Introduction
Primary and metastatic malignancies can occur in the
carinal region, leading to carinal stenosis (1,2). The
majority of patients with malignant carinal stenosis are diagnosed
in the advanced stages of the disease and cannot undergo surgical
resection (3). In these cases,
bronchoscopic interventions including stent placements may be the
only palliative option for maintaining lumen patency (4). Bronchoscopic interventions are
advantageous as they are less invasive and may be suitable for
critically ill patients (5).
Malignant carinal stenosis can occasionally be accompanied by
airway distortion, making stent selection and placement difficult.
Y-shaped silicon stents are traditionally used to treat malignant
carinal stenosis (6,7). However, their disadvantages include
poor shape-adaptability, difficult placement and secretion
retention (8,9). In addition, when one of the main
bronchi is completely obstructed and cannot be recanalized, or its
distal lung tissue has lost function, inserting a Y-shaped stent is
not possible (4). Micro-Tech stents
(Micro-Tech Co., Ltd., Nanjing, China) are self-expanding metal
stents available in different shapes and are individually
customizable. The current study described the use of Micro-Tech
stents in malignant carinal stenosis. To the best of our knowledge,
this is the first study to evaluate the feasibility of using the
bare cone-shaped metal stent to treat malignant carinal stenosis
for which Y-shaped stents are not suitable.
Materials and methods
Patients
A total of 47 patients (38 males and 9 females;
median age, 59 years; age range, 23–83 years) with malignant
carinal stenosis who underwent Micro-Tech stent placement in
Beijing Tian Tan Hospital (Beijing, China) between January 2004 and
October 2017 were enrolled. All patients could not undergo surgical
treatment due to advanced disease stage and 13 of them experienced
postoperative tumor recurrence. Data including patient
demographics, medical histories, interventional therapies
administered before stenting, complications during stenting and
outcomes following stenting were analyzed retrospectively. The
current study was approved by The Ethical Review Committee of
Beijing Tiantan Hospital, Capital Medical University (approval ID:
JS2013-007-02). All patients signed an informed consent form before
the insertion of the Micro-Tech stent.
Preparation prior to stenting
Prior to stent placement, patients underwent
examinations including electrocardiograms and blood tests including
routine blood counts, coagulation tests, liver and kidney function
tests and electrolyte levels. Computed tomography scans of the
chest, including coronal and sagittal reconstruction, and
bronchoscopy were performed to assess the extent, type and degree
of stenosis, which provided a reliable basis for stent selection
and size customization (10,11). Preoperative and preanesthetic
evaluations were conducted by interventional pulmonologists and
anesthetists, respectively. During the stent placements, dynamic
electrocardiograms, blood pressure and oxygen saturation levels
(SaO2) were monitored. If general anesthesia was
administered, arterial blood gases were also analyzed.
Stent selection and deployment
Uncovered Y-shaped and cone-shaped Micro-Tech stents
were used in the current study. The stents and stent delivery
systems were manufactured by Micro-Tech Co. Ltd.
Y-shaped stents
The Y-shaped stent has three bifurcations comprising
one tracheal and two bronchial limbs. The length and diameter of
the limbs and the angle between the two bronchial limbs can be
individually customized in various combinations. The tracheal limb
lengths of the Y-shaped stents used in the current study ranged
between 30 and 60 mm, and the diameters ranged between 14 and 20
mm. The bronchial limb lengths ranged between 10 and 45 mm, and
diameters ranged between 8 and 14 mm. The angles between the two
bronchial limbs ranged between 60 and 90°. The Y-shaped stent was
preferred when the two sides of the main bronchus remained
functional despite carinal involvement causing lower tracheal and
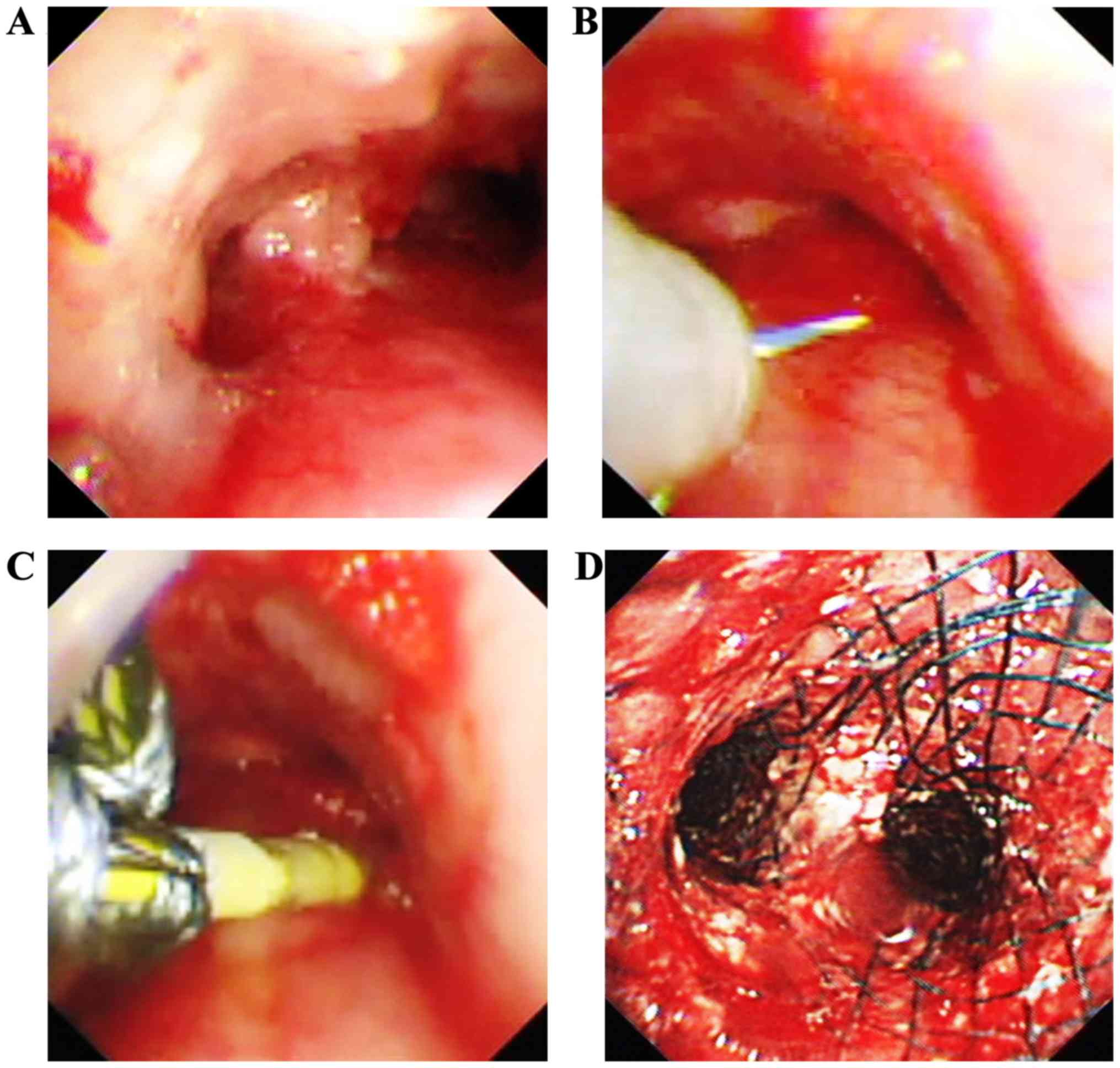
bilateral proximal main bronchial obstruction (Fig. 1A).
The Y-shaped stent was loaded into an introducer
sheath. Prior to stent placement, a rigid bronchoscope (RB) was
inserted. Through the RB, a 0.035-inch guide wire (Boston
Scientific Corporation, Marlborough, MA, USA) was inserted in the
left or right main bronchus using a bronchoscope. The bronchoscope
was subsequently withdrawn and the delivery system was advanced
into the carina with the corresponding bronchial limb of the stent
passing over the guide wire (Fig.
1B). The bronchial limbs were exposed following initial
retraction of the introducer sheath. Under direct visualization
through an ultra-thin flexible bronchoscope (outer diameter, 2.8
mm), the stent bronchial limbs bound by threads were inserted into
the relevant main bronchus (Fig.
1C). The bronchial limbs were released by pulling the threads
through the ring-pull in the delivery system. The tracheal limb was
released by further withdrawal of the introducer sheath, thus
completing the stent placement (Fig.
1D). The Y-shaped stent can also be inserted orally. With the
patients under total intravenous anesthesia and remaining
spontaneous respiration, both the guide wire and delivery system
were inserted orally. The release process of the stent was the same
as aforementioned. In the present study, 12 out of 28 Y-shaped
stents were inserted orally.
Cone-shaped stents
The cone-shaped stent is a special straight stent
constructed according to the authors' specifications. The opposite
ends of the stent have different diameters, allowing a smooth
transition between the large and small ends. The proximal
(tracheal) end should be positioned in the trachea while the distal
(bronchial) end should be positioned in the main bronchus, thus
maintaining tracheal-unilateral main bronchus patency. The diameter
of the two ends and the length of the stent can be individually
customized. The lengths of the cone-shaped stent used in this study
ranged between 50 and 80 mm. The stent diameters ranged between 10
and 18 mm, and the difference between the diameters of the two ends
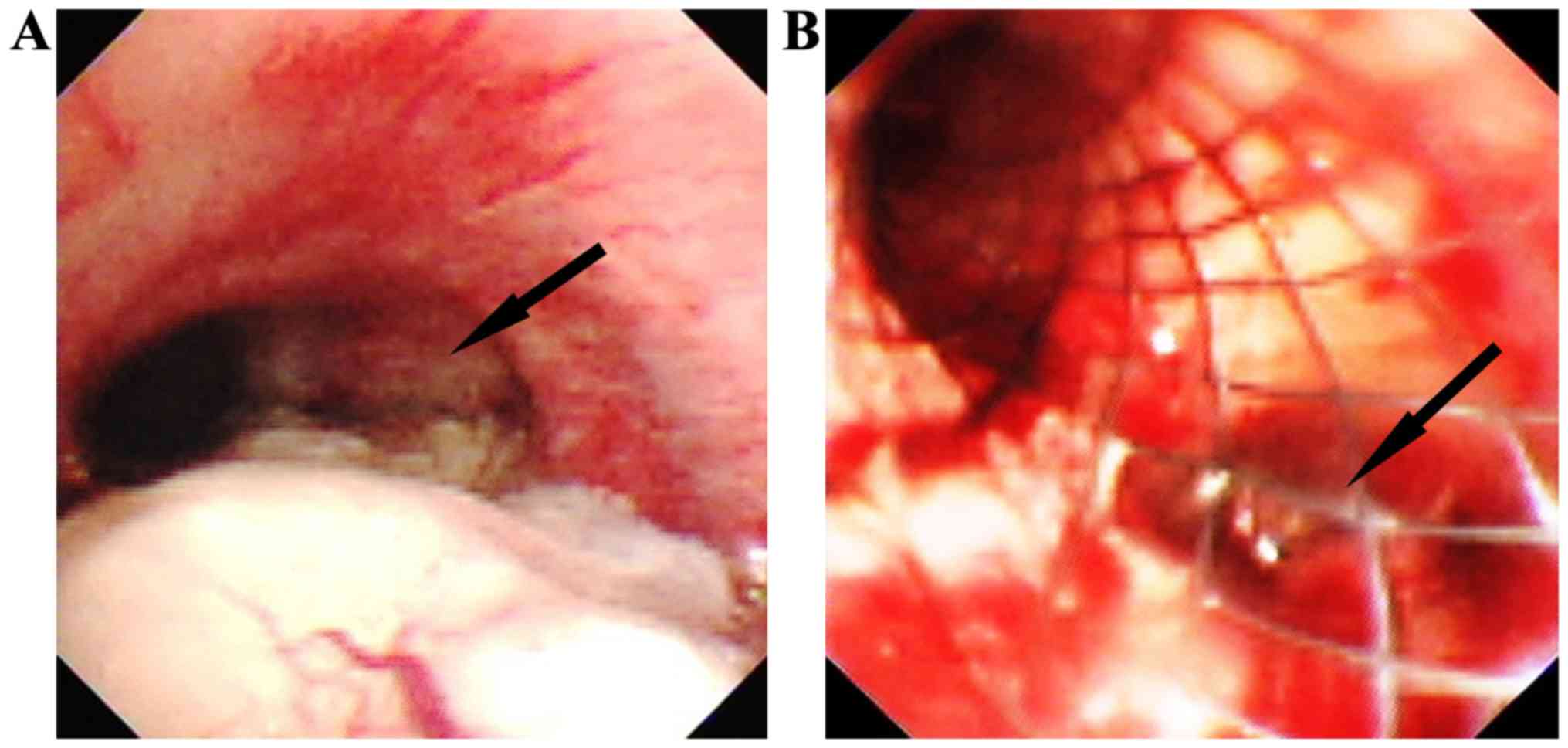
varied between 2 and 8 mm. Once placed in trachea-left (or right)
main bronchus, the stent blocked the opening of the other main
bronchus (Fig. 2B). Although airflow
could pass through the stent mesh, further bronchoscopic
interventions would not be possible. Only when a unilateral main
bronchus is obstructed and cannot be recanalized (Fig. 2A), or its distal lung tissue is
nonfunctional, can a cone-shaped stent insertion be considered
(4).
Cone-shaped stent insertions are simple and almost
identical to the process for traditional straight Micro-Tech
stents. Prior to stent insertion, the depth of the delivery system
to be inserted into the airway was measured with a bronchoscope.
The distance from the distal end of the bronchoscope to the
proximal end of the airway was measured. A guide wire was
subsequently inserted into the functional main bronchus through the
working channel of the bronchoscope. Following removal of the
bronchoscope, the delivery system was inserted into the airway,
passing over the guide wire until it reached the measured depth.
The stent was then released by withdrawing the introducer sheath.
Following the release of the stent, the bronchoscope was
re-inserted to confirm proper stent placement and expansion. If
necessary, biopsy forceps could be used to adjust the stent.
Efficacy evaluation
Procedural efficacy was evaluated according to
respiratory symptom improvement and according to the differences in
the American Thoracic Society Dyspnea Index (12) and Karnofsky score (13) prior to and following stent
placement.
Follow-up
Patients underwent bronchoscopy within one week
following stenting to assess early complications (≤1 week).
Bronchoscopy was subsequently performed every 1–3 months, or for
worsening dyspnea, and late complications (>1 week) were
recorded. When necessary, bronchoscopic interventions were
performed. The follow-up ended upon the start of this study
(January 2018), at the patient's last visit to our hospital, or
upon the patient's mortality.
Statistical analysis
Statistical data analysis was performed using SPSS
version 22.0 (IBM Corp., Armok, NY, USA). The American Thoracic
Society Dyspnea Index and Karnofsky score data are expressed as the
mean ± standard deviation. Comparisons of the American Thoracic
Society Dyspnea Index and Karnofsky score before and following
stent placement were made using paired-sample t-tests. P<0.05
was considered to indicate a statistically significant
difference.
Results
Characteristics of the patients
Forty-seven patients (38 males and 9 females) with a
median age of 59 years (ranging between 23 and 83 years) were
enrolled. The patients' symptoms included dyspnea (93.6%; 44/47),
cough (78.7%; 37/47), hemoptysis (48.9%; 23/47), dysphagia (6.4%;
3/47), chest pain (4.3%; 2/47), hoarseness (4.3%; 2/47) and stridor
(2.1%; 1/47). Of all the patients, 27.7% (13/47) had atelectasis
and 19.1% (9/47) had obstructive pneumonia. The lesion etiologies
included primary (87.2%; 41/47) and metastatic (12.8%; 6/47)
malignancies (Table I). Squamous
cell and esophageal carcinomas were the most common primary and
metastatic tumors, respectively. Twenty-nine patients had treatment
histories that included surgery (44.8%; 13/29), chemotherapy
(51.7%; 15/29), bronchoscopic intervention (31.0%; 9/29) and
radiotherapy (44.8%; 13/29). Prior to stent placement, 34 patients
underwent bronchoscopic interventions including argon plasma
coagulation (47.1%; 16/34), carbon dioxide (CO2)
cryotherapy (23.5%; 8/34), high-frequency electric knife (67.6%;
23/34), snare (17.6%; 6/34), balloon dilatation (5.9%; 2/34) and
laser therapy (17.6%; 6/34) to reduce airway obstruction.
 | Table I.Lesion etiology. |
Table I.
Lesion etiology.
| A, Primary
tumors |
|---|
|
|---|
| Lesion
etiology | n (patients) | % of 47
patients |
|---|
| Squamous cell
carcinoma | 26 | 55.3 |
| Adenocarcinoma | 7 | 14.9 |
| Adenoid cystic
carcinoma | 5 | 10.6 |
| Mucoepidermoid
carcinoma | 2 | 4.3 |
| Undifferentiated
carcinoma | 1 | 2.1 |
|
| B, Metastatic
tumors |
|
| Lesion
etiology | n
(patients) | % of 47
patients |
|
| Esophageal
cancer | 4 | 8.5 |
| Malignant
lymphoma | 1 | 2.1 |
| Liver cancer | 1 | 2.1 |
Anesthesia and ventilation
methods
Anesthesia and ventilation methods during stent
placement are presented in Table
II. In 12.5% (1/8) of the patients with an endotracheal tube
(ETT), part of the cone-shaped stent entered into the ETT following
release. When withdrawing the ETT, the stent migrated and required
removal. Ultimately, the stent was successfully reinserted through
a laryngeal mask (LAM). Obvious CO2 retention occurred
in 26.3% (5/19) of patients in whom an RB was used. Following stent
placement, RBs were replaced with LAMs to promote CO2
removal. Among patients with spontaneous ventilation under total
intravenous anesthesia (TIVA-SV), 8.3% (1/12) experienced a
decrease in SaO2 due to glossoptosis and nasopharyngeal
airways were required.
 | Table II.Anesthesia and ventilation
methods. |
Table II.
Anesthesia and ventilation
methods.
|
| n (cone-shaped
stent, Y-shaped stent) |
|---|
|
|
|
|---|
| Type of
anesthesia | LAM | ETT | RB | Tubeless |
|---|
| General
anesthesia | 8 (8,0) | 7 (7,0) | 19 (3,16) | 0 (0,0) |
| Local anesthesia +
conscious sedation | 0 (0,0) | 1 (1,0) | 0 (0,0) | 0 (0,0) |
| TIVA-SV | 0 (0,0) | 0 (0,0) | 0 (0,0) | 12 (0,12) |
Outcomes
Forty-seven bare stents including 28 Y-shaped and 19
cone-shaped stents were successfully inserted in all 47 patients.
Reversible bleeding (19.1%; 9/47) and glottic edema (4.3%; 2/47)
were the most common procedure-associated complications. No serious
complications were observed.
Intervention efficacy
All patients achieved immediate symptomatic
improvement, especially in dyspnea (100%; 44/44), cough (81.1%;
30/37) and stridor (100%; 1/1). The Karnofsky scores were
significantly increased from 62.77±12.105 to 80.64±8.445
(t=−17.769; P<0.001) and the American Thoracic Society Dyspnea
Index scores were significantly decreased from 3.06±0.895 to
1.60±0.712 (t=16.224; P<0.001).
Follow-up
A total of 42 patients were assessed for early
complications (Table III). Mucosal
necrosis was the most common early complication and was removed
using biopsy forceps. The early occurrence of granulation tissue
was mild and did not cause airway obstruction. One cone-shaped
stent migrated distally and was adjusted successfully using biopsy
forceps.
 | Table III.Early complications. |
Table III.
Early complications.
| Complication | Cone-shaped stent n
(% of 17 stents) | Y-shaped stent n (%
of 25 stents) | n (% of 42
stents) |
|---|
| Mucosal
necrosis | 11 (64.7) | 19 (76.0) | 30 (71.4) |
| Increased
secretions | 10 (58.8) | 18 (72.0) | 28 (66.7) |
| Granulation
tissue | 1 (5.9) | 1 (4.0) | 2 (4.8) |
| Mucositis | 0 (0.0) | 2 (8.0) | 2 (4.8) |
| Glottis edema | 0 (0.0) | 1 (4.0) | 1 (2.4) |
| Migration | 1 (5.9) | 0 (0.0) | 1 (2.4) |
| Bleeding | 1 (5.9) | 0 (0.0) | 1 (2.4) |
Twenty patients were followed-up long-term, with a
median length of 116 days (range, 16–1,537 days). Among the late
complications (Table IV), three
Y-shaped stents fractured and the duration of time prior to the
fractures was 32, 93 and 497 days, respectively. Despite fracture,
two out of the three stents did not compromise airway support. No
migrations, perforations, fistulas or stent-associated mortalities
were observed. Thirteen of the 20 patients underwent at least one
(range, 1–6) bronchoscopic intervention due to aggravation of
dyspnea caused by tumor overgrowth or stent-associated
complications. Following each interventional treatment, dyspnea was
improved to varying degrees. Following a median time of 88 days
(range, 35–388 days), initial bronchoscopic interventions were
performed due to tumor overgrowth (84.6%; 11/13), stent fracture
(7.7%; 1/13) and granulation tissue (7.7%; 1/13; data not shown).
Restenting was performed in two patients as stenosis progressed
over the existing stent (n=1) and a fractured stent led to
compromised airway support (n=1). Eighty-eight days following
insertion, a Y-shaped stent removal was attempted in a patient with
malignant lymphoma as the stenosis improved following
tumor-specific chemotherapy. As the stent was partly embedded in
the airway mucosa, the removal attempt failed.
 | Table IV.Late complications. |
Table IV.
Late complications.
| Complication | Cone-shaped stent n
(% of 7 stents) | Y-shaped stent n (%
of 13 stents) | n (% of 20
stents) |
|---|
| Tumor
overgrowth | 7 (100.0) | 9 (69.2) | 16 (80.0) |
| Phlegm
retention | 4 (57.1) | 5 (38.5) | 9 (45.0) |
| Granulation
tissue | 2 (28.6) | 6 (46.2) | 8 (40.0) |
| Fracture | 0 (0.0) | 3 (23.1) | 3 (15.0) |
| Bleeding | 1 (14.3) | 1 (7.7) | 2 (10.0) |
| Scarring | 0 (0.0) | 1 (7.7) | 1 (5.0) |
|
Epithelialization | 0 (0.0) | 1 (7.7) | 1 (5.0) |
Discussion
At present, treatments for malignant carinal
stenosis are challenging (14–16).
Various malignances can occur in the carinal region including the
lower trachea and the proximal end of the bilateral main bronchus
(1). Dyspnea, cough and hemoptysis
are commonbut nonspecific respiratory symptoms (17). Since the majority of patients are
already in the advanced stages of the disease at the time of
diagnosis, only a number of patients have the opportunity for
surgical treatment (3). Carinal
surgery is technically difficult and often accompanied by high
morbidity and mortality rates (18–20). It
is reported that mortality rates following carinal resection and
reconstruction range from 29–40% (3)
and surgery may be avoided at the expense of an improved prognosis
(14). Yamamoto et al
(14) recommended that if possible,
surgery should still be performed in selected patients. A study by
Shin et al (3) included 30
patients with locally advanced non-small cell lung cancer involving
the carinal and/or trachea underwent carinal resection and
reconstruction. The surgical candidacy was evaluated according to
guidelines based on pulmonary function, general conditions and
co-morbidity of the patient, as well as the extent of the tumor
invasion, nodal stage and alternative non-surgical modalities. For
patients who cannot be treated surgically, bronchoscopic
intervention is an alternative palliative treatment that can
effectively remove intraluminal tumors (21,22).
When the structure of the airway wall is destroyed by tumor
infiltration, or stenosis is caused by compression from an external
mass or lymph node, stent insertion should be considered (23). In the current study, certain patients
could not undergo surgical treatment due to advanced disease stage
or tumor recurrence following surgery. Although the majority of
patients (72.3%) underwent bronchoscopic intervention prior to
stent placement, stent insertion was still required due to mixed
obstructions.
Y-shaped stents are used to maintain patency of the
lower trachea and the proximal end of the bilateral main bronchus.
Y-shaped silicone stents are traditionally used and have favorable
safety and tolerance profiles (6,7).
However, they are difficult to insert, especially for complex
carinal stenosis with distorted airways. Once deployed, they can
interfere with mucociliary clearance, resulting in secretion
retention (23). Compared to
silicone stents, self-expanding Y-shaped metal stents are
relatively easy to insert and have improved expansion force
(16). Following insertion, they can
gradually expand to a predetermined shape that matches the contour
of the tracheobronchial tree and requires less routing care
(8). Studies on the treatment of
malignant carinal stenosis with Y-shaped metal stents have been
reported (15,24–26).
Madan et al (15) reported
one of the largest studies on Y-shaped metal stents. The authors
used the fully covered metal Y-shaped stent, which has the
advantage of preventing tumor ingrowth. In the present study, the
Y-shaped stents used were uncovered. The advantage of the uncovered
stent is that it does not easily migrate and has little effect on
mucociliary clearance (23). The
efficacy and safety of Y-shaped covered stents and Y-shaped
uncovered stents requires further comparison. In certain patients
with long segments of tracheal obstruction in addition to carinal
stenosis, combination airway stenting using tracheal and Y-shaped
stents may be required (27).
Malignant carinal stenosis can occasionally be
accompanied by loss of function of one of the main bronchi, making
insertion of a Y-shaped stent infeasible (4). In the current study, the most common
reasons for loss of function of a main bronchus are complete
luminal obstruction that precludes recanalization, or surgical
removal of the distal lung tissue. The current study demonstrated
the feasibility of inserting cone-shaped stents to maintain
tracheal and unilateral main bronchus patency in malignant carinal
stenosis.
Compared with silicone stent, inserting a Micro-Tech
stent is relatively easy (28). In
the current study, all stents were successfully inserted without
serious procedure-associated complications and immediate and
satisfactory effects were achieved. The choice of anesthesia and
ventilation methods during stent insertion should depend on the
stent type, location of lesions and severity of airway lesions
(29). In the current study, the
majority of stents were inserted through an artificial airway with
the patient under general anesthesia for the following reasons: i)
Patients were unable to tolerate local anesthesia due to severe
airway obstruction; ii) bronchoscopic intervention was performed to
remove intraluminal masses before stenting, and the operation time
was lengthy; iii) procedure-associated complications could occur
and would need to be managed; and iv) patients required general
anesthesia due to discomfort with local anesthesia. ETTs can
provide safe and reliable ventilation access, but they occupy part
of the airway space and are not conducive to stent release in the
upper and middle trachea (29). LAM
is a supraglottic airway device and provides excellent visibility
of the glottis and subglottis; thus, it could be regarded as a
reliable alternative for airway management during interventional
bronchoscopic procedures, particularly when they are located near
the glottis or in the upper trachea (30). When using an RB, the presence of
mobile teeth and the extent of neck mobility should be considered
(29). In addition, high-frequency
ventilation through RBs reduces exhalation time and may lead to
CO2 retention (31).
TIVA-SV is an alternative anesthetic method (32). In this current study, the insertion
of the Y-shaped stent with the patients under TIVA-SV was always
successful.
In the current study, complications following stent
placement could be effectively managed endoscopically when
necessary. Mucosal necrosis was the most common early complication.
This was usually observed in the areas of airway lesions or at the
ends of the stent. This may be due to the greater contact pressure
between the mucosa and the stent in these areas. Stent migration
was only observed as an early complication as opposed to a late
complication. Following long-term implantation, stents were
embedded in the malignant or granulation tissues, or
epithelialization occurred. These were also the reasons why metal
stents were difficult to remove. Metal stents can fracture
following placement, and the free stent wire could protrude into
the bronchial lumen or damage the surrounding tissue. In addition,
the fractured stent may lose the ability to support the airway and
should be replaced with a new one or covered by inserting a new
stent over the fracture (33). Tumor
overgrowth was the most common reason for repeated bronchoscopic
interventions following stent insertion (34). When the disease progresses and the
stenosis is beyond the scope of the original stent, restenting
remains an effective treatment method (33).
Removal of metal stents is challenging; potential
risks include stent fracture, mucosal tear, hemorrhage, restenosis,
pneumothorax and mortality (35).
The longer the stent is present in the airway, the more difficult
it is to remove (36). Due to the
limited survival rate of patients with malignant carinal stenosis,
few stent removals are considered. The main indication for stent
removal is disease improvement (37)
or severe stent-associated complications (38). In the current study, a patient with
malignant lymphoma exhibited disease improvement following
tumor-specific chemotherapy, and stent removal was attempted but
failed. Therefore, if possible, removable stents may be more
appropriate for patients with untreated malignancies that are
sensitive to radiotherapy and chemotherapy (9,39).
This study had a number of limitations. First, the
details of anesthesia and airway management performed by the
anesthetist were not presented as they were unavailable. Second,
the patients attended follow-up unequally. In this study, the
majority of patients were referred from other hospitals and
eventually lost to follow-up. Therefore, patients' survival time
was rarely recorded. Previous studies have indicated that the
median survival time of patients with malignant carinal stenosis
following stenting varied between 46 and 181 days, and even if
patients with malignant carinal stenosis receive bronchoscopic
interventions including stenting, their prognosis remains poor
(2,7,16).
In conclusion, the current study initially described
the insertion of uncovered cone-shaped stents and demonstrated the
feasibility of their use for maintaining tracheal-unilateral main
bronchus patency in malignant carinal stenosis. The uncovered
Micro-Tech stent placement (including Y-shaped and cone-shaped
types) is a safe and effective palliative treatment for patients
with malignant carinal stenosis.
Acknowledgements
The authors thank Dr Min Xu and Dr Chen-Yang Zhang
(both from the Department of Respiration, Beijing Tian Tan
Hospital, Capital Medical University, Beijing, China) for their
assistance in collecting data.
Funding
This study was supported by the Capital Health
Development Research Project (grant no. 2016-2-2048).
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JZ and JMN designed the study. JMN collected and
analyzed the data, and drafted the manuscript. JZ, XJQ, JW, YHP,
YLW, and TW performed the stent placements or bronchoscopic
interventions, and revised the manuscript. All authors have read
and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethical Review
Committee of Beijing Tiantan Hospital, Capital Medical University
(Beijing, China; approval ID: JS2013-007-02). All patients signed
an informed consent form before the insertion of the Micro-Tech
stent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Puchalski J and Musani AI:
Tracheobronchial stenosis: Causes and advances in management. Clin
Chest Med. 34:557–567. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tsukioka T, Takahama M, Nakajima R, Kimura
M, Tei K and Yamamoto R: Sequential stenting for extensive
malignant airway stenosis. Ann Thorac Cardiovasc Surg. 21:114–118.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shin S, Park JS, Shim YM, Kim HJ and Kim
J: Carinal resection and reconstruction in thoracic malignancies. J
Surg Oncol. 110:239–244. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fiorelli A, Caterino U, Raucci A and
Santini M: A conical self-expanding metallic stent for the
management of critical complex tracheobronchial malignant stenosis.
Interact Cardiovasc Thorac Surg. 24:293–295. 2017.PubMed/NCBI
|
|
5
|
Takeda T, Itano H, Fukita S, Saitoh M and
Takeda S: Bilateral self-expandable metallic stents for lung cancer
involving the carina. Respirol Case Rep. 1:48–51. 2013.PubMed/NCBI
|
|
6
|
Sehgal IS, Dhooria S, Madan K,
Pattabhiraman V, Mehta R, Goyal R, Akkaraju J and Agarwal R:
Placement of tracheobronchial silicone Y-stents: Multicenter
experience and systematic review of the literature. Lung India.
34:311–317. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dutau H, Toutblanc B, Lamb C and Seijo L:
Use of the dumon Y-stent in the management of malignant disease
involving the carina: A retrospective review of 86 patients. Chest.
126:951–958. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yang RM, Han XW, Wu G, Li YD and Li FB:
Implantation of a self-expandable metallic inverted Y-stent to
treat tracheobronchial stenosis in the carinal region: Initial
clinical experience. Clin Radiol. 62:1223–1228. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ayub A, Al-Ayoubi AM and Bhora FY: Stents
for airway strictures: Selection and results. J Thorac Dis. 9 Suppl
2:S116–S121. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Righini C, Aniwidyaningsih W, Ferretti G,
Pra Y, Raymond CS, Ferretti K, Hustache C, Diab S, Reyt E and Pison
CM: Computed tomography measurements for airway stent insertion in
malignant airway obstruction. J Bronchology Interv Pulmonol.
17:22–28. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Williams JM, Krebs IA, Riedesel EA and
Zhao Q: Comparison of fluoroscopy and computed tomography for
tracheal lumen diameter measurement and determination of
intraluminal stent size in healthy dogs. Vet Radiol Ultrasound.
57:269–275. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ernst A, Feller-Kopman D, Becker HD and
Mehta AC: Central airway obstruction. Am J Respir Crit Care Med.
169:1278–1297. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen H, Zhang J, Qiu XJ, Wang J, Pei YH
and Wang YL: Interventional bronchoscopic therapy in adult patients
with tracheobronchial mucoepidermoid carcinoma. Chin Med J (Engl).
130:2453–2458. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yamamoto K, Kosaba S, Ikeda T and Tokuyasu
H: Evaluation of therapeutic method for malignant tumors involving
the tracheal carina. Kyobu Geka. 54:581–584. 2001.(In Japanese).
PubMed/NCBI
|
|
15
|
Madan K, Dhooria S, Sehgal IS, Mohan A,
Mehta R, Pattabhiraman V, Goyal R and Agarwal R: A multicenter
experience with the placement of self-expanding metallic
tracheobronchial Y stents. J Bronchology Interv Pulmonol. 23:29–38.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Qiao Y, Fu YF, Cheng L, Niu S and Cao C:
Placement of integrated self-expanding Y-shaped airway stent in
management of carinal stenosis. Radiol Med. 121:744–750. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mudambi L, Miller R and Eapen GA:
Malignant central airway obstruction. J Thorac Dis. 9 Suppl
10:S1087–S1110. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Parissis H and Young V: Carinal surgery:
Experience of a single center and review of the current literature.
J Cardiothorac Surg. 5:512010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yamamoto K, Miyamoto Y, Ohsumi A, Imanishi
N and Kojima F: Surgical results of carinal reconstruction: An
alterative technique for tumors involving the tracheal carina. Ann
Thorac Surg. 84:216–220. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Maniwa Y: Surgical treatment of airway
disease. J Thorac Dis. 8:E78–E82. 2016.PubMed/NCBI
|
|
21
|
Chen CH, Wu BR, Cheng WC, Chen CY, Chen
WC, Hsia TC, Liao WC, Tu CY and Hsu WH: Interventional pulmonology
for patients with central airway obstruction: An 8-year
institutional experience. Medicine (Baltimore). 96:e56122017.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jeong BH, Um SW, Suh GY, Chung MP, Kwon
OJ, Kim H and Kim J: Results of interventional bronchoscopy in the
management of postoperative tracheobronchial stenosis. J Thorac
Cardiovasc Surg. 144:217–222. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Folch E and Keyes C: Airway stents. Ann
Cardiothorac Surg. 7:273–283. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ozdemir C, Sokucu SN, Karasulu L, Onur ST
and Dalar L: Placement of self-expandable bifurcated metallic
stents without use of fluoroscopic and guidewire guidance to
palliate central airway lesions. Multidiscip Respir Med. 11:152016.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Conforti S, Durkovic S, Rinaldo A,
Gagliardone MP, Montorsi E and Torre M: Self-expanding y stent for
the treatment of malignant tracheobronchial stenosis. Retrospective
study. Arch Bronconeumol. 52:e5–e7. 2016.(In English, Spanish).
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Fu YF, Wei N, Zhang K and Xu H: Subcarinal
ventilation-assisted Y-shaped stent insertion under local
anesthesia for patients with complex tracheobronchial stenosis:
Initial clinical experience. Diagn Interv Radiol. 20:330–334. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Madan K, Shrestha P, Garg R, Hadda V,
Mohan A and Guleria R: Bronchoscopic management of critical central
airway obstruction by thyroid cancer: Combination airway stenting
using tracheal and inverted-Y carinal self-expanding metallic
stents. Lung India. 34:202–205. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Fortin M, MacEachern P, Hergott CA, Chee
A, Dumoulin E and Tremblay A: Self-expandable metallic stents in
nonmalignant large airway disease. Can Respir J. 22:235–236. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhu JH, Lei M, Chen EG, Qiao Q and Zhong
TD: Ventilation strategy and anesthesia management in patients with
severe tracheal stenosis undergoing urgent tracheal stenting. Acta
Anaesthesiol Scand. 62:600–607. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Fadaizadeh L, Hosseini MS and Dabir S:
Role of laryngeal mask airway in interventional bronchoscopy
procedures for upper tracheal stenosis: Case series. Middle East J
Anaesthesiol. 22:223–227. 2013.PubMed/NCBI
|
|
31
|
Fernandez-Bustamante A, Ibanez V, Alfaro
JJ, de Miguel E, Germán MJ, Mayo A, Jimeno A, Pérez-Cerdá F and
Escribano PM: High-frequency jet ventilation in interventional
bronchoscopy: Factors with predictive value on high-frequency jet
ventilation complications. J Clin Anesth. 18:349–356. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Mieda H, Nagano Y, Iwasaki E, Oishi Y,
Sasai T, Shin Y, Watanabe Y, Oku S, Fukushima T and Tokioka H: Two
cases of airway stent placement to treat tracheal and bronchial
fistula using general anesthesia under spontaneous respiration.
Masui. 61:880–884. 2012.(In Japanese). PubMed/NCBI
|
|
33
|
Tanigawa N, Kariya S, Komemushi A,
Nakatani M, Yagi R and Sawada S: Metallic stent placement for
malignant airway stenosis. Minim Invasive Ther Allied Technol.
21:108–112. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wang Y, Guo JH, Zhu GY, Zhu HD, Chen L, Lu
J, Wang C and Teng GJ: A novel self-expandable, radioactive airway
stent loaded with (125)I seeds: A feasibility and safety study in
healthy beagle dog. Cardiovasc Intervent Radiol. 40:1086–1093.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Doyle DJ, Abdelmalak B, Machuzak M and
Gildea TR: Anesthesia and airway management for removing pulmonary
self-expanding metallic stents. J Clin Anesth. 21:529–532. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Alazemi S, Lunn W, Majid A, Berkowitz D,
Michaud G, Feller-Kopman D, Herth F and Ernst A: Outcomes,
health-care resources use, and costs of endoscopic removal of
metallic airway stents. Chest. 138:350–356. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Bhandari A, Wang YH, Lv SX, Xia EJ and
Wang OC: Novel strategy of stents in thyroid mass: A case series
report of managing severely dyspneic patients. Onco Targets Ther.
10:4997–5004. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Wang H, Zhou Y, Yamaguchi E, Zhou Y, Li D,
Zou H, Luo L and Ma H: Endoscopic removal of metallic airway
stents. J Bronchology Interv Pulmonol. 18:31–37. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Schmidt B, Massenkeil G, John M, Arnold R
and Witt C: Temporary tracheobronchial stenting in malignant
lymphoma. Ann Thorac Surg. 67:1448–1450. 1999. View Article : Google Scholar : PubMed/NCBI
|