Introduction
The extracellular matrix (ECM) is a complex meshwork
of proteins and carbohydrate polymers, which are secreted,
surrounded and anchored by cells of connective tissues. Modulation
of the ECM is important in the development and progression of
malignancy. Matrix metalloproteinases (MMPs) and the natural tissue
inhibitors of metalloproteinases (TIMPs) act synergistically to
regulate ECM turnover. Expression of MMPs and TIMPs is involved in
several key aspects of tumor growth, invasion and metastasis
(1,2).
It is hypothesized that MMPs may be associated with the level of
invasion and progression in endometrioid-type carcinoma.
MMP11, a member of the MMP family, is able to
degrade ECM components, and may serve functions in angiogenesis,
cell migration, proliferation, apoptosis and connective tissue
degradation. MMP11 is processed intracellularly and is secreted in
its active form, thus MMP11 differs from other MMPs that are
expressed as proenzymes and processed to active forms through
proteolytic cleavage activated extracellularly. This indicates that
MMPs may possess a unique function in tumor development and
progression; however, MMP11 is unable to degrade major ECM
components (3–7).
Endometrial carcinoma (EC) is the most common
malignancy of the female genital tract. It is estimated that there
are ~200,000 cases diagnosed worldwide annually, and that ~50,000
women will succumb to the disease. Despite the recognition of
several different histological subtypes of EC, these are commonly
explained using a dualistic model, which categorizes carcinomas
into two major types: Type I and type II. Type I (endometrioid)
comprises the vast majority of EC cases, as well as its
histological variants due to the histological similarity with
normal endometrial glands. Type I present precursor lesions
including glandular hyperplasia and are associated with
hyperestrogenism, which is defined by high levels of estrogenic
hormones. The mutations are located primarily in phosphatase and
tensin homolog, β catenin, MutL homolog (MLH)-1 and MLH-6 genes
(8,9).
Furthermore, patients with type I EC have more favorable prognosis
factors compared with type II EC (8–12). Several
risk factors have been previously associated with type I EC
including obesity and the use of estrogen therapies, which are
associated with an imbalance between estrogen and progesterone.
Combination therapy of oral contraceptives, which are associated
with predominant states of progesterone, decreases the risk of EC
(9,13–17). Other
risk factors include nulliparity, early menarche and late menopause
(9). A previous study investigating
the expression of MMP1 and MMP2 in EC demonstrated that these
biomarkers are associated with poor survival (18). Type II EC are high-grade carcinomas
that cannot be graduated and exhibit a poor prognosis; however,
these were not included in the present study owing to their
behavior, spreading through the serous, having a high stage at the
time of presentation and a poor prognostic.
In the present study, the expression levels of
MMP11 were measured using the reverse
transcription-polymerase chain reaction (RT-PCR) in 68 cases of
type I EC and associated with clinical pathological parameters
including histological grade (G1-G3), vascular invasion [verified
with D240 immunohistochemical (IHC) staining and cluster of
differentiation (CD)31], pathological tumor stage (pT1a/1b/2/3),
disease recurrence, and mortality. The present study verified
expression levels of hormone receptors (estrogen and progesterone
receptors) and cell proliferation index using IHC staining, and
associated gene expression and pathological parameters with overall
prognosis. To the best of our knowledge, there are no previous
studies, which have investigated gene association in patients with
type I EC. The expression of MMP11 at the protein level using IHC
was not performed due to limited sample availability.
Materials and methods
Ethical approval and consent to
participate
The ethics committee of the University Hospital of
the Autonomous University of Nuevo León (Monterrey, Mexico)
approved the present study. The requirement for consent to
participate was not applicable.
Samples and histopathological
analysis
In total, 68 cases of type I EC were obtained from
the archives of the Pathology Department of the University Hospital
of the Autonomous University of Nuevo León during a 5-year period
(January 2009 to December 2014). In total, 21 cases (30.8%) had
endometrial tissue adjacent to the tumor, which was included as an
internal control for the present study. In total, 20 control cases
of proliferative and secretory endometrium were included. EC cases
were assessed to verify type, histological grade (G1, well
differentiated; G2, moderately differentiated; G3, poorly
differentiated) and pT stage (pT1a, pT1b, pT2 and pT3a) according
to the College of American Pathologists and the International
Federation of Gynecology and Obstetrics. In each case, associated
clinical pathological data were obtained and analyzed.
IHC analysis
Fixation took place in 10% neutral buffered formalin
(NBF). The most representative tumor areas were selected and
3-µm-thick sections were produced. The sections were deparaffinized
through 3 10 min washes in xylene (98.3%) at room temperature,
rehydrated in a descending alcohol series (100, 95, 70 and 50%
ethanol, and finally PBS for 5 min) followed by microwave epitope
retrieval [750 W for 7.5 min and 500 W for 5 min (×4) in citrate
buffer (pH 6); Thermo Fisher Scientific, Inc., Waltham, MA, USA].
Endogenous peroxidase activity was blocked by incubation with 1%
hydrogen peroxide in methanol for 30 min before incubation for 1 h
(room temperature) with the polyclonal antibodies against estrogen
receptor α (ERα; clone 1D5 M704), progesterone receptor (PR; clone
PgR 636), Ki67 (clone A047), D240 (clone D2-40) and CD31 (clone
JC70A). The sections were stained according to the standard
avidin-biotin method from the manufacturer, for 30 min at room
temperature (Dako; Agilent Technologies, Inc., Santa Clara, CA,
USA) and counterstained with Harris hematoxylin (100%). All
antibodies were purchased from Dako; Agilent Technologies, Inc.
Tissue microarray slides were evaluated in a standard light
microscope (magnification, ×100) for immunohistochemical
staining.
IHC expression
Positive and negative controls for each marker were
included on each slide. Positivity indicated that >10% of cells
demonstrated nuclear positivity for ER and PR, and an index of high
proliferation was considered when >5% of cells demonstrated
nuclear positivity for Ki67. Furthermore, D240 and CD31 staining
was used to confirm the angiolymphatic invasion observed
histopathologically. Although no gold standard for identifying
angiolymphatic invasion exists, the presence of tumor cells within
a vascular space, red blood cells surrounding the tumor cells,
identification of endothelial lining of the space, a presence of an
elastic lamina surrounding the tumor and tumor cells attached to
the vascular wall may be beneficial data for the identification of
vascular invasion in the histological sections stained with
hematoxylin and eosin (H&E). The immunohistochemical stains for
CD31 and D2-40 were used to assist in the detection of
angiolymphatic invasion (Table
I).
 | Table I.Clinical and pathological parameters
of cases (n=68). |
Table I.
Clinical and pathological parameters
of cases (n=68).
| Variable | Frequency | Percentage |
|---|
| Grade |
|
|
| G1 | 3 | 4.4 |
| G2 | 57 | 83.8 |
| G3 | 8 | 11.7 |
| Vascular
invasiona |
|
|
|
Present | 43 | 63.2 |
|
Absent | 25 | 36.7 |
| pT stage |
|
|
|
pT1a | 38 | 55.8 |
|
pT1b | 19 | 27.9 |
|
pT2 | 4 | 5.7 |
|
pT3a | 7 | 10.2 |
| Lymph node
dissection |
|
|
|
Performed | 37 | 54.4b |
| Not
performed | 31 |
45.5 |
| Adjuvant
therapy |
|
|
|
Administered | 43 | 63.2 |
| Not
administered | 25 | 36.7 |
| Recurrence |
|
|
|
Present | 5 | 7.3 |
|
Absent | 63 | 92.6 |
|
Mortality | 3 | 4.4 |
RNA extraction and quantification
Macrodissections of the most representative areas of
EC tumor cases were performed and total RNA was obtained using an
All Prep DNA/RNA formalin-fixed paraffin-embedded kit (Qiagen,
Inc., Valencia, CA, USA), according to the manufacturer's protocol.
RNA was quantified and qualified using a NanoDrop 200
spectrophotometer (Thermo Fisher Scientific, Inc.).
Expression levels of MMP11 using
RT-PCR
To detect expression levels of MMP11 in
endometrial tissues, samples were analyzed using RT-PCR. For
relative quantification, RT was performed using
SuperScript® VILO™ cDNA Master Mix (Thermo Fisher
Scientific, Inc.) in the Verity Thermal Cycler (Applied Biosystems;
Thermo Fisher Scientific, Inc.) using 2 µg total RNA for cDNA
synthesis for 10 min at 25°C followed by an enzyme inactivation
step of 5 min at 85°C.
Expression levels were quantified using the
2−ΔΔCq method and normalized to the internal reference
gene β-actin (19). RT-PCRs were
performed using 2X TaqMan Universal Master Mix with
uracil-N-glycosylase (Applied Biosystems; Thermo Fisher Scientific,
Inc.) in the StepOnePlus™ RT-PCR system (Applied Biosystems; Thermo
Fisher Scientific, Inc.) with 250 ng cDNA using thermocycling
conditions outlined by the manufacturer's protocol, using TaqMan
probes (40 cycles of 15 sec at 95°C with an extension at 60°C for 1
min). To detect fluorescent signals, the pre-developed TaqMan Gene
Expression assay Hs00968295_m1 for MMP11 was used, and
Hs99999903_m1 for β-actin was utilized as an internal control
(forward, 5′-GTGGGCCGCTCTAGGCACCAA-3′, reverse,
3′-CTCTTTGATGTCACGCACGATTTC-5′, belong to Applied Biosystems;
Thermo Fisher Scientific, Inc.). RT-PCR was performed in
independent replicates. Two biological replicates for each sample
were used for RT-PCR analysis and three technical replicates were
analyzed for each biological replicate. A value of >1 was
considered as overexpression, and <1 was considered as
sub-expression, according to the standard value on control
secretory endometrium (the endometrial cycle has two secretory and
proliferative phases, which were used as controls). To analyze the
gene expression stability, geNORM v3.4 software (Genome Biology,
London, UK) was used.
Statistical analysis
An analysis of the possible association between
patterns of MMP11 expression and clinical pathological variables
including age, histological grade, pathological stage, vascular
invasion, recurrence and mortality, as well as expression levels of
hormone receptors (ER/PR) and Ki67, were performed using the
χ2 test. P<0.05 was considered to indicate a
statistically significant difference. Receiver operating
characteristic analysis was used to validate the overexpression of
MMP11 at a specificity of 0.49 with a confidence interval of
0.33–0.64, and sensibility of 0.75 with a confidence interval of
0.65–0.85.
Results
Clinical-pathological parameters
The mean age of patients with EC was 55 years
(range, 33–82 years). Histological grades for type I EC included G2
(83.8%) followed by G3 (11.7%) and G1 (4.4%). Angiolymphatic
(vascular) invasion was present in 63.2% of cases (Table I). Invasion in histological H&E
sections was investigated and analyzed for association with CD31
and D240 staining. No false positives or false negatives were
observed (Table I). The majority of
patients with angiolymphatic invasion demonstrated overexpression
(70.6%), and presented G2 staging in 87% of cases and stages pT1b,
2 and 3a in >90% of cases. With regard to the pathological
stage, the majority of cases were localized (stage 1A and B;
83.8%), no patient presented at stage IV. Patients underwent pelvic
lymph node dissection in 54% of cases and 8% demonstrated lymph
node metastases. In total, 63% of patients with EC received
adjuvant therapy (radiotherapy and chemotherapy) and disease
recurrence occurred in 7% of cases, all of which were localized at
the vaginal vault level. Within the first 2 years of surgery, 3
patients who had presented at advanced-stage at the time of
diagnosis had succumbed to the disease. Clinical pathological data
are presented in Table I.
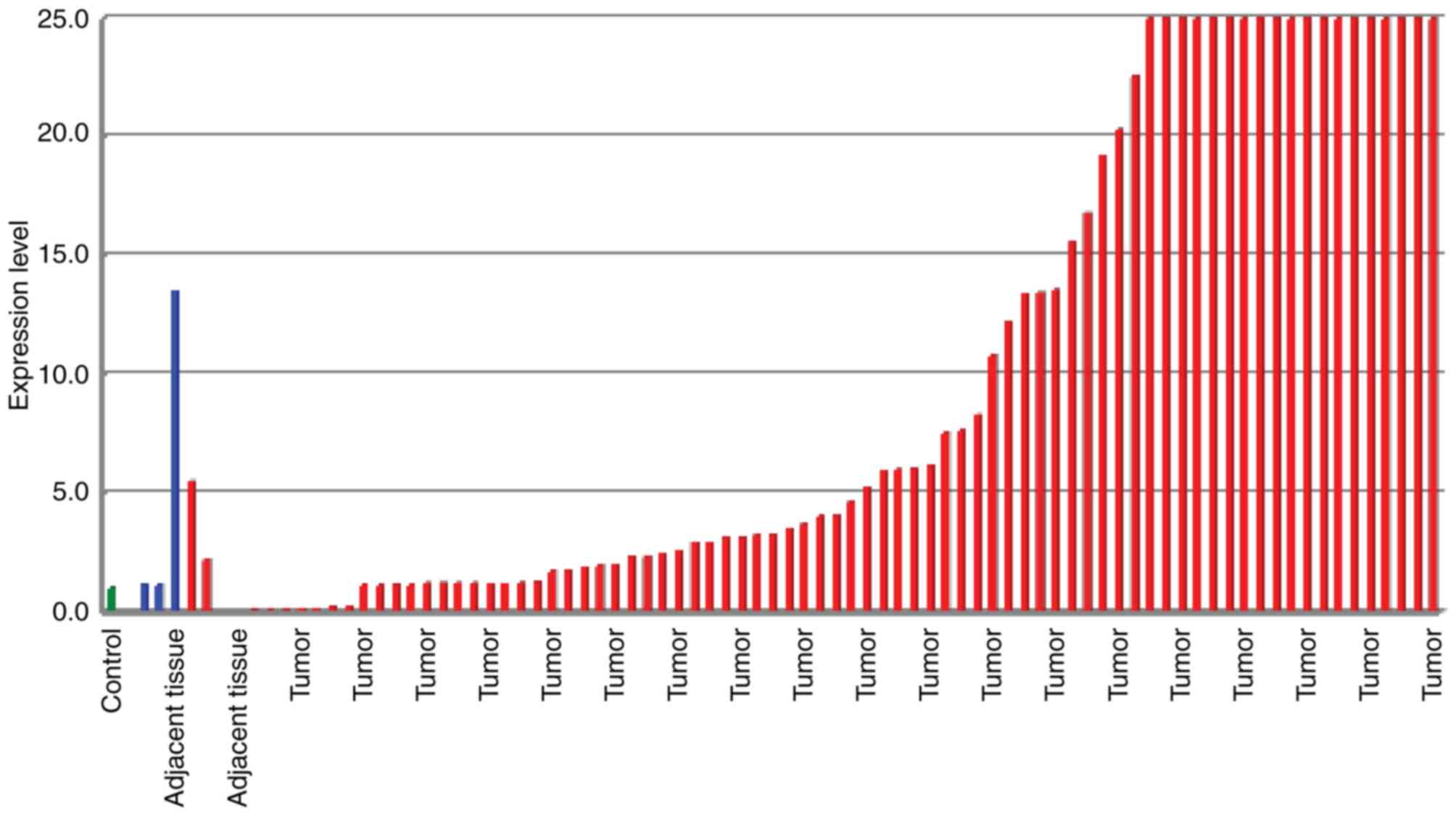
Expression levels of MMP11
MMP11 was overexpressed in 75% (n=51), and
sub-expressed in 25% (n=17) of EC cases. Levels of overexpression
ranged between 1.1- and 600-fold (Fig.
1). Cases with sub-expression were primarily associated with G1
(well-differentiated) followed by G2 (moderately differentiated);
however, all G3 (poorly differentiated) cases demonstrated
overexpression, and the remainder G2 cases were overexpressed. In
76.4% of cases with sub-expression, early pT stages (1A and B) were
demonstrated, and 23.6% presented at stage 2. The remaining
early-stage cases (23.6%), 76.4% of stage 2 cases and all stage 3
cases were overexpressed. In total, 29.4% of cases with
sub-expression demonstrated vascular invasion. Internal controls
with endometrium adjacent to the tumor demonstrated overexpression
in 66.6% with expression levels ranging between 1.1- and 3.5-fold,
and 33.4% with sub-expression of the gene MMP11 (Fig. 1).
Statistical analysis
No statistically significant association between
MMP11 expression and age, nuclear grade, adjuvant therapy,
recurrence or mortality was identified. However, pT pathological
stage and vascular invasion demonstrated a statistically
significant association with gene expression (P=0.03 and 0.01,
respectively; Table II).
 | Table II.Clinical and pathological parameters,
hormone receptors and Ki67 associated with matrix metalloproteinase
11 expression. |
Table II.
Clinical and pathological parameters,
hormone receptors and Ki67 associated with matrix metalloproteinase
11 expression.
| Variable | P-value |
|---|
| Age | 0.12 |
| Nuclear grade | 0.13 |
| pT pathological
stage | 0.03 |
| Metastatic lymph
nodes | 0.21 |
| Angiolymphatic
invasion | 0.01 |
| Adjuvant
therapy | 0.20 |
| Recurrence | 0.43 |
| Mortality owing to
disease | 0.75 |
| α-Estrogen
receptors | 0.25 |
| Progesterone
receptors | 0.20 |
| Ki67 | 0.04 |
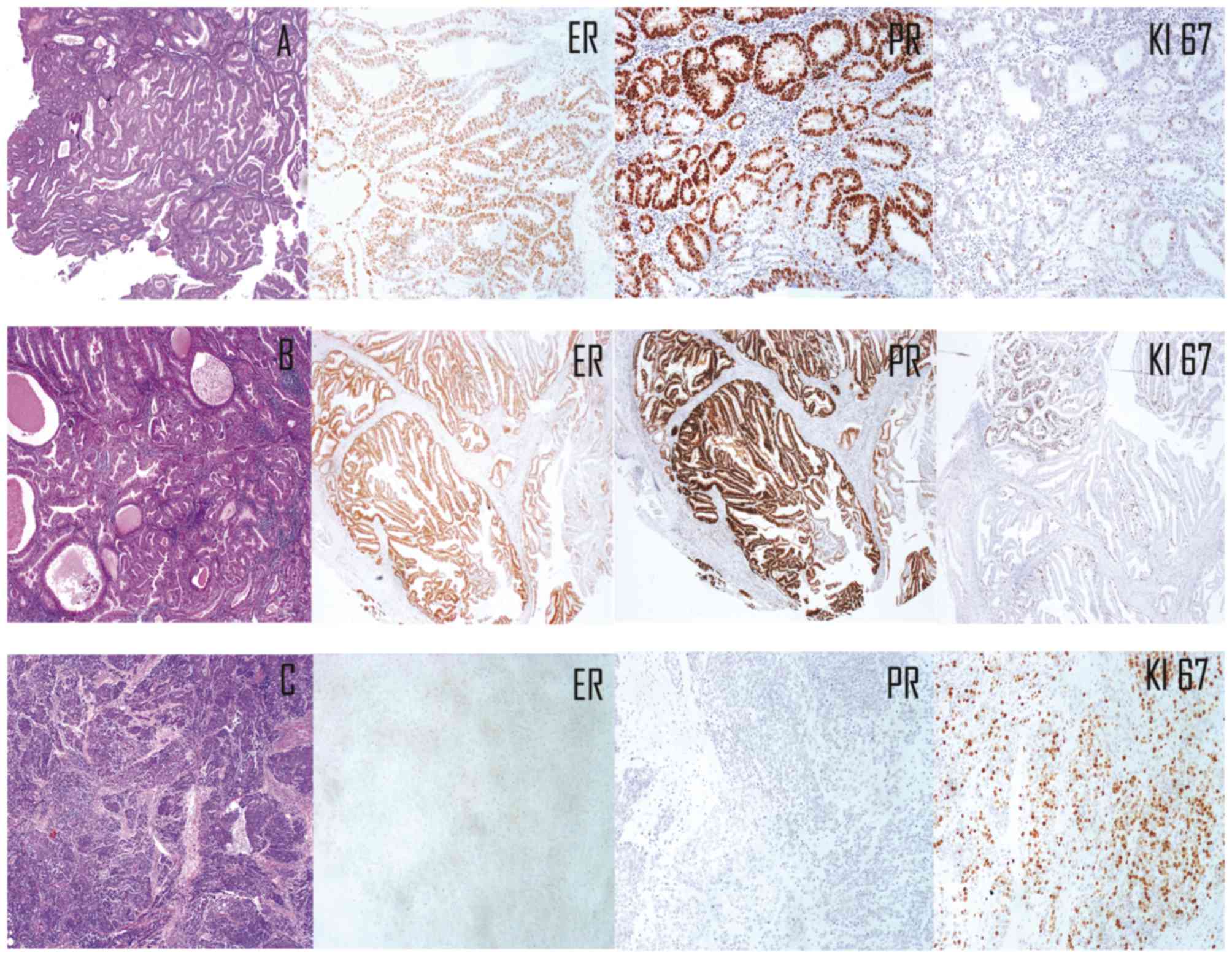
IHC expression
The ERα IHC stain was positive in 80.8% of cases,
and associated with histological grades 1 and 2 (92.7%). The PR IHQ
stain was expressed in 76.4% of cases; increased proportions of PR
were associated with low histological grades (92.4%) and early
pathological stages (90.5%). The rate of cell proliferation
determined using immunohistochemical staining with Ki67 was
increased in 45 (66%) of cases and decreased in 23 (44%) of cases;
95.6% of the latter demonstrated low nuclear grades (1 and 2), and
all cases presented at stages 1A and A (Fig. 2). Hormone receptors were not
statistically significant factors (P=0.25 and 0.20 for ER and PR,
respectively); however, the cell proliferation index of Ki67 was
significant (P=0.04; Table II).
Discussion
The expression of MMP in EC has been
previously studied; among these types 1, 2, 7 and 9 demonstrated
overexpression and were associated with a poor prognosis (19–28). MMP14
has been associated with increased myometrial and lymph node
invasion; however, the study was limited to a small number of cases
(26). Previous studies regarding
carcinomas within the biliary tract, oral cavity, thyroid and colon
demonstrated an association between MMP11 overexpression and
a poorer prognosis (27–29). In the present study, overexpression of
MMP11 ranging between 1.1- and 600-fold normal values was
demonstrated and was identified to be associated with adverse
histopathological characteristics including high nuclear grade,
advanced stages, angiolymphatic invasion, recurrence and mortality;
in contrast, cases with sub-expression which represented the total
number of cases with well-differentiated and moderately
differentiated histological grades presented at an early stage in
the disease process.
In the present study, the majority of the cases
(83.8%) were represented by a moderately differentiated
histological grade (G2), and were diagnosed in the early stages
pT1a and pT1b (83.7%), which coincides with results reported in
previous literature (30–33). This is a limitation of the present
study because of the low percentage of carcinomas that are well and
poorly differentiated, as well as a low number of late stages.
Furthermore, previous studies investigating cancer
cell lines associated with hormones, including breast, ovarian and
prostate carcinoma, demonstrated an association between
overexpression of MMPs and increased proliferation and invasion of
carcinogenic cells (34). In the
present study, the expression of hormone receptors (ERα and PR) was
evaluated in cases with type I EC (endometrioid and variants).
Cases with an increased percentage of positivity of hormone
receptors (ER and PR; >70%) were associated with fewer adverse
histopathological features when compared with cases that
demonstrated negativity or sub-expression of these receptors.
Previous studies have attempted to identify MMP11 as
a potential predictive tumor biomarker in patients with gastric
carcinoma; results demonstrated a significant increase in the serum
levels in these patients, thus proposing it as a biomarker for
diagnosing certain types of carcinomas. The results of the present
study suggest that EC may be included, once data are validated, as
the results in the present study are in agreement with those of a
previous study in terms of progression and prognosis (35).
However, to the best of our knowledge, there have
been no previous studies, which associated the cell proliferation
index with the expression of MMPs. In the present study, the rate
of proliferation was determined using Ki67 staining, in which an
increased rate of proliferation was identified to be associated
with adverse histopathological parameters, increased levels of
MMP11 expression (P=0.04), vascular invasion and
pathological staging. This supports the hypothesis that MMPs are
associated with the level of invasion and progression in
endometrioid-type carcinoma.
Despite previous evidence demonstrating that
MMP11 overexpression is a potential biomarker in this type
of neoplasia, a key limitation to the present study is the relative
lack of IHC analysis. It is recommended that future studies
increase the number of cases and perform MMP11 protein IHC analysis
in tissue microarrays to corroborate MMP11 overexpression as
a biomarker.
To conclude, the increased MMP11 expression
in type I EC is associated with a poor prognosis. Overexpression
may be used as a prognostic biomarker in patients with type I EC;
however, studies with a larger sample size are required to support
this hypothesis.
Acknowledgements
The authors would like to thank Dr Ricardo Cerda
Flores for providing support with statistical analysis. The present
study was supported by the Department of Pathology and
Cytopathology of the University Hospital of the Autonomous
University of Nuevo León (Monterrey, Mexico).
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GSGM, MLGR and DMO were responsible for the
conception and design of the study, and the acquisition, analysis
and interpretation of data. RGG, JAR, OBQ and HABS made substantial
contributions to conception and design and acquisition of data.
They were involved in revising it critically for intellectual
content and final approval of the version to be published.
Ethics approval and consent to
participate
The present study was approved by the ethics
committee of the University Hospital of the Autonomous University
of Nuevo León (approval no. AP 14-001).
Consent for publication
Not applicable for this manuscript.
Completing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
MMP
|
matrix metalloproteinase
|
|
RT-PCR
|
reverse transcription-polymerase chain
reaction
|
|
ECM
|
extracellular matrix
|
|
TIMP
|
tissue inhibitor of
metalloproteinases
|
|
ERα
|
estrogen receptor α
|
|
PR
|
progesterone receptor
|
References
|
1
|
Yan C and Boyd DD: Metalloproteinase gene
expression. J Cell Physiol. 211:19–26. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Roycik MD, Fang X and Sang OX: A fresh
prospect of extracellular hydrolytic enzymes and their substrates.
Curr Pharm Des. 15:1295–1308. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Murphy G and Nagase H: Progress in matrix
metalloproteinase research. Mol Aspects Med. 29:290–308. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Obokata A, Watanabe J, Nishimura Y, Arai
T, Kawaguchi M and Kuramoto H: Significance of matrix
metalloproteinase-7 [correction of matrix metalloproteinase-2], −11
and tissue inhibitor of metalloproteinase-1 expression in normal,
hyperplastic and neoplastic endometrium. Anticancer Res. 27:95–105.
2007.PubMed/NCBI
|
|
5
|
Mueller J, Brebeck B, Schmalfeldt B, Kuhn
W, Graeff H and Höfler H: Stromelysin-3 expression in invasive
ovarian carcinomas and tumors of low malignant potential. Virchows
Arch. 437:618–624. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Docherty AJ, Lyons A, Smith BJ, Wright EM,
Stephens PE, Harris TJ, Murphy G and Reynolds JJ: Sequence of human
tissue inhibitor of metalloproteinase and its identity to
erythroid-potentiating activity. Nature. 318:66–69. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hampton AL and Salamonen LA: Expression of
messenger ribonucleic acid encoding matrix metalloproteinases and
their tissue inhibitors is related to menstruation. J Endocrinol.
141:R1–R3. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Azueta A, Gatius S and Matias-Guiu X:
Endometrioid carcinoma of the endometrium: Pathologic and molecular
features. Semin Diagn Pathol. 27:226–240. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Felix AS, Weissfeld JL, Stone RA, Bowser
R, Chivukula M, Edwards RP and Linkov F: Factors associated with
type I and type II endometrial cancer. Cancer Causes Control.
21:1851–1856. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stoian SC, Simionescu C, Mărgăritescu C,
Stepan A and Nurciu M: Endometrial carcinomas: Correlation between
ER, PR, Ki67 status and histopathological prognostic parameters.
Rom J Morphol Embryol. 52:631–636. 2011.PubMed/NCBI
|
|
11
|
Gottwald L, Kubiak R, Sek P, Piekarski J,
Szwalski J, Pasz-Walczak G, Spych M, Suzin J, Tylińskis W and
Jeziorski A: The value of Ki-67 antigen expression in tissue
microarray method in prediction prognosis of patients with
endometrioid endometrial cancer. Ginekol Pol. 84:444–449. 2013.(In
Polish). View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Urabe R, Hachisuga T, Kurita T, Kagami S,
Kawagoe T, Matsuura Y and Shimajiri S: Prognostic significance of
overexpression of p53 in uterine endometrioid adenocarcinomas with
an analysis of nuclear grade. J Obstet Gynaecol Res. 40:812–819.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cancer Genome Atlas Research Network, .
Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y, Shen H,
Robertson AG, Pashtan I, Shen R, et al: Integrated genomic
characterization of endometrial carcinoma. Nature. 497:67–73. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
McCullough ML, Patel AV, Patel R,
Rodriguez C, Feigelson HS, Bandera EV, Gansler T, Thun MJ and Calle
EE: Body mass and endometrial cancer risk by hormone replacement
therapy and cancer subtype. Cancer Epidemiol Biomarkers Prev.
17:73–79. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sherman ME, Sturgeon S, Brinton LA,
Potischman N, Kurman RJ, Berman ML, Mortel R, Twiggs LB, Barrett
RJ, Wilbanks GD, et al: Risk factors and hormone levels in patients
with serous and endometrioid uterine carcinomas. Mod Pathol.
10:963–968. 1997.PubMed/NCBI
|
|
16
|
Uccella S, Mariani A, Wang AH, Vierkant
RA, Robien K, Anderson KE and Cerhan JR: Dietary and supplemental
intake of one-carbon nutrients and the risk of type I and type II
endometrial cancer: A prospective cohort study. Ann Oncol.
22:2129–2136. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yang HP, Wentzensen N, Trabert B, Gierach
GL, Felix AS, Gunter MJ, Hollenbeck A, Park Y, Sherman ME and
Brinton LA: Endometrial cancer risk factors by 2 main histologic
subtypes: The NIH-AARP Diet and Health Study. Am J Epidemiol.
177:142–151. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Honkavuori-Toivola M, Santala M, Soini Y,
Turpeenniemi-Hujanen T and Talvensaari-Mattila A: Combination of
strong MMP-2 and weak TIMP-2 immunostainings is a significant
prognostic factor in endometrial carcinoma. Dis Markers.
35:261–266. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Guo W, Chen G, Zhu C and Wang H:
Expression of matrix metalloproteinase-2, 9 and its tissue
inhibitor-1, 2 in endometrial carcinoma. Zhonghua Fu Chan Ke Za
Zhi. 37:604–607. 2002.(In Chinese). PubMed/NCBI
|
|
20
|
Karahan N, Güney M, Baspinar S, Oral B,
Kapucuoglu N and Mungan T: Expression of gelatinase (MMP-2 and
MMP-9) and cyclooxygenase-2 (COX-2) in endometrial carcinoma. Eur J
Gynaecol Oncol. 28:184–188. 2007.PubMed/NCBI
|
|
21
|
Honkavuori M, Talvensaari-Mattila A, Soini
Y, Turpeenniemi-Hujanen T and Santala M: MMP-2 expression
associates with CA 125 and clinical course in endometrial
carcinoma. Gynecol Oncol. 104:217–221. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Talvensaari-Mattila A, Santala M, Soini Y
and Turpeenniemi-Hujanen T: Prognostic value of matrix
etalloproteinase-2 (MMP-2) expression in endometrial endometrioid
adenocarcinoma. Anticancer Res. 25:4101–4105. 2005.PubMed/NCBI
|
|
23
|
Graesslin O, Cortez A, Uzan C, Birembaut
P, Quereux C and Daraï E: Endometrial tumor invasiveness is related
to metalloproteinase 2 and tissue inhibitor of metalloproteinase 2
expressions. Int J Gynecol Cancer. 16:1911–1917. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Graesslin O, Cortez A, Fauvet R, Lorenzato
M, Birembaut P and Daraï E: Metalloproteinase-2, −7 and −9 and
tissue inhibitor of metalloproteinase-1 and −2 expression in
normal, hyperplastic and neoplastic endometrium: A
clinical-pathological correlation study. Ann Oncol. 17:637–645.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Aglund K, Rauvala M, Puistola U, Angström
T, Turpeenniemi-Hujanen T, Zackrisson B and Stendahl U: Gelatinases
A and B (MMP-2 and MMP-9) in endometrial cancer-MMP-9 correlates to
the grade and the stage. Gynecol Oncol. 94:699–704. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Di Nezza LA, Misajon A, Zhang J, Jobling
T, Quinn MA, Ostör AG, Nie G, Lopata A and Salamonsen LA: Presence
of active gelatinases in endometrial carcinoma and correlation of
matrix metalloproteinase expression with increasing tumor grade and
invasion. Cancer. 94:1466–1475. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Tongtawee T, Kaewpitoon SJ, Loyd R,
Chanvitan S, Leelawat K, Praditpol N, Jujinda S and Kaewpitoon N:
High expression of matrix metalloproteinase-11 indicates poor
prognosis in human cholangiocarcinoma. Asian Pac J Cancer Prev.
16:3697–3701. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hsin CH, Chen MK, Tang CH, Lin HP, Chou
MY, Lin CW and Yang SF: High level of plasma matrix
metalloproteinase-11 is associated with clinic pathological
characteristics in patients with oral squamous cell carcinoma. PLoS
One. 9:e1131292014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Xu CJ and Xu F: MMP-11 and VEGF-C
expression correlate with clinical features of colorectal
adenocarcinoma. Int J Clin Exp Med. 7:2883–2888. 2014.PubMed/NCBI
|
|
30
|
Sanci M, Güngördük K, Gülseren V,
Karadeniz T, Kocaer M, Gungorduk O and Özdemir İA: MELF pattern for
predicting lymph node involvement and survival in grade I–II
endometrioid-type endometrial cancer. Int J Gynecol Pathol.
37:17–21. 2018.PubMed/NCBI
|
|
31
|
Mariani A, Dowdy SC, Cliby WA, Gostout BS,
Jones MB, Wilson TO and Podratz KC: Prospective assessment of
lymphatic dissemination in endometrial cancer: A paradigm shift in
surgical staging. Gynecol Oncol. 109:11–18. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yldirim ME, Karakuş S, Kurtulgan HK,
Kılıçgün H, Erşan S and Bakır S: The association of plasminogen
activator inhibitor type 1 (PAI-1) Level and PAI-1 4G/5G gene
polymorphism with the formation and the grade of endometrial
cancer. Biochem Genet. 55:314–321. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Roma AA, Rybicki LA, Barbuto D, Euscher E,
Djordjevic B, Frauenhoffer E, Kim I, Hong SR, Montiel D, Ali-Fehmi
R, et al: Risk factor analysis of recurrence in low-grade
endometrial adenocarcinoma. Hum Pathol. 46:1529–1539. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
O'Mara TA, Clements JA and Spurdle AB: The
use of predictive or prognostic genetic biomarkers in endometrial
and other hormone-related cancers: Justification for extensive
candidate gene single nucleotide polymorphism studies of the matrix
metalloproteinase family and their inhibitors. Cancer Epidemiol
Biomarkers Prev. 18:2352–2365. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yang YH, Deng H, Li WM, Zhang QY, Hu XT,
Xiao B, Zhu HH, Geng PL and Lu YY: Identification of matrix
metalloproteinase 11 as a predictive tumor marker in serum based on
gene expression profiling. Clin Cancer Res. 14:74–81. 2008.
View Article : Google Scholar : PubMed/NCBI
|