Introduction
Lung cancer is a malignant tumor with the highest
mortality rate in the world, with a prevalence of approximately
2–3:1 in men and women (1). With
industrial development, the incidence and mortality rate of lung
cancer are still rising (2). Radical
operation is the main treatment of lung cancer and is the only way
to cure lung cancer at present. However, it causes severe trauma to
the body and intense stimulation to the organ, which can easily
lead to a strong stress response in the body and cause a decrease
in immune function. While the autoimmune function of patients with
lung cancer is lower than healthy people, which is one of the
important factors leading to the not ideal results in radical
resection of lung cancer treatment (3–5).
Anesthesia is one of the most important auxiliary
means of surgery. Appropriate anesthesia has a decisive
significance in maintaining vital signs of patients and in helping
perioperative patients (6). However,
the current use of various narcotic drugs is not ideal, in order to
improve this deficiency, combined anesthesia came into being
(7). Combined anesthesia, also known
as balanced anesthesia, is the combination of two or more narcotic
drugs or anesthesia method in order to improve perioperative
analgesia effect and surgical conditions (8). Combined general epidural anesthesia is
currently the main method of combined anesthesia, it can reduce the
use of anesthetic drugs in surgery, can improve the analgesic
effect, reduce side effects and adverse reactions, improve surgical
safety, and also eliminate the fear and tension of patients, reduce
stress response, improve patient immune function (9,10).
The purpose of this study was to investigate the
effects of intravenous combined epidural anesthesia on patients
with lung cancer undergoing radical surgery and to investigate the
effects of intravenous combined epidural anesthesia on immune
function in patients with lung cancer by dynamically monitoring the
changes of CD3+, CD4+ and
CD4+CD25+.
Materials and methods
Patients
A total of 122 patients undergoing radical resection
of lung cancer treated in Zhejiang Cancer Hospital (Hangzhou,
China) from September 2013 to April 2016 were randomly divided into
two groups: Combined anesthesia group and intravenous anesthesia
group, 61 cases in each group. Patients in the combined anesthesia
group received intravenous combined epidural anesthesia. Patients
in the intravenous anesthesia group were given intravenous
anesthesia alone. Inclusion criteria were: Patients in Zhejiang
Cancer Hospital pathology department; no past history of tumor,
diagnosed and received a series of tests and treatment in Zhejiang
Cancer Hospital, willing to cooperate with medical staff in
Zhejiang Cancer Hospital. Exclusion criteria were: Patients with
other cardiovascular and cerebrovascular diseases, patients with
other gastrointestinal diseases, patients who were transferred
midway through the course of treatment or taking antibiotics not
prescribed by Zhejiang Cancer Hospital or those who had been
treated in a non-hospital setting for rehabilitation. This study
was approved by the Zhejiang Cancer Hospital Ethics Committee.
Written informed consents were collected and signed by the
patients.
Treatment method
Intravenous anesthesia group was given simple
intravenous anesthesia. Combined anesthesia group was given
intravenous combined epidural anesthesia. All patients were given
intramuscular injection of midazolam (0.05 mg/kg, H10980025;
Jiangsu Enhua Pharmaceutical Co., Ltd., Xuzhou, China) and atropine
(0.5 mg/patient, H44024022; Guangdong Nanguo Pharmaceutical Co.,
Ltd., Zhanjiang, China) for 30 min before entering the operating
room, and GT6800-12 monitor (Hunan Yimin Sunshine Technology Co.,
Ltd., Hunan, China) was used for monitoring of vital signs and
timely establishment of venous fluid path. Anesthesia was induced
by intravenous injection of fentanyl (2 µg/kg, H42022076; Yichang
Renfu Pharmaceutical Co., Ltd., Yichang, China) and propofol (2
mg/kg, H20163040; Xi'an Libang Pharmaceutical Co., Ltd.). After the
patient lost consciousness, atracurium (0.5 mg/kg, H20090202;
Zhejiang Xianju Pharmaceutical Co., Ltd., Zhejiang, China) was
given until the patient's vital signs became stable and then
tracheal intubation was performed.
Intravenous anesthesia: Intravenous
target-controlled infusion of remifentanil (0.02 µg/kg/min,
H20143314; Yichang Renfu Pharmaceutical Co., Ltd.) combined with
propofol (0.05 µg/kg/min) maintaining anesthesia until 10 min prior
to surgery with intermittent administration of atracurium (0.1
mg/kg).
Intravenous combined epidural anesthesia: After
endotracheal intubation, epidural puncture was performed in the
waist 5 to the waist 6 or waist 6 to the waist 7 levels of local
administration of 1% lidocaine (5 ml, H41023668; Sui Cheng
Pharmaceutical Co., Ltd.). Intraoperative target-controlled
infusion of propofol (0.05 µg/kg/min) was performed to maintain
anesthesia while administering 0.375% ropivacaine every 30 min (5
ml, H20113381; Guangdong Jiabo Pharmaceutical Co., Ltd., Guangzhou,
China) till 10 min before the end of the surgery, and atracurium
was given intermittently (0.1 mg/kg).
Observation indicators
Peripheral blood samples were collected before
anesthesia (T0), immediately after anesthesia (T1), after operation
(T2), 24 h after operation (T3) and 72 h after operation (T4), and
CD3+, CD4+ and
CD4+CD25+ levels were detected at all 5
time-points using a MACSQuant flow cytometer from Gene Tech Co.,
Ltd. (Hong Kong, China).
Statistical analysis
Statistical methods: SPSS 22.0 software (IBM Corp.,
Armonk, NY, USA) was used for statistical analysis. Enumeration
data were expressed as n (%) and were examined by χ2
test. Measurement data were expressed as mean ± SD. Comparison
between multiple groups was done using One-way ANOVA test followed
by post hoc test (Least Significant Difference). P<0.05 for the
difference was considered statistically significant.
Results
General information
There were 122 patients in line with the inclusion
criteria, 61 cases in intravenous anesthesia group. There were 36
male and 25 female patients, mean age 53.5±6.4 years, 61 cases of
joint anesthesia group, including 38 males and 23 females, mean age
54.3±6.6 years (Table I). There was
no significant difference in gender proportion and average age
between the two groups (P>0.05). Body mass index, operation time
and preoperative life parameters of two groups of patients showed
no difference (P>0.05).
 | Table I.Clinical data comparison of two
groups. |
Table I.
Clinical data comparison of two
groups.
| Items | Intravenous
anesthesia | Combined
anesthesia | t/χ2
value | P-value |
|---|
| No. of
patients | 61 | 61 |
|
|
| Sex |
|
| 0.371 | 0.711 |
|
Male | 36 | 38 |
|
|
|
Female | 25 | 23 |
|
|
| Age (years) | 53.5±6.4 | 54.3±6.6 | 0.680 | 0.498 |
| BMI
(kg/m2) | 24.82±10.13 | 25.17±10.46 | 0.188 | 0.851 |
| Operation time
(min) | 81.13±12.56 | 81.75±12.72 | 0.271 | 0.787 |
| Preoperative
diastolic blood pressure (mmHg) | 78.25±7.33 | 78.36±7.45 | 0.082 | 0.934 |
| Preoperative
systolic blood pressure (mmHg) | 133.46±14.12 | 133.17±13.69 | 0.115 | 0.909 |
| Preoperative heart
rate (beats/min) | 78.29±9.17 | 78.48±9.36 | 0.113 | 0.910 |
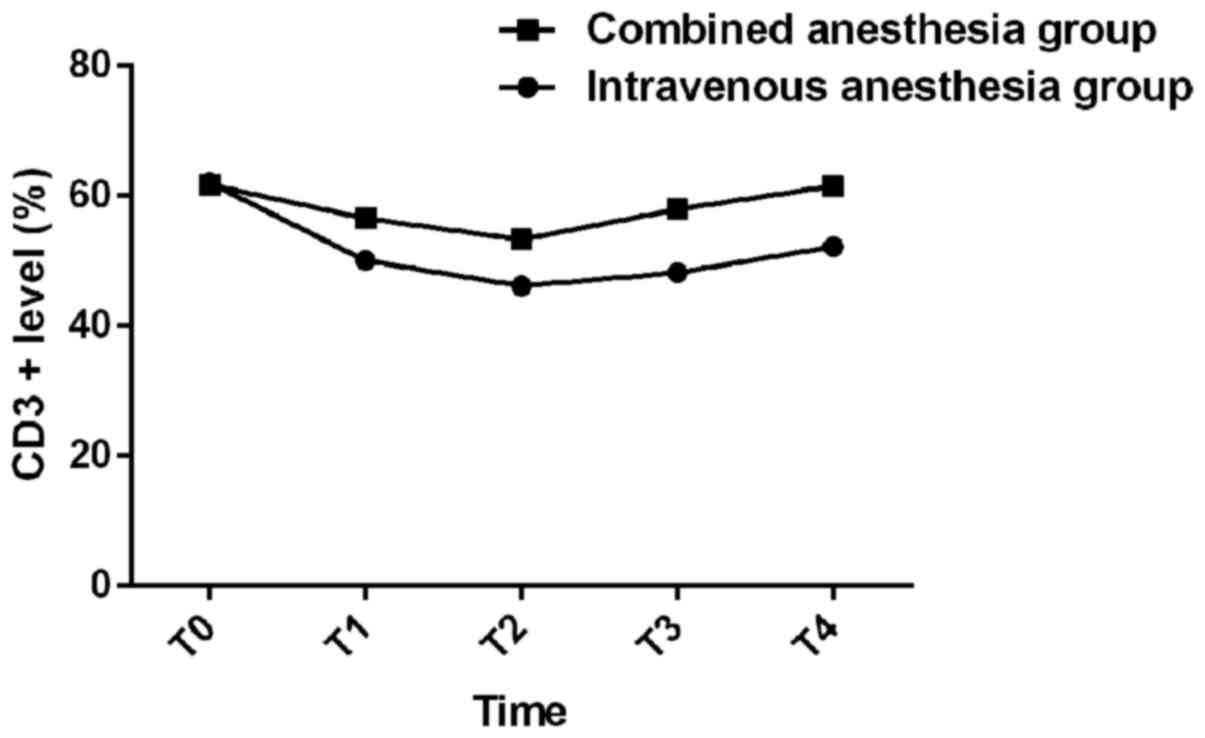
Analysis of T0, T1, T2, T3 and T4
CD3+ levels in the groups
There was no difference in CD3+ level at
T0 between the two groups (P>0.05). CD3+ levels at
T1, T2, T3 and T4 were significantly higher in the combined
anesthesia group than those in the intravenous anesthesia group
(P<0.05). The level of CD3+ at T2 and T1 was lower
than that at T0 (P<0.05), and the level of CD3+ at T2
was lower than that at T1 (P<0.05). After T3, the level of
CD3+ increased in both groups; the levels of
CD3+ at T3 and T4 were higher in both groups than those
in T2 and T1 (P<0.05). The levels of CD3+ at T4 were
higher than those at T3 in both groups (P<0.05). All
CD3+ levels at T3 and T4 were lower than T0 in both
groups (P<0.05) (Table II).
 | Table II.CD3+ level analysis at T0,
T1, T2, T3 and T4 (%). |
Table II.
CD3+ level analysis at T0,
T1, T2, T3 and T4 (%).
| Items | Intravenous
anesthesia | Combined
anesthesia | t-value | P-value |
|---|
| No. of
patients | 61 | 61 |
|
|
| T0a | 62.03±10.15 | 61.79±10.16 | 0.131 | 0.896 |
| T1b | 50.13±8.14 | 56.58±8.38 | 4.312 | <0.001 |
| T2c | 46.14±6.94 | 53.28±7.48 | 5.465 | <0.001 |
| T3d | 48.25±8.15 | 57.97±8.67 | 6.380 | <0.001 |
| T4e | 52.24±8.13 | 61.59±8.48 | 6.216 | <0.001 |
Analysis of CD4+ levels in
two groups at T0, T1, T2, T3 and T4
There was no significant difference in
CD4+ level between two groups at T0 (P>0.05).
CD4+ levels at T1, T2, T3 and T4 were significantly
higher in the combined anesthesia group than those in the
intravenous anesthesia group (P<0.05). After the start of
anesthesia, CD4+ levels of both groups started to
decrease. CD4+ levels at T2 and T1 were lower than those
at T0 (P<0.05), and CD4+ levels at T2 were lower than
those at T1 (P<0.05). After T3, the levels of CD4+ in
both groups began to increase (P<0.05); the levels of
CD4+ in both groups at T3 and T4 were higher than those
at T2 and T1 (P<0.05). The levels of CD4+ at T4 were
higher in both groups than those at T3 (P<0.05), but the level
of CD4+ at T3 and T4 were lower than those at T0
(P<0.05) (Table III).
 | Table III.CD4+ level analysis at T0,
T1, T2, T3 and T4 (%). |
Table III.
CD4+ level analysis at T0,
T1, T2, T3 and T4 (%).
| Items | Intravenous
anesthesia | Combined
anesthesia | t-value | P-value |
|---|
| No. of
patients | 61 | 61 |
|
|
| T0a | 39.12±7.04 | 39.17±7.01 | 0.039 | 0.969 |
| T1b | 30.03±6.19 | 34.22±6.73 | 3.579 | <0.001 |
| T2c | 26.13±6.32 | 31.82±6.91 | 4.746 | <0.001 |
| T3d | 30.97±5.12 | 35.88±5.38 | 5.163 | <0.001 |
| T4e | 34.01±4.84 | 37.69±5.13 | 4.075 | <0.001 |
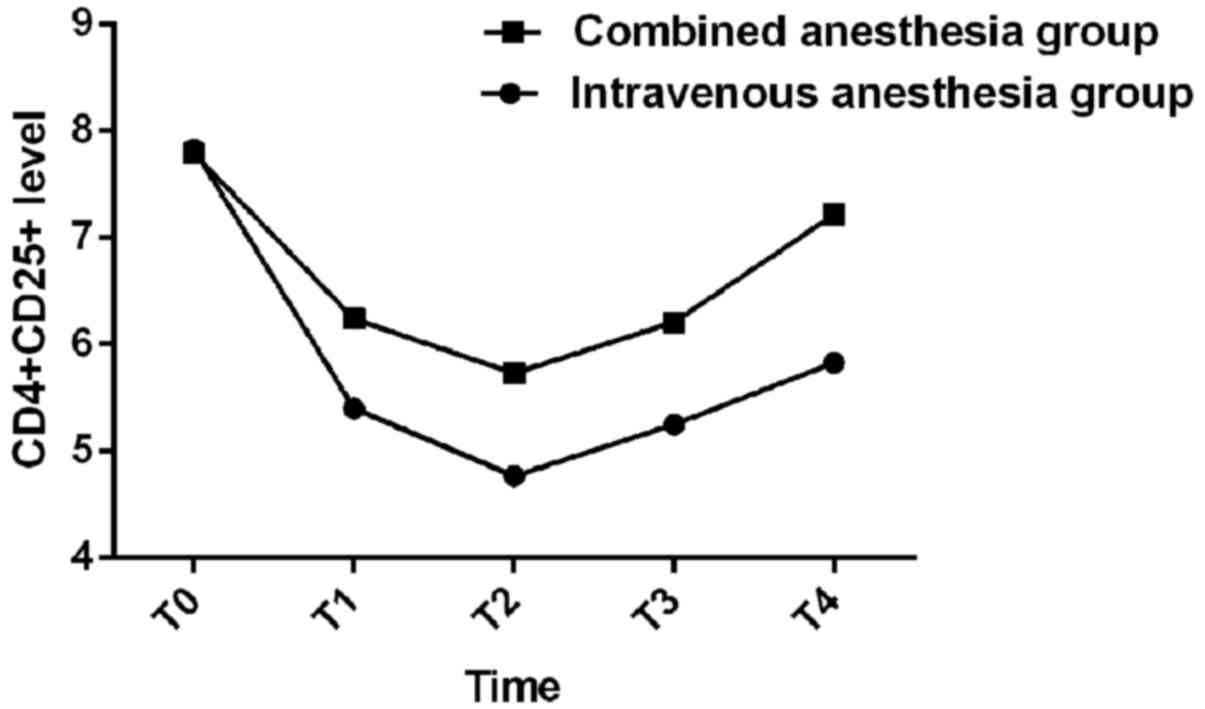
Analysis of
CD4+CD25+ levels in two groups at T0, T1, T2,
T3 and T4
There was no significant difference in
CD4+CD25+ level between the two groups at T0
(P>0.05). CD4+CD25+ levels at T1, T2, T3
and T4 were significantly higher in the combined anesthesia group
than those in the intravenous anesthesia group (P<0.05). After
the start of anesthesia, CD4+CD25+ levels of
both groups started to decrease, and
CD4+CD25+ levels at T2 and T1 were lower than
those at T0 (P<0.05), and CD4+CD25+ levels
at T2 were lower than those at T1 (P<0.05). After T3, the levels
of CD4+CD25+ in both groups began to increase
(P<0.05); the levels of CD4+CD25+ in both
groups at T3 and T4 were higher than those at T2 and T1
(P<0.05). The levels of CD4+CD25+ at T4
were higher in both groups than those at T3 (P<0.05), but the
level of CD4+CD25+ at T3 and T4 were lower
than those at T0 (P<0.05) (Table
IV). Changes of CD3+, CD4+ and
CD4+CD25+ are shown in Figs. 1–3.
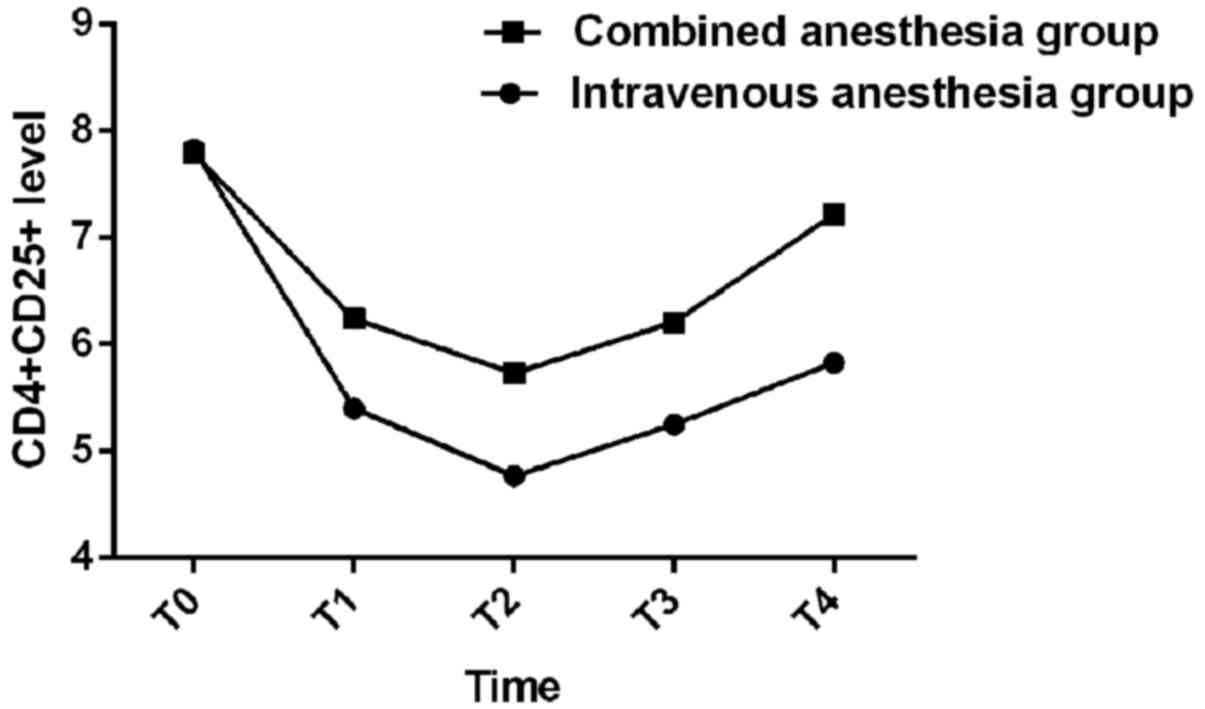 | Figure 3.Analysis of
CD4+CD25+ levels in two groups at T0, T1, T2,
T3 and T4. There was no significant difference in
CD4+CD25+ level in the two groups at T0
(P>0.05); CD4+CD25+ levels at T1, T2, T3
and T4 were significantly higher in the combined anesthesia group
than those in the intravenous anesthesia group (P<0.05). After
the start of anesthesia, CD4+CD25+ levels of
both groups started to decrease, and
CD4+CD25+ levels at T2 and T1 were lower than
those at T0 (P<0.05), and CD4+CD25+ levels
at T2 were lower than those at T1 (P<0.05). After T3, the levels
of CD4+CD25+ in both groups began to increase
(P<0.05); the levels of CD4+CD25+ in both
groups at T3 and T4 were higher than those at T2 and T1
(P<0.05). The levels of CD4+CD25+ at T4
were higher in both groups than those at T3 (P<0.05), but the
level of CD4+CD25+ at T3 and T4 were lower
than those at T0 (P<0.05). |
 | Table IV.CD4+CD25+ level
analysis at T0, T1, T2, T3 and T4 (%). |
Table IV.
CD4+CD25+ level
analysis at T0, T1, T2, T3 and T4 (%).
| Items | Intravenous
anesthesia | Combined
anesthesia | t-value | P-value |
|---|
| No. of
patients | 61 | 61 |
|
|
| T0a | 7.83±1.25 | 7.79±1.17 | 0.183 | 0.856 |
| T1b | 5.40±1.46 | 6.24±1.91 | 2.729 | 0.007 |
| T2c | 4.77±0.75 | 5.73±0.62 | 7.705 | <0.001 |
| T3d | 5.25±0.84 | 6.21±1.01 | 5.708 | <0.001 |
| T4e | 5.83±1.02 | 7.22±1.13 | 7.132 | <0.001 |
Discussion
Different methods of surgery and anesthesia often
cause different degrees of stress response in the patients. Due to
individual differences, patients also experience different ranges
of stress response (11). Stress
response within a certain range can enhance the body's immune
function, stimulate cell metabolism to speed up and improve the
body's resistance to external stimuli, but the stress response
exceeding the bodys limit will seriously hinder the treatment of
patients with prognosis, and it will inhibit immune function of the
body, causing cell and organ damage in patients (12,13).
Cellular immunity plays an important role in the anti-inflammatory
and antitumor responses of the body (14). This study explored the effects of
different anesthesia on the cellular immune function in patients
undergoing radical resection of lung cancer, in order to provide
reference for the choice of anesthesia in surgical treatment
opinion.
CD3+ is a mature T lymphocyte, which can
prompt the body's cellular immune function status; CD4+
is a helper T cells, which is the most important hub to regulate
the immune response; CD4+CD25+ is a subset of
T cells, which plays an important role in the body inflammation and
immune response (15,16). The results of this study showed that
the levels of CD3+, CD4+ and
CD4+CD25+ in the two groups were lower than
those before the operation, but the levels of CD3+,
CD4+ and CD4+CD25+ in the patients
receiving intravenous combined epidural anesthesia were
significantly higher than those in the simple intravenous
anesthesia. After surgery, two groups of patients with varying
degrees of CD3+, CD4+ and
CD4+CD25+ levels were restored. Patients
receiving intravenous composite epidural anesthesia were
significantly better than those who received intravenous anesthesia
alone, indicating that patients receiving intravenous composite
epidural anesthesia had more stable intraoperative immunologic
function and better postoperative immune function recovery. This
may be related to intravenous compound epidural anesthesia on the
inhibition of the stability of the autonomic nervous system;
epidural anesthesia can change autonomic nerve function (17), and stabilize the autonomic nervous
system, improve the level of peripheral neurotransmitters,
effectively improve the anesthesia of T Lymphocyte inhibition,
maintain patients with perioperative cellular immune function
stability and balance (18).
Ropivacaine is an anesthetic with small fat-soluble and relatively
diminished absolute efficacy. It blocks motor and sensory nerves
independently during maintenance anesthesia and relieves stress
stimulation of body anesthesia, surgery and postoperative pain
(19). Some studies (20) showed that intraoperative continuous
maintenance of ropivacaine in patients with T lymphocyte response
was significantly higher. Chen et al (21) in the study also showed that the
general anesthesia combined with epidural anesthesia can
effectively improve the patient's immune function. Kun et al
(22) also reported in the study that
systemic combined epidural anesthesia has a weaker NK cell
suppressive effect in gastric cancer surgery compared with pure
general anesthesia, which helps to maintain perioperative immune
function in patients. Their findings are similar to ours, but
because of the short duration of our study, we were unable to
assess the longer duration of immune function and adverse events.
Therefore, the findings and conclusions of this study need more
research and data for confirmation.
In conclusion, intravenous combined epidural
anesthesia can maintain a relatively stable immune function of
patients compared to simple intravenous anesthesia.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
SF wrote the manuscript and treated the patients.
PSQ detected CD3+, CD4+ levels. SNC treated
the patients and helped with detection of
CD4+CD25+ levels. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Zhejiang Cancer Hospital (Hangzhou, China). Patients who
participated in this research, signed the informed consent and had
complete clinical data.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rizvi NA, Hellmann MD, Snyder A, Kvistborg
P, Makarov V, Havel JJ, Lee W, Yuan J, Wong P, Ho TS, et al: Cancer
immunology. Mutational landscape determines sensitivity to PD-1
blockade in non-small cell lung cancer. Science. 348:124–128. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lortet-Tieulent J, Soerjomataram I, Ferlay
J, Rutherford M, Weiderpass E and Bray F: International trends in
lung cancer incidence by histological subtype: Adenocarcinoma
stabilizing in men but still increasing in women. Lung Cancer.
84:13–22. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Brahmer J, Reckamp KL, Baas P, Crinò L,
Eberhardt WE, Poddubskaya E, Antonia S, Pluzanski A, Vokes EE,
Holgado E, et al: Nivolumab versus docetaxel in advanced
squamous-cell non-small-cell lung cancer. N Engl J Med.
373:123–135. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Herbst RS, Baas P, Kim DW, Felip E,
Pérez-Gracia JL, Han JY, Molina J, Kim JH, Arvis CD, Ahn MJ, et al:
Pembrolizumab versus docetaxel for previously treated,
PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010):
A randomised controlled trial. Lancet. 387:1540–1550. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Horn L, Spigel DR, Vokes EE, Holgado E,
Ready N, Steins M, Poddubskaya E, Borghaei H, Felip E, Paz-Ares L,
et al: Nivolumab versus docetaxel in previously treated patients
with advanced non-small-cell lung cancer: Two-year outcomes from
two randomized, open-label, phase III trials (CheckMate 017 and
CheckMate 057). J Clin Oncol. 35:3924–3933. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen C, Li M, Wang K, Shen J, Yang L, Bu X
and Gao G: Protective effect of combined general and regional
anesthesia on postoperative cognitive function in older
arthroplasty patients. Int J Clin Exp Med. 10:15453–15458.
2017.
|
|
7
|
Zhang CH, Ma WQ, Yang YL, Dong FT, Wang HM
and Wei HM: Effect of the intraoperative wake-up test in
sevoflurane-sufentanil combined anesthesia during adolescent
idiopathic scoliosis surgery: A randomized study. J Clin Anesth.
25:263–267. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Segal D, Awad N, Nasir H, Mustafa S and
Lowenstein L: Combined spinal and general anesthesia vs. general
anesthesia for robotic sacrocervicopexy: A randomized controlled
trial. Int Urogynecol J. 25:369–374. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tsukamoto A, Serizawa K, Sato R, Yamazaki
J and Inomata T: Vital signs monitoring during injectable and
inhalant anesthesia in mice. Exp Anim. 64:57–64. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Browning RM, Fellingham WH, O'Loughlin EJ,
Brown NA and Paech MJ: Prophylactic ondansetron does not prevent
shivering or decrease shivering severity during cesarean delivery
under combined spinal epidural anesthesia: A randomized trial. Reg
Anesth Pain Med. 38:39–43. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhao J and Mo H: The impact of different
anesthesia methods on stress reaction and immune function of the
patients with gastric cancer during peri-operative period. J Med
Assoc Thai. 98:568–573. 2015.PubMed/NCBI
|
|
12
|
Hu LG, Pan JH, Li J, Kang F and Jiang L:
Effects of different doses of sufentanil and remifentanil combined
with propofol in target-controlled infusion on stress reaction in
elderly patients. Exp Ther Med. 5:807–812. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang L, Yuan R, Yao C, Wu Q, Christelle M,
Xie W, Zhang X, Sun W, Wang H and Yao S: Effects of resolvin D1 on
inflammatory responses and oxidative stress of
lipopolysaccharide-induced acute lung injury in mice. Chin Med J
(Engl). 127:803–809. 2014.PubMed/NCBI
|
|
14
|
Kirchheiner K, Czajka-Pepl A,
Ponocny-Seliger E, Scharbert G, Wetzel L, Nout RA, Sturdza A,
Dimopoulos JC, Dörr W and Pötter R: Posttraumatic stress disorder
after high-dose-rate brachytherapy for cervical cancer with 2
fractions in 1 application under spinal/epidural anesthesia:
Incidence and risk factors. Int J Radiat Oncol Biol Phys.
89:260–267. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ma C, Kesarwala AH, Eggert T,
Medina-Echeverz J, Kleiner DE, Jin P, Stroncek DF, Terabe M, Kapoor
V, ElGindi M, et al: NAFLD causes selective CD4(+) T lymphocyte
loss and promotes hepatocarcinogenesis. Nature. 531:253–257. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pentcheva-Hoang T, Simpson TR,
Montalvo-Ortiz W and Allison JP: Cytotoxic T lymphocyte antigen-4
blockade enhances antitumor immunity by stimulating
melanoma-specific T-cell motility. Cancer Immunol Res. 2:970–980.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Liu J, Cui F, Li S, Chen H, Shao W, Liang
L, Yin W, Lin Y and He J: Nonintubated video-assisted thoracoscopic
surgery under epidural anesthesia compared with conventional
anesthetic option: A randomized control study. Surg Innov.
22:123–130. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhang Y, Guan Z, Reader B, Shawler T,
Mandrekar-Colucci S, Huang K, Weil Z, Bratasz A, Wells J, Powell
ND, et al: Autonomic dysreflexia causes chronic immune suppression
after spinal cord injury. J Neurosci. 33:12970–12981. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Marhofer D, Kettner SC, Marhofer P, Pils
S, Weber M and Zeitlinger M: Dexmedetomidine as an adjuvant to
ropivacaine prolongs peripheral nerve block: A volunteer study. Br
J Anaesth. 110:438–442. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chloropoulou P, Iatrou C, Vogiatzaki T,
Kotsianidis I, Trypsianis G, Tsigalou C, Paschalidou E, Kazakos K,
Touloupidis S and Simopoulos K: Epidural anesthesia followed by
epidural analgesia produces less inflammatory response than spinal
anesthesia followed by intravenous morphine analgesia in patients
with total knee arthroplasty. Med Sci Monit. 19:73–80. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen WK, Ren L, Wei Y, Zhu DX, Miao CH and
Xu JM: General anesthesia combined with epidural anesthesia
ameliorates the effect of fast-track surgery by mitigating
immunosuppression and facilitating intestinal functional recovery
in colon cancer patients. Int J Colorectal Dis. 30:475–481. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kun L, Tang L, Wang J, Yang H and Ren J:
Effect of combined general/epidural anesthesia on postoperative NK
cell activity and cytokine response in gastric cancer patients
undergoing radical resection. Hepatogastroenterology. 61:1142–1147.
2014.PubMed/NCBI
|