Introduction
Caveolae are small bulb-like invaginations (50–80 nm
in diameter) in the plasma membrane, with a diverse array of signal
transduction functions (1–3). Functioning as a signal-transducing
platform, caveolae are actively involved in the transcellular
transport of ligands and receptor molecules, forming a specialized
transporting system that maintains the lipid content of plasma
membranes via transcytosis (4).
Caveolae have been implicated as crucial entities for cell-cell
communication via the endocytosis of signaling molecules, in
addition to their role as signaling platforms where membrane
receptors, including G-protein-coupled receptors, reside. Disrupted
signaling through key caveolar proteins results in various
pathologies, including cardiomuscular diseases, lipodystrophy, and,
most importantly, cancer (5).
Caveolar proteins exert their dynamic role in maintaining cell
growth, cell protection and overall cell function (6). Caveolae consist of complexes comprising
different transmembrane proteins, including caveolin, cavin,
dynamin-2, EH-domain containing 2 protein and protein kinase C and
casein kinase substrate in neurons protein 2, among which caveolins
are the core functional proteins (7). Cavins and caveolins (1–3) are the
fundamental proteins that mediate caveolar organization. Caveolins
provide a signaling platform for the coordination and interaction
of different growth factor receptors, protein kinases and various
intracellular signaling molecules (8). Dynamin-2, the product of the dynamin 2
(DNM2) gene, is a GTPase that directly interacts with
caveolin-1, the product of the caveolin-1 (Cav-1) gene,
mediating membrane scission, leading to endosome formation
(9). Caveolin-1 and dynamin-2 are
the key regulators of clathrin-independent endocytosis (10).
Among the caveolin proteins, caveolin-1 (molecular
mass, ~21 kDa) is known to be a key protein of the caveolae complex
that has an important role in maintaining cell metabolism,
anchorage-dependent growth, motility and signaling, and the
cellular microenvironment (11). In
fulfilling these crucial roles in cell growth and maintenance, the
altered expression and function of caveolin-1 is associated with
oncogenic cell transformation, cell metastasis, invasion and
tumorigenesis. Enhanced expression of Cav-1 promotes tumor
growth and invasion, resulting in the metastasis of human breast
cancer cells (12). Knockdown of
Cav-1 was demonstrated to inhibit tumor growth and
metastasis (13). Dynamin-2
(molecular mass ~100 kDa) is a GTPase that is actively involved in
membrane fission during the endocytosis of cell-surface receptors
and signaling molecules. The endosomes, also termed ‘caveosomes’,
thus formed are continually recycled to the cell surface (14). This mechanism of protein expression
on the cell membrane is disrupted in cancer cells. Dynamin-2
protein dysfunction results in the dysregulation of endosome
recycling, causing an imbalanced expression of regulatory growth
factor receptors, including epidermal growth factor receptor, on
the cell surface, promoting aberrant cell growth, invasion and
proliferation (15). Overexpression
of Cav-1 and DNM2 has been demonstrated to be
involved in cell lines of various types of cancer, including
pancreatic, colon, lung, breast and prostate cancer (13,16–22).
Bladder cancer is the ninth most common cancer
worldwide. Of all incident cases of different types of cancer in
the Pakistani population during the year 2012 (n=148,041), the
incidence rate of bladder cancer in the male population was 3,020,
which was increased compared with that in the female population
(n=946) (23). In muscle-invasive
bladder cancers, 58 genetic mutations have been demonstrated to be
causative factors for cancer progression in the bladder, and these
are associated with low survival rates (24). There are a number of genetic
alterations associated with bladder cancer progression.
Overexpression, and genetic mutation, of several different genes
that are critical in cell cycle regulation, apoptosis, signal
transduction and angiogenesis have been identified, among which
mutants of tumor protein (p53), fibroblast growth factor 3, Janus
kinase/signal transducers and activator of transcription,
hypoxia-inducible factor, retinoblastoma protein 1, HRas
proto-oncogene, GTPase (also known as transforming protein p21),
tuberous sclerosis 1, telomerase reverse transcriptase, and
ubiquitin carboxyl-terminal hydrolase BAP1 have been identified and
studied (24–26). Furthermore, numerous other previously
identified genetic alterations are associated with a poor
prognostic outcome, and these are currently undergoing validation
(27). Regulatory genes that are
involved in cell cycle regulation and apoptosis have been validated
as combined prognostic markers for bladder cancer, although these
are under investigation for use as single markers associated with
urothelial carcinoma (28). However,
genes/proteins that are involved in cell surface communication with
the extracellular environment, cell-to-cell communication,
endocytosis, and exocytosis are far more susceptible to cancer
development compared with intercellular proteins, particularly
caveolar proteins (29). The
upregulation of caveolar proteins has been demonstrated for various
different types of cancer, whereas only a few cancer types have
been associated with their downregulation (30,31).
Despite the contradictory roles identified for caveolin-1 in
different types of cancer, overexpression of Cav-1 has been
described for the majority of human cancer types. Previous studies
investigating the overall clinical value of Cav-1, and its
association with tumor aggressiveness, size, stage, grade and
differentiation, suggest that it may serve as a good candidate
prognostic marker for a majority of cancer types, including bladder
cancer (32,33). By contrast, the gene expression of
DNM2, and its association with cancer progression, has yet
to be fully investigated. However, the identification and
validation of the prognostic panel of disease markers for bladder
cancer is required. A number of studies have explored the
expression profiling of bladder cancer in humans, in which genome
coding sequences were decoded for evaluating genetic alterations
associated with the disease, and subsequently, the prognostic
marker panel could be selected. However, one disadvantage in terms
of ensuring its reproducibility is that this widely applied
approach is highly expensive (34–36).
Bladder cancer, based on its metastatic ability to
spread to other parts of the body, is divided into 4 stages (stages
I–IV) according to the tumor-node-metastasis (TNM) staging system
(37). Physiologically, bladder
tumors are essentially categorized into 2 grades: Low-grade
papillary urothelial carcinoma and high-grade papillary urothelial
carcinoma, according to the World Health Organization/International
Society of Urological Pathology classification system, published in
2004 (38). Previous studies have
demonstrated altered expression levels of Cav-1 and
DNM2 in bladder cancer cell lines (33,39–41).
Therefore, the present study aimed to investigate the degree of
correlation of gene expression in comparing between the
Cav-1 and DNM2 genes in bladder cancer tumor samples,
specifically with respect to the progressiveness of the tumors. The
results obtained revealed that the significant correlation between
the overexpression of Cav-1 and DNM2 in bladder
tumors was critical for cancer development, and for tumor stage and
grade progression. The overexpression of these 2 genes could be
considered clinically relevant and may prove as candidate risk
factors for bladder cancer progression.
Materials and methods
Tumor sampling
The present study was approved by the Ethical Review
Board of COMSATS University Islamabad (Islamabad, Pakistan;
approval no. CIIT/Bio/ERB/18/76). Samples were collected between
July, 2015 and March 2017. Tumor and normal tissue samples were
excised from patients with bladder cancer post-surgery, following
transurethral resection of bladder tumor (TURBT) surgery. Signed
written consent was obtained from all the patients involved in the
present study (n=66; male=47; female=19). The patients' age ranged
between 30 and 65 years and the median age was 43 years. The
histopathological histories of the patients were confirmed by the
Pathology Laboratory, Pakistan Institute of Medical Science (PIMS)
(Islamabad, Pakistan) and Shifa International Hospital (Islamabad,
Pakistan). Paired samples of tumors with their adjacent normal
tissues were obtained. Normal tissue samples were used as controls.
The tumor staging and grading was assessed by the team of
urologists at Pathology Laboratory, Department of Urology, PIMS.
The TNM system of staging was applied for evaluation of the tumor
stage. The revised guidelines by National Comprehensive Cancer
Network (NCCN) Clinical Practice Guidelines in Oncology (NCCN
Guidelines®) for Bladder Cancer and American Society of
Clinical Oncology (ACSO) 2015–2018 were followed during grading and
staging of tumor samples (42).
Reverse transcription quantitative
polymerase chain reaction (RT-qPCR)
Tissues extracted from the patients were stored in
RNAlater® (Ambion; Thermo Fisher Scientific, Inc.) at
4°C in a refrigerator. RNA extraction was performed using
TRIzol® (Invitrogen; Thermo Fisher Scientific, Inc.)
reagent according to the manufacturer's protocol (43). Subsequently, cDNA synthesis was
performed, followed by RNA quantification. The minimum
concentration of RNA used in these experiments was 1–2 µg for cDNA
synthesis. Thermo Scientific RevertAid First Strand cDNA Synthesis
kit was used for cDNA synthesis (Thermo Fisher Scientific, Inc.),
according to the manufacturer's protocols. The PrimerQuest tool
(Integrated DNA Technologies, Inc.) was used to design the primers,
which were subsequently altered manually to meet the required
specifications for RT-qPCR. The forward primer for Cav-1
(NM_001753.4) was designed to span exon 2 and the junction with
exon 3, and the reverse primer was selected from exon 3, whereas
the primer set for DNM2 (NM_001005360.2) was designed based
on the intron flanking exons 6 and 7 (Table I). Tubulin 3 was used as an
endogenous marker for evaluating changes in the expression levels
of Cav-1 and DNM2. In silico PCR (University
of California Santa Cruz) was performed to ensure amplification of
the 2 target genes. RT-qPCR using the Applied Biosystems™
StepOnePlus™ RealTime PCR system (Applied Biosystems, Inc.; Thermo
Fisher Scientific, Inc.) was performed for the Cav-1 and
DNM2 genes under standard conditions, as specified by the
protocol. The concentration of cDNA was rounded up to 2 µg/µl for
each sample, and the total volume per reaction was adjusted to 25
µl with SYBR™ Green Master mix (Maxima Syber Green/ROX qPCR Master
mix; Thermo Fisher Scientific, Inc.). The RT-qPCR conditions
consisted of an initial incubation at 95°C for 10 min, followed by
40 cycles of denaturation at 95°C for 30 sec, an annealing with
primer at 57°C for 30 sec and extension at 72°C for 30 sec. Final
extension was performed at 72°C for 10 min.
 | Table I.Primer sequence used for reverse
transcription quantitative polymerase chain reaction analysis. |
Table I.
Primer sequence used for reverse
transcription quantitative polymerase chain reaction analysis.
| Transcript | Forward primer | Reverse primer | Length, bp | Primer location
GRCh38.p12 |
|---|
| Cav-1 | GACGTGGTCAAGAT | GACGAAATACTGGT | 120 | (Chr7:
116526678..116526689//116558946-116558956) |
| (NM_001753.4) | TGACTTGA | TTTACCG |
| (Chr7:
116559032-116559053) |
| DNM2 | GCATGGGCACGCCA | GCTGCTGTCCCTGG | 119 | (Chr19:
10783083-10783102) |
|
(NM_001005360.2) | CATCTG | AGAAGGAG |
| (Chr19:
10786623-10786644) |
Gene expression analysis
The relative expression levels of Cav-1 and
DNM2 were calculated using the 2−ΔΔCq method
(44). Using TUBB3 as the
control reference gene (45),
relative differences in gene expression were obtained in terms of
the fold increase in expression. To obtain the expression data, the
Cq values of the Cav-1 and DNM2 genes were
normalized against the Cq value for endogenous
TUBB3.
Statistical analysis
Statistical analyses were performed using GraphPad
Prism 6 (GraphPad Software, Inc.) and OriginPro 2017 (OriginLab
Corporation) software. Contingencies of the patients' data were
determined using Fisher's exact two-tailed test, and the
correlation between the gene expression patterns was assessed using
Pearson's correlation coefficient test. Depending on the
experiment, the statistical significance of the resulting data was
determined using either the Wilcoxon test or one way analysis of
variance followed by the Tukey's honest significant difference
post-hoc test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Tumor histopathology
Tumor staging was evaluated by the Pathology
Laboratory of PIMS, according to the TNM system but incorporating
the revisions of the NCCN Clinical Practice Guidelines in Oncology
(NCCN Guidelines®) for Bladder Cancer and ACSO 2015–2018
(42). Distribution of the tumor
grade and stage data by sex and age groups was statistically
analyzed (Table II). In October
2017, The Cancer Genome Atlas (TCGA) published the prevalence and
incidence rates of bladder cancer (https://cancergenome.nih.gov/newsevents/newsannouncements/bladder-cancer_2017),
which was increased in the male population compared with females,
and, in terms of underlying causes, smoking was demonstrated to be
the major factor in that study (46). A comprehensive molecular
characterization study was also performed by TCGA research network,
which described the genetic alterations associated with bladder
cancer (24). In the present study,
a significant difference was identified in terms of the pathology
between the sexes in the different age groups (P=0.0024; Table II). A number of different diseases
were identified in patients from both age groups, but their
associations with bladder cancer were not statistically
significant. Conversely, the risk factors of active smoking
(P=0.0135) and passive smoking (P=0.0316) were identified to be
significantly associated with bladder cancer (Table III).
 | Table II.Tumor stage and grade data
distribution by sex and age. |
Table II.
Tumor stage and grade data
distribution by sex and age.
|
| Age groups,
years |
|
|---|
|
|
|
|
|---|
| Patient data | ≤50 | >50 | P-value |
|---|
| Sex |
|
|
|
|
Male | 32 | 15 | 0.0024a |
|
Female | 12 | 7 |
|
| Histology (%) |
|
|
|
| Tumor
grade |
|
|
|
|
High | 20 (45.4) | 12 (55.0) | 0.6032 |
|
Low | 24 (55.0) | 10 (45.4) |
|
| Tumor
stage |
|
|
|
|
Stage I |
|
|
|
|
Male | 16 (50.0) | 4
(27.1) | 0.0235a |
|
Female | 1
(8.3) | 4
(57.1) |
|
| Stage
II |
|
|
|
|
Male | 12 (38) | 2
(13.3) | 0.0441a |
|
Female | 1
(8.3) | 3
(42) |
|
| Stage
III (%) |
|
|
|
|
Male | 4
(12.5) | 9
(60.0) | 0.0116a |
|
Female | 10 (84.0) | 0
(0.0) |
|
 | Table III.Disease history and smoking habits in
bladder cancer. |
Table III.
Disease history and smoking habits in
bladder cancer.
|
| Age groups,
years |
|
|---|
|
|
|
|
|---|
| Patient data | ≤50 | >50 | P-value |
|---|
| Sex |
|
|
|
|
Male | 32 | 15 | 0.0024b |
|
Female | 12 | 7 |
|
| Previous disease
history (%) |
|
|
|
|
Hypertension |
|
|
|
|
Male | 3
(9.4) | 12 (80.0) | 0.3781 |
|
Female | 4
(33.3) | 6
(85.7) |
|
|
Diabetes mellitus |
|
|
|
|
Male | 5
(16.0) | 7
(47.0) | 0.6668 |
|
Female | 3
(25.0) | 5
(71.4) |
|
| Urinary
tract infections |
|
|
|
|
Male | 4
(12.5) | 5
(33.3) | 0.6563 |
|
Female | 6
(50.0) | 4
(57.1) |
|
| Family bladder
cancer history |
|
|
|
|
Male | 4
(12.5) | 5
(33.3) | 0.4909 |
|
Female | 0
(0.0) | 2
(29.0) |
|
| Smoking |
|
|
|
|
Male | 22 (68.7) | 14 (93.3) | 0.6327 |
|
Female | 2
(16.6) | 5
(71.4) |
|
|
Actively smoking | 24 (55.0) | 19 (86.3) | 0.0135b |
|
Non-smoking | 20 (45.4) | 3
(14.0) |
|
|
Smoke-free
environmenta | 15 (75.0) | 0
(0.0) | 0.0316b |
| Passive
smoking | 5
(25.0) | 3
(100.0) |
|
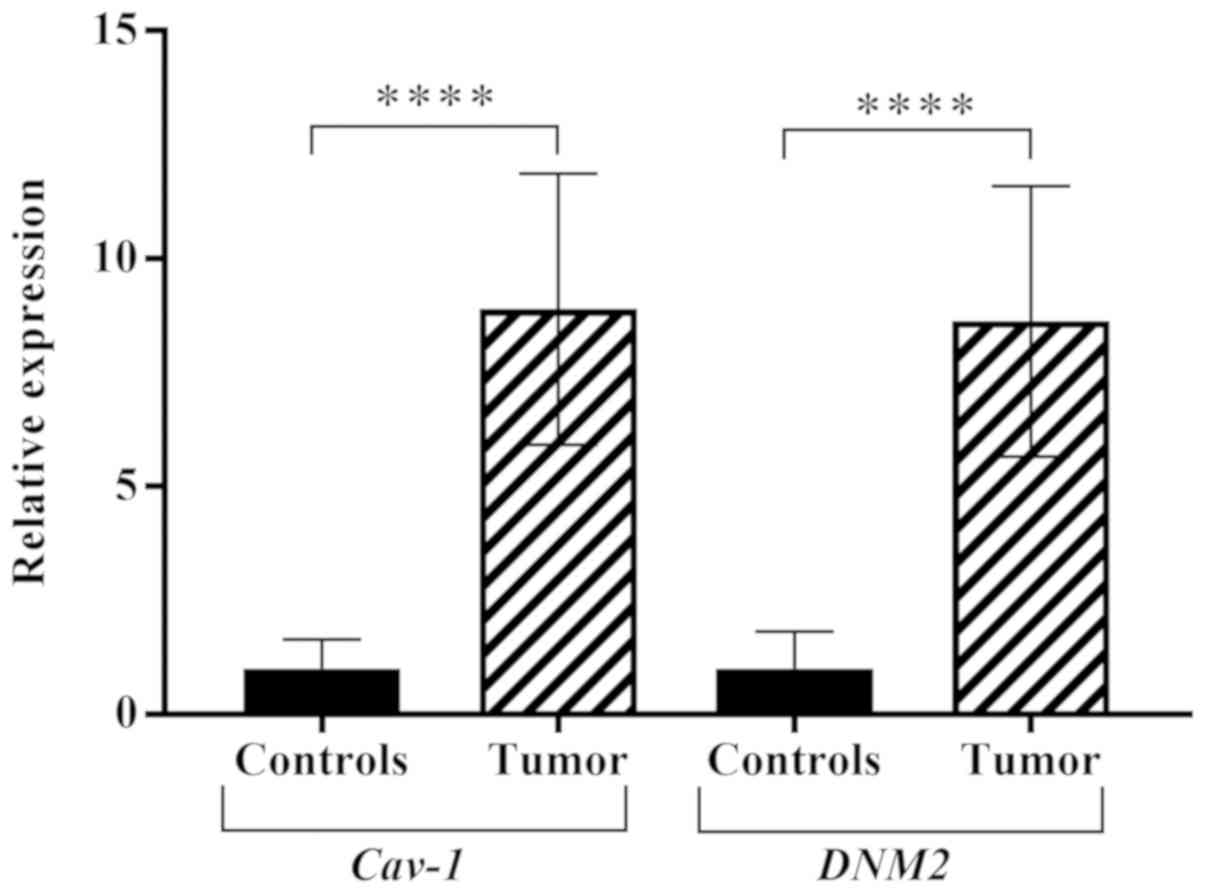
Cav-1 and DNM2 expression
In the tumor samples, the expression levels of
Cav-1 and DNM2 were experimentally analyzed using
RT-qPCR. The expression of Cav-1 in the tumor samples was
increased by 8.88-fold overall compared with the normal tissues.
Similarly, the expression level of DNM2 was also increased
by 8.6-fold compared with the normal adjacent, or control, tissues
(P<0.001). As demonstrated in Fig.
1, boxplots of normalized (mean ± standard error of the mean)
gene expression of Cav-1 and DNM2 revealed a
significant increase in gene expression in tumor tissues compared
with the adjacent normal tissue. Previous studies also demonstrated
increased expression levels of Cav-1 and DNM2 in
different cancer cell lines (39,41). The
genes exhibited enhanced expression levels in bladder tumor samples
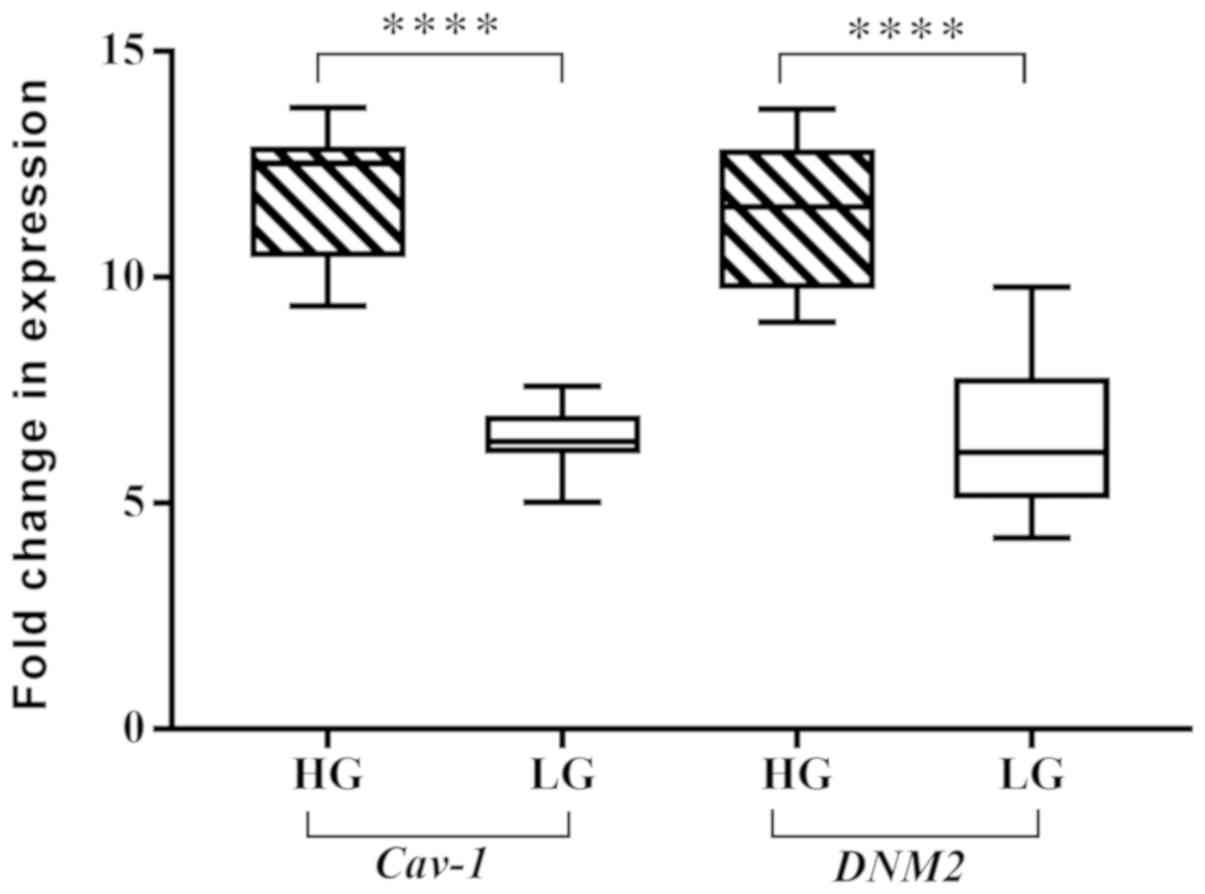
concomitantly with the progression of cancer. A significant
difference in expression levels was observed comparing between low-
and high-grade tumors (P<0.0001; Fig.
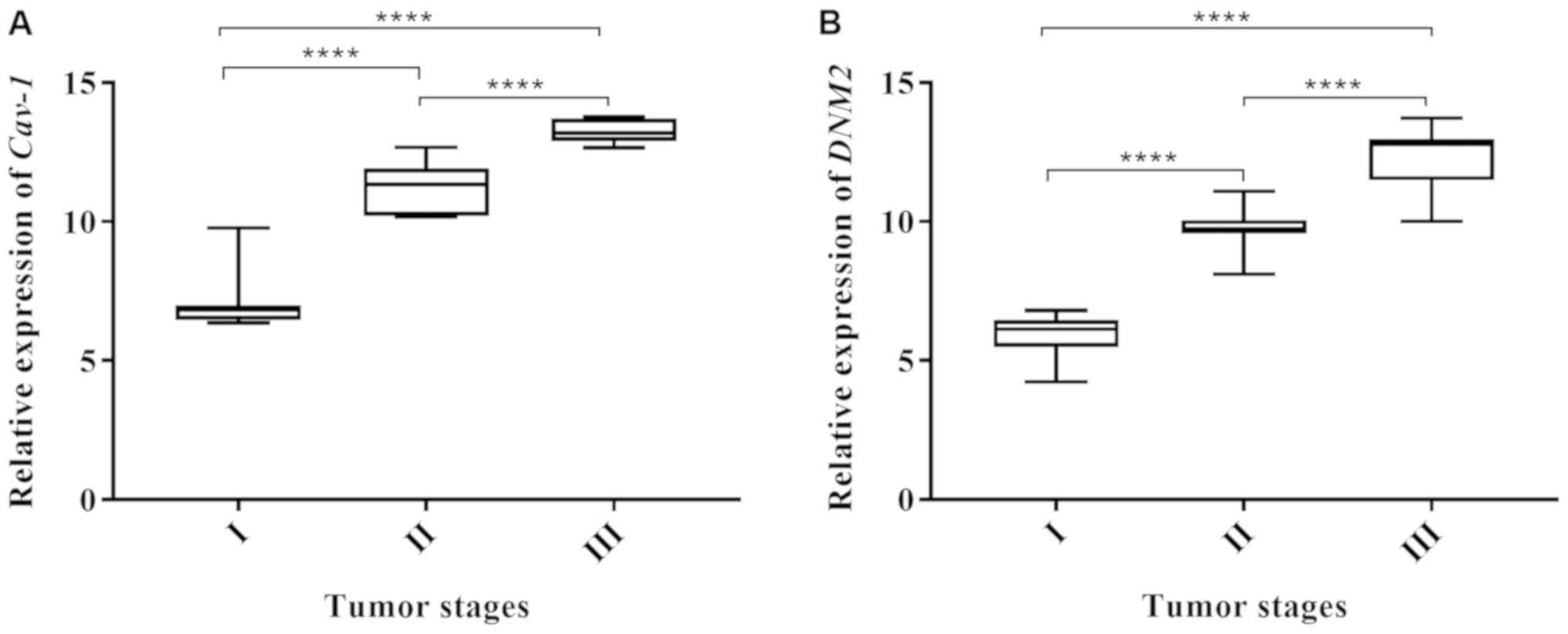
2). A similar trend was also observed with respect to the
cancer stages. Alterations in Cav-1 and DNM2
expression were revealed to be associated with the cancer stage, as
indicated in Fig. 3A and B. These
results demonstrated that the expression levels of the two genes
increased concomitantly with the development of higher disease
stages. However, highly significant differences in the expression
of Cav-1 and DNM2 were observed when stage I tumors were compared
with stage II tumors (P<0.0001), and when stage II tissues were
compared with stage III samples (P<0.0001). A similar difference
was also identified when comparing stage I tumors with stage III
tumors (P<0.0001; Fig 3A and
B).
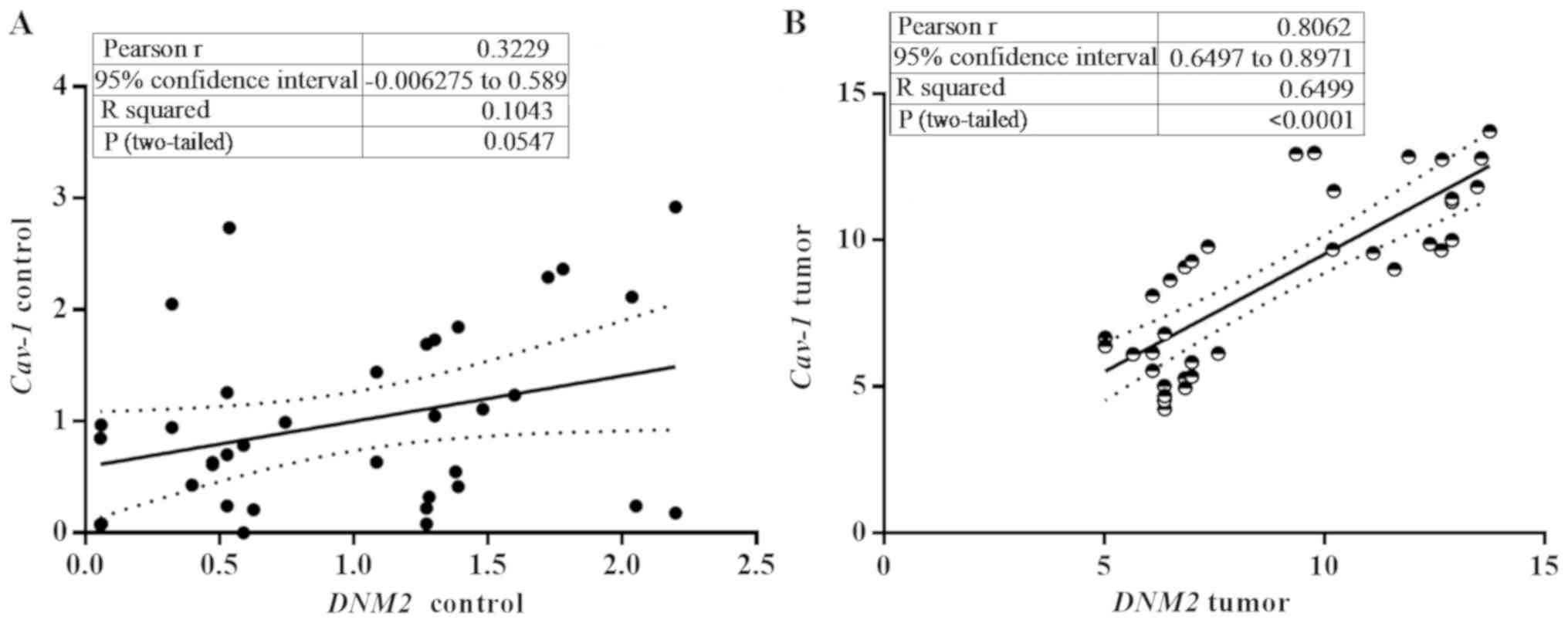
Correlation between Cav-1 and
DNM2
The Cav-1 and DNM2 genes serve an
important role in the functionality of clathrin-independent
endocytosis. Altered expression levels of the genes has been
demonstrated to be associated with pathological outcomes (32,47). In
the present study, the expression of Cav-1 was clearly
correlated with the expression of DNM2 (P<0.0001;
Pearson's coefficient, r=0.8617; Fig. 4A
and B). The segregation of DMN1/Cav-1 correlation data into two
clusters additionally confirmed the increased expression of the 2
genes in high-grade tumors compared with low-grade tumors
demonstrated in Fig. 2.
Discussion
Cav-1 is a key component of caveolae in terms
of their formation, arrangement and function. Together with
DNM2, Cav-1 initiates the process of endocytosis (32). Cav-1 has been demonstrated to
be a critical component of numerous types of cancer, including
breast, lung, colorectal, cervical and pancreatic cancer (21,48–50).
Previous studies have presented accumulating evidence revealing
that cancer cells are prone to modifying the microenvironment of
the tumor, inducing the adjacent cells to become malignant
(51–54). In this regard, Cav-1 is
implicated as an important protein that affects the metabolic
activity of cells during cancer progression (55). The results of the present study
revealed a progressive increase in the expression level of
Cav-1 concomitant with the higher stages of bladder cancer.
As the stage of bladder cancer progresses, cells that are cancerous
maintain their survival by utilizing key proteins that provide them
with the necessarily favorable environment to grow, invade and
migrate via regulating the respective functional proteins.
Increased expression levels of Cav-1 in higher grades of
bladder cancer enable an increased potential of the cells to invade
and proliferate (56). Therefore, in
the present study, the high-grade tumors were revealed to have
comparatively enhanced expression levels of Cav-1 compared
with low-grade tumors.
Altered expression of DNM2 also serves a role
in cancer progression. DNM2 has been implicated as a
therapeutic target for cervical cancer: In Hela cells, dynamin-2
inhibitors have been demonstrated to cause decreased migration and
invasion via decreasing the expression of matrix metallopeptidase
9, thereby lowering the rate of cell proliferation (57). Similar to Cav-1, an increase
in the expression of DNM2 has been demonstrated to
correspond to advances in the tumor stage (19). In the present study, the expression
levels of DNM2 and Cav-1 genes exhibited a marked
correlation with the progression of bladder tumor stage. These
results demonstrated that an increase in the expression of these 2
genes may stimulate the tumors to proliferate, invade and
metastasize to different adjacent organs. Cancer cells have their
own modified microenvironment through which they communicate with
adjacent cells for growth proliferation and survival (5).
Summarizing what is known concerning cancer
progression, cellular communication is the hallmark of
tumorigenesis. Interactions with signaling molecules provide a
major focus for disrupted signaling. Cav-1, being a key
protein of the caveolae, is critical for cancer development, as it
directly interacts with signaling proteins, including
phosphoinositide 3-kinase, Src, phospholipases, extracellular
signal-regulated kinase, G-proteins, endothelial nitric oxide
synthase, adenylyl cyclase, protein kinase C, p53 and cell division
control protein 42 homolog, and is involved in signal transduction
cascades (13,58,59).
Dysfunction of Cav-1, resulting from the aberrant expression
of the gene, triggers the activation of various growth-promoting
pathways (4,11). Previous studies have suggested
overexpression of Cav-1 to be a cause of cancer progression
(32,60,61).
Similarly, together with Cav-1, DNM2 also mediates effects
on cancer formation and progression. The 2 proteins are involved in
the endocytosis of a number of receptor proteins, ligands and
signaling molecules (19,62). However, it has been suggested that
there are several other interlinked signaling pathways that, in
response to overexpression of Cav-1 and DNM2, may be
activated and/or deactivated, resulting in tumor formation
(63).
Although the present study has described the genetic
expression of the target genes, there were several limitations.
Firstly, the samples were not obtained from stages 0a and 0is, the
2 preliminary stages of bladder cancer, or the final stage, stage
IV, as patients are not subjected to TURBT at the initial or the
last stages of disease. Consequently, all the patients within the
study cohort were diagnosed with mid-stage disease, for which TURBT
surgery is available. There is an urgent requirement for diagnoses
of bladder cancer at early stages. The target genes selected for
the present study may be considered as good prognostic marker for
bladder cancer. If bladder tumor samples from the initial to the
final stages had been available for analysis, then the differences
in expression of the target genes in the tumor samples could have
been validated more comprehensively. Future studies will aim to
investigate the protein expression of the target genes in bladder
tumor samples, and to explore the functional disruptions due to
overexpression of the target genes/proteins that may have caused
tumor aggressiveness during cancer progression. In the present
study, the observed association of the increased expression levels
of Cav-1 and DNM2 with advancing tumor stage could be
considered as a risk factor for bladder cancer, which may
additionally aid tumor and disease prognosis, and provide
potentially novel treatment options.
Acknowledgements
Not applicable.
Funding
The present study was supported by the COMSATS
Research Grant Program (grant no. 16/54/CRGP/CIIT/IBD/15/791) by
COMSATS University Islamabad.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
SAR was responsible for conception and design of the
study, performed the data analysis and its interpretation, and
prepared the manuscript. STAS refined the research design, and
performed data analysis and interpretation. KS assisted with the
experimental protocols and data acquisition. AY, AK, MN and AM
evaluated the tumor samples and prepared the histopathological
reports of the tumors. AT and NB contributed towards the research
design, and secured collaborations with the hospitals from which
the samples were obtained. MJK and AH also assisted with the
conception of the study, and with research supervision.
Ethics approval and consent to
participate
The study was approved by the ethical review board
of COMSATS Institute of Information Technology (approval no.
CIIT/Bio/ERB/18/76). Written signed consent was obtained from the
patients involved.
Patient consent for publication
Written signed consent was obtained from the
patients involved.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bastiani M and Parton RG: Caveolae at a
glance. J Cell Sci. 123:3831–3836. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Anderson RG: The Caveolae membrane system.
Annu Rev Biochem. 67:199–225. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yamada E: The fine structure of the gall
bladder epithelium of the mouse. J Biophys Biochem Cytol.
1:445–458. 1955. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cheng JPX and Nichols BJ: Caveolae: One
function or many? Trends Cell Biol. 26:177–189. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Martinez-Outschoorn UE, Sotgia F and
Lisanti MP: Caveolae and signalling in cancer. Nat Rev Cancer.
15:225–237. 2015. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Parton RG and Pozo MA: Caveolae as plasma
membrane sensors, protectors and organizers. Nat Rev Mol Cell Biol.
14:98–112. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ludwig A, Howard G, Mendoza-Topaz C,
Deerinck T, Mackey M, Sandin S, Ellisman MH and Nichols BJ:
Molecular composition and ultrastructure of the caveolar coat
complex. PLoS Biol. 11:e10016402013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Patel HH, Murray F and Insel PA: Caveolae
as organizers of pharmacologically relevant signal transduction
molecules. Annu Rev Pharmacol Toxicol. 48:359–391. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yao Q, Chen J, Cao H, Orth JD, McCaffery
JM, Stan RV and McNiven MA: Caveolin-1 interacts directly with
dynamin-2. J Mol Biol. 348:491–501. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mayor S, Parton RG and Donaldson JG:
Clathrin-independent pathways of endocytosis. Cold Spring Harb
Perspect Biol. 6:a0167582014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu P, Rudick M and Anderson RG: Multiple
functions of caveolin-1. J Biol Chem. 277:41295–41298. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Urra H, Torres VA, Ortiz RJ, Lobos L, Díaz
MI, Díaz N, Härtel S, Leyton L and Quest A: Caveolin-1-enhanced
motility and focal adhesion turnover require tyrosine-14 but not
accumulation to the rear in metastatic cancer cells. PLoS One.
7:e330852012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chatterjee M, Ben-Josef E, Thomas DG,
Morgan MA, Zalupski MM, Khan G, Andrew Robinson C, Griffith KA,
Chen CS, Ludwig T, et al: Caveolin-1 is associated with tumor
progression and confers a multi-modality resistance phenotype in
pancreatic cancer. Sci Rep. 5:108672015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hinshaw JE: Dynamin and its role in
membrane fission. Annu Rev Cell Dev Biol. 16:483–519. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Normanno N, De Luca A, Bianco C, Strizzi
L, Mancino M, Maiello MR, Carotenuto A, De Feo G, Caponigro F and
Salomon DS: Epidermal growth factor receptor (EGFR) signaling in
cancer. Gene. 366:2–16. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Basu Roy UK, Rial NS, Kachel KL and Gerner
EW: Activated K-RAS increases polyamine uptake in human colon
cancer cells through modulation of caveolar endocytosis. Mol
Carcinog. 47:538–553. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Feng H, Liu KW, Guo P, Zhang P, Cheng T,
McNiven MA, Johnson GR, Hu B and Cheng SY: Dynamin 2 mediates
PDGFRalpha-SHP-2-promoted glioblastoma growth and invasion.
Oncogene. 31:2691–2702. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Eppinga RD, Krueger EW, Weller SG, Zhang
L, Cao H and McNiven MA: Increased expression of the large GTPase
dynamin 2 potentiates metastatic migration and invasion of
pancreatic ductal carcinoma. Oncogene. 31:1228–1241. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Meng J: Distinct functions of dynamin
isoforms in tumorigenesis and their potential as therapeutic
targets in cancer. Oncotarget. 8:41701–41716. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Alshenawy HA and Ali MA: Differential
caveolin-1 expression in colon carcinoma and its relation to
E-cadherin-beta-catenin complex. Ann Diagn Pathol. 17:476–482.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Patlolla JM, Swamy MV, Raju J and Rao CV:
Overexpression of caveolin-1 in experimental colon adenocarcinomas
and human colon cancer cell lines. Oncol Rep. 11:957–963.
2004.PubMed/NCBI
|
|
22
|
Tanase CP: Caveolin-1: A marker for
pancreatic cancer diagnosis. Expert Rev Mol Diagn. 8:395–404. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sarwar MR and Saqib A: Cancer prevalence,
incidence and mortality rates in Pakistan in 2012. Cogent Med.
4:12887732017. View Article : Google Scholar
|
|
24
|
Robertson AG, Kim J, Al-Ahmadie H,
Bellmunt J, Guo G, Cherniack AD, Hinoue T, Laird PW, Hoadley KA,
Akbani R, et al: Comprehensive molecular characterization of
muscle-invasive bladder cancer. Cell. 171:540–556.e525. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhang X and Zhang Y: Bladder cancer and
genetic mutations. Cell Biochem Biophys. 73:65–69. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wang K, Liu T, Liu C, Meng Y, Yuan X, Liu
L, Ge N, Liu J, Wang C, Ren H, et al: TERT promoter mutations and
TERT mRNA but not FGFR3 mutations are urinary biomarkers in Han
Chinese patients with urothelial bladder cancer. Oncologist.
20:263–269. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhao M, He XL and Teng XD: Understanding
the molecular pathogenesis and prognostics of bladder cancer: An
overview. Chin J Cancer Res. 28:92–98. 2016.PubMed/NCBI
|
|
28
|
Rosenblatt R, Jonmarker S, Lewensohn R,
Egevad L, Sherif A, Kälkner KM, Nilsson S, Valdman A and Ullén A:
Current status of prognostic immunohistochemical markers for
urothelial bladder cancer. Tumour Biol. 29:311–322. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sever R and Brugge JS: Signal transduction
in cancer. Cold Spring Harb Perspect Med. 5:a0060982015. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Massey KA and Schnitzer JE: Caveolae and
cancer. Recent Results Cancer Res. 180:217–231. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Gupta R, Toufaily C and Annabi B: Caveolin
and cavin family members: Dual roles in cancer. Biochimie.
107:188–202. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chen D and Che G: Value of caveolin-1 in
cancer progression and prognosis: Emphasis on cancer-associated
fibroblasts, human cancer cells and mechanism of caveolin-1
expression (review). Oncol Lett. 8:1409–1421. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Soria F, Lucca I, Moschini M, Mathieu R,
Rouprêt M, Karakiewicz PI, Briganti A, Rink M, Gust KM, Hassler MR,
et al: Caveolin-1 as prognostic factor of disease recurrence and
survival in patients treated with radical cystectomy for bladder
cancer. Urol Oncol. 35:356–362. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Sanchez-Carbayo M, Socci ND, Lozano J,
Saint F and Cordon-Cardo C: Defining molecular profiles of poor
outcome in patients with invasive bladder cancer using
oligonucleotide microarrays. J Clin Oncol. 24:778–789. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Rosser CJ, Liu L, Sun Y, Villicana P,
McCullers M, Porvasnik S, Young PR, Parker AS and Goodison S:
Bladder cancer-associated gene expression signatures identified by
profiling of exfoliated urothelia. Cancer Epidemiol Biomarkers
Prev. 18:444–453. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Dyrskjot L, Zieger K, Kruhoffer M,
Thykjaer T, Jensen JL, Primdahl H, Aziz N, Marcussen N, Møller K
and Orntoft TF: A molecular signature in superficial bladder
carcinoma predicts clinical outcome. Clin Cancer Res. 11:4029–4036.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Gershenwald JE, Scolyer RA, Hess KR,
Sondak VK, Long GV, Ross MI, Lazar AJ, Faries MB, Kirkwood JM,
McArthur GA, et al: Melanoma staging: Evidence-based changes in the
American Joint Committee on cancer eighth edition cancer staging
manual. CA Cancer J Clin. 67:472–492. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Pan CC and Chang YH: The 2004 World Health
Organization/International Society of Urological Pathology
classification system for non-muscle-invasive bladder cancer. Urol
Sci. 24:96–100. 2013. View Article : Google Scholar
|
|
39
|
Zhang Y, Nolan M, Yamada H, Watanabe M,
Nasu Y, Takei K and Takeda T: Dynamin2 GTPase contributes to
invadopodia formation in invasive bladder cancer cells. Biochem
Biophys Res Commun. 480:409–414. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Ruan J and Weng ZL: Analysis of the
relationship between expression of caveolin-1 and prognosis in
bladder transitional cell carcinoma. Zhonghua Zhong Liu Za Zhi.
32:429–431. 2010.(In Chinese). PubMed/NCBI
|
|
41
|
Liang W, Hao Z, Han JL, Zhu DJ, Jin ZF and
Xie WL: CAV-1 contributes to bladder cancer progression by inducing
epithelial-to-mesenchymal transition. Urol Oncol. 32:855–863. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Spiess PE, Agarwal N, Bangs R, Boorjian
SA, Buyyounouski MK, Clark PE, Downs TM, Efstathiou JA, Flaig TW,
Friedlander T, et al: Bladder cancer, version 5.2017, NCCN clinical
practice guidelines in oncology. J Natl Compr Canc Netw.
15:1240–1267. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Rio DC, Ares M Jr, Hannon GJ and Nilsen
TW: Purification of RNA using TRIzol (TRI reagent). Cold Spring
Harb Protoc. 2010.pdb.prot5439, 2010. View Article : Google Scholar
|
|
44
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Bangaru ML, Park F, Hudmon A, McCallum JB
and Hogan QH: Quantification of gene expression after painful nerve
injury: Validation of optimal reference genes. J Mol Neurosci.
46:497–504. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Cancer. Net Editorial Board: Bladder
Cancer-Risk Factors. https://www.cancer.net/cancer-types/bladder-cancer/risk-factorsJune
25–2012
|
|
47
|
Aghbolaghi AG and Lechpammer M: A rare
case of centronuclear myopathy with DNM2 mutation:
Genotype-phenotype correlation. Autops Case Rep. 7:43–48. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Duregon E, Senetta R, Bertero L, Bussolati
B, Annaratone L, Pittaro A, Papotti M, Marchiò C and Cassoni P:
Caveolin 1 expression favors tumor growth and is associated with
poor survival in primary lung adenocarcinomas. Tumour Biol.
39:10104283176943112017. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Lee SW, Reimer CL, Oh P, Campbell DB and
Schnitzer JE: Tumor cell growth inhibition by caveolin
re-expression in human breast cancer cells. Oncogene. 16:1391–1397.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Lin M, DiVito MM, Merajver SD, Boyanapalli
M and van Golen KL: Regulation of pancreatic cancer cell migration
and invasion by RhoC GTPase and Caveolin-1. Mol Cancer. 4:212005.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Friedl P and Alexander S: Cancer invasion
and the microenvironment: Plasticity and reciprocity. Cell.
147:992–1009. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Kang HW, Kim WJ and Yun SJ: The role of
the tumor microenvironment in bladder cancer development and
progression. Transl Cancer Res. 6 (Suppl):S744–S758. 2017.
View Article : Google Scholar
|
|
53
|
Sotgia F, Martinez-Outschoorn UE, Howell
A, Pestell RG, Pavlides S and Lisanti MP: Caveolin-1 and cancer
metabolism in the tumor microenvironment: Markers, models, and
mechanisms. Annu Rev Pathol. 7:423–467. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Wang M, Zhao J, Zhang L, Wei F, Lian Y, Wu
Y, Gong Z, Zhang S, Zhou J, Cao K, et al: Role of tumor
microenvironment in tumorigenesis. J Cancer. 8:761–773. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Nwosu ZC, Ebert MP, Dooley S and Meyer C:
Caveolin-1 in the regulation of cell metabolism: A cancer
perspective. Mol Cancer. 15:712016. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Diaz-Valdivia N, Bravo D, Huerta H,
Henriquez S, Gabler F, Vega M, Romero C, Calderon C, Owen GI,
Leyton L and Quest AF: Enhanced caveolin-1 expression increases
migration, anchorage-independent growth and invasion of endometrial
adenocarcinoma cells. BMC Cancer. 15:4632015. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Girard E, Paul JL, Fournier N, Beaune P,
Johannes L, Lamaze C and Védie B: The Dynamin Chemical Inhibitor
Dynasore Impairs Cholesterol Trafficking and Sterol-Sensitive Genes
Transcription in Human HeLa Cells and Macrophages. PLoS One.
6:e290422011. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Lee YY, Jeon HK, Lee J, Do IG, Choi CH,
Kim TJ, Kim BG, Bae DS, Kim YC and Lee JW: Dynamin 2 inhibitors as
novel therapeutic agents against cervical cancer cells. Anticancer
Res. 36:6381–6388. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Galbiati F, Volonte D, Liu J, Capozza F,
Frank PG, Zhu L, Pestell RG and Lisanti MP: Caveolin-1 expression
negatively regulates cell cycle progression by inducing G(0)/G(1)
arrest via a p53/p21(WAF1/Cip1)-dependent mechanism. Mol Biol Cell.
12:2229–2244. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Nunez-Wehinger S, Ortiz RJ, Diaz N, Diaz
J, Lobos-Gonzalez L and Quest AF: Caveolin-1 in cell migration and
metastasis. Curr Mol Med. 14:255–274. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Sun DS, Hong SA, Won HS, Yoo SH, Lee HH,
Kim O and Ko YH: Prognostic value of metastatic tumoral caveolin-1
expression in patients with resected gastric cancer. Gastroenterol
Res Pract. 2017:59051732017. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Ge Z, Gu Y, Han Q, Zhao G, Li M, Li J,
Chen B, Sun T, Dovat S, Gale RP and Song C: Targeting HIGH
DYNAMIN-2 (DNM2) expression by restoring ikaros function in acute
lymphoblastic leukemia. Sci Rep. 6:380042016. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Quest AF, Gutierrez-Pajares JL and Torres
VA: Caveolin-1: An ambiguous partner in cell signalling and cancer.
J Cell Mol Med. 12:1130–1150. 2008. View Article : Google Scholar : PubMed/NCBI
|