Introduction
Colon cancer (CC) is one of the most common
malignancy types of the gastrointestinal tract and a leading cause
of cancer-associated mortalities worldwide in 2012 (1). Over the last decade, postoperative
chemotherapy has become the standard treatment for locally advanced
CCs, administered to avoid recurrences of cancer following surgery,
and has notably improved the prognostic outcomes of patients with
CC (2–6). In particular, adjuvant 5-fluorouracil
(5-FU) and oxaliplatin combination therapy, termed FOLFOX, is a
widely accepted standard regimen for resected stage III CC
(7). However, therapeutic responses
and clinical outcomes differ among individual patients.
Cancer stem cells (CSCs) represent a small
population of cancer cells that share common properties with normal
stem cells, including the ability of self-renewal and
multi-directional differentiation (8,9). Due to
these properties, subsequent to undergoing radio- or chemotherapy,
the residual CSCs can rapidly proliferate to re-establish the tumor
(10). Additionally, CSCs have
variable intrinsic or acquired drug resistance mechanisms,
including hypoxic stability, enhanced activity of repair enzymes
and expression of antiapoptotic proteins, including B-cell lymphoma
2 (10–12). Therefore, the presence of CSCs has
been considered to be a major contributor to the development of
chemoresistance in malignant tumor cases (13–15).
Expression of drug efflux transporters is also associated with the
chemoresistant properties of CSCs (14,16–18).
ATP-binding cassette (ABC) transporter proteins serve as efflux
pumps to actively extrude molecules out of cells, and expression of
ABC transporters in cancer cells is one of the major causes of
multidrug resistance, a key obstacle to cancer chemotherapy
(19). Multiple transporters,
including ABC subfamily B member 1 and ABC subfamily G member 2
(ABCG2), have been identified in CSCs and have been indicated to
serve an important role in the clinical resistance of CSCs to
anticancer drugs (17,18).
The prognostic importance of the transcript or
protein expression level of CSC markers and ABC transporter has
been reported in colorectal cancer (20–23), and
also investigated in colorectal cancer cohorts treated with
specific adjuvant or neoadjuvant treatment (24–27).
Furthermore, the association between ABC transporters or CSC
properties and chemoresponses has been reported using multiple
colorectal cancer cell lines (28–30).
Overexpression of leucine-rich repeat-containing G protein-coupled
receptor 5 (LGR5) reduced the sensitivity toward 5-FU and
oxaliplatin of Lovo, HT29 and HCT116 cells (29), and inhibition of ABC subfamily C
member 3 (ABCC3) increased sensitivity to 5-FU (30) in HT29 and SW480 cells. Expression of
ABC transporters in colorectal cancer tissues has been associated
with chemoresponse. Patients with metastatic colorectal cancer with
immunohistochemical (IHC) overexpression of ABCG2 indicated
resistance to 5-FU-based treatment (31), and aberrant ABCC3 protein expression
had been reported to be associated with chemo-radioresistance in
patients with rectal cancer (30).
Despite the aforementioned results, Hlavata et al (24) reported that transcript levels of
various ABC transporters, including ABC subfamily C member 6, ABC
subfamily C member 11, ABC subfamily F member 1 and ABC subfamily F
member 2, were decreased in non-responders to palliative
chemotherapy in patients with colorectal cancer.
The present study evaluated the expression of
multiple ABC transporters and CSC markers in cancer tissues from a
homogeneous group of patients with stage III CC postoperatively
receiving 5-fluorouracil, leucovorin and oxaliplatin combination
therapy (FOLFOX-4 regimen) using an IHC method and statistically
analyzed their prognostic significance. Through the literature
review, 3 ABC transporters, including ABCC2, ABCC3 and ABCG2, and 3
CSC markers, including LGR5, aldehyde dehydrogenase 1 (ALDH1) and
sex determining region Y-box 2 (SOX2) were selected, of which
primary antibodies for IHC staining were available and clinical
implications have been reported in patients with colorectal cancer
(21,22,24,26,27,30–34). The
results of the present study will provide fundamental data for
investigating the usefulness of ABC transporters and CSC markers as
prognostic markers and as target molecules.
Materials and methods
Patients and tissue samples
A total of 164 CC tissues were collected for the
present study from patients with stage III CC who had received
postoperative adjuvant therapy with the FOLFOX-4 regimen between
May 2003 and December 2010 at Seoul National University Bundang
Hospital (Seongnam, South Korea). The mean age of the patients at
diagnosis was 59.8±10.4 years. A total of 58 patients (35.4%) were
female and 106 (64.6%) were male (Table
I). Therapeutic and prognostic data were collected from the
archives of the Department of Internal Medicine of Seoul National
University Bundang Hospital. The inclusion criteria for patients
were as follows: the presence of histologically proven
adenocarcinomas of primary CCs, the availability of paraffin blocks
of the resected specimens and available information on the
follow-up conducted on these patients. Histopathological and
clinical data were obtained from the medical records and
pathological reports of the patients. Pathological stage was
determined per the grading system of the 8th edition of the
American Joint Committee on Cancer (35). Patients did not receive neoadjuvant
chemotherapy or radiotherapy, and were followed-up through November
1 2015. Follow-up of patients was scheduled at 3-monthly intervals
for up to 2 years, 6-monthly intervals for up to 5 years, and
annually thereafter. During follow-up visits, all relevant data
were collected. All tissue samples were fixed in 10% formalin at
24°C for 12 h and embedded in paraffin. This study was approved by
the Institutional Review Board for Research Using Human Subjects at
the Seoul National University Bundang Hospital (IRB no.
B1512-326/302).
 | Table I.Clinicopathological characteristics
of patients with CC. |
Table I.
Clinicopathological characteristics
of patients with CC.
| Variables | Value, n (%) |
|---|
| Age (years) |
| Mean ±
standard deviation (range) | 59.8±10.4
(28–80) |
| Sex (%) |
|
Female | 58 (35.4) |
|
Male | 106 (64.6) |
| Location (%) |
| Right
colon | 50 (30.5) |
| Left
colon | 114 (66.5) |
| Tumor size
(cm) |
| Mean ±
standard deviation (range) | 5.1±1.9
(1.5–11.0) |
| Gross type (%) |
|
Polypoid | 8 (4.9) |
|
Ulcerofungating | 91 (55.8) |
|
Ulceroinfiltrative | 63 (38.7) |
| Flat (%) | 1 (0.6) |
|
Microsatellite instability
statusa |
|
Microsatellite
instability-high | 8 (4.8) |
|
Microsatellite
instability-low | 9 (5.5) |
|
Microsatellite stable | 146 (89.6) |
| Differentiation
(%) |
| Well
differentiated | 3 (1.9) |
|
Moderately differentiated | 139 (88.0) |
| Poorly
differentiated | 16 (10.1) |
| Pathological T
stage (%)a |
|
pTis | 0 (0) |
|
pT1 | 2 (1.2) |
|
pT2 | 4 (2.4) |
|
pT3 | 124 (75.6) |
|
pT4a | 29 (17.7) |
|
pT4b | 5 (3.0) |
| Pathological N
stage (%)a |
| N0 | 0 (0) |
| N1 | 102 (62.6) |
| N2 | 62 (37.3) |
| Lymphatic invasion
(%) |
|
Present | 88 (53.7) |
| Not
identified | 76 (46.3) |
| Vascular invasion
(%) |
|
Present | 29 (17.7) |
| Not
identified | 135 (82.3) |
| Perineural invasion
(%) |
|
Present | 68 (41.5) |
| Not
identified | 96 (58.5) |
| Disease
progression | 29 (17.7) |
| Local
recurrence only | 4 (2.4) |
| Distant
metastasis only | 23 (14.0) |
| Local
recurrence and distant metastasis | 2 (1.2) |
| No
recurrence/metastasis | 135 (82.3) |
| Death | 16 (9.8) |
Chemotherapeutic treatment
A total of 12 cycles of the adjuvant FOLFOX-4
regimen were administered. Each cycle consisted of a 2-h infusion
of oxaliplatin at a dose of 85 mg/m2 administered
simultaneously with a 2-h infusion of leucovorin at a dose of 200
mg/m2, followed by a bolus of 5-FU at a dose of 400
mg/m2, and then a 22-h infusion of 5-FU at a dose of 600
mg/m2 administered on 2 consecutive days. This cycle was
repeated every 2 weeks. Detailed frequencies of adverse events were
presented in Table SI. The grade
for adverse event was determined according to Common Terminology
Criteria for Adverse Events v. 4.0 (36). Dosage of chemotherapy was determined
every cycle by each physician's discretion. The physicians were
affiliated with Seoul National University Bundang Hospital.
Relative dose intensities of oxaliplatin and 5-FU were not
different according to protein expression (data not shown).
Construction of tissue microarrays
(TMAs)
A representative tumor section slide and the
corresponding paraffin block (donor block) were collected from each
case following slide review. Following the marking of areas of high
tumor cell density on the selected slides, tumor cores (2 mm
diameter) were obtained from the corresponding areas of the
paraffin blocks, using a trephine apparatus. A total of 164
trephined paraffin tissue cores from 164 patients were
consecutively placed into recipient blocks (TMA blocks). Each TMA
block incorporated up to 60 samples.
IHC staining and interpretation of
results
Detailed information regarding used primary
antibodies is presented in Table
II. IHC staining was performed using a BenchMark XT automated
immunostaining system (Ventana Medical Systems, Inc., Tucson, AZ,
USA), according to the manufacturer's protocols. Briefly,
4-µm-thick sections were cut from each of the paraffin tissue
blocks, mounted on positively charged slides, and dried at 62°C for
30 min. Subsequent to undergoing heat epitope retrieval at 98°C for
60 min in ethylenediaminetetraacetic acid (pH 8.0) in the
autostainer, endogenous peroxidase activity was blocked by
immersing the slides in a 3% hydrogen peroxidase solution for 4 min
at 36°C. The samples were incubated with individual primary
antibodies at 36°C for 32 min and then incubated with a mixture of
horseradish peroxidase-labeled antibodies composed of goat
anti-rabbit antibody and goat anti-mouse antibody included in the
UltraView Universal DAB kit (cat. no. 760-500; Ventana Medical
Systems, Inc.) for 8 min at 36°C. Following treatment with 0.04%
hydrogen peroxide in a phosphate buffer solution and DAB chromogen
containing 0.2% 3,3′-diaminobenzidine tetrahydrochloride at 36°C
for 8 min, samples were treated with copper sulfate (5 µg/l) at
36°C for 4 min (all reagents used in these processes were included
in the UltraView Universal DAB kit; cat. no. 760-500; Ventana
Medical Systems, Inc.). Slides were counterstained with 0.5%
Modified Mayer's Hematoxylin at 36°C for 4 min. Placenta tissues
were mounted on each slide as a positive control for LGR5, ABCC3
and ABCG2, and hepatic tissues were mounted as a positive control
for ALDH1, SOX2 and ABCC2.
 | Table II.Antibodies used for
immunohistochemical staining. |
Table II.
Antibodies used for
immunohistochemical staining.
| Antibody | Company | Cat. no. | Clonality | Reactivity | Dilution |
|---|
| ABCC2 | Abcam, Cambridge,
UK | Ab3373 | Mouse
monoclonal | Human | 1:50 |
| ABCC3 | Abcam | Ab3375 | Mouse
monoclonal | Human | 1:20 |
| ABCG2 | Alexis
Biochemicals; Enzo Life Sciences, Inc., Farmingdale, NY, USA | ALX
801-029-C125 | Mouse
monoclonal | Human | 1:200 |
| LGR5 | Sigma-Aldrich;
Merck KGaA, | HPA012530 | Rabbit
polyclonal | Human | 1:100 |
| ALDH1 | BD Bioscience, San
Jose, CA, USA | 44/ALDH | Mouse
monoclonal | Human | 1:100 |
| SOX2 | EMD Millipore,
Billerica, MA, USA | 636675 | Mouse
monoclonal | Human | 1:500 |
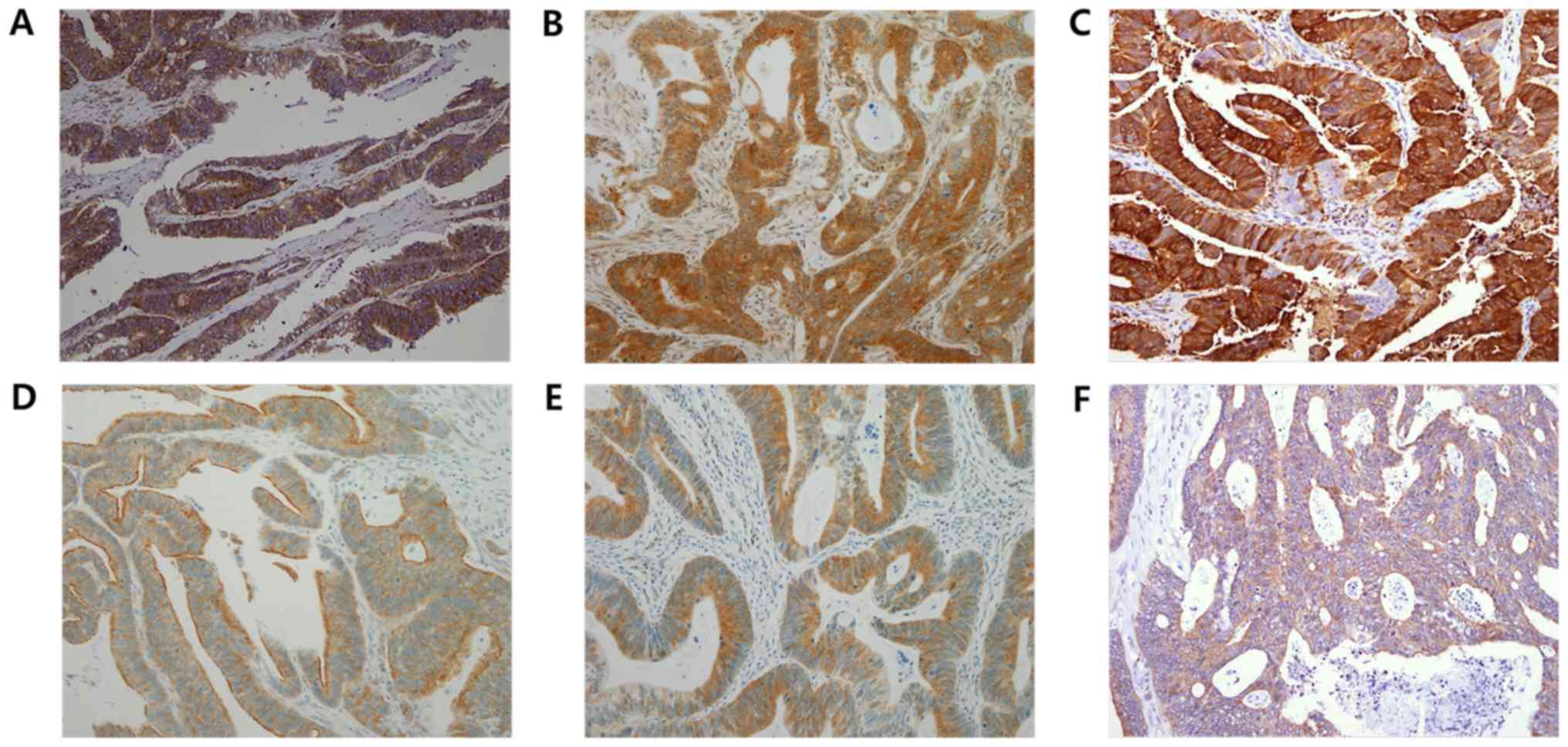
A total of two pathologists (ES and MLK) manually
evaluated the IHC stained slides at ×200 magnification in a blinded
fashion under a light microscope. Staining intensities were
semi-quantitatively scored as negative (score=0), weak (score=1),
moderate (score=2) or strong (score=3). Additionally, the
percentage of immune-reactive cells was assessed. There are no
established absolute criteria for immune-positivity for the
examined proteins; therefore, by testing a series of different
values, the staining results were deemed positive when >10% of
tumor cells had intensity scores of ≥1. The representative
immunostainings are presented in Fig.
1.
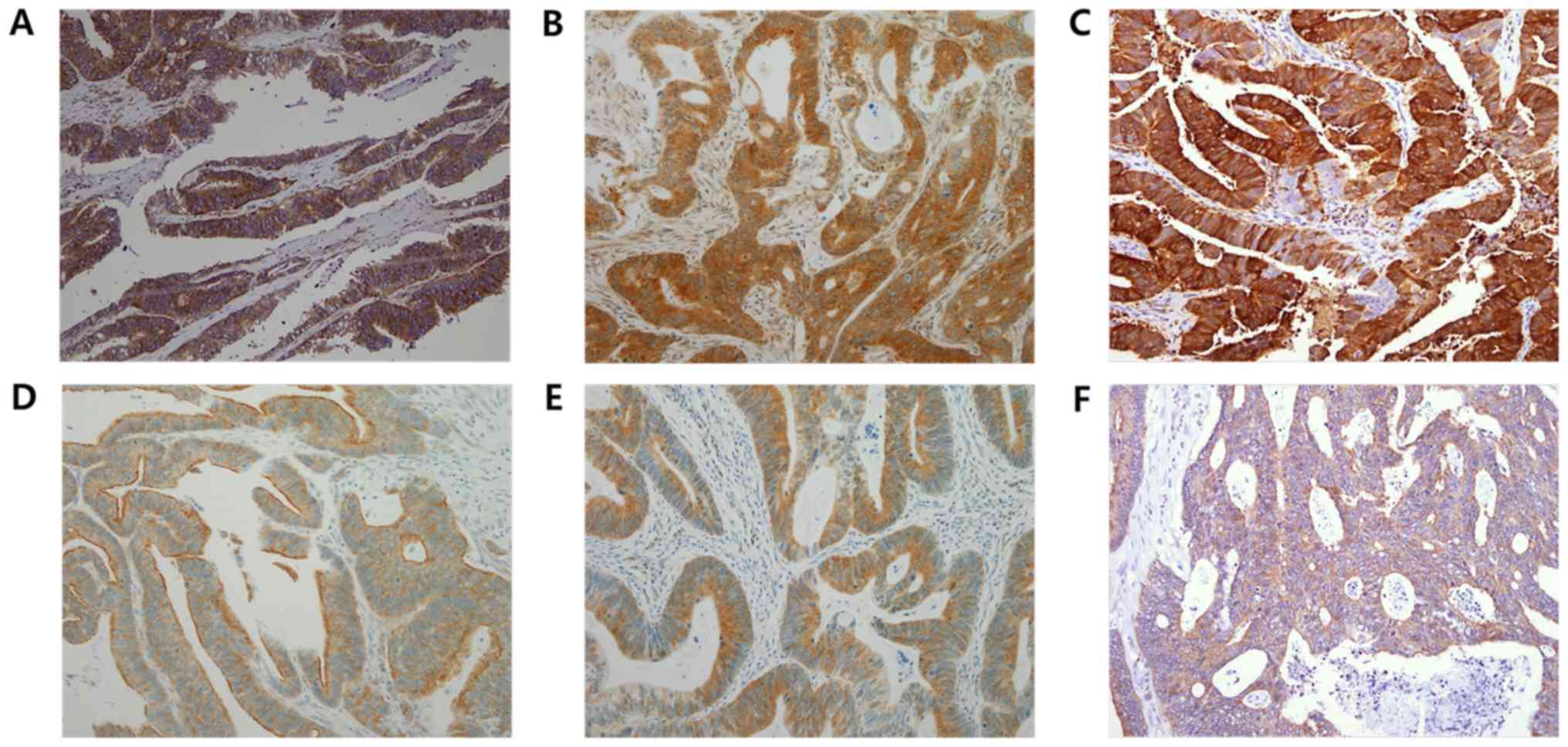 | Figure 1.Representative immunohistochemical
images of cancer stem cell markers and ABC transporters in colon
cancer. (A) ABCC2, (B) ABCC3, (C) ABCG2, (D) LGR5, (E) SOX2 and (F)
ALDH1 (magnification, ×200). ABCC2, ATP binding cassette subfamily
C member 2; ABCC3, ATP binding cassette subfamily C member 3;
ABCG2, ATP binding cassette subfamily G member 2; LGR5,
leucine-rich repeat containing G protein-coupled receptor 5; SOX2,
sex determining region Y-box 2; ALDH1, aldehyde dehydrogenase 1;
ABC, ATP-binding cassette. |
Statistical analysis
Statistical analysis was performed using the SPSS
21.0 software (IBM Corp., Armonk, NY, USA). Spearman's Rho
coefficient test was used to analyze correlations between
expression levels of proteins. The associations between the status
of expression of the different proteins and the clinicopathological
features of the corresponding patients were analyzed using
Pearson's χ2 test. For analysis of survival data, the
differences between survival rates were determined using the
log-rank test, and multivariate analysis was performed using the
backward conditional method of Cox proportional hazards regression
modeling. Disease-free survival rate (DFS) was calculated from the
date of surgery to the date of first recurrence or mortality.
Overall survival rate (OS) was defined as the interval from the
date of surgery to the date the patient succumbed. Continuous
variables are presented as the means ± standard deviation.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Characteristics of patients
The clinicopathological characteristics of patients
with CC receiving adjuvant FOLFOX-4 treatment are detailed in
Table I. By location, 30.5% of the
tumors were localized in the right colon and 66.5% in the left
colon. In 2 patients (1.2%), the CCs were classified as
pathological stage T1, in 4 (2.4%) as stage T2, in 124 (75.6%) as
stage T3, in 29 (17.7%) as stage T4a and in 5 (3.0%) as stage T4b.
All cases exhibited lymph node metastases; 102 (62.6%) cases were
classified as N1 and 62 (37.3%) cases were classified as N2
(Table I). Lymphatic, vascular and
perineural invasion were indicated in 88 (53.7%), 29 (17.7%) and 68
(41.5%) patients, respectively. During follow-up, 29 patients had
local recurrences or distant metastases, and 16 patients succumbed
(Table I).
Expression profiles of ABC
transporters and CSC markers
The expression frequencies of the examined ABC
transporters were as follows: 87.1 (142/163) for ABCC2, 44.8
(73/164) for ABCC3 and 85.4% (140/164) for ABCG2. The expression
frequencies of the CSC markers were 79.9 (131/164), 38.4 (63/164)
and 82.3% (135/164) for LGR5, ALDH1 and SOX2, respectively.
Immune-positivities with detailed case distribution according to
intensity score are presented in Table
III. Among the immune-positive cases, moderate intensity
(intensity score 2) was the most frequent expression pattern for
ABCC2, ABCC3 and LGFR5, while strong intensity was the most
frequent expression pattern for ALDH1, ABCG2 and SOX2
immunostaining. Particularly, the expression intensity of ALDH1 was
relatively strong with only one case exhibiting weak expression.
Expression of ABCC2 was significantly associated with that of ABCC3
and LGR5 (Spearman's Rho coefficient =0.347 and 0.354,
respectively; P<0.001). Additionally, there was an association
between the expression of ABCC3 and SOX2 (Spearman's Rho
coefficient =0.192; P=0.014) (data not shown).
 | Table III.Expression frequencies of ABC
transporters and stem cell markers. |
Table III.
Expression frequencies of ABC
transporters and stem cell markers.
|
|
| n (%) |
|---|
|
|
|
|
|---|
| Protein
classification | Protein | Intensity score
1 | Intensity score
2 | Intensity score
3 |
Immune-positivity |
|---|
| ABC
transporter | ABCC2 | 27/163
(16.6) | 71/163 (43.6) | 44/163 (27.0) | 142/163 (87.1) |
|
| ABCC3 | 13/164 (7.9) | 38/164 (23.2) | 22/164 (13.4) | 73/164
(44.5) |
|
| ABCG2 | 39/164
(23.8) | 49/164 (29.9) | 52/164 (31.7) | 140/164 (85.4) |
| Stem cell
marker | LGR5 | 23/164
(14.0) | 62/164 (37.8) | 46/164 (28.0) | 131/164 (79.9) |
|
| ALDH1 | 1/164
(0.6) | 20/164 (12.2) | 42/164 (25.6) | 63/164
(38.4) |
|
| SOX2 | 23/164
(14.0) | 52/164 (31.7) | 60/164 (36.6) | 135/164 (82.3) |
The association between the expression of ABC
transporters and CSC markers and the clinicopathological parameters
of the corresponding patients was tested using Pearson's
χ2 test. Expression of ALDH1 was significantly
associated with the right-sided location of tumors (P=0.010).
However, no statistically significant associations were observed
between expression of these proteins and the rest of the parameters
(data not shown).
Association between the expression of
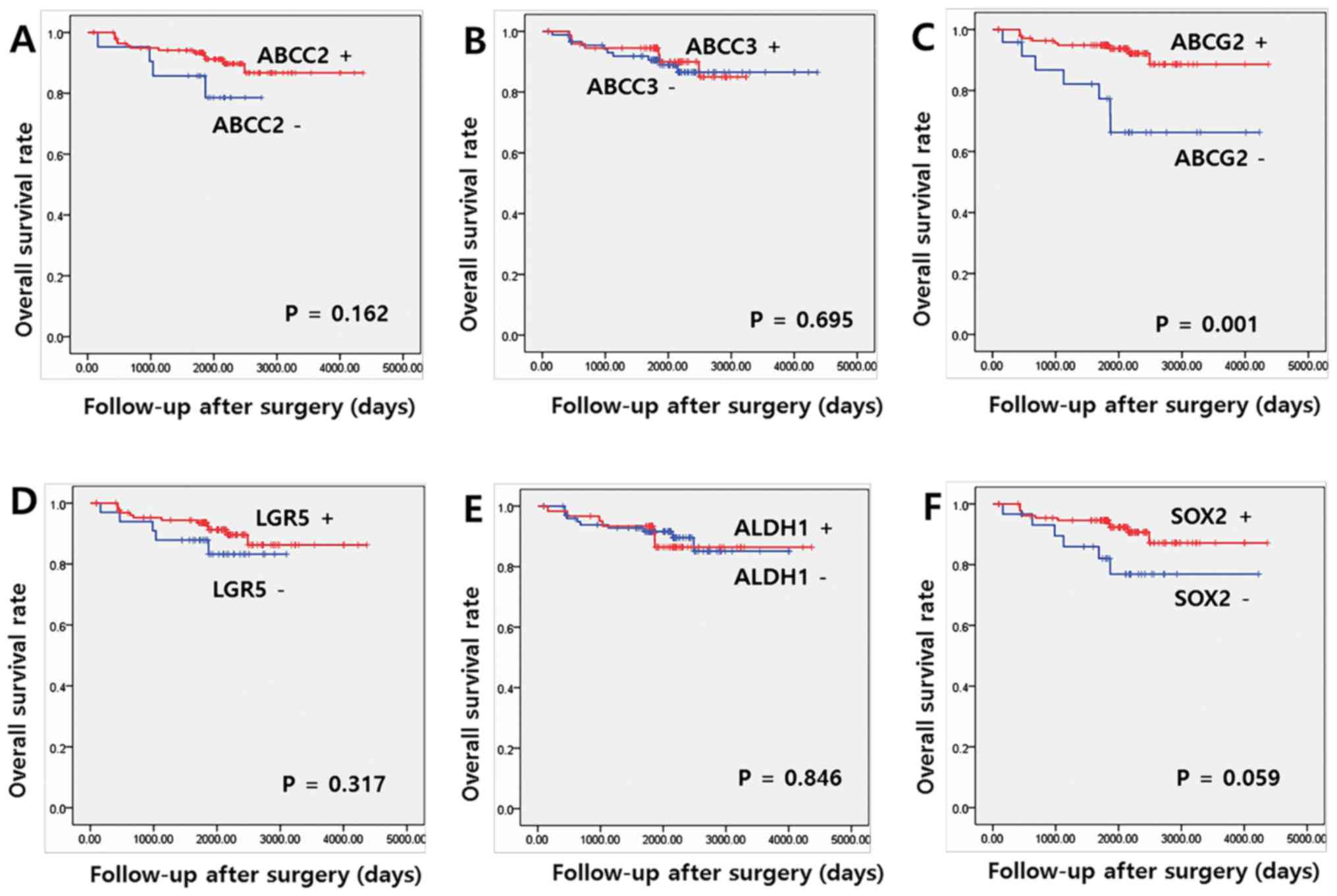
ABC transporters and CSC markers and OS
The median and mean OS at the last follow-up
appointment were 66.8 and 67.0 months, respectively. Univariate
analysis indicated that ABCG2 expression was significantly
associated with OS (P=0.001). Expression levels of other proteins,
including ABCC2, ABCC3, LGR5, ALDH1 and SOX2, indicated no
significant association with OS (Fig.
2). Among the clinicopathological parameters, pathological N
stage, lymphatic invasion and perineural invasion exhibited an
association with OS (P=0.040, 0.003 and 0.003, respectively; data
not shown). Multivariate Cox regression analyses identified ABCG2
overexpression as an independent positive prognostic indicator of
OS [hazard ratio (HR)=2.877 and 95% confidence interval
(CI)=1.019–8.119; P=0.046). Lymphatic invasion also had a
significant effect on OS in multivariate analysis (P=0.049;
Table IV).
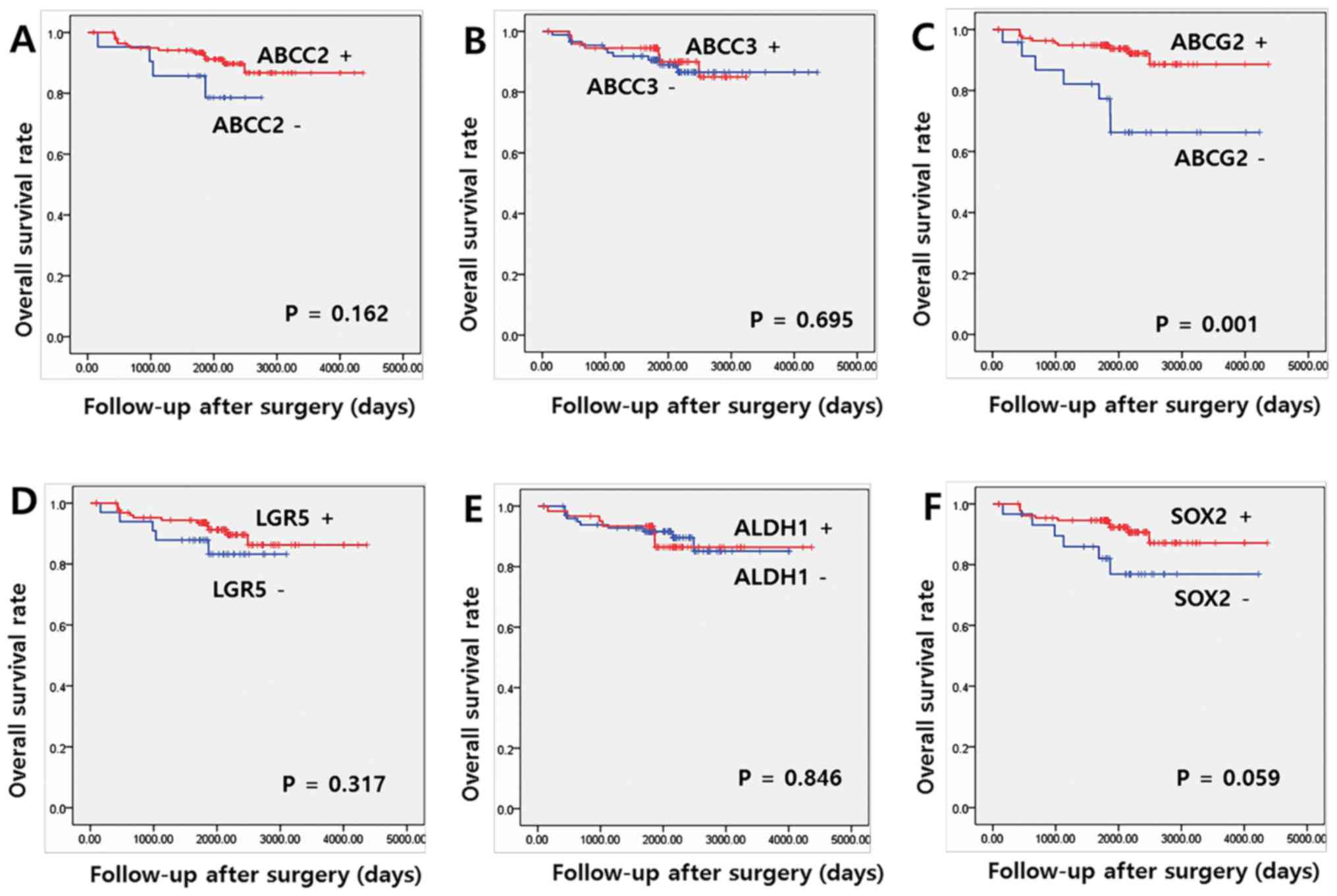 | Figure 2.Association between overall survival
rate, and expression of cancer stem cell markers and ABC
transporters. Kaplan-Meier overall survival curve for patients with
colon cancer according to (A) ABCC2, (B) ABCC3, (C) ABCG2, (D)
LGR5, (E) ALDH1 and (F) SOX2. ABCC2, ATP binding cassette subfamily
C member 2; ABCC3, ATP binding cassette subfamily C member 3;
ABCG2, ATP binding cassette subfamily G member 2; LGR5,
leucine-rich repeat containing G protein-coupled receptor 5; SOX2,
sex determining region Y-box 2; ALDH1, aldehyde dehydrogenase 1;
ABC, ATP-binding cassette. |
 | Table IV.Multivariate analyses for overall
survival rate in patients with colon cancer. |
Table IV.
Multivariate analyses for overall
survival rate in patients with colon cancer.
| Variable | HR | 95% CI | P-value |
|---|
| Lymph node
stage |
|
| 0.584 |
|
pN1 | 1 |
|
|
|
pN2 | 1.353 | 0.458–3.997 |
|
| Lymphatic
invasion |
|
|
0.049a |
|
Absent | 1 |
|
|
|
Present | 4.718 |
1.006–22.124 |
|
| Perineural
invasion |
|
| 0.070 |
|
Absent | 1 |
|
|
|
Present | 2.962 | 0.915–9.588 |
|
| ABCG2 |
|
|
0.046a |
|
Negative | 2.877 | 1.019–8.119 |
|
|
Positive | 1 |
|
|
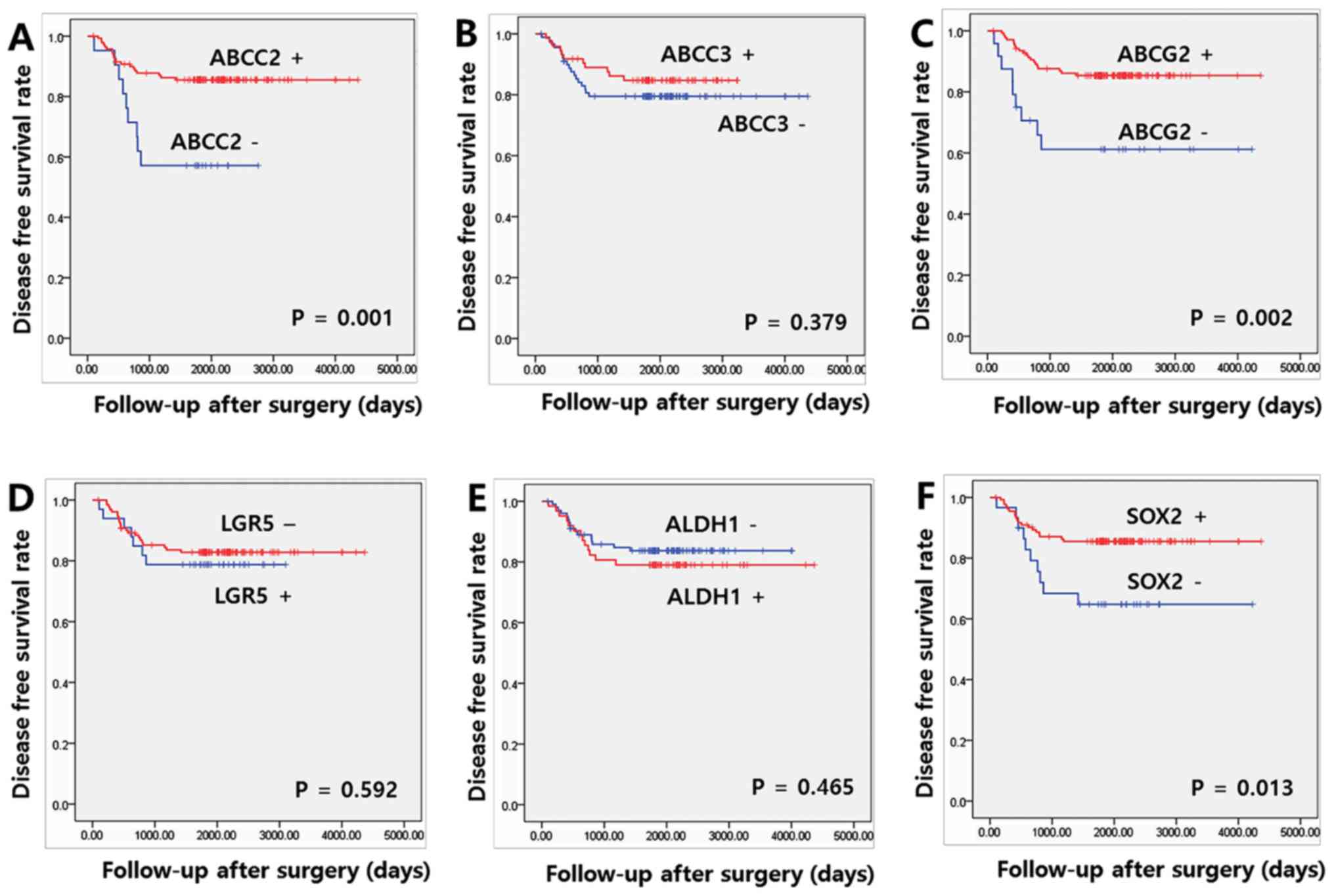
Association between the expression of
ABC transporters and CSC markers and DFS
The median and mean DFS at the last follow-up
appointment were 61.9 and 61.7, respectively. Significant increases
in DFS were observed in patients who were positive for ABCC2, ABCG2
and SOX2, compared with patients who were negative for these
proteins (P=0.001, 0.002 and 0.013, respectively; Fig. 3). Among the clinicopathological
parameters, only the presence of perineural invasion was associated
with a reduced DFS (P=0.013; data not shown). On multivariate Cox
regression analyses for DFS, expression of ABCC2 and SOX2 remained
independent prognostic factors of the FOLFOX group (HR=2.831, 95%
CI=1.238–6.474 and P=0.014; and HR=2.558, 95% CI=1.156–5.658 and
P=0.020, respectively; Table V).
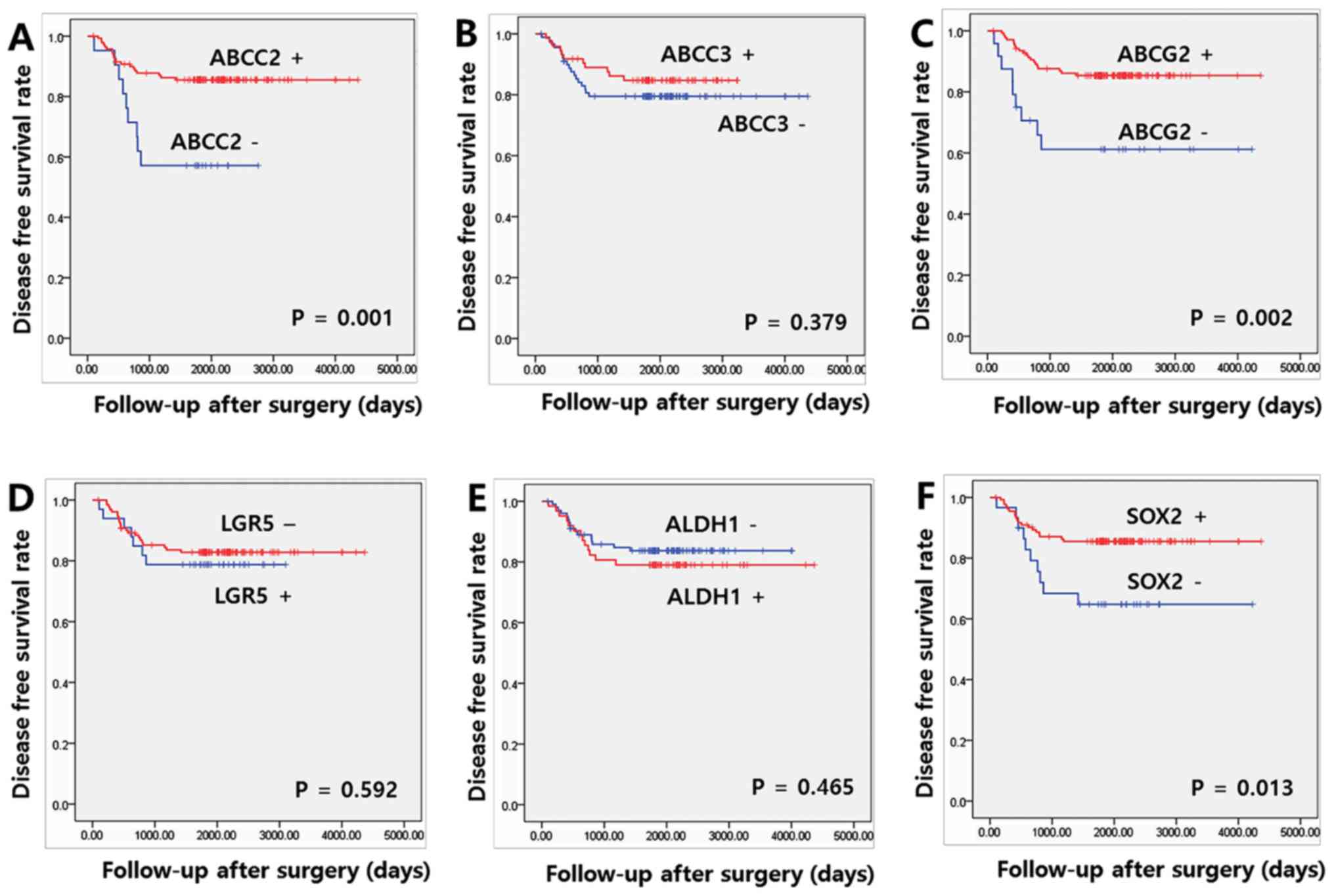 | Figure 3.Association between disease-free
survival rate and expression of cancer stem cell markers and ABC
transporters. Kaplan-Meier disease free survival curve for patients
with colon cancer according to (A) ABCC2, (B) ABCC3, (C) ABCG2, (D)
LGR5, (E) ALDH1 and (F) SOX2. ABCC2, ATP binding cassette subfamily
C member 2; ABCC3, ATP binding cassette subfamily C member 3;
ABCG2, ATP binding cassette subfamily G member 2; LGR5,
leucine-rich repeat containing G protein-coupled receptor 5; SOX2,
sex determining region Y-box 2; ALDH1, aldehyde dehydrogenase 1;
ABC, ATP-binding cassette. |
 | Table V.Multivariate analyses for
disease-free survival rate in patients with colon cancer. |
Table V.
Multivariate analyses for
disease-free survival rate in patients with colon cancer.
| Variable | HR | 95% CI | P-value |
|---|
| Perineural
invasion |
|
|
0.023a |
|
Absent | 1 |
|
|
|
Present | 2.465 | 1.129–5.380 |
|
| ABCC2 |
|
|
0.014a |
|
Negative | 2.831 | 1.238–6.474 |
|
|
Positive | 1 |
|
|
| ABCG2 |
|
| 0.063 |
|
Negative | 2.192 | 0.958–5.016 |
|
|
Positive | 1 |
|
|
| SOX2 |
|
|
0.020a |
|
Negative | 2.558 | 1.156–5.658 |
|
|
Positive | 1 |
|
|
Discussion
CSCs and ABC transporters have been proposed as
relevant prognostic biomarkers for outcomes and response to
chemotherapy (20–23). The aim of the present study was to
evaluate the potential use of CSC markers and ABC transporters as
prognostic biomarkers in patients with stage III CC who had
received the same adjuvant treatment, FOLFOX-4. It was indicated
that ABCC2, ABCG2 and SOX2 were independent favorable prognostic
markers in this CC cohort.
LGR5, expressed in the crypt base of the small and
large intestines, has received attention as a marker for normal
colon stem cells and colon CSCs (37). ALDH1, one of the common CSC markers,
has been indicated to endow tumor cells with chemoresistance, due
to its strong cellular detoxification activity (38,39). A
number of studies reported an association between the expression of
LGR5 or ALDH1 and patients' prognoses in various malignant tumor
types, including breast cancer and gastric cancer (32,40). In
patients with CC, an association between the expression of these
proteins in the tumor and an unfavorable prognosis has been
reported (21,22,27,33) and
a number of studies reported the same association in a CC cohort
treated with adjuvant or neoadjuvant chemo- or chemoradiation
treatment (26,27,41,42).
However, conflicting results have also been reported in malignant
tumor types of various organs, including the ovary and colorectum
(43–45), and in the present study, a prognostic
value for these proteins was not observed in patients with stage
III CC receiving adjuvant FOLFOX-4 treatment. SOX2, a transcription
factor that serves as a critical regulator of stem cell maintenance
and cell-fate decisions, is frequently used as a CSC marker in
various malignant tumor types, including skin squamous cell
carcinoma, bladder cancer and colorectal cancer (46–48).
Many studies reported that SOX2 could serve as a poor prognostic
marker in patients with various types of cancer, including rectum,
breast and oral cavity cancer (26,32,34).
However, contradictory results have been reported (49–51) and
in the present study, the expression of SOX2 indicated a favorable
prognosis in patients with stage III CC with adjuvant FOLFOX-4
chemotherapy. This may be due to another role of SOX2, as SOX2
decreases the expression levels of cyclin D1 and phosphorylated
retinoblastoma, and increases the expression levels of p27,
inducing cell-cycle arrest and apoptosis (52). Additionally, SOX2 directly
trans-activates phosphatase and tensin homolog in gastric cancer
(53). These results indicated that
the prognostic value of CSC markers in cancer may depend on the
types of cancer and their stage.
In the present study, ABCC2 was associated with a
prolonged DFS, and ABCG2 with prolonged DFS and OS. These results
were contradictory to our original hypothesis that expression of
ABC transporters may be associated with a reduced prognosis
following chemotherapy. This may be associated with role of ABCC2
and ABCG2 in phase II metabolism of platinum-based anticancer
agents (54). Limiting platinum-DNA
adduct formation by conjugation with sulfur-containing molecules,
including glutathione, is one of the major cellular mechanisms
involved in resistance against platinum-based anticancer agents,
including cisplatin or oxaliplatin (55). Sensitivity to platinum-based
anticancer agents is associated with cellular glutathione
concentration (55–58). ABCC2 is one of the glutathione
transporters, which exports glutathione outside the cell and
decreases the concentrations of glutathione (56). Theile et al (59) reported that 5-FU induces
overexpression of ABCC2 and proposed that upregulation of ABCC2 by
5-FU may favor the synergistic action of the drug combination in
the FOLFOX-4 regimen. Previous studies reported that ABCG2 is
associated with glutathione transport (60,61).
Krzyżanowski et al (60)
reported that the expression levels of glutathione were decreased
in cells that overexpressed ABCG2. Brechbuhl et al (61) reported that cells that overexpress
ABCG2 indicate an increase in basal extracellular glutathione
levels. Hlavata et al (24)
and Mirakhorli et al (25)
investigated the clinical implication of ABCC2 expression in a
small number of CC samples treated with a 5-FU containing regimen
and FOLFOX, respectively. Hlavata et al (24) reported no clinical significance for
the transcript level of ABCC2; however, Mirakhorli et al
(25) reported that the incidence of
metastasis or recurrence was not significantly reduced in the ABCC2
positive group, in accordance with the results of the present
study. In contrast, Lin et al (31) reported that high ABCG2 expression was
associated with resistance to palliative FOLFOX treatment in
patients with metastatic CC, indicating that the biological role of
ABC transporters in the chemoresponse may vary according to cancer
stage.
The expression of ABC transporters has been
indicated to be one of the factors that enhance the survival of
CSCs during chemotherapy and multiple ABC transporters, including
p-glycoprotein and ABCG2, have been identified in CSCs (14). The association between the expression
of CSC markers and the expression of ABC transporters, including
the associations between LGR5 and ABCC2, and SOX2 and ABCC3, was
examined in the present study, suggesting an association between
CSCs properties and ABC transporter expression.
The present study presents a limitation in that it
includes only retrospectively-collected cases. Further prospective
studies with larger cohorts are required, in order to confirm the
clinical use of these markers as prognostic marker for patients
with CC. It was indicated that the expression of SOX2, ABCC2 and
ABCG2 were associated with improved outcomes in patients with stage
III CC, who post-operatively received chemotherapy with the
FOLFOX-4 regimen. They may be beneficial prognostic markers in
patients with CC who have received adjuvant FOLFOX treatment and
promising candidate markers for a validation study on FOLFOX-4
therapy outcomes.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
This study was supported by grant no. 09-2014-004
from the Seoul National University Bundang Hospital Research Fund
(Seongnam, South Korea).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ES supervised the entire study, participated in
study design and coordination as well as the writing of the
manuscript. SHH and JWK made substantial contributions to the
acquisition, analysis, interpretation of data and writing of the
manuscript. MK, JHK and KWL performed acquisition of data, and BHK
and HK made substantial contributions to analysis of the data and
were involved in revising draft critically for important
intellectual content. HKO, DWK and SBK made substantial
contribution to case collection and data acquisition and revising
this article.
Ethics approval and consent to
participate
This study was approved by the Institutional Review
Board for Research Using Human Subjects at the Seoul National
University Bundang Hospital (IRB no. B1512-326/302). The present
study was exempt from obtaining written informed consent according
to the bioethics of our country because it was a retrospective
study, not expected to cause any harm, and the expected risk to the
patients was very low.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CC
|
colon cancer
|
|
5-FU
|
5-fluorouracil
|
|
CSC
|
cancer stem cell
|
|
TMA
|
tissue microarrays
|
|
IHC
|
immunohistochemical
|
|
DFS
|
disease-free survival rate
|
|
OS
|
overall survival rate
|
References
|
1
|
Ferlay J, Soerjomataram I, Dikshit R, Eser
S, Mathers C, Rebelo M, Parkin DM, Forman D and Bray F: Cancer
incidence and mortality worldwide: sources, methods and major
patterns in GLOBOCAN 2012. Int J Cancer. 136:E359–E386. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Haller DG, Catalano PJ, Macdonald JS,
O'Rourke MA, Frontiera MS, Jackson DV and Mayer RJ: Phase III study
of fluorouracil, leucovorin, and levamisole in high-risk stage II
and III colon cancer: final report of Intergroup 0089. J Clin
Oncol. 23:8671–8678. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Twelves C, Wong A, Nowacki MP, Abt M,
Burris H III, Carrato A, Cassidy J, Cervantes A, Fagerberg J,
Georgoulias V, et al: Capecitabine as adjuvant treatment for stage
III colon cancer. N Engl J Med. 352:2696–2704. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lembersky BC, Wieand HS, Petrelli NJ,
O'Connell MJ, Colangelo LH, Smith RE, Seay TE, Giguere JK, Marshall
ME, Jacobs AD, et al: Oral uracil and tegafur plus leucovorin
compared with intravenous fluorouracil and leucovorin in stage II
and III carcinoma of the colon: results from National Surgical
Adjuvant Breast and Bowel Project Protocol C-06. J Clin Oncol.
24:2059–2064. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
André T, Boni C, Mounedji-Boudiaf L,
Navarro M, Tabernero J, Hickish T, Topham C, Zaninelli M, Clingan
P, Bridgewater J, et al Multicenter International Study of
Oxaliplatin/5-Fluorouracil/Leucovorin in the Adjuvant Treatment of
Colon Cancer (MOSAIC) Investigators, : Oxaliplatin, fluorouracil,
and leucovorin as adjuvant treatment for colon cancer. N Engl J
Med. 350:2343–2351. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gramont A, Boni C, Navarro M, Tabernero J,
Hickish T, Topham C, Bonetti A, Clingan P, Marceau-Suissa J,
Lorenzato C and André T: Oxaliplatin/5FU/LV in the adjuvant
treatment of stage II and stage III colon cancer: efficacy results
with a median follow-up of 4 years. J Clin Oncol. 23 (Suppl
16):35012005. View Article : Google Scholar
|
|
7
|
Kuebler JP, Wieand HS, O'Connell MJ, Smith
RE, Colangelo LH, Yothers G, Petrelli NJ, Findlay MP, Seay TE,
Atkins JN, et al: Oxaliplatin combined with weekly bolus
fluorouracil and leucovorin as surgical adjuvant chemotherapy for
stage II and III colon cancer: results from NSABP C-07. J Clin
Oncol. 25:2198–2204. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Maenhaut C, Dumont JE, Roger PP and van
Staveren WC: Cancer stem cells: a reality, a myth, a fuzzy concept
or a misnomer? An analysis. Carcinogenesis. 31:149–158. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
O'Brien CA, Kreso A and Jamieson CH:
Cancer stem cells and self-renewal. Clin Cancer Res. 16:3113–3120.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Donnenberg VS and Donnenberg AD: Multiple
drug resistance in cancer revisited: the cancer stem cell
hypothesis. J Clin Pharmacol. 45:872–877. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dean M, Fojo T and Bates S: Tumour stem
cells and drug resistance. Nat Rev Cancer. 5:275–284. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dave B and Chang J: Treatment resistance
in stem cells and breast cancer. J Mammary Gland Biol Neoplasia.
14:79–82. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Crea F, Danesi R and Farrar WL: Cancer
stem cell epigenetics and chemoresistance. Epigenomics. 1:63–79.
2009. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Vinogradov S and Wei X: Cancer stem cells
and drug resistance: The potential of nanomedicine. Nanomedicine
(Lond). 7:597–615. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fábián A, Barok M, Vereb G and Szöllosi J:
Die hard: Are cancer stem cells the Bruce Willises of tumor
biology? Cytometry A. 75:67–74. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Moitra K, Lou H and Dean M: Multidrug
efflux pumps and cancer stem cells: Insights into multidrug
resistance and therapeutic development. Clin Pharmacol Ther.
89:491–502. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shervington A and Lu C: Expression of
multidrug resistance genes in normal and cancer stem cells. Cancer
Invest. 26:535–542. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gillet JP, Efferth T and Remacle J:
Chemotherapy-induced resistance by ATP-binding cassette transporter
genes. Biochim Biophys Acta. 1775:237–262. 2007.PubMed/NCBI
|
|
19
|
Li W, Zhang H, Assaraf YG, Zhao K, Xu X,
Xie J, Yang DH and Chen ZS: Overcoming ABC transporter-mediated
multidrug resistance: molecular mechanisms and novel therapeutic
drug strategies. Drug Resist Updat. 27:14–29. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Artells R, Moreno I, Díaz T, Martínez F,
Gel B, Navarro A, Ibeas R, Moreno J and Monzó M: Tumour CD133 mRNA
expression and clinical outcome in surgically resected colorectal
cancer patients. Eur J Cancer. 46:642–649. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kahlert C, Gaitzsch E, Steinert G, Mogler
C, Herpel E, Hoffmeister M, Jansen L, Benner A, Brenner H,
Chang-Claude J, et al: Expression analysis of aldehyde
dehydrogenase 1A1 (ALDH1A1) in colon and rectal cancer in
association with prognosis and response to chemotherapy. Ann Surg
Oncol. 19:4193–4201. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Liu Z, Dai W, Jiang L and Cheng Y:
Over-expression of LGR5 correlates with poor survival of colon
cancer in mice as well as in patients. Neoplasma. 61:177–185. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wang X, Xia B, Liang Y, Peng L, Wang Z,
Zhuo J, Wang W and Jiang B: Membranous ABCG2 expression in
colorectal cancer independently correlates with shortened patient
survival. Cancer Biomark. 13:81–88. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hlavata I, Mohelnikova-Duchonova B,
Vaclavikova R, Liska V, Pitule P, Novak P, Bruha J, Vycital O,
Holubec L, Treska V, et al: The role of ABC transporters in
progression and clinical outcome of colorectal cancer. Mutagenesis.
27:187–196. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mirakhorli M, Shayanfar N, Rahman SA,
Rosli R, Abdullah S and Khoshzaban A: Lack of association between
expression of MRP2 and early relapse of colorectal cancer in
patients receiving FOLFOX-4 chemotherapy. Oncol Lett. 4:893–897.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Saigusa S, Tanaka K, Toiyama Y, Yokoe T,
Okugawa Y, Ioue Y, Miki C and Kusunoki M: Correlation of CD133,
OCT4, and SOX2 in rectal cancer and their association with distant
recurrence after chemoradiotherapy. Ann Surg Oncol. 16:3488–3498.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hsu HC, Liu YS, Tseng KC, Hsu CL, Liang Y,
Yang TS, Chen JS, Tang RP, Chen SJ and Chen HC: Overexpression of
Lgr5 correlates with resistance to 5-FU-based chemotherapy in
colorectal cancer. Int J Colorectal Dis. 28:1535–1546. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hongo K, Tanaka J, Tsuno NH, Kawai K,
Nishikawa T, Shuno Y, Sasaki K, Kaneko M, Hiyoshi M, Sunami E, et
al: CD133(−) cells, derived from a single human colon cancer cell
line, are more resistant to 5-fluorouracil (FU) than CD133(+)
cells, dependent on the β1-integrin signaling. J Surg Res.
175:278–288. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Liu YS, Hsu HC, Tseng KC, Chen HC and Chen
SJ: Lgr5 promotes cancer stemness and confers chemoresistance
through ABCB1 in colorectal cancer. Biomed Pharmacother.
67:791–799. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Yu Z, Zhang C, Wang H, Xing J, Gong H, Yu
E, Zhang W, Zhang X, Cao G and Fu C: Multidrug
resistance-associated protein 3 confers resistance to
chemoradiotherapy for rectal cancer by regulating reactive oxygen
species and caspase-3-dependent apoptotic pathway. Cancer Lett.
353:182–193. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lin PC, Lin HH, Lin JK, Lin CC, Yang SH,
Li AF, Chen WS and Chang SC: Expression of ABCG2 associated with
tumor response in metastatic colorectal cancer patients receiving
first-line FOLFOX therapy-preliminary evidence. Int J Biol Markers.
28:182–186. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Shima H, Kutomi G, Satomi F, Maeda H,
Hirohashi Y, Hasegawa T, Mori M, Torigoe T and Takemasa I: SOX2 and
ALDH1 as predictors of operable breast cancer. Anticancer Res.
36:2945–2953. 2016.PubMed/NCBI
|
|
33
|
Chen J, Xia Q, Jiang B, Chang W, Yuan W,
Ma Z, Liu Z and Shu X: Prognostic value of cancer stem cell marker
ALDH1 expression in colorectal cancer: a systematic review and
meta-analysis. PLoS One. 10:e01451642015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yoshihama R, Yamaguchi K, Imajyo I, Mine
M, Hiyake N, Akimoto N, Kobayashi Y, Chigita S, Kumamaru W,
Kiyoshima T, et al: Expression levels of SOX2, KLF4 and brachyury
transcription factors are associated with metastasis and poor
prognosis in oral squamous cell carcinoma. Oncol Lett.
11:1435–1446. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Amin MB, Edge S, Greene F, Byrd DR,
Brookland RK, Washington MK, Gershenwald JE, Compton CC, Hess KR,
Sullivan DC, et al: AJCC cancer staging manual. 8th. Springer; New
York: 2017, View Article : Google Scholar
|
|
36
|
U.S. Department of Health Human Services,
National Institutes of Health, National Cancer Institute, . Comom
Terminology Criteria for Adverse Events (CTCAE). Version 4.0, 2009.
https://www.eortc.be/services/doc/ctc/ctcae_4.03_2010-06-14_quickreference_5×7.pdfMay
28–2009
|
|
37
|
Huang EH and Wicha MS: Colon cancer stem
cells: Implications for prevention and therapy. Trends Mol Med.
14:503–509. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Yoshida A, Rzhetsky A, Hsu LC and Chang C:
Human aldehyde dehydrogenase gene family. Eur J Biochem.
251:549–557. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Sophos NA and Vasiliou V: Aldehyde
dehydrogenase gene superfamily: the 2002 update. Chem Biol
Interact. 143-144:5–22. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Yamanoi K, Fukuma M, Uchida H, Kushima R,
Yamazaki K, Katai H, Kanai Y and Sakamoto M: Overexpression of
leucine-rich repeat-containing G protein-coupled receptor 5 in
gastric cancer. Pathol Int. 63:13–19. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Avoranta ST, Korkeila EA, Ristamäki RH,
Syrjänen KJ, Carpén OM, Pyrhönen SO and Sundström JT: ALDH1
expression indicates chemotherapy resistance and poor outcome in
node-negative rectal cancer. Hum Pathol. 44:966–974. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Saigusa S, Inoue Y, Tanaka K, Toiyama Y,
Kawamura M, Okugawa Y, Okigami M, Hiro J, Uchida K, Mohri Y, et al:
Significant correlation between LKB1 and LGR5 gene expression and
the association with poor recurrence-free survival in rectal cancer
after preoperative chemoradiotherapy. J Cancer Res Clin Oncol.
139:131–138. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Lugli A, Iezzi G, Hostettler I, Muraro MG,
Mele V, Tornillo L, Carafa V, Spagnoli G, Terracciano L and Zlobec
I: Prognostic impact of the expression of putative cancer stem cell
markers CD133, CD166, CD44s, EpCAM, and ALDH1 in colorectal cancer.
Br J Cancer. 103:382–390. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Tomita H, Tanaka K, Tanaka T and Hara A:
Aldehyde dehydrogenase 1A1 in stem cells and cancer. Oncotarget.
7:11018–11032. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Chang B, Liu G, Xue F, Rosen DG, Xiao L,
Wang X and Liu J: ALDH1 expression correlates with favorable
prognosis in ovarian cancers. Modern pathology: An official journal
of the United States and Canadian Academy of Pathology. Inc.
22:817–823. 2009.
|
|
46
|
Boumahdi S, Driessens G, Lapouge G, Rorive
S, Nassar D, Le Mercier M, Delatte B, Caauwe A, Lenglez S, Nkusi E,
et al: SOX2 controls tumour initiation and cancer stem-cell
functions in squamous-cell carcinoma. Nature. 511:246–250. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Zhu F, Qian W, Zhang H, Liang Y, Wu M,
Zhang Y, Zhang X, Gao Q and Li Y: SOX2 is a marker for stem-like
tumor cells in bladder cancer. Stem Cell Reports. 9:429–437. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Amini S, Fathi F, Mobalegi J,
Sofimajidpour H and Ghadimi T: The expressions of stem cell
markers: Oct4, Nanog, Sox2, nucleostemin, Bmi, Zfx, Tcl1, Tbx3,
Dppa4, and Esrrb in bladder, colon, and prostate cancer, and
certain cancer cell lines. Anat Cell Biol. 47:1–11. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Zhang X, Yu H, Yang Y, Zhu R, Bai J, Peng
Z, He Y, Chen L, Chen W, Fang D, et al: SOX2 in gastric carcinoma,
but not Hath1, is related to patients' clinicopathological features
and prognosis. J Gastrointest Surg. 14:1220–1226. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Kim BW, Cho H, Choi CH, Ylaya K, Chung JY,
Kim JH and Hewitt SM: Clinical significance of OCT4 and SOX2
protein expression in cervical cancer. BMC Cancer. 15:10152015.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Zheng S, Pan Y, Wang R, Li Y, Cheng C,
Shen X, Li B, Zheng D, Sun Y and Chen H: SOX2 expression is
associated with FGFR fusion genes and predicts favorable outcome in
lung squamous cell carcinomas. Onco Targets Ther. 8:3009–3016.
2015.PubMed/NCBI
|
|
52
|
Otsubo T, Akiyama Y, Yanagihara K and
Yuasa Y: SOX2 is frequently downregulated in gastric cancers and
inhibits cell growth through cell-cycle arrest and apoptosis. Br J
Cancer. 98:824–831. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Wang S, Tie J, Wang R, Hu F, Gao L, Wang
W, Wang L, Li Z, Hu S, Tang S, et al: SOX2, a predictor of survival
in gastric cancer, inhibits cell proliferation and metastasis by
regulating PTEN. Cancer Lett. 358:210–219. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Croom E: Metabolism of xenobiotics of
human environments. Prog Mol Biol Transl Sci. 112:31–88. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Burger H, Loos WJ, Eechoute K, Verweij J,
Mathijssen RH and Wiemer EA: Drug transporters of platinum-based
anticancer agents and their clinical significance. Drug Resist
Updat. 14:22–34. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Ballatori N, Hammond CL, Cunningham JB,
Krance SM and Marchan R: Molecular mechanisms of reduced
glutathione transport: Role of the MRP/CFTR/ABCC and OATP/SLC21A
families of membrane proteins. Toxicol Appl Pharmacol. 204:238–255.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
El-akawi Z, Abu-hadid M, Perez R, Glavy J,
Zdanowicz J, Creaven PJ and Pendyala L: Altered glutathione
metabolism in oxaliplatin resistant ovarian carcinoma cells. Cancer
Lett. 105:5–14. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Smitherman PK, Townsend AJ, Kute TE and
Morrow CS: Role of multidrug resistance protein 2 (MRP2, ABCC2) in
alkylating agent detoxification: MRP2 potentiates glutathione
S-transferase A1-1-mediated resistance to chlorambucil
cytotoxicity. J Pharmacol Exp Ther. 308:260–267. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Theile D, Grebhardt S, Haefeli WE and
Weiss J: Involvement of drug transporters in the synergistic action
of FOLFOX combination chemotherapy. Biochem Pharmacol.
78:1366–1373. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Krzyżanowski D, Bartosz G and Grzelak A:
Collateral sensitivity: ABCG2-overexpressing cells are more
vulnerable to oxidative stress. Free Radic Biol Med. 76:47–52.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Brechbuhl HM, Gould N, Kachadourian R,
Riekhof WR, Voelker DR and Day BJ: Glutathione transport is a
unique function of the ATP-binding cassette protein ABCG2. J Biol
Chem. 285:16582–16587. 2010. View Article : Google Scholar : PubMed/NCBI
|