Introduction
Gastric cancer is the most common gastrointestinal
tumor in the world. Variations in the dietary structure have led to
a gradual increase in the incidence of gastric cancer worldwide.
Both the incidence and mortality rates of gastric cancer rank
behind lung cancer, and are ranked second in malignant tumors
(1). Since most patients have a
relatively poor awareness of health care, detection and diagnosis
of gastric cancer occur once the disease has already progressed
into the middle or advanced stage (2).
The causes and pathogenesis of gastric cancer are
very complex, and the occurrence is induced by multiple factors and
procedures as well as progressive development. For example,
helicobacter pylori infection, environment, diet and genetic
factors are of great significance for the occurrence of gastric
cancer (3). Affected by various
factors, carcinogens lead to damage to DNA in human cells and
genetic damage will continuously accumulate without any timely
repair, eventually inducing abnormal proliferation and apoptosis of
cells, thus leading to gastric cancer (4). Nucleotide excision repair (NER) system
is the main and most important damage-repair pathway of DNA in the
human body. As a kind of NER gene, xeroderma pigmentosum
complementation group F (XPF) can exert a rate-limiting effect in
the repair pathway, which leads to carcinogenesis and resistance to
chemotherapy (5,6). In particular, a high expression of XPF
increases the risk of skin cancer (7).
In this study, we investigated the XPF expression of
gastric cancer patients, and analyzed the correlation of XPF
expression with occurrence and prognosis of gastric cancer.
Patients and methods
General material
We randomly selected a total of 76 patients who were
admitted to the Second People's Hospital of Dezhou City (Dezhou,
China) for treatment. Inclusion criteria for the study were: i)
patients whose diagnosis of progressive gastric cancer was
confirmed by pathological biopsy using electronic gastroscope,
contrast-enhanced computed tomography (CT) or magnetic resonance
imaging (MRI); ii) patients who received surgical treatment and
whose excised lesions were taken as specimens; iii) patients who
signed the informed consent. Exclusion criteria were: i) patients
whose maximal diameter of tumor was >10 cm; ii) patients with
other malignant tumors. Normal gastric mucosa tissues adjacent to
the lesion of gastric cancer were taken as the control group. The
basic characteristics of the patients are shown in Table I.
 | Table I.General characteristics of the
patients. |
Table I.
General characteristics of the
patients.
| Item | Case | Ratio (%) |
|---|
| Sex |
| Male | 42 | 55.26 |
|
Female | 34 | 44.74 |
| Age (years) |
|
<60 | 36 | 47.36 |
| ≥60 | 40 | 52.64 |
| Degree of
differentiation |
| Highly
differentiated adenocarcinoma | 36 | 47.36 |
|
Moderately differentiated
adenocarcinoma | 27 | 35.52 |
| Poorly
differentiated adenocarcinoma | 13 | 17.11 |
| Tumor size |
| <3
cm | 27 | 35.53 |
| 3–5
cm | 30 | 39.47 |
| >5
cm | 19 | 25.00 |
The study was approved by the Ethics Committee of
the Second People's Hospital of Dezhou City. Patients signed the
informed consent.
Methods
Collection of specimens
Lesion tissues that were excised in the surgical
treatment of patients and part of the normal gastric mucosa tissue
adjacent to the tumor of gastric cancer were taken as specimens.
Once obtained, fresh specimens were regularly dehydrated in an
ascending series of alcohol rinses, treated using dimethylbenzene
for transparency, and embedded in paraffin.
Experimental equipments and
material
Slicing machine (Leica, Mannheim, Germany),
micropipette (Eppendorf, Hamburg, Germany), microscope (BX40,
Olympus Corporation; Tokyo, Japan) electrothermostat, centrifuge
tubes in different specifications and autoclave were used.
Experimental reagents included: i) primary rabbit anti-human
polyclonal antibody; ii) secondary goat anti-rabbit polyclonal
antibody; iii) DAB (3,3′-diaminobenzidine) color development kit
(Fuzhou Maixin Biotechnology Co., Ltd.); iv) other assistant
reagents: dimethylbenzene, buffer, anhydrous ethanol, neutral
balsam and hydrogen peroxide solution.
Immunohistochemistry
Experimental procedures were: i) Histological
section: Serial sectioning was performed using the slicing machine
to cut the paraffin-embedded tissues into 6–8 sections with a
thickness of 4–5 µm; ii) Dewaxing: After sections were heated in an
electrothermostat for 45 min at 70°C, 5 ml of dimethylbenzene was
added onto the sections twice (5 min each time) followed by swing
in slow motion; then the sections were rinsed by cool anhydrous
ethanol twice (5 min each time); when there was no up-floated
floccules in the solution, ethanol in different concentrations (95,
85 and 75%) was sequentially added into the solution followed by 5
min of standing, respectively; and slices were then rinsed using
distilled water; iii) Phosphate-buffered saline (PBS) rinsing and
incubation: Sections were taken out and placed in an incubator, in
which 5 ml of PBS was added for rinsing 3 times. After the PBS was
fully removed, 50 µl hydrogen dioxide solution (3%) was added onto
each section followed by incubation for 10 min at 20°C in an
electrothermostat to block the activity of endogenous peroxidase.
The sections were then washed using 5 ml PBS (3 min each time),
after which the PBS was removed, 50 µl primary rabbit anti-human
polyclonal antibody (1:300; cat. no. 13465; Cell Signaling
Technology, Inc.; Danvers, MA, USA) was added onto each section
that was later incubated overnight at 4°C in a refrigerator, and
the next day, sections were rinsed using PBS 3 times. Secondary
goat anti-rabbit polyclonal antibody (1:1,000; cat. no. 7074; Cell
Signaling Technology, Inc.) was also added onto each section for 15
min of incubation at 20°C in an incubator, and the sections were
washed using PBS three times. For color development: DAB kit, and
reagents A, B and C (each 50 µl) were used to prepare the DAB color
development solution. After the extra water on each section was
cleaned, 50 µl of color development solution was added to each
section, and the section was observed under a microscope (Olympus
Corporation). After color development, the section was rinsed by
purified water to terminate the color development. Finally,
re-dyeing (30 sec each time) was carried out twice using
hematoxylin, and the sections were sealed using neutral balsam.
XPF expression was detected by immunohistochemistry.
Under high magnification (×400), we randomly selected 8
non-overlapping visions of high magnification of each section, and
100 cells were selected in each vision. According to the proportion
of positive cells in each section, we performed evaluation via
semi-quantitative scoring method using the following criteria: i) 0
point for section with the ratio of positive cells <5%; ii) 1
point for section with the ratio of positive cells between 5 and
25%; iii) 2 points for section with the ratio of positive cells
between 26 and 50%; iv) 3 points for section with the ratio of
positive cells between 51 and 75%; v) 4 points for section with the
ratio of positive cells >75%. Staining degree of cells was: i) 0
point for cells without any color; ii) 1 point for cells in fine
granule shape and canary yellow; iii) 2 points for cells in coarse
granule shape and brown yellow; iv) 3 points for cells in small
mass shape and dark brown. The total points of the above two
indexes were taken as the total score. In terms of expression
evaluation, expressions with a total score ≤3 points were
considered low expression, total score between 4 and 5 points
moderate expression, and total score ≥6 was considered high
expression. In the evaluation of the results, a total score ≤3
points was considered a negative result, and a total score >3
points was a positive result.
Statistical analysis
Data analysis was performed using SPSS 19.0 software
(Chicago, IL, USA). Correlation between the XPF expression and
clinicopathological indexes of gastric cancer was verified via
single-factor Chi-square test. The Cox proportional hazards
regression model was used in the analysis of influencing factors of
patient prognosis. The Kaplan-Meier was used to analyze the
survival rates of XPF-positive and -negative patients. Inspection
results were analyzed using the log-rank, Breslow and Tarone-Ware
tests. P<0.05 indicated that the difference had statistical
significance.
Results
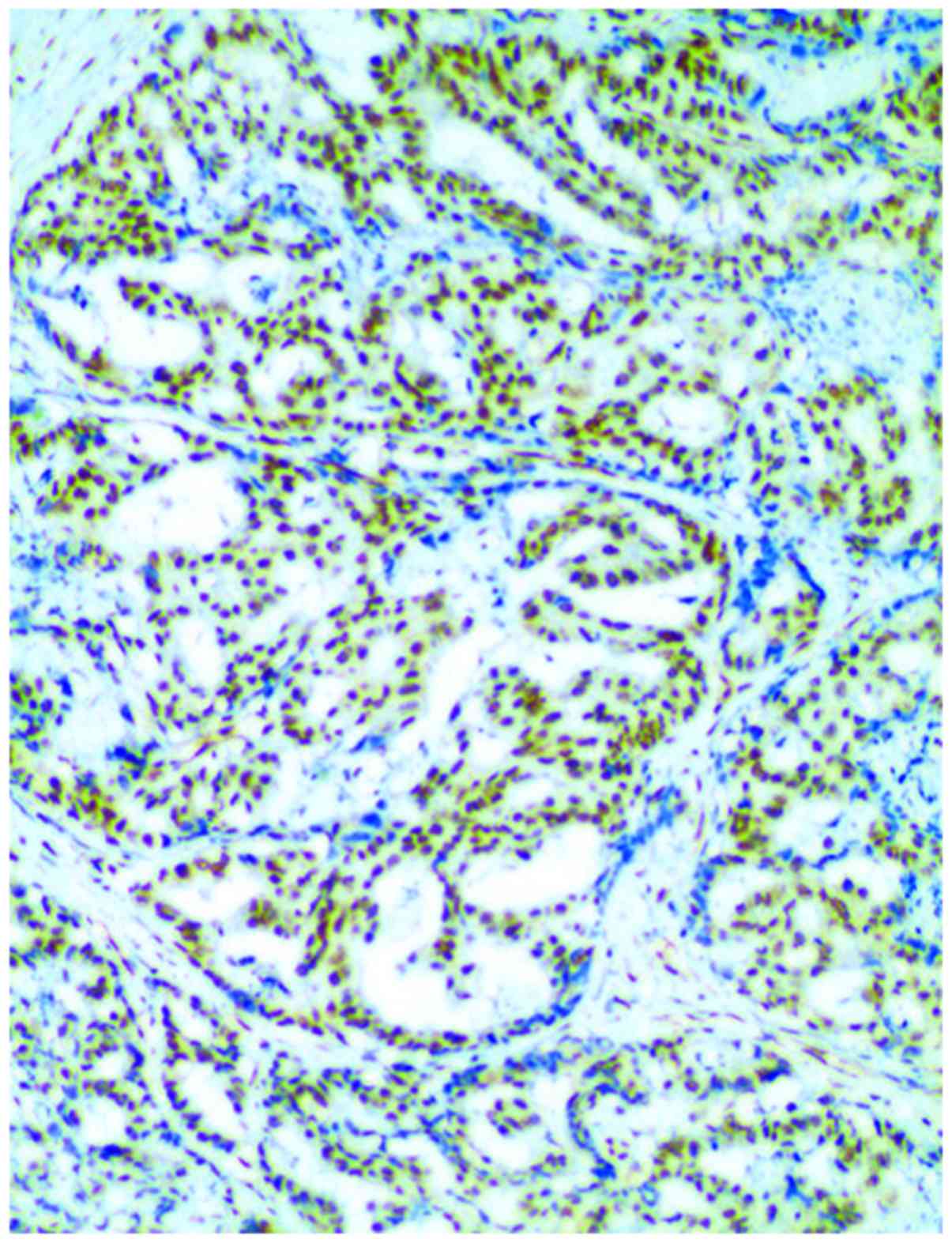
In comparison of XPF expression, we found that the
positive expression rate (71.05%) in the observation group was
obviously higher than that (36.84%) in the control group, and the
difference in the intergroup comparison had statistical
significance (P<0.05) (Table II
and Fig. 1).
 | Table II.Comparison of XPF expression between
the two groups. |
Table II.
Comparison of XPF expression between
the two groups.
|
|
| XPF expression |
|
|---|
|
|
|
|
|
|---|
| Group | N (case) | Negative cases | Positive cases | Ratio of positive
cases (%) |
|---|
| Observation
group | 76 | 22 | 54 | 71.05 |
| Control group | 76 | 48 | 28 | 36.84 |
| χ2 |
|
| 16.551 |
|
| P-value |
|
| <0.0001 |
|
XPF expression was significantly correlated with the
family history and Laurén classification and the difference had
statistical significance (P<0.05); XPF expression was not
correlated with patient's age, sex, tumor site, quantity of mass,
diameter of tumor, smoking, quantity of metastatic lymph nodes,
infiltration depth and tumor node metastasis (TNM) staging, and the
differences were not statistically significant (P>0.05)
(Table III).
 | Table III.Correlation between XPF expression and
each clinicopathological index. |
Table III.
Correlation between XPF expression and
each clinicopathological index.
|
|
| XPF expression |
|
|
|
|---|
|
|
|
|
|
|
|
|---|
| Clinicopathological
indexes | Cases | Negative case | Positive case | Positive rate
(%) | χ2 | P-value |
|---|
| Sex |
| Male | 42 | 12 | 30 | 71.42 | 0.002 | 0.956 |
|
Female | 34 | 9 | 25 | 73.35 |
|
|
| Age (year) |
|
<60 | 36 | 11 | 25 | 69.44 | 0.001 | 0.968 |
| ≥60 | 40 | 11 | 29 | 72.50 |
|
|
| History of liver
cancer in immediate family members |
| Yes | 32 | 7 | 25 | 78.12 | 9.949 | 0.014 |
| No | 44 | 23 | 21 | 52.27 |
|
|
| Tumor site |
| Gastric
body | 25 | 7 | 18 | 72.00 | 0.094 | 0.954 |
| Gastric
antrum | 36 | 11 | 25 | 69.44 |
|
|
| Gastric
cardia + gastric fundus | 15 | 4 | 11 | 73.33 |
| Quantity of mass |
| 1 | 35 | 10 | 25 | 71.42 | 0.007 | 0.929 |
| ≥2 | 41 | 11 | 30 | 73.17 |
|
|
| Diameter of tumor
(cm) |
|
<5 | 51 | 15 | 36 | 70.58 | 0.049 | 0.823 |
| ≥5 | 25 | 6 | 19 | 76.00 |
|
|
| Laurén
classification |
|
Diffuse-type | 31 | 18 | 13 | 41.93 | 12.420 | 0.002 |
|
Mixed-type | 17 | 2 | 15 | 88.23 |
|
|
|
Intestinal-type | 28 | 7 | 21 | 75.00 |
|
|
| Smoking |
|
Yes | 31 | 7 | 24 | 77.42 | 0. 309 | 0.578 |
| No | 45 | 14 | 31 | 68.89 |
|
|
| Lymphatic
metastasis (lymph nodes) |
| ≤5 | 46 | 13 | 33 | 71.74 | 0.012 | 0.912 |
|
>5 | 30 | 8 | 22 | 73.33 |
|
|
| Infiltration
depth |
| Mucosa
and submucosa | 17 | 5 | 12 | 70.58 | 0.404 | 0.817 |
|
Muscular layer | 35 | 9 | 26 | 74.28 |
|
|
| Serosal
or subserosal | 24 | 8 | 16 | 66.67 |
|
|
| TNM staging |
| I | 21 | 6 | 15 | 71.43 | 0.167 | 0.982 |
| II | 24 | 6 | 18 | 75.00 |
|
|
|
III | 18 | 5 | 13 | 72.22 |
|
|
| IV | 13 | 3 | 10 | 76.92 |
|
|
Factors affecting patient prognosis were analyzed
using the Cox hazards model. The results suggested that XPF
expression and TNM staging were independent factors affecting the
prognosis of gastric cancer (P<0.05) (Table IV).
 | Table IV.Analysis of factors affecting the
prognosis of gastric cancer via the Cox hazards model. |
Table IV.
Analysis of factors affecting the
prognosis of gastric cancer via the Cox hazards model.
| Related
factors | B | SE | Wald | OR (95% CI) | P-value |
|---|
| Sex | 0.042 | 0.013 | 0.543 | 0.567
(0.726–0.936) | 0.436 |
| Age (years) | 0.028 | 0.009 | 0.332 | 0.964
(0.824–1.137) | 0.202 |
| Smoking | −0.038 | 0.037 | 0.237 | 1.035
(0.228–1.425) | 0.113 |
| Tumor site | −0.043 | 0.084 | 1.143 | 0.937
(0.425–1.948) | 0.223 |
| Tumor size | 0.036 | 0.032 | 0.217 | 1.046
(1.035–1.876) | 0.535 |
| Laurén
classification | 0.015 | 0.042 | 1.085 | 0.875
(0.532–1.452) | 0.247 |
| TNM staging | 0.485 | 0.052 | 5.012 | 2.025
(1.023–3.627) | 0.003 |
| XPF
expressions | 0.463 | 0.026 | 6.015 | 3.564
(1.143–5.835) | 0.017 |
| Infiltration
depth | 0.516 | 0.037 | 0.437 | 0.875
(0.532–0.952) | 0.124 |
| Lymphatic
metastasis | −0.028 | 0.141 | 0.767 | 1.025
(0.623–1.627) | 0.215 |
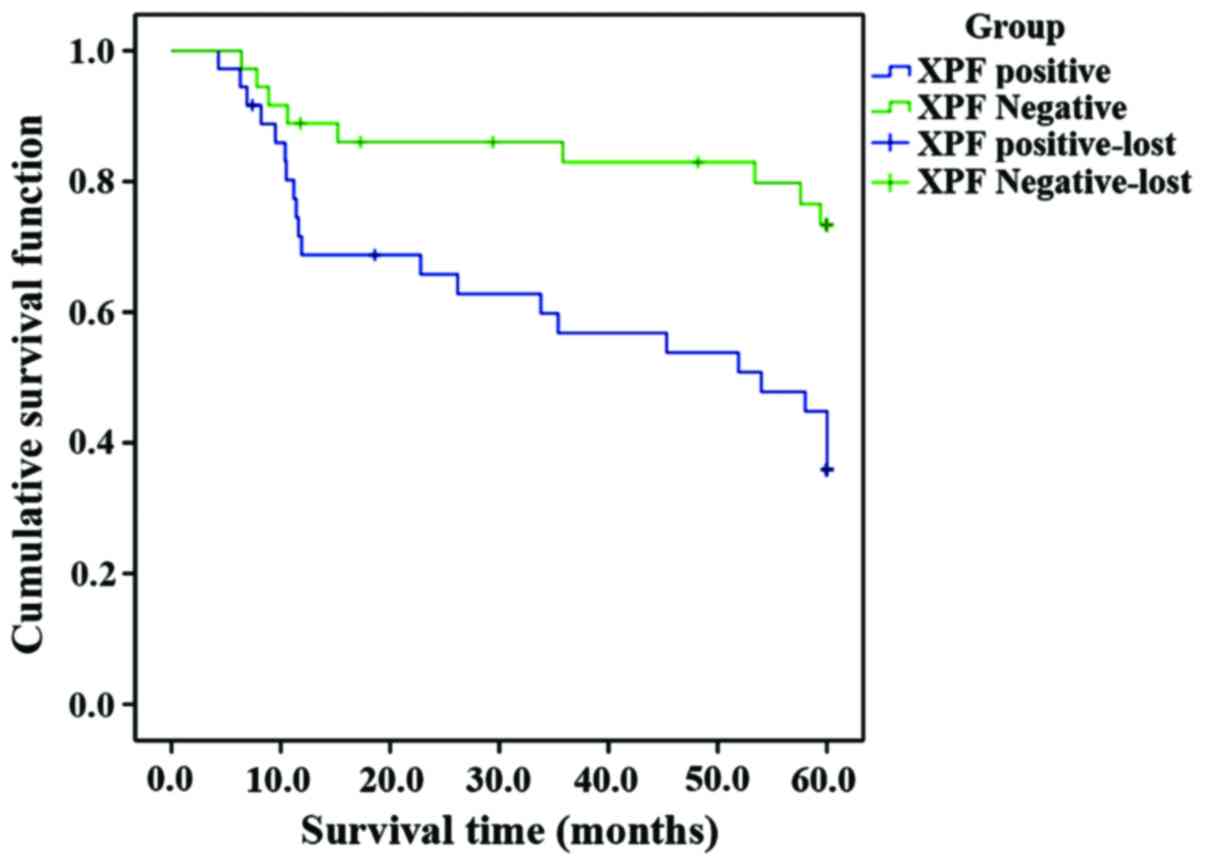
Kaplan-Meier survival analysis showed that the
survival time of XPF-positive patients was shorter than that of
XPF-negative patients. Inspection results using 3 different
statistics were basically the same, and the differences were
statistically significant (P<0.05) (Fig. 2 and Table
V).
 | Table V.Comparison of inspection results
using 3 different statistics for survival analysis. |
Table V.
Comparison of inspection results
using 3 different statistics for survival analysis.
| Type | χ2
value | df | P-value |
|---|
| Log Rank
(Mantel-Cox) | 9.205 | 1 | 0.002 |
| Breslow
(Generalized Wilcoxon) | 8.196 | 1 | 0.004 |
| Tarone-Ware | 8.772 | 1 | 0.003 |
Discussion
In human cells, DNA in normal metabolism can be
damaged due to the influences of various external factors, and such
damage can often be accumulated, finally inducing a variety of
cancers (8). In the human body, there
are several different pathways for genetic repair, among which NER
plays a major role. XPF gene, i.e., xeroderma pigmentosum
complementation group, can encode XPF protein, a rate-limiting
molecule in NER pathway; XPF protein, with the key effect in NER
repair, can identify damaged 5′ end in DNA repair (9,10). A
variety of studies (11) have shown
that XPF gene is correlated with the occurrence of various cancers,
such as colon cancer, lung cancer, breast cancer and bladder
cancer.
Significance of XPF expression in gastric cancer.
Genetic damage will cause cell apoptosis, and sometimes, a minor
damage can even induce cell apoptosis (12). However, the encoded product of XPF
gene, a key enzyme in NER pathway, plays a critical role in
anticancer activity, and, with the enhanced functions, can not only
induce the antagonistic effect of gastric tumor cells on the
platinum-based chemotherapy drugs, resulting in drug resistance and
failure in chemotherapy, but also give rise to the abnormality in
the repair of damaged DNA, leading to a significantly increased
risk of carcinoma (13,14). The activity of XPF gene is relatively
high when the capability of cell repair is in a relatively high
level; due to the stimulation generated by damage, NER will be
activated to induce the XPF expression and increase the activity
(15). According to the relevant
study (16), XPF expression in tumor
tissues is obviously higher than that in the tissues adjacent to
the tumors. In this study, we analyzed XPF expression in the
gastric cancer tissues of 76 gastric cancer patients, and found
that XPF expressions in the gastric cancer tissues were
significantly higher than those in the tissues adjacent to the
tumors (P<0.05).
Correlation between XPF expression and
clinicopathological indexes of gastric cancer. The results of this
study showed that XPF expression was correlated with Laurén
classification and family history; higher positive expression of
XPF gene were found in the patients with immediate family history
of liver cancer, and in mixed- or intestinal-type of Laurén
classification, and the difference had statistical significance
(P<0.05); XPF expression was not correlated with patient's sex,
age, smoking habit, tumor site, diameter and quantity of tumor,
infiltration depth, quantity of lymphatic metastasis and
TNM-staging (P>0.05). Due to the genetic susceptibility of
gastric cancer, many gastric cancer patients have a family history
of gastric cancer; a relevant study (17) showed that incidence rate of gastric
cancer of members with the family history of gastric cancer is
1.5–3 times higher than that of members without family history of
gastric cancer. In history, the family of Napoleon was a typical
example illustrating the genetic susceptibility in the family with
the history of gastric cancer. Among those patients with the family
history of gastric cancer, gene defect or mutation may be the major
cause for canceration, and the risk of gastric cancer will be
increased due to the inheritance of susceptibility gene (18). In Laurén classifications, non-tumor
mucosal atrophy has been scarcely found in peripheral tissues of
diffuse-type gastric cancer, but intestinal metaplasia and
extensive atrophy are often associated with the intestinal- and
mixed-type gastric cancer. Thus, damage to gene in varying degrees
may induce the translation of XPF proteins in different activity,
which will lead to the differences in rates of positive expression
(19).
Association between XPF expression and prognosis of
gastric cancer. Currently, exact pathogenesis of gastric cancer has
not been fully clarified; but many studies have shown that repair
gene is not only correlated with the occurrence and development of
gastric cancer, but also closely associated with the prognosis
(20). In this study, we performed
survival analysis for XPF-positive and -negative patients with
gastric cancer, and the results showed that the survival time of
XPF-negative patients was longer than that of XPF-positive patients
(P<0.05); we selected clinicopathological indexes according to
the prognostic factors of gastric cancer patients, performed
regression analysis using Cox's hazards model, and results
suggested that XPF was an independent prognostic factor. This
suggested that positive expression of XPF gene, in addition to its
critical effect on the formation of gastric cancer, exerts a larger
effect on the distant metastasis or recurrence of tumor in the
progressive stage. Thus, XPF can serve as an important index
affecting the prognosis of gastric cancer patients (21).
In conclusion, increased XPF expression plays an
important role in the occurrence, development and prognosis of
gastric cancer, and can serve as an index for evaluating the
prognosis of gastric cancer. This study was limited by sample size,
and in-depth investigation into the XPF expression in tissues of
human are expected.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors contributions
PL analyzed the general information of the patients.
PL and YM performed immunohistochemistry. Both authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Patients signed the informed consent. The study was
approved by the Ethics Committee of the Second People's Hospital of
Dezhou City (Dezhou, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ryu MH and Kang YK: ML17032 trial:
Capecitabine/cisplatin versus 5-fluorouracil/cisplatin as
first-line therapy in advanced gastric cancer. Expert Rev
Anticancer Ther. 9:1745–1751. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schinzari G, Cassano A, Orlandi A, Basso M
and Barone C: Targeted therapy in advanced gastric carcinoma: The
future is beginning. Curr Med Chem. 21:1026–1038. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Watari J, Chen N, Amenta PS, Fukui H,
Oshima T, Tomita T, Miwa H, Lim KJ and Das KM: Helicobacter pylori
associated chronic gastritis, clinical syndromes, precancerous
lesions, and pathogenesis of gastric cancer development. World J
Gastroenterol. 20:5461–5473. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Olivero M, Dettori D, Arena S, Zecchin D,
Lantelme E and Di Renzo MF: The stress phenotype makes cancer cells
addicted to CDT2, a substrate receptor of the CRL4 ubiquitin
ligase. Oncotarget. 5:5992–6002. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Marteijn JA, Lans H, Vermeulen W and
Hoeijmakers JH: Understanding nucleotide excision repair and its
roles in cancer and ageing. Nat Rev Mol Cell Biol. 15:465–481.
2014. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vaezi A, Wang X, Buch S, Gooding W, Wang
L, Seethala RR, Weaver DT, D'Andrea AD, Argiris A, Romkes M, et al:
XPF expression correlates with clinical outcome in squamous cell
carcinoma of the head and neck. Clin Cancer Res. 17:5513–5522.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gregg SQ, Robinson AR and Niedernhofer LJ:
Physiological consequences of defects in ERCC1-XPF DNA repair
endonuclease. DNA Repair (Amst). 10:781–791. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu L, Chang Y, Ye J and Kumar S: Abstract
1923: Distinct evolutionary and mutational patterns in oncogenes
and tumor suppressor genes. Cancer Res. 75:abs. 1923. 2015.doi:
10.1158/1538-7445.AM2015-1923.
|
|
9
|
Liu J, He C, Xing C and Yuan Y: Nucleotide
excision repair related gene polymorphisms and genetic
susceptibility, chemotherapeutic sensitivity and prognosis of
gastric cancer. Mutat Res. 765:11–21. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ying M, Deng XD, Yu F, Zhang W, Wang SX,
Liu Y and Liu H: Association of XPF, levels and genetic
polymorphism with susceptibility to ischemic stroke. J Mol
Neurosci. 59:1–9. 2016.PubMed/NCBI
|
|
11
|
Cheng HB, Xie C, Zhang RY, Hu SS, Wang Z
and Yue W: Xeroderma pigmentosum complementation group F
polymorphisms influence risk of glioma. Asian Pac J Cancer Prev.
14:4083–4087. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Singh VV, Dutta D, Ansari MA, Dutta S,
Chandran B and Longnecker R: Kaposi's sarcoma-associated
herpesvirus induces the ATM and H2AX DNA damage response early
during de novo infection of primary endothelial cells, which play
roles in latency establishment. J Virol. 88:2821–2834. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wei ZH, Guo WH, Wu J, Suo WH and Fu GH: A
nonsense mutation in the Xeroderma pigmentosum complementation
group F (XPF) gene is associated with gastric carcinogenesis. Gene.
537:238–244. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Graf N, Ang WH, Zhu G, Myint M and Lippard
SJ: Role of endonucleases XPF and XPG in nucleotide excision repair
of platinated DNA and cisplatin/oxaliplatin cytotoxicity.
Chembiochem. 12:1115–1123. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Matsumoto S, Fischer ES, Yasuda T, Dohmae
N, Iwai S, Mori T, Nishi R, Yoshino K, Sakai W, Hanaoka F, et al:
Functional regulation of the DNA damage-recognition factor DDB2 by
ubiquitination and interaction with xeroderma pigmentosum group C
protein. Nucleic Acids Res. 43:1700–1713. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Facista A, Nguyen H, Lewis C, Prasad AR,
Ramsey L, Zaitlin B, Nfonsam V, Krouse RS, Bernstein H, Payne CM,
et al: Deficient expression of DNA repair enzymes in early
progression to sporadic colon cancer. Genome Integr. 3:32012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jiang X, Tseng CC, Bernstein L and Wu AH:
Family history of cancer and gastroesophageal disorders and risk of
esophageal and gastric adenocarcinomas: A case-control study. BMC
Cancer. 14:602014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Reddy KM, Chang JI, Shi JM and Wu BU: Risk
of gastric cancer among patients with intestinal metaplasia of the
stomach in a United States Integrated Healthcare System. Clin
Gastroenterol Hepatol. 14:1420–1425. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Caruso RA, Branca G, Fedele F, Parisi A,
Finocchiaro G, Ieni A and Rigoli L: Eosinophil-specific granules in
tumor cell cytoplasm: Unusual ultrastructural findings in a case of
diffuse-type gastric carcinoma. Ultrastruct Pathol. 39:226–230.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Khaleghian M, Shakoori A, Razavi AE and
Azimi C: Relationship of amplification and expression of the C-MYC
gene with survival among gastric cancer patients. Asian Pac J
Cancer Prev. 16:7061–7069. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li J, Zuo X, Lv X, Kong F, Xu W and Yang
S: Association of DNA repair gene polymorphisms with response to
chemotherapy and prognosis of gastric cancer in a Chinese
population. Tumour Biol. 35:7569–7574. 2014. View Article : Google Scholar : PubMed/NCBI
|