Introduction
Src homology phosphotyrosine phosphatase 2 (Shp2)
encoded by PTPN11 is a non-receptor protein tyrosine
phosphatase (PTP), which is important in cell signal transudation.
Shp2 was the first confirmed proto-oncogene among the PTP
superfamily (1). It composes two
tandem SH2 domains at the N-terminus and a PTP domain at the
C-terminus (2). Shp2 can form an
intramolecular interface between the N-SH2 domain and the PTP
domain. Upon activation, N-SH2 domains can bind phosphotyrosine
residues and activate the activity of Shp2 by interrupting the
self-inhibitory interaction between N-SH2 and PTP domains (3). Shp2 has an overall positive effect in
transducing signals for a wide array of cytokines and growth
factors. It acts downstream of several receptors, including Met
receptor, fibroblast growth factor receptor, epidermal growth
factor receptor and insulin receptor, and is involved in multiple
cell signaling processes, including the Ras-extracellular
signal-regulated kinase (ERK), phosphoinositide 3-kinase-Akt, Janus
kinase-signal transducer and activator of transcription, nuclear
factor-κB, and mammalian target of rapamycin pathways (4).
Germline or somatic mutations in PTPN11 are
associated with Noonan syndrome, LEOPARD syndrome and juvenile
myelomonocytic leukemia (5). The
overexpression of Shp2 is also involved in human cancer (6,7), however,
the signaling mechanisms of Shp2 in cancer remain to be fully
elucidated. There are several conflicting reports on the
association between Shp2 and cancer. Certain studies have found
that the expression of Shp2 decreases in certain types of tumor
(8–10). However, the opposite was concluded in
hepatocellular carcinoma (11–13). Shp2
is predominantly localized in the cytoplasm matrix, however,
localization in other cellular subcompartments, including the
nucleus and the mitochondria, has also been found (14,15). The
different cellar localization suggests the different functions of
Shp2. Determining the function of Shp2 in these organelles is
likely to assist in understanding the molecular mechanisms involved
in Shp2-associated tumorigenesis.
Several Shp2 inhibitors have been identified
(16–21). It is noteworthy that the Shp2
inhibitor, SHP099, which maintains Shp2 in an auto-inhibited
conformation, shows potent antitumor efficacy in mouse tumor
xenograft models (22).
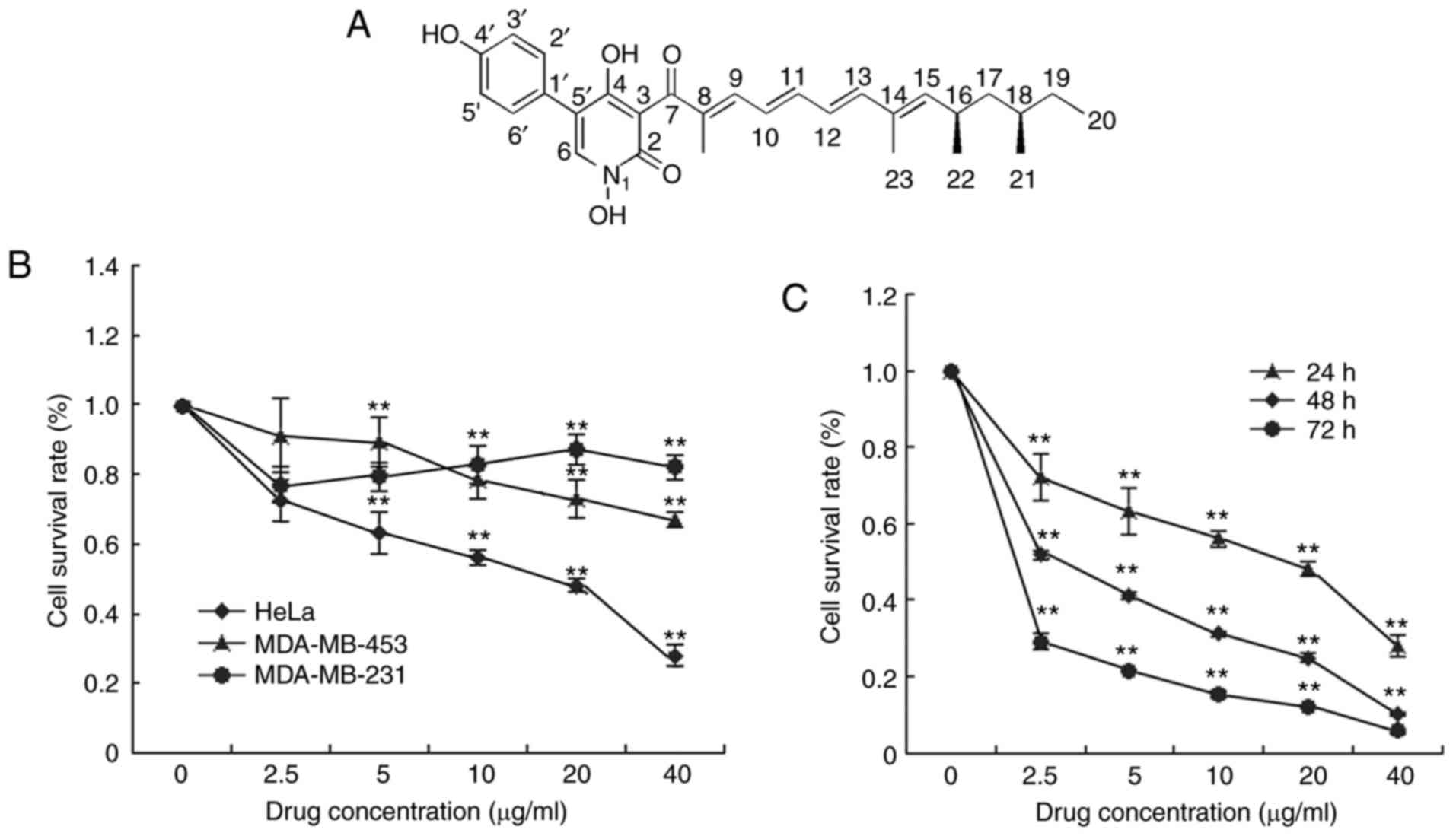
In our previous study, the novel compound,
fumosorinone (Fumos) was identified using a PTP enzyme-screening
assay (Fig. 1A). It showed high
selectivity towards Shp2, compared with other PTPs. Fumos inhibited
Shp2-mediated cell signaling without notable off-target effects in
human cancer lines (23). In the
present study, the cytotoxic activity of Fumos on different human
cell lines, and its effect on cell cycle arrest and tumor cell
migration were examined. The investigation focused on the tyrosine
(Tyr) phosphorylation of FAK involved in cell migration regulated
by Shp2. The combination effect of Fumos with other inhibitors,
including 5-fluoracil (5-FU) and p38 inhibitor, was also
detected.
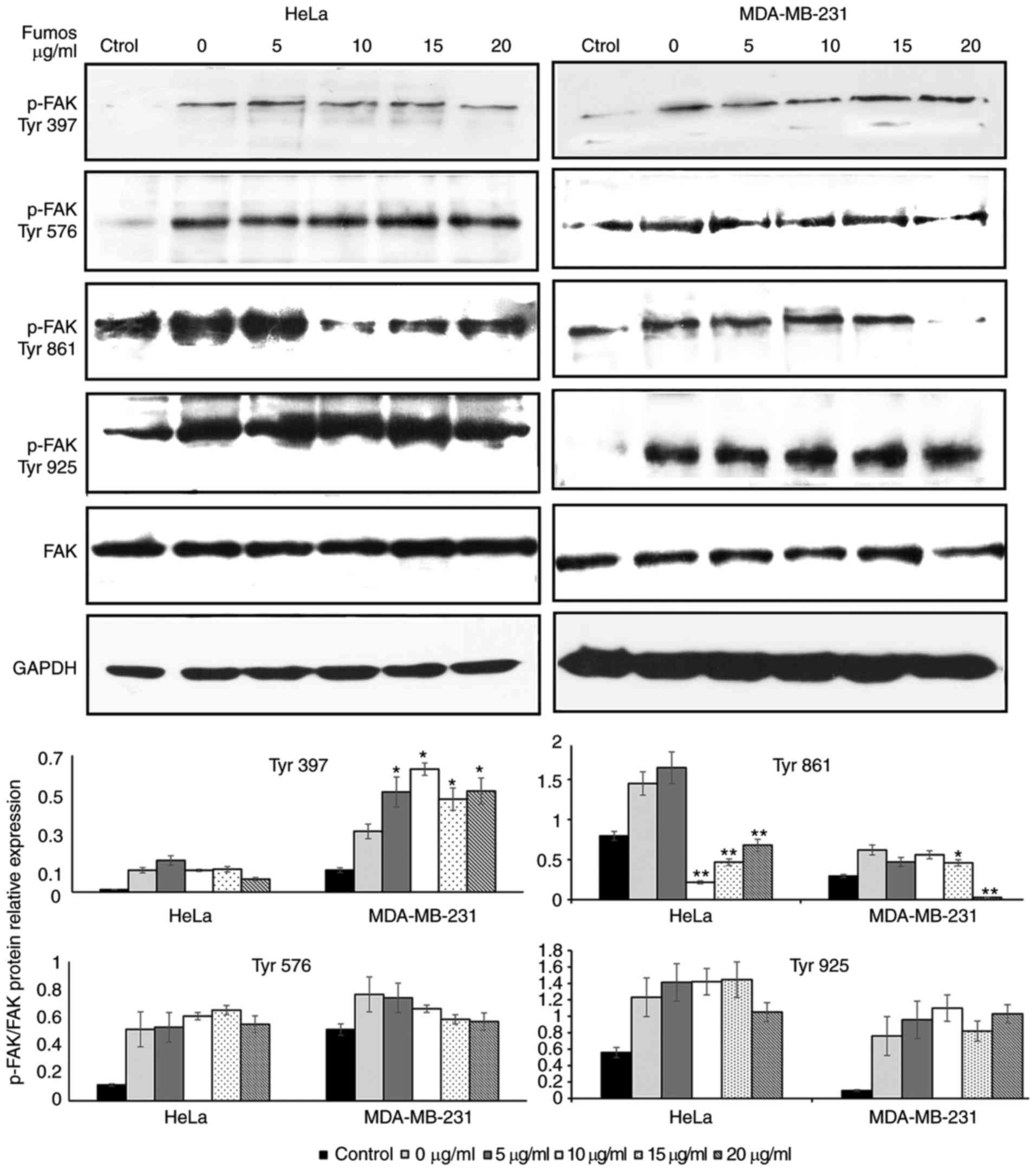
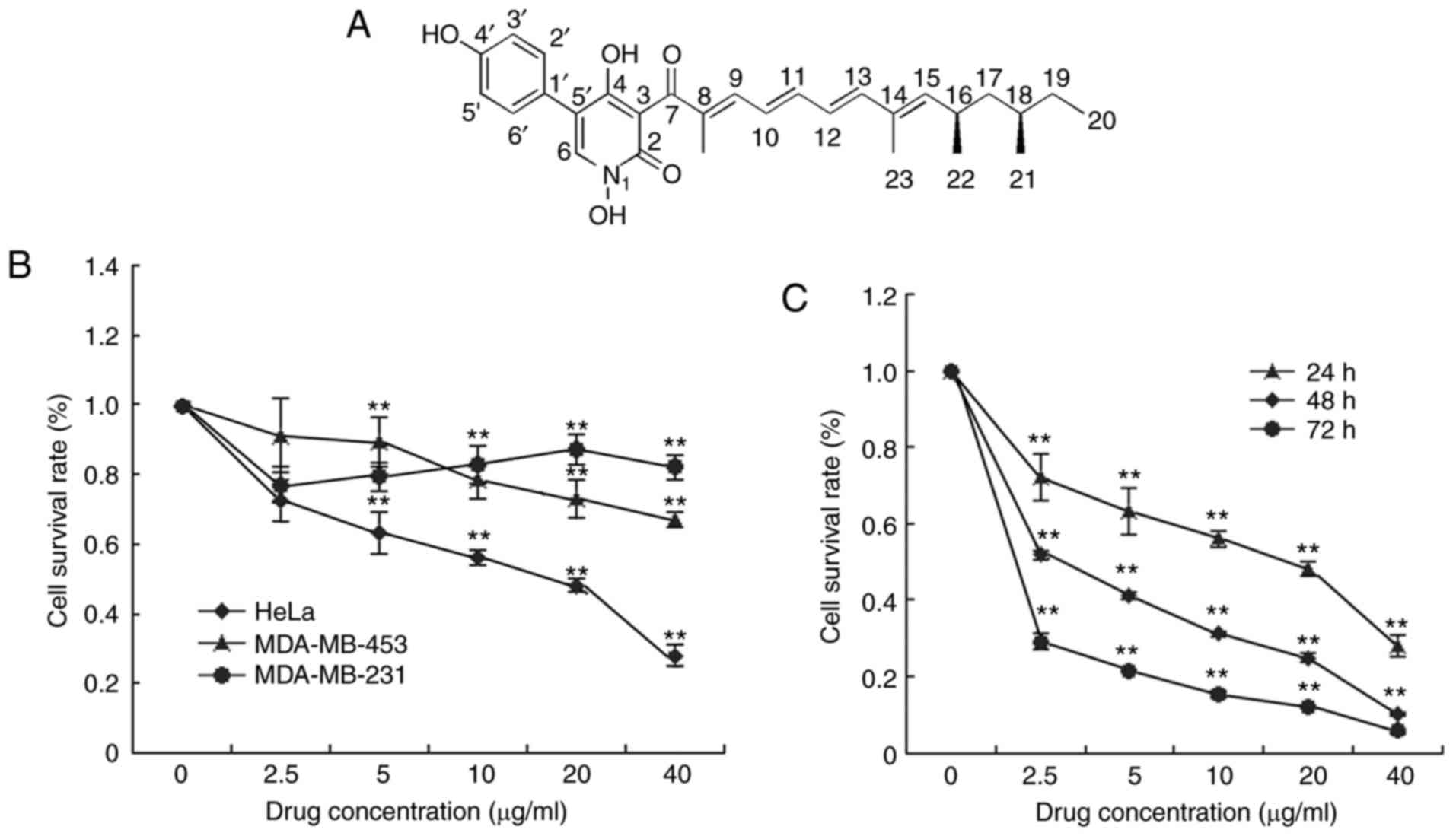 | Figure 1.Effect of Fumos on the viability of
different cell lines. (A) Structure of Fumos. (B) Cell
proliferation was examined using the MTT assay. Cells were treated
with 2.5, 5,10, 20 and 40 µg/ml Fumos, or with DMSO (0.5%) as the
vehicle control, for 24 h. The data are expressed as the mean ±
standard deviation of three independent experiments. (C) HeLa cells
were treated with 2.5, 5,10, 20 and 40 µg/ml Fumos, or with DMSO
(0.5%) as the vehicle control, for 24, 48 and 72 h. **P<0.01,
vs. untreated cells. One-way analysis followed by Tukey's test was
performed. Fumos, fumosorinone. |
Materials and methods
Chemicals and antibodies
Fumos was isolated and purified with a purity of 99%
according to the methods described by Chen et al (23). Phosphorylated (p-) FAK pTyr861 (cat.
no. 11059), p-FAK pTyr576 (cat. no. 11545) and p-FAK pTyr925 (cat.
no. 11123) antibodies were purchased from Signal way Antibody LLC
(College Park, MD, USA), FAK (cat. no. 3285) and p-FAK pTyr397
(cat. no. 3283) antibodies were purchased from Cell Signaling
Technology, Inc. (Danvers, MA, USA). GADPH (cat. no. sc-47724)
antibody was purchased from Santa Cruz Biotechnology, Inc. (Dallas,
TX, USA). Goat anti-rabbit IgG (H+L), HRP conjugate (cat. no.
SA00001-2) and Goat anti-mouse IgG (H+L), HRP conjugate (cat. no.
SA00001-1) antibodies were purchased from ProteinTech Group, Inc.
(Chicago, IL, USA). 5-FU and SB203580 were purchased from
Sigma-Aldrich (Merck KGaA, Darmstadt, Germany). Polyvinylidene
fluoride (PVDF) was obtained from EMD Millipore (Billerica, MA,
USA).
Cell culture
All cell lines were purchased from the Type Culture
Collection of the Chinese Academy of Sciences (Shanghai, China).
The HeLa cells were cultured in Dulbecco's modified Eagle's medium
(HyClone; GE Healthcare Life Sciences, Logan, UT, USA), and the
MDA-MB-231 and MDA-MB-453 cells were cultured in RPMI 1640 medium
supplemented with 10% fetal bovine serum (HyClone; GE Healthcare
Life Sciences) at 37°C, under 95% air and 5% CO2.
MTT assay
The exponentially growing cells (5×103)
were cultured in 96-well plates with 100 µl medium and treated with
0, 2.5, 5, 10, 20 and 40 µg/ml Fumos dissolved in DMSO at 37°C,
under 5% CO2 and 95% air for 24, 48 and 72 h, The DMSO
concentration was maintained <0.5%. Subsequently, 20 µl (5
mg/ml) of MTT was added to each well, and the plates were incubated
at 37°C for 4 h, following which 100 µl of 0.01 M SDS-HCl was added
prior to incubation at 37°C overnight. The absorbance at 570 nm was
detected using a microplate reader (Thermo Fisher Scientific, Inc.,
Waltham, MA, USA).
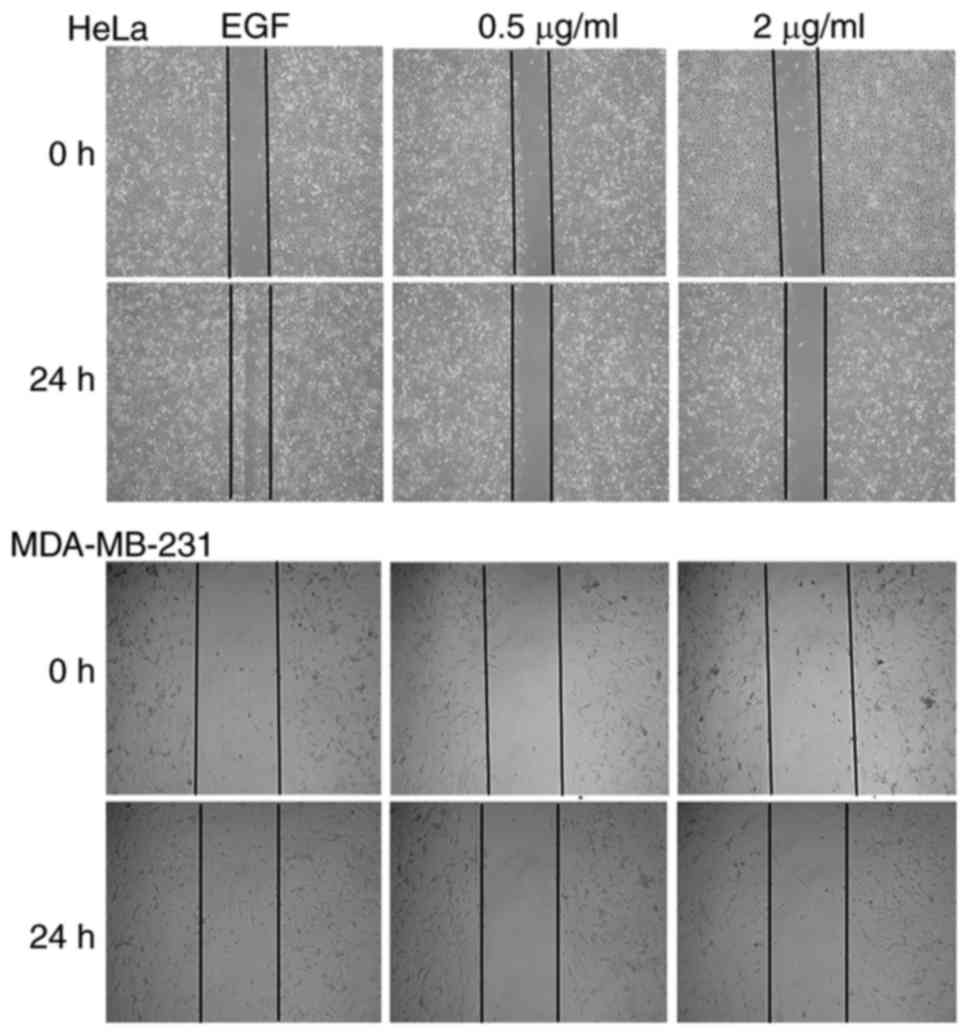
Wound-healing motility assay
The cells reached 70–80% confluence as a monolayer
in 6-well plates. A scratch across the center of the monolayer was
created in each well using a 200-µl pipette tip, and the cells were
then serum-starved for 12 h, following which 20 ng/ml epidermal
growth factor (EGF) and 0.5 and 2 µg/ml Fumos were added. Images of
each well were captured under an IX53 inverted fluorescence
microscope (Olympus Corporation, Tokyo, Japan).
Western blot analysis
The cells were incubated and dissolved in lysis
buffer (50 mM Hepes-NaOH, 100 mM NaCl, 2.5 mM EDTA, 0.5% NP-40, 10%
glycerol, 1 mM PMSF, 1 mM DTT, 2 µg/ml aprotinin, 0.7 µg/ml
pepstatin, 0.5 µg/ml leupetin and 2 µg/ml aprotinin). The cell
lysates were centrifuged at 12,000 g for 10 min at 4°C, following
which the supernatant was collected and the protein concentration
was determined using the Bradford assay. The proteins (30 µg) were
denatured in sample buffer and loaded onto a 10% sodium dodecyl
sulfate-polyacrylamide gel. Following electrophoresis, the proteins
were transferred onto a PVDF membrane. The PVDF membrane was
blocked with 5% non-fat milk powder (w/v) for 1 h at room
temperature, and then incubated with specific
primary/HRP-conjugated secondary antibodies. All the primary
antibodies were diluted at 1:1,000 and the secondary antibodies
were diluted at 1:2,000. PVDF membranes were incubated in the
antibody solution for 1 h at room temperature. The anti-GAPDH
antibody was used to ensure equal protein loading. The bands were
visualized with ECL reagent and exposed with FUJI X-ray films
(FUJIFILM Corporation, Tokyo, Japan). Photoshop CS6 (Adobe Systems
Inc; San Jose, CA, USA) was used for grayscale analysis after
scanning the band of exposed X-ray films.
Cell analysis by flow cytometry
The cells were treated with Fumos at a concentration
of 0, 5, 10, 15 or 20 µg/ml in a six-well plate at a density of
2×105 cells/well for 24 h and then collected by
centrifugation at 600 × g for 5 min, following which they were
washed twice with ice-cold PBS. The cells were treated according to
the Cycle test Plus DNA Reagent kit protocol (BD Biosciences,
Franklin Lakes, NJ, USA). A total of 10,000 cells were analyzed.
Cell cycle distribution was analyzed with flow cytometry
(FACSCalibur; BD Biosciences, NJ, USA). An apoptotic assay was
performed using the Annexin V-FITC Apoptosis Detection kit (BD
Biosciences).
Immunofluorescence technique
The HeLa cells were seeded onto a polylysine-coated
glass coverslip in a 24-well plate at a density of 2×103
cells/well. The cells were treated with 20 µg/ml Fumos for 48 h,
with DMSO used as a control. The cells were washed with PBS three
times and stained with 1 ng/ml DAPI. Images of the cells were
captured using an Olympus IX53 fluorescence microscope.
Drug combination evaluation
The cells were treated with 5-FU (30, 60 and 120
µg/ml) or SB203580 (12.5, 25 and 50 µg/ml) alone or in combination
with Fumos (5, 10 and 15 µg/ml). Cell viability was assessed using
the MTT assay. Synergism, additivity and antagonism were quantified
by determining the combination index (CI), which was calculated by
the Chou-Talalay equation using CalcuSyn software version 2.1
(Biosoft, Cambridge, UK).
Statistical analysis
SPSS software version 12 (SPSS, Inc., Chicago, IL,
USA) was used for statistical analysis. Statistical significance of
differences was assessed using one-way analysis of variance
followed by a Tukey's post hoc test for multiple comparisons.
P<0.01 was considered to indicate a statistically significant
difference.
Results
Effect of Fumos on cell viability in
different cell lines
It was identified that Fumos inhibited the
proliferation of the HeLa, MDA-MB-231 and MDA-MB-453 human cells to
different degrees. Treatment with Fumos for 24 h showed
cytotoxicity against HeLa (IC50 11 µg/ml) and MDA-MB-231
(IC50 30 µg/ml) and MDA-MB-453 (IC50 31
µg/ml) cells (Fig. 1B). Fumos showed
the highest cytotoxicity towards HeLa cells. Fumos also exhibited
potent cytotoxicity against the HeLa cell line over 48 h
(IC50 5 µg/ml) and 72 h (IC50 3 µg/ml;
Fig. 1C). This showed that Fumos
inhibited the proliferation of HeLa cells in a time- and
dose-dependent manner. All data indicated that Fumos exhibited
selective cytotoxic effects towards different human cell lines.
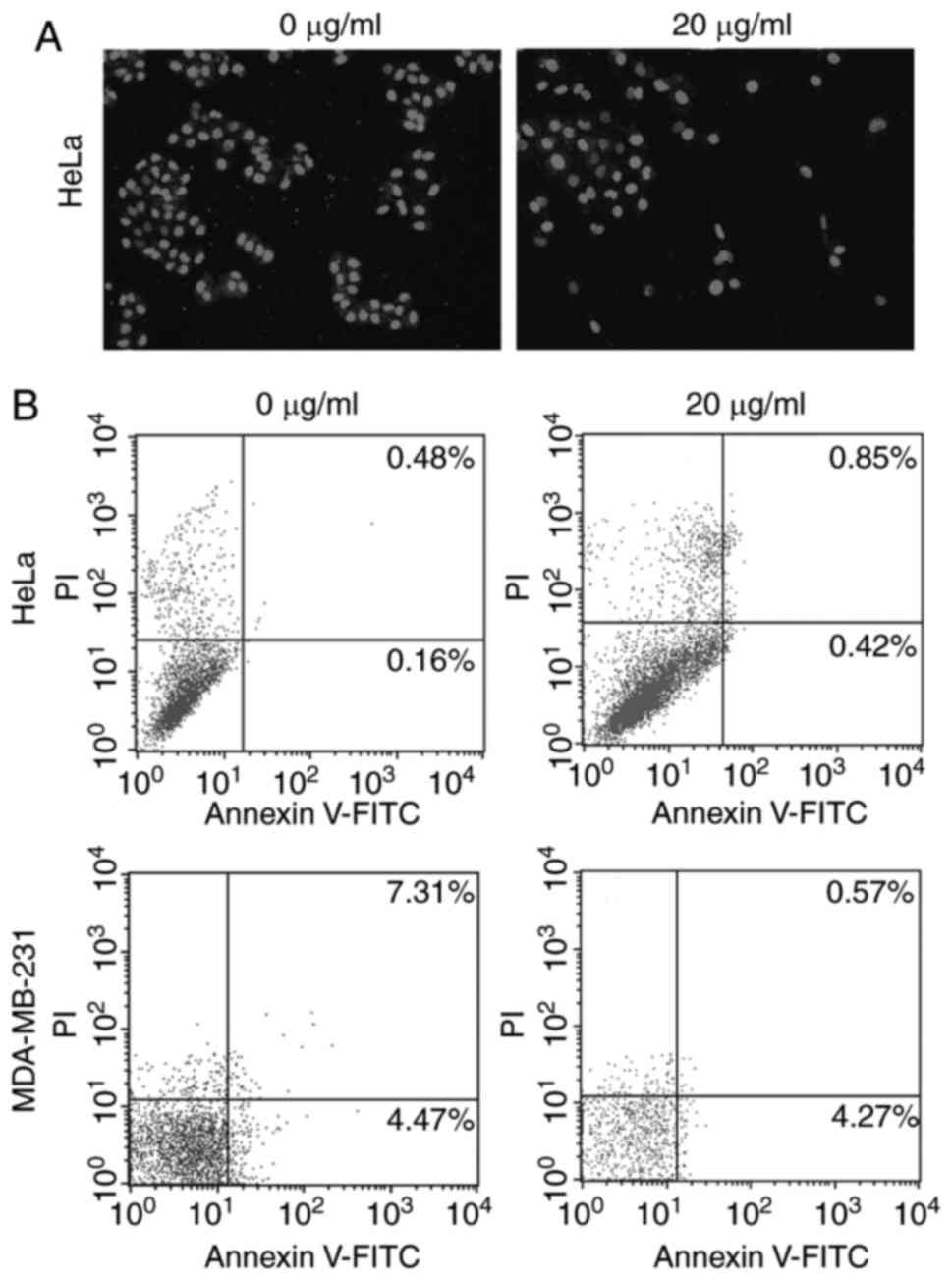
Effect of Fumos on cell apoptosis and
cell cycle
As Fumos inhibited the proliferation of human cells,
the present study also examined whether Fumos induced cell
apoptosis. Based on the IC50 values, four concentrations
of Fumos (0, 5, 10, 15 and 20 µg/ml) were selected to detect the
cell change at 48 h. Cell death and detachment from the culture
dishes leads to no cells being detected under higher concentrations
of Fumos, whereas very low concentrations of Fumos may induce no
changes in the cells (data not shown). A DAPI assay was used to
detect the nuclear changes and apoptotic body formation, which are
characteristic of apoptosis. The nuclear shape was intact following
Fumos treatment in the HeLa cells (Fig.
2A). In the MDA-MB-231 cells, the nuclear shape was also
unchanged (data not shown). The cytometric apoptosis assays also
showed that Fumos did not induce cell apoptosis in the HeLa or
MDA-MB-231 cells. The results of the highest concentration
treatment (20 µg/ml) at 48 h are shown in Fig. 2B. Subsequently, the present study
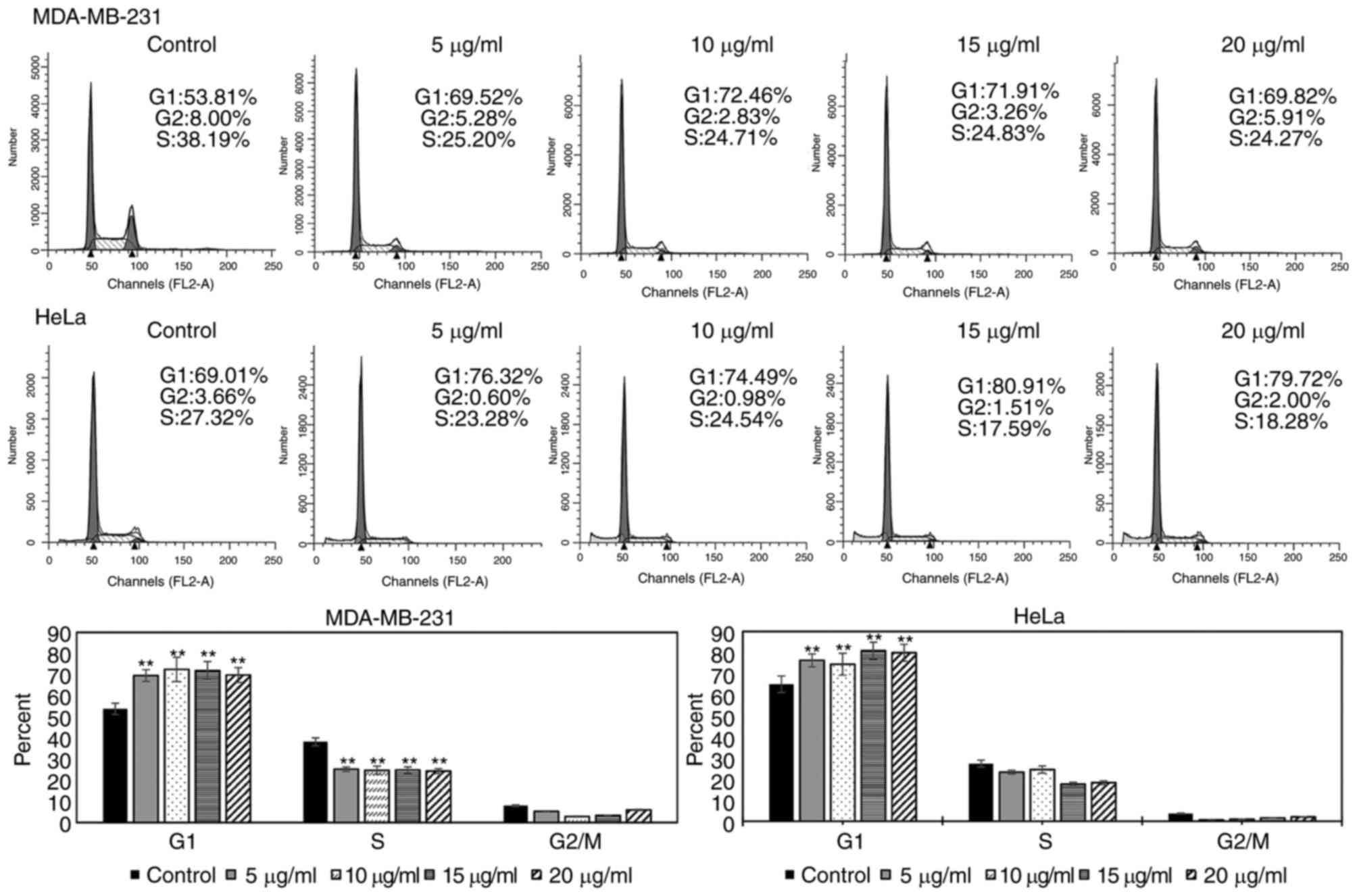
examined whether Fumos induced cell cycle arrest. As shown in
Fig. 3, Fumos induced cell cycle
arrest at the G1 phase. Following treatment for 24 h, Fumos
increased the percentage of HeLa cells in the G1 phase from 69.01
to 79.72%, compared with control. Fumos also caused the
accumulation of MDA-MB-231 cells in the G1 phase from 53.81 to
69.82%.
Effect of Fumos on tumor cell
migration
Increasing data have shown that Shp2 is linked to
cell migration (6). To examine the
effect of Fumos on cell migration, a wound healing assay was used
in the presence of 0.5 and 2 µg/ml Fumos. As shown in Fig. 4, EGF notably induced cell migration
and increased the rate of closure of the gap in the HeLa cells and
MDA-MB-231 cells. Fumos decreased the closure of the gap in the two
cell lines. In addition, the maximum concentration of 7 µg/ml Fumos
was used to examine its effect on cell migration. The higher
concentration also inhibited cell migration (data not shown). There
was no notable cell growth inhibition under these concentrations of
Fumos, thus the inhibition of cell migration was not due to the
cytotoxicity of Fumos. These results indicated that Fumos caused
the significant inhibition of tumor migration.
Effect of Fumos on the phosphorylation
of FAK involved in tumor cell migration
Hartman et al (24) found that Shp2 promoted EGF-induced
cell movement by regulating the activity of FAK through
dephosphorylating p-Tyr397. As Fumos inhibited the migration of the
HeLa and MDA-MB-231 cells, the present study examined whether Fumos
affected the phosphorylation of FAK involved in cell migration.
Fumos marginally increased the level of pTyr397, but had no effect
on the phosphorylation of pTyr576 or pTyr925 in the two cell lines
(Fig. 5). Fumos inhibited the
phosphorylation at pTyr861 of FAK in the HeLa cells, whereas the
inhibited phosphorylation of pTyr861 was only observed at a high
concentration of Fumos in the MDA-MB-231 cells. This indicated that
Shp2 regulated the phosphorylation of FAK in a different manner
depending on the cell type.
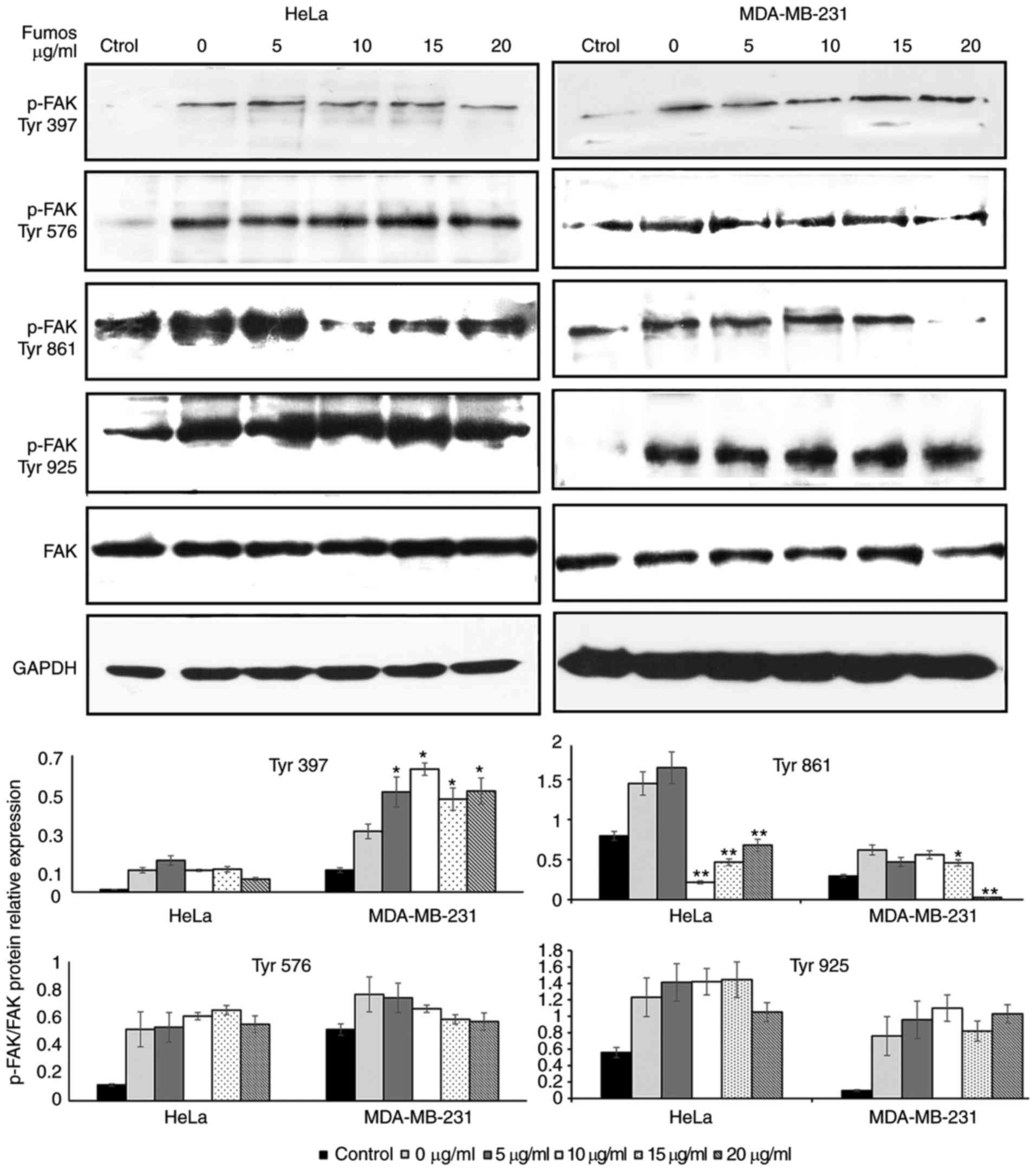 | Figure 5.Effect of Fumos on the
phosphorylation of FAK. Serum starved cells were pretreated with
various concentrations of Fumos (0, 5, 10, 15 and 20 µg/ml) for 24
h and then stimulated with EGF (20 ng/ml, 5 min). Western blot
analysis of the phosphorylation of FAK at sites 397, 576, 861 and
925 was performed. The histograms show the results of statistical
analysis. *P<0.05 and **P<0.01, vs. control. One-way analysis
of variance followed by Tukey's test was performed. Fumos,
fumosorinone; FAK, focal adhesion kinase; EGF, epidermal growth
factor; p-, phosphorylated. |
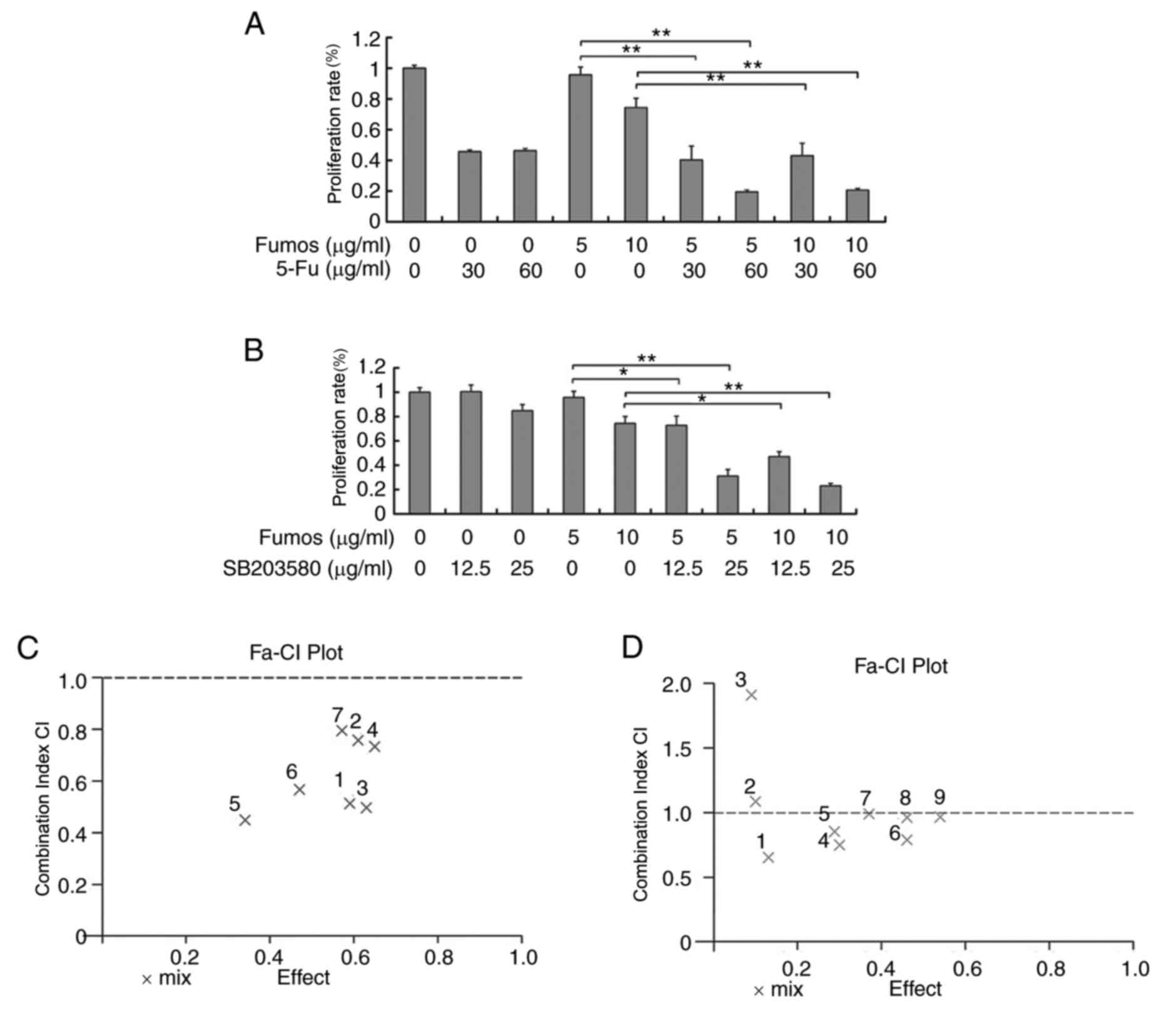
Combination effect of Fumos with other
agents
5-fluoracil (5-FU) is a potent, small-molecule DNA
synthesis inhibitor, and is widely used in chemotherapy for cancer
treatment. 5-FU can induce DNA damage and replication stress, and
disrupt the genome stability, whereas Shp2 can maintain genome
stability. The present study investigated whether the Shp2
inhibitor, Fumos, increased the sensitivity to 5-FU. The
combination effect of 5-FU and Fumos led to more potent inhibition
of HeLa cells, compared with the single treatment (Fig. 6A). Using CalcuSyn software, the
combined anti proliferative effects were examined. The resulting CI
theorem of Chou-Talalay offers quantitative definition for additive
effect (CI=1), synergism (CI<1), and antagonism (CI>1) in
drug combinations. A synergistic effect with low CIs (CI<1) was
found (Fig. 6B). The data showed that
Fumos synergized with 5-FU in suppressing cell growth. SB203580 is
a p38 mitogen-activated protein kinase (MAPK) inhibitor. The
combination of Fumos and p38 MAPK inhibitor increased the cell
death (Fig. 6C). At a low
concentration of SB203580, combination with Fumos showed no
synergism (CI>1). However, at a higher concentration of
SB203580, synergism was detected (CI<1; Fig. 6D). These results indicated that the
combination of Shp2 inhibitor with p38 MAPK inhibitor or 5-FU
resulted in the synergistic enhancement of growth inhibition.
Discussion
In our previous study, a novel Shp2 inhibitor, Fumos
was identified. It inhibited the Shp2-dependent activation of the
Ras/ERK signaling pathway induced by EGF (23). In the present study, the cytotoxity of
Fumos towards different cancer cell lines was examined. Fumos
showed varying degrees of cytotoxicity towards the human cell
lines, and this result suggested that Shp2-mediated cell signals
have various roles in different cell lines. The mechanism
underlying the cytotoxic effects of Fumos towards cells was also
examined. Flow cytometric assays showed that Fumos induced cell
arrest at the G1 phase, but did not cause cell apoptosis.
Shp2 is also important in cell migration (25,26). Shp2
has been shown to mediate tyrosine dephosphorylation of FAK. FAK is
a cytoplasmic tyrosine kinase, which is important in cell migration
(27). However, the major
phosphorylation sites of FAK regulated by Shp2 remain to be fully
elucidated. The phosphorylation of FAK was found to be moderately
upregulated upon Shp2 knockdown in prostate cancer cells and MCF7
cells (28,29). In Shp2-mutant Schwann cells, the
phosphorylation of FAK on Tyr925 and Tyr576/577, but not on Tyr397,
was markedly downregulated, however, in neural stem cells, Shp2
only affected the phosphorylation of FAK on Tyr397 (30,31). The
tyrosine phosphorylation of FAK and p130Cas has also been reported
to be unaffected by the inhibition of Shp2 in certain cells
(32). Fumos marginally increased
pTyr397, had no effect on phosphorylation at pTyr576 or pTyr925,
and reduced pTyr861 in the two cell lines. This discrepancy may be
due to differences in Shp2 regulating the signaling systems in the
different types of cells. Shp2 may mediate the activation as well
as inactivation of FAK. It is important to investigate whether Shp2
at other sites regulates the phosphorylation of FAK. The
association between FAK and Shp2 requires further
investigation.
Until now, only several highly selective Shp2
inhibitors have been reported. There are no reports of the
combination effect of Shp2 inhibitor and other chemical agents. The
present study examined the combined anticancer effect of Fumos with
5-FU or p38 MAPK inhibitor.
5-FU is a DNA synthesis inhibitor, which inhibits
the synthesis of DNA by inhibiting thymidine synthetase. 5-FU is
commonly used in combination chemotherapeutic programs for cancer
patients. Drug toxicity and resistance remain a significant
limitation in the clinical use of 5-FU (33). Novel therapeutic strategies are
urgently required to improve 5-FU sensitivity and cellular
responses. The Shp2 inhibitor, Fumos, synergizes with 5-FU in
suppressing cell growth. This is a novel strategy to improve 5-FU
sensibility. 5-FU can activate certain kinases involved in cell
cycle checkpoints and DNA repair, which are important for drug
resistance (34). Shp2 is also
important for DNA replication and damage checkpoints (35). Whether DNA damage checkpoints are
involved in the synergistic effect between Fumos and 5-FU requires
further investigation.
p38 MAPK is important in a wide variety of cellular
functions in response to a range of stimuli involved in cell
survival, cell death, cell inflammation and immune modulation
(36). p38 MAPK is also an attractive
target for intervention in certain types of solid tumor (37). The overexpression of Shp2 can increase
p38 enzyme activity (38). The Shp2
inhibitor, Fumos, synergized with p38 inhibitor in suppressing cell
growth. These findings demonstrated novel drug combinations, which
may potentiate the effectiveness of Shp2 inhibitor-based
treatments.
In conclusion, Fumos was shown to exhibit potent
anticancer properties alone and in combination with 5-FU and p38
MAPK inhibitor. Therefore, the combination treatment of Fumos and
5-FU or p38 MAPK inhibitor may serve as a novel effective
anticancer strategy for cancer treatment.
Acknowledgements
Not applicable.
Funding
This study was financially supported by the National
Natural Science Foundation of China (grant no. 31371957), the
Changjiang Scholars and Innovative Research Team in University
(grant no. IRT_15R16), the Foundation for High-level Talents in
Higher Education of Hebei, China (grant no. GCC2014034) and The
National Key Research and Development Program of China (grant nos.
2017YFD0201400 and 2017YFD0201401).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
CC and TDX performed the experiment. CC, TDX, PF,
JJW and LLM analyzed and interpreted the data. CC and DQL were
major contributors in writing and revising it critically for
important intellectual content. CC and DQL made substantial
contributions to conception and design. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mohi MG and Neel BG: The role of Shp2
(PTPN11) in cancer. Curr Opin Genet Dev. 17:23–30. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
He RJ, Yu ZH, Zhang RY and Zhang ZY:
Protein tyrosine phosphatases as potential therapeutic targets.
Acta Pharmacol Sin. 35:1227–1246. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chan G, Kalaitzidis D and Neel BG: The
tyrosine phosphatase Shp2 (PTPN11) in cancer. Cancer Metastasis
Rev. 27:179–192. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Matozaki T, Murata Y, Saito Y, Okazawa H
and Ohnishi H: Protein tyrosine phosphatase SHP-2: A proto-oncogene
product that promotes Ras activation. Cancer Sci. 100:1786–1793.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yang W, Wang J, Moore DC, Liang H, Dooner
M, Wu Q, Terek R, Chen Q, Ehrlich MG, Quesenberry PJ and Neel BG:
Ptpn11 deletion in a novel progenitor causes metachondromatosis by
inducing hedgehog signalling. Nature. 499:491–495. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Aceto N, Sausgruber N, Brinkhaus H,
Gaidatzis D, Martiny-Baron G, Mazzarol G, Confalonieri S, Quarto M,
Hu G, Balwierz PJ, et al: Tyrosine phosphatase SHP2 promotes breast
cancer progression and maintains tumor-initiating cells via
activation of key transcription factors and a positive feedback
signaling loop. Nat Med. 18:529–537. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhan Y, Counelis G and O'Rourke D: The
protein tyrosine phosphatase SHP-2 is required for EGFRvIII
oncogenic transformation in human glioblastoma cells. Exp Cell Res.
315:2343–2357. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jiang C, Hu F, Tai Y, Du J, Mao B, Yuan Z,
Wang Y and Wei L: The tumor suppressor role of Src homology
phosphotyrosine phosphatase 2 in hepatocellular carcinoma. J Cancer
Res Clin Oncol. 138:637–646. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tassidis H, Brokken LJ, Jirström K,
Bjartell A, Ulmert D, Härkönen P and Wingren AG: Low expression of
SHP-2 is associated with less favorable prostate cancer outcomes.
Tumor Biol. 34:637–642. 2013. View Article : Google Scholar
|
|
10
|
Yu SJ, Yu JK, Ge WT, Hu HG, Yuan Y and
Zheng S: SPARCL1, Shp2, MSH2, E-cadherin, p53, ADCY-2 and MAPK are
prognosis-related in colorectal cancer. World J Gastroenterol.
17:2028–2036. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Han T, Xiang D-M, Sun W, Liu N, Sun HL,
Wen W, Shen WF, Wang RY, Chen C, Wang X, et al: PTPN11/Shp2
overexpression enhances liver cancer progression and predicts poor
prognosis of patients. J Hepatol. 63:651–660. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bard-Chapeau EA, Li S, Ding J, Zhang SS,
Zhu HH, Princen F, Fang DD, Han T, Bailly-Maitre B, Poli V, et al:
Ptpn11/Shp2 acts as a tumor suppressor in hepatocellular
carcinogenesis. Cancer Cell. 19:629–639. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Xiang D, Cheng Z, Liu H, Wang X, Han T,
Sun W, Li X, Yang W, Chen C, Xia M, et al: Shp2 promotes liver
cancer stem cell expansion by augmenting β-catenin signaling and
predicts chemotherapeutic response of patients. Hepatology.
65:1566–1580. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tsutsumi R, Masoudi M, Takahashi A, Fujii
Y, Hayashi T, Kikuchi I, Satou Y, Taira M and Hatakeyama M: YAP and
TAZ, hippo signaling targets, act as a rheostat for nuclear SHP2
function. Dev Cell. 26:658–665. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zheng H, Li S, Hsu P and Qu CK: Induction
of a tumor-associated activating mutation in protein tyrosine
phosphatase Ptpn11 (Shp2) Enhances mitochondrial metabolism,
leading to oxidative stress and senescence. J Biol Chem.
288:25727–25738. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hellmuth K, Grosskopf S, Lum CT, Würtele
M, Röder N, von Kries JP, Rosario M, Rademann J and Birchmeier W:
Specific inhibitors of the protein tyrosine phosphatase Shp2
identified by high-throughput docking. Proc Natl Acad Sci USA.
105:7275–7280. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zeng LF, Zhang RY, Yu ZH, Li S, Wu L,
Gunawan AM, Lane BS, Mali RS, Li X, Chan RJ, et al: Therapeutic
potential of targeting the oncogenic SHP2 phosphatase. J Med Chem.
57:6594–6609. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Liu W, Yu B, Xu G, Xu WR, Loh ML, Tang LD
and Qu CK: Identification of cryptotanshinone as an inhibitor of
oncogenic protein tyrosine phosphatase SHP2 (PTPN11). J Med Chem.
56:7212–7221. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang X, He Y, Liu S, Yu Z, Jiang ZX, Yang
Z, Dong Y, Nabinger SC, Wu L, Gunawan AM, et al: Salicylic acid
based small molecule inhibitor for the oncogenic src homology-2
domain containing protein tyrosine phosphatase-2 (SHP2). J Med
Chem. 53:2482–2493. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chen L, Pernazza D, Scott LM, Lawrence HR,
Ren Y, Luo Y, Wu X, Sung SS, Guida WC, Sebti SM, et al: Inhibition
of cellular Shp2 activity by a methyl ester analog of SPI-112.
Biochem Pharmacol. 80:801–810. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen L, Sung SS, Yip ML, Lawrence HR, Ren
Y, Guida WC, Sebti SM, Lawrence NJ and Wu J: Discovery of a novel
shp2 protein tyrosine phosphatase inhibitor. Mol Pharmacol.
70:562–570. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chen YP, LaMarche MJ, Chan HM, Fekkes P,
Garcia-Fortanet J, Acker MG, Antonakos B, Chen CH, Chen Z, Cooke
VG, et al: Allosteric inhibition of SHP2 phosphatase inhibits
cancers driven by receptor tyrosine kinases. Nature. 535:148–152.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chen C, Cao M, Zhu S, Wang C, Liang F, Yan
L and Luo D: Discovery of a novel inhibitor of the protein tyrosine
phosphatase Shp2. Sci Rep. 5:176262015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hartman ZR, Schaller MD and Agazie YM: The
tyrosine phosphatase SHP2 regulates focal adhesion kinase to
promote EGF-induced lamellipodia persistence and cell migration.
Mol Cancer Res. 11:651–664. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sausgruber N, Coissieux MM, Britschgi A,
Wyckoff J, Aceto N, Leroy C, Stadler MB, Voshol H, Bonenfant D and
Bentires-Alj M: Tyrosine phosphatase SHP2 increases cell motility
in triple-negative breast cancer through the activation of
SRC-family kinases. Oncogene. 34:2272–2278. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhang RY, Yu ZH, Zeng L, Zhang S, Bai Y,
Miao J, Chen L, Xie J and Zhang ZY: SHP2 phosphatase as a novel
therapeutic target for melanoma treatment. Oncotarget.
7:73817–73829. 2016.PubMed/NCBI
|
|
27
|
Sieg DJ, Hauck CR, Ilic D, Klingbeil CK,
Schaefer E, Damsky CH and Schlaepfer DD: FAK integrates
growth-factor and integrin signals to promote cell migration. Nat
Cell Biol. 2:249–256. 2000. View
Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhang K, Zhao H, Ji Z, Zhang C, Zhou P,
Wang L, Chen Q, Wang J, Zhang P, Chen Z, et al: Shp2 promotes
metastasis of prostate cancer by attenuating the PAR3/PAR6/aPKC
polarity protein complex and enhancing epithelial-to-mesenchymal
transition. Oncogene. 35:1271–1282. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wang FM, Liu HQ, Liu SR, Tang SP, Yang L
and Feng GS: SHP-2 promoting migration and metastasis of MCF-7 with
loss of E-cadherin, dephosphorylation of FAK and secretion of MMP-9
induced by IL-1β in vivo and in vitro. Breast Cancer Res Treat.
89:5–14. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Grossmann KS, Wende H, Paul FE, Cheret C,
Garratt AN, Zurborg S, Feinberg K, Besser D, Schulz H, Peles E, et
al: The tyrosine phosphatase Shp2 (PTPN11) directs
Neuregulin-1/ErbB signaling throughout Schwann cell development.
Proc Natl Acad Sci USA. 106:16704–16709. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Huang YS, Cheng CY, Chueh SH, Hueng DY,
Huang YF, Chu CM, Wu ST, Tai MC, Liang CM, Liao MH, et al:
Involvement of SHP2 in focal adhesion, migration and
differentiation of neural stem cells. Brain Dev. 34:674–684. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Inagaki K, Noguchi T, Matozaki T, Horikawa
T, Fukunaga K, Tsuda M, Ichihashi M and Kasuga M: Roles for the
protein tyrosine phosphatase SHP-2 in cytoskeletal organization,
cell adhesion and cell migration revealed by overexpression of a
dominant negative mutant. Oncogene. 19:75–84. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Longley DB, Harkin DP and Johnston PG:
5-fluorouracil: Mechanisms of action and clinical strategies. Nat
Rev Cancer. 3:330–338. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
34
|
Fujinaka Y, Matsuoka K, Iimori M, Tuul M,
Sakasai R, Yoshinaga K, Saeki H, Morita M, Kakeji Y, Gillespie DA,
et al: ATR-Chk1 signaling pathway and homologous recombinational
repair protect cells from 5-fluorouracil cytotoxicity. DNA Repair
(Amst). 11:247–258. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Tsang YH, Han X, Man WY, Lee N and Poon
RY: Novel functions of the phosphatase SHP2 in the DNA replication
and damage checkpoints. PLoS One. 7:e499432012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Bradham C and McClay DR: p38 MAPK in
development and cancer. Cell Cycle. 5:824–828. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Koul HK, Pal M and Koul S: Role of p38 MAP
kinase signal transduction in solid tumors. Genes Cancer.
4:342–359. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Mamik MK and Ghorpade A: Src homology-2
domain-containing protein tyrosine phosphatase (SHP) 2 and p38
regulate the expression of chemokine CXCL8 in human astrocytes.
PLoS One. 7:e455962012. View Article : Google Scholar : PubMed/NCBI
|