Introduction
Extramedullary plasmacytoma (EMP) is rare,
accounting for approximately 3% of all plasma cell neoplasms. Up to
80% of EMP cases occur in the head and neck region, particularly in
the upper aerodigestive tract, which constitutes less than 1% of
head and neck tumors (1,2). Most head and neck EMPs occur in the
sinonasal region, and fewer are found in the larynx (3,4). Although
the primary cause of mortality is actually progression to multiple
myeloma (MM), conversion to MM is uncommon (11–30% incidence).
Here, we describe an individual with laryngeal EMP who developed
acute myeloid leukemia (AML), rather than MM. Due to the rarity of
this tumor, most previous studies focused on a case or case series.
In an effort to describe this rare tumor accurately, we made a
literature review about its clinical features, diagnosis, treatment
modalities, outcomes, and potential sequelae of this disease.
Materials and methods
Literature review
An electronic literature search was performed in
PubMed using the following terms ‘plasmacytoma’, ‘extramedullary
plasmacytoma’, ‘plasma cell tumor’ in combination with the terms
‘larynx or head and neck’. Articles published from January 1948 to
October 2017 were reviewed to identify cases of laryngeal EMP.
Nonhuman, duplicates, and non-English language research were
excluded. Abstracts were first reviewed to screen articles that
discussed cases of laryngeal EMP, and then full-text articles were
reviewed for extraction of data. References of the included studies
were also examined for additional cases. Individual patient data
were collected on age, sex, presentation, site of lesions,
treatment course, long-term follow-up and outcomes. Meanwhile,
articles for which individual patient data was not available or
which focused solely on radiologic, histopathological findings, and
diagnosis, were also excluded.
Statistical analysis
All the recorded treatment modalities are classified
in two main categories: Surgically based treatment including
surgical resection either alone or with adjuvant radiotherapy, and
no-surgically based treatment. Differences between the above two
treatment modalities were analyzed by chi-square test. SPSS version
20 statistical software (IBM Corp., Chicago, Illinois) was used,
and P<0.05 was considered to indicate a statistically
significant difference for all tests.
Ethics statement
This study was approved by the ethics committee of
the Second Xiangya Hospital, Central South University (Changsha,
China). Written informed consent was obtained from the patient.
Results
The initial database search yielded
2,022 studies
The articles that were in non-English language,
animal research, or duplicate articles were excluded, and 270
studies were left. Next, those unrelated abstracts such as solely
focusing on imaging examination or histopathological findings were
eliminated, and a total of 127 articles were left for further
analysis. The articles in which full-text was unavailable or
individual data was incomplete were ruled out. The bibliographies
were also examined for additional cases. Finally, 70 studies
comprising a total of 98 cases were left for analysis. Therefore, a
total of 99 unique patients including our case were identified and
the individual patient data collected are given in Table I (5–71). The
clinical characteristics for the 99 patients included were
summarized in Table II.
 | Table I.List of laryngeal EMP cases included
in analysis. |
Table I.
List of laryngeal EMP cases included
in analysis.
| Author, year | No/sex/age | Primary sites | Treatment | LR or MET | Follow-up | Outcome | (Refs.) |
|---|
| The present
case | 1/M/46 | Epiglottis and
aryepiglottic fold | RT + CT | AML | 61 ms | AWD |
|
| Pino et al,
2015 | 2/M/65 | Left false cord and
ventricle | S + RT | N | 54 ms | ANED | (5) |
| Wang et al,
2015 | 3/M/43 | Glottis,
supraglottis, and subglottis | S | MM | 88 ms | AWD | (6) |
| Haser et al,
2015 | 4/M/72 | Bilaterally vocal
cords and subglottis | RT | N | 1 y | ANED | (7) |
| Xing et al,
2015 | 5/F/47 | Left aryepiglottic
fold | S + RT | N | 18 ms | ANED | (8) |
| Abrari et
al, 2014 | 6/M/56 | Right vocal
cord | RT | N | NA | ANED | (9) |
| Loyo et al,
2013 | 7/F/80 | Right glottis | S | NA | NA | ANED | (10) |
| Ghatak et
al, 2013 | 8/F/29 | True vocal
cord | RT | N | 16 ms | ANED | (11) |
| Kim et al,
2012 | 9/M/58 | Left arytenoid | S | N | 2 ys | ANED | (12) |
| Pinto et al,
2012 | 10/F/49 | Left false
fold | S | N | 1 y | ANED | (13) |
| Ramírez-Anguiano
et al, 2012 | 11/M/57 | Right
subglottis | S + RT | Y | 1 y | ANED | (14) |
| De Zoysa et
al, 2012 | 12/F/62 | Left true vocal
fold | RT | N | 2 ms | ANED | (15) |
| Pichi et al,
2011 | 13/M/73 | Left glottis and
subglottis | RT | MM | 2 ys | DOD | (16) |
| Zhang et al,
2010 | 14/W/56 | Left false vocal
cord and ventricle | S | N | 2 ys | ANED | (17) |
| González Guijarro
et al, 2010 | 15/M/11 | Right
hemilarynx | S + RT | N | 3 ys | ANED | (18) |
| Vanan et al,
2009 | 16/F/16 | Right vocal
cord | RT | N | 1 y | ANED | (19) |
| Pratibha et
al, 2009 | 17/M/49 | False vocal cord,
vocal cord | RT | N | 6 ms | ANED | (20) |
| Iseri et al,
2009 | 18/F/46 | Aryepiglottic
fold | S + RT +CT | N | 2 ys | ANED | (21) |
| Rutherford et
al, 2009 | 19/F/13 | Subglottis,
nasopharynx | S + RT | N | 6 weeks | ANED | (22) |
| Ozbilen Acar et
al, 2008 | 20/F/43 | True vocal
cord | S | N | 2 ys | ANED | (23) |
| Straetmans and
Stokroos, 2008 | 21/M/57 | Epiglottis | S + RT | Y | 27 ms | ANED | (1) |
| Velez et al,
2007 | 22/M/64 | Right
hemilarynx | S + RT | N | 3 ys | ANED | (24) |
| Kusunoki et
al, 2007 | 23/F/76 | Supraglottis | Biopsy | N | 6 ms | AWD | (25) |
| Lewis et al,
2007 | 24/M/71 | Supraglottis, soft
palate | S | N | 2 ys | ANED | (26) |
| Nakashima et
al, 2006 | 25/M/39 | Left arytenoid | S + RT | N | 6 ys | ANED | (27) |
|
| 26/M/59 | Epiglottis | S | N | 15 ys | ANED |
|
| Sakiyama et
al, 2005 | 27/F/47 | Subglottis, the
chest wall | RT + CT | N | 7 ys | ANED | (28) |
| Chao et al,
2005 | 28/M/60 | Supraglotis | RT | N | 37 ms | DOC | (29) |
| Yavas et al,
2004 | 29/F/43 | Left vocal cord,
nasopharynx | RT | NA | NA | NA | (30) |
| Michalaki et
al, 2003 | 30/F/46 | Larynx | RT | N | 49 ms | ANED | (31) |
|
| 31/M/59 | Larynx | RT | N | 67 ms | ANED |
|
| Soni et al,
2002 | 32/M/65 | Subglottis | RT | N | 2 ys | ANED | (32) |
| Kamijo et
al, 2002 | 33/M/84 | False vocal
fold | S + RT | N | 2 years | ANED | (33) |
| Strojan et
al, 2002 | 34/M/65 | Left false vocal
cord | RT | N | 7.8 years | DOC | (34) |
| Strojan et
al, 2002 | 35/M/72 | Right true vocal
cord | S + RT | N | 4.7 ys | DOC |
|
|
| 36/F/50 | Right glottis | RT | N | 2.2 ys | ANED |
|
| Nagasaka et
al, 2001 | 37/F/12 | Right
subglottis | S + RT | N | 4 ys | ANED | (35) |
| Maheshwari et
al, 2001 | 38/M/65 | Subglottis | RT | N | 12 ms | ANED | (36) |
| Uppal and Harrison,
2001 | 39/M/54 | Left
hemilarynx | RT | MM | weeks | DOD | (37) |
| Rakover et
al, 2000 | 40/M/38 | Right true vocal
fold | S + RT | N | 3 ys | ANED | (38) |
| Hotz et al,
1999 | 41/NA/63 | Larynx,
nasopharynx, nasal fossa | S + RT | N | 108 ms | ANED | (39) |
|
| 42/NA/45 | Larynx,
nasopharynx | S + RT | Y | 108 ms | AWD |
|
| Alexiou, 1999 | 43/M/69 | Larynx | S | N | 62 ms | ANED | (3) |
|
| 44/M/40 | Aryepiglottic
fold | S + RT | N | 20 ms | ANED |
|
| Nowak-Sadzikowska
and Weiss, | 45/M/34 | Supraglottis | RT | N | 10 ys | ANED | (40) |
| 1998 | 46/M/50 | Glottis | RT | N | 10 ys | ANED |
|
|
| 47/M/36 | Supraglottis | RT | N | 10 ys | ANED |
|
|
| 48/F/68 | Supraglottis | RT | N | 10 ys | ANED |
|
|
| 49/M/48 | Glottis | RT | N | 10 ys | ANED |
|
| Bhattacharya et
al, 1998 | 50/F/49 | Supraglottis | Biopsy | N | 6
ms | DOC | (41) |
| Sulzner et
al, 1998 | 51/M/49 | Right
aryentoid | RT | N | 5 ys | ANED | (42) |
| Susnerwala,
1997 | 52/F/79 | Larynx | RT | N | 132 ms | ANED | (2) |
|
| 53/M/65 | Larynx | RT | N | 52 ms | ANED |
|
| Rolins et
al, 1995 | 54/M/43 | Epiglottis | S | N | 3 ys | ANED | (43) |
| Mochimatsu et
al, 1993 | 55/M/42 | Epiglottis | S + RT | MM | 12 ys | DOD | (44) |
| Weissman et
al, 1993 | 56/M/76 | Subglotis | S + RT | NA | NA | NA | (45) |
| Barbu et al,
1992 | 57/M/69 | Supraglottis | RT | N | 3 ys | ANED | (46) |
| Kost et al,
1990 | 58/M/43 | Left vocal
cord | RT | NA | NA | NA | (47) |
| Gambino, 1988 | 59/M/47 | Epiglottis | S + RT | NA | NA | NA | (48) |
| Gaffney et
al, 1987 | 60/M/80 | Larynx | RT | N | 7 ms | ANED | (49) |
| Burke et al,
1986 | 61/M/53 | Supraglottis, and
mouth | CT | N | 1 y | ANED | (50) |
| Gadomski et
al, 1986 | 62/F/54 | Bilateral true
vocal cords | S + CT | N | 15 ys | DOC | (51) |
|
| 63/F/51 | Right aryeplottic
fold | RT | N | 5 ys | ANED |
|
| Maniglia and Xue,
1983 | 64/F/64 | Hemilarynx | S + RT | N | 1 y | DOC | (52) |
| Bjelkenkrantz et
al, 1981 | 65/NA | Right false vocal
cord, left tonsil | S + RT | N | 7 ys | ANED | (53) |
| Bush et al,
1981 | 66/F/52 | Epiglottis,
supraorbital region | RT | N | 3 ys | DOC | (54) |
|
| 67/F/34 | Larynx | S + RT | Y | 5.9 ys | ANED |
|
| Singh, et al
1979 | 68/F/42 | Supraglottis | S + RT | N | 29 ms | ANED | (55) |
| Woodruff et
al, 1979 | 69/F/64 | Supraglottis | RT | N | 6.5 ys | DOC | (56) |
|
| 70/F/34 | Supraglottis | RT | N | Recently | ANED |
|
| Petrovich et
al, 1977 | 71/M/74 | Epiglottis | RT | N | 6 ys | ANED | (57) |
| Gorenstein et
al, 1977 | 72/M/58 | Right true vocal
cord | S + RT | N | 3 ys | ANED | (58) |
|
| 73/M/63 | Right true vocal
cord | S + RT | N | 25 ys | ANED |
|
|
| 74/M/59 | Subglottis | S | N | 5 ys | DOC |
|
|
| 75/M/32 | Subglottis | S | N | 10 ys | ANED |
|
|
| 76/M/42 | Bilateral true
cords | S | N | 5 ys | ANED |
|
|
| 77/M/61 | Supraglottis | RT | N | 6 ys | ANED |
|
| Muller and Fisher,
1976 | 78/M/44 | Supraglottis | Biopsy | NA | NA | AWD | (59) |
| Fishkinand
Spiegelberg, 1976 | 79/M/74 | Right
epiglottis | RT | Y | 4 ys | AWD | (60) |
| Stone and Cole,
1971 | 80/M/67 | Left false vocal
fold | RT + CT | N | 10 ms | ANED | (61) |
| Poole and
Marchetta, 1968 | 81/M/41 | Larynx, multiple
sites at autopsy | S + RT | Y | 3 ys 5 ms | DOD | (62) |
| Webb, 1962 | 82M/62 | Left supraglottis,
soft palate | RT | MM | 10 ys | DOD | (63) |
|
| 83/F/55 | Right vocal cord
and ventricle | S | N | 11 ys | ANED |
|
|
| 84/M/32 | Subglottis | S + RT | N | 10 ys | ANED |
|
| Dolin and Dewar,
1956 | 85/M/74 | Larynx | RT | N | 3.5 ys | DOC | (64) |
|
| 86/M/73 | Larynx | S | N | 1 y | ANED |
|
|
| 87/M/59 | Larynx | RT | N | 4 ys | ANED |
|
| Priest, 1952 | 88/M/50 | Larynx, pharynx,
and nose | S | Y | 4 ys | AWD | (65) |
| Ewing and Foote,
1952 | 89/M/76 | Larynx | RT | N | 6 ms | AWD | (66) |
| Costen, 1951 | 90/M/52 | Left
epiglottis | RT | MM | 1 y | AWD | (67) |
| Rawson et
al, 1950 | 91/F/59 | Larynx | S + RT | Y | 11 ys | AWD | (68) |
| Stout and Kenney,
1949 | 92/M/46 | Left epiglottis,
oropharynx | S | Y | 14 ys | ANED | (69) |
|
| 93/F/67 | Epiglottis | RT | Y | 6 ms | DOD |
|
|
| 94/NA | Larynx, nasopharynx
and conjunctiva | S | Y | 3 ys | AWD |
|
|
| 95/M/64 | Larynx,
nasopharynx | S | Y | 2 ys | AWD |
|
|
| 96/F/48 | Larynx,
nasopharynx, and nasal cavity | S | Y | 11 ys | AWD |
|
| Hodge and Wilson,
1948 | 97/M/53 | Left false vocal
cord | S | N | 1 y | ANED | (70) |
| Lumb and Prossor,
1948 | 98/M/34 | Larynx | RT | Y | 30 ms | AWD | (71) |
|
| 99/M/20 | Larynx, palate, and
tongue | S + RT | Y | 7 ys 6 ms | AWD |
|
 | Table II.Clinical features of included
cases. |
Table II.
Clinical features of included
cases.
| Characteristics
(n=95) | Measure, n (%
total) |
|---|
| Patient age, mean,
median (range), years | 53.3, 54
(11–80) |
| Male,
mean (n=65) | 54.9 |
| Female,
mean (n=30) | 50 |
| Symptoms
(n=67) |
|
|
Hoarseness | 46 (69) |
|
Dysphonia | 7 (10) |
|
Dyspnea | 13 (19) |
|
Dysphagia | 9 (13) |
|
Stridor | 6 (9) |
|
Cough | 6 (9) |
| Sore
throat | 3 (4) |
|
Hemoptysis | 3 (4) |
|
Laryngeal foreign body
sensation | 3 (4) |
| Laterality
(n=41) |
|
|
Right | 19 (46) |
|
Left | 17 (41) |
|
Both | 5 (12) |
| Primary site
(n=79) |
|
|
Glottis | 19 (24) |
|
Supraglottis | 41 (52) |
|
Epiglottis | 12 (15) |
|
Aryepiglottic
fold | 4 (5) |
|
Arytenoid | 3 (4) |
|
False vocal
cord | 8 (10) |
|
Multiple
sites | 2 (3) |
|
Unknown detailed
site | 12 (15) |
|
Subglottis | 10 (13) |
|
Hemilarynx or 2–3 parts of the
larynx | 9 (11) |
| Cervical lymph
nodes involvement (n=12) |
|
| Glottic
patient | 1 (8) |
|
Supraglottic patient | 8 (67) |
|
Hemilaryngeal patient | 1 (8) |
| Coexistence with
other body sites involved | 17 |
| Treatment
(n=96) |
|
|
Radiotherapy alone | 41 (43) |
| Surgery
alone | 21 (22) |
|
Chemotherapy alone | 1 (1) |
| Surgery
and radiotherapy | 28 (29) |
|
Radiotherapy and
chemotherapy | 3 (3) |
| Surgery
and chemotherapy | 1 (1) |
|
Radiotherapy, surgery, and
chemotherapy | 1 (1) |
| Radiotherapy dose,
mean, median (range), Gy | 49.6, 50
(30–70) |
| No treatment
(n=3) |
|
| Follow-up, mean,
median (range), ms (n=90) | 60, 45
(1.5–300) |
|
Recurrence or metastasis | 21 (23) |
| No
recurrence or metastasis | 69 (77) |
| MM | 6 (7) |
|
AML | 1 (1) |
| Outcome (n=91) |
|
|
ANED | 63 (69) |
|
AWD | 13 (14) |
|
DOD | 6 (7) |
|
DOC | 9 (10) |
Case presentation
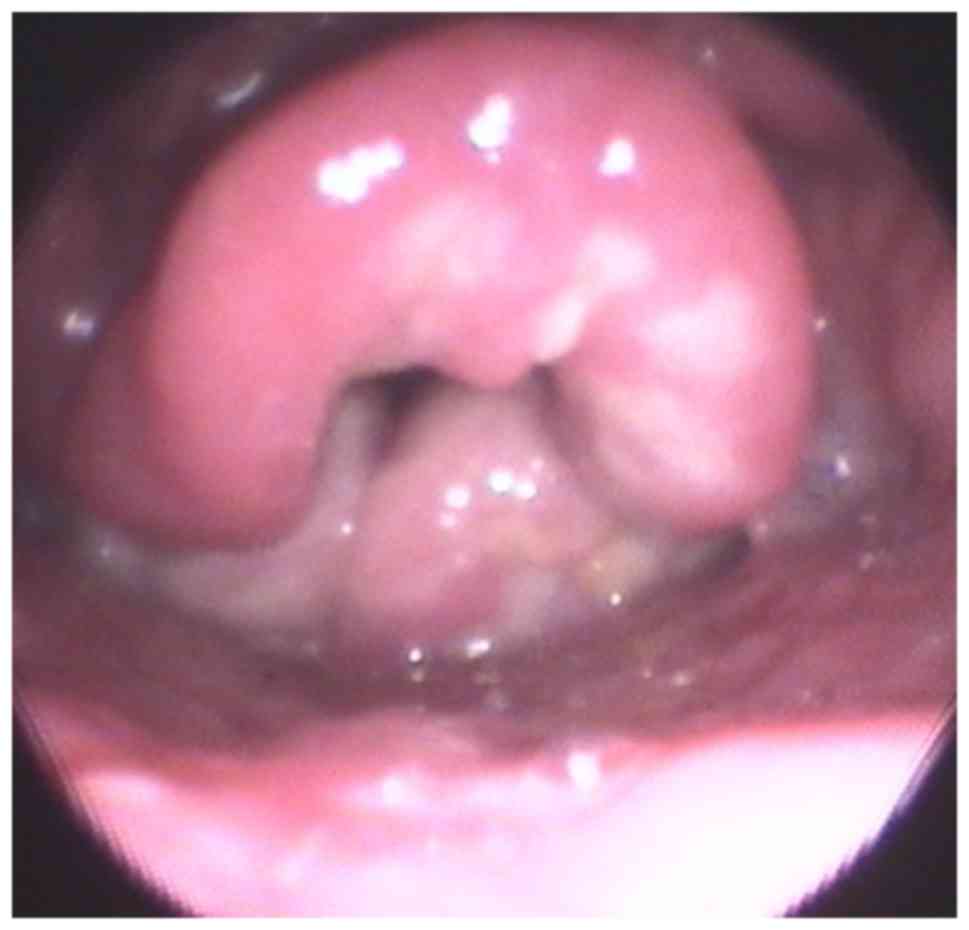
A 46-year old male presented to our hospital with
cough and sore throat of a 4 month duration. He had a history of
hypothyroidism for more than 10 years and received a diagnosis of
tuberculosis before presenting to our hospital, but his symptoms
persisted after anti-tuberculosis treatment. Fiberoptic
laryngoscopy showed swelling of the epiglottis and aryepiglottic
fold (Fig. 1). Laboratory findings
showed an increased erythrocyte sedimentation rate, other
examinations such as anti-tuberculosis antibody test and rheumatoid
factors were normal. Chest X-ray was normal. Computed tomography
(CT) and magnetic resonance imaging (MRI) of the neck revealed
substantial swelling and edema of the epiglottis and enlargement of
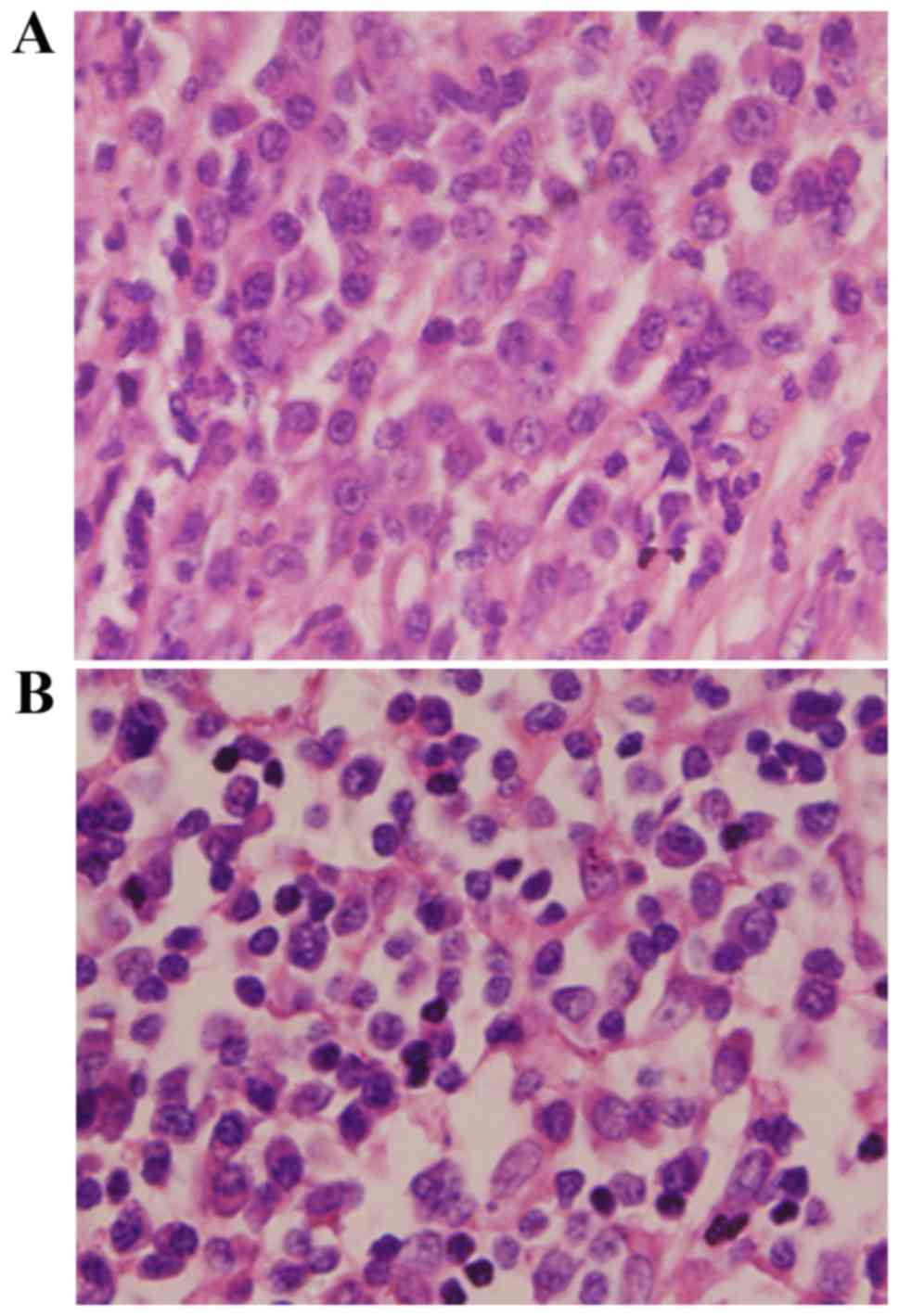
cervical lymph nodes. Biopsy of these two sites was performed under
general anesthesia and microscopic observation showed many
well-differentiated plasma cells and lymphocytes infiltration
(Fig. 2). Immunohistochemical
staining of the laryngeal specimen showed the most cells were
positive for CD79a, CD138, CD38, CD5, Ki67, and Lambda, whereas
negative for CD20, CD3, CD45RO, Cyclin D1, and PAX-5.
Immunohistochemical staining of the cervical lymph nodes showed the
most cells were positive for CD38, CD138, CD79a, CD45RO, CD31,
Ki67, CD68 and LgG. Gene rearrangement studies indicated monoclonal
rearrangements of the immunoglobulin heavy chain. A diagnosis of
EMP of the larynx was made and a series of examinations were
performed to exclude MM. Laboratory examinations including blood
protein electrophoresis, serum immunoglobulins, urinary tests for
Bence-Jones proteins were normal. Report of bone marrow biopsy was
also within the normal range. In addition to cervical
lymphadenopathy, PET-CT and other imaging examinations such as CT
and MRI of the chest, abdomen and pelvis showed no distant
metastasis. Complete surgical resection was not suitable for this
patient, so, he was referred to the Hematology-Oncology Department,
and received radiotherapy including 25 sessions of 55 Gy for
laryngeal lesion and cervical metastasis. Meanwhile, adjuvant
chemotherapy was also given with thalidomide, vincristine,
epirubicin, and cyclophosphamide. His symptoms disappeared after
treatment and he had monthly follow-ups.
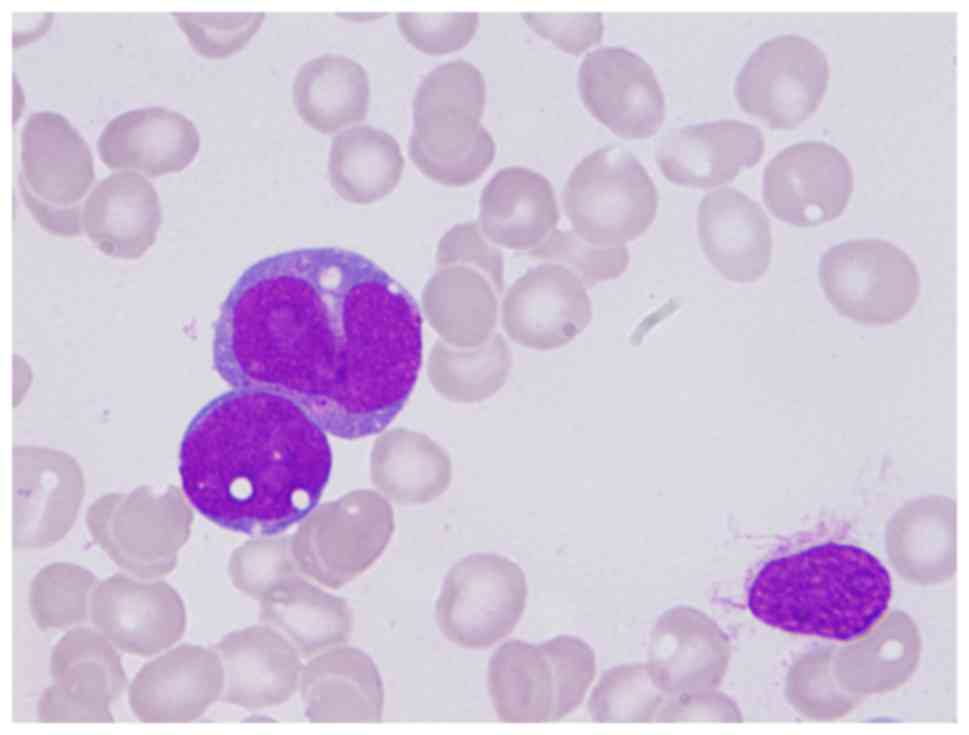
Five years later, he was readmitted with dizziness
that lasted 2 weeks. Complete blood count showed white blood cell
1.94×109/l, red blood cell 1.90×1012/l,
haemoglobin 66 g/l, platelet 16×109/l. Bone marrow
aspiration revealed a hyperplastic marrow: The granulocytes
accounted for 29%, and the myeloblasts accounted for 12.5%; the
mononucytes accounted for 32%, and the monoblasts and promonocytes
accounted for 21% (Fig. 3). The
blasts were positive for myeloperoxidase stain, and positive for
nonspecific esterase, which was inhibited by sodium fluoride.
Immunophenotyping of the bone marrow indicated that a group of
blast cells (accounting for 4.84%) were positive for CD13, CD34,
CD117, HLA-DR and negative for CD7, CD10, CD15, CD19, CD20, CD22,
CD33, CD11b, CD14, CD64; another group of blast cells (accounting
for 53.6%) were positive for CD13, CD33, CD15, CD64, CD11b, and
weak positive for CD10 and CD14. These data are consistent with AML
French-American-British (FAB) classification M4 subtype. Chromosome
karyotype was 46, XY. Then CAG chemotherapy (aclarubicin
hydrochloride, low-dose cytarabine and granulocyte
colony-stimulating factor) combined with decitabine were
administered accordingly and his condition alleviated. This patient
is still being followed.
Patient demographics
We found greater higher occurrence in men and this
was approximately two times more often than in women. The vocal
cords and epiglottis are commonly involved and the main symptom is
hoarseness often accompanied by dyspnea, dysphagia, and other
symptoms. Supraglottic EMP accounted for the majority of patients
with cervical lymphadenopathy. Likely this is due to association
with lymphatic vascularity in the supraglottis, which is much
denser than in the glottis or subglottis, and this causes greater
incidence of lymph node metastasis.
Treatment options
Of 96 recorded treatment modalities, radiotherapy
alone was the most common treatment modality, used in 41 cases,
followed by a combination of surgery and radiotherapy, and surgery
alone. Furthermore, we found that surgically based treatment was
the most common treatment modality for cases published in recent
years (Table III), despite there
was no statistically significant difference between surgically
based treatment and no-surgically based treatment modalities
reported in these annual intervals (P=0.65).
 | Table III.Treatment modalities by annual
interval. |
Table III.
Treatment modalities by annual
interval.
|
| Years |
|---|
|
|
|
|---|
| Treatment
modality | 1948–1989 | 1990–1999 | 2000–2009 | 2010–2017 |
|---|
| Surgically based
treatment (%) | 22 (55) | 7
(41) | 11 (46) | 9 (60) |
| No-surgically based
treatment (%) | 18 (45) | 10 (59) | 13 (54) | 6 (40) |
Outcomes and sequelaes
Overall treatment outcome was favorable, as a total
of 84% of patients were alive after a mean follow-up of 60 months,
independent of treatment modality. However, EMP outcomes for
patients with cervical lymphadenopathy or multiple sites
involvement were unfavorable, more than 40% with recurrence or
metastasis during the limited follow-up period. A total of 21
patients were reported with relapse or metastasis in the clinical
course, among which 12 cases were reported that EMP occurred in
either multiple sites of the larynx or coexistence with other body
sites, and 6 with cervical lymphadenopathy. A total of 6 cases
developed MM finally, of which 3 cases occurred in the multiple
sites of the larynx, and 2 originated in the supraglottis at the
initial visits.
Discussion
EMP of the larynx is an extremely rare plasma cell
neoplasm which constitutes less than 0.2% of the malignancies in
the larynx (3,4). EMP may occur in various sites of the
larynx such as the epiglottis, vocal folds, and subglottis.
Clinical symptoms are closely related to the location of tumor and
the degree of impairment of laryngeal structure. Laryngeal EMP may
present different morphologic forms, sometimes a single, smooth
polypoid mass, and sometimes diffuse swelling tissue just like our
patient. So it is easily misdiagnosed due to the fact that the
clinical symptoms and laryngoscope findings are nonspecific
compared with other diseases such as laryngeal lymphoma and
tuberculosis. Recently, imaging examination has been used more and
more widely. For example, CT and MRI of neck may be used to
identify the location of tumor and cervical lymphadenopathy,
evaluate the involvement of the adjacent structures and curative
effect. PET-CT has been used more and more to understand the nature
of the lesion and the existence of the distant metastasis. Although
radiological findings have acquired much achievement, diagnosis of
EMP mainly relies on histopathologic examination by the presence of
monoclonal plasma cell hyperplasia. However, the diagnosis could
not be made early sometimes by routine pathological observation
alone. Thus, immunohistochemistry and immunophenotype are proposed
to make a definitive diagnosis or differential diagnosis, for
example, most cells may be positive for CD138, CD38, CD79a, and
negative for CD20, CD3 (3,4,35).
Sometimes, immunoglobulin gene rearrangement analysis is also
advised to confirm the diagnosis of EMP.
Given that EMPs are radiosensitive, radiotherapy is
traditionally used as first-line treatment for solitary EMP
(72). Similarly, single-modality
radiotherapy was the most common treatment modality for laryngeal
EMP, followed by a combination of surgery and radiotherapy, and
surgery alone in our analysis. Recently, surgically based
treatment, including surgical resection either alone or with
adjuvant radiotherapy was proposed and proved that it could offer
better survival outcomes compared to radiotherapy alone (3,73). In
contrast, some studies showed no survival benefit for one treatment
modality over another, and even recommended that radical surgery
should be avoided for EMP (74). So
far, the optimal treatment modality for the management of EMP
remains controversial. But it has been generally accepted that
chemotherapy is not considered to be a first-line therapy option
and adjuvant chemotherapy is usually used in patients with
disseminated or recurrent disease, that resembles the present case
(3,72).
In our review, we found radiotherapy alone was the
most common treatment modality for cases published between 1990 and
1999, but for cases reported from 2010 and onward, the most common
treatment modality was surgically based treatment. There may be
some reasons for the shift toward surgical management of small
tumors. On the one hand, surgical techniques advance such as laser
excision application for laryngeal microsurgery has made it
possible to completely resection of lesion through minimally
invasive surgery. On the other hand, patients receiving
radiotherapy for head and neck EMP had a higher conversion to MM
(3), and we found 4 of 6 patients
that developed MM received radiotherapy alone in our review,
therefore, surgical management of laryngeal EMP should be
considered to avoid risk factors for conversion. However, whether
it could offer better survival outcomes compared to radiotherapy
alone is still to be further studied. Furthermore, patient outcomes
may be associated with tumor distribution or cervical
lymphadenopathy in addition to treatment modality. For example,
more than 40% of patients with cervical lymphadenopathy or multiple
sites involvement were reported with recurrence or metastasis, or
even died of disease in our review. In summary, patient outcomes
may be affected by many aspects, and management of laryngeal EMP
should also be considered on a case-by-case basis. Factors such as
tumor location; histological grade; regional lymphadenopathy;
feasibility of complete resection; laryngeal function; and
potential risk of recurrence or conversion to MM should be
considered when determining the most suitable treatment
modality.
EMPs tend to have more favorable outcomes than
solitary bone plasmacytomas or MM, and overall survival for 10
years is estimated to exceed 70% (73). We noted that 84% of patients in our
analysis were alive after a mean follow-up of 60 months. However,
we also found that patients with cervical lymphadenopathy, multiple
anatomical regions of the larynx or other organ involvement may be
prone to relapse or metastasis. The highest risk of conversion to
MM is reported to be in the first 2 years after diagnosis, but
conversion has also been noted more than 15 years later (4). In our analysis, 3 patients developed MM
in the first 2 years, and 1 subject developed MM 12 years later.
Although there is debate about high risk factors of conversion to
MM, once converted to MM, patients have poor prognosis, and fewer
than 10% of patients survive 10 years (3). Therefore, progression to MM maybe a poor
prognostic factor or a determinant factor for survival. Few
patients developed MM in our analysis, and this was less than the
expected range. This may be due to the relatively short follow-up
for most cases. Therefore, follow-up and regular screening for MM
is important.
To the best of our knowledge, this is the first case
of laryngeal EMP who subsequently developed AML. On one hand, AML,
as the primary second tumor, may occur subsequent to plasma cell
myeloma or MM. On the other hand, the occurrence of AML in this
case maybe closely related to chemotherapy or radiotherapy, and so
it is referred to as therapy-related AML (t-AML). At this time, it
is unclear whether this represents an intrinsic predisposition or
therapy-related phenomenon (75).
Similarly, the pathologic procedure and pathogenesis for this case
are unclear and must be elucidated. Even so, this unusual case
provides evidence that laryngeal EMP may develop therapy-related
myeloid neoplasms (t-MNs) even though this is rare.
In conclusion, we present a comprehensive literature
review spanning 60 years to increase awareness of laryngeal EMP.
Our findings suggest radiotherapy alone is the most common
treatment modality, but surgically based treatment has been the
most common treatment modality in recent years. EMP localized to a
single region of the larynx may have good outcomes. In addition to
MM, t-MNs should be considered during the follow-up period. Due to
the inherent limitations of this review, further study about
optimal treatment modalities should be considered with randomized
controlled clinical trials.
Acknowledgements
The authors would like to thank Dr Xunqiang Yin
(School of Public Health, Central South University, Changsha,
China) for his help in the statistical analysis of the paper and
Professor Xinming Yang (Department of Otolaryngology-Head and Neck
Surgery, The Second Xiangya Hospital, Changsha, China) for his
assistance in the drafting and revision of the manuscript.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant nos. 81100360 and
30700940).
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
YY conceived this study, interpreted the results and
revised the manuscript. SG analyzed the literature data and wrote
the manuscript. GZ performed the data collection and analysis. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
The Second Xiangya Hospital, Central South University and written
informed consent was obtained from the patient.
Patient consent for publication
Written informed consent was obtained from the
patient consent for the publication of their data and associated
images.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
EMP
|
extramedullary plasmacytoma
|
|
MM
|
multiple myeloma
|
|
AML
|
acute myeloid leukemia
|
|
t-AML
|
therapy-related acute myeloid
leukemia
|
|
MN
|
myeloid neoplasm
|
|
t-MNs
|
therapy-related myeloid neoplasms
|
References
|
1
|
Straetmans J and Stokroos R:
Extramedullary plasmacytomas in the head and neck region. Eur Arch
Otorhinolaryngol. 265:1417–1423. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Susnerwala SS, Shanks JH, Banerjee SS,
Scarffe JH, Farrington WT and Slevin NJ: Extramedullary
plasmacytoma of the head and neck region: Clinicopathological
correlation in 25 cases. Br J Cancer. 75:921–927. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Alexiou C, Kau RJ, Dietzfelbinger H,
Kremer M, Spiess JC, Schratzenstaller B and Arnold W:
Extramedullary plasmacytoma: Tumor occurrence and therapeutic
concepts. Cancer. 85:2305–2314. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bachar G, Goldstein D, Brown D, Tsang R,
Lockwood G, Perez-Ordonez B and Irish J: Solitary extramedullary
plasmacytoma of the head and neck-long-term outcome analysis of 68
cases. Head Neck. 30:1012–1019. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pino M, Farri F, Garofalo P, Taranto F,
Toso A and Aluffi P: Extramedullary plasmacytoma of the larynx
treated by a surgical endoscopic approach and radiotherapy. Case
Rep Otolaryngol. 2015:9515832015.PubMed/NCBI
|
|
6
|
Wang M, DU J, Zou J and Liu S:
Extramedullary plasmacytoma of the cricoid cartilage progressing to
multiple myeloma: A case report. Oncol Lett. 9:1764–1766. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Haser GC, Su HK, Pitman MJ and Khorsandi
AS: Extramedullary plasmacytoma of the cricoid cartilage with
solitary plasmacytoma of the rib. Am J Otolaryngol. 36:598–600.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Xing Y, Qiu J, Zhou ML, Zhou SH, Bao YY,
Wang QY and Zheng ZJ: Prognostic factors of laryngeal solitary
extramedullary plasmacytoma: A case report and review of
literature. Int J Clin Exp Pathol. 8:2415–2435. 2015.PubMed/NCBI
|
|
9
|
Abrari A and Bakshi V: Anaplastic:
Plasmablastic plasmacytoma of the vocal cord. Indian J Pathol
Microbiol. 57:659–660. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Loyo M, Baras A and Akst LM: Plasmacytoma
of the larynx. Am J Otolaryngol. 34:172–175. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ghatak S, Dutta M, Kundu I and Ganguly RP:
Primary solitary extramedullary plasmacytoma involving the true
vocal cords in a pregnant woman. Tumori. 99:e14–e18. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kim KS, Yang HS, Park ES and Bae TH:
Solitary extramedullary plasmacytoma of the apex of arytenoid:
Endoscopic, CT, and pathologic findings. Clin Exp Otorhinolaryngol.
5:107–111. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pinto JA, Sônego TB, Artico MS, Cde Leal F
and Bellotto S: Extramedullary plasmacytoma of the larynx. Int Arch
Otorhinolaryngol. 16:410–413. 2012.PubMed/NCBI
|
|
14
|
Ramírez-Anguiano J, Lara-Sánchez H,
Martínez-Baños D and Martínez-Benítez B: Extramedullary
plasmacytoma of the larynx: A case report of subglottic
localization. Case Rep Otolaryngol. 2012:4372642012.PubMed/NCBI
|
|
15
|
De Zoysa N, Sandler B, Amonoo-Kuofi K,
Swamy R, Kothari P and Mochloulis G: Extramedullary plasmacytoma of
the true vocal fold. Ear Nose Throat J. 91:E23–E25. 2012.PubMed/NCBI
|
|
16
|
Pichi B, Terenzi V, Covello R and Spriano
G: Cricoid-based extramedullary plasmocytoma. J Craniofac Surg.
22:2361–2363. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang XL, Li DQ, Li JJ, Li SS and Yang XM:
Synchronous occurrence of extramedullary plasmacytoma and squamous
cell carcinoma in situ in the larynx: A case report. Chin J Cancer.
29:1029–1034. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Guijarro González I, Díez González L,
Acevedo Rodriguez N and Pallas Pallas E: Extramedullary
plasmacytoma of the larynx. A case report. Acta Otorrinolaringol
Esp. 62:320–322. 2011.(In Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Vanan I, Redner A, Atlas M, Marin L,
Kadkade P, Bandovic J and Jaffe ES: Solitary extramedullary
plasmacytoma of the vocal cord in an adolescent. J Clin Oncol.
27:e244–e247. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Pratibha CB, Sreenivas V, Babu MK, Rout P
and Nayar RC: Plasmacytoma of larynx-a case report. J Voice.
23:735–738. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Iseri M, Ozturk M and Ulubil SA:
Synchronous presentation of extramedullary plasmacytoma in the
nasopharynx and the larynx. Ear Nose Throat J. 88:E9–12.
2009.PubMed/NCBI
|
|
22
|
Rutherford K, Parsons S and Cordes S:
Extramedullary plasmacytoma of the larynx in an adolescent: A case
report and review of the literature. Ear Nose Throat J. 88:E1–E7.
2009.PubMed/NCBI
|
|
23
|
Acar Ozbilen G, Yilmaz S, Güven Güvenc M,
Yilmaz M, Ozek H and Tüziner N: Isolated extramedullary
plasmacytoma of the true vocal cord. J Otolaryngol Head Neck Surg.
37:E129–E132. 2008.PubMed/NCBI
|
|
24
|
Velez D, Hinojar-Gutierrez A, Nam-Cha S
and Acevedo-Barbera A: Laryngeal plasmacytoma presenting as amyloid
tumour: A case report. Eur Arch Otorhinolaryngol. 264:959–961.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kusunoki T, Ikeda K, Murata K, Nishida S
and Tsubaki M: Extramedullary plasmacytoma of the larynx: a case
report from Japan. Ear Nose Throat J. 86:763–764. 2007.PubMed/NCBI
|
|
26
|
Lewis K, Thomas R, Grace R, Moffat C,
Manjaly G and Howlett DC: Extramedullary plasmacytomas of the
larynx and parapharyngeal space: Imaging and pathologic features.
Ear Nose Throat J. 86:567–569. 2007.PubMed/NCBI
|
|
27
|
Nakashima T, Matsuda K and Haruta A:
Extramedullary plasmacytoma of the larynx. Auris Nasus Larynx.
33:219–222. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Sakiyama S, Kondo K, Mitsuteru Y, Takizawa
H, Kenzaki K, Miyoshi T, Abe M, Wakatsuki S and Monden Y:
Extramedullary plasmacytoma immunoglobulin D (lambda) in the chest
wall and the subglottic region. J Thorac Cardiovasc Surg.
129:1168–1169. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chao MW, Gibbs P, Wirth A, Quong G, Guiney
MJ and Liew KH: Radiotherapy in the management of solitary
extramedullary plasmacytoma. Intern Med J. 35:211–215. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Yavas O, Altundag K and Sungur A:
Extramedullary plasmacytoma of nasopharynx and larynx: Synchronous
presentation. Am J Hematol. 75:264–265. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Michalaki VJ, Hall J, Henk JM, Nutting CM
and Harrington KJ: Definitive radiotherapy for extramedullary
plasmacytomas of the head and neck. Br J Radiol. 76:738–741. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Soni NK, Trivedi KA, Kumar A, Prajapati
JA, Goswami JV, Patel JJ and Patel DD: Solitary extramedullary
plasmacytoma-larynx. Indian J Otolaryngol Head Neck Surg.
54:309–310. 2002.PubMed/NCBI
|
|
33
|
Kamijo T, Inagi K, Nakajima M, Motoori T,
Tadokoro K and Nishiyama S: A case of extramedullary plasmacytoma
of the larynx. Acta Otolaryngol Suppl. 104–106. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Strojan P, Soba E, Lamovec J and Munda A:
Extramedullary plasmacytoma: Clinical and histopathologic study.
Int J Radiat Oncol Biol Phys. 53:692–701. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Nagasaka T, Lai R, Kuno K, Nakashima T and
Nakashima N: Localized amyloidosis and extramedullary plasmacytoma
involving the larynx of a child. Hum Pathol. 32:132–134. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Maheshwari GK, Baboo HA, Gopal U and Shah
NM: Extramedullary plasmacytoma of the larynx: A case report. J
Indian Med Assoc. 99:267–268. 2001.PubMed/NCBI
|
|
37
|
Uppal HS and Harrison P: Extramedullary
plasmacytoma of the larynx presenting with upper airway obstruction
in a patient with long-standing IgD myeloma. J Laryngol Otol.
115:745–746. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Rakover Y, Bennett M, David R and Rosen G:
Isolated extramedullary plasmacytoma of the true vocal fold. J
Laryngol Otol. 114:540–542. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hotz MA, Schwaab G, Bosq J and Munck JN:
Extramedullary solitary plasmacytoma of the head and neck. A
clinicopathological study. Ann Otol Rhinol Laryngol. 108:495–500.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Nowak-Sadzikowska J and Weiss M:
Extramedullary plasmacytoma of the larynx. Analysis of 5 cases. Eur
J Cancer. 34:14681998.PubMed/NCBI
|
|
41
|
Bhattacharya AK, Han K and Baredes S:
Extramedullary plasmacytoma of the head and neck associated with
the human immunodeficiency virus. Ear Nose Throat J. 77:61–62.
1998.PubMed/NCBI
|
|
42
|
Sulzner SE, Amdur RJ and Weider DJ:
Extramedullary plasmacytoma of the head and neck. Am J Otolaryngol.
19:203–208. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Rolins H, Levin M, Goldberg S, Mody K and
Forte FJ: Solitary extramedullary plasmacytoma of the epiglottis: A
case report and review of the literature. Otolaryngol Head Neck
Surg. 112:754–757. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Mochimatsu I, Tsukuda M, Sawaki S and
Nakatani Y: Extramedullary plasmacytoma of the larynx. J Laryngol
Otol. 107:1049–1051. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Weissman JL, Myers JN and Kapadia SB:
Extramedullary plasmacytoma of the larynx. Am J Otolaryngol.
14:128–131. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Barbu RR, Khan A, Port JL, Abramson A and
Gartenhaus WS: Case report: Extramedullary plasmacytoma of the
larynx. Comput Med Imaging Graph. 16:359–361. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Kost KM: Plasmacytomas of the larynx. J
Otolaryngol. 19:141–146. 1990.PubMed/NCBI
|
|
48
|
Gambino DR: Pathologic quiz case 2.
Extramedullary plasmacytoma. Arch Otolaryngol Head Neck Surg.
114(92–93): 951988.
|
|
49
|
Gaffney CC, Dawes PJ and Jackson D:
Plasmacytoma of the head and neck. Clin Radiol. 38:385–388. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Burke WA, Merritt CC and Briggaman RA:
Disseminated extramedullary plasmacytomas. J Am Acad Dermatol.
14:335–339. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Gadomski SP, Zwillenberg D and Choi HY:
Non-epidermoid carcinoma of the larynx: The Thomas Jefferson
University experience. Otolaryngol Head Neck Surg. 95:558–565.
1986. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Maniglia AJ and Xue JW: Plasmacytoma of
the larynx. Laryngoscope. 93:741–744. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Bjelkenkrantz K, Lundgren J and Olofsson
J: Extramedullary plasmacytoma of the larynx. J Otolaryngol.
10:28–34. 1981.PubMed/NCBI
|
|
54
|
Bush SE, Goffinet DR and Bagshaw MA:
Extramedullary plasmacytoma of the head and neck. Radiology.
140:801–805. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Singh B, Lahiri AK and Kakar PK:
Extramedullary plasmacytoma. J Laryngol Otol. 93:1239–1244. 1979.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Woodruff RK, Whittle JM and Malpas JS:
Solitary plasmacytoma. I: Extramedullary soft tissue plasmacytoma.
Cancer. 43:2340–2343. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Petrovich Z, Fishkin B, Hittle RE,
Acquarelli M and Barton R: Extramedullary plasmacytoma of the upper
respiratory passages. Int J Radiat Oncol Biol Phys. 2:723–730.
1977. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Gorenstein A, Neel HB, Devine KD and
Weiland LH: Solitary extramedullary plasmacytoma of the larynx.
Arch Otolaryngol. 103:159–161. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Muller SP and Fisher GH: Pathologic quiz
case 1: Extramedullary plasmacytoma of the larynx. Arch
Otolaryngol. 102:442–444. 1976.PubMed/NCBI
|
|
60
|
Fishkin BG and Spiegelberg HL: Cervical
lymph node metastasis as the first manifestation of localized
extramedullary plasmacytoma. Cancer. 38:1641–1644. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Stone HB III and Cole TB: Extramedullary
plasmacytomas of the head and neck. South Med J. 64:1386–1388.
1971. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Poole AG and Marchetta FC: Extramedullary
plasmacytoma of the head and neck. Cancer. 22:14–21. 1968.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Webb HE, Harrison EG, Masson JK and Remine
WH: Solitary extramedullary myeloma (plasmacytoma) of the upper
part of the respiratory tract and oropharynx. Cancer. 15:1142–1155.
1962. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Dolin S and Dewar JP: Extramedullary
plasmacytoma. Am J Pathol. 32:83–103. 1956.PubMed/NCBI
|
|
65
|
Priest RE: Extramedullary plasma cell
tumors of the nose, pharynx and larynx: A case report.
Laryngoscope. 62:277–283. 1952. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Ewing MR and Foote FW Jr: Plasma-cell
tumors of the mouth and upper air passages. Cancer. 5:499–513.
1952. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Costen JB: Plasmocytoma: A case with
original lesion of the epiglottis and metastasis to the tibia.
Laryngoscope. 61:266–270. 1951. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Rawson AJ, Eyler PW and Horn RC Jr: Plasma
cell tumors of the upper respiratory tract; a clinico-pathologic
study with emphasis on criteria for histologic diagnosis. Am J
Pathol. 26:445–461. 1950.PubMed/NCBI
|
|
69
|
Stout AP and Kenney FR: Primary
plasma-cell tumors of the upper air passages and oral cavity.
Cancer. 2:261–278. 1949. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Hodge GE and Wilson T: Extramedullary
plasmocytoma of the larynx. Can Med Assoc J. 59:1651948.PubMed/NCBI
|
|
71
|
Lumb G and Prossor TM: Plasma cell
tumours. J Bone Joint Surg Br. 30B:124–152. 1948. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
D'Aguillo C, Soni RS, Gordhan C, Liu JK,
Baredes S and Eloy JA: Sinonasal extramedullary plasmacytoma: A
systematic review of 175 patients. Int Forum Allergy Rhinol.
4:156–163. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Gerry D and Lentsch EJ: Epidemiologic
evidence of superior outcomes for extramedullary plasmacytoma of
the head and neck. Otolaryngol Head Neck Surg. 148:974–981. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Soutar R, Lucraft H, Jackson G, Reece A,
Bird J, Low E and Samson D: Guidelines Working Group of the UK
Myeloma Forum; British Committee for Standards in Haematology;
British Society for Haematology: Guidelines on the diagnosis and
management of solitary plasmacytoma of bone and solitary
extramedullary plasmacytoma. Br J Haematol. 124:717–726. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Reddi DM, Lu CM, Fedoriw G, Liu YC, Wang
FF, Ely S, Boswell EL, Louissaint A Jr, Arcasoy MO, Goodman BK and
Wang E: Myeloid neoplasms secondary to plasma cell myeloma: an
intrinsic predisposition or therapy-related phenomenon? A
clinicopathologic study of 41 cases and correlation of cytogenetic
features with treatment regimens. Am J Clin Pathol. 138:855–866.
2012. View Article : Google Scholar : PubMed/NCBI
|