Introduction
Thyroid carcinoma (TC) is the most common malignant
tumor in endocrine organs, and its incidence has increased in
recent decades (1). A major
histologic subtype of TC is papillary carcinoma (PC), which has a
good prognosis after surgical treatment. However, we rarely
encounter PC patients with an aggressive clinical course such as
bone or lung metastasis at the first clinic visit. Poorly
differentiated thyroid carcinoma (PDC) represents an aggressive
variant of TC with an incidence of 0.8 to 15%, depending on the
defining criteria and geographic location (2). Anaplastic carcinoma (AC) accounts for
<1% and has a median survival of 3 to 5 months (3). The initiation and progression of TC are
associated with the accumulated genetic and epigenetic changes. The
observed genetic changes frequently lead to activation of the MAPK
or PI3K/Akt signaling pathways. Approximately 70% of TC cases
demonstrated one of four genetic abnormalities: Point mutations in
the BRAF or RAS genes or one of two chromosomal
rearrangements (RET/PTC or PAX8/PPARγ) (4). PDC and AC are thought to arise from
pre-existing PC or follicular carcinoma (FC) through additional
genetic alterations, including CTNNB1 and TP53
mutations (5).
BRAF, a serine-threonine kinase and downstream
signaling molecule of Ras and RET, is a potent activator of the
MAPK signaling pathway (1,6). BRAF mutations have previously
been reported in a broad range of human cancers, with the highest
prevalence observed in melanoma and TC (6). A T1799A transversion mutation, which
occurs in the kinase domain of BRAF, located on chromosome
7, results in a single amino acid substitution of valine to
glutamic acid (V600E). The BRAF V600E mutation potently
increases the kinase activity of BRAF by evoking a 480-fold
increase in phosphorylation of ERK1/2 compared with wild-type BRAF,
resulting in the expression of a number of genes that are involved
in cell proliferation, differentiation, survival, tumorigenesis and
promotion of epithelial-mesenchymal transition (7).
PIK3CA, the α-type isoform of the catalytic subunit
of phosphatidylinositol-3-kinase (PI3K), has been shown to harbor
oncogenic mutations in human cancers (8). However, little is known about the role
of PIK3CA gene mutations in patients with TC (9,10). EGFR is
a tyrosine kinase of the ErbB family that regulates signaling
pathways for cellular proliferation and survival. Although many
types of somatic mutations in the EGFR gene have been
reported in non-small cell lung carcinoma (NSCLC), few reports have
described such mutations in patients with TC (11).
Next-generation sequencing (NGS) technology enables
the simultaneous analysis of hundreds of genes of interest using
targeted sequence panels. NGS has been used in molecular tumor
classification, and the prediction of recurrence and metastasis in
some human cancers (12). NGS data
are also useful in patient's management, facilitating risk
stratification of patients based on the risk of malignancy. In the
present report, we describe a patient with rare mutations and the
results of mutational analysis using NGS. We attempted to correlate
these mutations with clinicopathologic features of patients with
TC.
Patients and methods
Patients
The study group consisted of 50 Japanese patients
(45 females and 5 males) with a median age of 65 years (range, 26
to 86 years) who underwent curative surgery between 2012 and 2016
at Hokuto Hospital. Patients were classified according to the 8th
edition of the AJCC/TNM staging system (13). Histological diagnosis was reviewed by
the two experienced pathologists. PDC was diagnosed according to
the Turin criteria (14). Written
informed consent for publication of clinical details was obtained
from all patients. Sampling, storage, and analysis of the tumor
samples included in the present study were approved by the internal
review board on ethical issues of Hokuto Hospital, Obihiro, Japan
(Hokuto Hospital Institutional Ethics Committee no. 83).
Genetic analysis
Surgical specimens were obtained from 50 patients
with TC who underwent thyroidectomy. Genetic analysis was performed
according to the manufacturer's instructions (15,16).
Briefly, total DNA was extracted from 5-µm-thick formalin-fixed
paraffin-embedded (FFPE) tissue sections of TC specimens and areas
of no pathology using a Maxwell 16 FFPE Plus LEV DNA purification
kit (Promega, Madison, WI). The quality of genomic DNA was assessed
using a Qubit dsDNA BR assay kit (Life Technologies, Carlsbad, CA)
and a GeneRead DNA QuantiMIZE assay kit (Qiagen, Valencia, CA). The
GeneRead DNAseq Targeted Panels V2 Human Clinically Relevant Tumor
Panel (NGHS-101X; Qiagen) was used for amplicon sequencing of
targeted regions of 24 cancer-related genes (AKT1, ALK, AR,
BRAF, CTNNB1, DDR2, EGFR, ERBB2, FGFR3, GNA11, GNAQ, IDH1, IDH2,
KIT, KRAS, MAP2K1, MET, NRAS, PDGFRA, PIK3CA, PTEN, RET, STK11,
TP53). Library quality was assessed using an Agilent 2100
bioanalyzer (Agilent, Santa Clara, CA) and GeneRead Library Quant
kit (Qiagen). The libraries were sequenced using an Illumina MiSeq
(Illumina, San Diego, CA). Raw read data obtained from the amplicon
sequencing were processed using online analytical resources from
the GeneRead DNAseq Variant Calling Service for analysis of
mutations.
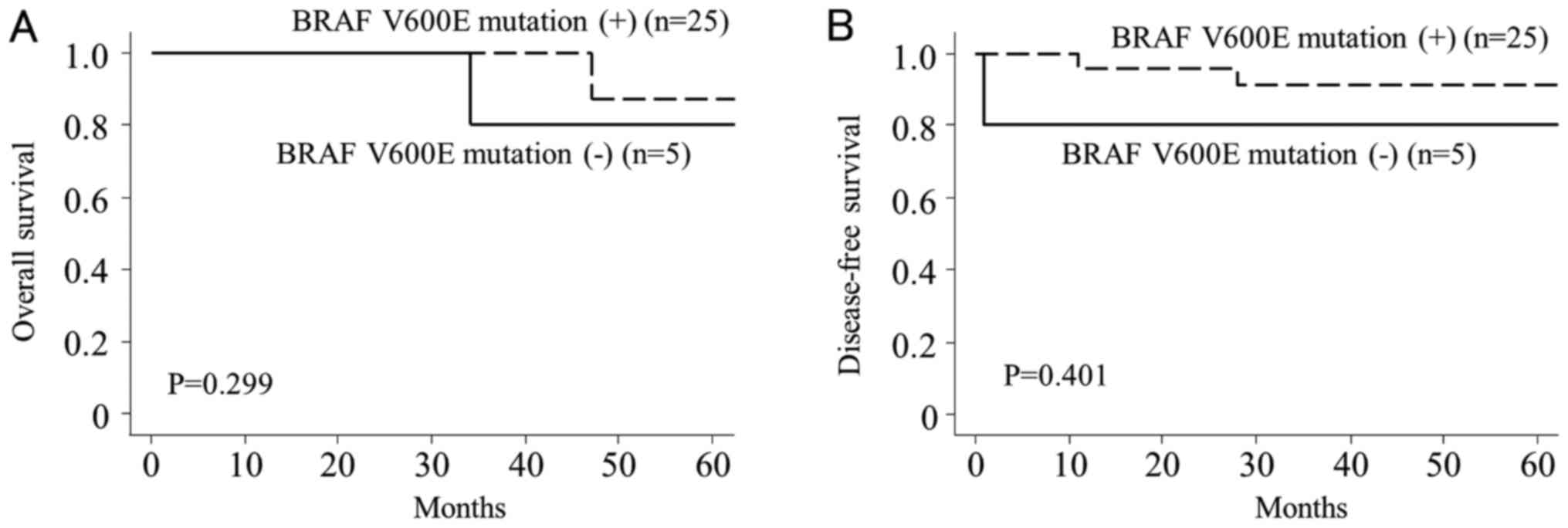
Statistical analysis
The significance of differences between two groups
was evaluated using Fisher's exact test and summarized with the
appropriate P-value. A P-value <0.05 was considered indicative
of statistical significance. Odds ratios and 95% confidence
intervals were also calculated. Overall survival time was measured
from the date of diagnosis to the date of death or date of last
follow-up visit. Disease-free survival time was measured from the
date of surgical removal of tumor to the date of first relapse or
the date of last follow-up. The probability of overall and
disease-free survival was calculated using the Kaplan-Meier method
and compared using the log-rank test.
Results
Clinicopathologic features
Clinicopathologic features and mutational pattern in
50 patients with TC are listed in Table
I. TC subtypes included 30 (60%) patients with PC, 2 (4%) with
papillary carcinoma tall cell variant (TVPC), 2 (4%) with papillary
carcinoma follicular variant (FVPC), 8 (16%) with FC, 7 (14) with PDC, and 1 (2%) with AC. Tumor size
ranged from 0.6 to 7.5 cm with a median size of 2.3 cm. A total of
22 patients (44%) were stage I, 17 (34%) were stage II, 8 (16%)
were stage III, and 3 (6%) were stage IVB. Hemi-thyroidectomy with
routine central compartment and lateral neck lymph node dissection
were performed in 29 (58%) and 4 (8%) patients, respectively. Total
thyroidectomy with routine central compartment and lateral neck
lymph node dissection were performed in 8 (16%) and 9 (18%)
patients, respectively. Disease pathologic T classification of was
T1a in 6 (12%) patients, T1b in 4 (8%), T2 in 7 (14%), T3a in 3
(6%), T3b in 16 (32%), T4a in 13 (26%) and T4b in 1 (2%). The
pathologic N classification was N0 in 24 (48%) patients, N1a in 12
(24%), and N1b in 14 (28%). Pathologic extrathyroidal extension and
multifocal tumors were observed in 30 (60%) and 23 (46%) patients,
respectively. Follow-up period ranged from 8 to 78 months, with a
median duration of 39 months for all patients. Forty-five (90%) of
the patients are alive without disease. Three (6%) patients (PC: 1,
PDC: 1, and AC: 1) died of disease due to distant metastasis. One
patient with PC was alive with neck lymph node recurrence, and 1
patient with PC was alive with lung metastasis at the time of this
report.
 | Table I.Clinicopathological features and
mutational pattern in 50 patients with thyroid carcinoma. |
Table I.
Clinicopathological features and
mutational pattern in 50 patients with thyroid carcinoma.
|
|
|
|
|
| Pathologic
findings | Mutation |
|---|
|
|
|
|
|
|
|
|
|---|
| No. | Age/sex | Histology | Tumor size, cm | Stage | pT | pN | Extension | Multifocality | BRAF | PIK3CA | TP53 | Other |
|---|
| 1 | 61/F | PC | 2.0 | I | 1b | 0 |
| + | V600E |
|
|
|
| 2 | 54/F | PC | 1.7 | I | 3b | 0 | + |
| V600E |
|
|
|
| 3 | 65/F | PC | 1.6 | I | 3b | 0 | + |
| V600E |
|
|
|
| 4 | 66/F | PC | 1.9 | I | 3b | 0 | + |
| V600E |
|
|
|
| 5 | 69/F | PC | 2.4 | I | 3b | 0 | + |
| V600E |
|
|
|
| 6 | 77/F | PC | 3.4 | I | 2 | 0 |
|
| V600E |
|
|
|
| 7 | 36/F | PC | 1.9 | I | 4a | 1a | + | + | V600E |
|
|
|
| 8 | 75/F | PC | 2.5 | I | 2 | 0 |
| + | V600E |
|
|
|
| 9 | 52/M | PC | 1.7 | I | 3b | 1a | + | + | V600E |
|
|
|
| 10 | 54/F | PC | 0.8 | I | 1a | 0 |
| + | V600E |
|
|
|
| 11 | 56/F | PC | 2.5 | II | 3b | 1a | + |
| V600E |
|
|
|
| 12 | 56/M | PC | 4.0 | II | 2 | 1a |
|
| V600E |
|
|
|
| 13 | 72/F | PC | 0.7 | II | 3b | 0 | + | + | V600E |
|
|
|
| 14 | 67/F | PC | 2.3 | II | 3b | 1a | + |
| V600E |
|
|
|
| 15 | 63/F | PC | 3.1 | II | 3b | 1b | + | + | V600E |
|
|
|
| 16 | 71/F | PC | 5.0 | II | 3b | 1b | + | + | V600E |
|
|
|
| 17 | 62/F | PC | 2.2 | II | 3b | 1a | + |
| V600E |
|
|
|
| 18 | 55/F | PC | 1.6 | III | 4a | 1a | + |
| V600E |
|
|
|
| 19 | 73/F | PC | 2.3 | III | 4a | 1a | + |
| V600E |
|
|
|
| 20 | 73/F | PC | 2.3 | III | 4a | 0 | + | + | V600E |
|
|
|
| 21 | 80/F | PC | 2.1 | III | 4a | 1b | + |
| V600E |
|
|
|
| 22 | 56/F | PC | 1.4 | III | 4a | 1b | + | + | V600E |
|
|
|
| 23 | 86/F | PC | 1.1 | III | 4a | 0 | + |
| V600E |
|
|
|
| 24 | 77/F | PC | 2.7 | III | 4a | 0 | + |
| V600E | delPV104P |
|
|
| 25 | 77/F | PC | 3.2 | II | 3b | 1b | + | + | V600E | A1046T | R306* | FGFR3
(G382R) |
| 26 | 86/F | PC | 5.0 | IVB | 4b | 1b | + | + |
| C420R |
| EGFR
(K852Q) |
| 27 | 49/F | PC | 5.9 | I | 4a | 1b | + |
|
|
|
|
|
| 28 | 83/F | PC | 1.0 | III | 4a | 1b | + |
|
|
|
|
|
| 29 | 78/F | PC | 1.1 | II | 3b | 0 | + | + |
|
|
|
|
| 30 | 51/M | PC | 1.5 | I | 4a | 1b | + | + |
|
|
|
|
| 31 | 26/F | TVPC | 0.8 | I | 3b | 1b | + | + | V600E |
|
|
|
| 32 | 83/F | TVPC | 4.5 | II | 3b | 1b | + | + | V600E |
|
|
|
| 33 | 85/F | FVPC | 4.4 | II | 3a | 0 |
|
|
|
|
|
|
| 34 | 56/F | FVPC | 1.7 | I | 1b | 0 |
| + |
|
|
| NRAS
(Q61K) |
| 35 | 49/F | FC | 3.2 | I | 2 | 0 |
|
|
|
|
|
|
| 36 | 76/F | FC | 3.6 | I | 2 | 0 |
|
|
|
|
|
|
| 37 | 71/F | FC | 1.0 | I | 1a | 0 |
|
|
|
|
|
|
| 38 | 56/F | FC | 3.4 | I | 2 | 0 |
|
|
|
|
|
|
| 39 | 55/F | FC | 7.5 | I | 1a | 0 |
|
|
|
|
|
|
| 40 | 54/F | FC | 3.6 | I | 2 | 0 |
|
|
|
|
|
|
| 41 | 74/F | FC | 6.5 | II | 3a | 0 |
|
|
|
|
|
|
| 42 | 71/M | FC | 4.6 | II | 3a | 0 |
|
|
|
|
|
|
| 43 | 76/F | PDC | 1.6 | II | 1b | 1a |
| + | V600E |
|
|
|
| 44 | 81/F | PDC | 4.2 | IVB | 4a | 1b | + | + | V600E |
|
|
|
| 45 | 74/F | PDC | 1.4 | II | 1b | 1a |
|
| V600E |
|
|
|
| 46 | 74/F | PDC | 2.0 | II | 3b | 0 | + |
| V600E |
|
|
|
| 47 | 51/F | PDC | 2.5 | I | 4a | 1a | + | + | V600E |
|
|
|
| 48 | 28/M | PDC | 1.0 | I | 1a | 1b |
| + |
| V600E | H1047R |
|
| 49 | 67/F | PDC | 0.7 | II | 1a | 1a |
| + |
|
|
|
|
| 50 | 86/F | AC | 0.6 | IVB | 1a | 1b |
| + |
| V600E |
| Q192* |
Mutational analysis
The BRAF V600E mutation was present in 25
(83%) of 30 patients with PC, in 2 (100%) of 2 with TVPC, in 6
(86%) of 7 with PDC, and in 1 AC patient (100%). PIK3CA
mutations were present in 3 (delPV104P, A1046T, and C420R; 10%) of
30 patients with PC and 1 (H1047R; 14%) of 7 with PDC. TP53
mutations were present in 1 (R306*; 3.3%) of 30 patients with PC
and 1 (Q152*; 14%) of 7 with PDC. An NRAS mutation (Q61K)
was present in 1 of 2 patients with FVPC. An FGFR3 mutation
(G382R) was present in 1 of 30 patients with PC, and an EGFR
mutation (K852Q) was present in 1 of 30 patients with PC.
Correlation of BRAF V600E mutation
with clinicopathologic factors in PC
Statistical analyses of the 30 patients with PC
showed no significant correlation between the BRAF V600E
mutation and clinicopathologic factors such as age, sex, tumor
size, stage, extrathyroidal extension, and multifocal tumor
(Table II). However, patients
without the BRAF V600E mutation had more advanced pathologic
T and N stages compared to patients with the mutation (P=0.047 and
P=0.019, respectively). Kaplan-Meier analysis showed that
BRAF V600E mutation was not significantly correlated with
overall (P=0.299, Fig. 1A) or
disease-free survival (P=0.401, Fig.
1B) in patients with PC.
 | Table II.Correlation of BRAF V600E
mutation with clinicopathologic factors in 30 patients with
papillary carcinoma. |
Table II.
Correlation of BRAF V600E
mutation with clinicopathologic factors in 30 patients with
papillary carcinoma.
|
|
| BRAF V600E
mutation |
|
|
|
|---|
|
|
|
|
|
|
|
|---|
| Variables | No. of
patients | + (n=25) | - (n=5) | P-value | OR | 95% CI |
|---|
| Age, years |
|
|
|
|
|
|
|
<55 | 6 | 4 | 2 | 0.254 | 1.00 |
|
|
≥55 | 24 | 21 | 3 |
| 0.29 | 0.04–2.30 |
| Sex |
|
|
|
|
|
|
|
Male | 3 | 2 | 1 | 0.434 | 1.00 |
|
|
Female | 27 | 23 | 4 |
| 0.35 | 0.02–4.80 |
| Tumor size, cm |
|
|
|
|
|
|
|
<2 | 14 | 11 | 3 | 0.642 | 1.00 |
|
| ≥2 | 16 | 14 | 2 |
| 0.52 | 0.07–3.70 |
| Stage |
|
|
|
|
|
|
| I,
II | 21 | 18 | 3 | 0.622 | 1.00 |
|
| III,
IVB | 9 | 7 | 2 |
| 1.71 | 0.23–12.60 |
| pT |
|
|
|
|
|
|
|
1a-3b | 19 | 18 | 1 | 0.047 | 1.00 |
|
| 4a,
4b | 11 | 7 | 4 |
| 10.29 | 1.00–109.00 |
| pN |
|
|
|
|
|
|
| 0,
1a | 21 | 20 | 1 | 0.019 | 1.00 |
|
| 1b | 9 | 5 | 4 |
| 16.00 | 1.45–177.00 |
| Extrathyroidal
extension |
|
|
|
|
|
|
| − | 5 | 5 | 0 | 0.556 | 1.00 |
|
| + | 25 | 20 | 5 |
| 1.25 | 1.02–1.52 |
| Multifocality |
|
|
|
|
|
|
| − | 16 | 14 | 2 | 0.642 | 1.00 |
|
| + | 14 | 11 | 3 |
| 1.91 | 0.27–13.50 |
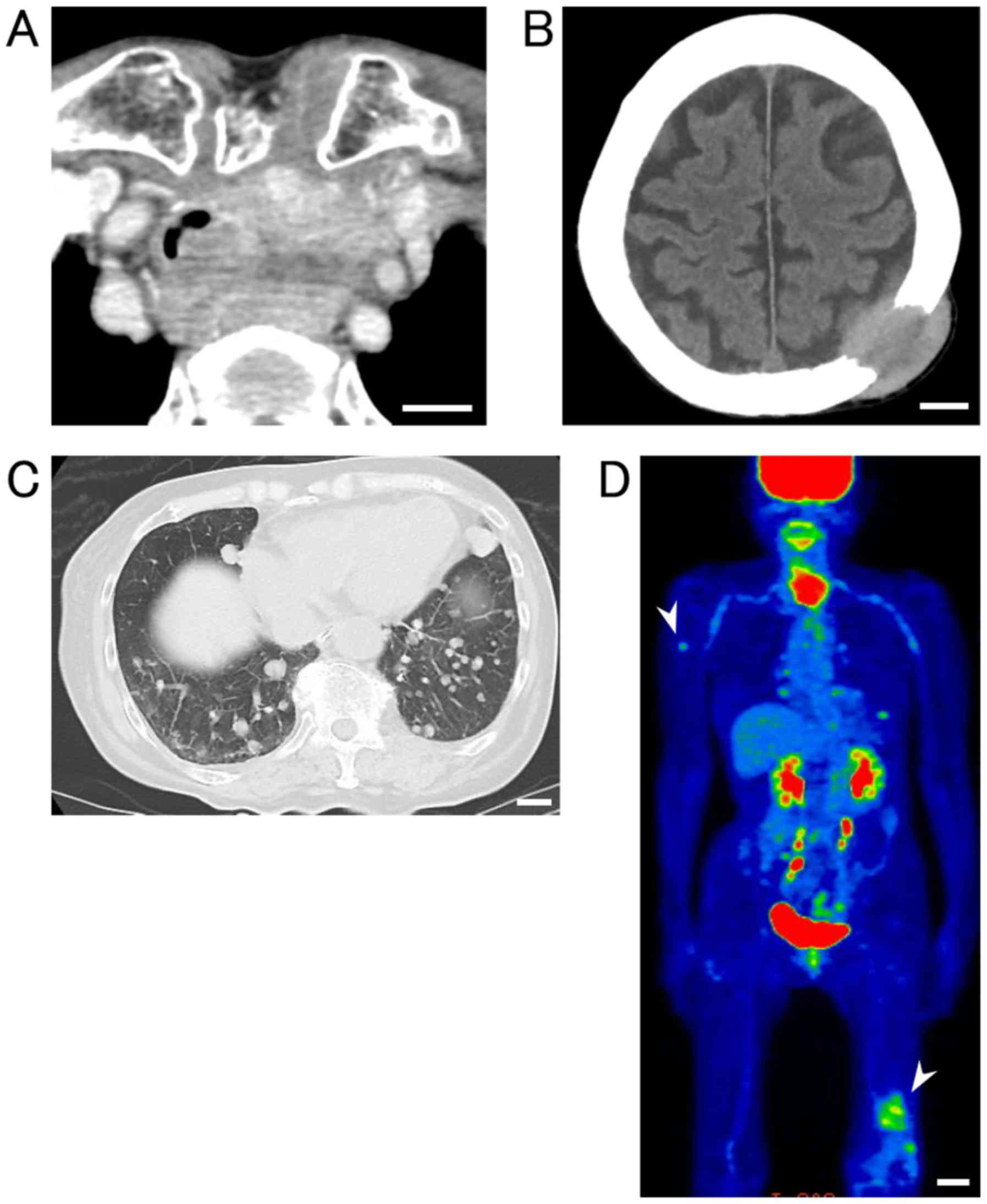
Case presentation of patient no.
26
An 86-year-old female complained of dyspnea and
suffered from pathologic fracture of the left femur. Enhanced
computed tomography (CT) scan revealed a thyroid tumor with
invasion of the trachea and esophagus (Fig. 2A). CT and fluorodeoxyglucose
(FDG)-positron emission tomography (PET)/CT scans showed multiple
bone metastases, including to the cranial bone (Fig. 2B), humerus, and femur (Fig. 2C), as well as multiple lung metastases
(Fig. 2D). Histologic analysis of
specimens from the thyroid tumor indicated PC. Genetic analysis of
the thyroid tumor using NGS showed that the patient harbored
EGFR (K852Q) and PIK3CA (C420R) mutations but no
BRAF mutation. After total thyroidectomy with tracheal
resection, the patient died, 34 months after the first clinic
visit.
Discussion
BRAF mutations in TC have been vigorously
investigated since the early 2000s (17,18). The
frequency of the BRAF V600E mutation reportedly ranges from
32 to 80% in patients with PC (4,19–21). Several large-scale multicenter studies
reported that the average frequency of the BRAF V600E
mutation in PC is approximately 48% (22,23). In
the present study, the frequency of the BRAF V600E mutation
in PC was 83%, which was higher than that previously reported. The
frequency in the present study may be biased due to the small
number of patients analyzed. However, the higher frequency could
also be attributed to tumors in patients from specific geographic
locations and to methodologic differences. Recent studies from
eastern Asia demonstrated a higher frequency of approximately 80%
for the BRAF V600E mutation in PC, which is consistent with
our results (24–27). Residents in eastern Asia commonly
consume seaweeds as a part of their regular diet. The region where
our hospital is located, and in which all the patients involved in
this study resided is well known for seaweed production and
consumption. Iodine intake has been linked with a higher frequency
of BRAF mutations in Korean patients with PC (28). Guan et al (29) reported that high iodine intake is
associated with a higher prevalence of the BRAF V600E
mutation in Chinese patients with PC. Elisei et al (30) suggested that iodine supplementation
might be associated with the increasing trend of BRAF
mutation in PC.
The frequency of BRAF mutations reported in
the literature has increased significantly over the years (31). This may be related to innovations in
methodologies used to detect mutations. The use of NGS could be
associated with the higher frequency of the BRAF V600E
mutation in patients with PC noted in the present study. To date,
the frequency of the BRAF V600E mutation in patients with PC
has been analyzed using Sanger sequencing (SGS) with FFPE (21,26), SGS
with frozen tissue (32,33), pyrosequencing (34) and real-time PCR (27). In the present study, we analyzed FFPE
tissue sections obtained from 50 patients with TC using an Illumina
Miseq sequencer. Since 2013, only 2 reports concerning PC and 2
reports concerning PDC and AC were published describing results of
mutational analyses using NGS with FFPE tissue sections (2,35–37). Tumor samples are histologically
heterogeneous (15), and
tumor-specific DNA contains varying proportions of contaminating
DNA from normal and inflammatory cells. NGS methods enables the
analysis of somatic mutation using a small amount of tumor-specific
DNA (38). NGS can detect a broad
range of mutations, including single nucleotide substitutions,
small insertions and deletions, and large genomic duplications.
Moreover, targeted NGS is more cost efficient and faster than SGS
(39). In general, the detection
sensitivity of NGS reported in previous studies is >94%
(40), which is greater than that of
SGS.
Results from numerous studies and meta-analyses have
associated the BRAF V600E mutation with high-risk
clinicopathologic features, such as larger tumor size,
extrathyroidal extension, higher stage at presentation, and lymph
node and distant metastases in patients with PC (4,20,22,30,31,41–43).
However, these associations remain controversial. A number of other
reports have suggested that there is no significant association
between the BRAF V600E mutation and high-risk
clinicopathologic features in patients with PC (25,34,44–46).
In the present study, contrary results were obtained, in that PC
patients without the BRAF V600E mutation had more advanced
pathologic T and N stages compared to patients with the mutation.
There have been few reports that support our results. The much
lower number of patients without the BRAF V600E mutation
(n=5) in our study compared with the number of patients with the
mutation (n=25) could have affected our results; that is, the
BRAF V600E mutation-negative group could have been biased.
However, 1 of the 5 PC patients without the BRAF V600E
mutation was previously described in the case presentation as
having PIK3CA and EGFR mutations. Three other
patients without the BRAF V600E mutation had copy number
alterations (CNAs) in either the PIK3CA, PTEN, DDR2, STK11,
or ERBB2 genes whereas only 2 of 25 patients with
BRAF V600E mutation had the alterations. We hypothesize that
the accumulation of other genetic alterations except for the
BRAF V600E mutation might have contributed to the advanced
pathologic stages in these patients.
A recent retrospective analysis of 1849 PC patients
found a mortality rate of 5.3% in BRAF V600E
mutation-positive patients vs. 1.1% in mutation-negative patients
(43). In contrast, Pelttari et
al (47) suggested that there was
no association between the BRAF V600E mutation and
recurrence following primary treatment with total thyroidectomy and
radioiodine remnant ablation in patients with PC. A study of
non-high-risk PC patients in Japan found no prognostic impact of
the BRAF V600E mutation on lymph node recurrence-free,
distant recurrence-free, or cause-specific survival (46). In the present study, there was no
correlation between the BRAF V600E mutation and overall and
disease-free survival in patients with PC. We obtained inconsistent
results, in that PC patients without the BRAF V600E mutation
had more advanced pathologic T and N stages but did not show poor
survival. That appropriate surgery was performed depending on the
extention of T and N stages in these subjects could explain this
inconsistency. Otherwise, other markers except for BRAF
V600E mutation may be associated with poorer prognosis. Shimamura
et al (48) suggested that the
BRAF V600E mutation alone is not sufficient for development
of PC. This, however, does not mean that BRAF V600E is not
the driver mutation, but rather that additional genetic and/or
epigenetic changes may be required for full transformation in PC.
Several other studies have agreed with this hypothesis, reporting
associations between development of PC and increased expression of
several tumor promoting molecules, including vimentin (49), matrix metalloproteinase (50), nuclear factor-κB (51), prohibitin (52), vascular endothelial growth factor
(53), and hepatocyte growth factor
receptor (54). A recent report
indicated that the telomerase reverse transcriptase (TERT)
promoter is a poor prognostic factor in patients with PC (55).
In the present study, 2 patients with TVPC harbored
the BRAF V600E mutation, whereas 2 patients with FVPC and 8
patients with FC did not harbor the BRAF V600E mutation.
TVPC, a subtype of PC, is characterized by a predominance of tall
and oncocytic tumor cells. Patients with TVPC exhibit a higher
recurrence rate and decreased disease-specific survival (56). The BRAF V600E mutation is
reportedly common in approximately 80% of TVPC cases (4). By contrast, in FVPC, another subtype of
PC, the BRAF V600E mutation is less common, reportedly found
in only approximately 10% of patients (4,57). FVPC is
instead characterized by a high prevalence of mutations other than
BRAF V600E, such as mutations in RAS and other
factors, which has been associated with follicular-pattern thyroid
tumors, including FC and follicular adenoma (4). The BRAF V600E mutation also
occurs in PDC and AC arising from PC (4,18). In the
present study, 7 PDCs and 1 AC were pathologically diagnosed as
derived from PC.
Mutations in PIK3CA that enhance PI3K/Akt
signaling are associated with tumor progression and
dedifferentiation in some human cancers and occur at an early stage
in tumorigenesis in TC (9). Using an
NGS approach, Nikiforova et al (35) showed that BRAF mutations are
the most frequent (59%), followed by mutation in PIK3CA
(11%), TP53 (7%), and NRAS (4%). Lee et al
(26) also demonstrated BRAF
mutations in 79.2% of PC patients and PIK3CA mutations in
10.4%. These data are consistent with our results demonstrating
that the second most frequent genetic mutations occurred in
PIK3CA in 10% of patients with PC. Over 90% of the mutations
in the PIK3CA gene in human cancers occur in 4 regions: The
p85 binding (exons 1 and 2), C2 (exon 7), helical (exon 9), and
catalytic (exon 20) domains (58).
Four mutations in PIK3CA we identified were located within
these regions, as previously reported. PIK3CA mutations are
related to tumor development, progression and more aggressive
behavior in TC (9). Therefore,
detecting PIK3CA mutations in patients with PC is also
critical (59).
In the case presentation, we presented a patient
with EGFR and PIK3CA mutations who exhibited an
aggressive clinical course. EGFR mutations are commonly
found in NSCLC, but they are less common in PC. The most common
genetic alterations in the EGFR gene are in-frame deletions
in exon 19 and point mutations in exon 21 in the intracellular
tyrosine kinase domain (60,61). The role of EGFR mutation in TC
remains unclear. Masago et al (11) reported 8PC patients with in-frame
deletion and/or L858R mutations in EGFR. One of the 8
patients showed distant metastasis as the initial manifestation. A
study of Korean patients found EGFR mutations and increased
copy number in 14 of 23 analyzed samples, suggesting that
EGFR genetic alterations are correlated with the biological
dedifferentiation process in TC (62). Of the 30 patients with PC in the
present study, the patient who showed multiple bone and lung
metastases at the first clinical visit and died with the disease
had an EGFR mutation. We hypothesize that EGFR
mutations in patients with PC are related to aggressive tumor
behaviors such as multiple lung and bone metastases.
There are some limitations to the present study.
First, we analyzed only 50 patients with TC, which was an
insufficient number of patients to correlate mutational status with
clinical significance. Most studies conducted to date were carried
out at a single institution using specific subtypes of TC with
small sample sizes. To overcome this limitation, multicenter
studies examining TC by geographic location will be required.
Second, we used a commercially available panel that targets only 24
cancer-related genes in the NGS analysis. The panel was not
specific for TC and not able to elucidate the underlying mechanism
of tumorigenesis in TC. Nikiforova et al has already
conducted an analysis of gene fusions, CNA, and abnormal gene
expression as well as mutational analysis of more than 100 genes
with the latest panel ThyroSeq v3 for thyroid tumor (63). In this way, a thyroid cancer-specific
gene panel that targets a larger number of cancer genes should be
employed in conjunction with NGS. Furthermore, analysis of
rearrangements in RET/PTC and PAX8/PPARγ in TC should
be carried out. Comprehensive molecular testing of both gene
mutations and rearrangements using new sequencing technologies will
contribute to the development of new screening systems for
predicting clinical outcome and assist in the development of new
molecular target treatments.
In conclusion, NGS analysis of 24 cancer-related
genes using FFPE tissue sections from 50 patients with TC revealed
the BRAF V600E mutation in 83% of patients with PC and 86%
of patients with PDC. Statistical analyses showed that patients
without this BRAF mutation had more advanced pathologic T
and N stages. A PC patient with EGFR and PIK3CA
mutations but without the BRAF V600E mutation showed an
aggressive course including multiple bone and lung metastases.
Analysis of cancer-related genes using NGS approaches can enhance
our understanding of the biological behavior of TC.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
NB, TG, MK, HI and KS performed surgery and acquired
data. TA, TS and TY performed the mutational analyses. HNa and YuK
confirmed the mutational analysis data. HNi and YaK performed the
pathologic diagnoses. HK and YH conceived the study design. NB
drafted the manuscript and analyzed the clinical data. All authors
read and approved the final version of the manuscript.
Ethics approval and consent to
participate
Written informed consent for publication of clinical
details was obtained from all patients. Sampling, storage, and
analysis of the tumor samples included in the present study were
approved by the internal review board on ethical issues of Hokuto
Hospital, Obihiro, Japan (Hokuto Hospital Institutional Ethics
Committee no. 83).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
TC
|
thyroid carcinoma
|
|
PC
|
papillary carcinoma
|
|
TVPC
|
papillary carcinoma tall cell
variant
|
|
FVPC
|
papillary carcinoma follicular
variant
|
|
FC
|
follicular carcinoma
|
|
PDC
|
poorly differentiated carcinoma
|
|
AC
|
anaplastic carcinoma
|
|
BRAF
|
v-raf murine sarcoma viral oncogene
homolog B1
|
|
PI3K/Akt
|
phosphatidylinositol-3 kinase/v-Akt
murine thymoma viral oncogene
|
|
PIK3CA
|
phosphatidylinositol-4,
5-bisphosphate 3-kinase catalytic subunit alpha isoform
|
|
EGFR
|
epidermal growth factor receptor
|
|
NGS
|
next-generation sequencing
|
References
|
1
|
Xing M: BRAF mutation in papillary thyroid
cancer: Pathogenic role, molecular bases, and clinical
implications. Endocr Rev. 28:742–762. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gerber TS, Schad A, Hartmann N, Springer
E, Zechner U and Musholt TJ: Targeted next-generation sequencing of
cancer genes in poorly differentiated thyroid cancer. Endocr
Connect. 7:47–55. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jeon MJ, Chun SM, Kim D, Kwon H, Jang EK,
Kim TY, Kim WB, Shong YK, Jang SJ, Song DE and Kim WG: Genomic
alterations of anaplastic thyroid carcinoma detected by targeted
massive parallel sequencing in a BRAF (V600E) mutation-prevalent
area. Thyroid. 26:683–690. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nikiforov YE: Molecular analysis of
thyroid tumors. Mod Pathol. 24 Suppl 2:S34–S43. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kondo T, Ezzat S and Asa SL: Pathogenetic
mechanisms in thyroid follicular-cell neoplasia. Nat Rev Cancer.
6:292–306. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Davies H, Bignell GR, Cox C, Stephens P,
Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W,
et al: Mutations of the BRAF gene in human cancer. Nature.
417:949–954. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Vasko V, Espinosa AV, Scouten W, He H,
Auer H, Liyanarachchi S, Larin A, Savchenko V, Francis GL, de la
Chapelle A, et al: Gene expression and functional evidence of
epithelial-to-mesenchymal transition in papillary thyroid carcinoma
invasion. Proc Natl Acad Sci USA. 104:2803–2808. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Karakas B, Bachman KE and Park BH:
Mutation of the PIK3CA oncogene in human cancers. Br J Cancer.
94:455–459. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liu D, Hou P, Liu Z, Wu G and Xing M:
Genetic alterations in the phosphoinositide 3-kinase/Akt signaling
pathway confer sensitivity of thyroid cancer cells to therapeutic
targeting of Akt and mammalian target of rapamycin. Cancer Res.
69:7311–7319. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wojciechowska-Durczyńska K,
Krawczyk-Rusiecka K, Cyniak-Magierska A, Zygmunt A, Gałecka E and
Lewiński A: Relative quantification of PIK3CA gene expression level
in fine-needle aspiration biopsy thyroid specimens collected from
patients with papillary thyroid carcinoma and non-toxic goitre by
real-time RT-PCR. Thyroid Res. 3:52010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Masago K, Asato R, Fujita S, Hirano S,
Tamura Y, Kanda T, Mio T, Katakami N, Mishima M and Ito J:
Epidermal growth factor receptor gene mutations in papillary
thyroid carcinoma. Int J Cancer. 124:2744–2749. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cha YJ and Koo JS: Next-generation
sequencing in thyroid cancer. J Transl Med. 14:3222016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tuttle RM, Haugen B and Perrier ND:
Updated American joint committee on cancer/tumor-node-metastasis
staging system for differentiated and anaplastic thyroid cancer
(Eighth Edition): What changed and why? Thyroid. 27:751–756. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Volante M, Collini P, Nikiforov YE,
Sakamoto A, Kakudo K, Katoh R, Lloyd RV, LiVolsi VA, Papotti M,
Sobrinho-Simoes M, et al: Poorly differentiated thyroid carcinoma:
The Turin proposal for the use of uniform diagnostic criteria and
an algorithmic diagnostic approach. Am J Surg Pathol. 31:1256–1264.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ellison G, Huang S, Carr H, Wallace A,
Ahdesmaki M, Bhaskar S and Mills J: A reliable method for the
detection of BRCA1 and BRCA2 mutations in fixed tumour tissue
utilising multiplex PCR-based targeted next generation sequencing.
BMC Clin Pathol. 15:52015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gremel G, Lee RJ, Girotti MR, Mandal AK,
Valpione S, Garner G, Ayub M, Wood S, Rothwell DG, Fusi A, et al:
Distinct subclonal tumour responses to therapy revealed by
circulating cell-free DNA. Ann Oncol. 27:1959–1965. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kimura ET, Nikiforova MN, Zhu Z, Knauf JA,
Nikiforov YE and Fagin JA: High prevalence of BRAF mutations in
thyroid cancer: Genetic evidence for constitutive activation of the
RET/PTC-RAS-BRAF signaling pathway in papillary thyroid carcinoma.
Cancer Res. 63:1454–1457. 2003.PubMed/NCBI
|
|
18
|
Namba H, Nakashima M, Hayashi T, Hayashida
N, Maeda S, Rogounovitch TI, Ohtsuru A, Saenko VA, Kanematsu T and
Yamashita S: Clinical implication of hot spot BRAF mutation, V599E,
in papillary thyroid cancers. J Clin Endocrinol Metab.
88:4393–4397. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Şahpaz A, Önal B, Yeşilyurt A, Han Ü and
Delibaşı T: BRAF (V600E) mutation, RET/PTC1 and PAX8-PPAR gamma
rearrangements in follicular epithelium derived thyroid
lesions-institutional experience and literature review. Balkan Med
J. 32:156–166. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Fernandez IJ, Piccin O, Sciascia S,
Cavicchi O, Repaci A, Vicennati V and Fiorentino M: Clinical
significance of BRAF mutation in thyroid papillary cancer.
Otolaryngol Head Neck Surg. 148:919–925. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li C, Aragon Han P, Lee KC, Lee LC, Fox
AC, Beninato T, Thiess M, Dy BM, Sebo TJ, Thompson GB, et al: Does
BRAF V600E mutation predict aggressive features in papillary
thyroid cancer? Results from four endocrine surgery centers. J Clin
Endocrinol Metab. 98:3702–3712. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kim TH, Park YJ, Lim JA, Ahn HY, Lee EK,
Lee YJ, Kim KW, Hahn SK, Youn YK, Kim KH, et al: The association of
the BRAF (V600E) mutation with prognostic factors and poor clinical
outcome in papillary thyroid cancer: A meta-analysis. Cancer.
118:1764–1773. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Xing M, Alzahrani AS, Carson KA, Shong YK,
Kim TY, Viola D, Elisei R, Bendlová B, Yip L, Mian C, et al:
Association between BRAF V600E mutation and recurrence of papillary
thyroid cancer. J Clin Oncol. 33:42–50. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Liang J, Cai W, Feng D, Teng H, Mao F,
Jiang Y, Hu S, Li X, Zhang Y, Liu B and Sun ZS: Genetic landscape
of papillary thyroid carcinoma in the Chinese population. J Pathol.
244:215–226. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yim JH, Kim WG, Jeon MJ, Han JM, Kim TY,
Yoon JH, Hong SJ, Song DE, Gong G, Shong YK and Kim WB: Association
between expression of X-linked inhibitor of apoptosis protein and
the clinical outcome in a BRAF V600E-prevalent papillary thyroid
cancer population. Thyroid. 24:689–694. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lee MY, Ku BM, Kim HS, Lee JY, Lim SH, Sun
JM, Lee SH, Park K, Oh YL, Hong M, et al: Genetic alterations and
their clinical implications in high-recurrence risk papillary
thyroid cancer. Cancer Res Treat. 49:906–914. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kim WW, Ha TK and Bae SK: Clinical
implications of the BRAF mutation in papillary thyroid carcinoma
and chronic lymphocytic thyroiditis. J Otolaryngol Head Neck Surg.
47:42018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kim HJ, Park HK, Byun DW, Suh K, Yoo MH,
Min YK, Kim SW and Chung JH: Iodine intake as a risk factor for
BRAF mutations in papillary thyroid cancer patients from an
iodine-replete area. Eur J Nutr. 57:809–815. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Guan H, Ji M, Bao R, Yu H, Wang Y, Hou P,
Zhang Y, Shan Z, Teng W and Xing M: Association of high iodine
intake with the T1799A BRAF mutation in papillary thyroid cancer. J
Clin Endocrinol Metab. 94:1612–1617. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Elisei R, Viola D, Torregrossa L, Giannini
R, Romei C, Ugolini C, Molinaro E, Agate L, Biagini A, Lupi C, et
al: The BRAF(V600E) mutation is an independent, poor prognostic
factor for the outcome of patients with low-risk intrathyroid
papillary thyroid carcinoma: Single-institution results from a
large cohort study. J Clin Endocrinol Metab. 97:4390–4398. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Vuong HG, Altibi AM, Abdelhamid AH, Ngoc
PU, Quan VD, Tantawi MY, Elfil M, Vu TL, Elgebaly A, Oishi N, et
al: The changing characteristics and molecular profiles of
papillary thyroid carcinoma over time: A systematic review.
Oncotarget. 8:10637–10649. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Jin L, Chen E, Dong S, Cai Y, Zhang X,
Zhou Y, Zeng R, Yang F, Pan C, Liu Y, et al: BRAF and TERT promoter
mutations in the aggressiveness of papillary thyroid carcinoma: A
study of 653 patients. Oncotarget. 7:18346–18355. 2015.
|
|
33
|
Nakayama H, Yoshida A, Nakamura Y, Hayashi
H, Miyagi Y, Wada N, Rino Y, Masuda M and Imada T: Clinical
significance of BRAF (V600E) mutation and Ki-67 labeling index in
papillary thyroid carcinomas. Anticancer Res. 27:3645–3649.
2007.PubMed/NCBI
|
|
34
|
Barbaro D, Incensati RM, Materazzi G, Boni
G, Grosso M, Panicucci E, Lapi P, Pasquini C and Miccoli P: The
BRAF V600E mutation in papillary thyroid cancer with positive or
suspected pre-surgical cytological finding is not associated with
advanced stages or worse prognosis. Endocrine. 45:462–468. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Nikiforova MN, Wald AI, Roy S, Durso MB
and Nikiforov YE: Targeted next-generation sequencing panel
(ThyroSeq) for detection of mutations in thyroid cancer. J Clin
Endocrinol Metab. 98:E1852–E1860. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Goldenberg D, Russo M, Houser K, Crist H,
Derr JB, Walter V, Warrick JI, Sheldon KE, Broach J and Bann DV:
Altered molecular profile in thyroid cancers from patients affected
by the three mile island nuclear accident. Laryngoscope. 127 Suppl
3:S1–S9. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Landa I, Ibrahimpasic T, Boucai L, Sinha
R, Knauf JA, Shah RH, Dogan S, Ricarte-Filho JC, Krishnamoorthy GP,
Xu B, et al: Genomic and transcriptomic hallmarks of poorly
differentiated and anaplastic thyroid cancers. J Clin Invest.
126:1052–1066. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Sims D, Sudbery I, Ilott NE, Heger A and
Ponting CP: Sequencing depth and coverage: Key considerations in
genomic analyses. Nat Rev Genet. 15:121–132. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Walsh T, Lee MK, Casadei S, Thornton AM,
Stray SM, Pennil C, Nord AS, Mandell JB, Swisher EM and King MC:
Detection of inherited mutations for breast and ovarian cancer
using genomic capture and massively parallel sequencing. Proc Natl
Acad Sci USA. 107:12629–12633. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Lin MT, Mosier SL, Thiess M, Beierl KF,
Debeljak M, Tseng LH, Chen G, Yegnasubramanian S, Ho H, Cope L, et
al: Clinical validation of KRAS BRAF, and EGFR mutation detection
using next-generation sequencing. Am J Clin Pathol. 141:856–866.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Lim JY, Hong SW, Lee YS, Kim BW, Park CS,
Chang HS and Cho JY: Clinicopathologic implications of the
BRAF(V600E) mutation in papillary thyroid cancer: A subgroup
analysis of 3130 cases in a single center. Thyroid. 23:1423–1430.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Chen Y, Sadow PM, Suh H, Lee KE, Choi JY,
Suh YJ, Wang TS and Lubitz CC: BRAF(V600E) is correlated with
recurrence of papillary thyroid microcarcinoma: A systematic
review, multi-institutional primary data analysis, and
meta-analysis. Thyroid. 26:248–255. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Xing M, Alzahrani AS, Carson KA, Viola D,
Elisei R, Bendlova B, Yip L, Mian C, Vianello F, Tuttle RM, et al:
Association between BRAF V600E mutation and mortality in patients
with papillary thyroid cancer. JAMA. 309:1493–1501. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Kim TY, Kim WB, Song JY, Rhee YS, Gong G,
Cho YM, Kim SY, Kim SC, Hong SJ and Shong YK: The BRAF mutation is
not associated with poor prognostic factors in Korean patients with
conventional papillary thyroid microcarcinoma. Clin Endocrinol
(Oxf). 63:588–593. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Nikiforov YE: Radiation-induced thyroid
cancer: What we have learned from chernobyl. Endocr Pathol.
17:307–317. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Ito Y, Yoshida H, Kihara M, Kobayashi K,
Miya A and Miyauchi A: BRAF(V600E) mutation analysis in papillary
thyroid carcinoma: Is it useful for all patients? World J Surg.
38:679–687. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Pelttari H, Schalin-Jäntti C, Arola J,
Löyttyniemi E, Knuutila S and Välimäki MJ: BRAF V600E mutation does
not predict recurrence after long-term follow-up in TNM stage I or
II papillary thyroid carcinoma patients. APMIS. 120:380–386. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Shimamura M, Nakahara M, Orim F, Kurashige
T, Mitsutake N, Nakashima M, Kondo S, Yamada M, Taguchi R, Kimura S
and Nagayama Y: Postnatal expression of BRAFV600E does not induce
thyroid cancer in mouse models of thyroid papillary carcinoma.
Endocrinology. 154:4423–4430. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Watanabe R, Hayashi Y, Sassa M, Kikumori
T, Imai T, Kiuchi T and Murata Y: Possible involvement of BRAFV600E
in altered gene expression in papillary thyroid cancer. Endocr J.
56:407–414. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Mesa C Jr, Mirza M, Mitsutake N, Sartor M,
Medvedovic M, Tomlinson C, Knauf JA, Weber GF and Fagin JA:
Conditional activation of RET/PTC3 and BRAFV600E in thyroid cells
is associated with gene expression profiles that predict a
preferential role of BRAF in extracellular matrix remodeling.
Cancer Res. 66:6521–6529. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Palona I, Namba H, Mitsutake N, Starenki
D, Podtcheko A, Sedliarou I, Ohtsuru A, Saenko V, Nagayama Y,
Umezawa K and Yamashita S: BRAFV600E promotes invasiveness of
thyroid cancer cells through nuclear factor kappaB activation.
Endocrinology. 147:5699–5707. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Franzoni A, Dima M, D'Agostino M, Puppin
C, Fabbro D, Loreto CD, Pandolfi M, Puxeddu E, Moretti S, Celano M,
et al: Prohibitin is overexpressed in papillary thyroid carcinomas
bearing the BRAF(V600E) mutation. Thyroid. 19:247–255. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Jo YS, Li S, Song JH, Kwon KH, Lee JC, Rha
SY, Lee HJ, Sul JY, Kweon GR, Ro HK, et al: Influence of the BRAF
V600E mutation on expression of vascular endothelial growth factor
in papillary thyroid cancer. J Clin Endocrinol Metab. 91:3667–3670.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Giordano TJ, Kuick R, Thomas DG, Misek DE,
Vinco M, Sanders D, Zhu Z, Ciampi R, Roh M, Shedden K, et al:
Molecular classification of papillary thyroid carcinoma: Distinct
BRAF RAS, and RET/PTC mutation-specific gene expression profiles
discovered by DNA microarray analysis. Oncogene. 24:6646–6656.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Oishi N, Kondo T, Ebina A, Sato Y, Akaishi
J, Hino R, Yamamoto N, Mochizuki K, Nakazawa T, Yokomichi H, et al:
Molecular alterations of coexisting thyroid papillary carcinoma and
anaplastic carcinoma: Identification of TERT mutation as an
independent risk factor for transformation. Mod Pathol.
30:1527–1537. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Penna GC, Vaisman F, Vaisman M,
Sobrinho-Simões M and Soares P: Molecular markers involved in
tumorigenesis of thyroid carcinoma: Focus on aggressive histotypes.
Cytogenet Genome Res. 150:194–207. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Jiang L, Chu H and Zheng H: B-Raf mutation
and papillary thyroid carcinoma patients. Oncol Lett. 11:2699–2705.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Samuels Y and Velculescu VE: Oncogenic
mutations of PIK3CA in human cancers. Cell Cycle. 3:1221–1224.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Arsenic R, Treue D, Lehmann A, Hummel M,
Dietel M, Denkert C and Budczies J: Comparison of targeted
next-generation sequencing and sanger sequencing for the detection
of PIK3CA mutations in breast cancer. BMC Clin Pathol. 15:202015.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Sharma SV, Bell DW, Settleman J and Haber
DA: Epidermal growth factor receptor mutations in lung cancer. Nat
Rev Cancer. 7:169–181. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Ciardiello F and Tortora G: EGFR
antagonists in cancer treatment. N Engl J Med. 358:1160–1174. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Lee DH, Lee GK, Kong SY, Kook MC, Yang SK,
Park SY, Park SH, Keam B, Park DJ, Cho BY, et al: Epidermal growth
factor receptor status in anaplastic thyroid carcinoma. J Clin
Pathol. 60:881–884. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Nikiforova MN, Mercurio S, Wald AI, Barbi
de Moura M, Callenberg K, Santana-Santos L, Gooding WE, Yip L,
Ferris RL and Nikiforov YE: Analytical performance of the ThyroSeq
v3 genomic classifier for cancer diagnosis in thyroid nodules.
Cancer. 124:1682–1690. 2018. View Article : Google Scholar : PubMed/NCBI
|