Introduction
Colorectal polyps is a general term used for all the
neoplasms protruding from the intestine. Colorectal polyps have a
high incidence rate globally, and the detection rate of colonoscopy
is 10–20%. Among the patients with colorectal polyps, there are
more male patients than females because colorectal polyps are
closely related to intestinal cancer (1,2). In
Gastroenterology, large intestine polyps are often diagnosed and
their incidence rates are constantly increasing (3). When the growth and death of colorectal
epithelial cells are out of balance, and a certain degree of
abnormal surface mucosal hyperplasia occurs, intestinal polyps
emerge (4). Gastrointestinal polyps
are roughly classified into pedicle and broad-based polyps
according to their shapes (5). There
are documents showing that proliferation of adenoma cancer is a
general pattern of colon cancer development (6). Therefore, early detection, early
treatment and post-treatment follow-up of colorectal polyps are
particularly important (7).
With the rapid development of endoscopic treatment
technology, endoscopic mucosal resection (EMR) has become the most
common polypectomy technique, which is easy to operate and less
painful for the patients. It is recognized as a method that is very
safe and does less harm to patients. Also it is very convenient to
operate (8) and has been widely used
in clinics (9). High-frequency
electric cutting is not easy under endoscopy, and there is a risk
of perforation and hemorrhage. If liquid is injected into the
bottom of the polyp, a layer of liquid pad is created and the polyp
ascends, which can reduce the incidence rates of complications
(5). It has been reported that the
use of submucosal injections during surgery can separate the
muscularis propria and mucosa layer. As a result, the boundary
between the normal mucosa and the polyp mucosa becomes more
obvious, which is beneficial in order to better grasp the range of
the snare during surgery and polyp residues can be prevented.
Moreover, the difference in the maintenance time of different
submucosal injection fluid pads directly affects the surgical
operation and wound healing (10).
In recent years, the use of high-frequency electrocoagulation for
the submucosal injection of saline is the most widely used method.
It is also very easy to operate, and is a safe and effective
mucosal resection method (11). The
injection of normal saline and the tissue fluid are in an isotonic
state, so they have a good compatibility. However, as the osmotic
pressure of normal saline and tissue is the same, the endoscopic
liquid pad disappears too fast during the resection process, which
requires multiple injections and therefore leads to substantial
inconvenience during the surgery (12). Glycerol fructose is a commonly used
submucosal injection in clinical practice and is a hypertonic
solution. Submucosal injection can reduce the risk of perforation
and hemorrhage. Submucosal injection of glycerol fructose during
endoscopic surgery does not stimulate tumor cell proliferation at
the area of the wound, and its mucosal elevation is higher and
longer than normal saline (13).
This study explored many aspects, such as the
complications and resection rates. The effect of submucosal
injection of normal saline and glycerol fructose on endoscopic
polypectomy in patients with large intestine was compared.
Patients and methods
General information
A total of 275 patients with colorectal polyps who
underwent endoscopic polypectomy from March 2013 to December 2016
were assigned. Among them, 150 cases who were treated with
submucosal injection of glycerol fructose were set as the
experimental group, including 98 cases of male patients and 52
cases of female patients, with an average age of 58.2±6.12 years
and average polyp diameter 0.93±0.23 cm. There were 44 multiple
cases, 106 single cases, 78 cases of hypertrophic polyp, 59 cases
of benign polyp and 13 cases of adenomatous polyp in this group. A
total of 125 cases who were treated with submucosal injection of
normal saline were set as the control group, including 70 cases of
male patients and 55 cases of female patients, with an average age
of 58.8±5.98 years and average polyp diameter 0.98±0.21 cm. There
were 35 multiple cases, 90 single cases, 66 cases of hypertrophic
polyp, 49 cases of benign polyp and 10 cases of adenomatous polyp
in this group.
Inclusion criteria: i) patients who met the
diagnostic criteria for intestinal polyps (14); ii) with complete basic clinical
information; iii) with polyp diameter <2.5 cm; iv) for which the
submucosal fluid injection showed a positive sign; and v) who
underwent routine examination before surgery.
Exclusion criteria: i) patients who were not
actively receiving treatment; ii) with endoscopy and
contraindications for treatment; iii) pregnant women; iv) patients
with severe medical conditions who could not undergo surgery; and
v) patients with malignant tumors, thrombocytopenia, and
coagulopathy.
The study was approved by the Ethics Committee of
Qingdao Chengyang People's Hospital (Qingdao, China). The
experimental procedures were described to the patients in detail,
and signed informed consents were obtained from the patients or
their guardians.
Main drugs and instruments
Fujinon 200 series electronic colonoscope (Fujifilm
Corp., Tokyo, Japan), ERBE (ICC 80) high-frequency generator (Erbe
Elektromedizin GmbH, Tuebingen, Germany), Olympus disposable polyp
snare (Olympus Corp., Tokyo, Japan), injection needle (Cook
Regentec, Indianapolis, IN, USA), adrenaline (national medicine
Zhunzi H11020584; Beijing Yongkang Pharmaceutical Co., Ltd.,
Beijing, China), methylene blue (National Pharmaceutical Standard
H32024827; Jiangsu Jumpcan Pharmaceutical Co., Ltd., Jiangsu,
China), sodium chloride solution (H20056130; Beijing Shuanghe
Pharmaceutical Co., Ltd., Beijing, China), glycerol fructose
(National Pharmaceutical Standard H20043355; Zhejiang Tianrui
Pharmaceutical Co., Ltd., Zhejiang, China).
Methods of treatment
Patient information was recorded and medical history
was requested before surgery. For patients with constipation, oral
phenolphthalein tablets were given before surgery (2 pieces/time, 1
or 2 times/day), applying 25 ml of castor oil before taking the
intestinal washing solution (3,000 ml). The method of clyster was
used for patients who could not take the intestinal washing
solution. Patients underwent intramuscular injection of 10 mg
diazepam (National Pharmaceutical Standard H41020631; Tianjin
Pharmaceutical Co., Ltd., Tianjin, China) and 10 mg anisodamine
(National Drug Standard H0000002121; Hangzhou Minsheng
Pharmaceutical Co., Ltd., Hangzhou, China). Oral mannitol was not
taken when cleaning the enema. The four factors of coagulation,
electrocardiogram and blood routine were performed simultaneously.
For older patients, ECG monitoring was also required during
surgery. After the polyps were found, the feces around the polyps
were first drained, the amount of inflation was increased, and it
was determined whether the polyps were suitable for high-frequency
electrotherapy. The snare was inserted to the biopsy hole keeping
the distance between the end of inner lens and the polyp to ~2 cm.
The submucosal injection for the observation group was 38 ml of
glycerol fructose, and for the control group was 38 ml of normal
saline, adding 0.4 ml of methylene blue (10 g/l) and 2 ml of
epinephrine (1 g/l) for both groups. Before the polyp was removed,
the submucosal injection was performed at a penetration angle of
<40° until the polyp was fully lifted for resection. Polyps
>2 cm usually take a one-time excision or partial resection. In
order to maintain the bulging state during the resection process,
the injection was repeated. If the submucosal injection did not
allow the lesion to remain in a raised state, then the operation
needed to be terminated and converted to a surgical operation.
After the polyp was removed, the wound was observed for 1–3 min
until the bleeding was stopped. After surgery, patients rested and
routinely antacids or antibacterials were applied. Crude fiber
foods and physical activities within 2 weeks should be avoided.
Observation indexes
The operation time, the number of repeated
injections, the amount of fluid used for pad injection, the time of
anesthesia and dosage, the en bloc resection rate (EBRR) and the
complete resection rate (CRR) were recorded. Then, the
postoperative complications and the total length of hospitalization
were observed. Patients were followed up for 3 months and their
recurrence was recorded until the deadline in March 2017.
Statistical analysis
Statistical analysis of experimental data was
performed using SPSS 17.0 statistical software (SPSS, Inc.,
Chicago, IL, USA). Data counting was expressed in n (%), and
Chi-square test was used to compare the differences between the
experimental and control group. The measurement data were expressed
as the mean ±standard deviation and paired t-test was used to
compare the differences between the experimental and control group.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Comparison of general data between the
groups
As shown in Table I,
there were no significant differences in terms of sex, average age,
average weight, average height, smoking or non-smoking, alcoholic
or non-alcoholic, average polyp diameter, pathological examination
classification, pathological type, and location of the disease
between the two groups (P>0.05), which suggested that the two
groups were comparable.
 | Table I.Comparison of general information
between experimental and control group [n (%), mean ± standard
deviation]. |
Table I.
Comparison of general information
between experimental and control group [n (%), mean ± standard
deviation].
| Characteristics | Experimental group
(n=150) | Control group
(n=125) | χ2/t | P-value |
|---|
| Sex |
|
| 2.499 | 0.114 |
| Male | 98
(65.3) | 70 (56.0) |
|
|
|
Female | 52
(34.7) | 55 (44.0) |
|
|
| Average age
(years) |
58.2±6.12 |
58.8±5.98 | 0.818 | 0.414 |
| Average weight
(kg) |
75.12±6.48 |
74.78±6.52 | 0.432 | 0.666 |
| Average height
(cm) | 165.41±3.76 |
166.12±3.82 | 1.548 | 0.123 |
| Smoking or
non-smoking |
|
| 0.367 | 0.545 |
|
Smoking | 87
(58.0) | 77 (61.6) |
|
|
|
Non-smoking | 63
(42.0) | 48 (38.4) |
|
|
| Alcoholic or
non-alcoholic |
|
| 0.199 | 0.655 |
|
Alcoholic | 128 (85.3) | 109 (87.2) |
|
|
|
Non-alcoholic | 22
(14.7) | 16
(12.8) |
|
|
| Average polyp
diameter (cm) |
0.93±0.23 |
0.98±0.21 | 1.867 | 0.630 |
| Pathological
examination classification |
|
|
|
|
|
Hypertrophic polyp | 78
(52.0) | 66 (52.8) | 0.017 | 0.895 |
| Benign
polyp | 59
(39.3) | 49 (39.2) | 0.001 | 0.982 |
|
Adenomatous polyp | 13 (8.7) | 10 (8.0) | 0.040 | 0.842 |
| Pathological
type |
|
| 0.059 | 0.808 |
|
Multiple | 44
(29.3) | 35 (28.0) |
|
|
|
Single | 106 (70.7) | 90 (72.0) |
|
|
| Area of
pathogenesis |
|
|
|
|
|
Rectum | 26
(17.3) | 20 (16.0) | 0.087 | 0.768 |
| Sigmoid
colon | 60
(40.0) | 51 (40.8) | 0.018 | 0.893 |
|
Descending colon | 19
(12.7) | 16 (12.8) | 0.001 | 0.974 |
| Ascending
colon | 25
(16.7) | 22 (17.6) | 0.042 | 0.839 |
|
Transverse colon | 20
(13.3) | 16 (12.8) | 0.017 | 0.896 |
Comparison of surgery time between the
groups
There was no significant difference (P>0.05) in
the time until the surgical colonscope insertion reached the
ileocecal valve between the two groups. The time of polyp treatment
and the total surgery time (anesthesia time) in the experimental
group were shorter than those in the control group, and the
differences were statistically significant (t=39.76 and 20.46,
respectively; P<0.05). The number of repeated injections in the
experimental group was less than that in the control group, and the
difference was statistically significant (t=5.875, P<0.05;
Table II).
 | Table II.Comparison of surgery conditions
between experimental and control group (mean ± standard
deviation). |
Table II.
Comparison of surgery conditions
between experimental and control group (mean ± standard
deviation).
| Groups | No. of cases | Time till colonscope
insertion reached ileocecal valve (min) | Time of processing
polyps (min) | Total surgery time
(anesthesia time) (min) | No. of repeated
injections |
|---|
| Experimental
group | 150 | 6.52±1.72 | 3.61±0.59 | 16.24±1.71 | 1 (0.7) |
| Control group | 125 | 6.59±1.75 | 7.42±0.98 | 21.08±2.21 | 7 (5.6) |
|
t/χ2 |
| 0.333 | 39.76 | 20.46 | 5.875 |
| P-value |
| 0.739 |
<0.001 |
<0.001 | 0.015 |
Comparison of the amount of fluid and
propofol injected into patients of the two groups
The amount of fluid used for pad injection and the
amount of propofol used during anesthesia were significantly lower
in the experimental group than that in the control group, and the
differences between the two groups were statistically significant.
(t=38.12 and 4.463, respectively; P<0.05; Table III).
 | Table III.Comparison of the amounts of fluid
and propofol injected in patients of the experimental and control
group (mean ± standard deviation). |
Table III.
Comparison of the amounts of fluid
and propofol injected in patients of the experimental and control
group (mean ± standard deviation).
| Groups | No. of cases | Injection volume
(ml) | Propofol dosage
(mg) |
|---|
| Experimental
group | 150 | 3.66±0.41 | 148.65±15.23 |
| Control group | 125 | 5.87±0.55 | 165.23±42.34 |
| t |
| 38.12 |
4.463 |
| P-value |
|
<0.001 | <0.001 |
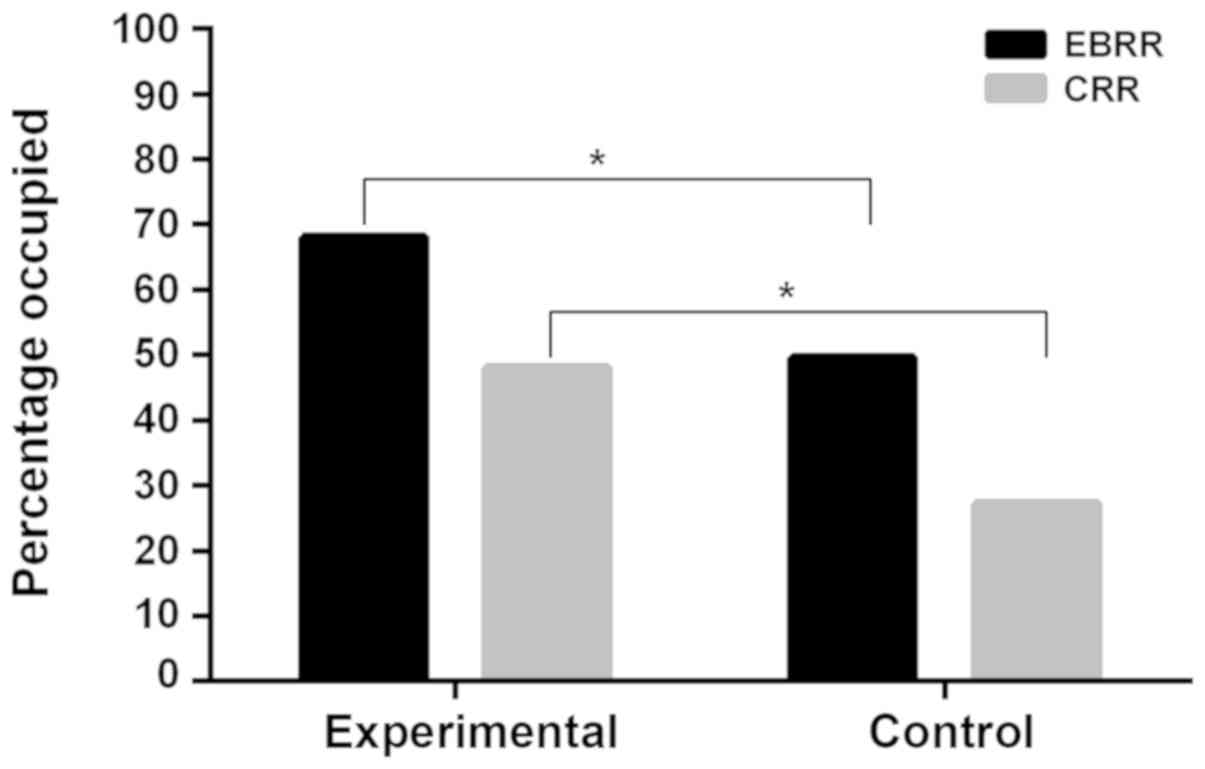
Comparison of resection rates between
the groups
EBRR and CRR in the experimental group were 68.0 and
48.0%, respectively. EBRR and CRR in the control group were 49.6
and 27.2%, respectively. As shown in Fig. 1, EBRR and CRR in the experimental
group were higher than those in the control group, and the
differences were statistically significant (P<0.05).
Comparison of complications between
the groups
There was no perforation in the two groups of
patients during surgery. Intraoperative hemorrhage occurred in 2
patients who underwent surgery and hemostasis was successful under
endoscopy. In the control group, 1 patient developed postoperative
hemorrhage on the 3rd day after surgery, but the amount of blood
loss was small. When colonoscopy was performed again, there was a
blood clot in the area of the wound and blood loss was stopped.
There was no need for endoscopic hemostasis and the patient was
successfully discharged on the 5th day after surgery. Specific
postoperative complications observed in the two groups are shown in
Table IV. There was no significant
difference in the incidence of postoperative complications between
the two groups (P>0.05).
 | Table IV.Comparison of postoperative
complications between experimental and control group [n (%)]. |
Table IV.
Comparison of postoperative
complications between experimental and control group [n (%)].
| Groups | No. of cases | Black stool | Stomach ache | Bloody stool | Perforation | Postoperative
bleeding | Incidence rate
(%) |
|---|
| Experimental
group | 150 | 2 (1.3) | 5 (3.3) | 1 (0.7) | 0 (0.0) | 0 (0.0) | 5.3 |
| Control group | 125 | 3 (2.4) | 4 (3.2) | 2 (1.6) | 0 (0.0) | 1 (0.8) | 8.0 |
| χ2 |
|
|
|
|
|
| 0.740 |
| P-value |
|
|
|
|
|
| 0.390 |
Comparison of average length of
hospitalization and recurrence rate between the groups
There was no significant difference in the average
length of hospitalization between the two groups (t=1.603,
P>0.05). After surgery, patients were followed up for 3 months
by telephone and revisiting the hospital. There was no relapse in
the experimental group and only 2 patients relapsed in the control
group, who were healed after treatment. There was no significant
difference in the recurrence rate between the two groups
(χ2=2.02, P>0.05; Table
V).
 | Table V.Comparison of the average length of
hospitalization and recurrence rate between the experimental and
control group (mean ± standard deviation). |
Table V.
Comparison of the average length of
hospitalization and recurrence rate between the experimental and
control group (mean ± standard deviation).
| Groups | No. of cases | Average length of
hospitalization (days) | Recurrence rate
(%) |
|---|
| Experimental
group | 150 | 3.63±0.49 | 0.00 |
| Control group | 125 | 3.54±0.43 | 1.60 |
|
χ2/t |
| 1.603 | 2.02 |
| P-value |
| 0.110 | 0.155 |
Discussion
Colorectal polyps are new organisms that originate
in the colon and rectal mucosa protruding into the lumen. It is a
common disease of the digestive system, and the risk of developing
colorectal polyps increases with age (15). Pathologically, they can be divided
into adenomatous and non-adenomatous polyps. Currently, it is
believed that most cases of colorectal cancer are evolved from
intestinal polyps. However, adenomatous polyps account for the
majority of them (16,17). As age increases, the rate of polyps
and the rate of malignant transformations also increase (18). There are also documents showing that
the appearance of colorectal polyps may indicate the emergence of
other diseases (19). Therefore, the
early treatment of colorectal polyps is particularly important.
EMR is the primary treatment for colorectal polyps
and can significantly reduce the risk of death from colorectal
cancer (20). However, there are
still risks involved in the surgery, such as infection and
perforation, and especially hemorrhage which is a common
complication (21). Therefore, good
endoscopic skills and clinical judgment are important during
surgery (22), and relevant measures
to reduce the occurrence of complications should be taken.
Injecting certain submucosal during EMR surgery can reduce
complications and make surgery more convenient. The submucosal
injections used in clinical practice are mainly normal saline and
glycerin fructose. Also glycerol fructose is a hypertonic solution
that has no adverse reactions to various systems and is widely used
clinically (23).
In this study, there was no significant difference
in the general clinical information between the experimental and
control group. The surgery time in the experimental group was
shorter than that in the control group. The number of repeated
injections in the experimental group was less than that in the
control group, and the difference was statistically significant
(P<0.05). This indicates that glycerol fructose has a longer
rising time on the mucosa than normal saline. Animal studies have
shown that hypertonic solutions, other than glycerol fructose, can
cause tissue damage to the mucosa (24). By comparing the amount of fluid and
propofol injected in the two groups, we found that the amount used
in the experimental group was less than that in the control group.
Since normal saline has the same osmotic pressure as that of the
tissue, the dispersion was fast. However, since glycerol fructose
is a hypertonic solution that prolongs the time of the fluid pad,
the number of injections were reduced. Propofol is mainly used for
induction and maintenance of anesthesia and is a commonly used drug
during anesthesia. It has the advantages of strong anesthesia
controllability, rapid recovery after surgery and it becomes
effective quickly. However, it can inhibit the human respiratory
and circulatory system (25).
Therefore, reducing the amount of anesthetic drugs can contribute
to the safety of the patient during surgery. EBRR and CRR in the
experimental group were higher than those in the control group, and
the differences were statistically significant (P<0.05). The
results showed that submucosal injection of glycerol fructose has
better effect on the safety and efficacy of endoscopic surgery than
normal saline. The results of the comparison between the recurrence
rate of normal saline and glycerol fructose are consistent with the
results of Uraoka et al (26). In this study, there was no
perforation in the two groups after surgery. There was 1 case of
postoperative hemorrhage in the control group, and there was no
significant difference in the incidence rates of postoperative
complications between the two groups. However, studies have shown
that submucosal injection of glycerol fructose can reduce surgical
complications (27). Also, there was
no significant difference in the average length of hospitalization
between the two groups. After 3 months of follow-up, there was no
statistically significant difference in the recurrence rate between
the two groups and incision wounds healed well in both groups. The
effect of different submucosal injections on endoscopic digestive
tract polypectomy were previously evaluated, and the patients were
followed up for 6 months and no recurrence was found in either
group (10).
In this study, we compared the general clinical
information, the amount of injection and propofol used in two
groups. We also compared the complications, the average length of
hospitalization and recurrence rates between the two groups. A more
comprehensive analysis was performed on the effects of the
injection of glycerol fructose and normal saline on endoscopic
resection of polyps in patients in the large intestine. There are,
still relatively few comparative studies between the two groups and
still many problems worthy of further study. Therefore, it is
crucial to find the best treatment and submucosal injection.
In conclusion, endoscopic colorectal polypectomy
with glycerol fructose as a submucosal injection can shorten the
surgery time, decrease the number of repeated injections, reduce
the amount of injections and dosage of propofol and increase EBRR
and CRR.
Acknowledgements
Not applicable.
Funding
This study was supported by the 2013 Chengyang
District People's Livelihood Science and Technology Development
Project (13–14-ms).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
HW conceived and designed the study, and drafted the
manuscript. HW and SW were responsible for the analysis of the
observation indexes. Both authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Qingdao Chengyang People's Hospital (Qingdao, China). Signed
informed consents were obtained from the patients or their
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Koessler T, Bichard P, Lepilliez V, Puppa
G, Ris F and Roth A: Epidemiology, treatment and follow-up of
colorectal polyps. Rev Med Suisse. 12:982–988. 2016.(In French).
PubMed/NCBI
|
|
2
|
Roperch JP, Incitti R, Forbin S, Bard F,
Mansour H, Mesli F, Baumgaertner I, Brunetti F and Sobhani I:
Aberrant methylation of NPY, PENK, and WIF1 as a promising marker
for blood-based diagnosis of colorectal cancer. BMC Cancer.
13:5662013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Passarelli MN, Newcomb PA, Makar KW,
Burnett-Hartman AN, Potter JD, Upton MP, Zhu LC, Rosenfeld ME,
Schwartz SM and Rutter CM: Blood lipids and colorectal polyps:
Testing an etiologic hypothesis using phenotypic measurements and
Mendelian randomization. Cancer Causes Control. 26:467–473. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gonçalves BM, Fontainhas V, Caetano AC,
Ferreira A, Gonçalves R, Bastos P and Rolanda C: Oncological
outcomes after endoscopic removal of malignant colorectal polyps.
Rev Esp Enferm Dig. 105:454–461. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Aferzon M and Millman B: Excision of
rhinophyma with high-frequency electrosurgery. Dermatol Surg.
28:735–738. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang JP, Yang ZL, Wang L, Dong WG, Huang
YH, Qin JZ and Zhan WH: Multi-variate regression analysis of
clinicopathological characteristics and prognosis of colorectal
cancer. Zhonghua Zhong Liu Za Zhi. 25:59–61. 2003.(In Chinese).
PubMed/NCBI
|
|
7
|
Rosenberg L, Boggs D, Wise LA, Palmer JR,
Roltsch MH, Makambi KH and Adams-Campbell LL: A follow-up study of
physical activity and incidence of colorectal polyps in
African-American women. Cancer Epidemiol Biomarkers Prev.
15:1438–1442. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fabricius R, Svenningsen P, Hillingsø J,
Svendsen LB and Sillesen M: Effect of transfusion strategy in acute
non-variceal upper gastrointestinal bleeding: a nationwide study of
5861 hospital admissions in Denmark. World J Surg. 40:1129–1136.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Repici A, Conio M, De Angelis C, Sapino A,
Malesci A, Arezzo A, Hervoso C, Pellicano R, Comunale S and
Rizzetto M: Insulated-tip knife endoscopic mucosal resection of
large colorectal polyps unsuitable for standard polypectomy. Am J
Gastroenterol. 102:1617–1623. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lang GD, Konda VJ, Siddiqui UD, Koons A
and Waxman I: A single-center experience of endoscopic submucosal
dissection performed in a Western setting. Dig Dis Sci. 60:531–536.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ahmad NA, Kochman ML, Long WB, Furth EE
and Ginsberg GG: Efficacy, safety, and clinical outcomes of
endoscopic mucosal resection: a study of 101 cases. Gastrointest
Endosc. 55:390–396. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Miyazaki H, Kato J, Kakizaki H, Nagata T,
Uetake H, Okudera H, Watanabe H, Hashimoto K and Omura K:
Submucosal glycerol injection-assisted laser surgical treatment of
oral lesions. Lasers Med Sci. 24:13–19. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fujishiro M, Yahagi N, Kashimura K,
Mizushima Y, Oka M, Enomoto S, Kakushima N, Kobayashi K, Hashimoto
T, Iguchi M, et al: Comparison of various submucosal injection
solutions for maintaining mucosal elevation during endoscopic
mucosal resection. Endoscopy. 36:579–583. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li K, Hu G, Xu M, Lu L, Wan R and Wang X:
Comparison of 1.9 µm Vela Laser versus high-frequency electronic
knife in the treatment of digestive tract big polyps. Zhonghua Yi
Xue Za Zhi. 94:3349–3351. 2014.(In Chinese). PubMed/NCBI
|
|
15
|
Mik M, Dziki Ł, Trzciński R and Dziki A:
Risk factors of 30-day mortality following surgery for colorectal
cancer. Pol Przegl Chir. 88:26–31. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Trecca A, Gaj F and Gagliardi G: Our
experience with endoscopic repair of large colonoscopic
perforations and review of the literature. Tech Coloproctol.
12:315–321; discussion 322. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yoon JH, Lee HL, Kim DW and Choi CR: Is
obesity a risk factor for advanced colon polyps in males?
Hepatogastroenterology. 58:1159–1162. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Corley DA, Jensen CD, Marks AR, Zhao WK,
de Boer J, Levin TR, Doubeni C, Fireman BH and Quesenberry CP:
Variation of adenoma prevalence by age, sex, race, and colon
location in a large population: Implications for screening and
quality programs. Clin Gastroenterol Hepatol. 11:172–180. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Karagianni V, Merikas E, Georgopoulos F,
Gikas A, Athanasopoulos N, Malgarinos G, Peros G and
Triantafillidis JK: Risk factors for colorectal polyps: Findings
from a Greek case- control study. Rev Med Chir Soc Med Nat Iasi.
114:662–670. 2010.PubMed/NCBI
|
|
20
|
Zauber AG, Winawer SJ, O'Brien MJ,
Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, Shi W, Bond JH,
Schapiro M, Panish JF, et al: Colonoscopic polypectomy and
long-term prevention of colorectal-cancer deaths. N Engl J Med.
366:687–696. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dobrowolski S, Dobosz M, Babicki A,
Głowacki J and Nałecz A: Blood supply of colorectal polyps
correlates with risk of bleeding after colonoscopic polypectomy.
Gastrointest Endosc. 63:1004–1009. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Herreros de Tejada A: ESD training: A
challenging path to excellence. World J Gastrointest Endosc.
6:112–120. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sakamaki M, Igarashi H, Nishiyama Y,
Hagiwara H, Ando J, Chishiki T, Curran BC and Katayama Y: Effect of
glycerol on ischemic cerebral edema assessed by magnetic resonance
imaging. J Neurol Sci. 209:69–74. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fujishiro M, Yahagi N, Kashimura K,
Matsuura T, Nakamura M, Kakushima N, Kodashima S, Ono S, Kobayashi
K, Hashimoto T, et al: Tissue damage of different submucosal
injection solutions for EMR. Gastrointest Endosc. 62:933–942. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Suzuki K, Yoshida H, Näppi J and Dachman
AH: Massive-training artificial neural network (MTANN) for
reduction of false positives in computer-aided detection of polyps:
Suppression of rectal tubes. Med Phys. 33:3814–3824. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Uraoka T, Fujii T, Saito Y, Sumiyoshi T,
Emura F, Bhandari P, Matsuda T, Fu KI and Saito D: Effectiveness of
glycerol as a submucosal injection for EMR. Gastrointest Endosc.
61:736–740. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Katsinelos P, Kountouras J, Paroutoglou G,
Zavos C, Rizos C and Beltsis A: Endoscopic mucosal resection of
large sessile colorectal polyps with submucosal injection of
hypertonic 50 percent dextrose-epinephrine solution. Dis Colon
Rectum. 49:1384–1392. 2006. View Article : Google Scholar : PubMed/NCBI
|