Introduction
Pancreatic cancer is a severe disease with a poor
5-year survival rate of <5% (1–3). Despite
the great strides made in the surgical and chemotherapeutic
management of pancreatic cancer, the disease continues to have a
poor prognosis. Pancreatic cancer has an unfavourable outcome
because it is difficult to detect at early stages. Patients are
typically diagnosed at a late stage when the cancer has already
locally advanced or spread to other parts of the body (4–7). The only
potentially curative therapy is surgical resection. However, when
patients are diagnosed with pancreatic cancer, more than half are
at an unresectable stage and are given chemotherapy, radiation,
palliative surgery or supportive care (8,9). Even if
patients undergo curative resection, their 5-year survival rates
are approximately 15–20%, with a median survival of 16 to 23 months
(10–13).
Peritoneal metastasis is one of the most important
prognostic factors for pancreatic cancer. According to the National
Comprehensive Cancer Network (NCCN), the presence of peritoneal
metastasis is an inoperative factor for pancreatic cancer (14).
Radical surgery is chosen among options including
pancreaticoduodenectomy (PD), distal pancreatectomy (DP) or total
pancreatectomy, according to the location of the pancreatic cancer.
These operations are relatively invasive surgeries (15–17).
It is important to diagnose peritoneal metastasis to
avoid unnecessary laparotomy and to determine the appropriate
therapy. However, it is difficult to detect small nodules suspected
to be peritoneal metastasis during pre-operative imaging
examinations, through techniques such as computed tomography (CT)
and 18F-fluoro-deoxy-glucose positron emission
tomography (FDG-PET). Small lesions can be diagnosed only by
intra-operative findings (9,18). Despite the availability of
high-resolution CT scans, occult distant metastases are still
observed in 11% of patients during surgery (18).
Sugiura et al have identified recurrent
disease (at the local, lymph node, peritoneum, liver and other
distant levels) in 76.9% of pancreatic cancer patients with an
R0-resection (curative resection with a negative pathologic margin)
(19). In Helsinki University
Hospital, in a subgroup of patients with T1-2 disease and an N0
[the Tumour-Node-Metastasis (TNM) classification of the Union for
International Cancer Control (UICC)] or R0-resection, the 5-year
survival was 49%, and the 10-year survival was 31% (17). Even after an R0-resection, some few
patients died from recurrence (12,17,19,20).
In the R0-resection patient group, the partial cause of recurrence
might be the difficulty of intraoperative assessment of small or
flat peritoneal metastases. It is necessary to be more precise in
detecting peritoneal metastases by intra-operative findings.
Staging laparoscopy has been proposed as a minimally
invasive technique to detect radiographically occult
intraperitoneal metastatic lesions (18,21–24).
However, diagnosis with standard laparoscopy has limitations.
Schnelldorfer et al have reported that standard laparoscopy
misses the majority of these metastases, thus resulting in a
substantial number of patients undergoing a nontherapeutic
laparotomy (18).
5-aminolevulinic acid (5-ALA) is a natural amino
acid that is metabolized into photosensitive protoporphyrin IX
(PpIX), which accumulates in cancer cells. PpIX emits red (peak
wavelength ~635 nm) fluorescence when it is excited with blue light
(peak wavelength ~405 nm), and the fluorescence diagnosis of cancer
by using this property is called photodynamic diagnosis (PDD)
(25,26). Recently, researchers have reported the
usefulness of PDD using 5-ALA (5-ALA-PDD) in the fields of
neurosurgery and urology (27–30).
Fluorescence cystoscopy has a sensitivity for detection of bladder
lesions of 94.2% and a specificity of 80.0% (27). We have previously reported the use of
5-ALA-PDD for detection of peritoneal dissemination and lymph node
metastasis in patients with gastric or colorectal cancer (31–36).
In the present study, we evaluated the usefulness of
5-ALA-PDD for detecting peritoneal metastasis of pancreatic cancer
during staging laparoscopy.
Materials and methods
Cell line and culture
The human pancreatic adenocarcinoma cell line AsPC-1
(Wako Pure Chemical Industries, Ltd., Osaka, Japan), which was
engineered to stably express green fluorescent protein (GFP), was
used. AsPC-1-GFP was cultured in RPMI-1640 medium supplemented with
10% foetal bovine serum and 1% penicillin/streptomycin in tissue
culture dishes humidified at 37°C in an atmosphere of 95% air and
5% carbon dioxide.
In vitro experiments
AsPC-1-GFP (1×106 cells) cells were
cultured for 3 days. Dishes were washed with PBS and incubated with
RPMI-1640 medium with 1 mM 5-ALA hydrochloride (Wako Pure Chemical
Industries) for 3 h. Then, we observed the fluorescence of PpIX
(excitation, 440 nm; emission, 575–675 nm) and GFP (excitation, 488
nm; emission, 500–560 nm) with an inverted microscope (IX81)
equipped with a confocal scanning system (FV1000; both Olympus,
Tokyo, Japan).
Animals
Five-week-old-female BALB/c nude mice were used in
this study. All in vivo experiments were approved and
followed the institutional guidelines of the Kyoto Prefectural
University of Medicine (Kyoto, Japan). The mice were housed in
plastic cages with stainless steel grid tops in an air-conditioned
environment with a 12-h light-dark cycle and had access to food and
water ad libitum.
Establishment of the mouse model of
peritoneal metastasis and fluorescence observation
An aliquot of 5×106 AsPC-1-GFP cells was
injected into the peritoneal cavities of mice under general
anaesthesia. After 3 weeks, the mice were intraperitoneally
injected with 5-ALA hydrochloride at a dose of 250 mg/kg body
weight. Four h after 5-ALA administration, the mice were
euthanized, and laparotomy was performed (37). Fluorescence observation was performed
with a stereoscopic microscope (SZX16; Olympus) equipped with a
colour charge-coupled digital camera (DP73) and a mercury lamp
(U-LH100HG; both Olympus). PpIX images (>430 nm; HQ430LP) were
acquired by excitation at 405±20 nm (D405/20×; both Chroma
Technology Corp., Rockingham, VT, USA), and GFP fluorescence images
(595–540 nm; GFPHQ cube) were acquired by excitation at 460 to 480
nm (GFPHQ cube, both Olympus). The merged image composites were
generated with image analysis software (ImageJ 1.45s, National
Institutes of Health, Bethesda, MD, USA).
Enrolled patients
Thirty-two patients clinically diagnosed with
pancreatic cancer and 2 patients clinically diagnosed with
intraductal papillary-mucinous carcinoma (IPMC) were enrolled in
the present study. They underwent surgery at the University
Hospital, Kyoto Prefectural University of Medicine, between April
2013 and February 2016. Peritoneal metastasis was not detected by
pre-operative imaging examinations, such as CT and FDG-PET.
The present study was approved by the Ethics
Committee of Kyoto Prefectural University of Medicine, Kyoto,
Japan. The patients provided signed informed consent
pre-operatively.
Laparoscopic procedure
5-ALA hydrochloride (Cosmo Bio Co., Ltd., Tokyo,
Japan) was orally administered to patients 3 h before surgery at a
dose of 20 mg per kg body weight (≤1 g per individual) (36,37). The
system used to perform fluorescence laparoscopy in 3 patients was
previously described (31).
Thirty-one patients were observed with a D-LIGHT C system (Karl
Storz GmbH & Co., Tuttlingen, Germany).
At the beginning of the staging laparoscopy, the
abdominal cavity was observed under white light and fluorescence
imaging with a long pass filter (>450 nm); images were obtained
under excitation with blue light (380–430 nm).
Results
Stereomicroscopic imaging analyses of
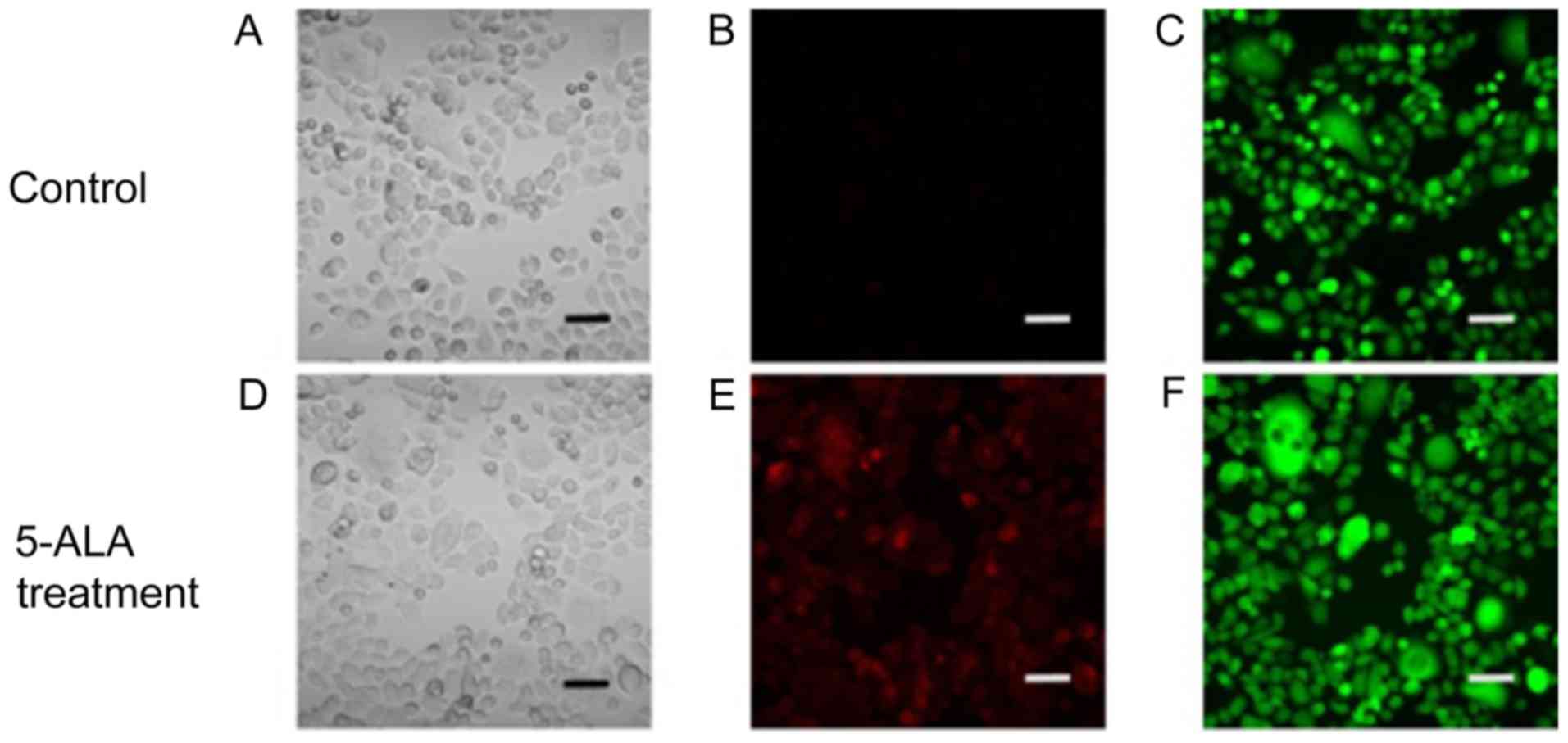
pancreatic cancer cell lines in vitro
As shown in Fig. 1,
PpIX-induced red fluorescence was observed in the ASPC-1-GFP cells
treated with 1 mM 5-ALA hydrochloride. The PpIX-induced red
fluorescence matched the observed GFP-induced green fluorescence.
These results indicated that PpIX had accumulated in the human
pancreatic cancer cells treated with 5-ALA.
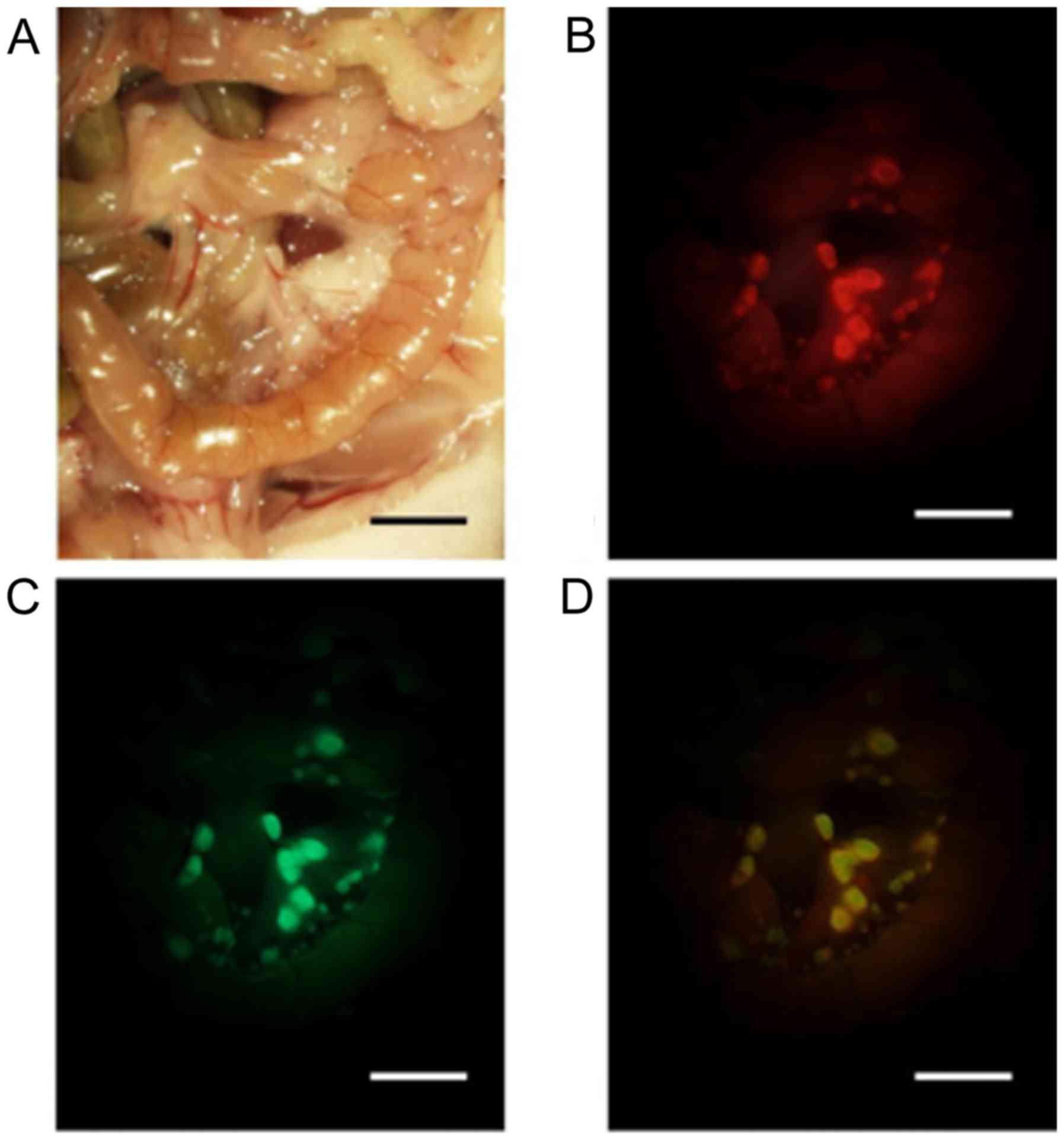
Stereomicroscopic imaging analyses of
peritoneal metastasis in a mouse model
To determine whether 5-ALA administration can be
used to specifically visualize peritoneal metastasis, a mouse model
of peritoneal metastasis was used. Three weeks after
intraperitoneal injection of ASPC-1-GFP cells, the peritoneal
metastases at the mesentery were visible macroscopically. Although
detection of the small nodules of the mesentery was difficult under
white light conditions, the small nodules were easily identified in
the fluorescence images. The 5-ALA-induced red fluorescent nodules
matched the observed GFP-induced green fluorescent nodules
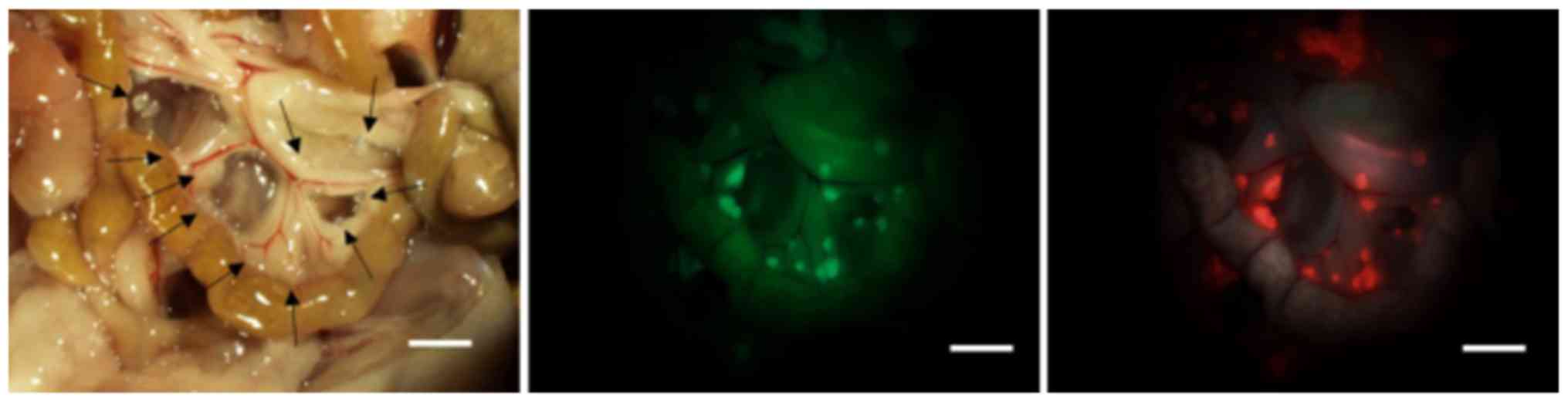
(Fig. 2). In our study, peritoneal
inspection was performed by counting the nodules by using the same
size field of view of the mesentery in five mice (Fig. 3). In the five mice examined, the tumor
detection rate using ALA-PDD was higher than that for white light
observation (100%; 184/184 vs. 21.2%; 39/184).
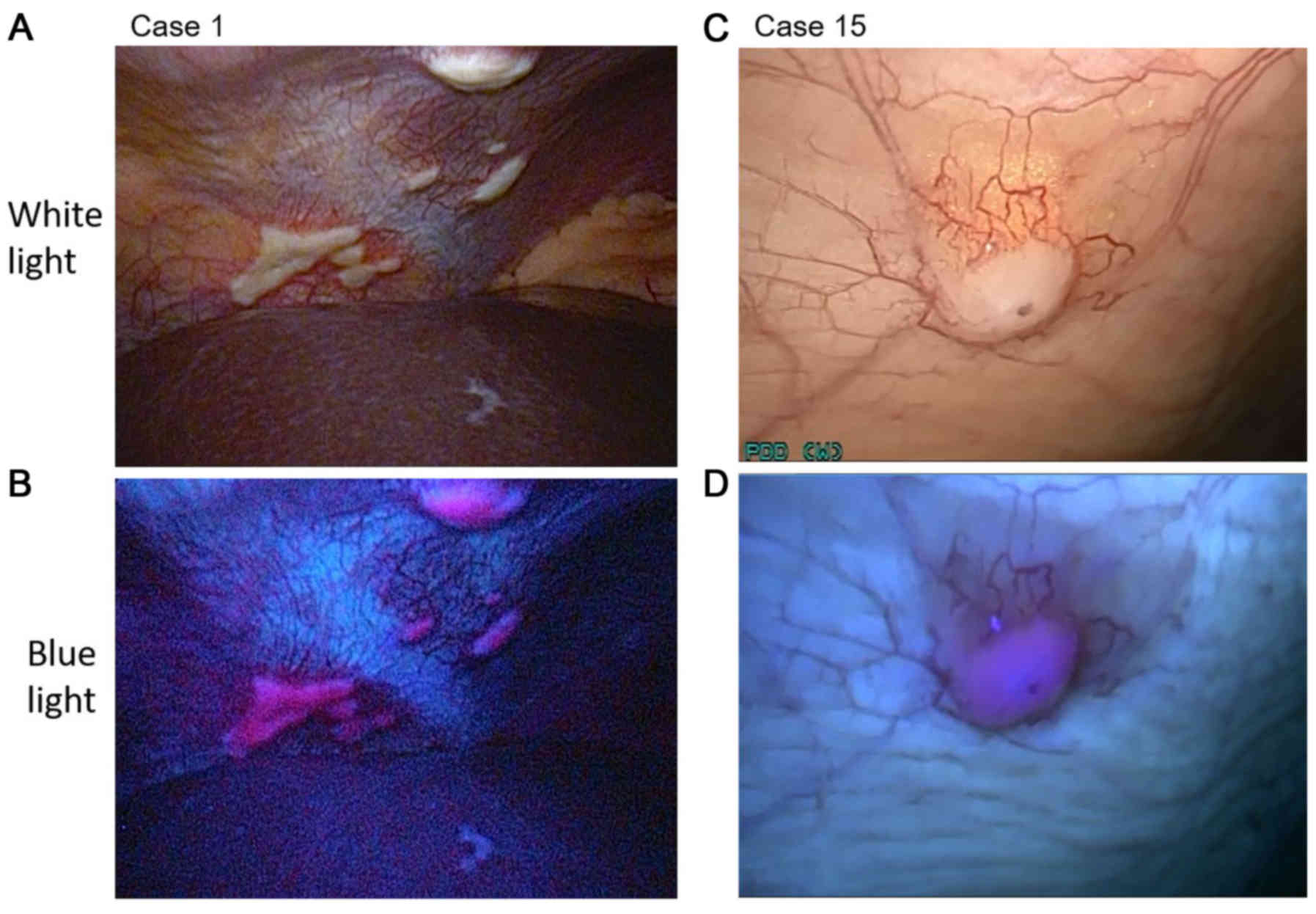
Laparoscopic 5-ALA-PDD of peritoneal
metastasis in pancreatic cancer patients
The details of the patient characteristics are
summarized in Tables I and II. The patients comprised 19 men and 15
women (median age, 70.5 years; range, 39–81 years) who had been
clinically diagnosed with Stage IA-III pancreatic cancer or IPMC
(UICC 6th TNM classification). All patients underwent conventional
staging laparoscopy and fluorescent observation. In 9 patients,
peritoneal nodules suspected to be peritoneal metastasis were
observed under white light. In 4 (case 1, 15, 29 and 34) of the 9
patients, nodules were detected in the fluorescence images. All
nodules were pathologically diagnosed as peritoneal metastasis
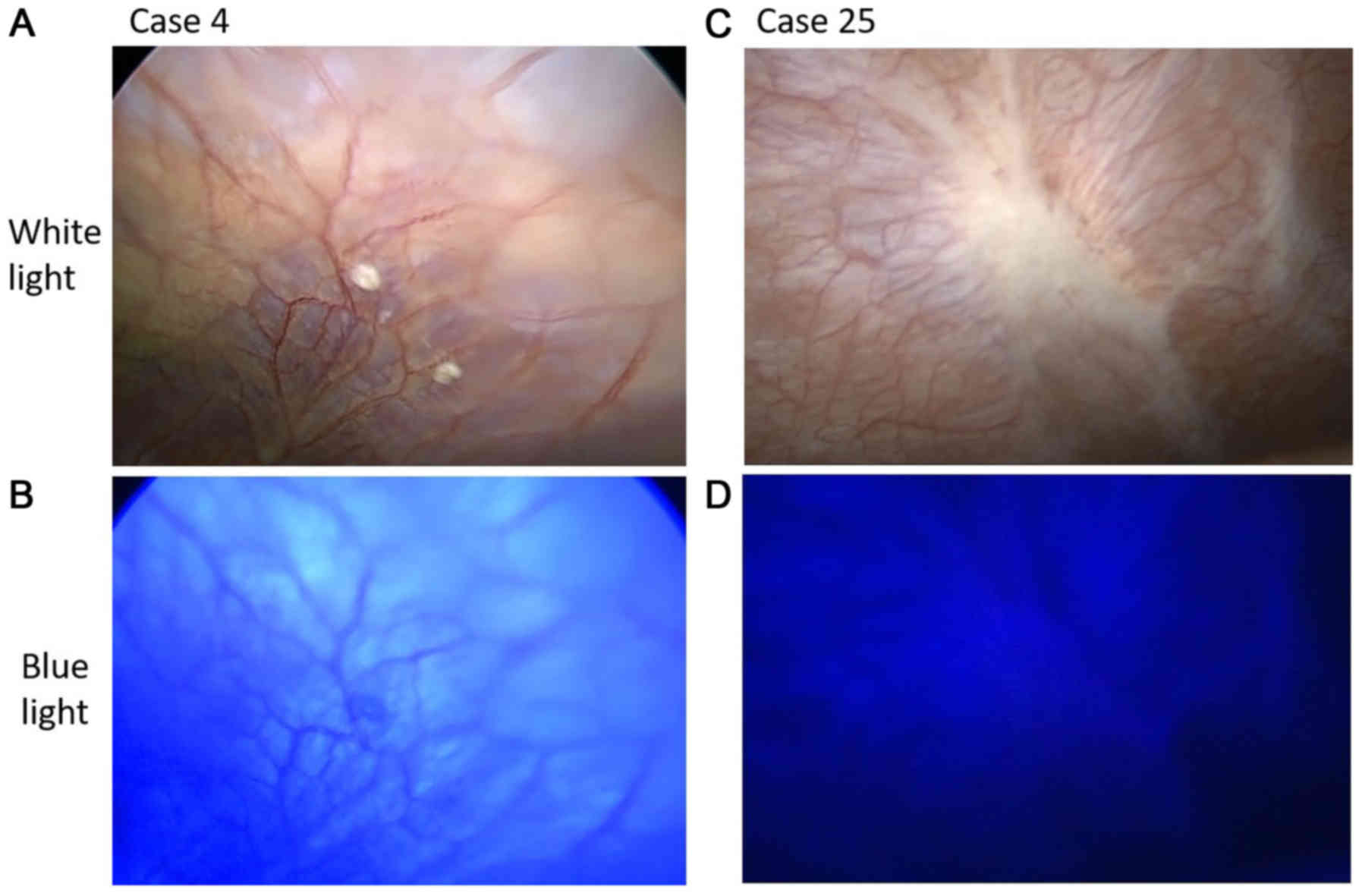
(Fig. 4). In the other five cases
(case 4, 25, 26, 28 and 33), the nodules that were observed under
white light but not under fluorescence excitation were diagnosed as
non-malignant by frozen section diagnosis (Fig. 5). The pathological results for cases 4
and 28 indicated fibroadipose tissue. Similarly, the results for
case 25 indicated fibrosis tissue, those for case 26 indicated
collagen fibre, and those for case 33 indicated fat and blood
vessels.
 | Table I.Patient characteristics (n=34). |
Table I.
Patient characteristics (n=34).
| Characteristic | Number of
patients |
|---|
| Sex |
|
|
Male | 19 |
|
Female | 15 |
| Age range (median),
years | 39–81 (70.5) |
| Cancer TNM
stagea |
|
| 0 | 0 |
| IA | 2 |
| IB | 2 |
|
IIA | 24 |
|
IIB | 2 |
|
III | 4 |
| IV | 0 |
 | Table II.Patient characteristics and
comparison of the detection of peritoneal metastases under white
light and fluorescence excitation. |
Table II.
Patient characteristics and
comparison of the detection of peritoneal metastases under white
light and fluorescence excitation.
|
|
|
|
|
| Peritoneal
assessment |
|---|
|
|
|
|
|
|
|
|---|
| Case | Clinical
diagnosis | Operation | Pathological
diagnosis of specimen | TNM
classificationa | WL | BL | Histological
diagnosis of nodule |
|---|
| 1 | PK | UR |
| T4N0M0 Stage
III/ | + | + | Pm |
|
|
|
|
| T4N0M1 Stage
IV |
|
|
|
| 2 | PK | PH | Lm | T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N0M1 Stage
IV |
|
|
|
| 3 | PK | DP | CP | T2N0M0 Stage
IIA/− |
| − |
|
| 4 | PK | PD | IDC | T3N0M0 Stage
IIA/ | + | − | − |
|
|
|
|
| T3N1M0 Stage
IIB |
|
|
|
| 5 | PK | PD | IPMC
(invasive) | TN0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N0M0 Stage
IIA |
|
|
|
| 6 | PK | DP | IDC | T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N1M0 Stage
IIB |
|
|
|
| 7 | PK | PD | IDC | T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N1M0 Stage
II |
|
|
|
| 8 | PK | DP | IDC | T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N0M0 Stage
IIA |
|
|
|
| 9 | PK | SL |
| T4N1M0 Stage
III/ |
| − |
|
|
|
|
|
| T4N1M0 Stage
III |
|
|
|
| 10 | PK | UR |
| T3N1M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T4N1M0 Stage
III |
|
|
|
| 11 | PK | SL |
| T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N0M0 Stage
IIA |
|
|
|
| 12 | PK | PD | IDC | T3N1M0 Stage
IIB/ |
| − |
|
|
|
|
|
| T3N0M0 Stage
IIA |
|
|
|
| 13 | PK | DP | IDC | T4N0M0 Stage
II/ |
| − |
|
|
|
|
|
| T3N1M0 Stage
IIB |
|
|
|
| 14 | PK | SL |
| T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N0M0 Stage
IIA |
|
|
|
| 15 | PK | UR |
| T3N0M0 Stage
IIA/ | + | + | Pm |
|
|
|
|
| T3N0M1 Stage
IV |
|
|
|
| 16 | PK | DP | In situ | T1N0M0 Stage
IA/ |
| − |
|
|
|
|
|
| TisN0M0 Stage
0 |
|
|
|
| 17 | PK | PD | In situ | T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| TisN0M0 Stage
0 |
|
|
|
| 18 | PK | DP | IDC | T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N1M0 Stage
IIB |
|
|
|
| 19 | IPMC | PD | IPMC | T1N0M0 Stage
IA/ |
| − |
|
|
|
|
|
| T1N0M0 Stage
IA |
|
|
|
| 20 | PK | PD | IPMC
(invasive) | T2N0M0 Stage
IB/ |
| − |
|
|
|
|
|
| T2N0M0 Stage
IB |
|
|
|
| 21 | PK | PD | IDC | T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N1M0 Stage
IIB |
|
|
|
| 22 | PK | DP, PH | IDC, HCC | T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N1M0 Stage
IIB |
|
|
|
| 23 | PK | DP | IDC | T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N1M0 Stage
IIB |
|
|
|
| 24 | PK | PD | IDC | T3N1M0 Stage
IIB/ |
| − |
|
|
|
|
|
| T3N1M0 Stage
IIB |
|
|
|
| 25 | PK | DP | IDC | T3N0M0 Stage
IIA/ | + | − | − |
|
|
|
|
| T3N1M0 Stage
IIB |
|
|
|
| 26 | PK | DP | IDC | T3N0M0 Stage
IIA/ | + | − | − |
|
|
|
|
| T3N0M0 Stage
IIA |
|
|
|
| 27 | PK | PD | IDC | T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N0M0 Stage
IIA |
|
|
|
| 28 | PK | PD | IDC | T3N0M0 Stage
IIA/ | + | − | − |
|
|
|
|
| T3N0M0 Stage
IIA |
|
|
|
| 29 | PK | UR |
| T3N0M0 Stage
IIA/ | + | + | Pm |
|
|
|
|
| T3N0M1 Stage
IV |
|
|
|
| 30 | PK | DP | CP | T3N0M0 Stage
IIA/− |
| − |
|
| 31 | PK | DP | IDC | T3N0M0 Stage
IIA/ |
| − |
|
|
|
|
|
| T3N0M0 Stage
IIA/ |
|
|
|
| 32 | PK | SL |
| T4N0M0 Stage
III/ |
| − |
|
|
|
|
|
| T4N0M0 Stage
III |
|
|
|
| 33 | IPMC | DP | IPMC
(invasive) | T3N0M0 Stage
IIA/ | + | − | − |
|
|
|
|
| T3N1M0 Stage
IIB |
|
|
|
| 34 | PK | UR |
| T3N0M0 Stage
IIA/ | + | + | Pm |
|
|
|
|
| T3N0M1 Stage
IV |
|
|
|
Four patients (case 9, 11, 14 and 32) were diagnosed
with borderline resectable pancreatic cancer by clinical
examination and underwent a preoperative staging laparoscopy. These
patients did not have inoperative factors and would have been
administered neoadjuvant therapy (38). In 5 patients (cases 1, 10, 15, 29 and
34), palliative procedures or an exploratory laparotomy were used
because unresectable factors existed (38). In 2 patients (cases 3 and 30), the
pathological diagnosis was chronic pancreatitis. No false positives
or false negatives were observed in these experiments. None of the
enrolled patients experienced any side effects due to 5-ALA
hydrochloride administration.
Discussion
Pancreatic cancer has one of the poorest prognoses
of any cancer (1–3). Radical surgery is very invasive
(15–17). It is important to diagnose peritoneal
metastasis to determine the appropriate therapy and to avoid
nontherapeutic laparotomy. However, detection of small nodules
suspected to be peritoneal metastases by pre-operative imaging
examinations, such as CT and FDG-PET, is difficult (9,18).
The use of diagnostic laparoscopy for pretherapeutic
staging of intraperitoneal tumours has been steadily increasing
(18,22–24). The
benefits of preoperative staging laparoscopy have been reported for
borderline resectable pancreatic cancer (38,39). The
complication rate of the staging laparoscopy is very low (24). No acute major complications were found
in this study. A major complication that can occur because of
treatment delays is the development of port-site metastasis, which
has been reported in up to 1% of diagnostic staging laparoscopies,
thus suggesting that this is an uncommon complication (24,40–42).
Preoperative staging laparoscopy reveals peritoneal
and superficial liver metastasis in ~25% of cases and therefore
helps to avoid unnecessary laparotomies. However, unresectable
tumours are found in open laparotomy after a staging laparoscopy in
12% of cases. In an additional 6.8% of cases, peritoneal metastases
are completely missed during the staging laparoscopy (21,23,24).
Recently, researchers have reported the utility of
5-ALA-PDD in the fields of neurosurgery and urology (27–30). 5-ALA
has few side effects and is a safe drug that has previously been
used to diagnose glioma and bladder cancer (27–30).
Although 5-ALA-PDD is a useful method, only a few reports have
examined the use 5-ALA-PDD for the diagnosis of peritoneal
metastasis in human intra-abdominal malignancy (23,24,36,43).
Gahlen et al have reported that the use of fluorescence
laparoscopy increases the visualization of intraperitoneal tumours
by 17.5%, as compared with white light laparoscopy (23). To our knowledge, the present study is
the first systematic report of the use of 5-ALA-PDD during staging
laparoscopy for detection of peritoneal metastasis of pancreatic
cancer. Our results suggest that the use of this method is
applicable for the detection of peritoneal metastasis of pancreatic
cancer in real time, which should improve the diagnostic accuracy
of peritoneal metastasis.
The 5-ALA-PDD method has some disadvantages. A weak
point of this technique is that deep observations are not possible
because the penetration of blue light is low in tissues (32,43).
Another problem is the undesirable effect of physiological
accumulation of PpIX and autofluorescence of the surrounding
tissues (36). 5-ALA hydrochloride is
administered orally. Therefore, this drug is problematic for
patients with symptoms due to gastroduodenal obstruction, such as
nausea, vomiting, and difficulty with oral intake. Patients with
pancreatic malignancies have a 13–20% risk of duodenal stenosis
(44).
We were not able to experience the persuasive case
that is difficult to recognize peritoneal metastasis under white
light but easy to recognize under fluorescent observation. We
showed that the all nodules suspected of peritoneal metastasis and
diagnosed as malignant histopathologically can be identified by the
fluorescent observation in realtime. False positive and false
negative cases were not observed in our study but would be
inevitable if the case series were increased. Negative proof, such
as the absence of false negatives, is difficult to provide. Gahlen
et al have suggested that open visual inspection and
palpation of the entire peritoneal surface are necessary to exclude
false negatives; however, it is almost impossible to examine the
entire peritoneal surface histopathologically (23). The prognosis should be continuously
followed-up.
In the present study, we demonstrated the presence
of PpIX-induced red fluorescence in pancreatic cells in
vitro and in vivo. In our human study, we observed red
fluorescence in peritoneal metastasis of pancreatic cancer by using
5-ALA-PDD during staging laparoscopy. This study indicates that
5-ALA-PDD is useful for detecting peritoneal metastasis during
staging laparoscopy in human pancreatic cancer patients.
In conclusion, we confirmed that the use of
5-ALA-PDD during staging laparoscopy is promising for the rapid
diagnosis of peritoneal metastasis in pancreatic cancer patients.
We suggest that future research assessing the clinical usefulness
of this method would be worthwhile.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
YM designed this study. HI and RM performed the
pancreatic operations. HM and HK helped perform the experiments. TT
advised on the use of 5-ALA within the study and interpreted the
data. HF, KO and EO analyzed and interpreted the data. KH performed
the experiments and analyzed the data. All authors read and
approved the final manuscript and agree to be accountable for all
aspects of the study in ensuring that question related to accuracy
or integrity of any part of the work are appropriately investigated
and resolved.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Kyoto Prefectural University of Medicine. All study
participants proved written informed consent. Animal
experimentation within this study was approved by the Institutional
Animal Care and Use Committee and performed according to the Animal
Experimentation Regulation of Kyoto Prefectural University of
Medicine.
Consent for publication
All participants provided written informed consent
for the publication of their data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2015. CA Cancer J Clin. 65:5–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tewari M: Pancreatic cancer: A challenge
to cure. Indian J Surg. 77:350–357. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vincent A, Herman J, Schulick R, Hruban RH
and Goggins M: Pancreatic cancer. Lancet. 378:607–620. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gall TM, Tsakok M, Wasan H and Jiao LR:
Pancreatic cancer: Current management and treatment strategies.
Postgrad Med J. 91:601–607. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Michl P, Pauls S and Gress TM:
Evidence-based diagnosis and staging of pancreatic cancer. Best
Pract Res Clin Gastroenterol. 20:227–251. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wolfgang CL, Herman JM, Laheru DA, Klein
AP, Erdek MA, Fishman EK and Hruban RH: Recent progress in
pancreatic cancer. CA Cancer J Clin. 63:318–348. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pietryga JA and Morgan DE: Imaging
preoperatively for pancreatic adenocarcinoma. J Gastrointest Oncol.
6:343–357. 2015.PubMed/NCBI
|
|
8
|
Cid-Arregui A and Juarez V: Perspectives
in the treatment of pancreatic adenocarcinoma. World J
Gastroenterol. 21:9297–9316. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Morak MJ, Hermans JJ, Smeenk HG, Renders
WM, Nuyttens JJ, Kazemier G and van Eijck CH: Staging for locally
advanced pancreatic cancer. Eur J Surg Oncol. 35:963–968. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Baekelandt BM, Hjermstad MJ, Nordby T,
Fagerland MW, Kure EH, Heiberg T, Buanes T and Labori KJ:
Preoperative cognitive function predicts survival in patients with
resectable pancreatic ductal adenocarcinoma. HPB (Oxford).
18:247–254. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gillen S, Schuster T, Meyer Zum
Büschenfelde C, Friess H and Kleeff J: Preoperative/neoadjuvant
therapy in pancreatic cancer: A systematic review and meta-analysis
of response and resection percentages. PLoS Med. 7:e10002672010.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hartwig W, Hackert T, Hinz U, Gluth A,
Bergmann F, Strobel O, Büchler MW and Werner J: Pancreatic cancer
surgery in the new millennium: Better prediction of outcome. Ann
Surg. 254:311–319. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
He J, Ahuja N, Makary MA, Cameron JL,
Eckhauser FE, Choti MA, Hruban RH, Pawlik TM and Wolfgang CL: 2564
resected periampullary adenocarcinomas at a single institution:
Trends over three decades. HPB (Oxford). 16:83–90. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yamaguchi K, Okusaka T, Shimizu K, Furuse
J, Ito Y, Hanada K and Shimosegawa T: Committee for revision of
clinical guidelines for pancreatic cancer of Japan Pancreas
Society: EBM-based Clinical Guidelines for Pancreatic Cancer (2013)
issued by the Japan Pancreas Society: A synopsis. Jpn J Clin Oncol.
44:883–888. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lermite E, Sommacale D, Piardi T, Arnaud
JP, Sauvanet A, Dejong CH and Pessaux P: Complications after
pancreatic resection: Diagnosis, prevention and management. Clin
Res Hepatol Gastroenterol. 37:230–239. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kimura W, Miyata H, Gotoh M, Hirai I,
Kenjo A, Kitagawa Y, Shimada M, Baba H, Tomita N, Nakagoe T, et al:
A pancreaticoduodenectomy risk model derived from 8575 cases from a
national single-race population (Japanese) using a web-based data
entry system: The 30-day and in-hospital mortality rates for
pancreaticoduodenectomy. Ann Surg. 259:773–780. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Seppänen H, Juuti A, Mustonen H, Haapamäki
C, Nordling S, Carpelan-Holmström M, Sirén J, Luettges J, Haglund C
and Kiviluoto T: The results of pancreatic resections and long-term
survival for pancreatic ductal adenocarcinoma: A single-institution
experience. Scand J Surg. 106:54–61. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schnelldorfer T, Gagnon AI, Birkett RT,
Reynolds G, Murphy KM and Jenkins RL: Staging laparoscopy in
pancreatic cancer: A potential role for advanced laparoscopic
techniques. J Am Coll Surg. 218:1201–1206. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sugiura T, Uesaka K, Mihara K, Sasaki K,
Kanemoto H, Mizuno T and Okamura Y: Margin status, recurrence
pattern, and prognosis after resection of pancreatic cancer.
Surgery. 154:1078–1086. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Adham M, Jaeck D, Le Borgne J,
Oussoultzouglou E, Chenard-Neu MP, Mosnier JF, Scoazec JY, Mornex F
and Partensky C: Long-term survival (5–20 years) after
pancreatectomy for pancreatic ductal adenocarcinoma: A series of 30
patients collected from 3 institutions. Pancreas. 37:352–357. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hemming AW, Nagy AG, Scudamore CH and
Edelmann K: Laparoscopic staging of intraabdominal malignancy. Surg
Endosc. 9:325–328. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mayo SC, Austin DF, Sheppard BC, Mori M,
Shipley DK and Billingsley KG: Evolving preoperative evaluation of
patients with pancreatic cancer: Does laparoscopy have a role in
the current era? J Am Coll Surg. 208:87–95. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gahlen J, Stern J, Laubach HH, Pietschmann
M and Herfarth C: Improving diagnostic staging laparoscopy using
intraperitoneal lavage of delta-aminolevulinic acid (ALA) for
laparoscopic fluorescence diagnosis. Surgery. 126:469–473. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zöpf T, Schneider AR, Weickert U, Riemann
JF and Arnold JC: Improved preoperative tumor staging by
5-aminolevulinic acid induced fluorescence laparoscopy.
Gastrointest Endosc. 62:763–767. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kennedy JC and Pottier RH: Endogenous
protoporphyrin IX, a clinically useful photosensitizer for
photodynamic therapy. J Photochem Photobiol B. 14:275–292. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Peng Q, Warloe T, Berg K, Moan J,
Kongshaug M, Giercksky KE and Nesland JM: 5-Aminolevulinic
acid-based photodynamic therapy. Clinical research and future
challenges. Cancer. 79:2282–2308. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kriegmair M, Baumgartner R, Knüchel R,
Stepp H, Hofstädter F and Hofstetter A: Detection of early bladder
cancer by 5-aminolevulinic acid induced porphyrin fluorescence. J
Urol. 155:105–110. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Jichlinski P, Forrer M, Mizeret J,
Glanzmann T, Braichotte D, Wagnières G, Zimmer G, Guillou L,
Schmidlin F, Graber P, et al: Clinical evaluation of a method for
detecting superficial surgical transitional cell carcinoma of the
bladder by light-induced fluorescence of protoporphyrin IX
following the topical application of 5-aminolevulinic acid:
Preliminary results. Lasers Surg Med. 20:402–408. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Stummer W, Stocker S, Wagner S, Stepp H,
Fritsch C, Goetz C, Goetz AE, Kiefmann R and Reulen HJ:
Intraoperative detection of malignant gliomas by 5-aminolevulinic
acid-induced porphyrin fluorescence. Neurosurgery. 42:518–526.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Friesen SA, Hjortland GO, Madsen SJ,
Hirschberg H, Engebraten O, Nesland JM and Peng Q: 5-Aminolevulinic
acid-based photodynamic detection and therapy of brain tumors
(review). Int J Oncol. 21:577–582. 2002.PubMed/NCBI
|
|
31
|
Murayama Y, Harada Y, Imaizumi K, Dai P,
Nakano K, Okamoto K, Otsuji E and Takamatsu T: Precise detection of
lymph node metastases in mouse rectal cancer by using
5-aminolevulinic acid. Int J Cancer. 125:2256–2263. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Murayama Y, Ichikawa D, Koizumi N, Komatsu
S, Shiozaki A, Kuriu Y, Ikoma H, Kubota T, Nakanishi M, Harada Y,
et al: Staging fluorescence laparoscopy for gastric cancer by using
5-aminolevulinic acid. Anticancer Res. 32:5421–5427.
2012.PubMed/NCBI
|
|
33
|
Hatakeyama T, Murayama Y, Komatsu S,
Shiozaki A, Kuriu Y, Ikoma H, Nakanishi M, Ichikawa D, Fujiwara H,
Okamoto K, et al: Efficacy of 5-aminolevulinic acid-mediated
photodynamic therapy using light-emitting diodes in human colon
cancer cells. Oncol Rep. 29:911–916. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Hino H, Murayama Y, Nakanishi M, Inoue K,
Nakajima M and Otsuji E: 5-Aminolevulinic acid-mediated
photodynamic therapy using light-emitting diodes of different
wavelengths in a mouse model of peritoneally disseminated gastric
cancer. J Surg Res. 185:119–126. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Koizumi N, Harada Y, Murayama Y, Harada K,
Beika M, Yamaoka Y, Dai P, Komatsu S, Kubota T, Ichikawa D, et al:
Detection of metastatic lymph nodes using 5-aminolevulinic acid in
patients with gastric cancer. Ann Surg Oncol. 20:3541–3548. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kondo Y, Murayama Y, Konishi H, Morimura
R, Komatsu S, Shiozaki A, Kuriu Y, Ikoma H, Kubota T, Nakanishi M,
et al: Fluorescent detection of peritoneal metastasis in human
colorectal cancer using 5-aminolevulinic acid. Int J Oncol.
45:41–46. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Nishimura M, Murayama Y, Harada K, Kamada
Y, Morimura R, Ikoma H, Ichikawa D, Fujiwara H, Okamoto K and
Otsuji E: Photodynamic diagnosis of hepatocellular carcinoma using
5-aminolevulinic acid. Anticancer Res. 36:4569–4574. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Hartwig W, Werner J, Jäger D, Debus J and
Büchler MW: Improvement of surgical results for pancreatic cancer.
Lancet Oncol. 14:e476–e485. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Callery MP, Chang KJ, Fishman EK,
Talamonti MS, Traverso William L and Linehan DC: Pretreatment
assessment of resectable and borderline resectable pancreatic
cancer: Expert consensus statement. Ann Surg Oncol. 16:1727–1733.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Pearlstone DB, Mansfield PF, Curley SA,
Kumparatana M, Cook P and Feig BW: Laparoscopy in 533 patients with
abdominal malignancy. Surgery. 125:67–72. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Shoup M, Brennan MF, Karpeh MS, Gillern
SM, McMahon RL and Conlon KC: Port site metastasis after diagnostic
laparoscopy for upper gastrointestinal tract malignancies: An
uncommon entity. Ann Surg Oncol. 9:632–636. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Reymond MA, Schneider C, Kastl S,
Hohenberger W and Köckerling F: The pathogenesis of port-site
recurrences. J Gastrointest Surg. 2:406–414. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kishi K, Fujiwara Y, Yano M, Inoue M,
Miyashiro I, Motoori M, Shingai T, Gotoh K, Takahashi H, Noura S,
et al: Staging laparoscopy using ALA-mediated photodynamic
diagnosis improves the detection of peritoneal metastases in
advanced gastric cancer. J Surg Oncol. 106:294–298. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Conio M, Demarquay JF, De Luca L, Marchi S
and Dumas R: Endoscopic treatment of pancreatico-biliary
malignancies. Crit Rev Oncol Hematol. 37:127–135. 2001. View Article : Google Scholar : PubMed/NCBI
|