Introduction
An estimated 300,400 novel cases and 145,400 deaths
from oral cavity cancer occurred in 2012 globally (1). Oral cancer is the most common head and
neck cancer. Among the different types of oral cancers, the
incidence of oral squamous cell carcinoma (OSCC) is the highest
(1). The prevention, early diagnosis,
treatment, and prognosis of OSCC remains unsatisfactory. The
occurrence, development, and prognosis of OSCC results from between
environmental and genetic factors interactions (2). The mechanisms underlying oral mucosal
carcinogenesis remain unknown, and this hinders treatment.
Researchers in the field have been focusing on exploring the
mechanisms underlying oral mucosa carcinogenesis and identifying
markers for OSCC diagnosis and treatment (3,4).
Genome-wide association studies (GWAS) use
microarray technology and DNA samples from patients enrolled in
large-scale case-control studies to identify genetic factors
influencing the risk of complex diseases. GWAS does not depend on a
specific gene selected based on a pathogenic hypothesis (5). Association studies of single nucleotide
polymorphisms (SNPs) and complex disease phenotypes provide
important genetic markers for the diagnosis and prevention of
complex diseases (5–7).
The occurrence of tumours is caused by many factors
influencing cell proliferation or apoptosis (8–10).
Different types of tumours have some common underlying mechanisms
in terms of the proteins and signalling pathways involved in the
onset of the disease (11–13). For example, a type of tumour
susceptibility loci may be associated with the onset of other
tumour types, especially if the tumours are of the same origin
(11,12,14). Thus,
the susceptible loci reported in the Cancer GWAS catalogue
[2012-03-09; (http://www.genome.gov/gwastudies)] (15) might be associated with the onset of
OSCC (11,12).
In the present study, a meta-analysis was performed
to screen common genetic susceptibility loci of malignant tumours
using the GWAS catalogue, leading to the identification of the OSCC
genetic susceptibility locus, rs2294008, which is located in the
prostate stem cell antigen (PSCA) gene.
The influence of PSCA gene polymorphisms on the
prognosis of patients with OSCC was explored through the analysis
of clinical data and postoperative follow-up of patients enrolled
in a case-control study. PSCA mRNA and protein expression was
assessed in OSCC cell lines and the mechanisms underlying the role
of PSCA in oral mucosa carcinogenesis were investigated.
Materials and methods
Screening for common SNPs associated with
susceptibility for malignant tumour using GWAS data
Data retrieval
Seven cancers having the highest incidences of
malignant tumour formation, including lung, breast, colorectal,
upper aerodigestive tract, prostate, liver, and bladder cancer, and
two cancers closely associated with oral cavity disease, skin
cancer and nasopharyngeal carcinoma (NPC), were chosen for the
screening of common genetic susceptibility loci, and these loci may
be susceptible to OSCC as well. The official directory Catalogue of
GWAS studies (2012-03-09) was downloaded, and relevant GWAS data on
the selected nine cancers were retrieved, including details of
authors, publication year, journal, tumour type, sample size, SNP
ID, P-value, OR value, and 95% confidence interval.
Statistical analysis
Regarding the nine types of malignant tumours as a
whole, different P-values of the same locus reported in different
studies (same tumour type or different tumour type) were merged
through Fisher's exact probability method using Stata 11.0
(StataCorp LP, College Station, USA). For the nine different types
of malignant tumours, related sites for each tumour type were
analysed, and different P-values of the same locus for the same
tumour type from different publications were merged through the
same method.
All susceptibility loci associated with malignant
tumour morbidity were imported to the dbSNP database, and gene loci
in the exon that may affect the corresponding encoding functions
were screened.
Association study between the selected
SNPs and OSCC
Study case inclusion
Twelve SNP loci located in the exons were selected
from the 225 SNP loci associated with the nine types of malignant
tumour in the GWAS Catalogue and utilized for the following
experiments. To determine a possible association between these 12
SNPs and OSCC, a multicentre case-control study, including Chinese
Han patients with OSCC and healthy volunteers, was performed, and
the distribution of the 12 loci alleles and genotypes was explored
to determine the genetic susceptibility loci associated with
OSCC.
Two-hundred and seventy-nine patients with OSCC (162
males, 114 females; average age: 59 years) who were treated at the
West China Hospital of Stomatology (Sichuan University), the
Beijing Stomatological Hospital (Capital Medical University), and
the Guangdong Provincial Stomatological Hospital from January 2003
to December 2011 (the case group) and 218 healthy volunteers (the
control group; 126 males, 112 females; average age, 54 years) who
were examined in the West China Hospital (Sichuan University) and
Stomatological Hospital of the Fourth Military Medical University
were enrolled in the present study. No patient in the case group
had a history of other tumours. The control group consisted of
healthy volunteers without a history of cancer.
Reagents
Primers for Polymerase Chain Reaction (PCR)
amplification and single-base extension were designed with
Genotyping Tools and MassARRAY Assay Design 3.1 software (Sequenom,
San Diego, CA, USA), and synthesized by Invitrogen; Thermo Fisher
Scientific, Inc. (Waltham, MA, USA). QIAamp DNA Blood Midi kit
(QIAGEN GmbH, Hilden, Germany) was used for DNA extraction, and
iPLEX® Gold Reagent kit purchased from Sequenom was used
for SNP genotyping.
DNA extraction
DNA in blood samples was extracted, and quantified
by using a spectrophotometer, and quality tested by using agarose
gel electrophoresis. The concentration of DNA samples that passed
the quality inspection was adjusted to 50 ng/µl, and samples were
stored at −20°C for later use.
PCR amplification and
purification
Multiplex PCR amplification was performed. The total
reaction volume was 5 µl, which included 10 ng of template DNA, 0.5
U of Hotstar Taq, 0.5 pmol amplification primer, and 0.1 µl of 25
mM dNTPs. The reaction conditions were as follows: pre-denaturation
at 94°C for 4 min, followed by 45 cycles of 94°C for 20 sec, 56°C
for 30 sec, and 72°C for 1 min. A final extension was performed at
72°C for 3 min, and the samples were stored at 4°C.
PCR products were processed with 0.5 U shrimp
alkaline phosphatase (SAP), and excess dNTP was removed. The total
reaction volume was 7 µl, which included the PCR product (5 µl) and
SAP mixture (2 µl; 0.5 U of SAP, 0.17 µl of buffer). The reaction
was performed at 37°C for 20 min and 85°C for 5 min, and the
samples were stored at 4°C.
Single-base extension and
purification
The total reaction volume for single base extension
was 9 µl including 7 µl of PCR products following processing with
SAP, primer extension reaction mixture (0.804 µl), iPLEX enzyme
(0.041 µl). The reaction conditions were as follows:
Pre-denaturation at 94°C for 30 sec and 94°C for 5 sec, followed by
5 cycles of 52°C for 5 sec and 80°C for 5 sec; and subsequently
return to 94°C for 5 sec for a total 40 cycles, finally followed by
extension at 72°C for 3 min and stored at 4°C. Each extension
reaction product was purified with 6 mg Spectro CLEAN™ resin
(Sequenom) (16).
Mass spectrometric detection
Purified products were placed in a 384-well
SpectroCHIP (Sequenom) chip, and the signals were analysed via
Matrix-assisted laser desorption/Ionization time of a flight
(MALDI-TOF) mass spectrometry; the results were classified with
TYPER 4.0 (Sequenom).
Statistical analysis
The case and control groups were tested using the
Hardy Weinberg-genetic equilibrium (HWE) test. Between groups, the
allele frequency at various points was calculated with the
chi-squared test, and Fisher's exact probability test was used to
assess differences in allele distribution between the OSCC and
control groups. Bilateral probability was estimated for the
statistical test (α=0.05). P<0.05 was considered to indicate a
statistically significant difference.
Cell lines
Oral cancer cells, H314; tongue cancer cells, HSC-3,
HSC-4, UM1, and UM2; buccal cancer cells, H413; pharyngeal cancer
cells, HN30, HN31; and normal oral mucosa epithelial keratinocytes,
NOK and HOK, were frozen at −150°C and cultured in Dulbecco's
modified Eagle's medium (Gibco; Thermo Fisher Scientific, Inc.)
supplemented with 10% heat inactivated foetal bovine serum (Gibco;
Thermo Fisher Scientific, Inc.), 100 U of penicillin G and 100 U of
streptomycin sulphate under 5% CO2 and a humidified air
atmosphere at 37°C. UM1 and UM2 cells (17) were provided by Dr Xiaofeng Zhou
(Centre for Molecular Biology of Oral Diseases, College of
Dentistry, University of Illinois at Chicago, Chicago, USA), HSC-3
and HSC-4 cells were obtained from the Japan Cancer Research
Resources Bank, H314 and H413 cells were obtained from the European
Collection of Cell Cultures, and NOK, HOK, HN30 and HN31 cells were
kindly provided by Dr JS Gutkind (National Institute of Dental and
Craniofacial Research, Bethesda, MD, USA).
Sera and paraffin specimens
Sera from 32 patients with OSCC and 10 healthy
volunteers were collected at the clinical laboratory of the West
China Hospital of Stomatology, Sichuan University from 2009 to
2011. Nine paraffin specimens (normal oral epithelia and squamous
cell carcinoma tissue) of OSCC were collected by the department of
pathology of West China Hospital of Stomatology, Sichuan University
from 2009 to 2011 (sera samples were obtained from all 32+10
patients and healthy controls, respectively, but paraffin specimens
were obtained from only 9+8 patients and healthy controls,
respectively). Clinical pathology data were obtained from medical
records and histopathologic reports. Eight normal oral epithelia
specimens were obtained from healthy patients who underwent oral
and maxillofacial plastic surgery.
Reagents
Reagent kit (including 5 X PrimeScriptTM buffer,
PrimeScriptTM RT Enzyme Mix I, Oligo dT Primer, Random 6 mers,
RNase Free dH2O and EASY Dilution buffer) for reverse transcription
(RT) and PCR was purchased from Takara Bio Inc. (Otsu, Japan).
Rabbit polyclonal anti-PSCA antibody was purchased from Abcam
(Cambridge, UK). Immunohistochemical kit was purchased from DAKO
(Agilent Technologies, Inc., Santa Clara, CA, USA). Human Prostate
Stem Cell Antigen (PSCA) ELISA kit (cat no. CSB-EL018840HU) was
purchased from CUSABIO BIOTECH (Stratech, Scientific, Ltd.,
UK).
RNA extraction and RT-PCR
Cells were separately homogenized using TRIzol™
reagent (Invitrogen; Thermo Fisher Scientific, Inc.) following the
manufacturer's protocol. Following the complete dissociation of
nucleoprotein complexes, phase separation was achieved using
chloroform and centrifugation (12,000 × g at 4°C for 15 min). The
precipitated RNA from the aqueous phase was washed using 75%
ethanol. RNA was dried and dissolved in RNase-free water. Following
RNA extraction, and the concentration was measured by using a
spectrophotometer. The RNA samples were reverse-transcribed to
cDNA. The obtained cDNA was used for PCR amplification. Primer
sequences of PSCA for RT-PCR were designed as follows: PSCA
forward, ATGGCAGGCTTGGCCCTGCAGCCAGGC and reverse,
CTAGAGCTGGCCGGGTCCCCAGAGCAG; GAPDH forward, GAGTCAACGGATTTGGTCGT
and reverse, TTGATTTTGGAGGGATCTCG was which was used as reference
gene. PCR amplification of the cDNA was performed at an initial
temperature of 94°C for 5 min followed by 30 cycles of 95°C for 30
sec, 55°C for 30 sec and 72°C for 30 sec, followed by a final
extension at 72°C for 10 min. The PCR products were loaded into a
2% agarose gel for electrophoresis.
Enzyme-linked immunosorbent assay
(ELISA)
The expression of PSCA proteins in different samples
was detected by ELISA kit. The main steps are as follows: a
standard curve was drawn. The sample to be tested was diluted and
100 µl solution was added to each well. Test solution (50 µl) was
added and incubated at room temperature for 1 h and chromogenic
substrate was added. The absorbance values were measured at 450 nm,
and the protein concentration in each sample was calculated
according to the standard curve given previously.
Immunohistochemistry (IHC)
All specimens were detected using a two-step IHC
method in the same conditions. Following deparaffinization, antigen
retrieval was performed in a 10 mM citrate buffer (self-prepared as
follows: Storage solution: Solution A: 0.1 M citric acid
monohydrate (C6H8O7•H2O
FW = 210.14); Solution B: 0.1 M trisodium citrate, dihydrate,
(C6H5O7Na3•2H2O
FW = 294.12). Working solution: 18 ml Solution A+ 82 ml Solution B+
900 ml water) at pH 6.0 in a pressure cooker for 3 min. Endogenous
peroxidase was blocked with 3% hydrogen peroxide in phosphate
buffered saline for 10 min at room temperature. The sections were
incubated with primary antibodies against PSCA (1:100; cat no.
ab64919; Abcam) at 4°C overnight, and subjected to incubation with
an goat anti-mouse and rabbit IgG antibody conjugated with
horseradish peroxidase (HRP; stock solution; cat. no. GK600505;
Gene Tech Biotechnology Co., Ltd., Shanghai, China) for 30 min at
room temperature. Positive staining was observed as brown yellow
granules. An immunoreactive score (IRS) was calculated for all
samples. Five fields were randomly selected at high magnification
(magnification, ×400), and the staining intensity (SI) and
percentage of positive cells (PP) were scored (SI evaluation) as
follows: Colourless - 0, buff - 1 point, tan - 2 points, brown - 3
points. PP evaluation scores were as follows: Negative - 0,
positive cells 10% or less - 1 point, 11–50% - 2 points, 51–80% - 3
points, >80% - 4 points. IRS was calculated using the equation,
IRS=SI × PP. IRS >3 points was considered positive. All of these
were analyzed using AperioImageScope software (Version 11; Leica
Microsystems, Inc., Buffalo Grove, IL, USA).
Statistical analysis
PSCA expression in OSCC and normal tissues was
compared via Fisher's exact probability test, and statistical
analysis was performed by SPSS 13.0 software (SPSS, Inc., Chicago,
IL, USA). P<0.05 was considered to indicate a statistically
significant difference.
Association study of PSCA polymorphism
and clinical prognosis of patients with OSCC
Previous experiments in the present study identified
the PSCA gene polymorphism locus, rs2294008, as a genetic
susceptibility locus of OSCC, and the CC genotype frequency was
significantly higher in patients with OSCC compared with controls.
OSCC patients clinical and postoperative follow-up data were
analysed to explore the association between PSCA polymorphism and
clinical prognosis of patients with OSCC.
Study case inclusion
Seventy-six OSCC cases (as aforementioned) were
derived from patients diagnosed as OSCC and who underwent oral and
maxillofacial surgery at West China Hospital of Stomatology,
Sichuan University. Recurrence or mortality incidence was recorded
based on a telephone follow-up. Rs2294008 genotype information of
patients with OSCC was obtained from the foregoing OSCC
case-control study results.
Statistical analysis
The association between rs2294008 locus gene type
and the clinical indicators was analysed through the single factor
chi-squared test, and Fisher's exact probability method was used to
compare values between groups. Survival curves were obtained
through the Kaplan-Meier method, and the independent impact of the
genotype and clinical variables on the prognosis of OSCC risk were
analysed by using the Cox proportional hazards regression model.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Meta-analysis results
The GWAS Catalogue (2012-03-09) screening resulted
in the identification of 91 articles published in 26 journals, and
225 SNP loci associated with nine types of malignant tumour were
identified. Among these, 11 loci were associated with bladder
cancer, 50 loci with breast cancer, 19 loci with colorectal cancer,
7 loci with liver cancer, 30 loci with lung cancer, 11 loci with
nasopharyngeal carcinoma, 74 loci with prostate cancer, 2 loci with
skin cancer, and 23 loci with digestive tract carcinoma. Two loci
were associated with two tumour types: rs401681 was associated with
lung and bladder cancer, and rs6983267 was associated with prostate
and colorectal cancer. Twelve loci (Table
I) were located in the exons of 11 genes, probably affecting
genes functions. Finally, there were two loci associated with more
than one malignant tumor.
 | Table I.SNPs located in exons. |
Table I.
SNPs located in exons.
| SNP | Gene symbol | SNP | Gene symbol |
|---|
| rs671 | ALDH2 | rs2274223 | PLCE1 |
| rs8170 | C19orf62 | rs3765524 | PLCE1 |
| rs130067 | CCHCR1 | rs2294008 | PSCA |
| rs971074 | ADH7 | rs2292884 | MLPH |
| rs1051730 | CHRNA3 | rs4072037 | MUC1 |
| rs1229984 | ADH1B | rs10936599 | MYNN |
Multicentre case-control study
The multicentre case-control study of a Chinese Han
population led to the identification of 12 polymorphism loci whose
distribution in patients with OSCC and healthy volunteers is
demonstrated in Table II.
 | Table II.Allele distribution of the 12
selected SNPs. |
Table II.
Allele distribution of the 12
selected SNPs.
| SNP ID | Gene symbol | A/a | HWE | Risk allele | MAF in case | MAF in control | P
(Chi-squared) |
|---|
| rs671 | ALDH2 | G/A | 0.2648 | A | 0.226 | 0.179 | 0.0674 |
| rs8170 | C19orf62 | C/T | 1b | T | 0.005 | 0.002 | 0.4569 |
| rs130067 | CCHCR1 | A/C | 0.1356 | C | 0.346 | 0.309 | 0.2178 |
| rs971074 | ADH7 | G/A | 0.6897 | G | 0.104 | 0.129 | 0.2115 |
| rs1051730 | CHRNA3 | C/T | 1b | T | 0.037 | 0.032 | 0.662 |
| rs1229984 | ADH1B | A/G | 0.0462b | A | 0.315 | 0.339 | 0.4224 |
| rs2274223 | PLCE1 | A/G | 0.549 | G | 0.228 | 0.198 | 0.2528 |
| rs2292884 | MLPH | A/G | 0.5995 | A | 0.279 | 0.29 | 0.6836 |
| rs2294008 | PSCA | C/T | 0.8509 | C | 0.258 | 0.323 | 0.0239a |
| rs3765524 | PLCE1 | C/T | 0.4102 | T | 0.227 | 0.195 | 0.2204 |
| rs4072037 | MUC1 | A/G |
2.29E-14b | A | 0.007 | 0.019 | 0.1023 |
| rs10936599 | MYNN | T/C | 0.0884 | T | 0.429 | 0.456 | 0.4001 |
The allele distribution of rs4072037 in MUC1,
rs1229984 in ADH1B, rs8170 in C19orf62, and rs1051730
in CHRNA3 did not conform HWE and were therefore excluded
from further analysis. The allele distribution of rs2294008
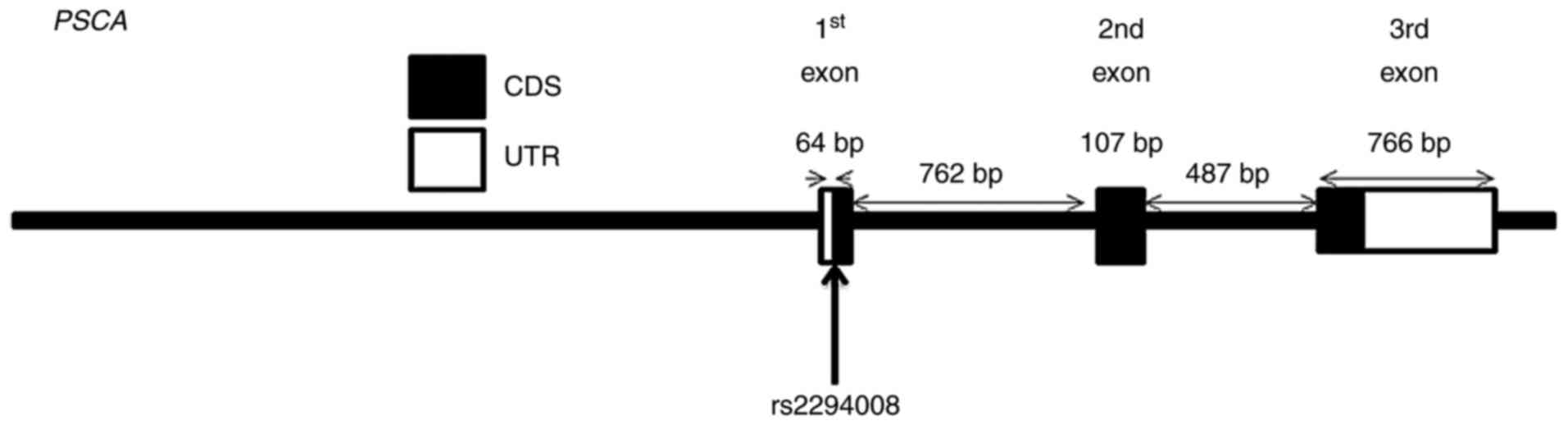
(Fig. 1) was significantly different
between patients with OSCC and healthy volunteers. The C allele
seems to be a risk allele for OSCC as its frequency was higher in
patients with OSCC compared with healthy volunteers [T vs. C;
OR=0.728 (0.552, 0.959); P<0.05].
The genotype distribution of the eight remaining
loci in patients with OSCC and normal controls is illustrated in
Table III. Using the recessive
inheritance model, rs2292884 and rs3765524 polymorphisms were
identified to be associated with OSCC (P<0.05). Rs2294008 in
PSCA was significantly different between patients with OSCC and
healthy controls (P<0.01). The CC vs. CT + TT model demonstrated
that the CC genotype frequency was significantly higher in patients
with OSCC than in the normal group (P<0.01). The CC genotype was
associated with OSCC risk [OR = 1.699 (1.188, 2.429); P<0.01].
No statistical difference was observed (P>0.05) in the CC + CT
vs. TT model (Table III).
 | Table III.Genotype distribution of the 8
SNPs. |
Table III.
Genotype distribution of the 8
SNPs.
| SNP ID | Gene symbol | A/a | Population | AA | Aa | aa | P-value | P (AA+Aa vs.
aa) | P (AA vs.
Aa+aa) |
|---|
| rs671 | ALDH2 | G/A | OSCC | 163 | 101 | 12 |
|
|
|
|
|
|
| Control | 139 | 67 | 4 | 0.142 | 0.135 | 0.108 |
| rs130067 | CCHCR1 | A/C | OSCC | 125 | 119 | 38 |
|
|
|
|
|
|
| Control | 107 | 86 | 24 | 0.49 | 0.417 | 0.269 |
| rs971074 | ADH7 | C/A | OSCC | 223 | 56 | 1 |
|
|
|
|
|
|
| Control | 165 | 48 | 4 | 0.207 | 0.1 | 0.335 |
| rs2274223 | PLCE1 | A/G | OSCC | 169 | 96 | 16 |
|
|
|
|
|
|
| Control | 134 | 77 | 4 | 0.099 | 0.031a | 0.621 |
| rs2292884 | MLPH | A/G | OSCC | 141 | 122 | 17 |
|
|
|
|
|
|
| Control | 111 | 86 | 20 | 0.351 | 0.185 | 0.86 |
| rs2294008 | PSCA | C/T | OSCC | 161 | 98 | 24 |
|
|
|
|
|
|
| Control | 94 | 103 | 18 | 0.009a | 0.966 | 0.004a |
| rs3765524 | PLCE1 | C/T | OSCC | 169 | 98 | 15 |
|
|
|
|
|
|
| Control | 137 | 77 | 4 | 0.128 | 0.043a | 0.507 |
| rs10936599 | MYNN | T/C | OSCC | 85 | 153 | 45 |
|
|
|
|
|
|
| Control | 61 | 113 | 42 | 0.581 | 0.301 | 0.662 |
PSCA transcription and expression in
OSCC cell lines and patient serum and specimens
With universal screening of genetic susceptibility
loci of malignant tumours and the multicentre case-control study,
rs2294008 (located in exon 1 of PSCA gene) was identified as the
OSCC genetic susceptibility locus. This result suggests that
changes in PSCA function may affect the occurrence of OSCC. Thus,
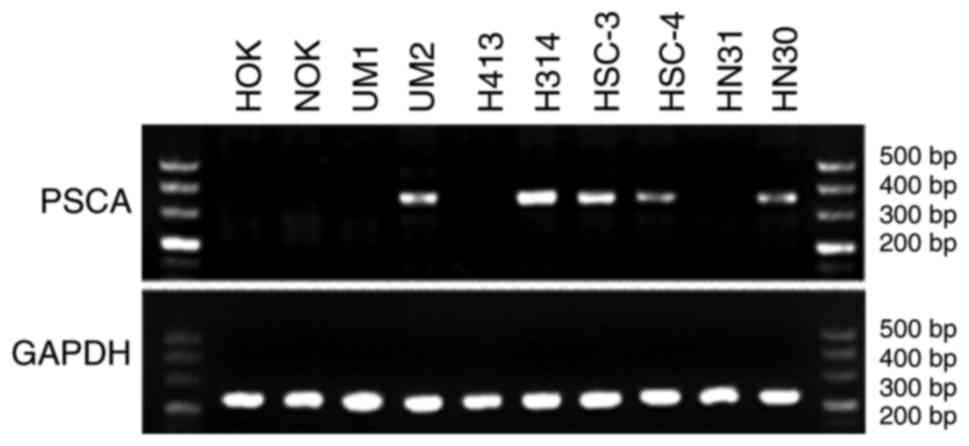
this locus was further investigated. As illustrated in Fig. 2, semi-quantitative PCR resulted in the
amplification of a band of 345 bp corresponding to PSCA.
PSCA mRNA expression was detected in OSCC cell lines, UM2, H314,
HSC-3, and HSC-4, and in HN30 pharyngeal cancer cells, but not in
HOK and NOK epithelial cells.
PSCA was detected in the sera of 14 of 32 patients
with OSCC. Six of 11 patients with OSCC presented with the CC
genotype and were positive for PSCA, while eight of 21 patients
with OSCC presented with the CT/TT genotype and were positive for
PSCA. No PSCA expression was detected in the serum of the 10
healthy subjects (Table IV).
 | Table IV.PSCA expression in OSCC and normal
serum. |
Table IV.
PSCA expression in OSCC and normal
serum.
| Serum type | Number of
patients | PSCA+ | PSCA- |
|---|
| Normal serum | 10 | 0 | 10 |
| Serum of OSCC | 32 | 14 | 18 |
| OSCC
CC-genotype | 11 | 6 | 5 |
| OSCC
CT/TT-genotype | 21 | 8 | 13 |
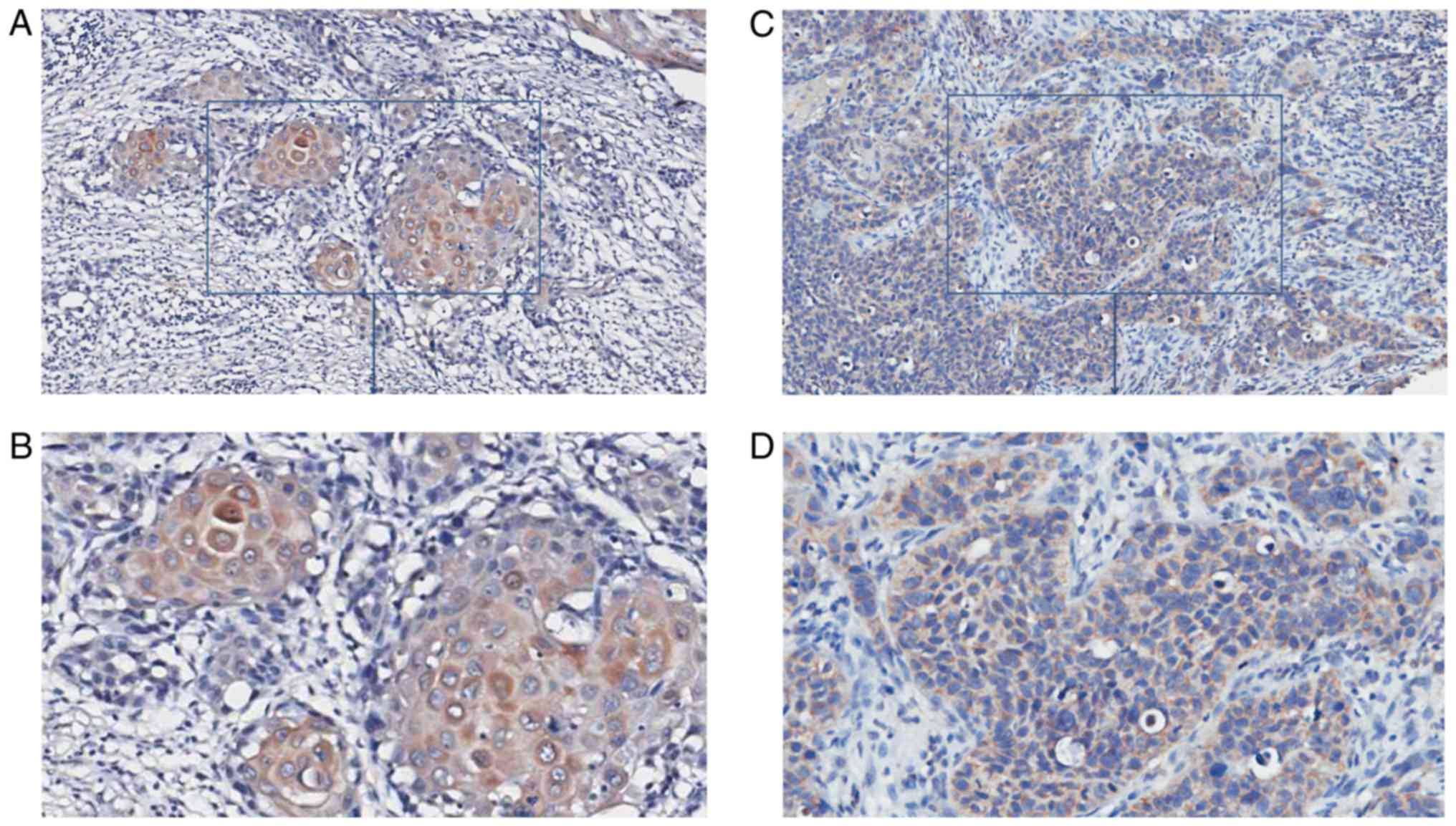
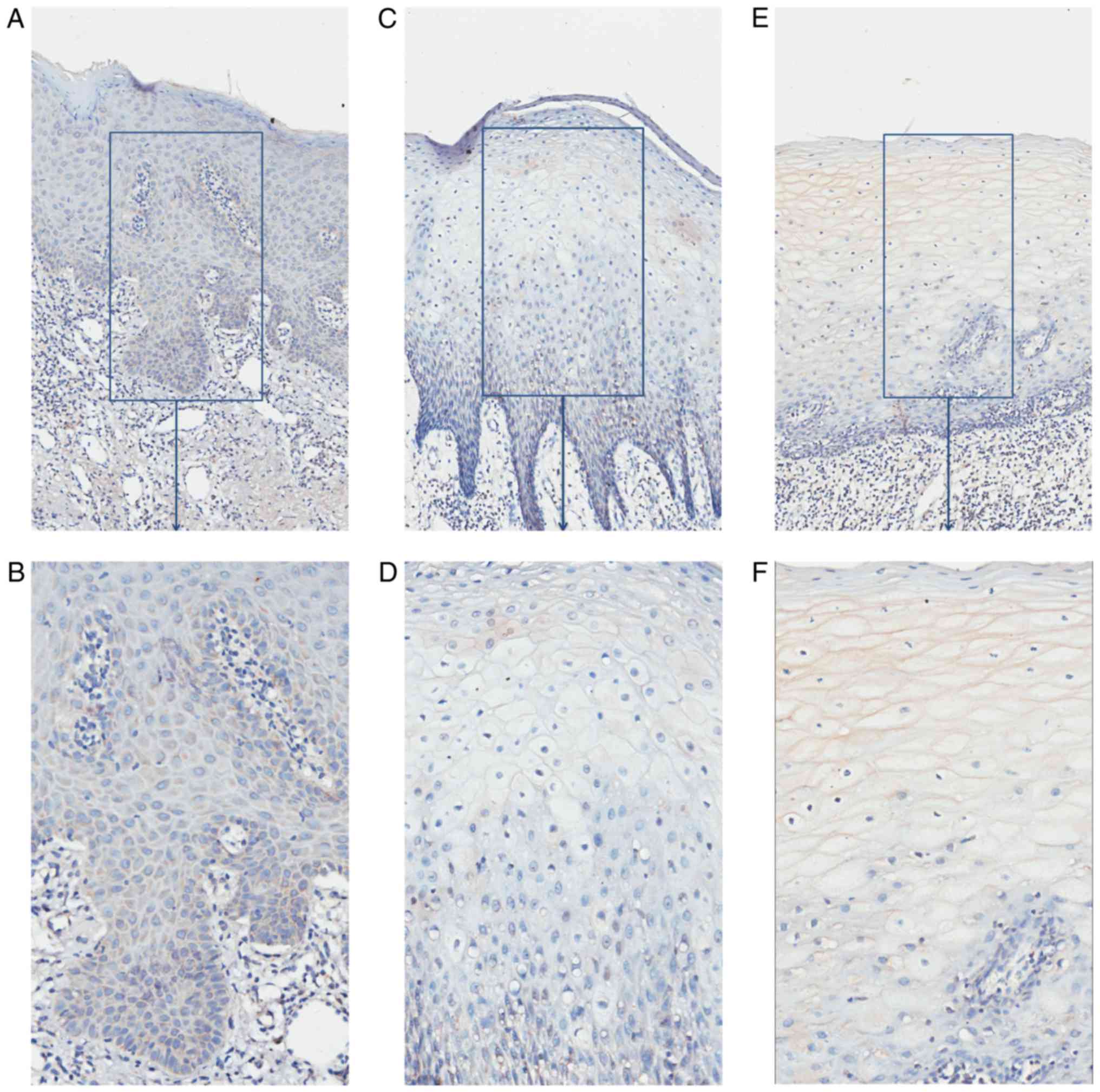
Paraffin specimens from nine patients with OSCC
(five patients with serum that was PSCA-positive, four serum
PSCA-negative; four CC genotypes, and five CT/TT genotypes) and
eight controls were collected and immunochemically stained; the
results are demonstrated in Table V.
In specimens from the nine OSCC cases, epithelium and nests of
eight cases were shaded, and the IRS scores of six cases were above
3 and were considered PSCA-positive (Fig.
3). It demonstrated that PSCA protein may be highly expressed
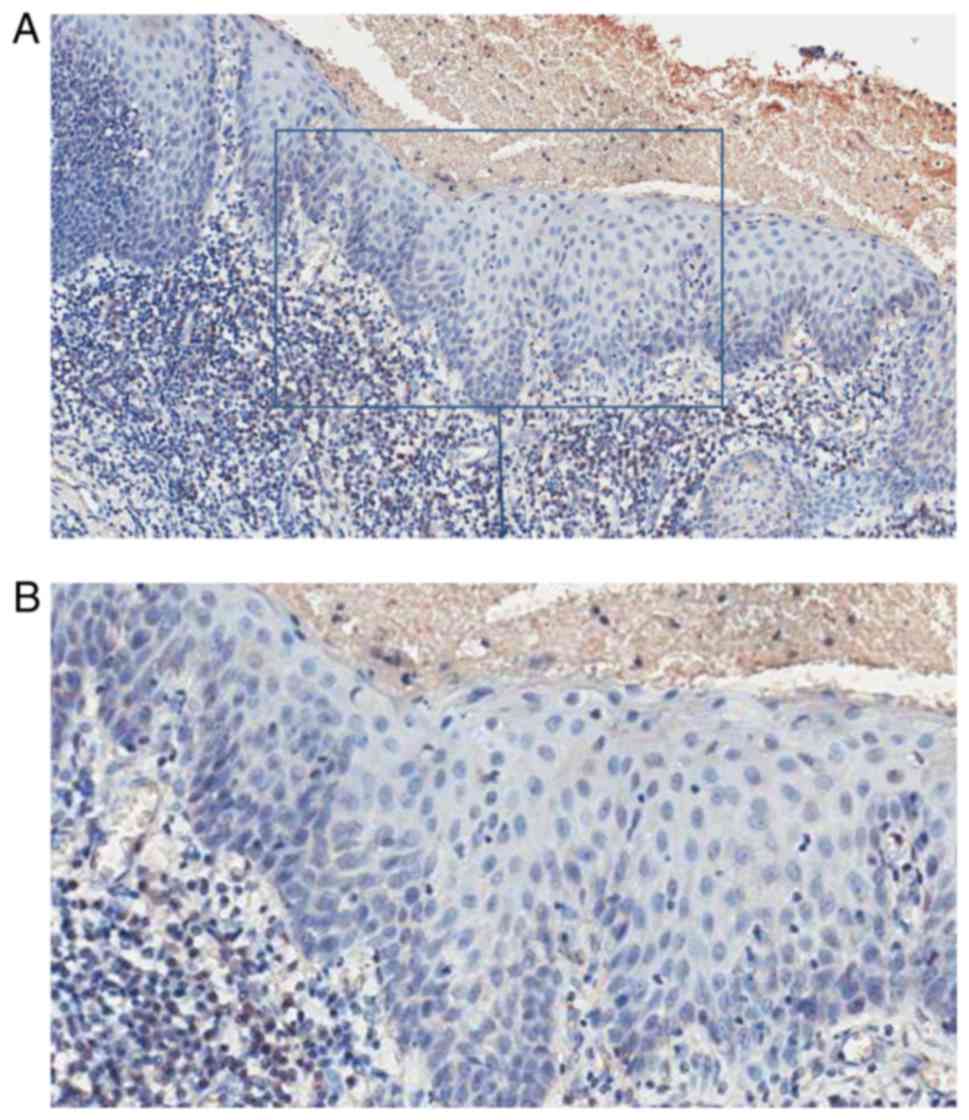
in the OSCC tissues. In specimens from eight controls, one
presented an IRS score of 3, while the IRS scores of the remaining
were <3 and were considered PSCA-negative (Fig. 4). The percentage of PSCA-positive
staining was significantly higher in the OSCC than in the normal
control group (P<0.05). PSCA staining was mainly observed in the
cytoplasm in OSCC and normal tissues. PSCA immunohistochemical
staining was positive in specimens from five patients with OSCC who
were positive for serum, while it was only positive in one of four
patients with OSCC who were negative for serum PSCA; the difference
was significant (P<0.05; Table V).
The percentage of PSCA positive staining was not statistically
different between OSCC patients with different genotypes
(P>0.05). However, PSCA protein localisation was different in
OSCC patients with different genotypes. The T allele of rs2294008
encodes a translation initiation codon upstream of the reported
site and changes protein localization from the cytoplasm to the
cell surface (18). In OSCC patients
with the CC genotype, the cytoplasm of cells from the epithelium
and nests was PSCA-positive. In OSCC patients with the CT/TT
genotype, the membrane of the epithelial cornification layer cells
was PSCA-positive, and the cytoplasm of the epithelial basal layer
cells and nests was PSCA-positive (Fig.
5).
 | Table V.PSCA protein expression in OSCC and
normal tissues. |
Table V.
PSCA protein expression in OSCC and
normal tissues.
| Tissue type | Number | PSCA+ | PSCA- |
P-valueb |
|---|
| OSCC | 9 | 6 | 3 |
|
| Normal tissue | 8 | 1 | 7 | 0.022a |
| OSCC Elisa+ | 5 | 5 | 0 |
|
| OSCC Elisa- | 4 | 1 | 3 | 0.012a |
| OSCC
CC-genotype | 4 | 3 | 1 |
|
| OSCC
CT/TT-genotype | 5 | 3 | 2 | 0.685 |
Association between rs229008
polymorphism and clinical and pathological characteristics of
patients with OSCC
The association between rs2294008 polymorphism
distribution and the clinical characteristics of 76 patients with
OSCC is illustrated in Table VI.
Patients with the CT/TT genotype drank less alcohol (P<0.05)
compared with patients with the CC genotype. The CT/TT genotype was
also associated with tumour size and T3/T4 stage when compared with
the CC genotype (P<0.05). In addition, some weak associations
(P<0.1) between the CT/TT genotype and smoking (P=0.085), lymph
node metastasis (P=0.052), and higher clinical stage (P=0.075) were
observed.
 | Table VI.Rs2294008 polymorphism and clinical
parameters. |
Table VI.
Rs2294008 polymorphism and clinical
parameters.
|
| Total | CC | CT&TT | P-value |
|---|
| Sex |
|
|
|
|
|
Female | 27 | 19 | 8 |
|
|
Male | 49 | 25 | 24 | 0.102 |
| Age, years |
|
|
|
|
|
≤65 | 58 | 34 | 24 |
|
|
>65 | 18 | 10 | 8 | 0.818 |
| Smoking |
|
|
|
|
|
Yes | 42 | 28 | 14 |
|
| No | 34 | 16 | 18 | 0.085 |
| Drinking |
|
|
|
|
|
Yes | 48 | 33 | 15 |
|
| No | 28 | 11 | 17 | 0.012a |
| Grading |
|
|
|
|
| 1 | 49 | 27 | 22 |
|
|
2&3 | 27 | 17 | 10 | 0.507 |
| Nodal status |
|
|
|
|
|
Negative | 52 | 34 | 18 |
|
|
Positive | 24 | 10 | 14 | 0.052 |
| Tumor size |
|
|
|
|
| T1 | 22 | 17 | 5 |
|
| T2 | 35 | 20 | 15 |
|
| T3 | 5 | 2 | 3 |
|
| T4 | 13 | 4 | 9 | 0.045a |
| Tumor stage |
|
|
|
|
| 1 | 20 | 15 | 5 |
|
| 2 | 23 | 14 | 9 |
|
| 3 | 14 | 8 | 6 |
|
| 4 | 18 | 6 | 12 | 0.075 |
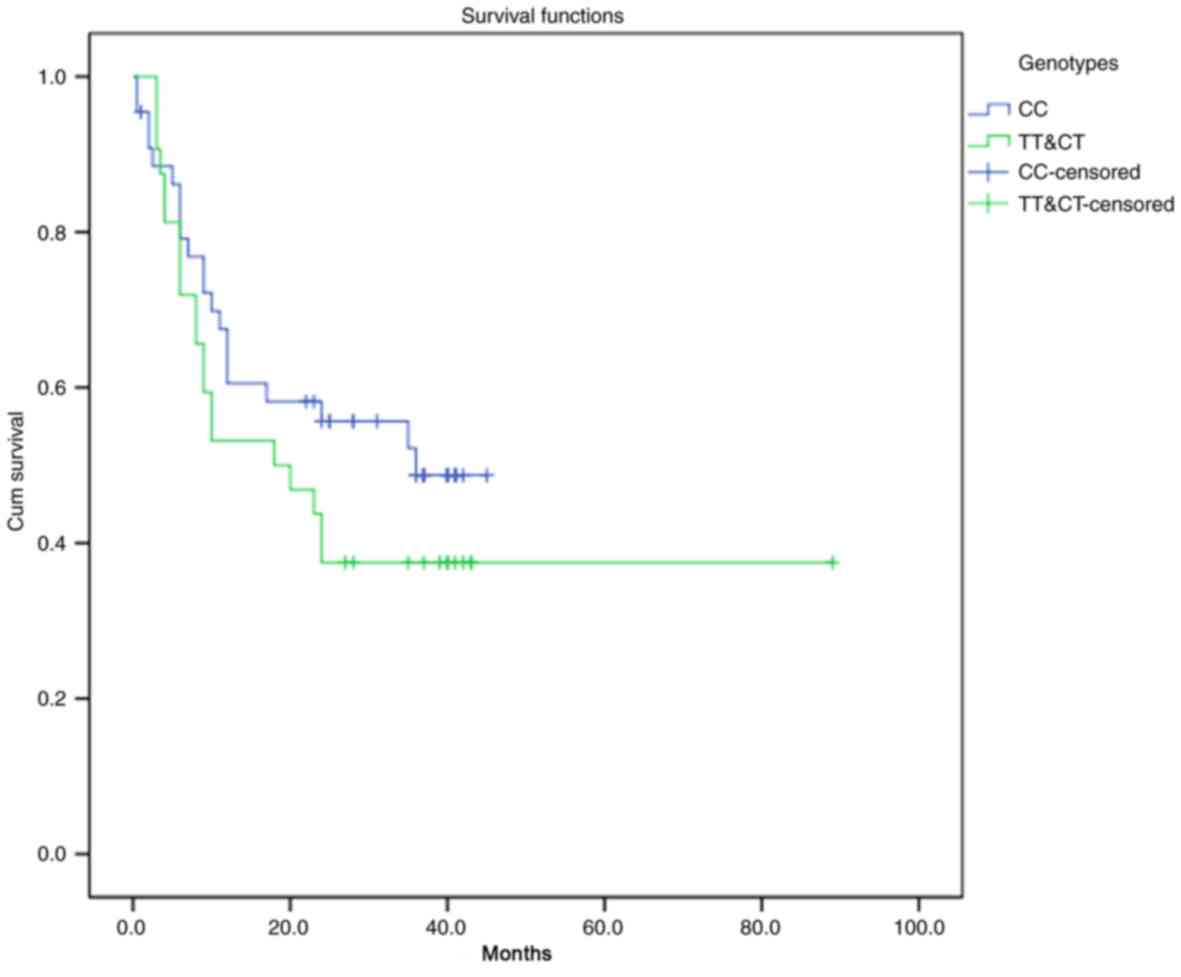
Since the follow-up time was <3 years for many
patients, the mortality percentage was <50%, and, therefore, the
results were not suitable for survival analysis based on mortality.
Therefore, the rate of survival was analysed based on cancer
recurrence in the 76 patients with OSCC (Table VII). The resulting survival curve
based on postoperative recurrence and the different genotypes is
demonstrated in Fig. 6. The
recurrence rate in OSCC patients presenting the CT/TT genotype was
62.5% and that in OSCC patients presenting the CC genotype was
47.7%; the difference was not statistically significant
(P>0.05). Postoperative recurrence tended to increase in OSCC
patients presenting the CT/TT genotype. As depicted in Table VIII, the COX proportional hazards
regression model indicated that the different genotypes at the
rs2294008 locus did not significantly influence postoperative
recurrence in patients with OSCC [OR=0.9248 (0.4513, 1.8951),
P>0.05]. Tumour size (P<0.05) and tumour clinical stage
(P<0.05) were independent factors influencing postoperative
recurrence in patients with OSCC.
 | Table VII.Recurrence analysis of 76 patients
with OSCC. |
Table VII.
Recurrence analysis of 76 patients
with OSCC.
| Genotype | Total | No recurrence | Percentage (%) | P-value |
|---|
| CC | 44 | 23 | 52.30 |
|
| CT+TT | 32 | 12 | 37.50 | 0.261 |
| Overall | 76 | 35 | 46.10 |
|
 | Table VIII.Result of COX proportional Hazards
model. |
Table VIII.
Result of COX proportional Hazards
model.
|
|
| 95.0% CI for
Exp(B) |
|
|---|
|
|
|
|
|
|---|
|
| OR | Lower | Upper | P-value |
|---|
| Genotype | 0.9248 | 0.4513 | 1.8951 | 0.8310 |
| Sex | 1.2570 | 0.4548 | 3.4739 | 0.6593 |
| Smoking | 0.7874 | 0.2831 | 2.1902 | 0.6470 |
| Drinking | 0.9204 | 0.3286 | 2.5784 | 0.8747 |
| Age | 1.4636 | 0.6350 | 3.3734 | 0.3713 |
| Grading | 1.4347 | 0.5838 | 3.5259 | 0.4315 |
| Tumor size |
|
|
| 0.0456a |
| T1 | 61.8182 | 3.2625 | 1171.3486 | 0.0060 |
| T2 | 10.8660 | 1.6237 | 72.7161 | 0.0139 |
| T3 | 17.3644 | 0.6132 | 491.7257 | 0.0943 |
| Nodal status |
|
|
| 0.7779 |
|
Negative | 1.0067 | 0.1147 | 8.8342 | 0.9952 |
|
Positive | 1.6820 | 0.3030 | 9.3381 | 0.5522 |
| Tumor stage |
|
|
| 0.0191a |
| 1 | 0.0049 | 0.0002 | 0.1463 | 0.0021 |
| 2 | 0.0740 | 0.0067 | 0.8171 | 0.0336 |
| 3 | 0.0449 | 0.0038 | 0.5359 | 0.0142 |
Discussion
Tumours are divided into many types according to
their location and histological characteristics and genetic
background may influence their development (13). In the current study, seven types of
cancers with the highest incidence and two types of cancer, skin
cancer and NPC, which have the same origin as OSCC, were used to
identify common SNPs associated with cancer susceptibility and to
evaluate their involvement in OSCC.
PSCA is located on chromosome 8 q24.3 and it belongs
to the Thy-1/Ly-6 super family. PSCA is highly expressed in
prostate cancer, and its expression is associated with
classification, clinical stage, metastasis, and prognosis of
patients with prostate cancer (19,20). It is
a marker for prostate cancer diagnosis and prognosis and a novel
target for the treatment of prostate cancer (19,21,22). PSCA
is also highly expressed in bladder, pancreatic, and kidney cancer
(23–25), while its expression level is low in
other tumours such as gastric, oesophageal, and gallbladder cancer
(26,27). As a type of membrane proteins with GPI
anchoring, PSCA may serve a role in T cell activation (21). As a member of the Thy-1 family, is
involved in the process of T cell activation, proliferation and
survival of stem cells, and cell factor response; PSCA may also be
involved in tumour formation, and activation and adhesion of tumour
cells (28,29). In 2002, De Nooij-van Dalen et
al (27) reported that PSCA was
transcribed in cancer cells and normal head and neck squamous
tissue. PSCA transcription was significantly different between head
and neck squamous carcinoma and normal tissues, suggesting it may
be involved in the development of head and neck squamous cell
carcinomas.
Although little is known regarding the mechanisms
underlying the regulation of PSCA expression, androgens are known
to be involved in this process (30).
Previous studies have detected androgen response elements in
prostate epithelial PSCA promoter regions (30). Bahrenberg et al (31)demonstrated that growing the bladder
cancer cell line RT112 in a hydrophobic medium resulted in cell
clustering, while PSCA mRNA levels increased significantly,
suggesting that PSCA expression may be involved in the regulation
of epithelial cell adhesion. Furthermore, following addition of
phorbol-12-myristate-13-acetate, PSCA mRNA levels increased
significantly, suggesting that PSCA transcription may be associated
with and indirectly regulated by protein kinase. In contrast,
epidermal growth factor, platelet-derived growth factor (PDGF),
tumour necrosis factor-alpha, and interferon gamma could not
increase PSCA transcription level (31). The authors pointed out that PSCA
expression was likely regulated by a strong induction type of
promoter by specific extracellular signals (31). A previous study has demonstrated that
PSCA expression is downregulated in telomerase-transduced urethral
epithelial cells, suggesting that PSCA may be regulated by a
mechanism involving telomerases (32).
Some studies have revealed that PSCA is associated
with the inhibition of tumour growth and metastasis and with
prolonged survival (33,34). In contrast, in a gastric cancer cell
line, PSCA inhibited cell growth, but had no effect on cell
apoptosis (35). PSCA is upregulated
or downregulated in various human tumours, suggesting that PSCA may
be carcinogenic or act as tumour suppressor, depending on the cell
type and the nature of the interaction between molecules and
signalling pathways (36,37).
H314 and H413 cells are both mutated for P53, but
the mutation position is different, suggesting that P53 mutation at
different sites may affect PSCA expression through complex
signalling pathways.
PSCA mRNA expression levels were higher in OSCC cell
lines than that in normal keratin epithelial cells.
The multicentre case-control study demonstrated that
the CC genotype frequency was higher in patients with OSCC than in
healthy subjects and that the CC genotype was an OSCC
susceptibility factor. However, in the present analysis of clinical
and pathological indices in patients with OSCC, the CT/TT genotype
was associated with tumour size, stage, and lymph node metastasis.
Although the association between the CT/TT genotype and recurrence
was not statistically significant, the CT/TT genotype may have an
adverse impact for recurrence based on the survival curve. This
seemingly contradictory phenomenon has also been reported by other
groups (35,38–41). The T
allele in the rs2294008 loci was confirmed as a risk allele of
diffuse gastric cancer (35,38–40), while
survival analysis by Wang et al (41) demonstrated that the CT/TT genotype had
a positive protective effect on the prognosis of patients with
gastric cancer. The study speculated that patients with the CC
genotype may be more resistant to radiation and chemotherapy than
patients with the CT/TT genotype, and hence lead to a poor
prognosis. Nevertheless, the role of the rs2294008 polymorphism and
PSCA in tumour pathogenesis remains unclear.
The present study has limitations given its small
sample size and the short follow-up time. In further research, the
influence of genotype should be verified at the mRNA and protein
levels.
To conclude, rs2294008 polymorphism may be
associated with OSCC development. The corresponding gene,
PSCA, was expressed in OSCC but not in normal cell lines. No
association was detected between the rs2294008 polymorphism and
OSCC recurrence, but positive association was observed between the
CT/TT genotype and smoking history, drinking history, lymph node
metastasis, tumour size, and clinical stage. The present study
demonstrated that PSCA may serve a role in OSCC and provided a
novel perspective for future OSCC study.
Acknowledgements
Not applicable
Funding
The present study was supported by the National
Natural Science Foundation of China (grant nos. 81321002, 81472533
and 81500864), and the Nonprofit Industry Research Specific Fund of
National Health and Family Planning Commission of China (grant no.
201502018).
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KZ and XL conceived and designed the study. JL
guided the experiments. KZ, XL, JL, JW and WG performed the
experiments. LJ and HD collected and processed the clinical data.
HX and JW analyzed and interpreted the patient data. KZ and XL
wrote the paper, and JL, XZ and QC reviewed and edited the
manuscript. XZ and QC contributed to the conception of the study
and helped perform the analysis with constructive discussions. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was conducted in accordance with
the standards of the Declaration of Helsinki and approved by the
Ethical Review Committee of West China Hospital of Stomatology,
Sichuan University, China (approval no. 2010056). All patients
provided written informed consent for their information to be
stored and used in the hospital database.
Consent for publication
All patients provided informed consent for the
publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
OSCC
|
oral squamous cell carcinoma
|
|
GWAS
|
genome-wide association study
|
|
SNPs
|
single nucleotide polymorphisms
|
|
PSCA
|
prostate stem cell antigen
|
|
UADT
|
upper aerodigestive tract
|
|
HWE
|
Hardy Weinberg equilibrium
|
|
PCR
|
polymerase chain reaction
|
|
ELISA
|
enzyme-linked immunosorbent assay
|
|
IHC
|
immunohistochemistry
|
|
IRS
|
immunoreactive score
|
|
PKC
|
protein kinase C
|
References
|
1
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Podlodowska J, Szumiło J, Podlodowski W,
Starosławska E and Burdan F: Epidemiology and risk factors of the
oral carcinoma. Pol Merkur Lekarski. 32:135–137. 2012.(In Polish).
PubMed/NCBI
|
|
3
|
Wang Z, Jiang L, Huang C, Li Z, Chen L,
Gou L, Chen P, Tong A, Tang M, Gao F, et al: Comparative proteomics
approach to screening of potential diagnostic and therapeutic
targets for oral squamous cell carcinoma. Mol Cell Proteomics.
7:1639–1650. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Noguti J, De Moura CF, De Jesus GP, Da
Silva VH, Hossaka TA, Oshima CT and Ribeiro DA: Metastasis from
oral cancer: An overview. Cancer Genomics Proteomics. 9:329–335.
2012.PubMed/NCBI
|
|
5
|
Hardy J and Singleton A: Genomewide
association studies and human disease. N Engl J Med. 360:1759–1768.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Habibi I, Sfar I, Kort F, Aounallah-Skhiri
H, Chebil A, Chouchene I, Bouraoui R, Limaiem R, Largheche L,
Jendoubi-Ayed S, et al: Y402H polymorphism in complement factor H
and age-related macular degeneration in the Tunisian population.
Ophthalmic Res. 49:177–184. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Varghese JS and Easton DF: Genome-wide
association studies in common cancers-what have we learnt. Curr
Opin Genet Dev. 20:201–209. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wang Q, Wang JY, Zhang XP, Lv ZW, Fu D, Lu
YC, Hu GH, Luo C and Chen JX: RLIP76 is overexpressed in human
glioblastomas and is required for proliferation, tumorigenesis and
suppression of apoptosis. Carcinogenesis. 34:916–926. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tan B, Anaka M, Deb S, Freyer C, Ebert LM,
Chueh AC, Al-Obaidi S, Behren A, Jayachandran A, Cebon J, et al:
FOXP3 over-expression inhibits melanoma tumorigenesis via effects
on proliferation and apoptosis. Oncotarget. 5:264–276. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ma GZ, Liu CH, Wei B, Qiao J, Lu T, Wei
HC, Chen HD and He CD: Baicalein inhibits DMBA/TPA-induced skin
tumorigenesis in mice by modulating proliferation, apoptosis, and
inflammation. Inflammation. 36:457–467. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang J, Cao C, Luo H, Xiong S, Xu Y and
Xiong W: Tumour necrosis factor alpha −308G/A polymorphism and risk
of the four most frequent cancers: A meta-analysis. Int J
Immunogenet. 38:311–320. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kotnis A, Kannan S, Sarin R and Mulherkar
R: Case-control study and meta-analysis of sult1a1 arg213his
polymorphism for gene, ethnicity and environment interaction for
cancer risk. Br J Cancer. 99:1340–1347. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dong LM, Potter JD, White E, Ulrich CM,
Cardon LR and Peters U: Genetic susceptibility to cancer: The role
of polymorphisms in candidate genes. JAMA. 299:2423–2436. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Levine DM, Ek WE, Zhang R, Liu X, Onstad
L, Sather C, Lao-Sirieix P, Gammon MD, Corley DA, Shaheen NJ, et
al: A genome-wide association study identifies new susceptibility
loci for esophageal adenocarcinoma and Barrett's esophagus. Nat
Genet. 45:1487–1493. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hindorff LA, MacArthur J; (European
Bioinformatics Institute), Morales J (European Bioinformatics
Institute), ; Junkins HA, Hall PN, Klemm AK and Manolio TA: A
Catalog of Published Genome-Wide Association Studies. A Catalog of
Published Genome-Wide Association Studies. https://www.genome.gov/gwastudiesSeptember 3–2012
|
|
16
|
Hartmer R, Storm N, Boecker S, Rodi CP,
Hillenkamp F, Jurinke C and van den Boom D: RNase T1 mediated
base-specific cleavage and MALDI-TOF MS for high-throughput
comparative sequence analysis. Nucleic Acids Res. 31:e472003.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nakayama S, Sasaki A, Mese H, Alcalde RE
and Matsumura T: Establishment of high and low metastasis cell
lines derived from a human tongue squamous cell carcinoma. Invasion
Metastasis. 18:219–228. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tanikawa C, Urabe Y, Matsuo K, Kubo M,
Takahashi A, Ito H, Tajima K, Kamatani N, Nakamura Y and Matsuda K:
A genome-wide association study identifies two susceptibility loci
for duodenal ulcer in the Japanese population. Nat Genet.
44:430–434. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gu Z, Thomas G, Yamashiro J, Shintaku IP,
Dorey F, Raitano A, Witte ON, Said JW, Loda M and Reiter RE:
Prostate stem cell antigen (PSCA) expression increases with high
gleason score, advanced stage and bone metastasis in prostate
cancer. Oncogene. 19:1288–1296. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Reiter RE, Sato I, Thomas G, Qian J, Gu Z,
Watabe T, Loda M and Jenkins RB: Coamplification of prostate stem
cell antigen (PSCA) and MYC in locally advanced prostate cancer.
Genes Chromosomes Cancer. 27:95–103. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Reiter RE, Gu Z, Watabe T, Thomas G,
Szigeti K, Davis E, Wahl M, Nisitani S, Yamashiro J, Le Beau MM, et
al: Prostate stem cell antigen: A cell surface marker overexpressed
in prostate cancer. Proc Natl Acad Sci USA. 95:1735–1740. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Naz RK and Shiley B: Prophylactic vaccines
for prevention of prostate cancer. Front Biosci (Schol Ed).
4:932–940. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
23
|
Fu YP, Kohaar I, Rothman N, Earl J,
Figueroa JD, Ye Y, Malats N, Tang W, Liu L, Garcia-Closas M, et al:
Common genetic variants in the PSCA gene influence gene expression
and bladder cancer risk. Proc Natl Acad Sci USA. 109:4974–4979.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hao JY, Yang YL, Li S, Qian XL, Liu FF and
Fu L: PSCA expression in invasive micropapillary carcinoma of
breast. Zhonghua Bing Li Xue Za Zhi. 40:382–386. 2011.(In Chinese).
PubMed/NCBI
|
|
25
|
Wang D, Wang Z, Tian J, He X, Chowdhury
WH, Zhang X, Li S and Rodriguez R: Prostate stem cell antigen
enhancer and uroplakin II promoter based bladder cancer targeted
tissue-specific vector. Urol Oncol. 28:164–169. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ono H, Hiraoka N, Lee YS, Woo SM, Lee WJ,
Choi IJ, Saito A, Yanagihara K, Kanai Y, Ohnami S, et al: Prostate
stem cell antigen, a presumable organ-dependent tumor suppressor
gene, is down-regulated in gallbladder carcinogenesis. Genes
Chromosomes Cancer. 51:30–41. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
de Nooij-van Dalen AG, van Dongen GA,
Smeets SJ, Nieuwenhuis EJ, Stigter-van Walsum M, Snow GB and
Brakenhoff RH: Characterization of the human Ly-6 antigens, the
newly annotated member Ly-6K included, as molecular markers for
head-and-neck squamous cell carcinoma. Int J Cancer. 103:768–774.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Bamezai A: Mouse Ly-6 proteins and their
extended family: Markers of cell differentiation and regulators of
cell signaling. Arch Immunol Ther Exp (Warsz). 52:255–266.
2004.PubMed/NCBI
|
|
29
|
Hruska M, Keefe J, Wert D, Tekinay AB,
Hulce JJ, Ibañez-Tallon I and Nishi R: Prostate stem cell antigen
is an endogenous lynx1-like prototoxin that antagonizes
alpha7-containing nicotinic receptors and prevents programmed cell
death of parasympathetic neurons. J Neurosci. 29:14847–14854. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jain A, Lam A, Vivanco I, Carey MF and
Reiter RE: Identification of an androgen-dependent enhancer within
the prostate stem cell antigen gene. Mol Endocrinol. 16:2323–2337.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Bahrenberg G, Brauers A, Joost HG and
Jakse G: PSCA expression is regulated by phorbol ester and cell
adhesion in the bladder carcinoma cell line RT112. Cancer Lett.
168:37–43. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chapman EJ, Kelly G and Knowles MA: Genes
involved in differentiation, stem cell renewal, and tumorigenesis
are modulated in telomerase-immortalized human urothelial cells.
Mol Cancer Res. 6:1154–1168. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Saffran DC, Raitano AB, Hubert RS, Witte
ON, Reiter RE and Jakobovits A: Anti-PSCA mAbs inhibit tumor growth
and metastasis formation and prolong the survival of mice bearing
human prostate cancer xenografts. Proc Natl Acad Sci USA.
98:2658–2663. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Gu Z, Yamashiro J, Kono E and Reiter RE:
Anti-prostate stem cell antigen monoclonal antibody 1G8 induces
cell death in vitro and inhibits tumor growth in vivo via a
Fc-independent mechanism. Cancer Res. 65:9495–9500. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Study Group of Millennium Genome Project
for Cancer, . Sakamoto H, Yoshimura K, Saeki N, Katai H, Shimoda T,
Matsuno Y, Saito D, Sugimura H, Tanioka F, et al: Genetic variation
in PSCA is associated with susceptibility to diffuse-type gastric
cancer. Nat Genet. 40:730–740. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
36
|
Yang L, Han Y, Saiz Suarez F and Minden
MD: A tumor suppressor and oncogene: The WT1 story. Leukemia.
21:868–876. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Radtke F and Raj K: The role of Notch in
tumorigenesis: Oncogene or tumour suppressor. Nat Rev Cancer.
3:756–767. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Wu C, Wang G, Yang M, Huang L, Yu D, Tan W
and Lin D: Two genetic variants in prostate stem cell antigen and
gastric cancer susceptibility in a Chinese population. Mol
Carcinog. 48:1131–1138. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Ou J, Li K, Ren H, Bai H, Zeng D and Zhang
C: Association and haplotype analysis of prostate stem cell antigen
with gastric cancer in Tibetans. DNA Cell Biol. 29:319–323. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Matsuo K, Tajima K, Suzuki T, Kawase T,
Watanabe M, Shitara K, Misawa K, Ito S, Sawaki A, Muro K, et al:
Association of prostate stem cell antigen gene polymorphisms with
the risk of stomach cancer in Japanese. Int J Cancer.
125:1961–1964. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Wang M, Bai J, Tan Y, Wang S, Tian Y, Gong
W, Zhou Y, Gao Y, Zhou J and Zhang Z: Genetic variant in PSCA
predicts survival of diffuse-type gastric cancer in a Chinese
population. Int J Cancer. 129:1207–1213. 2011. View Article : Google Scholar : PubMed/NCBI
|