Introduction
Spinal osseous tumors have complex lesion types,
which can be divided into metastatic tumor and primary tumor, in
which primary spinal osseous tumor is a rare tumor disease taking
up approximately 7% in systemic tumors, and its rate of
deterioration is relatively high with the occurrence of disease
(1,2).
The highest proportion of metastatic tumor is >50%, half of
which are benign tumors and the remaining half are malignant
tumors. It is characterized by various types, low differences in
imaging features and difficult diagnosis. As the nerves and
capillaries are densely distributed around the spine, removal of
the tumor with minimal wound can be reached only after the
occurrence site and the scope of the tumor are mastered well
(3). Therefore, in order to reduce
misdiagnosis and postoperative recurrence rates, a total of 69
patients with primary spinal osseous tumors were analyzed to
further explore the imaging features and provide guidance for
clinical diagnosis and treatment.
Patients and methods
General patient data
A total of 69 patients with primary spinal osseous
tumors who received treatment in Nankai Hospital (Tianjin, China)
from July 2016 to June 2017 were selected into the study. It was
confirmed by pathological diagnosis that all the patients suffered
from the disease, and all of them received X-ray, computed
tomography (CT) and magnetic resonance imaging (MRI) examinations
(4). General data of study patients
are given in Table I. The study was
approved by the Ethics Committee of Nankai Hospital and informed
consents were signed by the patients or guardians.
 | Table I.General data of the patients. |
Table I.
General data of the patients.
| Items | Subject (n=69) |
|---|
| Male (n, %) | 36 (52.17) |
| Female (n, %) | 33 (47.83) |
| Age (years) | 10–70 |
| Average age
(years) | 24.36±4.49 |
| Clinical
manifestation |
|
| Chest and back
pain | 52 (75.36) |
| Radioactive pain | 14 (20.29) |
| Fever | 19 (27.54) |
| Local swelling | 5 (7.25) |
| Perspiration
dysfunction | 11 (15.94) |
| Limited mobility | 3 (4.35) |
X-ray examination
X-ray examination was conducted for all the
patients. Siemens digital radiography (DR) machine was adopted for
X-ray on the posteroanterior and single lateralposition of the pain
site of the patient. X-ray was conducted on double oblique
positions if necessary.
CT examination
All the patients received CT examinations in a
supine position using a dual-source 64-row CT scanner (produced by
Siemens, Munich, Germany). Parameters of the CT scanner were set as
follows. Current: 260–300 msec; voltage: 120 kV; layer thickness: 5
mm; interlayer spacing: 1 mm; matrix: 512×512. The scanning was
conducted on the spine with lesions and the adjacent vertebral
body. An enhanced scan was conducted with iohexol [produced by
Guangzhou Schering Pharmaceutical Co., Ltd., Guangzhou, China,
concentration: 300 mg I/ml], a non-ionic iodine-containing contrast
agent, in a dose of 1.5 ml/kg (body weight) by bolus injection with
a high-pressure syringe in the same method as plain scan.
MRI examination
All the patients received MRI examinations with an
MRI scanner (MR 3.0T HDX TWINSP produced by General Electric Co.,
Fairfield, CT, USA). Routine T1 weighted imaging (T1WI) and T2
weighted imaging (T2WI) examinations were conducted, in which T1WI:
time of repetition (TR): 200–540 msec, time to echo (TE): 2–14
msec; T2WI: TR = 3,000-5,000 msec, TE = 23–138 msec. The scanning
site was the center of the patient's pain site, and the scope of
the scanning was the spine and the adjacent vertebral body of the
patient.
Evaluation methods
The imaging results were analyzed by two senior
imaging diagnosis physicians (with more than 10-year working
experience). When the results obtained by them were inconsistent,
they would reach a common conclusion by discussion. Sensitivity
(Sen), specificity (Spe), positive predictive value
(PV+), negative predictive value (PV−) and
accuracy (Acc) were compared among the three examination methods
using the pathological results as the gold standard.
Statistical analysis
Four parameters (including true positive, false
positive, true negative and false negative) were established for
X-ray, CT and MRI diagnosis tests, respectively, using the
pathological results as the gold standard, and indicators of
diagnostic efficacy were calculated. Positive referred to malignant
tumors, while negative referred to benign tumors. Statistical
Product and Service Solutions (SPSS) 19.0 (SPSS Inc., Chicago, IL,
USA) was adopted for statistics. A paired χ2 test was
performed to analyze the difference and consistency of accuracy of
X-ray, CT and MRI examinations in diagnosing primary spinal osseous
tumors. ANOVA was used for comparison between multiple groups and
the post hoc test was LSD test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparison of imaging features of
different examination methods
CT scan had obvious advantages in diagnosing tumors
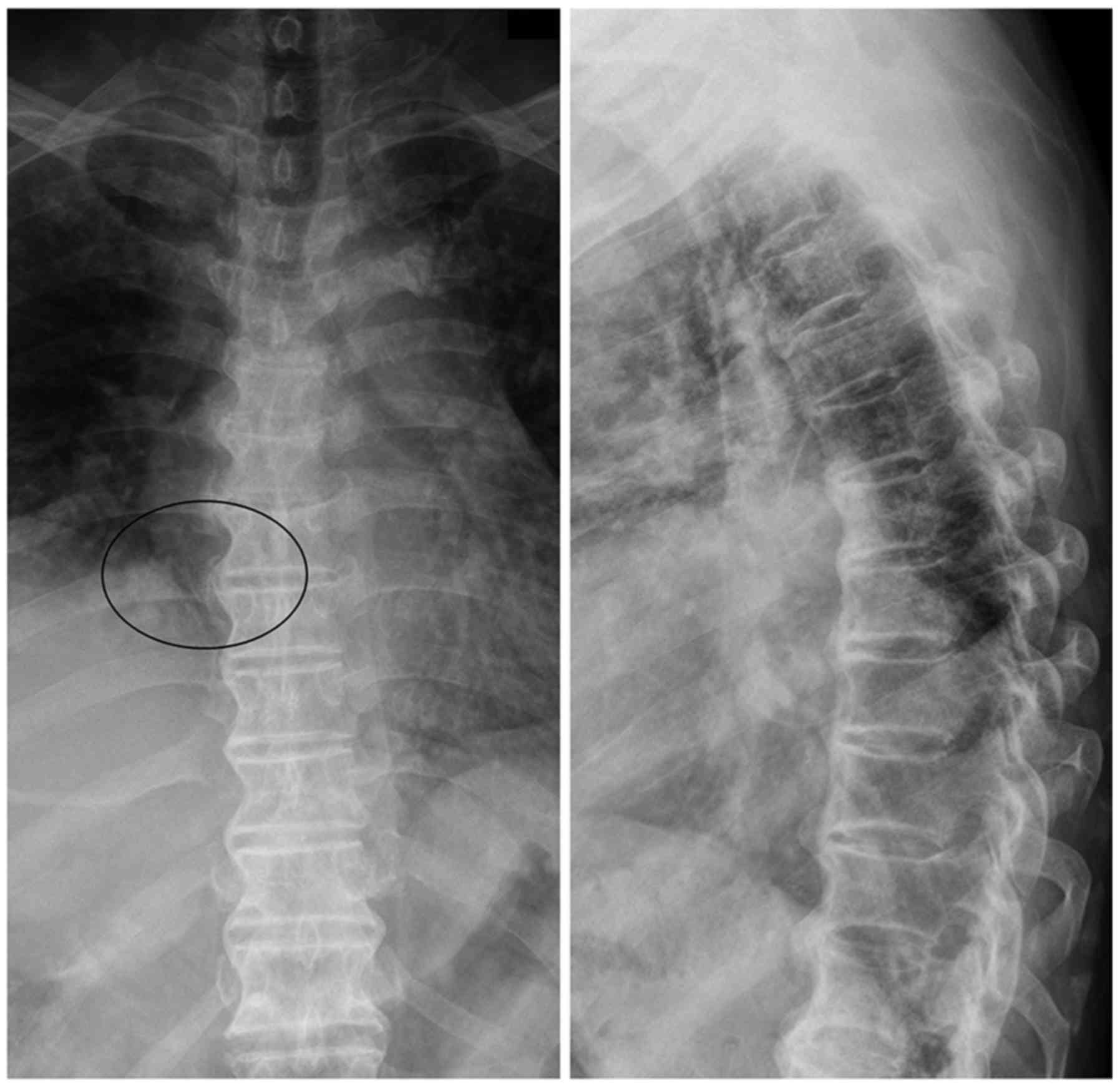
such as lesion calcification and osteolytic destruction (Fig. 1); X-ray showed better contrast and
clarity of the spine, and bone structure could be seen clearly by
this method (Fig. 2); MRI was more
sensitive to the imaging of the spinal cord, which could be used to
discover early tumor lesion based on the change in bone marrow
signal (Fig. 3).
Comparison of diagnostic efficacy of
different examination methods
X-ray, CT and MRI examination showed that Sen, Acc
and PV− of the three examination methods in diagnosing
spinal osseous tumors were significantly different. MRI examination
showed the highest Sen (P<0.05). Spe and PV+ of the
three examination methods had no obvious differences (P>0.05)
(Table II).
 | Table II.Comparison of diagnostic efficacy
among X-ray, CT and MRI examination methods (%). |
Table II.
Comparison of diagnostic efficacy
among X-ray, CT and MRI examination methods (%).
| Examination
method | Sen | Spe | Acc | PV+ | PV− |
|---|
| X-ray | 76.81 | 86.96 | 78.26 | 92.75 | 62.32 |
| CT | 86.96 | 88.41 | 86.96 | 94.20 | 72.46 |
| MRI | 92.75a | 89.86 | 91.30a | 95.65 | 85.51a |
Diagnostic consistency of MRI and CT
with pathological results
The diagnostic results of primary spinal osseous
tumors obtained with MRI examination and those obtained with CT
scan were compared with the pathological results, respectively,
which showed that 45 patients had consistent results with the
pathological results by the two methods, and that 19 patients had
inconsistent results with the pathological results by the two
methods. The two methods had relatively high consistency in
diagnosing primary spinal osseous tumors (κ-value = 0.72) (Table III).
 | Table III.Comparison between MRI examination and
CT scan (n). |
Table III.
Comparison between MRI examination and
CT scan (n).
|
| Results obtained with
CT scan vs. pathological results |
|
|---|
|
|
|
|
|---|
| Results obtained with
MRI examination vs. pathological results | Consistent | Inconsistent | Total |
|---|
| Consistent | 45 | 3 | 48 |
| Inconsistent | 5 | 16 | 21 |
| Total | 50 | 19 | 69 |
Diagnostic consistency of CT and X-ray
with pathological results
The diagnostic results of primary spinal osseous
tumors obtained with CT scan and those obtained with X-ray were
compared with the pathological results, which showed that 42
patients had consistent results with the pathological results by
the two methods, and that 12 patients had inconsistent results with
the pathological results by the two methods. The two methods had
relatively low consistency in diagnosing primary spinal osseous
tumors (κ-value = 0.47) (Table
IV).
 | Table IV.Comparison between CT scan and X-ray
(n). |
Table IV.
Comparison between CT scan and X-ray
(n).
|
| Results obtained with
X-ray vs. pathological results |
|
|---|
|
|
|
|
|---|
| Results obtained with
CT scan vs. pathological results | Consistent | Inconsistent | Total |
|---|
| Consistent | 42 | 11 | 53 |
| Inconsistent | 4 | 12 | 16 |
| Total | 46 | 23 | 69 |
Diagnostic consistency of MRI and
X-ray with pathological results
The diagnostic results of primary spinal osseous
tumors obtained with MRI examination and those obtained with X-ray
were compared with the pathological results, respectively, which
showed that 41 patients had consistent results with the
pathological results by the two methods, and that 11 patients had
inconsistent results with the pathological results by the two
methods. The two methods had relatively low consistency in
diagnosing primary spinal osseous tumors (κ-value=0.41) (Table V).
 | Table V.Comparison between MRI examination and
X-ray (n). |
Table V.
Comparison between MRI examination and
X-ray (n).
|
| Results obtained with
X-ray vs. pathological results |
|
|---|
|
|
|
|
|---|
| Results obtained with
MRI examination vs. pathological results | Consistent | Inconsistent | Total |
|---|
| Consistent | 41 | 13 | 54 |
| Inconsistent | 4 | 11 | 15 |
| Total | 45 | 24 | 69 |
Discussion
Spinal osseous tumors can occur in any part of the
vertebrae, mainly in the thoracic vertebrae, followed by the sacral
and lumbar spine, but rarely occur in cervical spine (5,6). They
include benign tumors (such as giant cell tumor of bone,
osteochondroma, hemangioma and aneurysmal bone cyst) and malignant
tumors (such as chordoma, myeloma, chondrosarcoma and Ewing's
sarcoma), of which the malignant spinal tumor frequently occurs in
the middle-aged and the elderly, while the benign tumors are mainly
concentrated in the young people (7).
Surgical treatments such as radiotherapy, chemotherapy and
laminectomy are usually adopted in clinic for the treatment of
spinal osseous tumors. With the continuous development of imaging
and related medical technology, early detection and surgical
treatment have become indispensable treatment methods (8).
X-ray plain film can be available to find most of
the vertebral tumors. Its diagnostic principle is that it has
relatively high sensitivity and relatively high spatial resolution
in imaging bone tissues, and can clearly show the size and the
structure of the bone as well as the destruction on the bones in
the skeleton and the periosteal reaction based on the change in
bone mineral density caused by the change in the concentration of
calcium in the spine (4,9). However, it cannot be used for the
examination and analysis of cartilage lesions due to its
limitations, and the adnexal tumors and those under the adnexa are
easy to be omitted. The examination is the most basic method for
the diagnosis of tumors (10).
Vertebral tumors can be diagnosed with CT examination by the
discovery of calcified lesions (11).
The imaging of spinal tumors with MRI examination is characterized
by clear lesion site and the generation of ‘salt and pepper’ sign.
In addition to displaying the change in morphology of the tumors,
it can also reflect the change in signal strength of the lesion,
thus effectively improving the accuracy of diagnosis (12).
With the continuous development of imaging
diagnosis, CT and MRI techniques have been commonly used in the
diagnosis of skeletal diseases, and the early diagnosis of bone
tumors and the confirmation of benign lesions are improved. Imaging
diagnosis can be used to know the extent of the lesion, and
understand whether the surrounding tissues are changed, which is of
great significance for clinical diagnosis and treatment (13). The results of this study showed that
Sen, Acc and PV− of the three examination methods had no
obvious differences in the diagnosis of spinal osseous tumors. MRI
examination showed the highest Sen (P<0.05). Spe and
PV+ of the three examination methods had no obvious
differences (P>0.05). This is because the displaying of soft
tissue mass of spinal osseous tumors on the X-ray plain film is
sometimes unobvious even though X-ray examination is easy to be
performed with strong integrity (14). However, CT examination is more
sensitive to the resolution of calcified lesions, especially
lobular calcified lesions. For example, chondrosarcoma often occurs
in the sacrococcygeal vertebra and the thoracic vertebra, and the
soft-tissue mass will be ring-arc shaped, and represented as
osteolytic destruction, which can be displayed clearly by enhanced
CT scan (15). With the progress of
the disease, osteolytic destruction is aggravated, the tumor shows
invasive growth, and the blood supply in the center of the mass is
insufficient. Upon MRI examination, the distribution of density and
signal of the tumor is not uniform, most of T1WI show relatively
low signal, while T2WI shows relatively high mixed signals.
Moreover, MRI has the advantages of direct multi-plane imaging and
high resolution. It is more accurate than X-ray plain film and CT
scan in displaying tumors inside and outside the spine (16).
The results of this study showed that MRI and CT had
no obvious difference in diagnosing primary spinal osseous tumors
(P>0.05), and they had relatively high consistency in diagnosing
primary spinal osseous tumors (κ=0.72); CT and X-ray film had
obvious difference in diagnosing primary spinal osseous tumors
(P<0.05), and they had relatively low consistency in diagnosing
primary spinal osseous tumors (κ=0.47); MRI and X-ray film had
obvious difference in diagnosing primary spinal osseous tumors
(P<0.05), and they had relatively low consistency in diagnosing
primary spinal osseous tumors (κ=0.41). This is because X-ray plain
film mainly relies on the display of change in bone mineral density
to diagnose bone tumors, while it has relatively low sensitivity in
diagnosing tumors such as hemangioma and chondrosarcoma. CT scan
has the advantages of rapid scanning speed and clear images. With
the rapid development of medical imaging technology, CT scan has
grown from the past 4 rows to 8, 16 and 64 rows, and even higher
(17). Multi-row CT scan reduces the
scanning time, and its interference by the motion artifact is
reduced. Moreover, Z-axis resolution is higher, which is conducive
to showing tiny lesions clearly, thus realizing early detection of
primary spinal osseous tumors, and effectively avoiding the
shortcomings of X-ray plain film. However, CT scan still has some
defects. For example, it is not sensitive to the micro-periosteal
reaction of the spinal osseous tumors, which causes missed
diagnosis or misdiagnosis. In addition, the radiation generated
during examination is harmful to the patient, and frequent
examinations in a short term are not appropriate (18). MRI is an imaging technology developed
on the basis of magnetic resonance phenomenon. It is a
non-radioactive examination with the advantages of high spatial
resolution and multi-directional and multi-sequential imaging. It
has relatively high sensitivity for the examination in a local
range, and can determine the scope of the lesions in the parts
involved by the tumors. Furthermore, it has relatively high
resolution for tissues, and is more sensitive for displaying the
change in osteogenesis of osteoblastoma (19). The scope of the lesion in the spinal
cord can be shown effectively and the anatomical structure of the
bone with tumor can be reflected clearly through T1WI sequence
examination. The correlation of the lesion with blood vessels,
nerves and muscles at the adjacent vertebral segment can be shown
through T2WI sequence examination, thus effectively judging the
violation of the lesion on the surrounding soft tissues. Therefore,
MRI examination has relatively high consistency with pathological
examination (20).
In conclusion, X-ray, CT and MRI examinations have
their own advantages in diagnosing primary spinal osseous tumors.
Comparatively speaking, CT and MRI examinations have higher
accuracy, and they are more conducive to improving the accuracy in
the diagnosis of primary spinal osseous tumors. Thus, they have
higher clinical values.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LY contributed to the planning and implementation of
the experiments. SZ and RG wrote the manuscript and analyzed
general patient data. SZ was responsible for X-ray examination. MW
and LY helped with CT examination. CP contributed to MRI
examination. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Nankai Hospital (Tianjin, China). Signed written informed consents
were obtained from the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Guzik G: Current incidence of different
morphological types of malignant metastases to the spine based on
magnetic resonance imaging. Ortop Traumatol Rehabil. 19:137–144.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gupta PK, Misra S, Verma R, Soni N, Lamin
JC, Mishra RK, Behari S and Kumar S: Primary intradural cervical
spine melanocytoma: A rare tumor and review of literature. Neurol
India. 65:653–657. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yang P, Lin J, Liu H, Shen H and Yang HL:
Primary bone mantle cell lymphomas with multiple vertebral
compression fractures: A case report. Oncol Lett. 13:1288–1292.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Konovalov NA, Nazarenko AG, Asyutin DS,
Onoprienko RA, Korolishin VA, Cherkiev IU, Martynova MA, Zakirov
BA, Timonin SY and Kosyr'kova AV: The use of intraoperative
neuroimaging tools and a navigation system in surgical treatment of
primary and metastatic tumors of the spine. Vopr Neirokhir.
80:5–14. 2016.(In Russian). View Article : Google Scholar
|
|
5
|
Zhou Z, Wang X, Wu Z, Huang W and Xiao J:
Epidemiological characteristics of primary spinal osseous tumors in
Eastern China. World J Surg Oncol. 15:732017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tomasian A, Wallace A, Northrup B, Hillen
TJ and Jennings JW: Spine cryoablation: Pain palliation and local
tumor control for vertebral metastases. AJNR Am J Neuroradiol.
37:189–195. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Welte SE, Wiskemann J,
Scharhag-Rosenberger F, Förster R, Bostel T, Bruckner T, Schlampp
I, Meyerhof E, Sprave T, Nicolay NH, et al: Differentiated
resistance training of the paravertebral muscles in patients with
unstable spinal bone metastasis under concomitant radiotherapy:
Study protocol for a randomized pilot trial. Trials. 18:1552017.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sciubba DM, De la Garza Ramos R, Goodwin
CR, Xu R, Bydon A, Witham TF, Gokaslan ZL and Wolinsky JP: Total en
bloc spondylectomy for locally aggressive and primary malignant
tumors of the lumbar spine. Eur Spine J. 25:4080–4087. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Boriani S, Gasbarrini A, Bandiera S,
Ghermandi R and Lador R: Predictors for surgical complications of
en bloc resections in the spine: Review of 220 cases treated by the
same team. Eur Spine J. 25:3932–3941. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kumar N, Zaw AS, Khoo BL, Nandi S, Lai Z,
Singh G, Lim CT and Thiery JP: Intraoperative cell salvage in
metastatic spine tumour surgery reduces potential for reinfusion of
viable cancer cells. Eur Spine J. 25:4008–4015. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tamam MÖ, Tamam C, Yıldırım D, Mülazımoğlu
M and Kamalı G: Intramedullary spinal cord metastasis from
malignant mesenchymal tumor: Detection with FDG-PET/CT. Mol Imaging
Radionucl Ther. 24 Suppl 1:22–24. 2015. View Article : Google Scholar
|
|
12
|
Monserrate A, Zussman B, Ozpinar A,
Niranjan A, Flickinger JC and Gerszten PC: Stereotactic
radiosurgery for intradural spine tumors using cone-beam CT image
guidance. Neurosurg Focus. 42:E112017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Klinaki I, Al-Nahhas A, Soneji N and Win
Z: 68Ga DOTATATE PET/CT uptake in spinal lesions and MRI
correlation on a patient with neuroendocrine tumor: Potential
pitfalls. Clin Nucl Med. 38:e449–e453. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kobayashi K, Imagama S, Ando K, Hida T,
Ito K, Tsushima M, Ishikawa Y, Matsumoto A, Morozumi M, Tanaka S,
et al: Contrast MRI findings for spinal schwannoma as predictors of
tumor proliferation and motor status. Spine. 42:E150–E155. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mechl M, Šprláková-Puková A and Keřkovský
M: CT and MRI of spinal tumors - Review and differential diagnosis
of most common abnormalities. Cesk Radiol. 66:369–378. 2012.
|
|
16
|
Tarnoki DL, Tarnoki AD, Ohlmann-Knafo S
and Pickuth D: Pattern of tumour spread of common primary tumours
as seen on magnetic resonance imaging. Pathol Oncol Res. 22:79–85.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chou CT, Chen RC, Lin WC, Ko CJ, Chen CB
and Chen YL: Prediction of microvascular invasion of hepatocellular
carcinoma: Preoperative CT and histopathologic correlation. AJR Am
J Roentgenol. 203:W253–W259. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sahinarslan A, Erbas G, Kocaman SA, Bas D,
Akyel A, Karaer D, Ergun MA, Arac M and Boyaci B: Comparison of
radiation-induced damage between CT angiography and conventional
coronary angiography. Acta Cardiol. 68:291–297. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ganten MK, Schuessler M, Bäuerle T,
Muenter M, Schlemmer HP, Jensen A, Brand K, Dueck M, Dinkel J,
Kopp-Schneider A, et al: The role of perfusion effects in
monitoring of chemoradiotherapy of rectal carcinoma using
diffusion-weighted imaging. Cancer Imaging. 13:548–556. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
D'Andrea K, Dreyer J and Fahim DK: Utility
of preoperative magnetic resonance imaging coregistered with
intraoperative computed tomographic scan for the resection of
complex tumors of the spine. World Neurosurg. 84:1804–1815. 2015.
View Article : Google Scholar : PubMed/NCBI
|