Introduction
Cancer is one of the most important public health
problems faced by human beings all over the world, and lung cancer
(LC) is one of the most common cancers with the highest mortality
rate among all malignant tumors (1).
Approximately 2 million patients in developing countries die each
year due to LC, and incidence and mortality of LC showed an
increasing trend in recent years, and the onset age is becoming
increasingly younger (2,3). LC mainly affects patients between 60–70
years, and the incidence is higher in men than in women. Surgical
treatment is the main treatment for patients with LC, while most
patients are diagnosed at advanced stages and chemotherapy and
targeted drug therapy for those patients failed to significantly
improve the 5-year survival rate, leading to poor prognosis
(4). Therefore, early diagnosis and
treatment is critical for the survival of patients with LC.
Idiopathic pulmonary fibrosis (IPF) is a
characteristic pathological change from common interstitial
pneumonia to chronic inflammatory interstitial lung disease. The
main manifestations of IPF include pulmonary fibrosis and diffuse
alveolitis. Fibrosis of lung tissue leads to increase in hardness
of the lung tissue and decrease in compliance (5,6). The
median survival time of IPF patients after diagnosis is as short as
2–3 years, and 5-year survival rate is only 20%, seriously
influencing the patient's life. Current diagnostic methods for IPF
are mainly based on pulmonary imaging examinations and clinical
features, but these methods do not provide information for the
prognosis of those patients during treatment (7).
In recent years, studies have shown that FGFs and
FGFRs form the FGFR pathway. Studies have shown that the FGFR
pathway participates in the body's growth and development, wound
healing, tumor formation, fibrosis and inflammatory reactions
(8). Therefore, we detected the
expression of FGF2 and FGFR2 in LC and IPF. Our findings provide
new insights into the diagnosis and treatment of LC and IPF.
Patients and methods
Clinical data
In this study, 108 patients with LC who were treated
in Shanghai Pulmonary Hospital (Shanghai, China) from May 2013 to
July 2016 were collected. Cancerous tissues and adjacent healthy
tissues were collected during surgery. Tissues were stored in
liquid nitrogen. In addition, 88 cases of IPF patients and 100
normal people with cough were also collected in Shanghai Pulmonary
Hospital. Lavage fluid was collected from IPF patients and normal
controls. This study was approved by the Medical Ethics Committee
of Shanghai Pulmonary Hospital (Shanghai, China), and all patients
were informed and signed informed consent. Clinical data of
patients were collected for further analysis.
Inclusion and exclusion criteria
Inclusion criteria
Patients >18 years, and course of the disease
longer that 6 months; patients who were not treated with anti-tumor
drugs; patients who received no radiotherapy or chemotherapy.
Exclusion criteria
Patients with digestive disease; patients with blood
relationship with other patients; patients with cirrhosis or
autoimmune disease; patients with serious infection; patients who
received blood transfusion recently.
Detection method
Reverse transcription-quantitative PCR
(RT-qPCR)
Tissues were ground in liquid nitrogen and total RNA
was extracted using TRIzol reagent (Shanghai Pufei Biotechnology,
Co., Ltd., Shanghai, China). RNA quality was tested by an
ultraviolet spectrophotometer (Hitachi, Tokyo, Japan), and only RNA
samples with a 260/280 ratio between 1.8–2.2 were used in reverse
transcription to synthesize cDNA using a reverse transcription kit
(Applied Biosystems; Thermo Fisher Scientific, Inc., Waltham, MA,
USA). PCR reaction system was prepared using a PCR kit (Applied
Biosystems; Thermo Fisher Scientific, Inc.): 10 µl of TaqMan 2 ×
Universal Master Mix II, 2 µl of each of the upstream and
downstream primers, 2 µl of cDNA template and 4 µl of water. PCR
reaction conditions: 95°C for 5 min, followed by 40 cycles of 95°C
for 15 sec, 55°C for 35 sec and 72°C for 20 sec. Each experiment
was performed 3 times with GAPDH as endogenous control. Sequences
of primers used in PCR reactions are listed in Table I.
 | Table I.Primer sequences. |
Table I.
Primer sequences.
| Genes | Forward | Reverse |
|---|
| FGF2 |
5′-CGGCTGTACTGCAAAAACGG-3′ |
5′-GATGTGAGGGTCGCTCTTCTCC-3′ |
| FGFR2 |
5′-TACCAAATCTCCCAACCAGAAG-3′ |
5′-CCCATCCTTAGTCCAACTGAT-3′ |
| GAPDH |
5′-CAGGGCTGCTTTTAACTCTGGTAA-3′ |
5′-GGGTGGAATCATATTGGAACATGT-3′ |
Western blotting
Lung tissues were mixed with protein lysate
containing protease inhibitor and ground on ice. Collected lavage
fluid was centrifuged at 2,500 × g using a cryogenic centrifuge for
5 min at 4°C to remove the supernatant. Centrifugation was
performed again to remove the supernatant. Then protein lysate
containing protease inhibitor was added and incubated on ice. BCA
kit (Thermo Fisher Scientific, Inc.) was used to measure protein
concentration. After 10% SDS-PAGE gel electrophoresis (80–120 V)
for 100 min, gel transfer to a PVDF membrane was performed. The
membranes were blocked with 5% skimmed milk for 1.5 h at room
temperature. After washing with TBST, the membranes were incubated
with primary antibodies (1:1,000; SAB Biotherapeutics, Inc., Sioux
Falls, SD, USA) overnight at 4°C. After washing with TBST, the
membranes were further incubated with secondary antibody (1:2,000)
at room temperature for 1 h. Finally, TBST (ProteinTech Group,
Inc., Chicago, IL, USA) was added to develop signals. The relative
expression of each protein was normalized to β-actin. Primary
rabbit polyclonal FGF2 antibody (dilution: 1/1,000; cat. no.
ab8880), rabbit polyclonal FGFR2 antibody (dilution: 1/1,000; cat.
no. ab10648), rabbit polyclonal β-actin antibody (dilution:
1/1,000; cat. no. ab8227) and secondary goat anti-rabbit (HRP) IgG
antibody (dilution: 1/2,000; cat. no. ab6721) were all purchased
from Abcam (Cambridge, MA, USA).
Statistical analysis
SPSS 20.0 software package (IBM SPSS, Armonk, NY,
USA) was used to process the collected data. Measured data were
expressed as mean ± standard deviation and compared by t-test.
Count data were expressed as % and compared by Chi-square test.
Comparisons among multiple groups were performed using one-way
ANOVA followed by post hoc test (Least Significant Difference).
P<0.05 was considered to indicate a statistically significant
difference.
Results
Comparison of clinical data among
groups
No significant differences in sex, age, IBM, smoking
history, alcoholism, exercise habits, place of residence, and
marital status were found among groups (P>0.05) (Table II).
 | Table II.Comparison of clinical data among
groups. |
Table II.
Comparison of clinical data among
groups.
| Groups | n | LC patients
(n=108) | IPF patients
(n=88) | Normal controls
(n=100) | F-value | P-value |
|---|
| Sex |
|
|
|
| 0.060 | 0.971 |
| Male | 203 | 75 | 60 | 68 |
|
|
|
Female | 93 | 33 | 28 | 32 |
|
|
| Age |
|
|
|
| 0.498 | 0.780 |
|
>60 | 174 | 65 | 49 | 60 |
|
|
| ≤60 | 122 | 43 | 39 | 40 |
|
|
| Smoking history |
|
|
|
| 1.356 | 0.508 |
| Yes | 205 | 78 | 62 | 65 |
|
|
| No | 91 | 30 | 26 | 35 |
|
|
| Alcoholism |
|
|
|
| 0.858 | 0.651 |
| Yes | 49 | 20 | 12 | 17 |
|
|
| No | 247 | 88 | 76 | 83 |
|
|
| Exercise habits |
|
|
|
| 0.612 | 0.736 |
| Yes | 36 | 15 | 9 | 12 |
|
|
| No | 260 | 93 | 79 | 88 |
|
|
| Place of
residence |
|
|
|
| 0.511 | 0.775 |
| Urban
area | 267 | 99 | 78 | 90 |
|
|
| Rural
area | 29 | 9 | 10 | 10 |
|
|
| Marital status |
|
|
|
| 0.166 | 0.920 |
|
Married | 273 | 99 | 82 | 92 |
|
|
|
Unmarried | 23 | 9 | 6 | 8 |
|
|
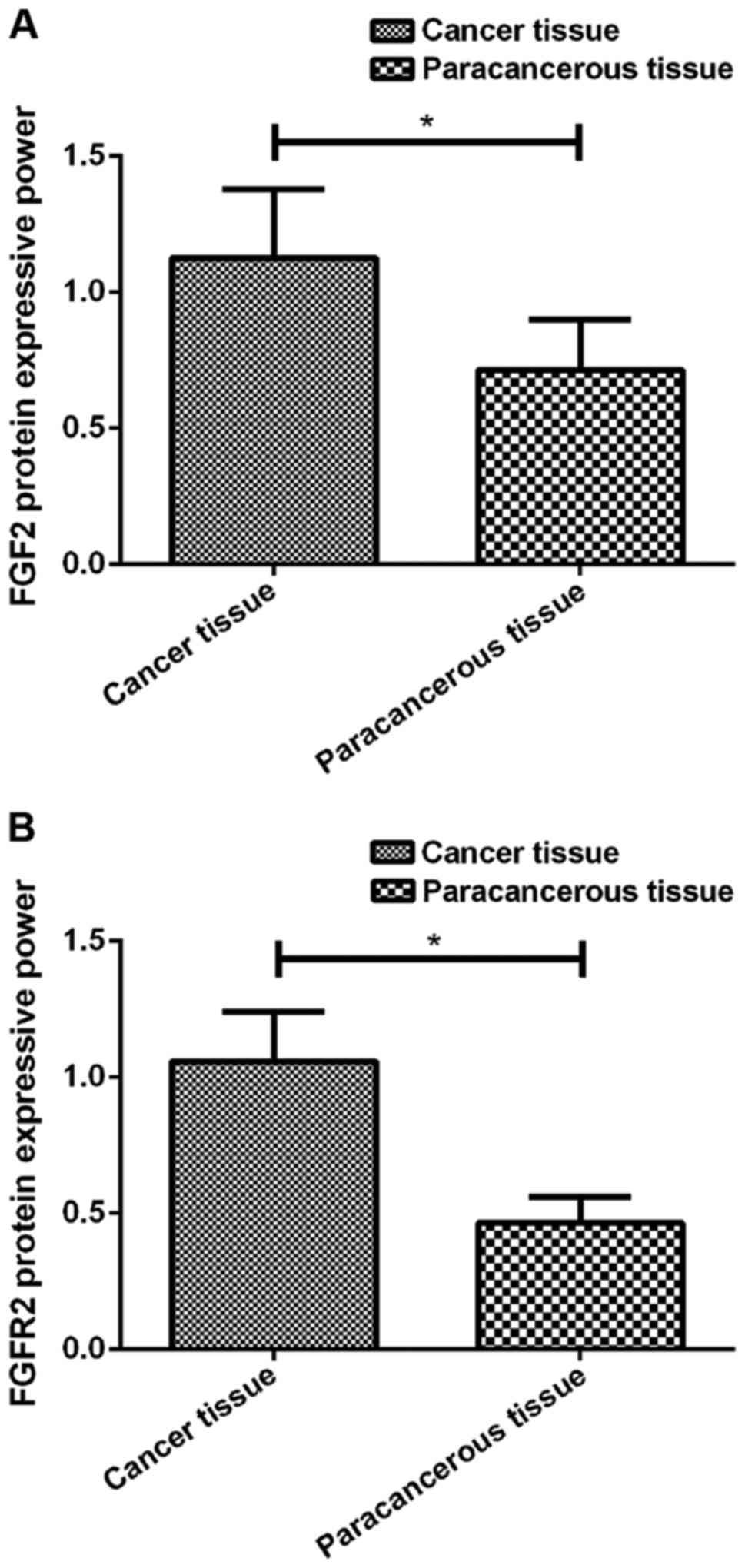
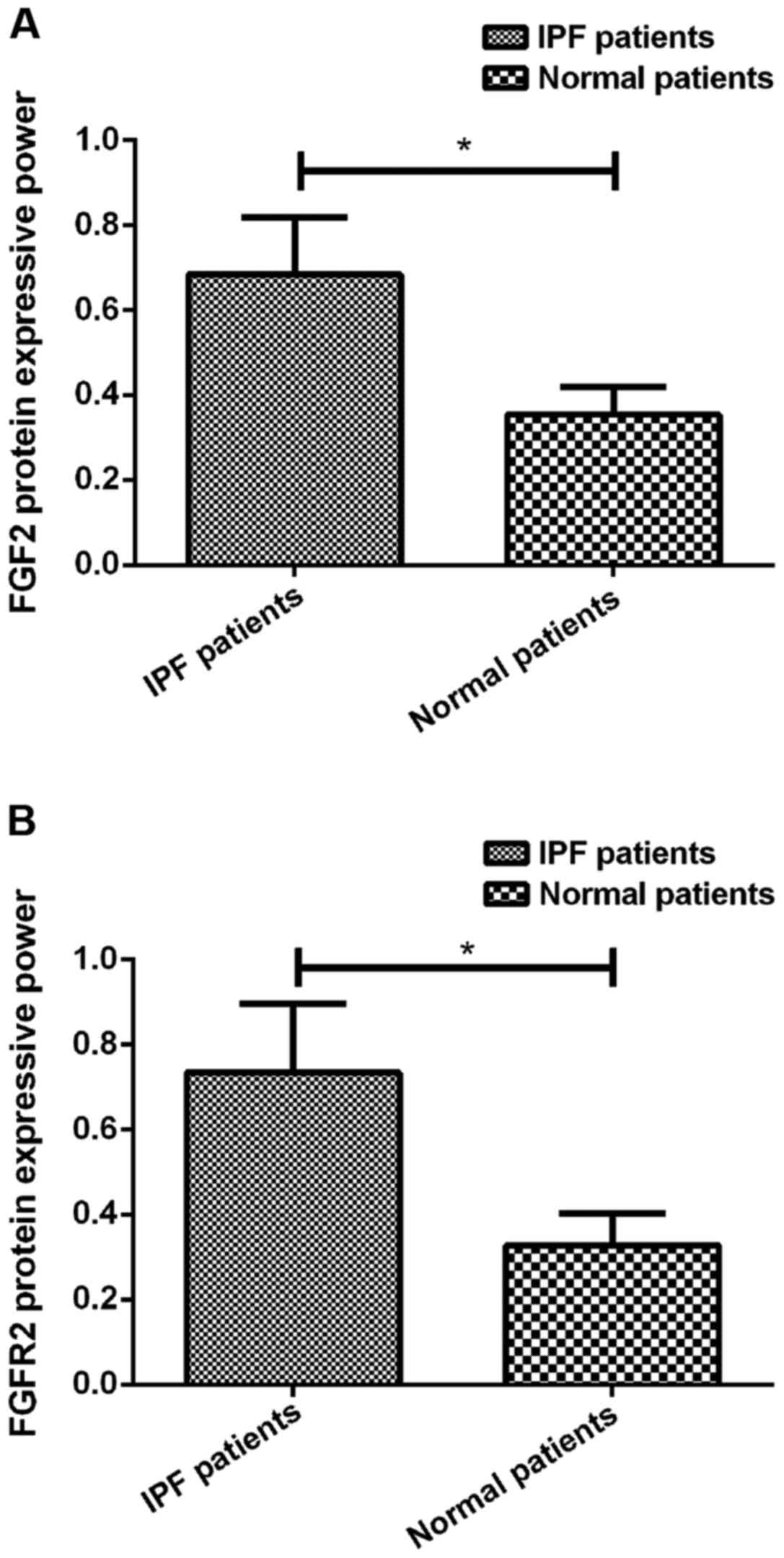
Relative expression levels of FGF2 and
FGFR2 in each group
RT-qPCR and western blotting results showed that
FGF2 mRNA and protein was highly expressed in cancer tissues
of LC patients, and the expression levels were significantly higher
than that in the adjacent tissues (P<0.05). In addition,
FGFR2 mRNA and protein was highly expressed in cancer
tissues of LC patients, and the expression levels were
significantly higher than that in the adjacent tissues (P<0.05).
Besides that, the expression levels of FGF2 and FGFR2 proteins were
also significantly higher in IPF patients than in the normal
patients (P<0.05) (Table III;
Figs. 1 and 2).
 | Table III.Expression of FGF2 and
FGFR2 in tissues of patients with LC and lavage fluid of
patients with IPF and normal controls. |
Table III.
Expression of FGF2 and
FGFR2 in tissues of patients with LC and lavage fluid of
patients with IPF and normal controls.
|
| LC patients |
|
|
|---|
|
|
|
|
|
|---|
| Groups | Cancer tissues | Adjacent healthy
tissues | t | P-value |
|---|
| FGF2
mRNA | 0.984±0.134 | 0.274±0.064 | 49.687 | 0.001 |
| FGFR2
mRNA | 1.115±0.184 | 0.405±0.861 |
|
|
Correlation between expression of FGF2
and FGFR2 and clinicopathological data of LC patients
Correlation analysis between the expression of
FGF2 and FGFR2 mRNA in cancer tissues of LC patients
and patients' clinicopathological data showed that expression of
FGF2 and FGFR2 in LC lung tissues was not significantly correlated
with age, sex and smoking history (P>0.05), but was
significantly correlated with lymph node metastasis, tumor
differentiation, and TNM stage (P<0.05) (Table IV).
 | Table IV.Correlation between expression of
FGF2 and FGFR2 and clinicopathological data of LC
patients. |
Table IV.
Correlation between expression of
FGF2 and FGFR2 and clinicopathological data of LC
patients.
| Clinicopathological
data | n=108 | FGF2 mRNA | t/F | P-value | FGFR2 mRNA | t/F | P-value |
|---|
| Age |
|
| 1.259 | 0.211 |
| 1.211 | 0.229 |
|
≥60 | 65 | 0.984±0.131 |
|
| 1.025±0.158 |
|
|
|
<60 | 43 | 0.953±0.116 |
|
| 1.063±0.162 |
|
|
| Sex |
|
| 0.179 | 0.856 |
| 0.328 | 0.744 |
|
Male | 75 | 0.973±0.138 |
|
| 1.084±0.162 |
|
|
|
Female | 33 | 0.968±0.124 |
|
| 1.073±0.158 |
|
|
| Smoking
history |
|
| 0.708 | 0.480 |
| 0.269 | 0.788 |
|
Yes | 78 | 0.975±0.132 |
|
| 1.101±0.158 |
|
|
| No | 30 | 0.955±0.130 |
|
| 1.092±0.149 |
|
|
| Lymph node
metastasis |
|
| 3.783 | 0.001 |
| 2.203 | 0.030 |
|
Yes | 97 | 1.135±0.164 |
|
| 1.154±0.164 |
|
|
| No | 11 | 0.942±0.120 |
|
| 1.041±0.132 |
|
|
|
Differentiation |
|
| 6.684 | 0.002 |
| 3.257 | 0.042 |
|
Low | 18 | 1.105±0.142 |
|
| 1.112±0.178 |
|
|
|
Moderate | 55 | 0.988±0.137 |
|
| 1.035±0.163 |
|
|
|
High | 35 | 0.965±0.133 |
|
| 0.994±0.143 |
|
|
| TNM stage |
|
| 13.958 | 0.001 |
| 4.682 | 0.011 |
| I | 16 | 0.958±0.122 |
|
| 0.998±0.149 |
|
|
| II | 45 | 0.994±0.143 |
|
| 1.054±0.158 |
|
|
|
III+IV | 47 | 1.132±0.155 |
|
| 1.132±0.183 |
|
|
Discussion
LC as the most common type of malignancy in clinical
practice is also one of the leading causes of cancer-related deaths
in both developed and developing countries. Studies have shown that
the incidence of LC is increasing every year, and the incidence
rate in urban areas is the highest (9). Surgical resection is the most common
treatment for LC patients, but is not acceptable for most patients.
In clinical practice, chemotherapy and radiotherapy are mostly
used. However, patients with long-term radiotherapy and
chemotherapy will develop severe adverse reactions. IPF is a
fibrosis-specific lesion, and the cause of IPF is unknown. The
occurrence of IPF is related to age, sex, working environment, and
smoking history (10). Hutchinson
(11) retrospectively analyzed the
prevalence of IPF in 21 countries, and it was found that the
prevalence of IPF in the world is on the rise. With the growth of
the aging population and aggregated air pollution, the incidence of
IPF has been further increased. Studies have shown that the
occurrence of IPF and LC share the same genetic mutations and
abnormal activation of signal pathways (12), suggesting a potential link between IPF
and LC.
FGFR signaling pathway is composed of FGFs and
FGFRs, which were expressed in all tissues of the human body and
participate in a variety of physiological processes (13). FGFs circulate through a variety of
secretory pathways (autocrine, paracrine, and endocrine). FGFs bind
to heparin sulfate proteoglycans to protect ligands and assist
FGFRs in the activation of downstream signaling molecules (14). FGFR2 receptor is a tyrosine kinase,
and studies have shown that FGFR2 is closely related to tumor
angiogenesis, tumor metastasis, cancer prognosis, and plays an
important role in target gene therapy (15).
In this study, the expression of FGF2 and FGFR2 in
LC patients and IPF patients was detected at mRNA and protein
levels. We found that FGF2 and FGFR2 expression was significantly
upregulated in cancer tissues compared to the adjacent tissues in
LC patients. Studies have shown that (16) FGF2 is highly expressed in various
cancer tissues, Siegfried et al (17) found that FGF2 is also highly expressed
in patients with non-small cell LC, which is consistent with the
findings in our study. Correlation analysis between the expression
of FGF2 and FGFR2 in cancer tissues of LC patients and patients'
clinicopathological data showed that expression of FGF2 and FGFR2
in LC lung tissues was not significantly correlated with age, sex,
histological types and smoking history, but was significantly
positively correlated with lymph node metastasis and TNM stage
(P<0.05). After the binding of FGFs to FGFRs, their receptors
will dimerize and activate downstream pathways to promote cell
proliferation, invasion, migration, and epithelial-mesenchymal
transition (18). Therefore, we
speculated that the high expression levels of FGFs and FGFRs were
associated with tumor invasion. In this study, the expression
levels of FGF2 and FGFR2 proteins in lavage fluid were also found
to be significantly higher in IPF patients than in the normal
patients.
Studies have shown that (19,20)
upregulation of FGF2 expression plays an important role in the
development of chronic silica dust, silicosis and IPF, and FGF2 is
directly involved in the development of lung damage after
bleomycin-induced lung injury in mice. In addition, studies on
bluntin-induced lung injury in mice showed that FGF2 is directly
involved in cell proliferation and fibrosis formation in mice after
lung injury. Therefore, we hypothesized that neovascularization in
patients with IPF may be mediated by the FGF2/FGFR2 pathway.
However, our study also has some limitations. The
expression of FGF2 and FGFR2 in IPF patients was not detected at
the mRNA level, and the downstream pathways were not investigated.
All patients were from the local region, and regional differences
were not excluded. We will try to detect FGF2 and FGFR2 mRNA in the
peripheral blood of patients with IPF, increase the number of test
items, and increase the sample size in our future studies to
further validate our conclusions.
In conclusion, FGF2 and FGFR2 proteins were highly
expressed in cancer tissues of LC patients and lavage fluid of
patients with IPF. The expression of FGF2 mRNA and FGFR2 mRNA was
correlated with lymph node metastasis and TNM stage. The high
expression levels of FGF2 mRNA and FGFR2 mRNA were associated with
tumor metastasis and poor prognosis of LC patients.
Acknowledgements
Not applicable.
Funding
The study was supported by the Foundation project of
Shanghai Municipal Health and Family Planning Commission 2016
(20164Y0241).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LL drafted the manuscript. LL and SZ were mainly
devoted to collecting and interpreting the basic data of patients.
LW and ZW helped with RT-qPCR. WM, FL and YQ were responsible for
statistical analysis. All authors read and approved the final
study.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Shanghai Pulmonary Hospital (Shanghai, China). Signed informed
consents were obtained from the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zhang Y, Wei X and Pan T: Simultaneous
surgical treatment of non-small cell lung cancer and off-pump
coronary artery bypass grafting. Zhongguo Fei Ai Za Zhi.
12:332–336. 2009.(In Chinese). PubMed/NCBI
|
|
2
|
Sheffield BS, Fulton R, Kalloger SE, Milne
K, Geller G, Jones M, Jacquemont C, Zachara S, Zhao E, Pleasance E,
et al: Investigation of PD-L1 biomarker testing methods for PD-1
axis inhibition in non-squamous non-small cell lung cancer. J
Histochem Cytochem. 64:587–600. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sorber L, Zwaenepoel K, Deschoolmeester V,
van Schil PE, van Meerbeeck J, Lardon F, Rolfo C and Pauwels P:
Circulating cell-free nucleic acids and platelets as a liquid
biopsy in the provision of personalized therapy for lung cancer
patients. Lung Cancer. 107:100–107. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhang X, Liu Y, Shao H and Zheng X:
Obesity paradox in lung cancer prognosis: Evolving biological
insights and clinical implications. J Thorac Oncol. 12:1478–1488.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Richeldi L, Collard HR and Jones MG:
Idiopathic pulmonary fibrosis. Lancet. 389:1941–1952. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Raghu G, Brown KK, Collard HR, Cottin V,
Gibson KF, Kaner RJ, Lederer DJ, Martinez FJ, Noble PW, Song JW, et
al: Efficacy of simtuzumab versus placebo in patients with
idiopathic pulmonary fibrosis: A randomised, double-blind,
controlled, phase 2 trial. Lancet Respir Med. 5:22–32. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Raghu G, Wells AU, Nicholson AG, Richeldi
L, Flaherty KR, Le Maulf F, Stowasser S, Schlenker-Herceg R and
Hansell DM: Effect of nintedanib in subgroups of idiopathic
pulmonary fibrosis by diagnostic criteria. Am J Respir Crit Care
Med. 195:78–85. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Morrissey C, Corey E, Brown L, Coleman I,
Nguyen H, Schweizer M and Nelson P: Targeting the FGFR pathway in
androgen receptor negative castration resistant prostate cancer.
Cancer Res. 77:Abst 2076. 2017.doi:10.1158/1538-7445.AM2017-2076.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Riihimäki M, Hemminki A, Fallah M, Thomsen
H, Sundquist K, Sundquist J and Hemminki K: Metastatic sites and
survival in lung cancer. Lung Cancer. 86:78–84. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Martinez FJ, de Andrade JA, Anstrom KJ,
King TE Jr and Raghu G; Idiopathic Pulmonary Fibrosis Clinical
Research Network: Randomized trial of acetylcysteine in idiopathic
pulmonary fibrosis. N Engl J Med. 370:2093–2101. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hutchinson J: Idiopathic pulmonary
fibrosis: Another step in understanding the burden of this disease.
Eur Respir J. 48:26–28. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen DL, Wang ZQ, Zeng ZL, Wu WJ, Zhang
DS, Luo HY, Wang F, Qiu MZ, Wang DS, Ren C, et al: Identification
of microRNA-214 as a negative regulator of colorectal cancer liver
metastasis by way of regulation of fibroblast growth factor
receptor 1 expression. Hepatology. 60:598–609. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Katoh M and Nakagama H: FGF receptors:
Cancer biology and therapeutics. Med Res Rev. 34:280–300. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Goyal L, Saha SK, Liu LY, Siravegna G,
Leshchiner I, Ahronian LG, Lennerz JK, Vu P, Deshpande V,
Kambadakone A, et al: Polyclonal secondary FGFR2 mutations drive
acquired resistance to FGFR inhibition in patients with FGFR2
fusion-positive cholangiocarcinoma. Cancer Discov. 7:252–263. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li D, Zhang H, Ma L, Han Y, Xu M, Wang Z,
Jiang H, Zhang W, Wang L and Pan Y: Associations between microRNA
binding site SNPs in FGFs and FGFRs and the risk of non-syndromic
orofacial cleft. Sci Rep. 6:310542016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Soulitzis N, Karyotis I, Delakas D and
Spandidos DA: Expression analysis of peptide growth factors VEGF,
FGF2, TGFB1, EGF and IGF1 in prostate cancer and benign prostatic
hyperplasia. Int J Oncol. 29:305–314. 2006.PubMed/NCBI
|
|
17
|
Siegfried JM, Farooqui M, Rothenberger NJ,
Dacic S and Stabile LP: Interaction between the estrogen receptor
and fibroblast growth factor receptor pathways in non-small cell
lung cancer. Oncotarget. 8:24063–24076. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Babina IS and Turner NC: Advances and
challenges in targeting FGFR signalling in cancer. Nat Rev Cancer.
17:318–332. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mori Y, Nakamura S, Kishimoto S, Kawakami
M, Suzuki S, Matsui T and Ishihara M: Preparation and
characterization of low-molecular-weight heparin/protamine
nanoparticles (LMW-H/P NPs) as FGF-2 carrier. Int J Nanomed.
5:147–155. 2010. View Article : Google Scholar
|
|
20
|
Hasday JD, Scheraga RG, Thompson C,
Tulapurkar M, Cowan MJ, Sun JF, Cai RM, Logun C, Todd NW, Shelhamer
J, et al: Heat-Shock accelerates human lung epithelial wound
healing by activating expression of fibroblast growth factor
(FGF)-1: Implications for idiopathic pulmonary fibrosis (IPF). Am J
Respir Crit Care Med. 193:A14612016.
|