Introduction
Glioma is a malignant tumor that is a threat to
human health, with a median survival time of only 14.6–17 months
for World Health Organization grade IV gliomas and an incidence
rate of ~5/100,000 in China in 2011 (1,2).
Chemotherapy remains the major therapeutic method for glioma
treatment (3,4). Currently, temozolomide (TMZ) is used
clinically for the treatment of glioma; however, its clinical
application is limited due to toxicity (5). Therefore, a number of studies have been
initiated with the aim of developing a new antitumor drug with
reduced toxicity (6,7).
A number of lipid synthesis-associated genes are
involved in tumorigenesis (8).
Previous studies have indicated that alkylglycerone phosphate
synthase (AGPS) is a critical enzyme in ether lipids synthesis and
it is upregulated in several types of cancer cells and primary
tumors. It increases the malignancy of many types of tumor,
including prostate cancer, melanoma, breast cancer and glioma by
altering the balance of structural and signaling lipids which
affect cancer pathogenicity (9).
Therefore, the present research team hypothesized that AGPS may be
a viable target for anticancer drugs, and designed and synthesized
anovel series of AGPS-targeting carboxamide derivatives by
computer-aided drug design (10,11).
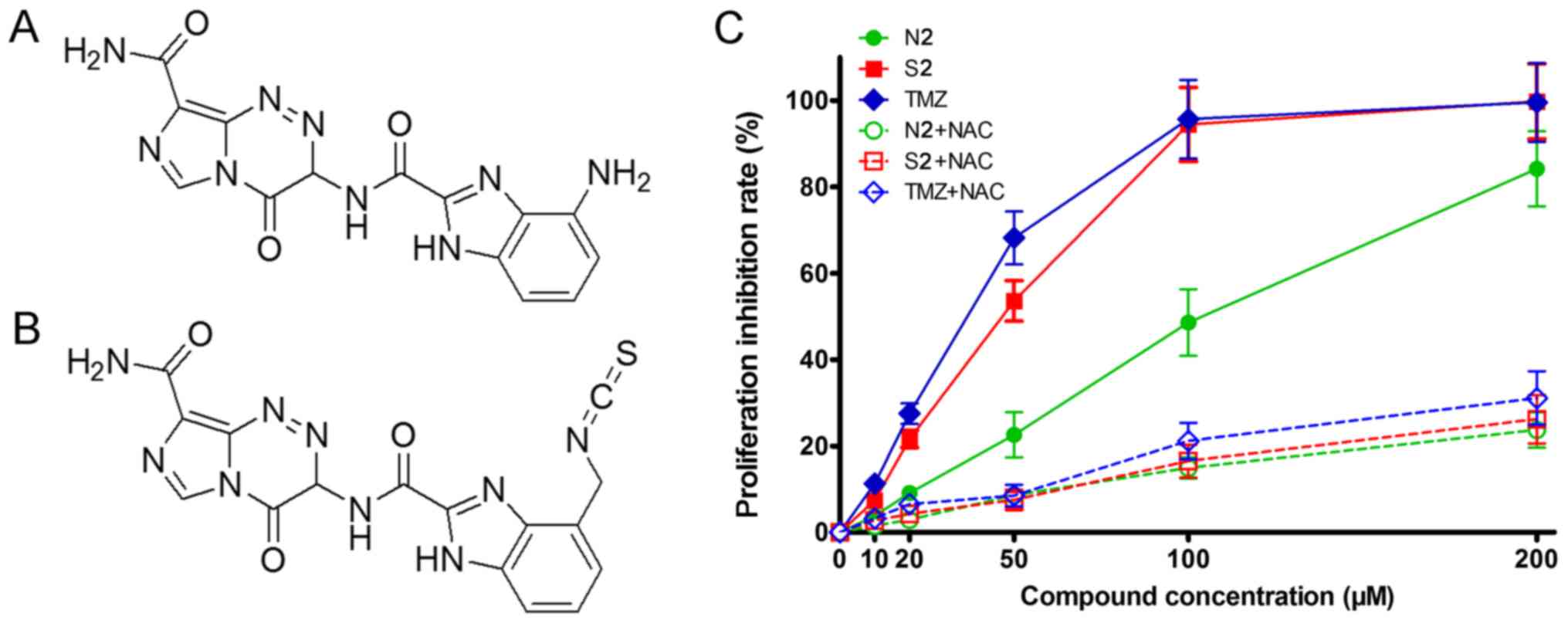
These derivatives include N2 and S2 (Fig. 1A and B).
There is an excellent docking score of N2 and S2 in
our previous study (10). To examine
the potential of these derivatives as novel anti-glioma drugs,
their effects on glioma cells were examined in this study, in
comparison with TMZ, and the mechanism underlying their effects was
investigated.
Materials and methods
Compounds, cell lines and culture
The compounds N2 and S2 were synthesized by Werian
Biotech Co. (Jinan, China). Human glioma U251 and H4 cell lines and
the PC12 rat pheochromocytoma cell line were purchased from the
American Type Culture Collection (Manassas, VA, USA). The U251 and
H4 cell lines were cultured in DMEM with 10% fetal bovine serum
(Gibco; Thermo Fisher Scientifc, Inc., Waltham, MA, USA),
penicillin (100 U/ml) and streptomycin (100 mg/ml) at 37°C and 5%
CO2. The PC12 cell line was cultured in Ham's F12K
(Gibco; Thermo Fisher Scientifc, Inc.) with 10% fetal bovine serum,
penicillin (100 U/ml) and streptomycin (100 mg/ml) at 37°C and 5%
CO2.
MTS assays
U251, H4 and PC12 cells were cultured on 96-well
plates (3×103/well) overnight. Different concentrations
(0, 10, 20, 50, 100 and 200 µM) of N2, S2 and TMZ (Sigma-Aldrich;
Merck KGaA) were added to the cells, which were then cultured for
72 h at 37°C. A total of 20 µl MTS was added and cells were
cultured for 4 h at 37°C. The optical density (OD) was then
measured at a wavelength of 490 nm. Inhibition percentage was
calculated as=(1-OD valuetreatment group/OD value 0
µM) ×100. 20 µM of the antioxidant N-acetyl-L-cysteine (NAC)
(Beyotime Institute of Biotechnology) was added with N2, S2 and
TMZ.
Flow cytometry assay
U251 cells (2×105/well) were cultured in
6-wellplates. The cells were cultured with N2 (50 and 80 µM), S2
(20 and 30 µM) or TMZ (10 and 20 µM) for 72 h at 37°C. Cells were
then collected, and apoptosis was assessed using the Annexin
V-FITC/PI kit (BD Biosciences, Franklin Lakes, NJ, USA), according
to the manufacturer's protocol, with incubation for 15 min at room
temperature in the dark. Apoptosis was measured by flow cytometry
(FACSAria; BD Biosciences) at a wavelength of 488 nm by Diva
software (version 8.0.1; FACSAria; BD Biosciences).
Reactive oxygen species (ROS)
assay
ROS are responsible for oxidative damage (12). U251 cells (2×105/well)
were cultured in 6-well plates. Following the addition of N2 (25
and 40 µM), S2 (10 and 15 µM) or TMZ (5 and 10 µM), the cells were
cultured for 72 h at 37°C. The cells were then collected and
stained with 2,7-dichlorodihydrofluorescein diacetate (Beyotime
Institute of Biotechnology). ROS were quantified using a microplate
reader at a wavelength of 488 nm.
Caspase-3, −8 and −9 activity
assays
U251cells (2×105/well) were cultured in
6-wellplates with N2 (25 and 40 µM), S2 (10 and 15 µM) or TMZ (5
and 10 µM) for 72 h at 37°C. The caspase-3, −8 and −9activities of
the cells were then measured using caspase detection kits (cat.
nos. 93, 99 and 912; Immunochemistry Technologies, LLC), with a
microplate reader at a wavelength of 488 nm.
Western blot analysis
U251 cells (2×105/well) were cultured in
a6-well plate with N2 (25 and 40 µM), S2 (10 and 15 µM) or TMZ (5
and 10 µM) for 72 h at 37°C. The cells were then lysed using cell
lysis buffer (Beyotime Institute of Biotechnology), containing 20
mM Tris (pH 7.5), 150 mM NaCl and 1% Triton X-100, and total
proteins were extracted. A total of 50 µg protein/lane determined
by BCA Protein Assay Kit (Beyotime Institute of Biotechnology) was
separated via 12% SDS-PAGE and transferred onto a polyvinylidene
fluoride membrane. The membrane was then blocked using 1% bovine
serum albumin (Beyotime Institute of Biotechnology) for 1 h at
37°C. The membrane was incubated with Bcl-2 (Santa Cruz
Biotechnology, Inc., Santa Cruz, CA, USA; cat. no. sc-7382;
1:1,500) and survivin (Santa Cruz Biotechnology, Inc.; cat. no.
sc-101433; 1:1,500) antibodies overnight at 4°C, and then incubated
for 1 h at 37°C with mouse anti-rabbit IgG-HRP (Santa Cruz
Biotechnology, Inc.; cat. no. sc-2357; 1:2,000). The membrane was
visualized using Immobilon Western chemiluminescent horseradish
peroxidase substrate (EMD Millipore, Billerica, MA, USA). β-actin
(Santa Cruz Biotechnology, Inc.; cat. no. sc-81178; 1:5,000) was
used as the loading control. Quantification was performed using
Image J software (version 1.8.0; National Institutes of Health,
Bethesda, MD, USA).
Reverse transcription-quantitative PCR
(RT-qPCR) assay
U251 cells (2×105/well) were cultured in
6-well plates with N2 (25 and 40 µM), S2 (10 and 15 µM) or TMZ (5
and 10 µM) for 72 h at 37°C. Total RNA was extracted using TRIzol
(Thermo Fisher Scientific, Inc., Waltham, MA, USA). Total RNA was
reverse transcribed using BeyoFast™ SYBR Green qPCR Mix kit
including reverse transcriptase, buffer and dNTPs (Beyotime
Institute of Biotechnology) and expression of the target genes were
detected using a qPCR assay (cat. no. ABI7500; Applied Biosystems;
Thermo Fisher Scientific, Inc.) with the following conditions:
Denaturation at 95°C for 10 min, followed by 40 cycles at 95°C for
15 sec, 60°C for 60 sec and a final extension step at 95°Cfor 15
sec. Expression was normalized to β-actin. The full details of the
primers used in these experiments are shown in Table I. The quantified results were
calculated using the 2−ΔΔCq method (13).
 | Table I.Primer sequences used in reverse
transcription-quantitative PCR. |
Table I.
Primer sequences used in reverse
transcription-quantitative PCR.
| Gene | Primers |
|---|
| Bcl-2 | Forward:
5′-CGTACAGTTCCACAAAGGCA-3′ |
|
| Reverse:
5′-ATGTGTGTGGAGAGCGTCAA-3′ |
| Survivin | Forward:
5′-TCCGCAGTTTCCTCAAATTC-3′ |
|
| Reverse:
5′-GTTGCGCTTTCCTTTCTGTC-3′ |
| β-actin | Forward:
5′-AGGCACCAGGGCGTGAT-3′ |
|
| Reverse:
5′-GCCCACATAGGAATCCTTCTGAC-3′ |
Statistical analysis
Experimental data is presented as the mean ±
standard deviation of three experimental repeats. SPSS statistical
software (version 11.0; IBM Corp., Armonk, NY, USA) was used to
perform a one-way analysis of variance with the least significant
difference post hoc test. P≤0.05 was considered to indicate a
statistically significant difference.
Results
Effects of carboxamide derivatives on
the proliferation of U251 cells
The MTS assay results revealed that the carboxamide
derivatives and TMZ inhibited the proliferation of U251, H4 and
PC12 cells. However, the antiproliferative effect of the
carboxamide derivatives was decreased compared with that of TMZ, as
revealed by their higherhalf maximal inhibitory concentrations
(Table II). This indicates that the
carboxamide derivatives had a lower toxicity compared with TMZ. The
MTS assay also revealed that the inhibition of proliferation by S2
and N2 was significantly decreased by NAC in U251 cells, suggesting
that the activity of the carboxamide derivatives may partly involve
oxidative damage (Fig. 1C). The
non-toxic doses (inhibition rate <10%) for N2 (25 µM), S2 (10
µM) and TMZ (5 µM), and low-toxicity doses (inhibition rate
<15%) for N2 (40 µM), S2 (15 µM) and TMZ (10 µM), were taken
forward to the following experiments, with the exception of the
apoptosis assay, to avoid inhibiting cell proliferation. A 0 µM
concentration was included as the control group.
 | Table II.IC50 values of carboxamide
derivatives and TMZ in PC12, H4 and U251 cell lines. |
Table II.
IC50 values of carboxamide
derivatives and TMZ in PC12, H4 and U251 cell lines.
|
| IC50
(µM) |
|---|
|
|
|
|---|
| Compound | PC12 | H4 | U251 |
|---|
| N2 | 87.6 | 108.3 | 122.7 |
| S2 | 42.3 | 53.8 | 47.4 |
| TMZ | 34.3 | 42.8 | 37.5 |
Carboxamide derivatives are inducers
of apoptosis and oxidative damage inU251 cells
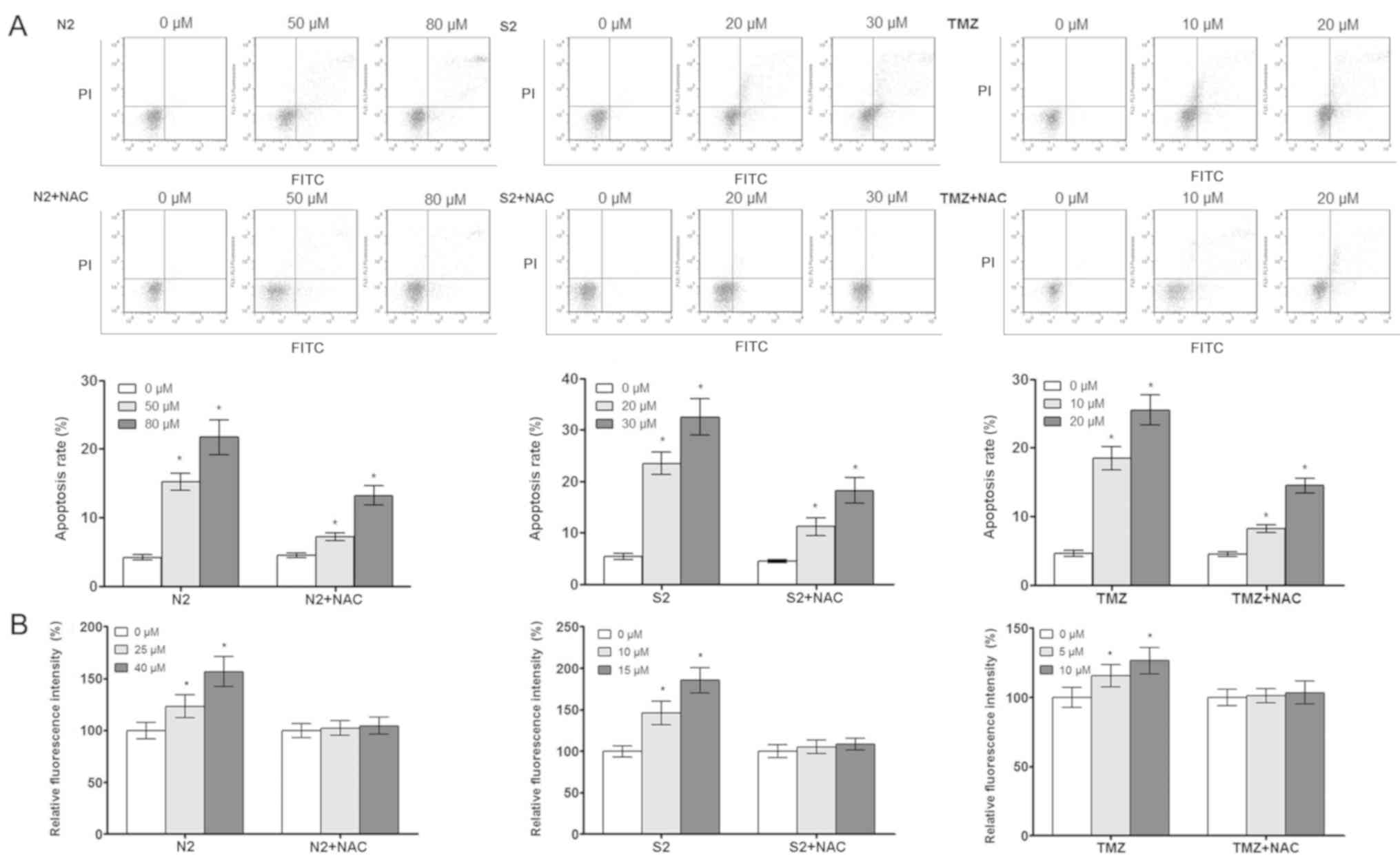
The flow cytometry and ROS assay results show that
the carboxamide derivatives induced apoptosis (Fig. 2A) and oxidative damage (Fig. 2B) in the U251 cells, indicating that
the carboxamide derivatives may suppress the proliferation of U251
cells via these mechanisms. The ROS-inducing effects of N2 and S2
were eliminated by 20 µM NAC (Fig.
2B), further supporting the suggestion that oxidative damage
may be an important mechanism for the antitumor activity of these
compounds.
Effects of carboxamide derivatives on
caspase activity and apoptosis-associated mRNA in U251 cells
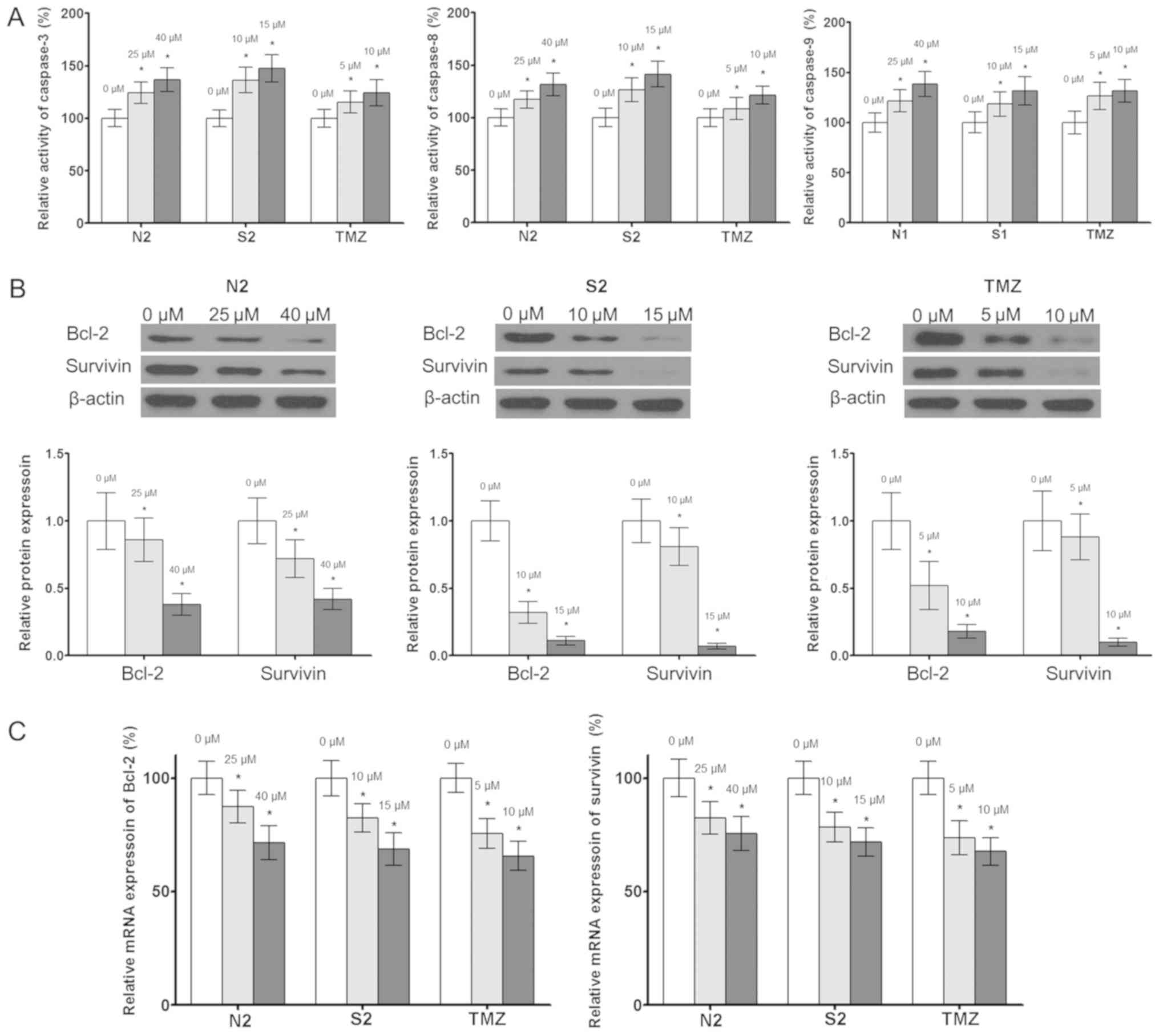
The results of the caspase-3, −8 and −9 activity
assays demonstrated that the carboxamide derivatives were able to
induce caspase-3, −8 and −9 activity (Fig. 3A). In addition, western blotting and
RT-qPCR results indicated that the carboxamide derivatives reduced
the protein (Fig. 3B) and mRNA
(Fig. 3C) expression levels of Bcl-2
and survivin in U251 cells. This indicates that these carboxamide
derivatives may induce the apoptosis of U251 cells by altering the
activity of caspases-3, −8 and 9, and the expression of
apoptosis-associated genes.
Discussion
TMZ is a common anti-glioma drug used worldwide;
however, its toxicity is a limitation for clinical application
(14,15). Therefore, the aim of the present
study was to develop novel compounds with lower toxicity in order
to reduce the side-effects of antitumor treatment.
The activity of two carboxamide derivatives as
inhibitors of cell proliferation was investigated, and it was found
that N2 in particular displayed reduced inhibitory activity
compared with TMZ, suggesting the carboxamide derivatives may have
potential as drugs with lower toxicity.
‘Survival with tumor’ is a novel tumor therapeutics
concept in which the aim is not to kill all tumor cells, but to
improve the quality of life of the patient and enable them to
survive with the tumor via a less toxic treatment with fewer side
effects (16). With this idea in
mind, carboxamide derivative N2 and the structurally similar
compound S2were selected from two series of AGPS-targeting
carboxamide derivatives, and their anti-glioma activity in the U251
cell line was measured. The mechanism of these carboxamide
derivatives was also investigated.
The inhibitory effect of N2, S2 and TMZ on the
proliferation of U251, H4 and PC12 cells was measured, and the
results indicated that the inhibitory activity of N2 was markedly
reduced compared with that of S2 and TMZ in all cell lines,
indicating its potential to be used for ‘survival with tumor’
treatment.
Apoptosis is an important mechanism of action of
antitumor drugs (17). The mechanism
underlying the effects of carboxamide derivatives on the
proliferation of glioma cells was examined, and the flow cytometric
quantification of TUNEL staining indicated that the carboxamide
derivatives could induce the apoptosis of U251 cells. Therefore, it
was speculated that apoptosis may be one of the mechanisms by which
carboxamide derivatives suppress the growth of glioma cells. Bcl-2
and survivin are apoptosis resistance genes, and the expression of
both is increased in tumor cells, which affects the activity of
antitumor drugs with the inactivation of caspases (18,19). The
present study demonstrated that Bcl-2 and survivin expression
levels were suppressed, and the activities of caspase-3, −8 and −9
were increased in U251 cells following treatment with the
carboxamide derivatives N2 and S2, indicating that the carboxamide
derivatives induce apoptosis via the regulation of
apoptosis-associated genes.
Oxidative damage is one of major mechanisms by which
apoptosis is induced (20,21). The present study indicated that
carboxamide derivatives induce the oxidative damage of U251 cells,
and their oxidative activity was attenuated by the antioxidant NAC
(22), indicating the effect of the
compound partially involved the triggering of oxidative stress.
Furthermore, it was observed that there was greater inhibition of
proliferation and oxidative damage with compound S2 compared with
N2. It is speculated that the stronger oxidative effect of S2 may
be associated with the isothiocyanate group, which is reported to
possess strong oxidation activity (23,24). The
cell cycle also has an effect on cell proliferation, and further
studies of the effects of carboxamide derivatives on the cell cycle
remain to be performed. However, a limitation of the present study
is that a rat cell line, not a human cell line, was used as the
normal control.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant no. 81200957).
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
LH conceived and designed the study. JZ acquired the
data. TY performed the data analysis.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cioca A, Olteanu EG, Gisca MD, Morosanu
CO, Marin I and Florian IS: Expression of EGFR in paired new and
recurrent glioblastomas. Asian Pac J Cancer Prev. 9:4205–4208.
2016.
|
|
2
|
Li C, Sun J, Xiang Q, Liang Y, Zhao N,
Zhang Z, Liu Q and Cui Y: Prognostic role of microRNA-21 expression
in gliomas: A meta-analysis. J Neurooncol. 130:11–17. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang N, Zhang Q, Ning B, Luo L and Fang Y:
β-Asarone promotes Temozolomide's entry into glioma cells and
decreases the expression of P-glycoprotein and MDR1. Biomed
Pharmacother. 90:368–374. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Narayan RS, Fedrigo CA, Brands E, Dik R,
Stalpers LJ, Baumert BG, Slotman BJ, Westerman BA, Peters GJ and
Sminia P: The allosteric AKT inhibitor MK2206 shows a synergistic
interaction with chemotherapy and radiotherapy in glioblastoma
spheroid cultures. BMC Cancer. 17:2042017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bureta C, Saitoh Y, Tokumoto H, Sasaki H,
Maeda S, Nagano S, Komiya S, Taniguchi N and Setoguchi T:
Synergistic effect of arsenic trioxide, vismodegib and temozolomide
on glioblastoma. Oncol Rep. 6:3404–3412. 2019.
|
|
6
|
Tang J, Zhou H, Hou X, Wang L, Li Y, Pang
Y, Chen C, Jiang G and Liu Y: Enhanced anti-tumor efficacy of
temozolomide-loaded carboxylated poly(amido-amine) combined with
photothermal/photodynamic therapy for melanoma treatment. Cancer
Lett. 423:16–26. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Коbylinska LI, Klyuchivska OY, Grytsyna
II, Finiuk N, Panchuk RR, Starykovych MO, Lehka L, Lesyk RB,
Zіmenkovsky BS and Stoika RS: Differential pro-apoptotic effects of
synthetic 4-thiazolidinone derivative Les-3288, doxorubicin and
temozolomide in human glioma U251 cells. Croat Med J. 58:150–159.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Piano V, Benjamin DI, Valente S, Nenci S,
Marrocco B, Mai A, Aliverti A, Nomura DK and Mattevi A: Discovery
of inhibitors for the ether Lipid-generating enzyme AGPS as
Anti-cancer agents. ACS Chem Biol. 11:2589–2597. 2015. View Article : Google Scholar
|
|
9
|
Zhu Y, Zhu L, Lu L, Zhang L, Zhang G, Wang
Q and Yang P: Role and mechanism of the alkylglycerone phosphate
synthase in suppressing the invasion potential of human glioma and
hepatic carcinoma cells in vitro. Oncol Rep. 32:431–436.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yang B, Li X, He L and Zhu Y:
Computer-aided design of temozolomide derivatives based on
alkylglycerone phosphate synthase structure with isothiocyanate and
their pharmacokinetic/toxicity prediction and anti-tumor activity
in vitro. Biomed Rep. 8:235–240. 2018.PubMed/NCBI
|
|
11
|
Zhu Y, Han Y, Ma Y and Yang P:
ADME/toxicity prediction and antitumor activity of novel
nitrogenous heterocyclic compounds designed by computer targeting
of alkylglycerone phosphate synthase. Oncol Lett. 16:1431–1438.
2018.PubMed/NCBI
|
|
12
|
Xu N, Kan P, Yao X, Yang P, Wang J, Xiang
L and Zhu Y: Astragaloside IV reversed the autophagy and oxidative
stress induced by the intestinal microbiota of AIS in mice. J
Microbiol. 56:838–846. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen TC, Cho HY, Wang W, Wetzel SJ, Singh
A, Nguyen J, Hofman FM and Schönthal AH: Chemotherapeutic effect of
a novel temozolomide analog on nasopharyngeal carcinoma in vitro
and in vivo. J Biomed Sci. 22:712015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Iorio AL, da Ros M, Genitori L, Lucchesi
M, Colelli F, Signorino G, Cardile F, Laffi G, de Martino M, Pisano
C and Sardi I: Tumor response of temozolomide in combination with
morphine in a xenograft model of human glioblastoma. Oncotarget.
52:89595–89606. 2017.
|
|
16
|
Sousa F, Moura RP, Moreira E, Martins C
and Sarmento B: Therapeutic monoclonal antibodies delivery for the
glioblastoma treatment. Adv Protein Chem Struct Biol. 112:61–80.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Vellanki SH, Cruz RGB, Richards CE, Smith
YE, Hudson L, Jahns H and Hopkins AM: Antibiotic Tetrocarcin-A
Down-regulates JAM-A, IAPs and induces apoptosis in triple-negative
breast cancer models. Anticancer Res. 39:1197–1204. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bae IS, Kim CH, Kim JM, Cheong JH, Ryu JI
and Han MH: Correlation of survivin and B-cell lymphoma 2
expression with pathological malignancy and anti-apoptotic
properties of glial cell tumors. Biomed Rep. 4:396–400. 2017.
View Article : Google Scholar
|
|
19
|
Karpel-Massler G, Banu MA, Shu C, Halatsch
ME, Westhoff MA, Bruce JN, Canoll P and Siegelin MD: Inhibition of
deubiquitinases primes glioblastoma cells to apoptosis in vitro and
in vivo. Oncotarget. 7:12791–12805. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sharma N, Colangelo NW, de Toledo SM and
Azzam EI: Diffusible factors secreted by glioblastoma and
medulloblastoma cells induce oxidative stress in bystander neural
stem progenitors. ASN Neuro. 8(pii):
17590914166628082016.PubMed/NCBI
|
|
21
|
Nakayama N, Yamaguchi S, Sasaki Y and
Chikuma T: Hydrogen Peroxide-induced oxidative stress activates
proteasomal Trypsin-like activity in human U373 glioma cells. J Mol
Neurosci. 58:297–305. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yan H, Zhu Y, Liu B, Wu H, Li Y, Wu X,
Zhou Q and Xu K: Mitogen-activated protein kinase mediates the
apoptosis of highly metastatic human non-small cell lung cancer
cells induced by isothiocyanates. Br J Nutr. 12:1779–1791. 2011.
View Article : Google Scholar
|
|
23
|
Jiang B, Xin S, Liu Y, He H, Li L, Tang Y,
Luo S and Bi X: The role of thiocyanate in enhancing the process of
sulfite reducing Cr(VI) by inhibiting the formation of reactive
oxygen species. J Hazard Mater. 343:1–9. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tarozzi A, Morroni F, Bolondi C, Sita G,
Hrelia P, Djemil A and Cantelli-Forti G: Neuroprotective effects of
erucin against 6-hydroxydopamine-induced oxidative damage in a
dopaminergic-like neuroblastoma cell line. Int J Mol Sci.
13:10899–10910. 2012. View Article : Google Scholar : PubMed/NCBI
|