Introduction
Oral squamous cell carcinoma (OSCC) is the most
common malignancy arising in the head and neck globally (1). Over the previous decades, the incidence
of OSCC has significantly increased, and only a small improvement
in the 5-year survival rate has been demonstrated (from 56% in
1989–1994 to 62% in 2007–2011) in a Netherlands study between 1989
and 2011, despite advances in surgical techniques, radiation and
chemotherapy (2). It is widely
accepted that angiogenesis serves an important role in tumor growth
and is one of the hallmarks of malignant tumors, including OSCC
(3–5).
Therefore, inhibiting angiogenesis provides opportunities for the
development of novel therapeutic agents and strategies for
OSCC.
Vascular endothelial growth factor (VEGF) is one of
the potent regulators of tumor angiogenesis and is considered to be
an important therapeutic target (4,5). VEGF-A is
a key VEGF family member that is known to be involved in tumor
angiogenesis in a number of malignancies (6,7). Several
groups have indicated that marked VEGF-A expression is observed in
70% of OSCC tissues (8), and that its
expression levels are significantly increased in patients with OSCC
with lymph node metastasis or a poor prognosis compared with those
with a good prognosis (9–11).
One of the well-recognized VEGF-targeting drugs is
bevacizumab, a recombinant humanized monoclonal antibody against
VEGF-A, which inhibits the biological activity of VEGF (12). It is clinically administered by
intravenous injection. Previous studies have indicated that the
preclinical and clinical use of bevacizumab has beneficial effects
on a variety of malignant tumors, including metastatic colorectal
(13), breast (14) and lung cancer (15). In addition, the antitumor effects of
bevacizumab have been demonstrated in nude mouse xenograft models
of head and neck squamous cell carcinoma (HNSCC) (16–19).
Generally, as life expectancy extends, the number of
elderly patients (≥65 years) with HNSCC increases (20). This results in difficulties in
treatment, as intravenous chemotherapy against HNSCC, including
OSCC, intensifies the side effects experienced by elderly patients
(21). Antitumor agents may be
delivered directly into tumor tissues by local injection. These
local injections enhance the antitumor activity and diminish the
side effects of the chemotherapeutic agents. Intratumoral
injections, representing one of multiple local injection
techniques, have already been established in the treatment of lung
cancer (22). Intratumoral injections
of bevacizumab were indicated to reduce tumor growth in squamous
cell carcinoma (SCC) xenografts (19). However, the antitumor effects of
peritumoral bevacizumab injection in mouse models of SCC, including
OSCC, are not well understood. Therefore, the present study
investigated the antitumor effects of peritumoral bevacizumab
injections on OSCC xenografts. To the best of our knowledge, this
is the first study to demonstrate the effects of peritumoral
bevacizumab injections on OSCC.
Materials and methods
Reagents
Bevacizumab was purchased from Chugai Pharmaceutical
Co., Ltd. (Tokyo, Japan) and dissolved in saline. Rat anti-mouse
cluster of differentiation (CD)31 monoclonal antibody was purchased
from DIANOVA Vertriebs Gesellschaft mbH (Hamburg, Germany).
Anti-α-smooth muscle actin (α-SMA) was purchased from Abcam
(Cambridge, MA, USA). Indigocarmine was purchased from Daiichi
Sankyo Company (Tokyo, Japan). All other chemicals and reagents
were purchased from Invitrogen; Thermo Fisher Scientific, Inc.
(Waltham, MA, USA), Sigma-Aldrich; Merck KGaA (Darmstadt, Germany)
and Wako Pure Chemical Industries, Ltd. (Osaka, Japan), unless
otherwise specified.
Cell lines and culture conditions
The HSC-3 cell line (Japanese Cancer Research
Resources Bank, Tokyo, Japan), a human OSCC cell line, was used in
the present study. The cells were maintained in α-minimum essential
medium (α-MEM) (Invitrogen; Thermo Fisher Scientific, Inc.)
supplemented with 10% fetal bovine serum (BioWest, Nuaillé,
France), 100 IU/ml penicillin and 100 mg/ml streptomycin
(Invitrogen; Thermo Fisher Scientific, Inc.) and grown at 37°C in a
5% CO2 atmosphere.
OSCC treatment model
A total of 18 female BALB/c nude (nu/nu) mice
weighing 18.9±1.0 g (5-week-old; CLEA Japan, Inc., Tokyo, Japan)
were used in the present study. All mice were kept in housing
conditions of 21–25°C and 40–70% humidity, in a 12 h dark/light
cycle with free access to food and water. A total of
5×106 HSC-3 cells were re-suspended in 50 µl α-MEM mixed
with 50 µl of Matrigel (BD Biosciences, San Jose, CA, USA;
non-diluted), and injected subcutaneously into the flank of
anesthetized mice. Tumor-bearing mice were randomly divided into
three groups (n=6 each), and tumors were allowed to reach ~40
mm3 in size. Weight loss exceeding 20% was considered a
humane endpoint.
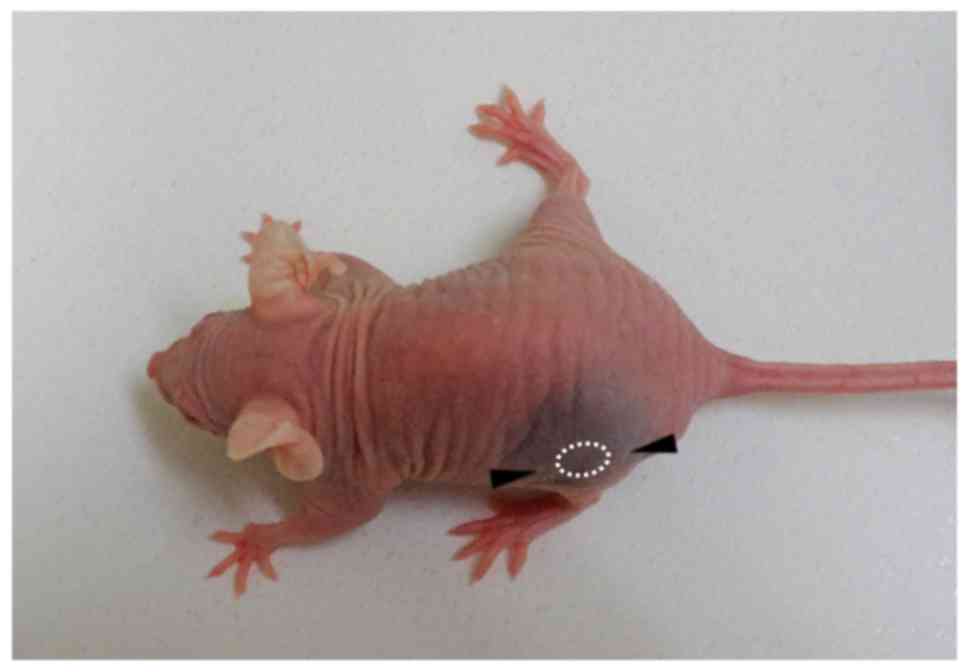
The model in the present study used peritumoral
injection, not intratumoral, to avoid artificial injury by the
needle and to surround the tumor mass with the injected solution.
The following method was demonstrated to be most suitable for
spreading the injected solution around the tumor. A Hamilton
microliter syringe (50 µl; Hamilton Company, Reno, NV, USA) with a
26-gauge needle was used. The needle was inserted subcutaneously a
distance of 5 mm from the tumor periphery into the caudal-rostral
side, positioned to a distance of 2 mm from the tumor periphery,
and then 25 µl indigocarmine was subcutaneously injected. The other
25 µl indigocarmine was subcutaneously injected into the rostral
side by the same method. Consequently, the tissue around the tumor
was stained blue (Fig. 1), and the
injected solution did not indicate any leakage from the injection
points.
Based on the aforementioned method, the mice were
treated by peritumoral injection when the tumor mass reached ~40
mm3 in size. Briefly, 25 µl of 10 mg/ml bevacizumab or
saline was subcutaneously injected into the caudal and rostral
sides, respectively) using the Hamilton microliter syringe. Each 25
µl from both sides (a total of 50 µl) was administered twice a week
for 4 weeks. The mice in the control group did not receive any
treatment.
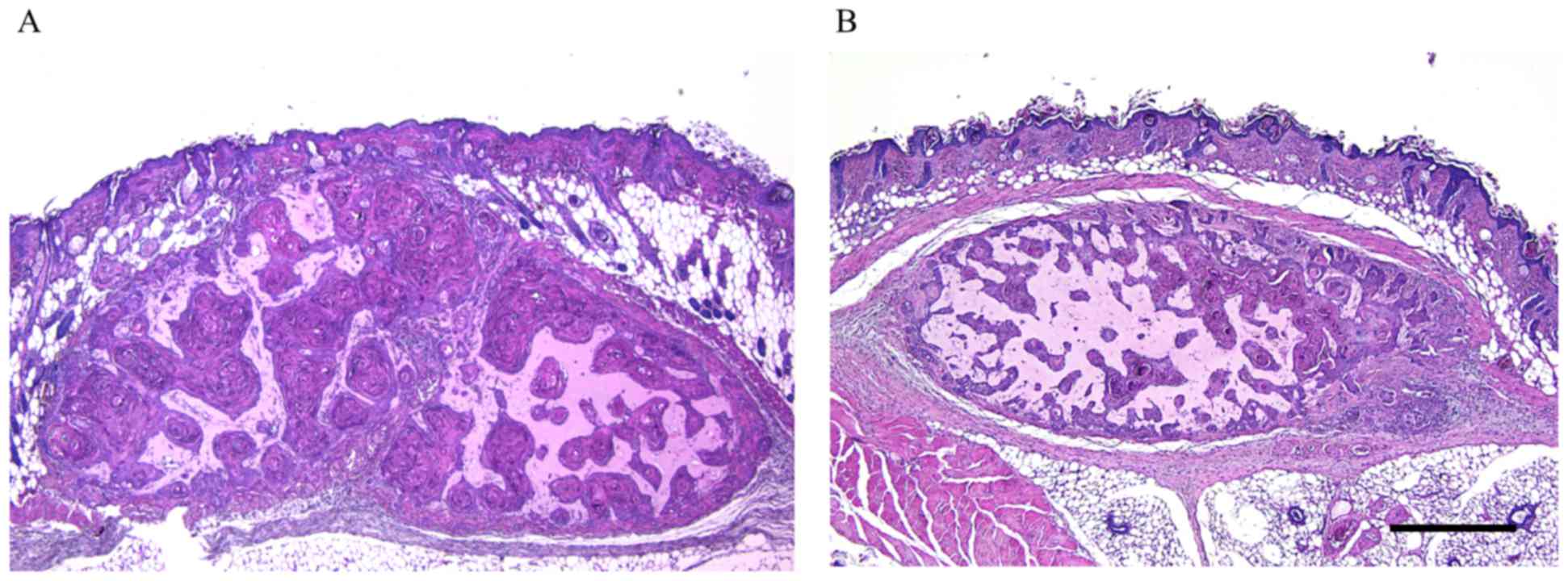
Tumor diameters were measured twice a week for 28
days. Tumor volume was determined using the following formula: (0.5
× length × width2), as described by Fujita et al
(16). Mice were then euthanized and
the tumor was carefully removed along with the overlying skin and
the surrounding tissue (Fig. 2).
Whole tumor specimens were fixed immediately with 4%
paraformaldehyde and embedded in paraffin for subsequent
histological examinations. All animal experiments were approved by
the Animal Ethics Committee of the University of Fukui (approval
no. 28075) and performed in accordance with the Guide for the Care
and Use of Laboratory Animals (National Institutes of Health)
(23).
Immunohistochemistry
CD31 is mainly expressed in the vascular endothelia.
In addition, α-SMA is found in perivascular interstitial cells of
microvascular proliferation. Thus, immunoreactivity to CD31 and
α-SMA shows the appearance of immature and mature tumor vessels,
respectively (24). In order to
evaluate the endothelial cells of intratumoral microvessels and the
recruitment of vascular mural cells, immunostaining for CD31 and
α-SMA was performed. The sections were de-paraffinized in Clear
Plus (Falma Co., Ltd., Tokyo, Japan) for 15 min and rehydrated in
100% ethanol for 15 min at room temperature. The endogenous
peroxide activity was eliminated with a solution of 0.3%
H2O2 in methanol for 15 min at room
temperature. For antigen retrieval, the sections were immersed in 1
mM EDTA-2Na/10 mM Tris buffer (pH 9.0) and autoclaved at 105°C for
15 min. Protein Block Serum-Free solution (Dako; Agilent
Technologies, Inc., Santa Clara, CA, USA; non-diluted) was used to
block non-specific immunoreactions for 10 min at room temperature.
The sections were incubated with primary antibodies against CD31
(cat no. DIA-310; DIANOVA Vertriebs Gesellschaft mbH; dilution,
1:20) and α-SMA (cat no. ab5649; Abcam; dilution, 1:100) for 60 min
at room temperature. The sections were then incubated with
biotinylated rabbit anti-rat IgG (cat no. BA-4000; Vector
Laboratories, Burlingame, CA, USA; dilution, 1:100) for CD31 or
Histofine simple stain MAX-PO (cat. no. 424151; Nichirei
Biosciences, Inc., Tokyo, Japan; non-diluted) for α-SMA for 30 min
at room temperature. This was followed by treatment with
streptavidin-horseradish peroxidase for 60 min at room temperature
(Vector Laboratories; dilution, 1:500). Immunoreactivity was
visualized by immersing the sections in 3,3′-diaminobenzidine (DAB;
DAB substrate kit; Dako; Agilent Technologies, Inc.). Subsequently,
sections were counterstained with hematoxylin for 5 min at room
temperature, dehydrated in 100% ethanol and replaced by Clear Plus
at room temperature. The sections were rinsed three times in TBS
between all steps. We observed them using a light microscope at
magnification, ×400.
Quantification of microvessel density
(MVD) with CD31 and α-SMA
CD31- and α-SMA-stained tissue sections were
analyzed, and all CD31- and α-SMA-positive intratumoral
microvessels were identified at magnification, ×400. These vessels
were then counted in each individual microscopic field (×400), as
described by Cao et al (17);
at least 7 microscopic fields per histological section were
included in the analysis. The results were presented as the average
MVD per high power field.
Evaluation of apoptosis
The terminal deoxynucleotidyl-transferase-mediated
dUTP-biotin nick labeling (TUNEL) method was applied to evaluate
apoptosis using the in situ Apoptosis Detection kit (Takara
Bio, Inc., Otsu, Japan) according to the manufacturer's protocol.
Briefly, the sections were de-paraffinized in Clear Plus for 15
min, rehydrated in 100% ethanol for 15 min and permeabilized using
10 µg/ml proteinase K (Invitrogen; Thermo Fisher Scientific, Inc.)
for 10 min at room temperature. The endogenous peroxide activity
was eliminated with a solution of 3% H2O2 for
5 min at room temperature. The sections were incubated with 50 µl
of labeling reaction mixture (consisting of TdT Enzyme 5 µl +
Labeling Safe Buffer 45 µl; Apoptosis Detection kit; Takara Bio,
Inc., Otsu, Japan) in a 37°C humidified chamber for 90 min. Then,
they were reacted with 70 µl anti-FITC horseradish peroxidase (not
diluted, cat no. MK503; Takara Bio, Inc.) for 30 min at 37°C.
Immunoreactivity was visualized by immersing the sections in
3,3′-diaminobenzidine (DAB; Dako, Agilent Technologies, Inc., Santa
Clara, CA, USA) for 10 min at room temperature. Subsequently,
sections were counterstained with 3% methylgreen for 5 min,
dehydrated in 100% ethanol, and replaced by Clear Plus. EXCEL Mount
(Falma, Tokyo, Japan) was used for mounting. The sections were
rinsed three times in TBS between all steps. Apoptotic cells were
counted at magnification, ×400. The apoptosis index (the proportion
of apoptotic cells) was determined by counting the TUNEL-positive
cells per total number of tumor cells, avoiding necrotic tumor
areas, from a minimum of 5 microscopic fields in each individual
section using a light microscope.
Statistical analysis
All statistical analyses were performed using Excel
Statistics 2012 software (version 1.13, Social Survey Research
Information Co., Ltd., Tokyo, Japan; for windows). Measured values
are presented as the mean ± standard deviation (SD). Tumor volumes,
MVD and apoptosis indices were analyzed using a one-way analysis of
variance with the Tukey-Kramer multiple comparison post-hoc test.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Antitumor effects of bevacizumab on
OSCC xenografts
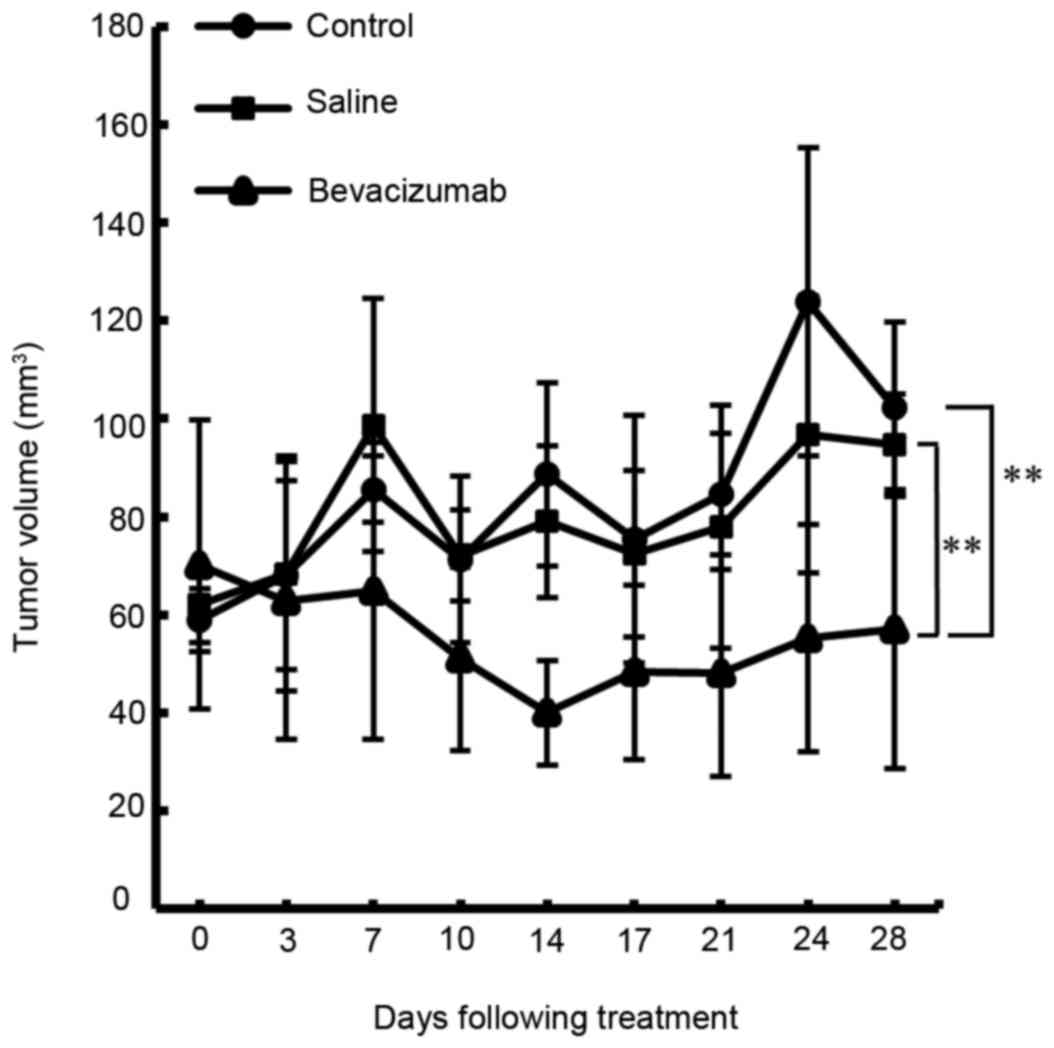
The antitumor effects of bevacizumab on HSC-3 tumors
propagated in nude mice were investigated. As indicated in Table I and Fig.
3, the tumor volume was reduced without any apparent toxicity
in all bevacizumab-treated groups compared with the saline-treated
groups and untreated controls. The differences between groups were
statistically significant at 28 days following treatment
(P<0.01).
 | Table I.Tumor volume in each group. |
Table I.
Tumor volume in each group.
|
| Tumor volume,
mm3 |
|---|
|
|
|
|---|
| Treatment
group | 0 | 7 days | 14 days | 21 days | 28 days |
|---|
| Control (n=6) | 58.9±6.4 | 85.6±6.8 | 88.7±18.7 | 84.7±12.4 | 102.2±17.6 |
| Saline (n=6) | 62.2±7.9 | 98.7±25.9 | 79.0±15.5 | 77.9±24.8 | 94.6±10.5 |
| Bevacizumab
(n=6) | 70.2±29.5 | 64.9±30.2 | 40.0±10.6 | 48.1±21.2 | 57.1±28.4 |
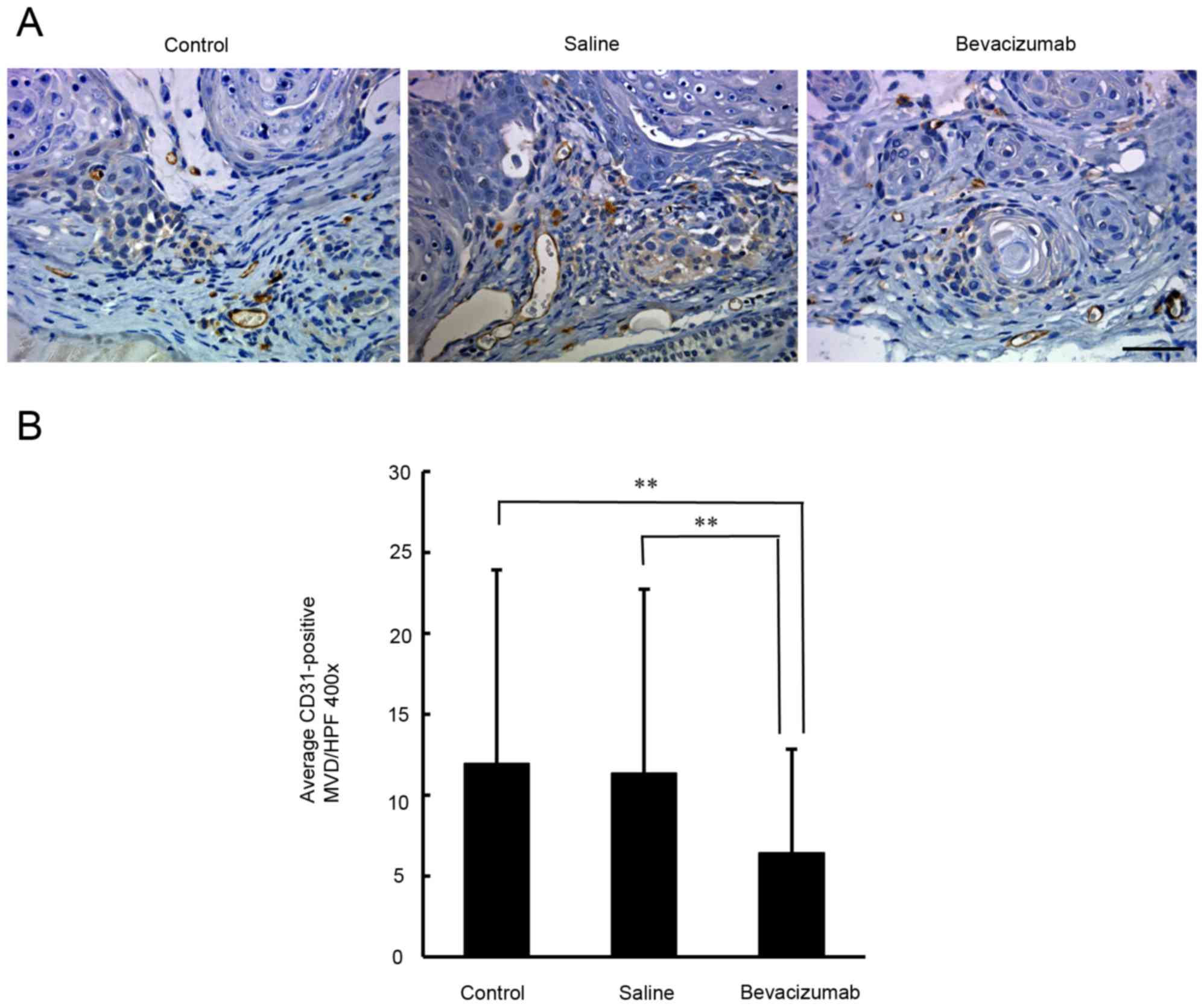
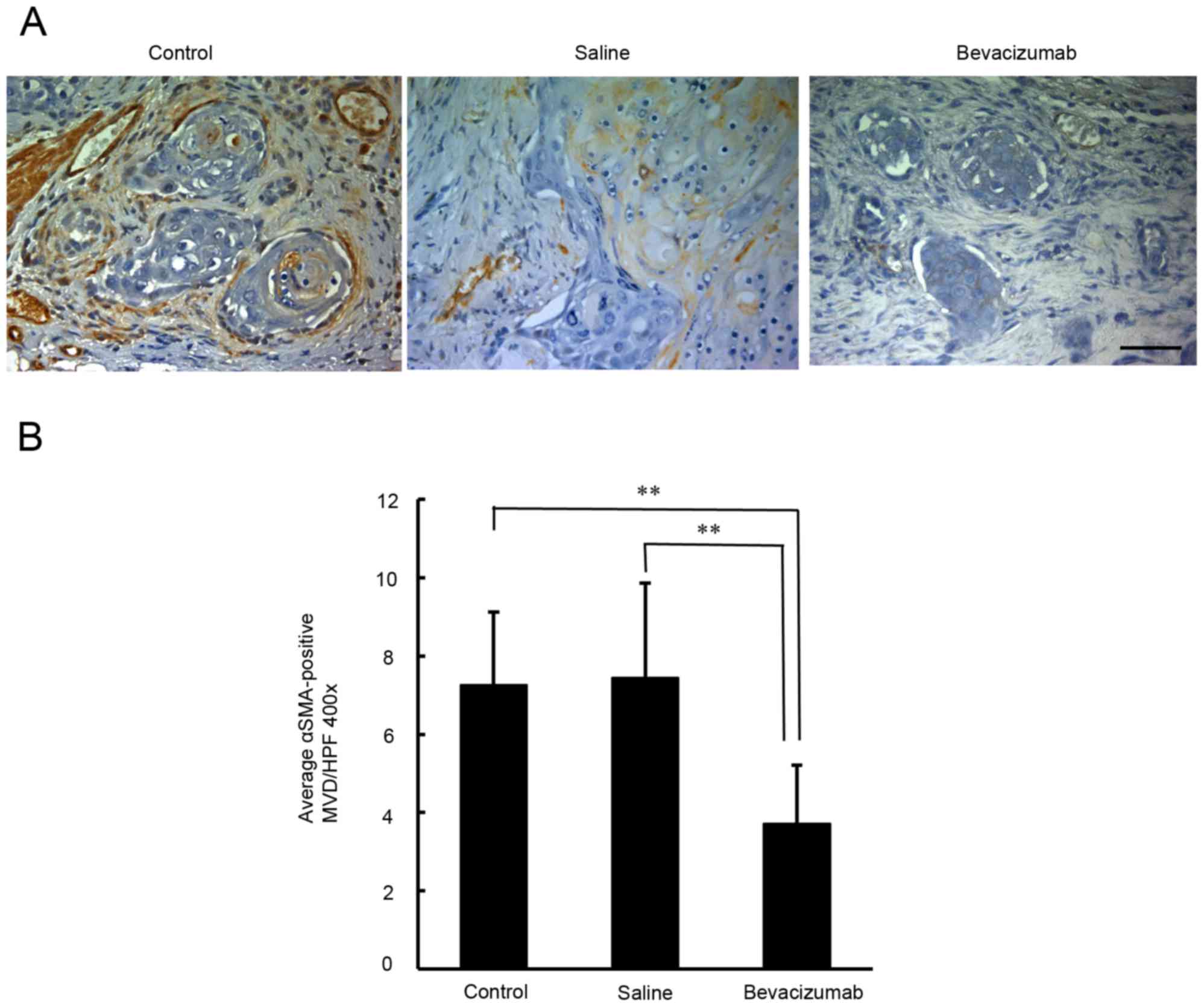
Quantification of the density of CD31
and α-SMA-positive microvessels in OSCC xenografts
In order to determine whether angiogenesis had been
inhibited, the microvessel density in the xenograft tumors was
examined by immunostaining for CD31. As demonstrated in Fig. 4, the densities of the CD31-positive
microvessels in the untreated, saline-treated and
bevacizumab-treated groups were 11.9±4.5, 11.4±3.8, and 6.4±3.0,
respectively. There was a significant difference in the densities
of the CD31-positive microvessels between the bevacizumab-treated
and the two control groups (P<0.01). To understand the
recruitment of vascular mural cells, the densities of
α-SMA-positive microvessels were examined. As indicated in Fig. 5, the density of α-SMA-positive
microvessels in the untreated, saline-treated and
bevacizumab-treated groups were 7.3±1.9, 7.4±2.4 and 3.7±1.5,
respectively. There was a significant difference in the densities
of α-SMA-positive microvessels between the bevacizumab-treated
group and the two control groups (P<0.01).
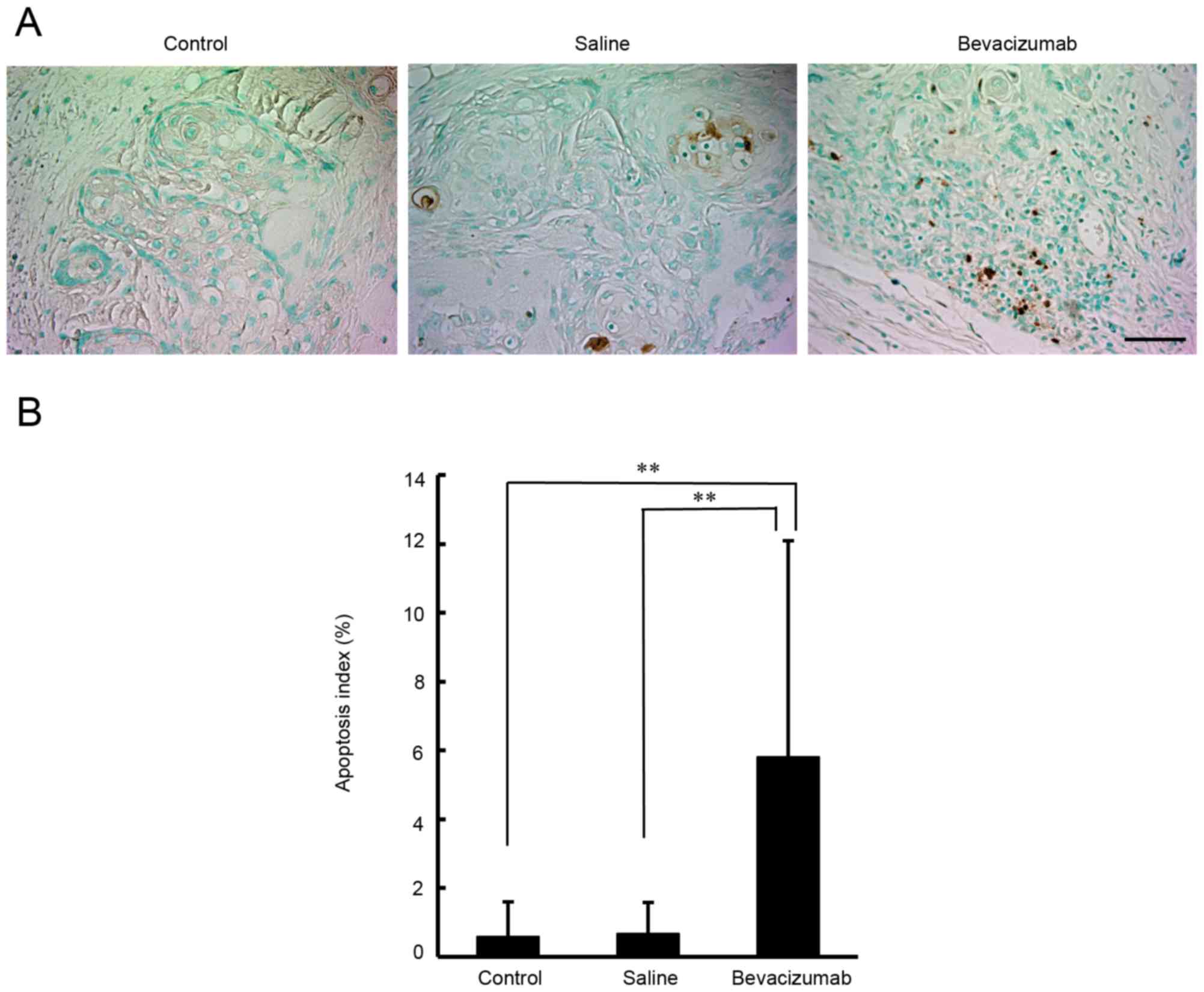
Effects of bevacizumab treatment on
apoptosis in OSCC xenografts
A histopathological analysis was performed with
TUNEL staining, in order to examine apoptosis in the OSCC
xenografts. As demonstrated in Fig.
6, the apoptosis indexes in the untreated, saline-treated and
bevacizumab-treated groups were 0.6±1.0, 0.7±0.9 and 5.9±6.3%,
respectively. There was a significant difference in apoptosis
levels between tumors treated with bevacizumab and tumors treated
with either saline or left untreated (P<0.01).
Discussion
In the present study, the in vivo antitumor
effects of bevacizumab were investigated in an OSCC xenograft
model. It was identified that bevacizumab significantly inhibited
tumor growth in the HSC-3-bearing nude mouse model.
Histopathological analysis with CD31 staining of the xenograft
samples indicated that bevacizumab treatment significantly
decreased microvessel density compared to saline treatment or no
treatment. These data are concordant with previous studies stating
that treatment with bevacizumab induced significant microvessel
damage and tumor necrosis in HNSCC (17,18). It
was also identified that bevacizumab treatment significantly
reduced the density of α-SMA-positive microvessels compared with
the control treatments. A previous study revealed that the
expression ratio of α-SMA/CD31 in a high VEGF group was
significantly increased compared with that in a low VEGF group in
glioblastoma multiforme (25).
Furthermore, inhibition of VEGF by bevacizumab treatment
significantly decreased the density of α-SMA-positive microvessels
in neuroblastoma compared with untreated control (26). These data support our hypothesis that
bevacizumab treatment may mediate the suppression of immature and
mature tumor vessels in an OSCC xenograft model.
The data of the present study also indicate that
peritumoral bevacizumab injections have significant antitumor
effects in an OSCC xenograft model. It is well known that local
administration enhances antitumor effects in the treatment of SCC.
For example, local injection of OK-432, a penicillin-killed and
lyophilized preparation of a low-virulence strain of
Streptococcus pyogenes (group A), was revealed to be
effective in the treatment of SCC, including OSCC and esophageal
carcinoma (27,28). Yamada et al (29) confirmed that local OK-432 injection
induced tumor necrosis in SCC mouse models. In the present study,
it was identified that apoptosis was significantly induced in
xenograft tumors treated with bevacizumab as compared with those
treated with either saline or left untreated. Other previous
studies have also suggested that local administration of
bevacizumab was able to induce apoptosis in SCC xenografts
(16,18,19),
indicating that it may be beneficial for the induction of apoptosis
in OSCC.
The primary purpose of the present study was to
evaluate inhibition of angiogenesis by peritumoral injection of
bevacizumab. To examine the microvessels around the tumor, the
tumor along with the overlying skin and the surrounding tissues was
removed. Tumor growth was determined by estimated tumor volumes,
not by the tumor weights. In their study on the photodynamic
therapy for R3230AC mammary carcinoma, Gibson et al
(30) compared the calculated tumor
volumes by tumor width and height to the surgically removed tumor
volumes by their water displacement (30). They confirmed that the difference
between calculated tumor volumes and water replacement data was
~20%, and based on these data, they monitored tumor growth by
calculating tumor volumes (30).
Other studies have also used calculated tumor volume as an
indicator of tumor growth (16,17,19).
The experimental methods in the present study have
some limitations. The present study focused on tumor angiogenesis
and examined the densities of CD31- and α-SMA-positive microvessels
around the tumor, and the tissues removed from the mice included
skin, subdermal and tumor tissues. Thus, it was difficult to
perform specific experiments, including western blotting, to
evaluate the protein expression associated with the antitumor
effect of peritumoral bevacizumab injection.
In the present study, peritumoral injections were
selected over intratumoral injections for the administration of
bevacizumab. Dvorak and Gresser (31)
also employed peritumoral injections to avoid the possibility of
needle-induced injury caused by intratumoral injections, and
indicated that peritumoral injections of interferon damaged tumor
microvessels and markedly suppressed tumor growth in their mouse
model. In addition, Marumo et al (32) demonstrated that peritumoral injections
were superior to subcutaneous injections in their ability to
inhibit tumor growth in a nude mouse model of renal cell carcinoma.
These data suggest that peritumoral injection is an effective
method for the tumor treatments.
Regarding the method of peritumoral injection, a
Hamilton microliter syringe with a 26-gauge needle was used in the
present study. The needle was subcutaneously inserted a distance of
5 mm from the tumor periphery into the caudal side, positioned to a
distance of 2 mm from the tumor periphery, and then 25 µl
bevacizumab or saline solution was injected. The other 25 µl of the
solution was injected into the rostral side by the same method.
Consequently, the tumor was surrounded by the solution injected
without any leakage. Yang et al (33) described a model in which macrophages
were peritumorally injected at 4 locations surrounding the tumor
mass. They tested intratumoral and peritumoral injections of
macrophages, and found that the peritumoral injection was more
efficient than intratumoral injection. Kitamura et al
(34) described a method in which
they administered 125I monoclonal antibody peritumorally
at one location (the distal portion) of the tumor in nude mice. It
was concluded that antibody recruitment into the tumor was more
efficient using the peritumoral injection than the intravenous
injection. These 2 reports demonstrate that the peritumoral
injection at 4 locations or one location surrounding the tumor was
more effective than other injections, including the intratumoral
and intravenous injection.
VEGF binds two primary tyrosine kinase receptors,
VEGF receptor (VEGFR)-1 and VEGFR-2, in the vascular endothelium
(35). The binding of VEGF with its
receptors serves an important role in regulation of angiogenesis
(35). VEGF expression was increased
in tumor cells, and VEGF receptor expression was increased in
CD31-positive endothelial cells in a mouse xenograft model of HNSCC
(36). Henriques et al
(37) demonstrated that VEGF was
expressed in tumor and stromal cells in OSCC (37), and serum levels of VEGF were
demonstrated to be increased in advanced T3/T4 tumors compared with
early T1/T2 tumors (38), indicating
that VEGF promotes tumor growth in OSCC. Conversely, bevacizumab is
known to inhibit biological activity of VEGF (12). Therefore, peritumoral bevacizumab
injection may have suppressed tumor angiogenesis and growth by
inhibiting VEGF, which binds VEGF receptors in the tumor stroma
(39), in this OSCC nude mouse
xenograft model. However, additional studies are required to
confirm the mechanism of inhibiting tumor growth by peritumoral
bevacizumab injection.
In conclusion, peritumoral bevacizumab injections
were identified to inhibit tumor growth in OSCC xenografts. It was
also demonstrated that treatment with bevacizumab significantly
reduced the densities of the CD31- and α-SMA-positive microvessels,
and increased the tumor apoptosis index compared with the
saline-treated or untreated groups. These data collectively suggest
an experimental basis for the clinical development of peritumoral
bevacizumab injections for the treatment of OSCC.
Acknowledgements
Not applicable.
Funding
The present study was supported by a Grant-in-Aid
for Scientific Research (grant no. 26462999) from the Japan Society
for the Promotion of Science, Japan.
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HisY, HitY and KS designed the experiments. HisY,
HitY, SM, TR, MK and KS performed the experiments. HisY, HitY, SM,
TK, MK and KS analyzed the data. HisY, HitY and KS wrote the
manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
All animal experiments were approved by the Animal
Ethics Committee of the University of Fukui (approval no.
28075).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Braakhuis BJ, Leemans CR and Visser O:
Incidence and survival trends of head and neck squamous cell
carcinoma in the Netherlands between 1989 and 2011. Oral Oncol.
50:670–675. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Folkman J: Tumor angiogenesis: Therapeutic
implications. N Engl J Med. 285:1182–1186. 1971. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hsu HW, Wall NR, Hsueh CT, Kim S, Ferris
RL, Chen CS and Mirshahidi S: Combination antiangiogenic therapy
and radiation in head and neck cancers. Oral Oncol. 50:19–26. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Vassilakopoulou M, Psyrri A and Argiris A:
Targeting angiogenesis in head and neck cancer. Oral Oncol.
51:409–415. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ferrara N, Gerber HP and LeCouter J: The
biology of VEGF and its receptors. Nat Med. 9:669–676. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Christopoulos A, Ahn SM, Klein JD and Kim
S: Biology of vascular endothelial growth factor and its receptors
in head and neck cancer: Beyond angiogenesis. Head Neck.
33:1220–1229. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nayak S, Goel MM, Chandra S, Bhatia V,
Mehrotra D, Kumar S, Makker A, Rath SK and Agarwal SP: VEGF-A
immunohistochemical and mRNA expression in tissues and its serum
levels in potentially malignant oral lesions and oral squamous cell
carcinomas. Oral Oncol. 48:233–239. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Uehara M, Sano K, Ikeda H, Sekine J, Irie
A, Yokota T, Tobita T, Ohba S and Inokuchi T: Expression of
vascular endothelial growth factor and prognosis of oral squamous
cell carcinoma. Oral Oncol. 40:321–325. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Seki S, Fujiwara M, Matsuura M, Fujita S,
Ikeda H, Asahina I and Ikeda T: Prediction of outcome of patients
with oral squamous cell carcinoma using vascular invasion and the
strongly positive expression of vascular endothelial growth
factors. Oral Oncol. 47:588–593. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhao SF, Yang XD, Lu MX, Sun GW, Wang YX,
Zhang YK, Pu YM and Tang EY: Prognostic significance of VEGF
immunohistochemical expression in oral cancer: A meta-analysis of
the literature. Tumour Biol. 34:3165–3171. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Presta LG, Chen H, O'Connor SJ, Chisholm
V, Meng YG, Krummen L, Winkler M and Ferrara N: Humanization of an
anti-vascular endothelial growth factor monoclonal antibody for the
therapy of solid tumors and other disorders. Cancer Res.
57:4593–4599. 1997.PubMed/NCBI
|
|
13
|
Hurwitz H, Fehrenbacher L, Novotny W,
Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S,
Holmgren E, et al: Bevacizumab plus irinotecan, fluorouracil, and
leucovorin for metastatic colorectal cancer. N Engl J Med.
350:2335–2342. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dickler MN, Rugo HS, Eberle CA, Brogi E,
Caravelli JF, Panageas KS, Boyd J, Yeh B, Lake DE, Dang CT, et al:
A phase II trial of erlotinib in combination with bevacizumab in
patients with metastatic breast cancer. Clin Cancer Res.
14:7878–7883. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sandler A, Gray R, Perry MC, Brahmer J,
Schiller JH, Dowlati A, Lilenbaum R and Johnson DH:
Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell
lung cancer. N Engl J Med. 355:2542–2550. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fujita K, Sano D, Kimura M, Yamashita Y,
Kawakami M, Ishiguro Y, Nishimura G, Matsuda H and Tsukuda M:
Anti-tumor effects of bevacizumab in combination with paclitaxel on
head and neck squamous cell carcinoma. Oncol Rep. 18:47–51.
2007.PubMed/NCBI
|
|
17
|
Cao S, Durrani FA, Toth K, Rustum YM and
Seshadri M: Bevacizumab enhances the therapeutic efficacy of
Irinotecan against human head and neck squamous cell carcinoma
xenografts. Oral Oncol. 47:459–466. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gyanchandani R, Sano D, Alves Ortega MV,
Klein JD, Knapick BA, Oh S, Myers JN and Kim S: Interleukin-8 as a
modulator of response to bevacizumab in preclinical models of head
and neck squamous cell carcinoma. Oral Oncol. 49:761–770. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang Y, Dong L, Bi Q, Ge X, Zhang X, Wu D,
Fu J, Zhang C, Wang C and Li S: Beyond antiangiogenesis:
Intratumorally injected bevacizumab plays a cisplatin-sensitizing
role in squamous cell carcinomas in mice. Chemotherapy. 57:244–252.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yancik R and Ries LA: Cancer in older
persons: An international issue in an aging world. Semin Oncol.
31:128–136. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Argiris A, Li Y, Murphy BA, Langer CJ and
Forastiere AA: Outcome of elderly patients with recurrent or
metastatic head and neck cancer treated with cisplatin-based
chemotherapy. J Clin Oncol. 22:262–268. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Takahashi T, Ueda S, Kono K and Majima S:
Attempt at local administration of anticancer agents in the form of
fat emulsion. Cancer. 38:1507–1514. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
National Research Council: Guide for the
Care and Use of Laboratory Animals. 8th edition. The National
Academies Press; Washington, DC: 2011, https://grants.nih.gov/grants/olaw/guide-for-the-care-and-use-of-laboratory-animals.pdf
|
|
24
|
Sorace AG, Quarles CC, Whisenant JG,
Hanker AB, McIntyre JO, Sanchez VM and Yankeelov TE: Trastuzumab
improves tumor perfusion and vascular delivery of cytotoxic therapy
in a murine model of HER2+ breast cancer: Preliminary
results. Breast Cancer Res Treat. 155:273–284. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Takeuchi H, Hashimoto N, Kitai R, Kubota T
and Kikuta K: Proliferation of vascular smooth muscle cells in
glioblastoma multiforme. J Neurosurg. 113:218–224. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Patterson DM, Gao D, Trahan DN, Johnson
BA, Ludwig A, Barbieri E, Chen Z, Diaz-Miron J, Vassilev L, Shohet
JM and Kim ES: Effect of MDM2 and vascular endothelial growth
factor inhibition on tumor angiogenesis and metastasis in
neuroblastoma. Angiogenesis. 14:255–266. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Mukai M, Kubota S, Morita S and Akanuma A:
A pilot study of combination therapy of radiation and local
administration of OK-432 for esophageal cancer. Five-year survival
and local control rate. Cancer. 75:2276–2280. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Tano T, Okamoto M, Kan S, Bando T, Goda H,
Nakashiro K, Shimodaira S, Koido S, Homma S, Fujita T, et al:
Immunochemoradiotherapy for patients with oral squamous cell
carcinoma: Augmentation of OK-432-induced helper T cell 1 response
by 5-FU and X-ray irradiation. Neoplasia. 15:805–814. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Yamada T, Hayashi Y, Kaneko R, Tohnai I,
Ueda M and Ito M: Effect of the combination of a local OK-432
injection and hyperthermia on SCC VII tumors in mice. J Radiat Res.
39:101–109. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Gibson SL, VanDerMeid KR, Murant RS,
Raubertas RF and Hilf R: Effects of various photoradiation regimens
on the antitumor efficacy of photodynamic therapy for R3230AC
mammary carcinomas. Cancer Res. 50:7236–7241. 1990.PubMed/NCBI
|
|
31
|
Dvorak HF and Gresser I: Microvascular
injury in pathogenesis of interferon-induced necrosis of
subcutaneous tumors in mice. J Natl Cancer Inst. 81:497–502. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Marumo K, Oya M and Murai M: Application
of the interferon minipellet to human renal cell carcinoma in nude
mice. Int J Urol. 4:55–61. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yang TD, Choi W, Yoon TH, Lee KJ, Lee JS,
Joo JH, Lee MG, Yim HS, Choi KM, Kim B, et al: In vivo photothermal
treatment by the peritumoral injection of macrophages loaded with
goldnanoshells. Biomed Opt Express. 7:185–193. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kitamura K, Takahashi T, Kotani T,
Miyagaki T, Yamaoka N, Tsurumi H, Noguchi A and Yamaguchi T: Local
administration of monoclonal antibody-drug conjugate: A new
strategy to reduce the local recurrence of colorectal cancer.
Cancer Res. 52:6323–6328. 1992.PubMed/NCBI
|
|
35
|
Kliche S and Waltenberger J: VEGF receptor
signaling and endothelial function. IUBMB Life. 52:61–66. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Yazama H, Kitatani K, Fujiwara K, Kato M,
Hashimoto-Nishimura M, Kawamoto K, Hasegawa K, Kitano H, Bielawska
A, Bielawski J and Okazaki T: Dietary glucosylceramides suppress
tumor growth in a mouse xenograft model of head and neck squamous
cell carcinoma by the inhibition of angiogenesis through an
increase in ceramide. Int J Clin Oncol. 20:438–446. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Henriques AC, de Matos FR, Galvão HC and
Freitas Rde A: Immunohistochemical expression of MMP-9 and VEGF in
squamous cell carcinoma of the tongue. J Oral Sci. 54:105–111.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Aggarwal S, Devaraja K, Sharma SC and Das
SN: Expression of vascular endothelial growth factor (VEGF) in
patients with oral squamous cell carcinoma and its clinical
significance. Clin Chim Acta. 436:35–40. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Folkman J: Role of angiogenesis in tumor
growth and metastasis. Semin Oncol. 29 Suppl 16:S15–S18. 2002.
View Article : Google Scholar
|