Introduction
Lung cancer is the leading cause of
cancer-associated mortality worldwide, with the highest rate of
morbidity and mortality of all cancer types (1). Non-small cell lung cancer (NSCLC)
accounts for >80% of newly diagnosed patients (2), with an overall 5-year survival rate of
~17% (3). Unfortunately, majority of
patients with NSCLC are diagnosed at an advanced stage (4), and only 20% of patients have the
opportunity to undergo surgical therapy (5). Therefore, early diagnosis is important,
and a reliable and inexpensive biomarker is required to identify
accurate staging.
For clinicians, the Tumor-Node-Metastasis (TNM)
staging system provides reliable guidelines for the routine
prognosis prediction and treatment of NSCLC (6). This system characterizes the tumor
itself, the regional lymph nodes and potentially metastatic sites.
Furthermore, TNM stages provide a standard by which patients are
classified into different groups with similar prognoses for each
staging category (6). The TNM staging
system is capable of improving the prediction of outcomes for
patients with cancer, including lung cancer, renal cell carcinoma
and colorectal cancer (7–9). In addition to early detection, accurate
TNM staging exhibited more significant clinical effects.
It is widely acknowledged that inflammation
contributes to the development of numerous types of cancer and
inflammation is the seventh hallmark of cancer (10), and systemic inflammatory response is
important in tumorigenesis and carcinogenesis. Accumulating
evidence has suggested that the neutrophil-to-lymphocyte (NLR) and
the platelet-to-lymphocyte ratio (PLR), are potential indicators of
systemic inflammation and immune response (11,12). These
ratios are easily calculated based on the full blood count and have
been recognized as convenient, reliable and inexpensive markers to
predict the prognosis, progression, survival, metastasis and
regional lymph node invasion of patients with various types of
solid tumors (13–15). Several meta-analyses with large sample
sizes have evaluated the prognostic role of preoperative NLR and
PLR in different types of cancer, revealing that these two ratios
are associated with tumor progression and overall survival (OS),
including prostate cancer, esophageal cancer and breast cancer
(13,16,17).
Although a number of studies have confirmed the role of
cancer-related inflammation markers, the majority of studies have
focused on prognosis and treatment outcomes (18,19).
Recently, an increasing amount of evidence has
demonstrated that systemic inflammation is involved in stages of
solid tumor development (20,21). The NLR and PLR, as biomarkers
conveying information regarding systematic inflammatory response,
are described to be used as valuable predictive parameters for
tumor stages (20,22). For example, in papillary thyroid
cancer, significant elevation of NLR was correlated with an
advanced disease stage (20).
However, the association between these two ratios and TNM stages in
patients with NSCLC has not been fully elucidated. Therefore, the
present study aimed to exclusively investigate whether these two
indicators may provide useful information for the early detection
of NSCLC and may serve important roles in predicting disease
stages.
Materials and methods
Patient selection
This retrospective analysis included data from the
hospital records of 171 patients with NSCLC who had undergone
surgical treatment at Huashan Hospital, Fudan University (Shanghai,
China) between October 2013 and March 2016. This included 104 male
patients and 67 female patients, with a mean age of 59.313 and an
age range of 33–80 years old. The patient exclusion criteria were
as follows: Any sign of inflammatory condition, blood transfusion
within 3 months, active bleeding during the preceding 2 months,
bleeding diathesis, hyperthyroidism or hypothyroidism, connective
tissue diseases, anti-coagulant therapy or anti-inflammatory
treatment during the preceding week, or receipt of any
cancer-specific pretreatment.
The data of healthy controls were obtained from the
Physical Examination Center of Huashan, Fudan University. Annual
health examinations were performed at the hospital. The exclusion
criteria were as described earlier. Additionally, participants with
any other diseases or conditions that may confound the
interpretation of data (e.g., cancer, immune diseases or pregnancy)
were not recruited.
The present study was approved by the Ethics
Committee of Huashan Hospital, Fudan University. Written informed
consent was obtained from every participant according to the
institutional guidelines of Huashan Hospital, Fudan University when
they were enrolled.
Data collection and calculation
The records of patients were collected when they
first attended the hospital, including identification number, name,
age, sex, and TNM stages (according to the seventh edition of the
American Joint Committee on Cancer guidelines), and blood counts
were routinely measured on the first day the patients were
hospitalized. The data of the healthy controls were collected from
online medical reports. Next, the NLR ratio was calculated as ratio
of the absolute neutrophil number and the absolute lymphocyte
number per microliter of whole blood; and the PLR ratio was
calculated as ratio of the absolute platelet number and the
absolute lymphocyte number per microliter of whole blood.
Statistical analysis
For comparisons between cancer patients and healthy
controls, all data were expressed at as the mean ± standard error
of mean or median and maximum/minimum or median and interquartile
range (25–75%). Student's t-tests and Mann-Whitney U tests were
used to compare normally and not normally distributed variables,
respectively. One-way analysis of variance, followed by
Bonferroni's post hoc test, was used for the comparison between
different stages. Statistical analyses were performed using
GraphPad Prism 6 (GraphPad Software, Inc., La Jolla, CA, USA) and
SPSS version 19 (IBM Corp., Armonk, NY, USA) software. Receiver
operating characteristic (ROC) analyses were used to predict the
efficacy of NLR and PLR. The associations between NLR or PLR and
TNM stages were evaluated using the Kruskal-Wallis test and a
multivariate regression model. P<0.05 was considered to indicate
a statistically significant difference.
Results
Patient characteristics
There were ultimately 171 patients and 105 controls
available with complete clinical data who were subsequently
enrolled in the present study. Table
I demonstrates the patient characteristics. The percentages of
patients with different stages of cancer were as follows: 80
(46.78%) with Stage I disease, 24 (14.04%) with Stage II disease,
43 (25.14%) with Stage III disease and 24 (14.04%) with Stage IV
disease. According to the T, N and M stages, 23.39% patients
exhibited deep tumor infiltration (T stage>2), 38.60% exhibited
lymphatic invasion (N stage>0) and distant metastasis was
observed in 12.28% of patients (M stage=1).
 | Table I.Demographic information of patients
with non-small cell lung cancer and healthy controls. |
Table I.
Demographic information of patients
with non-small cell lung cancer and healthy controls.
| Variable | Cancer
patients | Controls | P-value |
|---|
| All cases, n | 171 | 105 |
|
| Age, mean ±
SEM | 59.313±0.7335 | 46.11±0.8590 |
<0.0001a |
| Sex, n |
|
|
|
|
Male | 104 | 85 |
0.0008 |
|
Female | 67 | 20 |
|
| Smoking history,
n |
|
|
|
|
Yes | 48 | 38 |
0.1811 |
| No | 123 | 67 |
|
| Histology, n |
|
|
|
|
Adenocarcinoma | 116 |
|
|
|
Squamous cell carcinoma | 45 |
|
|
| Large
cell carcinoma | 1 |
|
|
|
Adenosquamous carcinoma | 7 |
|
|
|
Pleomorphic carcinoma | 2 |
|
|
| TNM stage, n
(%) |
|
|
|
| I | 80 (46.78) |
|
|
| II | 24 (14.04) |
|
|
|
III | 43 (25.14) |
|
|
| IV | 24 (14.04) |
|
|
| T stage, n (%) |
|
|
|
| T1 | 41 (23.99) |
|
|
| T2 | 90 (52.63) |
|
|
| T3 | 29 (16.96) |
|
|
| T4 | 11 (6.43) |
|
|
| N stage, n (%) |
|
|
|
| N0 | 105 (61.40) |
|
|
| N1 | 28 (16.37) |
|
|
| N2 | 24 (14.04) |
|
|
| N3 | 14 (8.19) |
|
|
| M stage |
|
|
|
| M0 | 150 (87.72) |
|
|
| M1 | 21 (12.28) |
|
|
| WBC, median
(range) | 6.370
(2.82–18.31) | 5.790
(3.37–9.76) |
0.0020a |
| Lymphocyte, median
(range) | 1.802
(0.508–3.604) | 1.989
(0.482–3.639) |
0.0278a |
| Neutrophil, median
(range) | 3.74
(0.790–16.050) | 3.259
(1.381–6.127) |
0.0020a |
| PLT, median
(range) | 205 (84–324) | 219 (74–520) |
0.0088a |
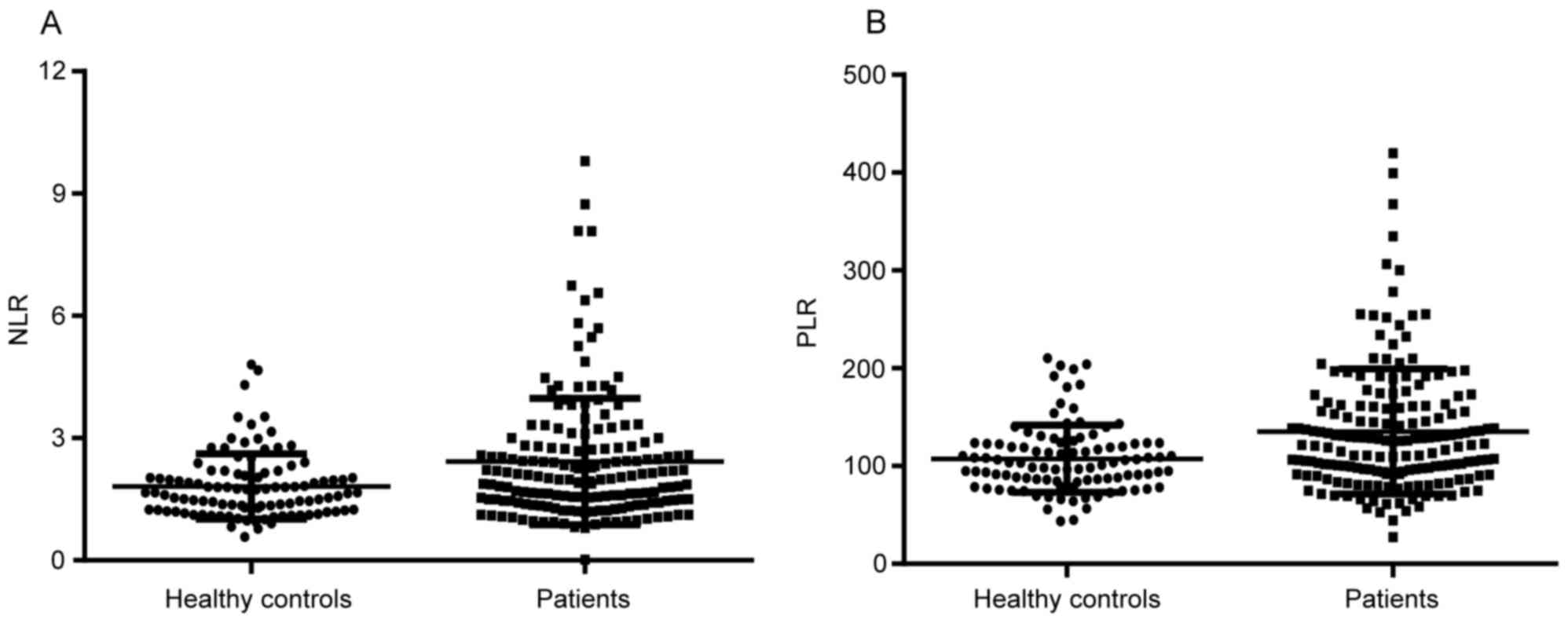
Comparison of NLR and PLR in patients
with NSCLC and healthy controls
As demonstrated in Table
I, compared with controls, NSCLC patients had higher white
blood cell (WBC), neutrophil and platelet counts (all P<0.05),
but a lower lymphocyte count (P<0.05). Despite this, as
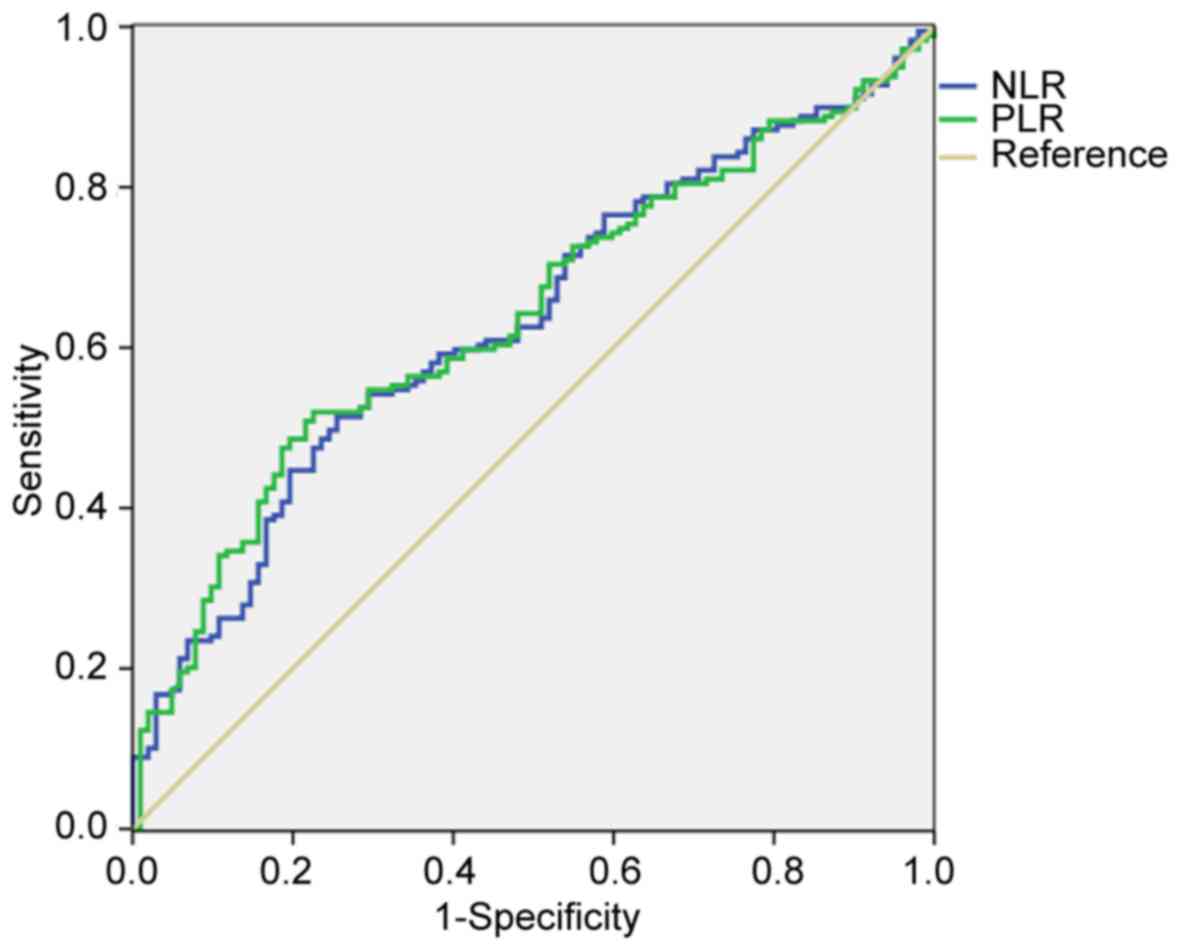
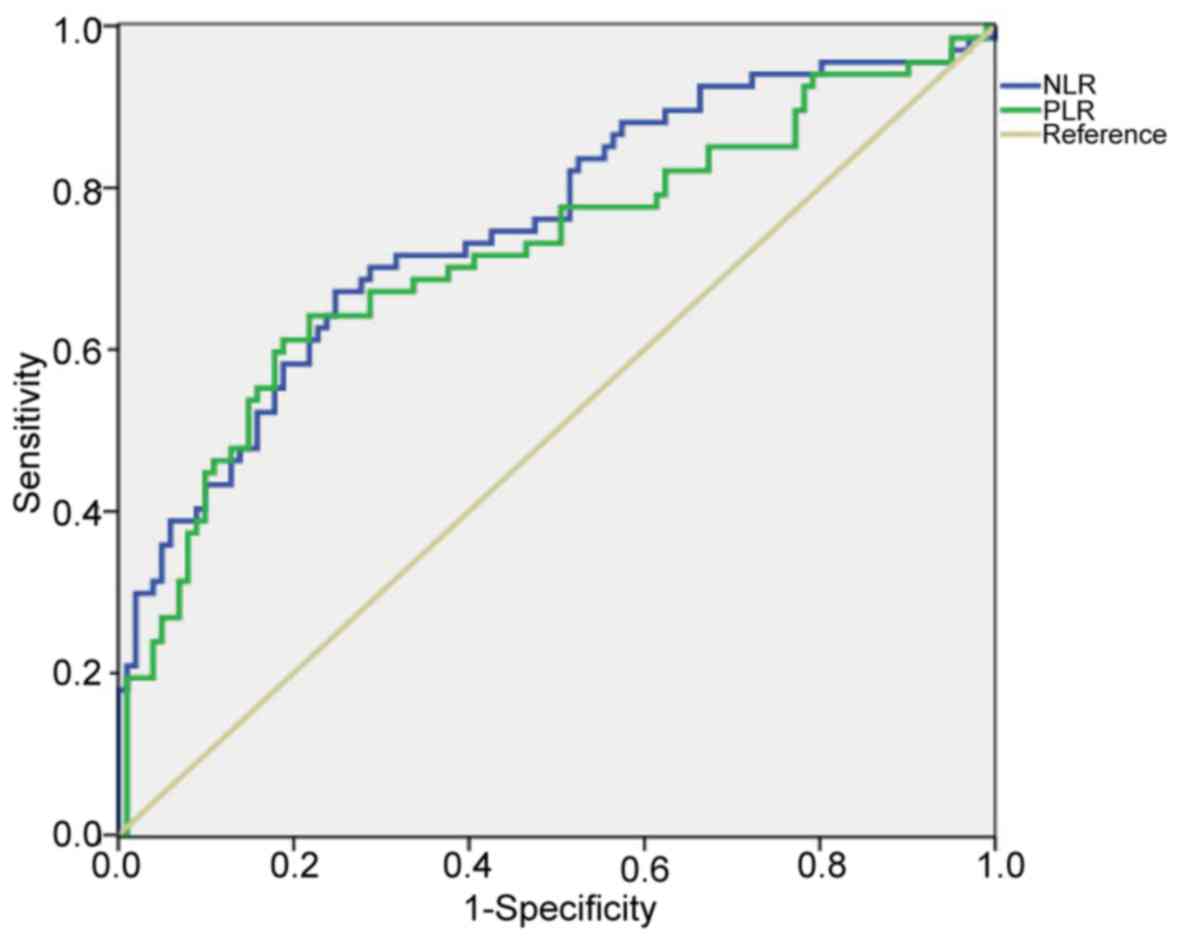
demonstrated in Fig. 1 and Table II, there were significant differences
in the levels of NLR and PLR between the patient and control groups
(NLR, 2.719±0.183 vs. 1.813±0.079, P<0.01; PLR, 135.800±4.778
vs. 112.000±5.651, P<0.01, respectively). ROC analyses were
performed to evaluate the accuracy of NLR and PLR in diagnosing
NSCLC. The AUC values for NLR and PLR were 0.633 and 0.639,
respectively (Fig. 2). These data
suggested that these two markers had certain predictive value for
the presence of NSCLC.
 | Table II.Association between NLR or PLR and
TNM stages in lung cancer. |
Table II.
Association between NLR or PLR and
TNM stages in lung cancer.
| Variable | n (%) | NLR, mean
(IQR) | PLR, mean
(IQR) |
|---|
| Lung cancer |
|
|
|
| TNM
stage I | 80 (46.78) | 1.613
(1.222–2.435) | 106.800
(87.480–137.600) |
| TNM
stage II | 24 (14.04) | 2.170
(1.597–3.294) | 110.300
(97.700–168.100) |
| TNM
stage III | 43 (25.14) | 2.307
(1.636–3.559)b | 136.100
(93.890–177.600) |
| TNM
stage IV | 24 (14.04) | 3.108
(1.990–4.285)b | 139.900
(105.100–196.100)b |
| Total | 171 (100) | 2.096
(1.466–2.892) | 125.100
(93.890–161.700) |
| Control | 105 (100) | 1.668
(1.231–2.085) | 103.200
(85.250–123.600) |
| P value |
|
<0.0001a |
<0.0001a |
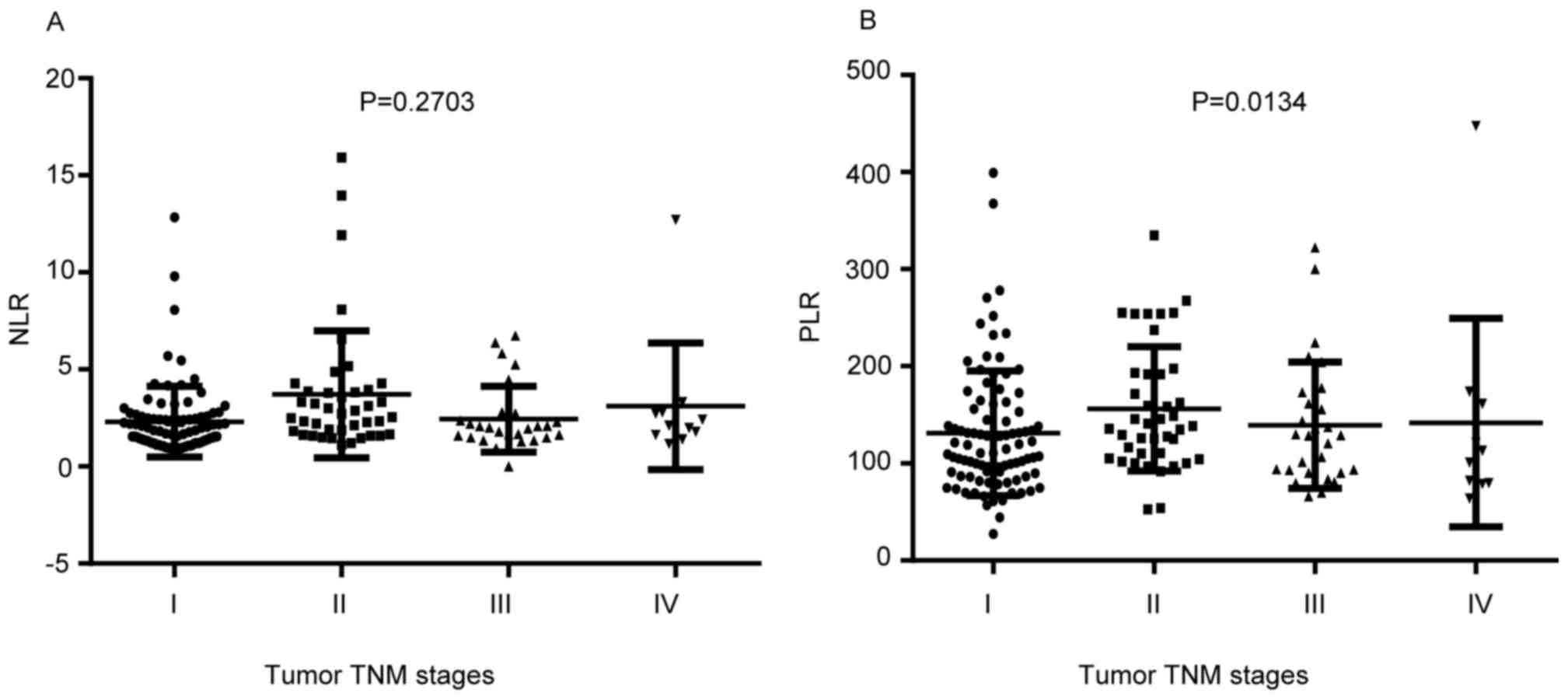
Association between NLR or PLR and TNM
stages in patients with NSCLC
In patients with NSCLC, there were significant
differences among the four stages in NLR and PLR (both P<0.01,
Fig. 3). Therefore, as demonstrated
in Table II and Fig. 3A, a significant increase in the NLR
was observed in patients with stage III or IV disease, compared
with those with stage I disease (both P<0.05). For the PLR
values, an increasing trend following the tumor stages was observed
(Fig. 3B). In comparison with stage
I, there was a significantly higher PLR value in stage II (Fig. 3B, P<0.05). Compared with the
control group, the levels of NLR and PLR were significantly raised
in patients with stage III or IV disease (all P<0.01; Table II). There was no detectable
interaction between stage I or II disease and either of these two
markers (all P>0.05; Table
II).
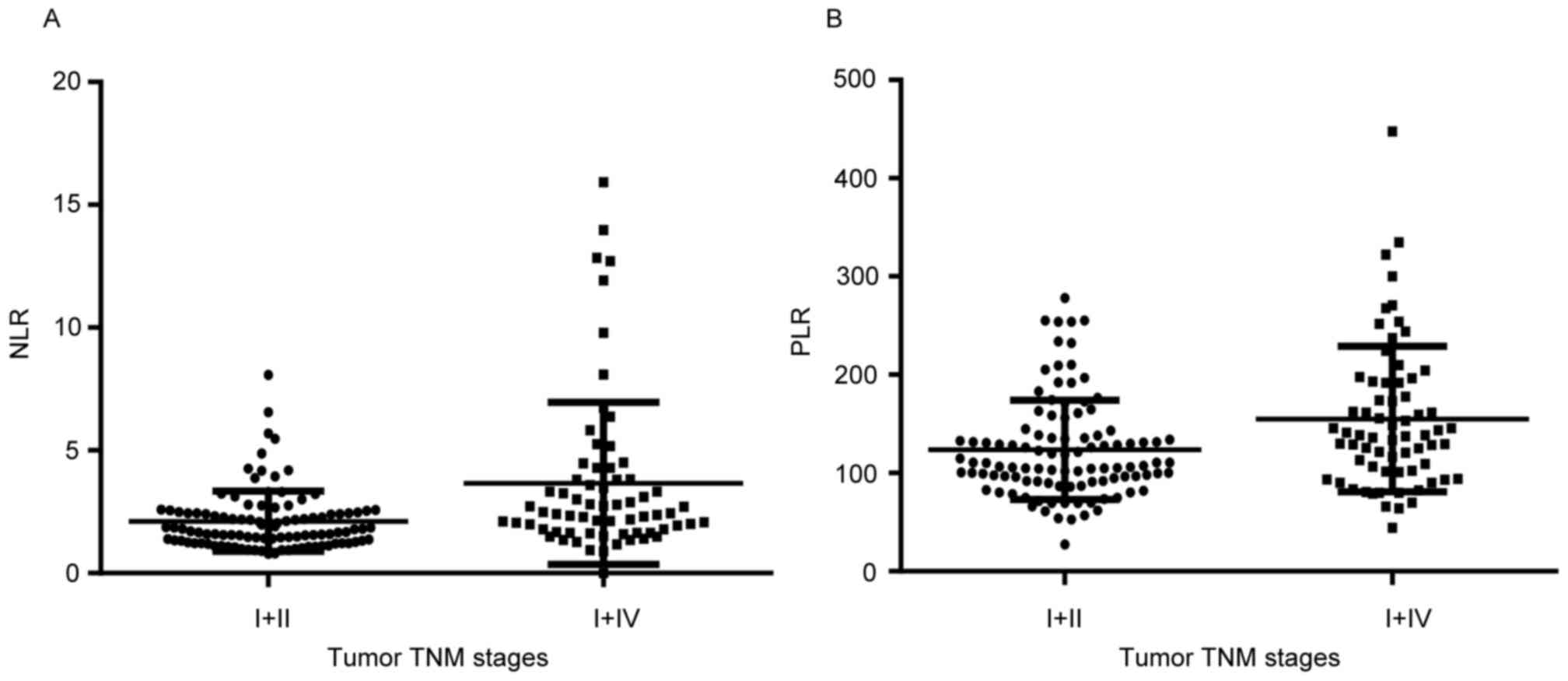
Evaluation of the diagnostic efficacy
for NLR and PLR
Table II demonstrates
that levels of NLR and PLR were higher in the patients with stage
III or IV disease, compared with the healthy controls (all
P<0.01). In addition, significant increases in NLR and PLR were
observed in patients with stage III/IV disease, compared with those
with stage I/II disease (NLR, 2.115±0.1207 vs. 3.657±0.4031;
P<0.0001; PLR, 123.6±4.961 vs. 154.9±9.025, P=0.0012,
respectively; Fig. 4. Notably, ROC
analysis revealed AUC values for NLR and PLR at 0.752 and 0.719
(Fig. 5), in identifying patients
with advanced-stage (III and IV) NSCLC.
Association between NLR or PLR and
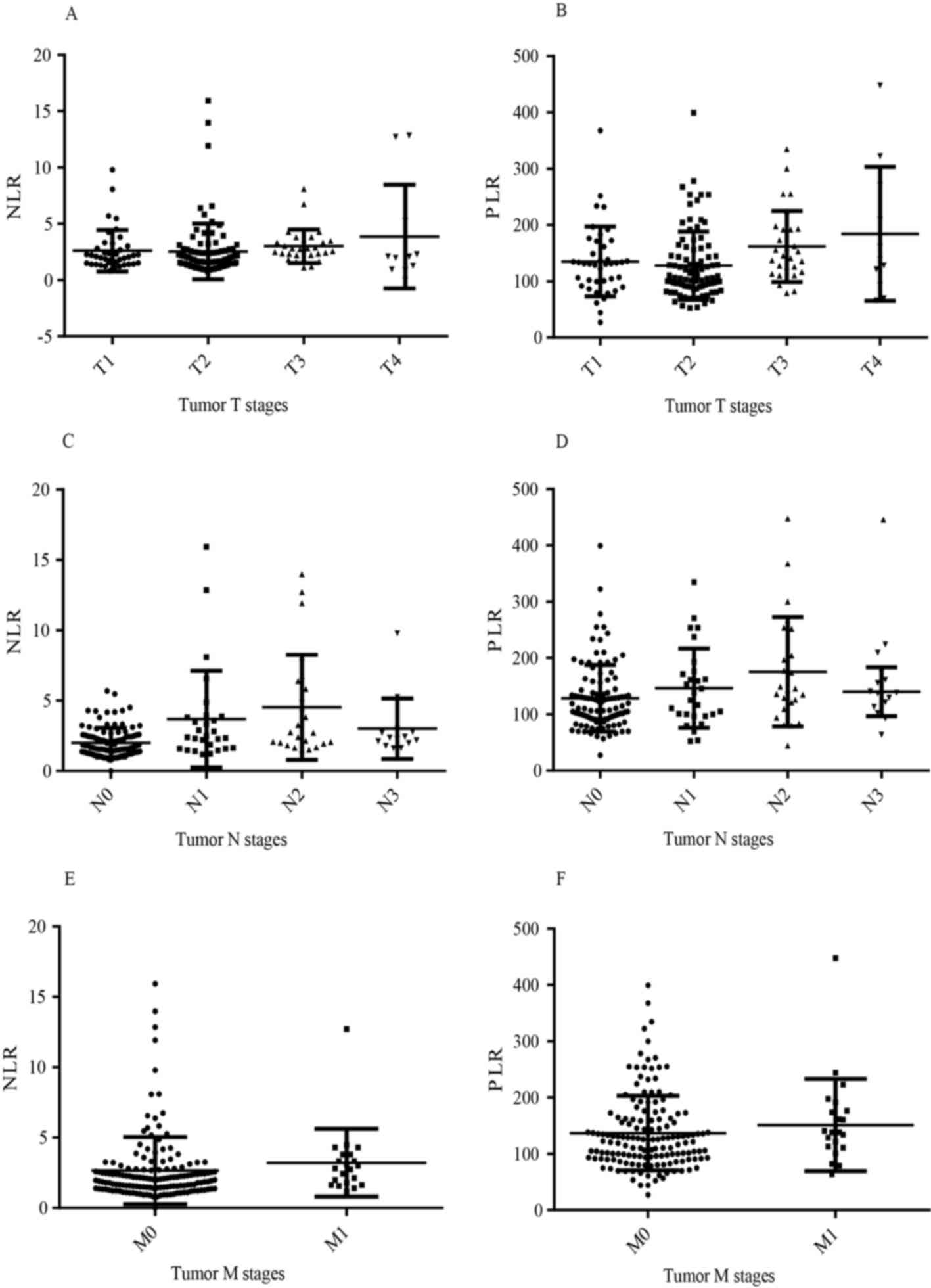
independent T, N and M stages in patients with NSCLC
Following the aforementioned results that NLR and
PLR are independently associated with TNM stages, the present study
further investigated whether NLR and PLR are independently
associated with T, N or M stages. As demonstrated in Fig. 6A-D, Kruskal-Wallis analysis revealed
an association between T stage and increased levels of PLR
(P<0.05), and NLR (P<0.0001) and PLR (P<0.05) exhibited an
N stage-dependent increase. There was an increasing tendency, but
not any significant association, between NLP or PLR and an M stage
of M1 (both P>0.05, Fig. 6E and
F).
Furthermore, multivariate linear regression (MLR)
analyses were employed to evaluate the association between NLR or
PLR and T or N stage. MLR detected significant associations between
PLR and T stage (P<0.0001), and between NLR and N stage
(P<0.0001). However, there was no significant association
between PLR and N stage (P=0.768).
Discussion
As stated previously, systemic inflammation serves a
critical role in the pathogenesis and progression of cancer
(23). As biomarkers of systemic
inflammation, NLR and PLR are known to be associated with the
progression of different types of cancer (22,24).
Notably, previous studies (20–22) have
focused on the prognostic role of inflammation. The present study
revealed that preoperative levels of NLR and PLR were generally
significantly associated with TNM stages. Compared with healthy
individuals, patients with NSCLC exhibited higher levels of NLR and
PLR. Furthermore, NLR was revealed to be significantly elevated
from stage III and IV while PLR was associated with a
stage-dependent increase from stage I to stage IV. Additionally,
PLR and NLR were independent predictors for T and N stage,
respectively. Taken together, the results of the present study
indicated that NLR and PLR were involved in different stages of
NSCLC and provided important information for advanced disease
stages, III and IV.
To the best of our knowledge, the present study was
the first to evaluate the association between these two parameters
and TNM stages in NSCLC. Accurate staging is not only prognostic,
but also helps determine the most appropriate treatment (25,26). To
date, TNM stages are determined depending on surgery, pathology,
computed tomography (CT) or positron emission tomography (PET)-CT
(27,28). At present, great progresses have been
made in investigating measures for novel predictive factors,
including genetic tests (29).
However, they are of high heterogeneity, and are complex and
expensive which limits their usage (30). NLR and PLR are fairly simple,
convenient and inexpensive as blood parameters for routine clinical
monitoring without specialized equipment (31). With regards to NLR and PLR, several
published studies have reported that they served reliable roles in
predicting and identifying cancer (24,32).
In line with the results of a previous study
(32,33), the present study detected that the
levels of NLR and PLR were higher in the lung cancer patient group
than in the control group, and that NLR and PLR served an important
role in the diagnosis of lung cancer. In addition, the results of
the present study indicated that these factors were associated with
advanced disease stages (stages III and IV), for which the AUC
values were 0.752 and 0.719, respectively, highlighting the precise
value of the two markers in the detection of NSCLC, particularly
for advanced NSCLC.
Furthermore, growing evidence has suggested an
association between inflammatory response and disease stage
(20,21,34,35).
Elevated preoperative NLR was associated with advanced TNM stage,
advanced T stage and lymph node metastasis (20,36).
Consistent with previous studies, the results of the present study
provided further evidence supporting the notion that NLR and PLR
were associated with advanced stages of NSCLC. Notably, the results
of the present study expanded on previous findings and revealed
that PLR and NLR were independent factors for T and N stage,
respectively, in MLR analyses (both P<0.0001), which was in
accordance with the results of a recent published study by Jia
et al (21). Other factors,
including NLR and different disease stages of the included
patients, may have influenced PLR, as there was no significant
difference between PLR and N stage in MLR analysis (P=0.768). In
line with the aforementioned results, a high PLR has been revealed
to be associated with advanced disease stages (37) and to be a complement of NLR (38).
Neutrophils and lymphocytes are predominant
proportions of total circulating leukocytes serving vital roles in
the systemic inflammatory response. They may inhibit or promote
cancer progression by regulating microenvironment immune
interactions. It is more emphasized now that routinely available
markers of the systemic inflammatory response, including the NLR
and PLR, are associated with tumor length, T stage, cancer
development and progression (16,24).
Patients with high NLR and PLR have neutrophilia and relative
lymphocytopenia, measurable in the peripheral blood (39). It is well known that T-lymphocytes are
important components mediating the immune response to cancer cells
(40). CD8+ T cells serve a
substantial role in inhibiting tumor growth by killing cytotoxic
cells and producing cytokine (41). A
relative lymphocytopenia is indicative of an immunosuppressive
status that inhibits proliferation and metastatic activity of tumor
cells (42). By contrast, an
increased level of neutrophils represents the host inflammation
status, which provides an appropriate environment for tumor growth
(43). Numerous lines of evidence
have indicated that cancer cells may induce platelet activation
and, in turn, that the activated platelets promote cancer cell
proliferation, angiogenesis and metastasis and protect tumor cells
from apoptosis (44,45). Additionally, platelets are associated
with cancer growth and progression (45). NLR and PLR are novel composite
inflammatory markers reflecting the immune status of an individual
(17,46). Furthermore, it is now indisputable
that NLR and PLR provide information regarding the activity of
tumor cells, and metastasis and invasion in patients, and that they
reflect the degree of cancer progression (22,24,32).
The present study has certain limitations. To begin
with, the sample size was relatively small. Additionally, it was a
retrospective and single-center study, with certain bias in
recruiting participants. Finally, due to the retrospective nature
of the study, it was not possible to control potential factors
affecting inflammatory response, including occult infection.
Therefore, it is necessary to further investigate the associations
between NLR or PLR and the TNM stages of NSCLC in a prospective,
large sample, multi-center study.
To conclude, the present study demonstrated that a
higher level of NLR and PLR was observed in patients with NSCLC,
compared with healthy controls, and that NLR and PLR served vital
roles in the early diagnosis of NSCLC, particularly for patients
with advanced stages of disease. Therefore, the results of the
present study have provided evidence that NLR and PLR were
significantly associated with TNM stages in NSCLC. In addition, PLR
and NLR may be potential and independent predictive markers for T
and N stage, respectively. These observations may provide insight
for clinical practice for the diagnosis of NSCLC and for
determining an appropriate treatment regimen.
Acknowledgements
The authors would like to thank Dr Zihui Tang for
providing statistical guidance.
Funding
The present study was supported by the Natural
Science Foundation of China (grant nos. 81673916 and 81403148) and
the Development Project of Shanghai Peak Disciplines-Integrative
Medicine (grant no. 20150407).
Availability of data and materials
The data analyzed during the current study are
available from the corresponding author on reasonable request.
Authors' contributions
FX, PX, BL and JD conceived and designed the study.
FX, WG and YW assisted in data collection and evaluation and
analyzed the data. FX and PX wrote the manuscript. BL and JD
revised the manuscript and supervised the project.
Ethics statement and consent to
participate
The present study was approved by the Ethics
Committee of Huashan Hospital, Fudan University. Written informed
consent was obtained from every participant according to the
institutional guidelines of Huashan Hospital, Fudan University when
they were enrolled.
Consent for publication
Written informed consent for publication was
obtained from every participant.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
TNM
|
Tumor-Node-Metastasis
|
|
NLR
|
neutrophil-to-lymphocyte ratio
|
|
PLR
|
platelet-to-lymphocyte ratio
|
References
|
1
|
Ferlay J, Soerjomataram I, Ervik M,
Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D and
Bray F: GLOBOÊN 2012 v1.0. Cancer Incidence and Mortality
Worldwide: IARC cancer base no. 11. 2016:http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspxNovember
12–2015
|
|
2
|
Fossella F, Pereira JR, von Pawel J,
Pluzanska A, Gorbounova V, Kaukel E, Mattson KV, Ramlau R, Szczesna
A, Fidias P, et al: Randomized, multinational, phase III study of
docetaxel plus platinum combinations versus vinorelbine plus
cisplatin for advanced non-small-cell lung cancer: The TAX 326
study group. J Clin Oncol. 21:3016–3024. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2015. CA Cancer J Clin. 65:5–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mccarthy N: A surprising competitor. Nat
Rev Cancer. 14:732014. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Park BJ and Rusch VW: Lung cancer workup
and stagingSellke FW, del Nido PJ and Swanson SJ: Surgery of the
chest. 7th ed. Philadelphia, PA: Elsevier; pp. 241–251. 2005
|
|
6
|
Andrade FM, Mourad OM and Judice LF: The
revised tumor-node-metastasis staging system for lung cancer:
Changes and perspectives. J Bras Pneumol. 36:617–620. 2010.(In
English, Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kucuk U, Pala EE, Sezer O, Cakir E, Bayol
U and Divrik RT: Significance of TNM staging, demographic and
histologic features in predicting the prognosis of renal cell
carcinoma. Acta Chir Belg. 115:202–207. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Costi R, Beggi F, Reggiani V, Riccò M,
Crafa P, Bersanelli M, Tartamella F, Violi V, Roncoroni L and Sarli
L: Lymph node ratio improves TNM and Astler-Coller's assessment of
colorectal cancer prognosis: An analysis of 761 node positive
cases. J Gastrointest Surg. 18:1824–1836. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Marquette D, Pichon E, Deschasse G,
Lemaire B, Lemarie E, Diot P and Marchand-Adam S: Lung cancer in
adults: Better prognosis of patients aged 45 and under related to
good condition and lower TNM stage (a comparative and retrospective
study). Presse Med. 41:e250–e256. 2012.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mantovani A: Cancer: Inflaming metastasis.
Nature. 457:36–37. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Faria SS, Fernandes PJ Jr, Silva MJ, Lima
VC, Fontes W, Freitas-Junior R, Eterovic AK and Forget P: The
neutrophil-to-lymphocyte ratio: A narrative review.
Ecancermedicalscience. 10:7022016.PubMed/NCBI
|
|
12
|
Marchioni M, Primiceri G, Ingrosso M,
Filograna R, Castellan P, De Francesco P and Schips L: The clinical
use of the neutrophil to lymphocyte ratio (NLR) in urothelial
cancer: A systematic review. Clin Genitourin Cancer. 14:473–484.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yodying H, Matsuda A, Miyashita M,
Matsumoto S, Sakurazawa N, Yamada M and Uchida E: Prognostic
significance of neutrophil-to-lymphocyte ratio and
platelet-to-lymphocyte ratio in oncologic outcomes of esophageal
cancer: A systematic review and meta-analysis. Ann Surg Oncol.
23:646–654. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kim JH, Lee JY, Kim HK, Lee JW, Jung SG,
Jung K, Kim SE, Moon W, Park MI and Park SJ: Prognostic
significance of the neutrophil-to-lymphocyte ratio and
platelet-to-lymphocyte ratio in patients with stage III and IV
colorectal cancer. World J Gastroenterol. 23:505–515. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sun X, Liu X, Liu J, Chen S, Xu D, Li W,
Zhan Y, Li Y, Chen Y and Zhou Z: Preoperative
neutrophil-to-lymphocyte ratio plus platelet-to-lymphocyte ratio in
predicting survival for patients with stage I–II gastric cancer.
Chin J Cancer. 35:572016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gu X, Gao X, Li X, Qi X, Ma M, Qin S, Yu
H, Sun S, Zhou D and Wang W: Prognostic significance of
neutrophil-to-lymphocyte ratio in prostate cancer: Evidence from
16,266 patients. Sci Rep. 6:220892016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Templeton AJ, McNamara MG, Šeruga B,
Vera-Badillo FE, Aneja P, Ocaña A, Leibowitz-Amit R, Sonpavde G,
Knox JJ, Tran B, et al: Prognostic role of neutrophil-to-lymphocyte
ratio in solid tumors: A systematic review and meta-analysis. J
Natl Cancer Inst. 106:dju1242014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Todoric J, Antonucci L and Karin M:
Targeting inflammation in cancer prevention and therapy. Cancer
Prev Res (Phila). 9:895–905. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Qi Q, Zhuang L, Shen Y, Geng Y, Yu S, Chen
H, Liu L, Meng Z, Wang P and Chen Z: A novel systemic inflammation
response index (SIRI) for predicting the survival of patients with
pancreatic cancer after chemotherapy. Cancer. 122:2158–2167. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gong W, Yang S, Yang X and Guo F: Blood
preoperative neutrophil-to-lymphocyte ratio is correlated with TNM
stage in patients with papillary thyroid cancer. Clinics (Sao
Paulo). 71:311–314. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Jia J, Zheng X, Chen Y, Wang L, Lin L, Ye
X, Chen Y, Chen D and Dettke M: Stage-dependent changes of
preoperative neutrophil to lymphocyte ratio and platelet to
lymphocyte ratio in colorectal cancer. Tumour Biol. 36:9319–9325.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Özgehan G, Kahramanca Ş, Kaya IO, Bilgen
K, Bostanci H, Güzel H, Küçükpinar T and Kargici H:
Neutrophil-lymphocyte ratio as a predictive factor for tumor
staging in colorectal cancer. Turk J Med Sci. 44:365–368. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shalapour S and Karin M: Immunity,
inflammation, and cancer: An eternal fight between good and evil. J
Clin Invest. 125:3347–3355. 2015. View
Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bar-Ad V, Palmer J, Li L, Lai Y, Lu B,
Myers RE, Ye Z, Axelrod R, Johnson JM, Werner-Wasik M, et al:
Neutrophil to lymphocyte ratio associated with prognosis of lung
cancer. Clin Transl Oncol. 19:711–717. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wang L, Liang D, Xu X, Jin J, Li S, Tian
G, Gao Z, Liu C and He Y: The prognostic value of neutrophil to
lymphocyte and platelet to lymphocyte ratios for patients with lung
cancer. Oncol Lett. 14:6449–6456. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Marijon H, Bouyon A, Vignot S and Besse B:
Prognostic and predictive factors in lung cancer. Bull Cancer.
96:391–404. 2009.(In French). PubMed/NCBI
|
|
27
|
Haberkorn U and Schoenberg SO: Imaging of
lung cancer with CT, MRT and PET. Lung Cancer. 34 Suppl 3:S13–S23.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Quint LE: Staging non-small cell lung
cancer. Cancer Imaging. 7:148–159. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Foulkes WD, Knoppers BM and Turnbull C:
Population genetic testing for cancer susceptibility: Founder
mutations to genomes. Nat Rev Clin Oncol. 13:41–54. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Afghahi A and Kurian AW: The changing
landscape of genetic testing for inherited breast cancer
predisposition. Curr Treat Options Oncol. 18:272017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Semeniuk-Wojtas A, Lubas A, Stec R, Syrylo
T, Niemczyk S and Szczylik C: Neutrophil-to-lymphocyte ratio,
platelet-to-lymphocyte ratio, and C-reactive protein as new and
simple prognostic factors in patients with metastatic renal cell
cancer treated with tyrosine kinase inhibitors: A systemic review
and meta-analysis. Clin Genitourin Cancer. Feb 2–2018.(Epub ahead
of print). View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Nikolić I, Kukulj S, Samaržija M, Jeleč V,
Žarak M, Orehovec B, Taradi I, Romić D, Kolak T and Patrlj L:
Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio help
identify patients with lung cancer, but do not differentiate
between lung cancer subtypes. Croat Med J. 57:287–292. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kemal Y, Yucel I, Ekiz K, Demirag G,
Yilmaz B, Teker F and Ozdemir M: Elevated serum neutrophil to
lymphocyte and platelet to lymphocyte ratios could be useful in
lung cancer diagnosis. Asian Pac J Cancer Prev. 15:2651–2654. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Celik O, Akand M, Keskin MZ, Yoldas M and
Ilbey YO: Preoperative neutrophil-to-lymphocyte ratio (NLR) may be
predictive of pathologic stage in patients with bladder cancer
larger than 3 cm. Eur Rev Med Pharmacol Sci. 20:652–656.
2016.PubMed/NCBI
|
|
35
|
Kim YW, Kim SK, Kim CS, Kim IY, Cho MY and
Kim NK: Association of serum and intratumoral cytokine profiles
with tumor stage and neutrophil lymphocyte ratio in colorectal
cancer. Anticancer Res. 34:3481–3487. 2014.PubMed/NCBI
|
|
36
|
Wang J, Jia Y, Wang N, Zhang X, Tan B,
Zhang G and Cheng Y: The clinical significance of
tumor-infiltrating neutrophils and neutrophil-to-CD8+ lymphocyte
ratio in patients with resectable esophageal squamous cell
carcinoma. J Transl Med. 12:72014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Xu Z and Xu W, Cheng H, Shen W, Ying J,
Cheng F and Xu W: The prognostic role of the platelet-lymphocytes
ratio in gastric cancer: A meta-analysis. PLoS One.
11:e1637192016.
|
|
38
|
Wu G, Yao Y, Bai C, Zeng J, Shi D, Gu X,
Shi X and Song Y: Combination of platelet to lymphocyte ratio and
neutrophil to lymphocyte ratio is a useful prognostic factor in
advanced non-small cell lung cancer patients. Thorac Cancer.
6:275–287. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Sun H, Hu P, Du J and Wang X: Predictive
value of inflammatory indexes on the chemotherapeutic response in
patients with unresectable lung cancer: A retrospective study.
Oncol Lett. 15:4017–4025. 2018.PubMed/NCBI
|
|
40
|
Chae YK, Galvez C, Anker JF, Iams WT and
Bhave M: Cancer immunotherapy in a neglected population: The
current use and future of T-cell-mediated checkpoint inhibitors in
organ transplant patients. Cancer Treat Rev. 63:116–121. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Durgeau A, Virk Y, Corgnac S and
Mami-Chouaib F: Recent advances in targeting CD8 T-Cell immunity
for more effective cancer immunotherapy. Front Immunol. 9:142018.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Wu ES, Oduyebo T, Cobb LP, Cholakian D,
Kong X, Fader AN, Levinson KL, Tanner EJ III, Stone RL, Piotrowski
A, et al: Lymphopenia and its association with survival in patients
with locally advanced cervical cancer. Gynecol Oncol. 140:76–82.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Hwang JE, Kim HN, Kim DE, Choi HJ, Jung
SH, Shim HJ, Bae WK, Hwang EC, Cho SH and Chung IJ: Prognostic
significance of a systemic inflammatory response in patients
receiving first-line palliative chemotherapy for recurred or
metastatic gastric cancer. BMC Cancer. 11:4892011. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
van Es N, Sturk A, Middeldorp S and
Nieuwland R: Effects of cancer on platelets. Semin Oncol.
41:311–318. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Li N: Platelets in cancer metastasis: To
help the ‘villain’ to do evil. Int J Cancer. 138:2078–2087. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Templeton AJ, Ace O, McNamara MG,
Al-Mubarak M, Vera-Badillo FE, Hermanns T, Seruga B, Ocaña A,
Tannock IF and Amir E: Prognostic role of platelet to lymphocyte
ratio in solid tumors: A systematic review and meta-analysis.
Cancer Epidemiol Biomarkers Prev. 23:1204–1212. 2014. View Article : Google Scholar : PubMed/NCBI
|