Introduction
Endometrial cancer is the most commonly diagnosed
gynecologic malignancy in the United States. In 2015, approximately
55,000 new cases (7% of total cancer cases) and approximately
10,000 deaths (4% of total cancer deaths) were reported (1), and this same trend was also observed in
China (2). The epidemiology of
endometrial cancer is multifactorial. The most common risk factors
associated with the development of endometrial cancer are unopposed
estrogen exposure and obesity (endometrioid endometrial cancer). A
smaller subset of sporadic cancers is associated with aging and
unique genetic/molecular changes, producing a more aggressive
variant, serous/clear cell type (non-endometrioid endometrial
cancer) (3). For patients with
advanced endometrial cancer, neoadjuvant chemotherapy (NAC) is
recommended. The standard first-line therapy consists of cisplatin
(CDDP) and a doxorubicin (DOX) ± paclitaxel combination and/or
carboplatin plus paclitaxel (4).
Understanding the process of tumor resistance is critical, and
defining which patients are more likely to respond to the
established or novel therapies is our greatest challenge.
Calreticulin (CRT) is an endoplasmic reticulum (ER)
resident protein that is critical for maintaining Ca2+ homeostasis
and glycoprotein folding in the ER. CRT was identified on the cell
surface of apoptotic and necrotic cells and plays a role in
immunogenic cell death (ICD) and other extracellular functions
(5). The ER responds to stress by
activating an adaptive mechanism called the unfolded protein
response (UPR). Three distinct sensors activate the UPR: i)
Inositol-requiring enzyme 1 (IRE1) (an ER kinase and
endoribonuclease); ii) activating transcription factor 6 (ATF6);
and iii) PKR-like endoplasmic reticulum kinase (PERK). The
activation of PERK leads to the attenuation of global protein
translation via the phosphorylation and inhibition of the α subunit
of eIF2α. However, the inhibition of IRE1 and ATF6 does not affect
the expression of ecto-CRT on the plasma membrane (6), suggesting that the PERK pathway is the
key UPR sensor involved in chemotherapy-induced ICD. Activated PERK
is considered a classical precursor for ICD-associated ecto-CRT
expression in vitro and ICD in vivo, but the
activation of PERK alone does not always result in increased
ecto-CRT (7). This suggests that ER
stress is required to induce the ICD-associated translocation of
CRT to the cell surface. The ecto-CRT serves as a potent ‘eat me’
signal for local patrolling dendritic cells (DCs).
CRT is recognized as a protein that alters tumor
growth. High CRT expression, which is likely driven by an ER stress
response, constitutes a positive prognostic biomarker in NSCLC
patients. The local presence of CRT in a constitutively expressed
manner at the surface of transformed epithelial cells might enable
DC-dependent anticancer immunosurveillance (8). On the contrary, a high expression of CRT
and 78-kDa glucose-regulated protein (GRP78) was correlated with a
poor prognosis by a Kaplan-Meier analysis and a log rank analysis
in Chinese esophageal squamous cell carcinoma (9). A higher cellular CRT protein expression
in effusions is associated with a better response to chemotherapy
at diagnosis in high-grade ovarian serous carcinoma (10). Recent studies demonstrate that the
therapeutic outcome following specific chemotherapeutic agents
(e.g., anthracyclines) correlates strongly with the ability of the
drugs to induce a process of ICD in cancer cells. Extensive studies
reveal that chemotherapy-induced ICD occurs via the
exposure/release of CRT, ATP, chemokine (C-X-C motif) ligand 10
(CXCL10), and high mobility group box 1 (HMGB1) (11). Chemotherapy resistance and tumor
escape from the host immunosurveillance system are the main reasons
that anthracycline-based regimens in breast cancer fail, and an
effective chemo-immunosensitizing strategy is lacking.
To date, no studies have demonstrated an association
between CRT overexpression and the overall survival of patients
with endometrial cancer. The expression of CRT in endometrial
cancer with DOX-NAC is still unknown. In the present study, we
performed a retrospective investigation of the association between
CRT, phosphorylated eukaryotic initiation factor 2α (p-eIF2α), and
Ki67 overexpression, clinicopathological parameters, and
progression-free and overall survival in patients with endometrial
cancer. In addition, the relationship between the expression of
CRT, PERK, p-eIF2α, and Ki67 and clinicopathological parameters
were investigated in a cohort of patients with endometrial cancer
receiving DOX-NAC.
Materials and methods
Patients and tissue collection
Our study was approved by the Ethics Committee of
the Fujian Cancer Hospital, which is affiliated with the Fujian
Medical University in China. Informed consent was obtained from
each patient in groups A and B for the use of tissues for the
study. In group A, the samples from the 105 patients with
endometrial cancer who have not received preoperative chemotherapy
or radiotherapy were collected between 2009 and 2010 for IHC
analysis. All patients were followed up until December 2014 or
death. The Group A is retrospective study. No prior radiation
therapy or chemotherapy before surgery was allowed in group A.
In group B, 66 patients with advanced endometrial
cancer were collected between 2012 and 2015 for IHC analysis. Group
B is prospective study. In group B, the NAC was DOX 50–60
mg/m2 D1 every 3 weeks for 2 cycles. Patients were
classified as having DOX sensitive or resistant tumors to the
chemotherapy they received in the first cycle if they achieved ≥25
or <25% reduction in tumor dimensions by MRI, respectively
(12). All the patients after DOX-NAC
were operated in our hospital.
All the patients in Group A and B were screened for
eligibility after surgery consisting of hysterectomy (total or
modified radical or radical), bilateral salpingo-oophorectomy,
pelvic lymphadenectomy and/or para-aortic lymphadenectomy, and
adequate surgical staging no more than eight weeks prior to the
start of radiation therapy in both groups. All patients were
required to have normal hematological, liver, and renal function
with laboratory parameters being within the normal range (including
a creatinine clearance ≥40 ml/min, leucocytes ≥4.0×109/l, platelets
≥100×109/l and hemoglobin ≥10 g/dl). Patients suffering from a
secondary malignancy, serious concomitant systemic disorders or
psychiatric disease were excluded from the study.
In group A, we focused on the relationship between
the expression of CRT, p-eIF2a, Ki67 and the clinicopathological
features and survival of endometrial cancer patients. In group B,
we focused on the relationship of the expression of CRT, p-eIF2a,
Ki67 and the sensitivity of endometrial cancer to DOX.
Fresh endometrial cancer tissue samples of
twenty-four patients from pre- and post-treatment of DOX-NAC were
collected for the western blot analysis. Twelve of the samples were
DOX-resistant tissues and another 12 were DOX-sensitive.
Study endpoints
The primary endpoint of the protocol was
progression-free survival (PFS). PFS was defined as the time from
the date of enrollment to the date of disease progression or death
from any cause. The secondary endpoints included local-regional
failure, distant failure, and overall survival (OS).
Reagents
Primary antibodies against CRT (MAB3898), p-eIF2a
(AF705) and PERK (AF3999) were purchased from R&D systems.
Primary antibodies against Ki67 (ab15580), and β-Actin (ab8226)
were purchased from Abcam (Cambridge, UK). Secondary horseradish
peroxidase (HRP)-labeled anti-mouse or anti-rabbit antibodies were
purchased from Santa Cruz Biotechnology, Inc. (Dallas, TX,
USA).
Immunohistochemistry
IHC assays were performed on formalin-fixed and
paraffinembedded sections. Sections (thickness=5 µm) were cut and
deparaffinized in xylene and rehydrated a graded series of
alcohols. The avidin-biotin complex method was used throughout the
whole IHC procedure. Antigen retrieval was performed using a
steamer for 20 min in a 1xethylenediaminetetraacetic acid buffer.
Endogenous peroxidase activity was blocked by 3% hydrogen peroxide
in methanol for 20 min. A 5% solution of nonfat milk was used to
block the reaction (1 h). The slides were then incubated with
rabbit polyclonal antibodies directed against human CRT (1:50
dilution), p-eIF2α (1:50 dilution), or Ki67 (1:100 dilution) for 1
h at room temperature. Then, the slides were reacted with the
MaxVision™ HRP-polymer anti-rabbit or anti-mouse secondary antibody
and was counterstained with Mayer's hematoxylin following staining
with diaminobenzidine. The mean value of the densitometric units of
five visual fields was used to rate the intensity of the expression
of CRT, p-eIF2α, and Ki67. The tumor cells with membranous or
cytoplasmic staining were considered positive for expression of CRT
and p-eIF2α. The tumor cells with nuclear staining was considered
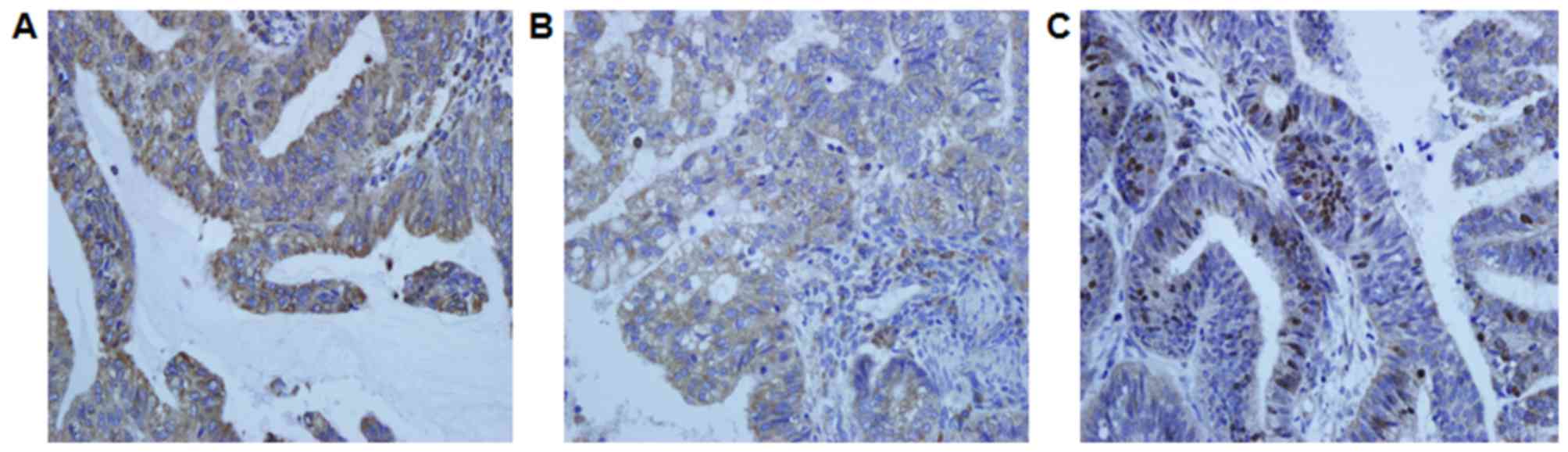
positive for expression of Ki67 (Fig.
1). As the negative control of CRT, p-eIF2α, and Ki67,
distilled water were used instead of primary antibody. The digital
images of five representative visual fields from each slide that
were positive for CRT, p-eIF2α, and Ki67 were analyzed using
Image-Pro Plus 6.0 software (Media Cybernetics, Inc., Bethesda, MD,
USA). As positive controls, colon cancer for CRT and breast cancer
for p-eIF2a were used, respectively. The IHC-stained tissue
sections were reviewed and scored separately by two pathologists
who were blinded to the clinical parameters. The staining intensity
was scored on a four-point scale that ranged from (−) to (+++) and
was read as negative (−), <10%; weak (+), 10–25%; medium (++),
26–50%; or strong (+++), ≥50%. The percentage of positive cells was
calculated by counting the number of positively stained cells
showing immunoreactivity on the cell membranes and/or cytoplasm in
10 representative microscopic fields.
Western blot analysis
The samples were lysed with a
radioimmunoprecipitation assay buffer containing 100-M
phenylmethylsulfonyl fluoride, and the protein concentrations were
determined using a bicinchoninic acid kit (Pierce; Thermo Fisher
Scientific, Inc., Waltham, MA, USA). Equal amounts of total protein
were separated on 12% SDS-PAGE gels and were then transferred to
PVDF membranes. The membranes were immunoblotted with the
appropriate primary antibody that was diluted in tris-buffered
saline containing 0.05% Tween-20 and 5% nonfat dry milk at room
temperature for 2 h. After extensive washing, the membranes were
incubated with an HRP-labeled antibody for 1 h at room temperature.
Protein bands were revealed by ECL detection. CT26 cells was used
as positive control of CRT and p-eIF2a (6).
Statistical analyses
The statistical analyses were performed using SPSS
software (version 17.0; SPSS, Inc., Chicago, IL, USA). Correlations
between the expression levels were studied using the spearman
coefficient. The chi-square test was used to compare between the
groups. Survival curves were calculated according to the
Kaplan-Meier method, and the log-rank test was used to analyze the
differences between the curves. The relative influence of CRT,
p-eIF2α, and Ki67 on PFS and OS was examined using a multivariate
analysis according to the nonparametric hazards model of Cox.
Significance was set at P<0.05. The data from the Western blot
analysis was expressed as the mean ± standard deviations from at
least three independent experiments. Statistical significance was
determined using a Student's t-test and a one-way analysis of
variance. P<0.05 was considered to indicate a statistically
significant difference.
Results
Immunoreactivity of CRT, p-eIF2α, and
Ki67 in endometrial cancer
Group A: Tissue specimens from 105 endometrial
cancer patients were examined for the expression of CRT, p-eIF2α,
and Ki67 using IHC. CRT and p-eIF2α were noted in the cytoplasm and
cell membrane of the tumor cells, and Ki67 was mainly observed in
the nucleus (Fig. 1). CRT, p-eIF2α,
and Ki67 were highly expressed in 78 (74.3%), 62 (59.0%), and 36 of
the 105 cases (34.3%), respectively (Table I). There was no significant
relationship between the expression of CRT and p-eIF2α.
 | Table I.Relationship between CRT, p-eIF2a,
Ki67 expression and clinicopathological features of endometrial
cancer. |
Table I.
Relationship between CRT, p-eIF2a,
Ki67 expression and clinicopathological features of endometrial
cancer.
| Clinical
features | n | CRT (−/+) | CRT (++-+++) | P-value | p-eIF2a (−/+) | p-eIF2a (++-+++) | P | Ki67 (−/+) | Ki67 (++-+++) | P-value |
|---|
|
| 105 | 27 | 78 |
| 43 | 62 |
| 69 | 36 |
|
| Age |
|
|
| 0.368 |
|
| 0.836 |
|
| 0.462 |
| ≤45 | 28 | 8 | 20 |
| 11 | 17 |
| 20 | 8 |
|
|
>45 | 77 | 19 | 58 |
| 32 | 45 |
| 49 | 28 |
|
| Clinical stage
(FIGO) |
|
|
|
0.001a |
|
| 0.877 |
|
|
0.010a |
| I | 29 | 4 | 25 |
| 11 | 18 |
| 22 | 7 |
|
| II | 35 | 6 | 29 |
| 15 | 20 |
| 26 | 9 |
|
|
III | 25 | 7 | 18 |
| 11 | 14 |
| 15 | 10 |
|
| IV | 16 | 10 | 6 |
| 6 | 10 |
| 6 | 10 |
|
| Histology |
|
|
|
<0.001a |
|
| 0.699 |
|
|
0.019a |
|
Non-endometrioid | 31 | 13 | 18 |
| 12 | 19 |
| 16 | 15 |
|
|
Endometrioid | 74 | 14 | 60 |
| 31 | 43 |
| 53 | 21 |
|
| Lymphnode
metastasis |
|
|
| 0.056 |
|
| 0.496 |
|
| 0.269 |
|
Positive | 28 | 11 | 17 |
| 13 | 15 |
| 16 | 12 |
|
|
Negative | 77 | 16 | 61 |
| 30 | 47 |
| 53 | 24 |
|
|
Differentiation |
|
|
|
0.001a |
|
| 0.689 |
|
|
0.018a |
| G1 | 28 | 3 | 25 |
| 13 | 15 |
| 22 | 6 |
|
| G2 | 40 | 7 | 33 |
| 15 | 25 |
| 28 | 12 |
|
| G3 | 37 | 17 | 20 |
| 15 | 22 |
| 19 | 18 |
|
| Muscle
invasion |
|
|
| 0.404 |
|
| 0.728 |
|
| 0.306 |
|
>1/2 | 54 | 12 | 42 |
| 23 | 31 |
| 38 | 16 |
|
|
≤1/2 | 51 | 15 | 36 |
| 20 | 31 |
| 31 | 20 |
|
| CRT |
|
|
|
|
|
|
|
|
| 0.201 |
|
(−/+) | 27 | / | / |
| / | / |
| 15 | 12 |
|
|
(++/+++) | 78 | / | / |
| / | / |
| 54 | 24 |
|
| p-eIF-2a |
|
|
| 0.672 |
|
| / |
|
| 0.759 |
|
(−/+) | 43 | 12 | 31 |
| / | / |
| 29 | 14 |
|
|
(++/+++) | 62 | 15 | 47 |
| / | / |
| 40 | 22 |
|
Group B: Tissue specimens from 66 advanced
endometrial cancer patients receiving DOX-NAC were examined by IHC
for the expression of CRT, p-eIF2α, and Ki67. CRT, p-eIF2α, and
Ki67 were highly expressed in 36 (54.5%), 66 (48.5%), and in 29 of
the 66 cases (39.4%), respectively (Table II), before NAC. There was a
significant difference in the CRT (P=0.001), p-eIF2α (P=0.029),
Ki67 (P=0.005) expressions between the pre-NAC and post-NAC. CRT,
p-eIF2α, and Ki67 were highly expressed in 48 (72.7%), 43 (65.1%),
and in 24 of the 66 cases (36.4%), respectively (Table III), after NAC.
 | Table II.Relationship between CRT, eIF-2a,
Ki67 expression and clinicopathological features of endometrial
carcinoma patients with NAC. |
Table II.
Relationship between CRT, eIF-2a,
Ki67 expression and clinicopathological features of endometrial
carcinoma patients with NAC.
| Clinical
features | n | pre-NAC CRT
(−/+) | pre-NAC CRT
(++-+++) | P-value | pre-NAC p-eIF2a
(−/+) | pre-NAC p-eIF2a
(++-+++) | P-value | pre-NAC Ki67
(−/+) | pre-NAC ki67
(++-+++) | P-value |
|---|
|
| 66 | 30 | 36 |
| 34 | 32 |
| 37 | 29 |
|
| NAC |
|
|
|
<0.001a |
|
| 0.058 |
|
|
0.019a |
|
Sensitivity | 40 | 11 | 29 |
| 17 | 23 |
| 27 | 13 |
|
|
Resistance | 26 | 19 | 7 |
| 17 | 9 |
| 10 | 16 |
|
| Histology |
|
|
|
0.001a |
|
| 0.163 |
|
|
0.043a |
|
Non-endometrioid | 17 | 14 | 3 |
| 11 | 6 |
| 6 | 11 |
|
|
Endometrioid | 49 | 16 | 33 |
| 23 | 26 |
| 31 | 18 |
|
| Lymphnode
metastasis |
|
|
| 0.418 |
|
| 0.281 |
|
| 0.492 |
|
Positive | 24 | 10 | 14 |
| 14 | 10 |
| 14 | 10 |
|
|
Negative | 42 | 20 | 22 |
| 20 | 22 |
| 23 | 19 |
|
|
Differentiation |
|
|
| 0.171 |
|
| 0.424 |
|
| 0.101 |
| G1 | 25 | 9 | 16 |
| 12 | 13 |
| 17 | 8 |
|
| G2,
G3 | 41 | 21 | 20 |
| 22 | 19 |
| 20 | 21 |
|
| Muscle
invasion |
|
|
| 0.187 |
|
| 0.23 |
|
| 0.161 |
|
>1/2 | 33 | 12 | 21 |
| 15 | 18 |
| 21 | 12 |
|
|
≤1/2 | 33 | 18 | 15 |
| 19 | 14 |
| 16 | 17 |
|
| pre-NAC
p-eIF2a |
|
|
| 0.491 |
|
| / |
|
| 0.238 |
|
(−/+) | 34 | 16 | 18 |
| / | / |
| 21 | 13 |
|
|
(++/+++) | 32 | 14 | 18 |
| / | / |
| 16 | 16 |
|
| post-NAC CRT |
|
|
|
0.001a |
|
| / |
|
| / |
|
(−/+) | 20 | 16 | 4 |
| / | / |
| / | / |
|
|
(++/+++) | 46 | 14 | 32 |
| / | / |
| / | / |
|
| post-NAC
p-eIF2a |
|
|
| / |
|
|
0.029a |
|
| / |
|
(−/+) | 23 | / | / |
| 16 | 7 |
| / | / |
|
|
(++/+++) | 43 | / | / |
| 18 | 25 |
| / | / |
|
| post-NAC Ki67 |
|
|
| / |
|
| / |
|
|
0.005a |
|
(−/+) | 42 | / | / |
| / | / |
| 29 | 13 |
|
|
(++/+++) | 24 | / | / |
| / | / |
| 8 | 16 |
|
 | Table III.Association between CRT, eIF-2a, Ki67
expression and clinicopathological features of advanced endometrial
cancer patients after NAC. |
Table III.
Association between CRT, eIF-2a, Ki67
expression and clinicopathological features of advanced endometrial
cancer patients after NAC.
| Clinical
features | n | post-NAC CRT
(−/+) | post-NAC CRT
(++-+++) | P-value | post-NAC p-eIF2a
(−/+) | post-NAC p-eIF2a
(++-+++) | P-value | post-NAC Ki67
(−/+) | post-NAC ki67
(++-+++) | P-value |
|---|
|
| 66 | 18 | 48 |
| 23 | 43 |
| 42 | 24 |
|
| NAC |
|
|
|
0.007a |
|
|
<0.001a |
|
|
<0.001a |
|
Sense | 40 | 6 | 34 |
| 7 | 33 |
| 34 | 6 |
|
|
Resistance | 26 | 12 | 14 |
| 16 | 10 |
| 8 | 18 |
|
| Histology |
|
|
| 0.287 |
|
| 0.362 |
|
|
0.027a |
|
Non-endometrioid | 17 | 6 | 11 |
| 7 | 10 |
| 7 | 10 |
|
|
Endometrioid | 49 | 12 | 37 |
| 16 | 33 |
| 35 | 14 |
|
| Lymphnode
metastasis |
|
|
| 0.119 |
|
| 0.532 |
|
| 0.117 |
|
Positive | 24 | 4 | 20 |
| 8 | 16 |
| 18 | 6 |
|
|
Negative | 42 | 14 | 28 |
| 15 | 27 |
| 24 | 18 |
|
|
Differentiation |
|
|
| 0.432 |
|
| 0.261 |
|
| 0.38 |
| G1 | 25 | 6 | 19 |
| 7 | 18 |
| 17 | 8 |
|
| G2,
G3 | 41 | 12 | 29 |
| 16 | 25 |
| 25 | 16 |
|
| Muscle
invasion |
|
|
| 0.391 |
|
| 0.5 |
|
| 0.222 |
|
>1/2 | 33 | 8 | 25 |
| 12 | 21 |
| 23 | 10 |
|
|
≤1/2 | 33 | 10 | 23 |
| 11 | 22 |
| 19 | 14 |
|
Correlation to age, FIGO stage,
histology, lymph node metastasis, differentiation, and muscle
invasion
Group A: The correlations between CRT, p-eIF2α, and
Ki67 protein content and various clinical factors are listed in
Table I. There was a significant
association between CRT and Ki67 and FIGO stage
(PCRT=0.001; Pki67=0.010), histology
(PCRT=0.000; Pki67=0.019), and
differentiation (PCRT=0.001; Pki67=0.018). No
associations were noted between the intense immunostaining for CRT
and Ki67 and age, lymph node metastasis, and muscle invasion.
Group B: The correlations between CRT, p-eIF2α, and
Ki67 protein content and various clinical factors before NAC are
listed in Table II. There was a
significant association between CRT and Ki67 and NAC
(PCRT=0.000; Pki67=0.019) and histology
(PCRT=0.001; Pki67=0.043) pre-NAC. No
associations were noted between the intense immunostaining for CRT
and Ki67 and differentiation, lymph node metastasis, and muscle
invasion. There was no significant association between p-eIF2α and
histology, differentiation, NAC, lymph node metastasis, and muscle
invasion in the pre-NAC group.
The correlations between CRT, p-eIF2α, and Ki67
protein content and various clinical factors after NAC are listed
in Table III. There was a
significant association between CRT, p-eIF2α, Ki67 and NAC
(PCRT=0.007; Pp-eIF2a=0.000,
Pki67=0.000) and histology (Pki67=0.027)
post-NAC. No associations were noted between the intense
immunostaining for CRT, p-eIF2α, and Ki67 and differentiation,
lymph node metastasis, muscle invasion, and histology post-NAC.
Analysis of the correlation between
the expressions of CRT, p-eIF2α, and Ki67 and therapy outcome in
group A
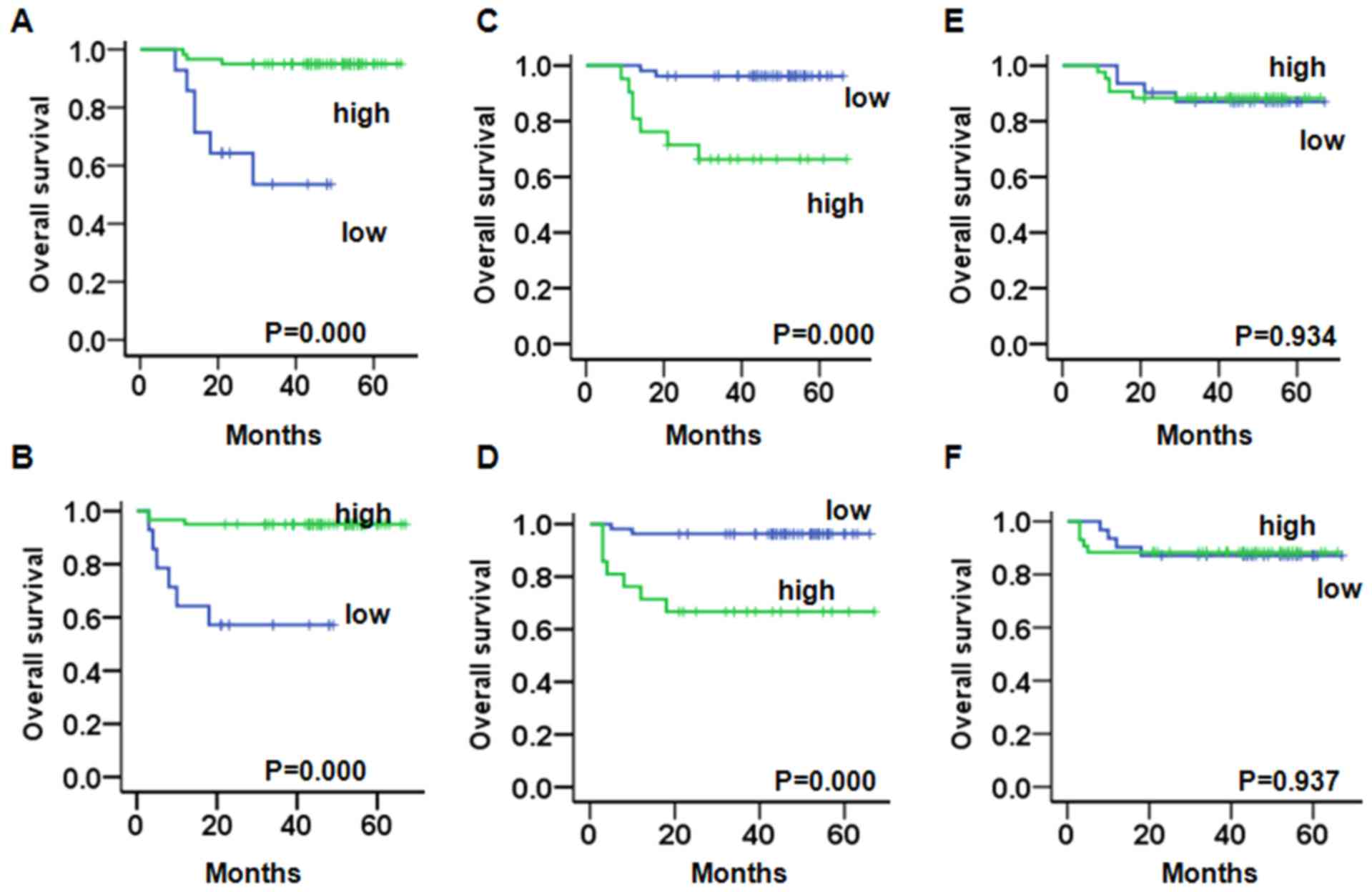
We evaluated the prognostic value of CRT, p-eIF2α,
and Ki67 on PFS and OS in endometrioid endometrial cancer and
non-endometrioid endometrial cancer patients. A Kaplan-Meier
analysis demonstrated that in endometrioid endometrial cancer
patients with a weak expression of CRT had a significantly worse OS
(PCRT=0.000) (Fig. 2A) and
PFS (PCRT=0.000) (Fig. 2B)
compared to patients with a strong expression. Patients with a
strong expression of Ki67 had a significantly worse OS
(Pki67=0.000) (Fig. 2C)
and PFS compared to patients with a weak expression
(Pki67=0.000) (Fig. 2D).
There was no significant change between the weak or strong
expression of p-eIF2α and the OS (Fig.
2E) and PFS (Fig. 2F).
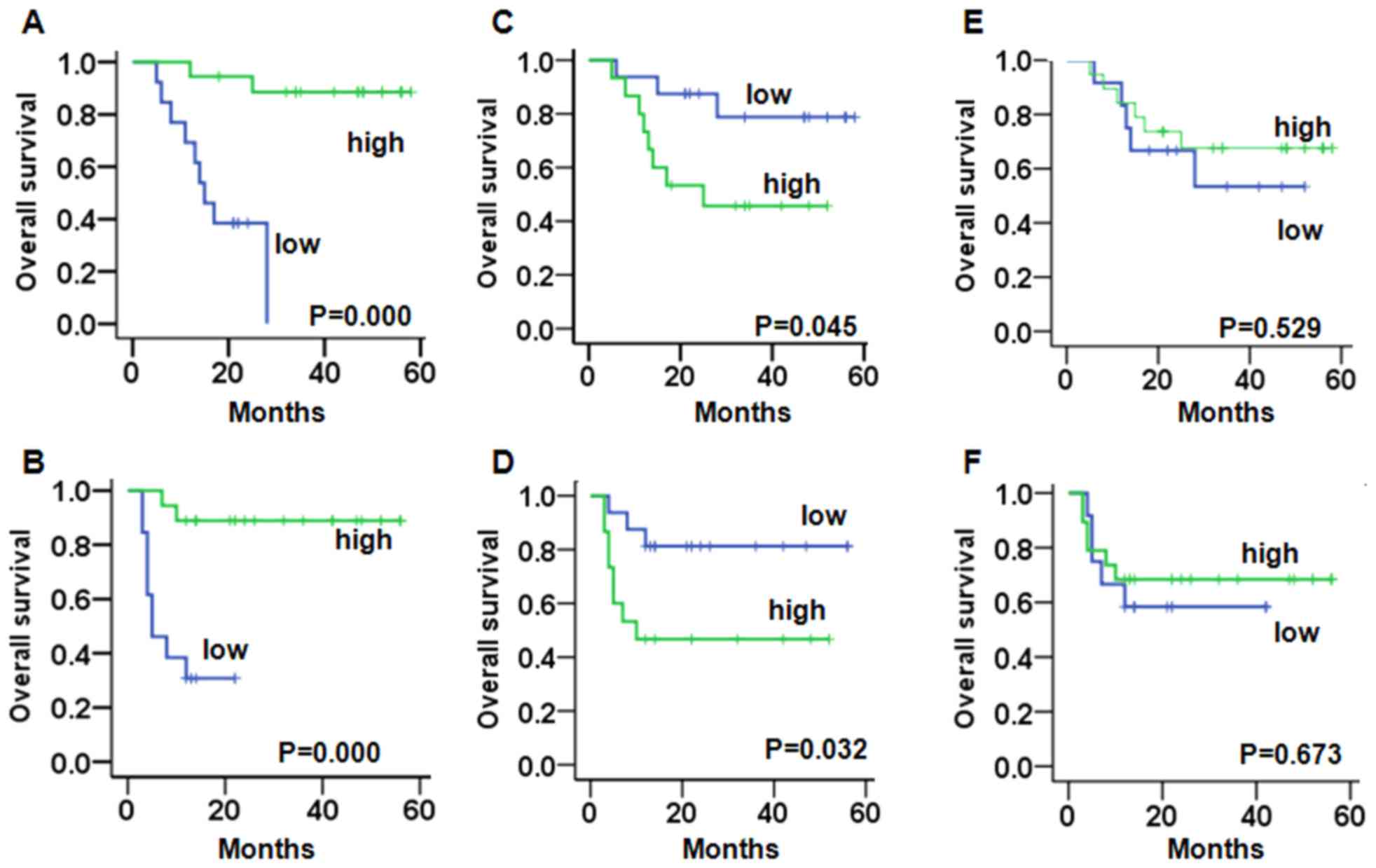
A Kaplan-Meier analysis demonstrated that in
non-endometrioid endometrial cancer patients with a weak expression
of CRT had a significantly worse OS (PCRT=0.000)
(Fig. 3A) and PFS
(PCRT=0.000) (Fig. 3B)
compared to patients with a strong expression. Patients with a
strong expression of Ki67 had a significantly worse OS
(Pki67=0.045) (Fig. 3C)
and PFS (Pki67=0.032) compared to patients with a weak
expression (Fig. 3D). There was no
significant change between the weak or strong expression of p-eIF2α
and the OS (Fig. 3E) and PFS
(Fig. 3F).
Multivariate analysis of prognosis
variables in patients with endometrioid endometrial cancer in group
A
In the multivariate OS analysis, CRT, p-eIF2α, Ki67,
stage, muscle invasion, and lymph node metastases were entered into
the Cox regression analysis. CRT expression (hazard ratio (HR),
0.147; P=0.012; 95% confidence interval (CI), 0.033–0.661) was an
independently significant prognostic factor. Ki67 expression
(hazard ratio (HR), 7.559; P=0.020; 95% confidence interval (CI),
1.370–41.709) was an independently significant prognostic factor
(Table IV). In the multivariate PFS
analysis, CRT expression (hazard ratio (HR), 0.164; P=0.018; 95%
confidence interval (CI), 0.037–0.732) was an independent
significant prognostic factor. Ki67 expression (hazard ratio (HR),
7.077; P=0.024; 95% confidence interval (CI), 1.293–38.725) was an
independently significant prognostic factor (Table IV).
 | Table IV.Prognostic factors by multivariate
analysis for endometrioid endometrial cancer patients. |
Table IV.
Prognostic factors by multivariate
analysis for endometrioid endometrial cancer patients.
| A, PFS |
|---|
|
|---|
| Parameters | Hazard ratio | P-value | 95% CI |
|---|
| Lymph node
metastases | 0.562 | 0.628 | 0.055–5.785 |
|
Positive |
|
|
|
|
Negative |
|
|
|
| Stage | 1.036 | 0.957 | 0.286–3.750 |
|
I/II |
|
|
|
|
III/IV |
|
|
|
| Muscle
invasion | 0.161 | 0.128 | 0.015–1.695 |
|
>1/2 |
|
|
|
|
≤1/2 |
|
|
|
| CRT | 0.164 |
0.018a | 0.037–0.732 |
| p-eIF-2a | 1.219 | 0.779 | 0.305–4.865 |
| Ki67 | 7.077 |
0.024a | 1.293–38.725 |
|
| B, OS |
|
| Parameters | Hazard ratio | P-value | 95% CI |
|
| Lymph node
metastases | 0.600 | 0.666 | 0.059–6.118 |
|
Positive |
|
|
|
|
Negative |
|
|
|
| Stage | 1.003 | 0.997 | 0.274–3.672 |
|
I/II |
|
|
|
|
III/IV |
|
|
|
| Muscle
invasion | 0.146 | 0.118 | 0.013–1.634 |
|
>1/2 |
|
|
|
|
≤1/2 |
|
|
|
| CRT | 0.147 | 0.012a | 0.033–0.661 |
| p-eIF-2a | 1.365 | 0.662 | 0.338–5.519 |
| Ki67 | 7.559 | 0.020a | 1.370–41.709 |
Multivariate analysis of prognosis
variables in patients with non-endometrioid endometrial cancer in
group A
In the multivariate OS analysis, CRT, p-eIF2α, Ki67,
stage, muscle invasion, and lymph node metastases were entered into
the Cox regression analysis. Stage (hazard ratio (HR), 8.930;
P=0.027; 95% confidence interval (CI), 1.284–62.111) was an
independently significant prognostic factor. Ki67 expression
(hazard ratio (HR), 10.011; P=0.013; 95% confidence interval (CI),
1.633–61.357) was an independently significant prognostic factor
(Table V). In the multivariate PFS
analysis, CRT expression (hazard ratio (HR), 0.068; P=0.038; 95%
confidence interval (CI), 0.005–0.858) was an independent
significant prognostic factor. Ki67 expression (hazard ratio (HR),
21.326; P=0.009; 95% confidence interval (CI), 2.120–214.573) was
an independently significant prognostic factor (Table V).
 | Table V.Prognostic factors by multivariate
analysis for non-endometrioid endometrial cancer patients. |
Table V.
Prognostic factors by multivariate
analysis for non-endometrioid endometrial cancer patients.
| A, PFS |
|---|
|
|---|
| Parameters | Hazard ratio | P-value | 95% CI |
|---|
| Lymph node
metastases | 2.624 | 0.302 | 0.420–16.408 |
|
Positive |
|
|
|
|
Negative |
|
|
|
| Stage | 3.006 | 0.158 | 0.652–13.868 |
|
I/II |
|
|
|
|
III/IV |
|
|
|
| Muscle
invasion | 1.002 | 0.998 | 0.264–3.807 |
|
>1/2 |
|
|
|
|
≤1/2 |
|
|
|
| CRT | 0.068 |
0.038a | 0.005–0.858 |
| p-eIF-2a | 1.712 | 0.483 | 0.381–7.703 |
| Ki67 | 21.326 |
0.009a | 2.120–214.573 |
|
| B, OS |
|
| Parameters | Hazard ratio | P-value | 95% CI |
|
| Lymph node
metastases | 1.640 | 0.602 | 0.256–10.488 |
|
Positive |
|
|
|
|
Negative |
|
|
|
| Stage | 8.930 |
0.027a | 1.284–62.111 |
|
I/II |
|
|
|
|
III/IV |
|
|
|
| Muscle
invasion | 1.043 | 0.953 | 0.251–4.346 |
|
>1/2 |
|
|
|
|
≤1/2 |
|
|
|
| CRT | 0.080 | 0.050 | 0.006–1.005 |
| p-eIF-2a | 1.241 | 0.782 | 0.270–5.697 |
| Ki67 | 10.011 |
0.013a | 1.633–61.357 |
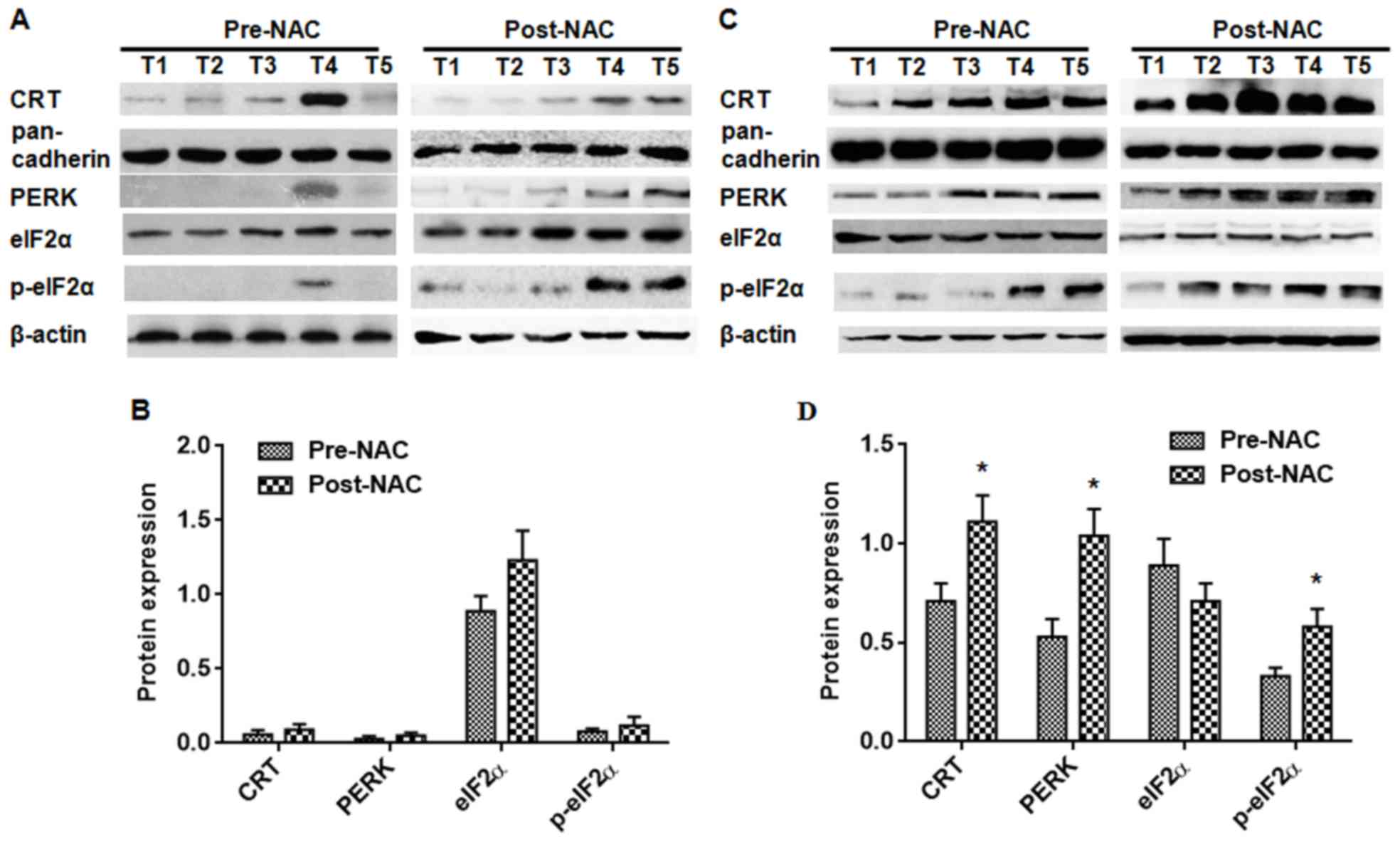
The expression of CRT, PERK, eIF2α,
and p-eIF2α in advanced endometrial cancer tissues by western
blot
To investigate the potential role of CRT in the
tumorigenesis of endometrial cancer, a Western blot was performed
on tissue from endometrial cancer patients receiving DOX-NAC. The
CRT, PERK, and p-eIF2α protein content was not significantly
correlated with pre-NAC and post-NAC in DOX-resistant endometrial
cancer (Fig. 4A and B). In the
DOX-sensitive endometrial cancer patient tissues, the CRT, PERK,
and p-eIF2α protein content was lowly expressed in the pre-NAC
group compared with the post-NAC group (Fig. 4C and D) (P<0.05). There was no
significant difference on the expression of eIF2α in both the
DOX-sensitive group and the DOX-resistant group (Fig. 4).
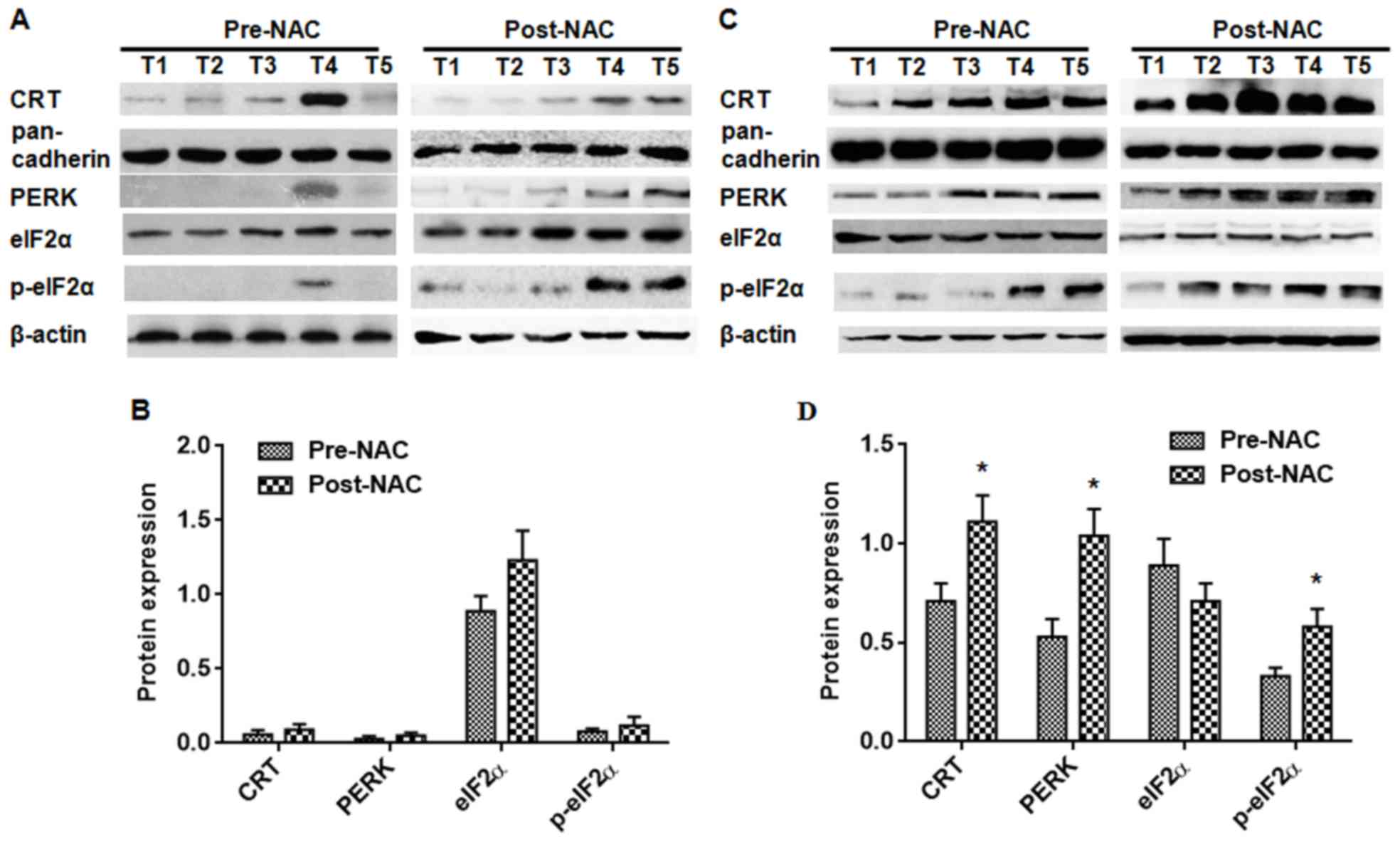 | Figure 4.Assessment of CRT, PERK, eIF2α, and
p-eIF2α protein content by Western blot analysis. The protein
content of CRT, PERK, eIF2α, and p-eIF2α in 12 pairs of
DOX-resistant endometrial cancer patients and DOX-sensitive
endometrial cancer patients was assessed. In the DOX-resistant
endometrial cancer samples, the CRT, PERK, eIF2α, and p-eIF2α
protein content was not significantly different between the pre-NAC
and post-NAC. (A) In the DOX-sensitive endometrial cancer samples,
the CRT, PERK, and p-eIF2α protein content was significantly
increased in the post-NAC group compared with the pre-NAC group.
(C) There was not a significant change in the eIF2α protein content
in the DOX-sensitive endometrial cancer samples. The expression
levels were normalized to the actin/pan-cadherin expression values.
(B and D) The data are expressed as the means ± standard
deviations, which were calculated from three parallel experiments.
*P<0.05. CRT; calreticulin; PERK, PKR-like endoplasmic reticulum
kinase. |
Discussion
CRT has been evaluated as a potential biomarker in
several types of cancer, including neuroblastoma (13), bladder (14), gastric (15), breast cancer (16), and acute myeloid leukemia (17). To our knowledge, the expression of CRT
is not reported in endometrial cancer, and the prognostic impact of
CRT levels has not been studied. Here, we assessed the prognostic
value of CRT expression in two independent retrospective cohorts of
patients with endometrial cancer. One cohort was treated by primary
surgery without DOX-NAC (n=105), and the second cohort was treated
with DOX-NAC followed by surgery (n=66). In this retrospective
study, we evaluated the expression of CRT, PERK, eIF2α, p-eIF2α,
and Ki67 in endometrial cancer and examined the prognostic
implications. The overexpression of CRT was associated with the
survival of patients with endometrial cancer, and a low expression
of CRT was associated with DOX-resistance in endometrial
cancer.
In the primary surgery, CRT expression correlated
with the FIGO stage, the histology, and the differentiation of
endometrial cancer. The Cox multivariate regression analyses
confirmed that CRT and Ki67 expression were independent prognostic
factors in endometrioid endometrial cancer. High CRT levels were
associated with a longer survival both in the endometrioid
endometrial cancer group examined. Neuroblastoma is the most common
malignancy in infants, and a positive CRT staining was correlated
with a better prognosis and a higher patient survival (13). In addition, a stronger CRT expression
and a higher infiltration of CD3+ and CD45RO+ cells in colon cancer
were associated with a higher 5-year survival rate (18). Kageyama et al observed higher
amounts of CRT in the urine samples of patients with bladder cancer
and proposed CRT as a biomarker in bladder cancer (14). CRT protein expression is correlated
with tumor size and metastatic potential in breast cancer (19), suggesting that CRT levels might only
predict patient survival in certain cancer types.
Previous studies demonstrate that the cell surface
expression of CRT serves as an ‘eat me’ signal (20) and induces immunogenic tumor cell death
(21–23). Activated PERK is a classical precursor
for ICD-associated CRT expression. We have demonstrated that in
vitro DOX induced the death of tumor cells by ER stress
(p-eIF2a, PERK)-mediated CRT expression in EC cells. Induction of
ER stress by p-eIF2a in drug-resistant EC cells up-regulated the
membrane expression of CRT (in press). The increased expression of
ATF6, GRP78, and CHOP/GADD153 in estrogen-related endometrioid
carcinomas tissues indicates that ER stress is activated in
endometrial cancer (24). PFS and OS
are not associated with the expression of PERK, EGFR, the estrogen
receptor, and the progesterone receptor in primary and recurrent
endometrial cancer (25).
To date, the expression of p-eIF2α in endometrial
cancer tissues or cell lines has not been reported. The
relationship between the expression of p-eIF2α and OS/PFS in
endometrial cancer patients is still unknown. Our data revealed
that the expression of p-eIF2α was not associated with the
clinicopathological features of endometrial carcinoma patients
treated by primary surgery. ER stress induced by realgar quantum
dots was confirmed by the increased expression of GADD153 and GRP78
at both the mRNA and protein levels and led to endometrial
carcinoma cell apoptosis and necrosis (26). However, whether the ER stress
stimulates and processes the ICD-associated CRT expression in
endometrial cancer remains to be investigated.
Historically, chemotherapy is thought to induce
cancer cell death in an immunogenically silent manner. However,
recent studies demonstrate that the therapeutic outcomes with
specific chemotherapeutic agents (e.g., anthracyclines) correlate
strongly with their ability to induce ICD in cancer cells. After
chemotherapy with doxorubin, CRT is translocated from the ER to the
cytosol and then, subsequently to the cell surface. Interestingly,
when immunocopetent mice were injected with cancer cells and
treated ex vivo with anthracyclines recombinant CRT was
successfully used as an anti-tumor vaccination (27). Moreover, DOX failed to promote the
translocation of CRT and the phagocytosis of the drug-resistant
HT29-dx and HT29 iNOS-cells, which resulted in both a
chemoresistant and an immunoresistant phenotype (28). In our study, among the patients in
group B, there was a significant increase in the expression of CRT
in the DOX-sensitive endometrial cancer patients both in pre-NAC
and post-NAC by IHC. In addition, the protein expressions of CRT,
PERK, and p-eIF2α were significantly increased after DOX-NAC in the
DOX-sensitive patient samples. There were no significant difference
in the protein expression of CRT, PERK, and p-eIF2α after DOX-NAC
in the DOX-resistant patient samples. This suggests that DOX-NAC in
advanced endometrial cancer might be associated with a strong
constitutive ER stress response that culminates in CRT expression
and exposure, facilitating anticancer immunosurveillance.
In conclusion, a high CRT expression, which is
likely driven by an ER stress response, constitutes a positive
prognostic biomarker in endometrial cancer. CRT expression is
associated with the sensitivity of DOX chemotherapy. Low CRT
expression in endometrial cancer might represent a new mechanism of
immune escape, and monitoring the increasing expression level of
CRT on the membrane might indicate new therapeutic strategies for
DOX-resistant endometrial cancer.
Acknowledgements
This study was supported in part by Grants-in-Aid
for Scientific Research (81302280) from the National Natural
Science Foundation of China (from December 2013 to December
2016).
References
|
1
|
American Cancer Society, . Cancer Facts
& Figures 2015. American Cancer Society; Atlanta, GA: 2015
|
|
2
|
Wei KR, Chen WQ, Zhang SW, Zheng RS, Wang
YN and Liang ZH: Epidemiology of uterine corpus cancer in some
cancer registering areas of China from 2003–2007. Zhonghua Fu Chan
Ke Za Zhi. 47:445–451. 2012.(In Chinese). PubMed/NCBI
|
|
3
|
Schouten LJ, Goldbohm RA and van den
Brandt PA: Anthropometry, physical activity, and endometrial cancer
risk: Results from the Netherlands cohort study. Int J Gynecol
Cancer. 16 Suppl 2:S4922006. View Article : Google Scholar
|
|
4
|
Thigpen JT, Brady MF, Homesley HD,
Malfetano J, DuBeshter B, Burger RA and Liao S: Phase III trial of
doxorubicin with or without cisplatin in advanced endometrial
carcinoma: A gynecologic oncology group study. J Clin Oncol.
22:3902–3908. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Eggleton P, Bremer E, Dudek E and Michalak
M: Calreticulin, a therapeutic target? Expert Opin Ther Targets.
20:1137–1147. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Panaretakis T, Kepp O, Brockmeier U,
Tesniere A, Bjorklund AC, Chapman DC, Durchschlag M, Joza N,
Pierron G, van Endert P, et al: Mechanisms of pre-apoptotic
calreticulin exposure in immunogenic cell death. EMBO J.
28:578–590. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Garg AD, Krysko DV, Verfaillie T,
Kaczmarek A, Ferreira GB, Marysael T, Rubio N, Firczuk M, Mathieu
C, Roebroek AJ, et al: A novel pathway combining calreticulin
exposure and ATP secretion in immunogenic cancer cell death. EMBO
J. 31:1062–1079. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fucikova J, Becht E, Iribarren K, Goc J,
Remark R, Damotte D, Alifano M, Devi P, Biton J, Germain C, et al:
Calreticulin expression in human non-small cell lung cancers
correlates with increased accumulation of antitumor immune cells
and favorable prognosis. Cancer Res. 76:1746–1756. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Du XL, Hu H, Lin DC, Xia SH, Shen XM,
Zhang Y, Luo ML, Feng YB, Cai Y, Xu X, et al: Proteomic profiling
of proteins dysregulated in Chinese esophageal squamous cell
carcinoma. J Mol Med (Berl). 85:863–875. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Vaksman O, Davidson B, Tropé C and Reich
R: Calreticulin expression is reduced in high-grade ovarian serous
carcinoma effusions compared with primary tumors and solid
metastases. Hum Pathol. 44:2677–2683. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gebremeskel S and Johnston B: Concepts and
mechanisms underlying chemotherapy induced immunogenic cell death:
Impact on clinical studies and considerations for combined
therapies. Oncotarget. 6:41600–41619. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang T, Srivastava S, Hartman M, Buhari
SA, Chan CW, Iau P, Khin LW, Wong A, Tan SH, Goh BC and Lee SC:
High expression of intratumoral stromal proteins is associated with
chemotherapy resistance in breast cancer. Oncotarget.
7:55155–55168. 2016.PubMed/NCBI
|
|
13
|
Hsu WM, Hsieh FJ, Jeng YM, Kuo ML, Chen
CN, Lai DM, Hsieh LJ, Wang BT, Tsao PN, Lee H, et al: Calreticulin
expression in neuroblastoma-a novel independent prognostic factor.
Ann Oncol. 16:314–321. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kageyama S, Isono T, Matsuda S, Ushio Y,
Satomura S, Terai A, Arai Y, Kawakita M, Okada Y and Yoshiki T:
Urinary calreticulin in the diagnosis of bladder urothelial
carcinoma. Int J Urol. 16:481–486. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chen CN, Chang CC, Su TE, Hsu WM, Jeng YM,
Ho MC, Hsieh FJ, Lee PH, Kuo ML, Lee H and Chang KJ: Identification
of calreticulin as a prognosis marker and angiogenic regulator in
human gastric cancer. Ann Surg Oncol. 16:524–533. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Erić A, Juranić Z, Milovanović Z, Marković
I, Inić M, Stanojević-Bakić N and Vojinović-Golubović V: Effects of
humoral immunity and calreticulin overexpression on postoperative
course in breast cancer. Pathol Oncol Res. 15:89–90. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wemeau M, Kepp O, Tesnière A, Panaretakis
T, Flament C, De Botton S, Zitvogel L, Kroemer G and Chaput N:
Calreticulin exposure on malignant blasts predicts a cellular
anticancer immune response in patients with acute myeloid leukemia.
Cell Death Dis. 1:e1042010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Peng RQ, Chen YB, Ding Y, Zhang R, Zhang
X, Yu XJ, Zhou ZW, Zeng YX and Zhang XS: Expression of calreticulin
is associated with infiltration of T-cells in stage IIIB colon
cancer. World J Gastroenterol. 16:2428–2434. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lwin ZM, Guo C, Salim A, Yip GW, Chew FT,
Nan J, Thike AA, Tan PH and Bay BH: Clinicopathological
significance of calreticulin in breast invasive ductal carcinoma.
Mod Pathol. 23:1559–1566. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gardai SJ, McPhillips KA, Frasch SC,
Janssen WJ, Starefeldt A, Murphy-Ullrich JE, Bratton DL, Oldenborg
PA, Michalak M and Henson PM: Cell-surface calreticulin initiates
clearance of viable or apoptotic cells through trans-activation of
LRP on the phagocyte. Cell. 123:321–334. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tongu M, Harashima N, Yamada T, Harada T
and Harada M: Immunogenic chemotherapy with cyclophosphamide and
doxorubicin against established murine carcinoma. Cancer Immunol
Immunother. 59:769–777. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Perez CA, Fu A, Onishko H, Hallahan DE and
Geng L: Radiation induces an antitumour immune response to mouse
melanoma. Int J Radiat Biol. 85:1126–1136. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Obeid M, Panaretakis T, Joza N, Tufi R,
Tesniere A, van Endert P, Zitvogel L and Kroemer G: Calreticulin
exposure is required for the immunogenicity of gamma-irradiation
and UVC light-induced apoptosis. Cell Death Differ. 14:1848–1850.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bifulco G, Miele C, Di Jeso B, Beguinot F,
Nappi C, Di Carlo C, Capuozzo S, Terrazzano G, Insabato L and
Ulianich L: Endoplasmic reticulum stress is activated in
endometrial adenocarcinoma. Gynecol Oncol. 125:220–225. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Leslie KK, Sill MW, Fischer E, Darcy KM,
Mannel RS, Tewari KS, Hanjani P, Wilken JA, Baron AT, Godwin AK, et
al: A phase II evaluation of gefitinib in the treatment of
persistent or recurrent endometrial cancer: A gynecologic oncology
group study. Gynecol Oncol. 129:486–494. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wang H, Liu Z, Gou Y, Qin Y, Xu Y, Liu J
and Wu JZ: Apoptosis and necrosis induced by novel realgar quantum
dots in human endometrial cancer cells via endoplasmic reticulum
stress signaling pathway. Int J Nanomedicine. 10:5505–5512. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Obeid M, Tesniere A, Ghiringhelli F, Fimia
GM, Apetoh L, Perfettini JL, Castedo M, Mignot G, Panaretakis T,
Casares N, et al: Calreticulin exposure dictates the immunogenicity
of cancer cell death. Nat Med. 13:54–61. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
De Boo S, Kopecka J, Brusa D, Gazzano E,
Matera L, Ghigo D, Bosia A and Riganti C: iNOS activity is
necessary for the cytotoxic and immunogenic effects of doxorubicin
in human colon cancer cells. Mol Cancer. 8:1082009. View Article : Google Scholar : PubMed/NCBI
|