeonol
thiosemicarbazone analogues as mushroom tyrosinase inhibitors. Int
J Biol Macromol. 62:589–595. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gan C, Cui J, Su S, Lin Q, Jia L, Fan L
and Huang Y: Synthesis and antiproliferative activity of some
steroidal thiosemicarbazones, semicarbazones and hydrozones.
Steroids. 87:99–107. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Xie W, Xie S, Zhou Y, Tang X, Liu J, Yang
W and Qiu M: Design and synthesis of novel 5,6-disubstituted
pyridine-2,3-dione-3-thiosemicarbazone derivatives as potential
anticancer agents. Eur J Med Chem. 81:22–27. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Akgemci EG, Saf AO, Tasdemir HU, Türkkan
E, Bingol H, Turan SO and Akkiprik M: Spectrophotometric,
voltammetric and cytotoxicity studies of
2-hydroxy-5-methoxyacetophenone thiosemicarbazone and its
N(4)-substituted derivatives: A combined experimental-computational
study. Spectrochim Acta A Mol Biomol Spectrosc. 136:719–725. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhang N, Tai Y, Li M, Ma P, Zhao J and Niu
J: Main group bismuth(III), gallium(III) and diorganotin(IV)
complexes derived from bis(2-acetylpyrazine)thiocarbonohydrazone:
Synthesis, crystal structures and biological evaluation. Dalton
Trans. 43:5182–5189. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ma B, Goh BC, Tan EH, Lam KC, Soo R, Leong
SS, Wang LZ, Mo F, Chan AT, Zee B and Mok T: A multicenter phase II
trial of 3-aminopyridine-2-carboxaldehyde thiosemicarbazone (3-AP,
Triapine) and gemcitabine in advanced non-small-cell lung cancer
with pharmacokinetic evaluation using peripheral blood mononuclear
cells. Invest New Drugs. 26:169–173. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lovejoy DB, Jansson PJ, Brunk UT, Wong J,
Ponka P and Richardson DR: Antitumor activity of metal-chelating
compound Dp44mT is mediated by formation of a redox-active copper
complex that accumulates in lysosomes. Cancer Res. 71:5871–5880.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kovacevic Z, Chikhani S, Lovejoy DB and
Richardson DR: Novel thiosemicarbazone iron chelators induce
up-regulation and phosphorylation of the metastasis suppressor
N-myc down-stream regulated gene 1: A new strategy for the
treatment of pancreatic cancer. Mol Pharmacol. 80:598–609. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Merolla F, Mascolo M, Ilardi G, Siano M,
Russo D, Graziano V, Celetti A and Staibano S: Nucleotide excision
repair and head and neck cancers. Front Biosci (Landmark Ed).
21:55–69. 2016. View
Article : Google Scholar : PubMed/NCBI
|
|
31
|
Han Yue CD and Guo Hongliang: Advances in
DNA damage response. Chin J Cancer Prev Treat. 20:1775–78.
2013.
|
|
32
|
Chen Z, Zhou Q, Zou D, Tian Y, Liu B,
Zhang Y and Wu Z: Chloro-benzoquinones cause oxidative DNA damage
through iron-mediated ROS production in Escherichia coli.
Chemosphere. 135:379–386. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Melis JP, van Steeg H and Luijten M:
Oxidative DNA damage and nucleotide excision repair. Antioxid Redox
Signal. 18:2409–2419. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Park JS, Na HJ, Pyo JH, Jeon HJ, Kim YS
and Yoo MA: Requirement of ATR for maintenance of intestinal stem
cells in aging Drosophila. Aging (Albany NY). 7:307–318. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Tang S, Hou Y, Zhang H, Tu G, Yang L, Sun
Y, Lang L, Tang X, Du YE, Zhou M, et al: Oxidized ATM promotes
abnormal proliferation of breast CAFs through maintaining
intracellular redox homeostasis and activating the PI3K-AKT,
MEK-ERK, and Wnt-β-catenin signaling pathways. Cell Cycle.
14:1908–1924. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Le NT and Richardson DR: Iron chelators
with high antiproliferative activity up-regulate the expression of
a growth inhibitory and metastasis suppressor gene: A link between
iron metabolism and proliferation. Blood. 104:2967–2975. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Sun J, Zhang D, Zheng Y, Zhao Q, Zheng M,
Kovacevic Z and Richardson DR: Targeting the metastasis suppressor,
NDRG1, using novel iron chelators: Regulation of stress
fiber-mediated tumor cell migration via modulation of the
ROCK1/pMLC2 signaling pathway. Mol Pharmacol. 83:454–469. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Seebacher NA, Lane DJ, Jansson PJ and
Richardson DR: Glucose modulation induces lysosome formation and
increases lysosomotropic drug sequestration via the P-glycoprotein
drug transporter. J Biol Chem. 291:3796–3820. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wong FC, Ng AW, Lee VH, Lui CM, Yuen KK,
Sze WK, Leung TW and Tung SY: Whole-field simultaneous
integrated-boost intensity-modulated radiotherapy for patients with
nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 76:138–145.
2010. View Article : Google Scholar : PubMed/NCBI
|